Abstract
The 12‐item World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) is a brief measurement tool used cross‐culturally to capture the multi‐dimensional nature of disablement through six domains, including: understanding and interacting with the world; moving and getting around; self‐care; getting on with people; life activities; and participation in society. Previous psychometric research supports that the WHODAS 2.0 functions as a general factor of disablement. In a pooled dataset from community samples of adults (N = 447) we used confirmatory factor analysis to confirm a one‐factor structure. Latent class analysis was used to identify subgroups of individuals based on their patterns of responses. We identified four distinct classes, or patterns of disablement: (1) pervasive disability; (2) physical disability; (3) emotional, cognitive, or interpersonal disability; (4) no/low disability. Convergent validity of the latent class subgroups was found with respect to socio‐demographic characteristics, number of days affected by disabilities, stress, mental health, and substance use. These classes offer a simple and meaningful way to classify people with disabilities based on the 12‐item WHODAS 2.0. Focusing on individuals with a high probability of being in the first three classes may help guide interventions.
Keywords: confirmatory factor analysis (CFA), disability, latent class analysis (LCA), WHODAS
1. INTRODUCTION
The World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0; Üstün, Kostanjsek, Chatterji, & Rehm, 2010b) was developed with the goal of moving beyond diagnosing a person with a mental health problem to improving understanding of the impact of the disease on a person's functioning, ability and quality of life (Üstün & Chatterji, 1998; Üstun et al., 2001). Unlike other assessments which have combined distinct concepts such as disability, psychiatric symptomology, social support, and subjective well‐being into one measure, the WHODAS 2.0 focuses on disability (Rehm et al., 1999) based on the International Classification of Functioning, Disability and Health (ICF) [International Classification of Impairments, Disabilities, and Handicaps (ICIDH); Üstun et al., 2001; World Health Organization, 1980, 1997, 2001]. The WHODAS 2.0 captures the multi‐dimensional nature of disablement (Rehm et al., 1999; Üstün et al., 2010a; Üstün et al., 2010b), including items from six domains: understanding and communicating with the world; moving and getting around; self‐care; getting along with people; life activities (domestic responsibilities, leisure, work and school); and participation in community activities (Rehm et al., 1999). The WHODAS 2.0 is noted for its usefulness in population surveys, monitoring health outcomes and evaluating treatment effects (Üstün et al., 2010a).
The WHODAS 2.0 was developed for broad applicability across cultures and subpopulations. It originally consisted of 96 items and was subsequently reduced to a 36‐item inventory based on both classical test theory and item response theory (Üstün et al., 2010b). A short 12‐item screener version of the WHODAS 2.0 was developed for use as a brief assessment of overall functioning. It includes items across the six domains of the 36‐item WHODAS and has been found to explain 81% of the variance of the full WHODAS 2.0 and to identify over 90% of individuals with disabilities on the full scale (Üstün et al., 2010b). The 12‐item scale was supported for use across cultures, sexes, age groups, and types of health conditions (Üstün et al., 2010b). However, although extensive psychometric evaluations have been conducted for the full 36‐item WHODAS 2.0 (Üstün et al., 2010b) there remains a relative paucity of research on the 12‐item screener, especially outside of clinical settings.
Research examining the psychometric properties of the 12‐item WHODAS 2.0 has been conducted in primary care patients with a first major depressive episode (Luciano et al., 2010a, 2010b), patients with myocardial infarction (Kirchberger, Braitmayer, Coenen, Oberhauser, & Meisinger, 2014), neurosurgical patients (Schiavolin et al., 2014), trauma patients (Abedzadeh‐Kalahroudi, Razi, Sehat, & Asadi‐Lari, 2016), patients with chronic musculoskeletal pain (Saltychev et al., 2016), and older adults from low‐ and middle‐income countries (Sousa et al., 2010). This research has demonstrated high internal consistency, construct validity, convergent and discriminant validity, and no bias in the way participants respond to items based on gender, age, education, marital status, presence of comorbidities, overall health status, and smoking status. That is, when these groups (e.g. older and younger individuals) had the same level of disability, they responded to items in the same way.
Furthermore, these studies largely support a one‐factor solution which points to a general factor of disablement rather than a multidimensional structure. However, latent class analysis (LCA) can uncover other patterns that may exist. For example, subgroups of people may score high on only a subset of items such as cognitive disablement, whereas others may score high on the full set of items. Identifying distinct classes of individuals (i.e. different subgroups based on their patterns of responses) can be useful for delineating subtypes of disability patterns, which may have important implications for screening and treatment. To our knowledge, no research has investigated patterns of disablement in the adult population.
In a pooled dataset of community samples of adults, the main objectives of this study were:
to use confirmatory factor analysis (CFA) to determine whether a one factor solution fits the data, as has been found previously in the literature;
to investigate the structure of responses to the 12 items in terms of prototypical profiles using LCA;
to evaluate the convergent validity of latent class subgroups with respect to socio‐demographic variables as well as number of days affected by disabilities and measures of stress, mental health and substance use.
2. METHODS
2.1. Participants
The present analyses were based on data collected in four studies conducted as part of a multidisciplinary team project, Researching Health in Ontario Communities, which tested innovative methods for studying mental health, substance use and violence problems in diverse communities using a mobile research laboratory (Wells et al., 2011). Four studies were conducted in four communities of varying sizes (populations of approximately 18,000 to over 200,000) in southern Ontario, Canada.
The Consumer Journey study (n = 132 consumers, 68 family members) recruited adults (aged 18 and over) who had mental health and/or substance use problems and had sought treatment for either or both type of problem (i.e. consumers) and family members of consumers through posters placed in local treatment agencies and other public settings in four communities. Interviews were conducted to better understand experiences of seeking and receiving care for people who have mental health and/or substance use problems.
The Valuations of Health States study (n = 101) assessed perceptions regarding the disabling effects of different health conditions in two communities. Adults (aged 18 and over) were recruited using advertisements and posters placed at various locations in the community requesting volunteers who “sometimes feel sad or blue or think you drink too much.”
The Communication and Conflict and Young Adults study (n = 58) recruited young adults (aged 18–29) to examine conflict in intimate partner relationships in two communities. Participants were recruited using respondent‐driven sampling, a form of chain referral or snowball sampling involving recruitment of a small number of initial participants known as “seeds” who then recruit additional eligible participants (Heckathorn, 1997). The seeds were recruited using posters in public places or were approached at a local shopping mall and asked to participate.
The Random Walk study (n = 92) used a modified “random walk” strategy to generate a random sample of the general population in one community. This involved a two‐stage cluster sampling design, with the random selection of blocks using Canadian census data and the random selection of households within blocks (Flynn, Tremblay, Rehm, & Wells, 2013).
All participants, regardless of the study, completed a core questionnaire which included a wide range of questions relating to stress and mental health. The combined sample included 451 participants; however from people were excluded from the LCA due to missing data needed to calculate probability of membership in each class (N = 447). The diversity of this pooled sample is considered ideal for factor analytic studies because it increases variance in the variables (Kline, 1994).
2.2. Self‐report measures
2.2.1. Disability
To assess disablement or daily functioning, the 12‐item WHODAS 2.0 was used (Üstün et al., 2010b). Items are rated on the extent of difficulty doing the activity in the past 30 days on 5‐point scales (none, mild, moderate, severe, extreme/cannot do). To facilitate estimation in the latent class analyses, the items were dichotomized: (1) none/mild versus (2) moderate/extreme/cannot do.
2.2.2. Number of days affected by disabilities
As part of the WHODAS 2.0, three additional questions were included to assess the extent of burden of disabilities. Specifically, participants were asked how many days difficulties were present, how many days participants were totally unable to carry out usual activities or work because of any health condition, and how many days they had to cut back or reduce usual activities or work because of any health condition.
2.2.3. Stress
Stress was measured with the 10‐item Perceived Stress Scale (PSS; Cohen, Kamarck, & Mermelstein, 1983) which asks about frequency of stress in the previous month. Each item ranges from 0 = never to 4 = very often with a total score ranging from 0 to 40. A 17‐item Chronic Stress Scale composed of yes/no questions (ranging from 0 to 17) was also used. This scale captures ongoing stress in a person's life and uses several items from Turner, Wheaton, and Lloyd (1995), as used by Shields (2004).
2.2.4. Mental health
The Diagnostic and Statistical Manual of Mental Disorders, Fourth edition (DSM‐IV) University of Michigan version of the Composite International Diagnostic Interview (UM‐CIDI) was used to measure depression, from which two variables were computed: (1) meeting criteria for a diagnosis of major depression (based on a score of three or higher) and (2) total score (ranging from 0 to 7) (Kessler, Andrews, Mroczek, Ustun, & Wittchen, 1998). For anxiety, two screener items from the CIDI Short Form were used, with endorsement of both indicating anxiety problems.
2.2.5. Substance use
For prescription drug use, respondents were asked whether they had used antidepressants or sedatives/tranquilizers in the previous 12 months. To assess hazardous/harmful alcohol consumption, the 10‐item Alcohol Use Disorders Identification Test (AUDIT) was used (Saunders, Aasland, Babor, De La Fuente, & Grant, 1993). The total score was used in addition to a cutoff of 16 or more to indicate harmful drinking. Because the total AUDIT score is largely driven by responses to the first three items on alcohol consumption (Bernards, Graham, Demers, Kairouz, & Wells, 2007), we calculated two subscores on the AUDIT: (1) consumption and (2) alcohol dependence/consequences (Babor, Higgins‐Biddle, Saunders, & Monteiro, 2001). For tobacco use, participants were asked whether they were a current smoker and usual number of cigarettes smoked per day (Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989). They were also asked about any marijuana use and use of other illicit drugs in the previous 12 months.
2.3. Analysis
CFA of the items was conducted in Mplus 6.12 (Muthén & Muthén, 1998–2012) with a weighted least squares estimator using mean and variance adjusted chi‐square test statistics (WLSMV). The “categorical” outcome variable option was specified to indicate that items were measured on an ordered discrete category “scale” rather than on a continuous scale. In Mplus, this specification refers to Samejima's graded response models (Baker & Kim, 2004; Samejima, 1969).
LCA with Mplus was used to classify participants into distinct classes based on patterns of responses on the WHODAS 2.0 items. A maximum likelihood robust estimator was used. LCA is conceptually similar to cluster analysis in that both techniques aim to identify meaningful groups of subjects who have similar responses to a set of variables. However, LCA uses a modelling approach to derive the classes. A latent categorical variable is modelled with a specific number of classes that account for particular patterns of responses on the observed variables and likelihood of membership in the classes. Thus, the class to which a person is more likely to belong is thought to explain his/her scores (level) on the observed indicator variables. The central assumption in LCA is conditional independence, which means that the covariances between the items are explained by the class latent variable. As such, no residual correlations between the items should exist.
The optimal number of classes was determined by comparing models differing in number of classes starting with one class and continuing upward until the best model fit was obtained (Nylund, Asparouhov, & Muthén, 2007). Indices of model fit were considered, including Akaike's Information Criterion (AIC; Akaike, 1987) and the adjusted Bayesian Information Criterion (BIC; Schwartz, 1978). We also used an approximation of the chi square difference test (Lo, Mendell, & Rubin, 2001) as well as the index, Entropy, which indicates the precision of classification (Magidson & Vermunt, 2002). Finally, Mplus provides a parametric bootstrap method, the bootstrap likelihood ratio test (BLRT), to estimate the distribution of the log likelihood difference test and provide a test to compare the increase in model fit by adding a class.
After deriving the latent classes, we assessed whether membership in these classes was associated with socio‐demographic variables as well as days affected by disabilities, stress, mental health, and substance use using chi‐square tests and one‐way analysis of variance (ANOVA). For pairwise post hoc comparisons, Bonferroni corrections were used in ANOVA and chi‐square tests were conducted to examine specific contrasts as recommended by McDonald (2014). Finally, multinomial logistic regression analyses were performed to assess whether class membership was associated with days affected by disabilities, stress, mental health, and substance use, controlling for the socio‐demographic variables.
3. RESULTS
3.1. Confirmatory factor analysis (CFA)
A series of nested models presented in Table 1 was estimated: a one‐factor model, followed by a one‐factor model with one, two, and three correlated residuals, respectively. These correlated residuals are theoretically valid because they refer to items from the same subdomains (i.e. items 1 and 7 “getting around”, items 8 and 9 “self‐care”, and items 10 and 11 “getting along with people”). These models show that the final model with one factor and three correlated residuals has the best fit. The item loadings and response proportions are presented in Table 2. It can be seen that all items have substantial loadings and variability in the responses. The coefficient alpha for the scale was 0.90, which can be considered excellent for internal consistency given the overall instrument length.
Table 1.
Confirmatory factor analysis (CFA) fit indices
| Model | χ 2 | df | Δ χ 2 (1df) | CFI | TLI | RMSEA |
|---|---|---|---|---|---|---|
| One‐factor | 525.14 | 54 | .94 | .92 | .14 | |
| One‐factor, Covariance e1–e7 | 310.79 | 53 | 214.35* | .97 | .96 | .10 |
| One‐factor, Covariance e1–e7, e8–e9 | 214.34 | 52 | 96.45* | .98 | .97 | .08 |
| One‐factor, Covariance e1–e7, e8–e9, e10–e11 | 188.91 | 51 | 25.43* | .98 | .98 | .08 |
Note. e1–e7 indicates error covariance between item 1 and item 7; e8–e9 indicates error covariance between item 8 and item 8; e10–e11 indicates error covariance between item 10 and item 11; χ2, chi‐square; CFI, Comparative Fit Index; RMSEA, root mean square error of approximation; TLI, Tucker–Lewis Index.
p < 0.001.
Table 2.
Confirmatory factor analysis (CFA) of WHODAS 2.0 items
| Items | CFA loadings | Means (SD) | Response proportions | ||||
|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |||
| 1. Standing for long periods such as 30 minutes? | .68 | 2.05 (1.25) | .51 | .13 | .19 | .13 | .04 |
| 2. Taking care of your household responsibilities? | .80 | 2.05 (1.07) | .42 | .25 | .22 | .10 | .01 |
| 3. Learning a new task, for example, learning to get to a new place? | .71 | 1.70 (0.97) | .60 | .18 | .17 | .05 | .01 |
| 4. How much of a problem did you have joining in community activities (for example, festivities, religious or other activities) in the same way as anyone else can? | .76 | 2.12 (1.25) | .45 | .19 | .18 | .13 | .05 |
| 5. How much have you been emotionally affected by your health problems? | .80 | 2.65 (1.28) | .26 | .21 | .22 | .25 | .07 |
| 6. Concentrating on doing something for ten minutes? | .72 | 1.86 (1.09) | .53 | .19 | .18 | .08 | .02 |
| 7. Walking a long distance such as a kilometre? | .71 | 2.07 (1.34) | .52 | .16 | .14 | .11 | .08 |
| 8. Washing your whole body? | .73 | 1.34 (0.76) | .80 | .10 | .07 | .03 | .00 |
| 9. Getting dressed? | .75 | 1.35 (0.76) | .78 | .13 | .06 | .03 | .00 |
| 10. Dealing with people you do not know? | .74 | 1.91 (1.14) | .52 | .21 | .15 | .09 | .03 |
| 11. Maintaining a friendship? | .73 | 1.72 (1.05) | .61 | .18 | .13 | .06 | .02 |
| 12. Your day‐to‐day work? | .85 | 2.08 (1.21) | .47 | .21 | .19 | .08 | .05 |
Note. Response categories: 1 = none; 2 = mild; 3 = moderate; 4 = severe; 5 = extreme or cannot do.
3.2. Latent class analysis (LCA)
Models from one to five classes were tested, and the four‐class model was selected based on indices of fit (Table 3). The decision to retain the model with four classes rather than five was based on the fact that, although the BLRT was significant in both the four and five class models, the likelihood ratio test (Lo et al., 2001) approached significance for only the four‐class model. Conditional item probabilities associated with each class were inspected and are illustrated in Figure 1 for the four classes. These show the probabilities that an individual in a given class will endorse that item (i.e. none/mild versus moderate/severe/extreme) and suggest four distinct patterns. In addition to these indices, the posterior probabilities indicate the probability that an individual will be classified in a given class, and individuals are classified based on their highest class probability. The number of individuals classified in each class is presented at the bottom of Table 3. Notably, the present findings are based on dichotomized WHODAS items (none/mild versus moderate/extreme/cannot do); these analyses were also performed using a different cutoff (i.e. none versus all other categories) and the results were similar.
Table 3.
Latent class analyses
| Fit index and classification indices | Number of classes | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Loglikelihood | −2948.022 | −2385.174 | −2294.951 | −2248.947 | −2217.669 |
| AIC | 5920.045 | 4820.348 | 4665.901 | 4599.893 | 4563.338 |
| Adjusted BIC | 5931.192 | 4843.572 | 4701.202 | 4647.271 | 4622.792 |
| Lo–Mendell‐Rubin LRT p‐value | 1111.684 p = .0000 | 178.200 p = .0028 | 90.863 p = .0516 | 61.776 p = .1006 | |
| Bootstrapped LRT p‐value | 1125.696 p = .000 | 180.447 p = .000 | 92.008 p = .000 | 62.555 p = .000 | |
| Entropy | 0.876 | 0.826 | 0.846 | .850 | |
| Number of people in each category | 190, 247 | 87, 162, 198 | 86, 48, 123, 190 | 107, 38, 61, 51, 190 | |
Note. AIC, Akaike's Information Criterion; BIC, Bayesian Information Criterion; LRT, likelihood ratio test.
Figure 1.
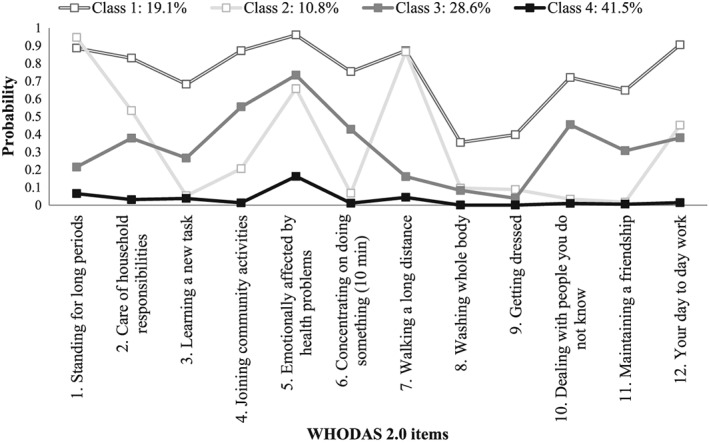
Latent class analysis profiles
The classes as shown in Figure 1 can be described semantically by referring to items with high probabilities. We can apply the concept of simple structure in factor analysis to LCA to refer to latent class separation (Collins & Lanza, 2010). In the four‐class model, the first class which can be labelled “pervasive disability” defines 19.1% of the sample. Individuals in this category have a high likelihood of endorsing all items with the exception of washing the whole body and getting dressed. These last two items have a probability of less than 50% but are endorsed more frequently by individuals in this class than those in the other classes.
The second class denoted “physical disability” includes 10.8% of the sample and can be distinguished by a high probability of difficulty standing for long periods and walking long distances, and a moderate probability of difficulty with household responsibilities, being emotionally affected by health problems and having difficulty with day‐to‐day work. Overall, this class seems to capture difficulty with daily physical activities.
The third class denoted “emotional, cognitive, or interpersonal disability” includes 28.6% of the sample and reflects difficulties joining community activities, concentrating on doing something, dealing with people they do not know, and being emotionally affected by health problems. This class appears to capture difficulties in social and cognitive functioning as well as dealing with the emotional impact of health issues.
The fourth category denoted “no/low disability” includes 41.5% of the sample and refers to the lack of any disabilities with low probability of endorsing any of the 12 items. This class therefore represents a substantial proportion of individuals who do not report any disabilities.
3.3. Association between latent classes and socio‐demographics
Table 4 presents bivariate descriptive statistics for the socio‐demographic variables and chi‐square tests of independence assessing whether probability of membership in the four different classes is associated with the socio‐demographic characteristics of participants. Individuals in Class 1 (pervasive disabilities) were more likely to be single, and less likely to be working for pay compared to those in Class 4, less likely to have completed high school than those in Classes 2 and 4, and they were most likely to have the lowest household income compared to all other classes. Individuals in Class 2 (physical disabilities) were more likely to have a household income of $40,000+ compared to those in Class 1. Those in Class 3 (emotional, cognitive, or interpersonal disabilities) were more likely to not have completed high school, to not be working for pay, and to have a lower household income (i.e. < $20,000) compared to Class 4. Individuals in Class 4 (no/low disability) were slightly younger (e.g. 18–29 years) than those in Classes 1 and 2 and were more likely to be married/living with a partner compared to those in Class 1 and they were more likely to have completed high school, and to have a higher household income than Classes 1 and 3 and more likely to be working for pay than all other classes.
Table 4.
Socio‐demographic characteristics of study participants and likelihood of belonging to each latent class as a function of demographics
| Demographic characteristics | Total sample (N = 447) | Class 1 Pervasive disability (N = 86) | Class 2 Physical disability (N = 48) | Class 3 Emotional, cognitive, or interpersonal disability (N = 123) | Class 4 No/low disability (N = 190) | Chi‐square |
|---|---|---|---|---|---|---|
| Gender | ||||||
| Female | 56.8% | 65.1% | 64.6% | 50.4% | 55.3% | χ 2 = 5.842, 3df, |
| Male | 43.2% | 34.9% | 35.4% | 49.6% | 44.7% | p = .120 |
| Age – Mean | 41.94 | 42.29 | 48.883,4 | 41.312 | 40.422,3 | F = 4.053, 3/437 df, p = .007 |
| 18–29 | 27.7% | 17.6%4 | 16.7%4 | 24.2% | 37.2%1 ,2 | χ 2 = 37.431, 9df, |
| 30–49 | 39.5% | 55.3%2 ,4 | 27.1%1 | 45.0% | 31.9%1 | p < .001 |
| 50–64 | 26.8% | 24.7% | 41.7% | 27.5% | 23.4% | |
| 65+ | 6.1% | 2.4% | 14.6% | 3.3% | 7.4% | |
| Marital status | ||||||
| Married or living with a partnera | 46.3% | 31.8%4 | 50.0% | 46.3% | 51.9%1 | χ 2 = 9.831, 3df, p = .020 |
| Education | ||||||
| Did not complete high school | 19.3% | 30.2%2 .4 | 10.4%1 | 27.0%4 | 11.6%1 ,3 | χ 2 = 23.194, 6df, p = .001 |
| Completed high school | 28.7% | 27.9% | 31.2% | 21.3% | 33.2% | |
| Some or completed college or university | 52.0% | 41.9% | 58.3% | 51.6% | 55.3% | |
| Employment | ||||||
| Working for pay | 34.5% | 12.8%4 | 31.2%4 | 23.8%4 | 52.1%1 ,2,3 | χ 2 = 50.255, 3df, p < .001 |
| Household income | ||||||
| Less than $20,000 | 45.2% | 71.6%2 ,3,4 | 39.1%1 | 51.8%1 ,4 | 30.9%1 ,3 | χ 2 = 60.794, 9df, p < .001 |
| $20,000–$39,999 | 21.8% | 22.2% | 19.6% | 24.5% | 20.4% | |
| $40,000–$59,999 | 11.7% | 2.5%2 ,4 | 19.6%1 | 10.0% | 14.9%1 | |
| $60,000 or more | 21.3% | 3.7%2 ,4 | 21.7%1 | 13.6%4 | 33.7%1 ,3 | |
| Study | ||||||
| Consumer Journey – Consumers | 29.5% | 46.5%2 ,4 | 18.8%1 ,3 | 46.3%2 ,4 | 13.7%1 ,3 | χ 2 = 77.536, 12df, p < .001 |
| Consumer Journey – Family | 14.5% | 12.8% | 20.8% | 14.6% | 13.7% | |
| Valuation of Health States | 21.5% | 26.7% | 22.9% | 17.9% | 23.2% | |
| Communication and Conflict | 22.4% | 3.5%4 | 6.2% | 9.8%4 | 21.1%1 ,3 | |
| Random Walk | 20.6% | 10.5%2 ,4 | 31.2%1 ,3 | 11.4%2 ,4 | 28.4%1 ,3 |
Compared to never married, separated, widowed, divorced.
1,2,3,4Indicates significant differences between classes (p < 0.05) (i.e. in the Class 1 column; 2,3,4indicates that the category is different for Class 1 compared to all other classes); Bonferroni‐adjusted p‐value for significance at p < 0.05 for proportions is p = 0.008.
As shown in Table 4, class membership was also associated with type of study (χ2 = 77.536, 12df, p < 0.001), with more people in Classes 1 and 3 being consumers from the Consumer Journey study (46.5% and 46.3%, respectively) or participants in the Valuations of Health States study (i.e. those who self‐identified as being sad, blue or depressed; 26.7% and 17.9%, respectively) than from the Random Walk and Communication and Conflict studies. By comparison, Classes 2 and 4 were most represented by people from the Random Walk study (general population sample; 31.2% and 28.4%, respectively) with smaller proportions in the other samples.
3.4. Associations between latent classes and number of days affected by disabilities, stress, mental health and substance use
Table 5 shows the four different classes by number of days affected by disabilities, stress, mental health and substance use, with means provided for continuous scales and proportions reported for dichotomous measures. Class 1 (pervasive disability) membership was associated with having significantly higher scores or higher prevalence levels on most variables compared to all other classes (except where noted). These included a larger number of days disabilities present (compared to Classes 3 and 4), days unable to do usual activities, and days with reduced activities as well as higher perceived stress, chronic stress, depression, depressive symptoms, anxiety, antidepressant use, sedative/tranquilizer use and illicit drug use (compared to Classes 2 and 4), marijuana use (compared to Class 2), alcohol dependence/consequences, smoking, and average number of cigarettes (compared to Class 4).
Table 5.
Associations of latent classes with days affected by disabilities, stress, mental health, and substance use
| Means or % in “yes” category | Statistical test | |||||
|---|---|---|---|---|---|---|
| Total sample (N = 447) | Class 1 Pervasive disability (N = 86) | Class 2 Physical disability (N = 48) | Class 3 Emotional, cognitive, or interpersonal disability (N = 123) | Class 4 No/low disability (N = 190) | ||
| Days affected by disabilities | ||||||
| Days difficulties present | 12.45 | 21.9233,4 | 19.823,4 | 15.421,2,4 | 4.181,2,3 | F = 105.341, 3/423df, p < .001 |
| Days unable to do usual activities | 5.63 | 13.352,3,4 | 8.211,4 | 6.251,4 | 0.961,2,3 | F = 59.595, 3/423df, p < .001 |
| Days reduce usual activities | 7.23 | 15.272,3,4 | 10.911,4 | 8.271,4 | 1.931,2,3 | F = 63.032, 3/424df, p < .001 |
| Stress | ||||||
| Perceived stress score | 19.59 | 26.922,3,4 | 16.851,3 | 22.321,2,4 | 15.221,3 | F = 58.716, 3/437df, p < .001 |
| Chronic stress score | 5.35 | 8.052,3,4 | 4.701 | 6.081,4 | 3.881,3 | F = 27.547, 3/420df, p < .001 |
| Mental health | ||||||
| Met criteria for major depression | 40.8% | 76.9%2 ,3,4 | 31.0%1 ,3 | 56.9%1 ,2,4 | 17.5%1 ,3 | χ 2 = 97.440, 3df, p < .001 |
| Total number of symptoms of depression | 2.40 | 4.692,3,4 | 1.761,3 | 3.311,2,4 | 0.981,3 | F = 45.475, 3/415df, p < .001 |
| Met screening criteria for anxiety problems | 32.8% | 75.3%2 ,3,4 | 26.1%1 ,4 | 41.2%1 ,4 | 10.1%1 ,2,3 | χ 2 = 118.729, 3df, p < .001 |
| Prescription drug use | ||||||
| Antidepressants | 34.2% | 65.8%2 ,3,4 | 25.6%1 | 44.8%1 ,4 | 15.8%1 ,3 | χ 2 = 69.734, 3df, p < .001 |
| Sedatives/tranquilizers | 35.0% | 62.0%2 ,4 | 20.9%1 ,3 | 44.5%2 ,4 | 20.3%1 ,3 | χ 2 = 51.088, 3df, p < .001 |
| Alcohol use | ||||||
| AUDIT total score | 7.91 | 9.67 | 6.42 | 8.32 | 7.24 | F = 2.340, 3/436df, p = .073 |
| AUDIT 16+ | 16.4% | 21.4% | 12.5% | 17.6% | 14.3% | χ 2 = 2.838, 3df, p = .417 |
| AUDIT consumption | 4.29 | 4.49 | 3.78 | 4.16 | 4.42 | F = 0.565, 3/423df, p = .638 |
| AUDIT dependence/consequences | 3.64 | 5.164 | 2.81 | 4.27 | 2.801 | F = 4.433, 3/430df, p = .004 |
| Smoking | ||||||
| Smoke daily or occasionally | 50.8% | 63.5%4 | 45.8% | 54.9% | 43.7%1 | χ 2 = 10.661, 3df, p = .014 |
| Number of cigarettes (smokers only; n = 226) | 17.98 | 21.854 | 16.18 | 20.834 | 13.711,3 | F = 6.490, 3/218df, p < .001 |
| Other drug use | ||||||
| Marijuana | 44.1% | 51.9%2 | 27.1%1 ,3 | 55.5%2 ,4 | 37.6%3 | χ 2 = 16.832, 3df, p = .001 |
| Illicit drugs (not marijuana) | 32.5% | 43.4%2 ,4 | 14.9%1 ,3 | 46.3%2 ,4 | 23.3%1 ,3 | χ 2 = 28.913, 3df, p < .001 |
Note. AUDIT, Alcohol Use Disorders Identification Test.
1,2,3,4Indicates significant differences between classes (p < 0.05) (i.e. in the Class 1 column; 2,3,4indicates that the variable is different for Class 1 compared to all other classes); Bonferroni‐adjusted p‐value for significance at p < 0.05 for proportions is p = 0.008.
Class 2 (physical disability) membership was associated with more days of difficulties present (compared to Classes 3 and 4) as well as more days unable to do usual activities and days of reduced usual activities compared to Class 4 but fewer days when compared to Class 1. Class 2 was also more likely to have anxiety compared to Class 4. Class 3 (emotional, cognitive, or interpersonal disability) membership was associated with more perceived stress, depression, depressive symptoms, sedative/tranquilizer use, and marijuana and illicit drug use compared to Classes 2 and 4. Class 3 membership was also associated with more days of difficulties present, days unable to do usual activities, days of reduced usual activities as well as more chronic stress, anxiety, antidepressant use, and average number of cigarettes compared to Class 4. Individuals in Class 4 (no/low disability) had the lowest scores and prevalence on most of the earlier variables.
Finally, Table 6 shows the adjusted relative risk ratios (RRRs) for number of days affected by disabilities, stress, mental health and substance use for the first three classes (Classes 1, 2 and 3) compared to the no/low disability class (Class 4), controlling for socio‐demographic variables that were found to be significant in the analyses above (i.e. age, marital status, education, income, employment and income). These analyses were conducted to determine whether differences in mental health/substance use variables remained significant despite any differences across the classes in the socio‐demographic variables. Overall, most of the differences detected earlier remained significant controlling for the socio‐demographic variables, with the exception of smoking (difference between Classes 1 and 4) and marijuana use (between Classes 3 and 4) which became non‐significant with these additional controls.
Table 6.
Days affected by disabilities, stress, mental health and substance use and relative risk ratios (RRRs) of belonging to each latent class compared to the no/low disability class (Class 4)
| Class 1 Pervasive disability (N = 86)
Adjusteda RRR, p‐value |
Class 2 Physical disability (N = 48)
Adjusteda RRR, p‐value |
Class 3 Emotional, cognitive, or interpersonal disability (N = 123)
Adjusteda RRR, p‐value |
|
|---|---|---|---|
| Days affected by disabilities | |||
| Days difficulties present | 1.225, p < .001 | 1.210, p < .001 | 1.158, p < .001 |
| Days unable to do usual activities | 1.394, p < .001 | 1.355, p < .001 | 1.307, p < .001 |
| Days reduce usual activities | 1.263, p < .001 | 1.232, p < .001 | 1.173, p < .001 |
| Stress | |||
| Perceived stress score | 1.278, p < .001 | 1.053, p = .036 | 1.139, p < .001 |
| Chronic stress score | 1.349, p < .001 | 1.102, p = .070 | 1.195, p < .001 |
| Mental health | |||
| Met criteria for major depression | 11.634, p < .001 | 2.484, p = .040 | 6.523, p < .001 |
| Total number of symptoms of depression | 1.566, p < .001 | 1.187, p = .025 | 1.389, p < .001 |
| Met screening criteria for anxiety problems | 24.721, p < .001 | 3.458, p = .005 | 5.637, p < .001 |
| Prescription drug use | |||
| Antidepressants | 8.258, p < .001 | 1.663, p = .228 | 4.063, p < .001 |
| Sedatives/tranquilizers | 64.841, p < .001 | 0.940, p = .892 | 3.030, p < .001 |
| Alcohol use | |||
| AUDIT total score | 1.043, p = .021 | 1.008, p = .746 | 1.014, p = .419 |
| AUDIT 16+ | 2.038, p = .073 | 1.195, p = .726 | 1.291, p = .487 |
| AUDIT consumption | 1.043, p = .352 | 1.002, p = .972 | 0.979, p = .597 |
| AUDIT dependence/consequences | 1.078, p = .008 | 1.023, p = .526 | 1.045, p = .093 |
| Smoking | |||
| Smoke daily or occasionally | 1.321, p = .384 | 1.327, p = .440 | 1.118, p = .683 |
| Number of cigarettes (smokers only; n = 226) | 1.040, p = .068 | 1.006, p = .829 | 1.048, p = .024 |
| Other drug use | |||
| Marijuana | 1.576, p = .189 | 0.760, p = .512 | 1.729, p = .065 |
| Illicit drugs (not marijuana) | 1.980, p = .038 | 0.714, p = .470 | 2.653, p < .001 |
Note. AUDIT, Alcohol Use Disorders Identification Test.
RRRs were adjusted for significant demographics (i.e. age, marital status, education, employment, and household income).
4. DISCUSSION
4.1. Support for a one‐factor solution
This study provided support for the psychometric soundness of the 12‐item WHODAS 2.0. Consistent with other studies, we found support for a one‐factor model. However, including three correlated residuals among items from related subdomains improved fit. In particular, standing for long periods of time (item 1) was correlated with walking a long distance (item 7, “getting around” domain). Washing your whole body (item 8) was correlated with getting dressed (item 9, “self‐care” domain). Dealing with people you do not know (item 10) was correlated with maintaining a friendship (item 11, “getting along with people” domain). These three error covariances were also found by Luciano et al. (2010b). These covariances violate item response theory assumptions; however, item response theory is considered robust to this violation when examining scales with more than 10 items (Edelen & Reeve, 2007). Thus, it is preferable to retain the full set of items and the scale may be considered unidimensional. These findings suggest that the WHODAS 2.0 measures a general factor of disablement.
4.2. Prototypical profiles
Although our findings support a general factor of disablement, LCA identified four different subgroups of people with distinct patterns of responses (classes). These four classes were indicative of: (1) pervasive disability (19.1%); (2) physical disability (10.8%); (3) emotional, cognitive, or interpersonal disability (28.6%); (4) no/low disability (41.5%).
4.2.1. Pervasive disability class
Individuals in the pervasive disability class had a high likelihood of endorsing most of the disability items (except washing and getting dressed). Thus, individuals in this class appear to have disabilities spanning several domains, including understanding and interacting with the world, moving and getting around, getting along with people, life activities and participation in society. Individuals with pervasive disabilities were the most likely to occupy low socio‐economic status positions, including not working for pay, having less education and lower household income. Given that this class most likely reflects people with more severe disabilities, this finding appears to be consistent with evidence that people with severe disabilities are more likely to have lower education levels, to be unemployed, and to have lower income levels (Statistics Canada, 2015). For example, Turcotte (2014) found that 26% of those with very severe disabilities were employed compared to 54% of those with moderate disabilities and 84% of those with no disabilities.
Individuals in the pervasive disability class were also found to have a wide range of mental health and substance use problems. This group was characterized by having higher levels of stress, including perceived stress and chronic stress and they were more likely to meet criteria for depression and anxiety. This finding is consistent with the literature on general links of disability with depression and anxiety (Deschênes, Burns, & Schmitz, 2015; el‐Guebaly et al., 2007; Karvonen‐Gutierrez & Ylitalo, 2013; Mitra, Wilber, Allen, & Walker, 2005; Robinson‐Whelen, Taylor, Hughes, & Nosek, 2013; Wilber, Mitra, Walker, & Allen, 2002). For example, using the 12‐item WHODAS 2.0, Deschênes et al. (2015) found that major depressive disorder was positively associated with functional disability and more disability days, and this effect was moderated by chronic physical health conditions. Additionally, Hendriks et al. (2014) found that all anxiety disorders were associated with greater disability.
Individuals in the pervasive disability class were also more likely to report prescription drug use, alcohol dependence/consequences, marijuana and illicit drug use, smoking, and a higher number of cigarettes per day when compared to individuals within the physical disabilities or no/low disability classes. These findings are consistent with Glazier and Kling (2013) who found that people with disabilities were more likely to use prescription drugs and illicit drugs than people without disabilties. Pathways thought to explain the association between substance use and disability are that: (1) substance use is a causal factor in disability, (2) substance use is a mediating factor in recovery for people with disabilities (or used for coping), or (3) there is less access to addiction/substance misuse services for people with disabilities (Glazier & Kling, 2013). Interestingly, while tobacco use was higher in the pervasive disability class than the no/low disability class in the bivariate analyses, this effect became non‐significant controlling for socio‐demographic variables, suggesting that this difference may have reflected socio‐demographic differences between these classes.
4.2.2. Physical disability class
The physical disability class mainly had difficulties standing, walking, and working (both at home and at work) but were also emotionally affected by health problems. This group tended to be older (65+ years) than both those with emotional, cognitive, and interpersonal disabilities and no/low disability, consistent with evidence that physical disabilities increase with age (Statistics Canada, 2015). Individuals in this class were also less likely to be working for pay compared to those with no/low disability but had a higher household income ($40,000+) than those with pervasive disabilities. Relative to those with no/low disability, individuals in the physical disability class reported more perceived stress and mental health problems, including depression and anxiety. This finding is generally consistent with evidence that physical disability is correlated with stress. For example, one study of women with physical disabilities found that stress was linked to more mobility limitations and higher levels of required assistance (Hughes, Taylor, Robinson‐Whelen, & Nosek, 2005).
4.2.3. Emotional, cognitive, or interpersonal disability class
The emotional, cognitive, or interpersonal disability class was characterized by having more difficulties getting along with other people, including dealing with people they do not know and joining community activities. They also had trouble concentrating and were emotionally affected by their health problems. Thus, this class appears to represent individuals who have mental health‐related disabilities. Members of this class tended to be younger (i.e. 30–49 years) than those with no/low disability. This class was also over‐represented in the lower socio‐economic categories, including lower education, not working for pay, and lower income compared to those with no/low disability. This finding supports evidence that people who have mental‐health related disabilities tend to have lower levels of education, are less likely to be employed and have lower income levels (Bizier, Marshall, & Fawcett, 2015). This is consistent with a social determinants of health perspective, suggesting that people's living conditions and social disadvantage can contribute to mental health challenges (see Raphael, 2009). Disabilities stemming from mental health problems may also influence socio‐economic factors, such as being able to find employment (Canadian Mental Health Association, Centre for Addiction and Mental Health, 2010).
Similar to individuals in the pervasive disability class, individuals in the emotional, cognitive, or interpersonal disability class were more likely than those with no/low disability (and often those in the physical disabilities class) to have high levels of stress, depression and anxiety, and use prescription drugs, marijuana, and illicit drugs. However, the effect for marijuana became non‐significant controlling for the socio‐demographic variables, suggesting that differences between Classes 3 and 4 in use of marijuana may reflect socio‐demographic differences. Finally, heavy smoking (i.e. number of cigarettes per day) was more common among smokers in this class compared to smokers in the no/low disability class. This effect remained significant controlling for socio‐demographics and is consistent with Jarrett and Pignataro (2013) who found that individuals with mental disabilities reported the highest rates of smoking compared with individuals with other disabilities (learning, sensory, and physical disabilities).
4.3. Limitations
This study used a pooled database from different substudies. The samples from these substudies were found to be associated with the resultant latent classes. Not surprisingly, the Consumer Journey study sample (people with mental health and/or substance use problems) consisted of the largest proportion of people in the pervasive disability and the emotional, cognitive, interpersonal disability classes while the Random Walk study sample (general population) had the smallest proportion of people in these classes. An advantage of using the pooled database is that we were able to collect data from diverse populations, including people who had mental health and/or substance use problems. However, the sub‐study sample sizes were too small for separate LCA. In any LCA, the nature of the classes and their prevalence depend partly on the characteristics of the sample. Therefore, future analyses are needed to determine whether the latent class structure can be replicated in a larger and more generalizable sample. Additionally, while LCA was useful in identifying homogeneous subgroups of individuals with different types of disabilities, further research is needed to assess the predictive validity of the latent classes in a prospective study.
While the CFA suggests that the 12‐item WHODAS 2.0 can be used as a single factor reflecting overall functioning, the LCA reveals qualitatively different patterns (i.e. classes differing in shape) as well as evidence of latent classes differing in level of overall functioning. Recent developments in mixture modelling research such as factor mixture models provide a way to combine factor and latent class analyses (see e.g. Hallquist & Wright, 2014; Lubke & Miller, 2015; Miettunen, Nordström, Kaakinen, & Ahmed, 2016). Although it is beyond the scope of this paper to attempt to disentangle shape from level effects in disability item responses using these newer techniques, future studies with larger samples aimed specifically at comparing various latent models would add to construct validation research of the WHODAS 2.0.
4.4. Implications
These findings are largely consistent with the literature and offer support for convergent validity of the WHODAS 2.0 latent classes, with the classes representing disability ranking higher on most measures of stress and mental health compared to the no/low disability class. In some instances, these classes also ranked higher on substance use measures, including alcohol dependence/consequences, smoking, and illicit drug use. These classes offer a simple and meaningful way to classify people with disabilities based on the 12‐item WHODAS 2.0. Karvonen‐Gutierrez and Ylitalo (2013) suggested that the 36‐item WHODAS 2.0 could be used to assess each of the original six domains to gather information about the nature of one's disability. Using the present four classes provides an alternative way to examine the nature of one's disability as individuals scoring high on one domain may also score high on others in differing combinations. Focusing on individuals with a high probability of being in one of the first three classes may also help guide interventions.
DECLARATION OF INTEREST STATEMENT
The authors have no competing interests.
ACKNOWLEDGEMENTS
The authors extend their thanks to Sue Steinback for editorial assistance, Roseanne Pulford for preparing and processing study materials, and the research staff who assisted with recruitment and data collection.
MacLeod, M. A. , Tremblay, P. F. , Graham, K. , Bernards, S. , Rehm, J. , and Wells, S. (2016) Psychometric properties and a latent class analysis of the 12‐item World Health Organization Disability Assessment Schedule 2.0 (WHODAS 2.0) in a pooled dataset of community samples. Int J Methods Psychiatr Res, 25: 243–254. doi: 10.1002/mpr.1523.
Funding Information: This project was funded by the Canadian Institutes for Health Research (CIHR), Emerging Team Grant (CBG – 101926) and by the Canada Foundation for Innovation (#20289) and the Ontario Ministry of Research and Innovation.
REFERENCES
- Abedzadeh‐Kalahroudi, M. , Razi, E. , Sehat, M. , & Asadi‐Lari, M. (2016). Psychometric properties of the world health organization disability assessment schedule II −12 Item (WHODAS II) in trauma patients. Injury, 47(5), 1104–1108. DOI: 10.1016/j.injury.2015.11.046 [DOI] [PubMed] [Google Scholar]
- Akaike, H. (1987). Factor analysis and AIC. Psychometrika, 52, 317–332. DOI: 10.1007/BF02294359 [DOI] [Google Scholar]
- Babor, T. F. , Higgins‐Biddle, J. C. , Saunders, J. B. , & Monteiro, M. G. (2001). AUDIT – The Alcohol Use Disorders Identification Test: Guidelines for use in primary care (2nd ed.). Geneva: World Health Organization, Department of Mental Health and Substance Dependence. [Google Scholar]
- Baker, F. B. , & Kim, S.‐H. (2004). Item response theory: Parameter estimation techniques. New York, NY: Marcel Dekker. [Google Scholar]
- Bernards, S. , Graham, K. , Demers, A. , Kairouz, S. , & Wells, S. (2007). Gender and the assessment of at‐risk drinking: Evidence from the GENACIS Canada (2004–2005) telephone survey version of the AUDIT. Drug & Alcohol Dependence, 88, 282–290. DOI: 10.1016/j.drugalcdep.2006.11.013 [DOI] [PubMed] [Google Scholar]
- Bizier, C. , Marshall, C. , & Fawcett, G. (2015). Mental health‐related disabilities among Canadians aged 15 years and older, 2012 In Canadian Survey on Disability, 2012. Ottawa, ON: Statistics Canada. [Google Scholar]
- Canadian Mental Health Association, Centre for Addiction and Mental Health (2010). Employment and education for people with mental illness, Discussion paper. Toronto, ON: Canadian Mental Health Association. [Google Scholar]
- Cohen, S. , Kamarck, T. , & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health & Social Behavior, 24, 385–396. DOI: 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Collins, L. M. , & Lanza, S. T. (2010). Latent class and latent transition analysis In With applications in the social, behavioral, and health sciences. Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Deschênes, S. S. , Burns, R. J. , & Schmitz, N. (2015). Associations between depression, chronic physical health conditions, and disability in a community sample: A focus on the persistence of depression. Journal of Affective Disorders, 179, 6–13. DOI: 10.1016/j.jad.2015.03.020 [DOI] [PubMed] [Google Scholar]
- Edelen, M. O. , & Reeve, B. B. (2007). Applying Item Response Theory (IRT) modeling to questionnaire development, evaluation, and refinement. Quality of Life Research, 16(Suppl 1), 5–18. DOI: 10.1007/s11136-007-9198-0 [DOI] [PubMed] [Google Scholar]
- el‐Guebaly, N. , Currie, S. , Williams, J. , Wang, J. , Beck, C. A. , Maxwell, C. , & Patten, S. B. (2007). Association of mood, anxiety, and substance use disorders with occupational status and disability in a community sample. Psychiatric Services, 58(5), 659–667. DOI: 10.1176/appi.ps.58.5.659 [DOI] [PubMed] [Google Scholar]
- Flynn, A. , Tremblay, P. F. , Rehm, J. , & Wells, S. (2013). A modified random walk door‐to‐door recruitment strategy for collecting social and biological data relating to mental health, substance use/addictions and violence problems in a Canadian community. IJADR, 2(2), 7–16. DOI: 10.7895/ijadr.v2i2.143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glazier, R. E. , & Kling, R. N. (2013). Recent trends in substance abuse among persons with disabilities compared to that of persons without disabilities. Disability & Health Journal, 6, 107–115. DOI: 10.1016/j.dhjo.2013.01.007 [DOI] [PubMed] [Google Scholar]
- Hallquist, M. N. , & Wright, A. G. (2014). Mixture modeling methods for the assessment of normal and abnormal personality, Part I: Cross‐sectional models. Journal of Personality Assessment, 96(3), 256–268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heatherton, T. F. , Kozlowski, L. T. , Frecker, R. C. , Rickert, W. , & Robinson, J. (1989). Measuring the heaviness of smoking: Using self‐reported time to the first cigarette of the day and number of cigarettes smoked per day. British Journal of Addiction, 84(7), 791–799. DOI: 10.1111/j.1360-0443.1989.tb03059.x [DOI] [PubMed] [Google Scholar]
- Heckathorn, D. D. (1997). Respondent‐driven sampling: A new approach to the study of hidden populations. Social Problems, 44(2), 174–199. DOI: 10.2307/3096941 [DOI] [Google Scholar]
- Hendriks, S. M. , Spijker, J. , Licht, C. M. M. , Beekman, A. T. F. , Hardeveld, F. , De Graaf, R. , … Penninx, B. W. J. H. (2014). Disability in anxiety disorders. Journal of Affective Disorders, 166, 227–233. DOI: 10.1016/j.jad.2014.05.006 [DOI] [PubMed] [Google Scholar]
- Hughes, R. B. , Taylor, H. B. , Robinson‐Whelen, S. , & Nosek, M. A. (2005). Stress and women with physical disabilities: Identifying correlates. Womens Health Issues, 15, 14–20. DOI: 10.1016/j.whi.204.09.001 [DOI] [PubMed] [Google Scholar]
- Jarrett, T. , & Pignataro, R. M. (2013). Cigarette smoking among college students with disabilities: National College Health Assessment II, Fall 2008‐Spring 2009. Disability & Health Journal, 6(3), 204–212. DOI: 10.1016/j.dhjo.2013.01.011 [DOI] [PubMed] [Google Scholar]
- Karvonen‐Gutierrez, C. A. , & Ylitalo, K. R. (2013). Prevalence and correlates of disability in a late middle‐aged population of women. Journal of Aging Health, 25(4), 701–717. DOI: 10.1177/0898264313488165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler, R. C. , Andrews, G. , Mroczek, D. , Ustun, B. , & Wittchen, H.‐U. (1998). The World Health Organization Composite International Diagnostic Interview Short Form (CIDI‐SF). International Journal of Methods in Psychiatric Research, 7, 171–185. DOI: 10.1002/mpr.47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirchberger, I. , Braitmayer, K. , Coenen, M. , Oberhauser, C. , & Meisinger, C. (2014). Feasibility and psychometric properties of the German 12‐item WHO Disability Assessment Schedule (WHODAS 2.0) in a population‐based sample of patients with myocardial infarction from the MONICA/KORA myocardial infarction registry. Population Health Metrics, 12, 27 DOI: 10.1186/s12963-014-0027-8 [DOI] [Google Scholar]
- Kline, P. (1994). An easy guide to factor analysis. New York, NY: Routledge. [Google Scholar]
- Lo, Y. , Mendell, N. R. , & Rubin, D. B. (2001). Testing the number of components in a normal mixture. Biometrika, 88(3), 767–778. DOI: 10.1093/biomet/88.3.767 [DOI] [Google Scholar]
- Lubke, G. H. , & Miller, P. J. (2015). Does nature have joints worth carving? A discussion of taxometrics, model‐based clustering and latent variable mixture modeling. Psychological Medicine, 45(4), 705–715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luciano, J. V. , Ayuso‐Mateos, J. L. , Aguado, J. , Fernandez, A. , Serano‐Blanco, A. , Roca, M. , & Haro, J. M. (2010a). The 12‐item World Health Organization Disability Assessment Schedule II (WHO‐DAS II): A nonparametric item response analysis. BMC Medical Research Methodology, 10, 45 DOI: 10.1186/1471-2288-10-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luciano, J. V. , Ayuso‐Mateos, J. L. , Fernández, A. , Serrano‐Blanco, A. , Roca, M. , & Haro, J. M. (2010b). Psychometric properties of the twelve item WHODAS 2.0 in Spanish primary care patients with a first major depressive episode. Journal of Affective Disorders, 121, 52–58. DOI: 10.1016/j.jad.2009.05.008 [DOI] [PubMed] [Google Scholar]
- Magidson, J. , & Vermunt, J. K. (2002). Latent class models for clustering: A comparison with K‐means. Canadian Journal of Marketing Research, 20, 37–44. [Google Scholar]
- McDonald, J. H. (2014). Handbook of biological statistics. Baltimore, MD: Sparky House Publishing. [Google Scholar]
- Miettunen, J. , Nordström, T. , Kaakinen, M. , & Ahmed, A. O. (2016). Latent variable mixture modeling in psychiatric research‐‐a review and application. Psychological Medicine, 46(3), 457–467. [DOI] [PubMed] [Google Scholar]
- Mitra, M. , Wilber, N. , Allen, D. , & Walker, D. K. (2005). Prevalence and correlates of depression as a secondary condition among adults with disabilities. American Journal of Orthopsychiatry, 75(1), 76–85. DOI: 10.1037/0002-9432.75.1.76 [DOI] [PubMed] [Google Scholar]
- Muthén, L. K. , & Muthén, B. O. (1998–2012). Mplus User's Guide. Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nylund, K. L. , Asparouhov, T. , & Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo Simulation Study. Structural Equation Modeling, 14(4), 535–569. DOI: 10.1080/10705510701575396 [DOI] [Google Scholar]
- Raphael, D. (2009). Restructuring society in the service of mental health promotion: Are we willing to address the social determinants of mental health? International Journal of Mental Health Promotion, 11(3), 18–31. DOI: 10.1080/14623730.2009.9721789 [DOI] [Google Scholar]
- Rehm, J. , Üstun, T. B. , Saxena, S. , Nelson, C. B. , Chatterji, S. , Ivis, F. , & Adlaf, E. (1999). On the development and psychometric testing of the WHO screening instrument to assess disablement in the general population. International Journal of Methods in Psychiatric Research, 8(2), 110–122. DOI: 10.1002/mpr.61 [DOI] [Google Scholar]
- Robinson‐Whelen, S. , Taylor, H. B. , Hughes, R. B. , & Nosek, M. A. (2013). Depressive symptoms in women with physical disabilities: Identifying correlates to inform practice. Archives of Physical Medicine and Rehabilitation, 94, 2410–2416. DOI: 10.1016/j.apmr.2013.07.013 [DOI] [PubMed] [Google Scholar]
- Saltychev, M. , Bärlund, E. , Mattie, R. , McCormick, Z. , Paltamaa, J. , & Laimi, K. (2016). A study of the psychometric properties of 12‐item World Health Organization Disability Assessment Schedule 2.0 in a large population of people with chronic musculoskeletal pain. Clinical Rehabilitation, 1(11) [Epub ahead of print]. DOI: 10.1177/0269215516631385 [DOI] [PubMed] [Google Scholar]
- Samejima, F. (1969). Estimation of latent ability using a response pattern of graded scores (Psychometric Monograph No. 17). Richmond, VA: Psychometric Society. [Google Scholar]
- Saunders, J. B. , Aasland, O. G. , Babor, T. F. , De La Fuente, J. R. , & Grant, M. (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption‐II. Addiction, 88, 791–804. DOI: 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Schiavolin, S. , Ferroli, P. , Acerbi, F. , Brock, S. , Broggi, M. , Cusin, A. , … Raggi, A. (2014). Disability in Intalian neurosurgical patients: Validity of the 12‐item World Health Organization Disability Assessment Schedule. International Journal of Rehabilitation Research, 37(3), 267–270. DOI: 10.1097/MRR.0000000000000064 [DOI] [PubMed] [Google Scholar]
- Schwartz, G. (1978). Estimating the dimension of a model. Annals of Statistics, 6(2), 461–464. DOI: 10.1214/aos/1176344136 [DOI] [Google Scholar]
- Shields, M. (2004). Stress, health and the benefit of social support. Health Reports, 15(1), 9–38. [PubMed] [Google Scholar]
- Sousa, R. M. , Dewey, M. E. , Acosta, D. , Jotheeswaran, A. T. , Castro‐Costa, E. , Ferri, C. P. , … Prince, M. J. (2010). Measuring disability across cultures – the psychometric properties of the WHODAS II in older people from seven low‐ and middle‐income countries. The 10/66 Dementia Research Group population‐based survey. International Journal of Methods in Psychiatric Research, 19(1), 1–17. DOI: 10.1002/mpr.299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada (2015). A profile of persons with disabilities among Canadians aged 15 years or older, 2012. Ottawa, ON: Statistics Canada. [Google Scholar]
- Turcotte, M. (2014). Persons with disabilities and employment. Ottawa, ON: Statistics Canada. [Google Scholar]
- Turner, R. J. , Wheaton, B. , & Lloyd, D. A. (1995). The epidemiology of social stress. American Sociological Review, 60(1), 104–125. DOI: 10.2307/2096348. [DOI] [Google Scholar]
- Üstün, T. B. , & Chatterji, S. (1998). Editorial: Measuring functioning and disability – a common framework. International Journal of Methods in Psychiatric Research, 7(2), 79–83. [Google Scholar]
- Üstun T. B., Chatterji S., Bickenbach J. E., Trotter R. T. I., Room R., Rehm J., Saxena S., & On behalf of the World Health Organization (Eds). (2001). Disability and culture: Universalism and diversity. Göttingen: Hogrefe & Huber Publisher. [Google Scholar]
- Üstün, T. B. , Chatterji, S. , Kostanjsek, N. , Rehm, J. , Kennedy, C. , Epping‐Jordan, J. , … In collaboration with WHO/NIH Joint Project (2010a). Developing the World Health Organization Disability Assessment Schedule 2.0. Bulletin of the World Health Organization, 88(11), 815–823. DOI: 10.2471/BLT.09.067231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Üstün T. B., Kostanjsek N., Chatterji S., & Rehm J. (Eds). (2010b). Measuring health and disability. Manual for WHO Disability Assessment Schedule. WHODAS 2.0. Geneva: World Health Organization. [Google Scholar]
- Wells, S. , Flynn, A. , Graham, K. , Rehm, J. , Cairney, J. , Kates, N. , … Verjee, Z. (2011). Using a mobile laboratory to study mental health, addictions, and violence: A research plan. Challenges, 2(1), 1–18. DOI: 10.3390/challe2010001 [DOI] [Google Scholar]
- Wilber, N. , Mitra, M. , Walker, D. K. , & Allen, D. (2002). Disability as a public health issue: Findings and reflections from the Massachusetts Survey of Secondary Conditions. Milbank Quarterly, 80(2), 393–421. DOI: 10.1111/1468-0009.00009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (1980). International classification of impairments, disabilities and handicaps: A manual of classification relating to consequences of disease. Geneva: World Health Organization. [Google Scholar]
- World Health Organization (1997). International classification of impairments, activities and participation. A manual of dimensions of disablement and functioning. Beta‐1 draft for field trials. Geneva: World Health Organization. [Google Scholar]
- World Health Organization (2001). International classification of functioning, disability and health. Geneva: World Health Organization. [Google Scholar]


