Abstract
Domestic violence, in particular intimate partner violence (IPV), has been recognized as a leading cause of mortality and morbidity among women of reproductive age. The effects of IPV against women on their children's health, especially their nutritional status has received less attention but needs to be evaluated to understand the comprehensive public health implications of IPV. The aim of current study was to investigate the association between women's exposure to IPV and their children's nutritional status, using data from the 2007 Bangladesh Demographic and Health Survey (BDHS). Logistic regression models were used to estimate association between ever‐married women's lifetime exposure to physical and sexual violence by their spouses and nutritional status of their children under 5 years. Of 2042 women in the BDHS survey with at least one child under 5 years of age, 49.4% reported lifetime experience of physical partner violence while 18.4% reported experience of sexual partner violence. The prevalence of stunting, wasting and underweight in their children under 5 years was 44.3%, 18.4% and 42.0%, respectively. Women were more likely to have a stunted child if they had lifetime experience of physical IPV [odds ratio n = 2027 (OR)adj, 1.48; 95% confidence interval (CI), 1.23–1.79] or had been exposed to sexual IPV (n = 2027 ORadj, 1.28; 95% CI, 1.02–1.61). The present findings contribute to growing body of evidence showing that IPV can also compromise children's growth, supporting the need to incorporate efforts to address IPV in child health and nutrition programmes and policies.
Keywords: intimate partner violence, children, malnutrition, Bangladesh
Introduction
Domestic violence, in particular violence against women by their intimate partner, is a serious human rights abuse and public health concern that manifests as a complex pattern of physical, sexual, psychological and emotional abuse often accompanied by controlling behaviour (Garcia‐Moreno et al. 2006; Flury et al. 2010). Intimate partner violence (IPV) can affect women of any nationality regardless of their level of education, income, age or ethnicity (UNICEF 2000; Flury et al. 2010). The World Health Organization (WHO) multi‐country study on women's health and domestic violence reported lifetime experience of physical or sexual violence, or both, among 15–71% of ever partnered women (Garcia‐Moreno et al. 2006). IPV has been recognized as a leading cause of mortality and morbidity among women of reproductive age (Krug et al. 2002). In fact, constant association between IPV and a broad array of physical and mental health problems including injuries, gastrointestinal and gynaecological disorders, depression, post‐traumatic stress disorders and suicidality has been documented in several studies (Coker et al. 2000; Bonomi et al. 2006; Ellsberg et al. 2008; Ribeiro et al. 2009; Devries et al. 2011). Studies have also shown that negative consequences of IPV on women's mental and physical health can remain even if the actual act of violence has ceased (Bonomi et al. 2006; Ellsberg et al. 2008).
Negative consequences of IPV against women can be extended and may also affect their children's health both through direct and indirect pathways. IPV can negatively affect child's health indirectly by impairing maternal caretaking abilities. A wide range of physical and psychological problems induced by IPV can make abused mothers less physically and emotionally capable of providing their children's basic needs (Erel & Burman 1995; Levendosky & Graham‐Bermann 2001; Levendosky et al. 2003; Yount et al. 2011). Further, IPV can result in unintended pregnancy (Stephenson et al. 2008; Miller et al. 2010), which can also affect maternal caretaking behaviour (Cheng et al. 2009). In a more direct pathway, witnessing violence between parents may increase children's psychological stress, which has been shown to negatively influence their health (Wyman et al. 2007; Caserta et al. 2008). Further, IPV against women is also a risk factor for child abuse and maltreatment, (Ellsberg et al. 2000; Herrenkohl et al. 2008), which is also shown to negatively affect children's physical and mental health (Krug et al. 2002; Kitzmann et al. 2003; Shay‐Zapien & Bullock 2010).
Negative consequences of IPV on children's general health have previously been reported. In a national sample of data from five developing countries, IPV was found to be associated with child mortality in Kenya, Honduras and Malawi (Rico et al. 2011). The results of this study were consistent with those from previous studies in Bangladesh (Asling‐Monemi et al. 2008), India (Ackerson & Subramanian 2009) and Nicaragua (Asling‐Monemi et al. 2003). Higher odds of diarrhoea, respiratory tract infection and acute infant illnesses have been observed among the children of mothers who were exposed to IPV in Bangladesh (Asling‐Monemi et al. 2009a; Silverman et al. 2009) and Uganda (Karamagi et al. 2007).
Women's exposure to IPV has been shown to reduce birthweight (Rosen et al. 2007; Asling‐Monemi et al. 2009b, Shah & Shah 2010), but research evaluating the consequences of IPV against women on their children's nutritional status later in life is still limited, and at times, conflicting results have been shown. Studies using nationally representative samples of data showed an association between lifetime exposure to physical and/or sexual IPV and child stunting in children below 5 years of age in Kenya while no such association was shown in Egypt, Honduras, Malawi and Rwanda (Rico et al. 2011). In India, maternal exposure to multiple incidences of physical family violence in previous years was associated with all measurements of malnutrition including stunting, wasting and underweight among their 12–35–month old children (Ackerson & Subramanian 2008). In a hospital‐based, case control study in Brazil, higher odds of severe acute malnutrition was observed among the 1–24–month old children of mothers reporting severe physical partner violence in previous years (Hasselmann & Reichenheim 2006). A cohort study in rural Bangladesh showed an association between maternal exposure to any (physical, emotional and/or sexual) lifetime IPV and early childhood growth impairment (Asling‐Monemi et al. 2009b).
Child malnutrition is highly prevalent in south Asia (Pasricha & Biggs 2010). While several risk factors for child malnutrition in this region including food insecurity and maternal malnutrition have been identified (Black et al. 2008; Pasricha & Biggs 2010), evidence from India and selected geographical areas of Bangladesh showed IPV may also have an important contribution. The association between different forms of IPV (including physical and sexual violence) and child malnutrition still needs to be confirmed in large nationally representative studies. Besides, considering long‐term negative consequences of IPV both for survivor women (Ellsberg et al. 2008) and exposed children (Martin 2002; Shay‐Zapien & Bullock 2010), it is important to study women's lifetime exposure to IPV in these evaluations.
According to the WHO multi‐country study on women's health and domestic violence, between 53.4% (in urban) and 61.7% (in rural) women in Bangladesh reported lifetime experience of either sexual or physical or both kinds of partner violence (Garcia‐Moreno et al. 2006). The country also has one of the highest prevalence of underweight children (41%) in the world (UNICEF 2010). The present study aimed to evaluate the association between ever‐married Bangladeshi women's lifetime exposure to violence by their spouses and their pre‐school children's nutritional status using a nationally representative set of data.
Key messages
-
•
Both violence against women by their intimate partners as well as child malnutrition are highly prevalent in Bangladesh.
-
•
Women's exposure to IPV is associated with increased risk of having a stunted pre‐school–aged child.
-
•
There is an urgent need to increase efforts to prevent violence against women not only to improve women's health, but also that of their children's.
Materials and methods
Data
The current cross‐sectional study used data from the Bangladesh 2007 Demographic and Health Survey (2007 BDHS) conducted under the authority of the National Institute for Population Research and Training (NIPORT) of the Ministry of Health and Family Welfare [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009]. DHS provides nationally representative data on maternal and child health indicators in over than 85 countries [United States Agency for International Development (USAID) n.d.]. The 2007 BDHS used standardized two‐stage sampling of households representing the whole population living in private dwelling units in Bangladesh [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009]. The details of the sampling design are available elsewhere [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009]. Briefly, a team of trained field staff conducted face‐to‐face interviews with an adult member of 10 400 households (99.4% of eligible households) from 24 March to 11 August 2007. In each household, one adult member, either man or woman, was selected to answer the IPV questionnaire module. The selected ever‐married women aged 15–49 were asked about their experience of specific sexual and physical violence by either current or former husband. Anthropometric characteristics of women and their children aged under 5 years were also collected.
Background characteristics such as age, education, household wealth and place of residence of women selected for IPV component is shown to be similar to women not selected confirming that the selected women are representative of the entire population of adult women in the BDHS [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009].
Exposure: intimate partner violence
To assess women's experience of IPV, a shortened and modified conflict tactic scale was used, which measured physical or sexual partner violence [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009]. Each selected woman was asked if her current/former husband has ever (1) pushed, shacked or thrown something at her; (2) slapped her; (3) twisted her arm or pulled her hair; (4) punched her with his fist or with something that could hurt her; (5) kicked, dragged, or beat her up; (6) threatened or attacked her with a knife, gun, or any other weapon; (7) tried to choke or burn her on purpose; and (8) physically forced her to have sexual intercourse with him even when she did not want to [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009].
Using the collected IPV data, three binary exposure variables were developed: experience of any physical partner violence (y/n), experience of any sexual partner violence (y/n) and experience of any physical and/or sexual partner violence (y/n). As only ever‐married women were selected in 2007 BDHS, our measurement of IPV is in fact spousal violence and partner thus refers to current or former husband.
Outcome variable: nutritional status
Using the anthropometric indicators in the 2007 BDHS, nutritional status of children under 5 years of age was classified into underweight, wasted and stunted according to the WHO growth standard and criteria (World Health Organization Multicentre Growth Reference Study Group 2006). The detail of anthropometric measurements has been reported elsewhere [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009]. All children under 5 years of the selected women have been included in the analysis. Accordingly, three binary outcome variables were developed: whether or not the woman had any stunted child under 5 years, whether or not the woman had any wasted child under 5 years and whether or not the woman had any underweight child under 5 years.
Covariates
Based on previous research on child nutrition (Rahman & Chowdhury 2007; Jesmin et al. 2011), as well as determinants of IPV in the context of Bangladesh (Johnston & Naved 2008), the following factors were identified as potential confounding factors for this study: level of education (women and husband); household wealth; number of children under 5 years; rural or urban residence; marital duration; and woman's height and weight. Woman's and her husband's educational level was classified into four groups (none = 0; primary = 1; secondary = 2; and college and higher = 3). The household wealth index was generated using information on housing characteristics and household assets [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009]. The wealth index was divided into quintiles from 1 (lowest) to 5 (highest). Marital duration was classified into four groups (0–4 years; 5–9 years; 10–14 years; and more than 15 years).Women's weight and height was used to calculate body mass index (BMI), which was used to classify the women as either underweight (BMI < 18.5), normal (18.5 ≤ BMI ≤ 24.9) or overweight (BMI ≥ 25).
Ethical considerations
The original survey was administrated in accordance with the WHO ethical and safety guidelines for research on IPV. These included attaining individual informed consent and ensuring privacy and confidentiality in order to protect the safety of both respondents and field staff [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009]. Interviewers were all provided with a list of organizations helping women in difficult situations. They were trained to give this information in a safe and confidential way to women if they ask for any assistance [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009]. Strict confidentiality was maintained in handling the data. The data was only available to a small group of research team members and no information enabling identification of the study participants was reported. Identifiers of the participants were not available in the dataset for secondary analysis.
Statistical analysis
Descriptive characteristics of the study sample are presented by percentage and mean. We used chi‐squared to compare proportions. To adjust for confounding the identified potential confounding factors were in bivariate analyses assessed for correlation (P < 0.10) with both IPV and child nutrition (Table 2). If associated with both factors, they were included in the statistical models. Covariates were retained in the final models if they influenced the effect estimate more than 5%. Woman and husband's educational level and household wealth were kept in adjusted models as they changed the effects estimate more than 5%. Maternal height was retained in all statistical models as it is a strong predictor of child height. The crude and adjusted association between women's exposure to IPV and child nutritional status have been presented. All statistical models were adjusting for cluster sampling by use of generalized estimating equations. Statistical significance was considered if P < 0.05. For analyses, the Statistical Package for the Social Sciences (SPSS version 18.0; SPSS Inc., Chicago, IL, USA) was used.
Results
During 24 March to 11 August 2007, a total number of 10 996 ever‐married women were interviewed in BDHS [National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International 2009]. Among these women, 4781 had at least one child younger than 5 years and of these ever‐married women, 2042 had been selected to answer IPV module (Fig. 1).
Figure 1.
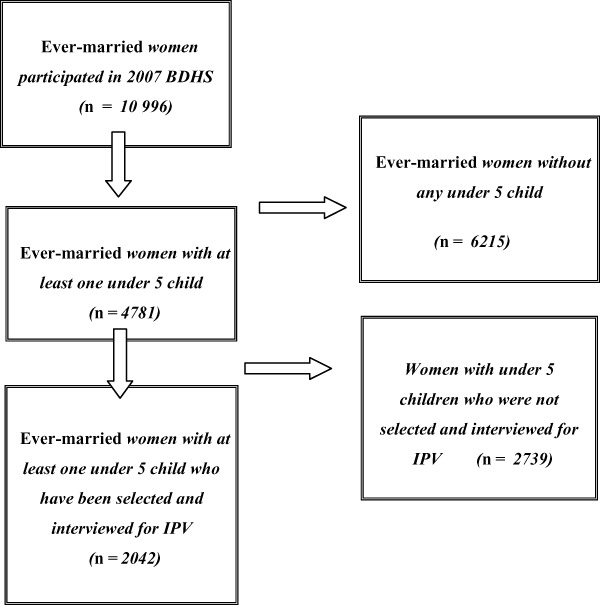
Flowchart of interviewed women. BDHS, Bangladesh Demographic and Health Survey; IPV, intimate partner violence.
Descriptive characteristics of the women and their children under 5 years included in the study are presented in Table 1. Most of the women were in their mid‐20s, and almost 28% had no formal education. Nearly one‐third of the women were malnourished (BMI < 18.5 kg m−2; Table 1).
Table 1.
Descriptive characteristics of women and their children under 5 years included in the study in Bangladesh 2007 demographic and health survey
| Women's sample (n = 2042)* | Children's sample (n = 2480)* | ||
|---|---|---|---|
| Variable | Variable | ||
| Place of residence, n (%) | Place of residence, n (%) | ||
| Rural | 1321 (64.7) | Rural | 1630 (65.7) |
| Urban | 721 (35.3) | Urban | 850 (34.3) |
| Age group, n (%) | Gender, n (%) | ||
| 15–19 | 269 (13.2) | Female | 1227 (49.5) |
| 20–24 | 636 (31.1) | ||
| 25–29 | 568 (27.8) | Nutritional status, n (%) | |
| 30–34 | 343 (16.8) | Stunting | 1021 (44.3) |
| 35–39 | 171 (8.4) | Wasting | 425 (18.4) |
| ≥40 | 55 (2.7) | Underweight | 967 (42.0) |
| Women's educational level, n (%) | |||
| Not educated | 576 (28.2) | ||
| Primary | 622 (30.5) | ||
| Secondary | 683 (33.5) | ||
| College and higher | 160 (7.8) | ||
| Husband's educational level, n (%) | |||
| Not educated | 711 (34.8) | ||
| Primary | 591 (29.0) | ||
| Secondary | 507 (24.8) | ||
| College and higher | 232 (11.4) | ||
| Woman is currently working, n (%) | |||
| Yes | 536 (26.2) | ||
| Women's body mass index, n (%) | |||
| <18.5 | 650 (32.1) | ||
| 18.5–25 | 1187 (58.7) | ||
| >25 | 187 (9.2) | ||
| Marital duration, n (%) | |||
| 0–4 years | 422 (20.7) | ||
| 5–9 years | 639 (31.3) | ||
| 10–14 years | 485 (23.8) | ||
| ≥15 years | 496 (24.3) | ||
| Exposed to intimate partner violence | |||
| Physical violence | 1008 (49.4) | ||
| Sexual violence | 375 (18.4) | ||
| Both/either physical or sexual violence | 1090 (53.4) | ||
Total sample size varies due to the missing values.
The average age of the 2480 children under 5 years included in the study was 29 months. A high level of malnutrition was observed among these children: 44.3% were stunted, 18.4% were wasted and 42.0% were underweight for their age (Table 1).
More than half of the women reported lifetime experience of either sexual/physical or both form of partner violence. Lifetime prevalence of sexual partner violence among these women was considerably less than physical violence (18.4% compared with 49.4%, respectively; Table 1).
In bivariate analyses, women in lower wealth quintile or with lower educational level were more likely to have experienced partner violence (Table 2). Prevalence of IPV was also higher if the woman was working or her husband and had lower level of education. Further, experience of IPV was more prevalent among malnourished women. No differences in IPV prevalence were found between rural and urban residence or in relation to women's age. Women were more likely to have a malnourished child if living in a rural area, if they were within lower wealth quintiles and if they or their husband's had lower level of education. Women with lower BMI more frequently had malnourished children (Table 2).
Table 2.
Descriptive statistics according to women's experience of IPV and their children nutritional status using Bangladesh 2007 demographic and health survey
| Descriptive characteristics (n = 2042)* | Any experience of IPV | P value † | Any stunted <5 children | P value † | Any wasted <5 children | P value † | Any underweight <5 children | P value † |
|---|---|---|---|---|---|---|---|---|
| Place of residence, n (%) | ||||||||
| Rural | 718/1321 (54.4) | 0.23 | 646/1321(48.9) | <0.01 | 283/1321(21.4) | 0.02 | 613/1321 (46.4) | <0.01 |
| Urban | 372/721 (51.6) | 274/721(38.0) | 123/721(17.1) | 264/721 (36.6) | ||||
| Age group (years), n (%) | ||||||||
| 15–19 | 153/269 (56.9) | 0.89 | 116/269 (43.1) | 0.31 | 55/269 (20.4) | 0.74 | 122/269 (45.4) | 0.47 |
| 20–24 | 338/636 (53.1) | 281/636 (44.2) | 132/636 (20.8) | 266/636 (41.8) | ||||
| 25–29 | 298/568 (52.5) | 245/568 (43.1) | 115/568 (20.2) | 234/568 (41.2) | ||||
| 30–34 | 181/343 (52.8) | 165/343 (48.1) | 68/343 (19.8) | 156/343 (45.5) | ||||
| 35–39 | 90/171 (52.6) | 86/171 (50.3) | 27/171 (15.8) | 75/171 (43.9) | ||||
| ≥40 | 30/55 (54.6) | 27/55 (49.1) | 9/55 (16.4) | 24/55 (43.6) | ||||
| Wealth index, n (%) | ||||||||
| Poorest | 279/447 (62.4) | <0.01 | 257/477 (57.5) | <0.01 | 111/447 (24.8) | <0.01 | 252/447 (56.4) | <0.01 |
| Poorer | 265/438 (60.5) | 244/438 (55.7) | 94/438 (21.5) | 218/438 (49.8) | ||||
| Middle | 200/355 (56.3) | 156/355 (43.9) | 73/355 (20.6) | 155/355 (43.7) | ||||
| Richer | 184/360 (51.1) | 139/360 (38.6) | 60/360 (16.7) | 131/360 (36.4) | ||||
| Richest | 162/442 (36.7) | 124/442 (28.1) | 68/442 (15.4) | 121/442 (27.4) | ||||
| Women's educational level, n (%) | ||||||||
| Not educated | 349/576 (60.6) | <0.01 | 334/576 (58.0) | <0.01 | 137/576 (23.8) | <0.01 | 306/576 (53.1) | <0.01 |
| Primary | 374/622 (60.1) | 298/622 (47.9) | 135/622 (21.7) | 298/622 (47.9) | ||||
| Secondary | 321/683 (47.0) | 254/683 (37.2) | 112/683 (16.4) | 237/683 (34.7) | ||||
| College and higher | 46/160 (28.7) | 33/160 (20.6) | 22/160 (13.8) | 35/160 (21.9) | ||||
| Husband's educational level, n (%) | ||||||||
| Not educated | 429/711 (60.3) | <0.01 | 391/711 (55.0) | <0.01 | 171/711 (24.1) | <0.01 | 364/711 (51.2) | <0.01 |
| Primary | 353/591 (59.7) | 285/591 (48.2) | 114/591 (19.3) | 286/591 (48.4) | ||||
| Secondary | 234/507 (46.2) | 188/507 (37.1) | 84/507 (16.6) | 173/507 (34.1) | ||||
| College and higher | 74/232 (31.9) | 56/232 (24.1) | 37/232 (15.9) | 54/232 (23.3) | ||||
| Woman is currently working, n (%) | ||||||||
| Yes | 326/536 (60.8) | <0.01 | 245/536 (54.7) | 0.72 | 93/536 (17.4) | 0.09 | 230/536 (42.9) | 1.00 |
| No | 764/1506 (50.7) | 675/1506 (44.8) | 313/1506 (20.8) | 647/1506 (43.0) | ||||
| Women's BMI, n (%) | ||||||||
| <18.5 | 381/650 (58.6) | <0.01 | 340/560 (52.3) | <0.01 | 178/650 (27.4) | <0.01 | 359/650 (55.2) | <0.01 |
| 18.5–25 | 639/1187 (53.8) | 534/1187 (45.0) | 211/1187 (17.8) | 479/1187 (40.4) | ||||
| >25 | 59/187 (31.6) | 42/187 (22.5) | 15/187 (8.0) | 36/187 (19.3) | ||||
| Number of children under 5 years | ||||||||
| 1 | 860/1629 (52.8) | 0.26 | 653/1629 (40.1) | <0.01 | 278/1629 (17.1) | <0.01 | 632/1629 (38.8) | <0.01 |
| 2 | 213/388 (54.9) | 247/388 (63.7) | 119/388 (30.7) | 226/388 (58.2) | ||||
| 3 | 17/25 (68.0) | 20/25 (80.0) | 9/25 (36.0) | 19/25 (76.0) | ||||
| Marital duration (years) | ||||||||
| 0–4 | 192/422 (45.5) | <0.01 | 164/422 (38.9) | <0.01 | 79/422 (18.7) | 0.84 | 158/422 (37.4) | 0.05 |
| 5–9 | 338/639 (52.9) | 279/639 (43.7) | 133/639 (20.8) | 272/639 (42.6) | ||||
| 10–14 | 276/485 (56.9) | 224/485 (46.2) | 98/485 (20.2) | 222/485 (45.8) | ||||
| ≥15 | 284/496 (57.3) | 253/496 (51.0) | 96/496 (19.4) | 225/496 (45.4) |
IPV, intimate partner violence; BMI, body mass index. *Total sample size varies because of the missing values. †Chi‐squared was used to compare proportion.
In unadjusted models, women who had lifetime experience of physical, sexual or any form of physical and/or sexual partner violence were significantly more likely to have at least one stunted child. Odds ratio (OR) for having any stunted child was 1.85 [95% confidence interval (CI), 1.54–2.21] for physical partner violence, (1.44; 95% CI, 1.16–1.81) for sexual partner violence and (1.84; 95% CI, 1.53–2.22) for physical and/or sexual partner violence, respectively (Table 3). Adjustment for potential confounders reduced the magnitude of this association to some extent; however, having any stunted children under 5 years remained significantly associated with women's lifetime experience of any physical (OR, 1.48; 95% CI, 1.23–1.79), sexual (OR, 1.28; 95% CI, 1.02–1.61) and physical and/or sexual (OR, 1.51; 95% CI, 1.25–1.84) violence by their partners.
Table 3.
Odds of having any stunted, wasted or underweight child under 5 years of age by women's lifetime experience of IPV in Bangladesh 2007 demographic and health survey
| Women's exposure to IPV (n = 2027) | Any stunted <5 child per woman | Any wasted <5 child per woman | Any underweight <5 child per woman | |||
|---|---|---|---|---|---|---|
| Unadjusted OR (95% CI) | Adjusted OR † (95% CI) | Unadjusted OR (95% CI) | Adjusted OR † (95% CI) | Unadjusted OR (95% CI) | Adjusted OR † (95% CI) | |
| No exposure | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) | 1.00 (Ref) |
| Exposure to physical IPV | 1.85* (1.54–2.21) | 1.48* (1.23–1.79) | 1.24 (0.99–1.56) | 1.12 (0.88–1.42) | 1.45* (1.21–1.73) | 1.14 (0.94–1.38) |
| Exposure to sexual IPV | 1.44* (1.16–1.81) | 1.28** (1.02–1.61) | 1.12 (0.86–1.45) | 1.04 (0.79–1.37) | 1.19 (0.95–1.48) | 1.03 (0.82–1.29) |
| Exposure to any form of physical and/or sexual IPV | 1.84* (1.53–2.22) | 1.51* (1.25–1.84) | 1.30** (1.04–1.64) | 1.19 (0.93–1.51) | 1.47* (1.23–1.76) | 1.18 (0.98–1.43) |
OR, odds ratio; CI, confidence interval; IPV, intimate partner violence. *P < 0.01; **P < 0.05. †Adjusted for woman's educational level, husband's educational level, woman's height, and household wealth using multivariate logistic regression.
Although there was a significant association between women's exposure to IPV and having a wasted or an underweight child under 5 years in unadjusted analyses, after adjustment for potential confounders, these associations did not remain statistically significant (Table 3).
Discussion
We found both a high prevalence of women who had experienced physical or sexual partner violence and a high prevalence of malnutrition in their children. Women who had any lifetime experience of IPV had significantly higher odds (1.51) of having a stunted child. No associations were found between women's exposure to IPV and childhood wasting or underweight.
Our finding of an association between women's exposure to IPV and child stunting was in line with that of a previous study in Matlab, Bangladesh (Asling‐Monemi et al. 2009b) where they reported lower height development in children up to 2 years of age as a results of IPV. Our results also confirmed previous results in India (Ackerson & Subramanian 2008) showing increased odds (1.14) of stunting in children 12–36 months with mothers with multiple experience of family violence in the previous year. Outside the continent, higher odds (1.36) of stunting have been reported among children of mothers with any lifetime exposure to IPV in Kenya (Rico et al. 2011) and with previous year's exposure to sexual partner violence in Liberia (Sobkoviak et al. 2012). The odds of stunting in our study was higher than that in India, which may possibly be explained by our inclusion of children up to 5 years of age. Considering the fact that violence is a pattern of behaviour that usually is perpetrated repeatedly (Garcia‐Moreno et al. 2006; Johnston & Naved 2008) and that stunting is the result of a cumulative negative experience developing over time, one could expect more children in our study to have time to become stunted as a result of IPV as compared with the younger children in India.
Although we did not find any statistically significant associations between women's exposure to IPV and child's wasting nor underweight, the association between these measures and IPV are reported in both previous studies in Bangladesh (Asling‐Monemi et al. 2009b) and India (Ackerson & Subramanian 2008). However, our non‐significant odds of wasting (1.19) and underweight (1.18) are much similar to the odds reported in India, wasting (1.18) and underweight (1.21) (Ackerson & Subramanian 2008). The much larger sample size in India may have allowed significant differences to be found suggesting that our sample size was limited in finding odds of this size. Further, wasting is commonly more prominent at lower age, and the larger age range in our study may have included children less prone to wasting, which may have contributed to lack of association.
We found that women's exposure to sexual partner violence was associated with increased risk of having a stunted child which, is in agreement with previous reports (Asling‐Monemi et al. 2009b; Rico et al. 2011; Sobkoviak et al. 2012). Considering negative influences of sexual partner violence on women's physical and mental health (Bonomi et al. 2006; Ellsberg et al. 2008), one could also expect association with child nutrition. However, it is difficult to disentangle association between different types of partner violence. In our study, there was a great deal of overlap such that 78% of women exposed to sexual partner violence also had experienced physical violence making it difficult to evaluate independent effect of sexual partner violence on child malnutrition.
There are several possible explanations for higher odds of malnutrition among children of abused women. IPV has been linked to maternal mental and physical health problems (Ellsberg et al. 2008; Naved & Akhtar 2008; Devries et al. 2011), which may affect pregnancy outcome and women's caring ability. Mothers are mainly primary caregivers of young children; accordingly, their physical and emotional health is critical for their children's health and well‐being. Women's experience of violence is often accompanied by high level of controlling behaviour in marriage and lower level of autonomy, self‐esteem and functional capacity (Forte et al. 1996; McCaw et al. 2007). Such mental and physical health impairment along with limited decision‐making authority can reduce mother's caregiving ability to meet child's physical and emotional needs (Shroff et al. 2009). Studies have linked exposure to IPV with mother's lower score in parenting style (Levendosky & Graham‐Bermann 2001) and inconsistent parenting behaviour (Levendosky & Graham‐Bermann 2000). Besides, maternal exposure to IPV has been documented to have negative effects on initiation (Lau & Chan 2007) and duration of breastfeeding (Silverman et al. 2006; Moraes et al. 2011) as well as mother–infant feeding interaction (Frith 2006). Several of these mechanism have been shown to be relevant for Bangladesh including maternal health (Ellsberg et al. 2008; Naved & Akhtar 2008), birthweight (Asling‐Monemi et al. 2009b) and feeding interaction (Frith 2006).
Moreover, children witnessing aggressive behaviour between parents may have a deregulation of their stress–responsive system and subsequently an increase in biomarkers of stress (Davies et al. 2008), which can disturb their metabolic activity and energy release and result in growth impairment (Fernald & Grantham‐McGregor 2002; Mead et al. 2010). Furthermore, exposure to IPV can undermine children's emotional security and increase their psychological stress (Kitzmann et al. 2003; Hibel et al. 2009), which has the potential to alter children's immune functions and increase their susceptibility to illnesses (Wyman et al. 2007; Caserta et al. 2008) and eventual malnutrition (Checkley et al. 2008, Weisz et al. 2011). Finally, maternal exposure to IPV could be an important predictor of child maltreatment (Herrenkohl et al. 2008). Negative effects of being abused on children's physical and mental health as well as growth failure have been documented in several studies (Olivan 2003; Scarborough et al. 2009).
Our study has limitations that must be considered when interpreting the results. Although great effort has been made by the DHS in order to ensure validity of IPV data by utilizing the most widely accepted measurement tools and emphasizing privacy and confidentiality principles, we should not undervalue the potential bias in the collected data. Evidence show under‐reporting of violence exposure is generally more common than over‐reporting (Ellsberg et al. 2001). Further, because we studied women's lifetime experience of IPV while it appears not likely, our data might be affected by recall bias possibly leading to under‐reporting; although, if under disclosure is the case, it tends to weaken rather than strengthen the association between IPV and the reported outcome. It may also be discussed whether estimating lifetime exposure rather than a shorter period may provide a more relevant indicator of IPV in relation to cumulative experiences such as stunting. In WHO multi‐country study there was substantially higher (approximate double) prevalence if exposure had been estimated over lifetime or previous year (Garcia‐Moreno et al. 2006). Considering the lasting effect of IPV on maternal health it appears important to capture lifetime exposure to IPV.
Our study sample includes only ever‐married women with living children under 5 years of age. Unmarried mothers are rare in Bangladesh and we are likely to have a representative sample of women with children. However, childhood malnutrition is one of the leading causes of mortality in children under 5 years in developing countries (Faruque et al. 2008) including in Bangladesh. Thus, some of the most malnourished children may not have survived leaving the better‐off children to be included in the study.
Further, although we applied a rigorous adjustment for confounding factors, there might be residual confounding. Finally, the nature of cross‐sectional study did not allow us to make statements on causal relation. However, we find it less likely that our observed effect is due to reversed causality i.e. stress and frustration resulting from poor child growth would result in increased risk of partner abuse than a matter of the opposite.
Despite the limitations mentioned earlier, our study contributes to a small, but growing body of literature demonstrating an association between IPV and young child malnutrition. Although the nature of IPV depends on the social, demographic and cultural context in which it occurs, there is no reason to assume that negative association with children's health and well‐being is restricted to this setting only. High prevalence of IPV and its association with poor maternal and child health stresses the importance to urgently increase efforts to prevent IPV not only for the sake of the abused women but also for the sake of their children.
Source of funding
None.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
SZ analyzed and interpreted the data and wrote the initial draft of the manuscript. ECE provided guidance in data analyses and interpretation of results. RTN assisted in the interpretation of results. All co‐authors participated in manuscript preparation and critically reviewed all sections of the text for important intellectual content.
Acknowledgement
The authors wish to acknowledge measure DHS (http://www.measuredhs.com) for providing us access to Bangladesh Demographic and Health Survey 2007 data. The authors also gratefully acknowledge Professor Lars Ake Persson for his invaluable comments and suggestions.
References
- Ackerson L.K. & Subramanian S.V. ( 2008. ) Domestic violence and chronic malnutrition among women and children in India . American Journal of Epidemiology 167 , 1188 – 1196 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ackerson L.K. & Subramanian S.V. ( 2009. ) Intimate partner violence and death among infants and children in India . Pediatrics 124 , e878 – e889 . [DOI] [PubMed] [Google Scholar]
- Asling‐Monemi K. , Pena R. , Ellsberg M.C. & Persson L.A. ( 2003. ) Violence against women increases the risk of infant and child mortality: a case‐referent study in Nicaragua . Bulletin of the World Health Organization 81 , 10 – 16 . [PMC free article] [PubMed] [Google Scholar]
- Asling‐Monemi K. , Tabassum Naved R. & Persson L.A. ( 2008. ) Violence against women and the risk of under‐five mortality: analysis of community‐based data from rural Bangladesh . Acta Paediatrica (Oslo, Norway: 1992) 97 , 226 – 232 . [DOI] [PubMed] [Google Scholar]
- Asling‐Monemi K. , Naved R.T. & Persson L.A. ( 2009a. ) Violence against women and increases in the risk of diarrheal disease and respiratory tract infections in infancy: a prospective cohort study in Bangladesh . Archives of Pediatrics & Adolescent Medicine 163 , 931 – 936 . [DOI] [PubMed] [Google Scholar]
- Asling‐Monemi K. , Naved R.T. & Persson L.A. ( 2009b. ) Violence against women and the risk of fetal and early childhood growth impairment: a cohort study in rural Bangladesh . Archives of Disease in Childhood 94 , 775 – 779 . [DOI] [PubMed] [Google Scholar]
- Black R.E. , Allen L.H. , Bhutta Z.A. , Caulfield L.E. , De Onis M. , Ezzati M. , Mathers C. & Rivera J. ( 2008. ) Maternal and child undernutrition: global and regional exposures and health consequences . Lancet 371 , 243 – 260 . [DOI] [PubMed] [Google Scholar]
- Bonomi A.E. , Thompson R.S. , Anderson M. , Reid R.J. , Carrell D. , Dimer J.A. et al . ( 2006. ) Intimate partner violence and women's physical, mental, and social functioning . American Journal of Preventive Medicine 30 , 458 – 466 . [DOI] [PubMed] [Google Scholar]
- Caserta M.T. , O'connor T.G. , Wyman P.A. , Wang H. , Moynihan J. , Cross W. et al . ( 2008. ) The associations between psychosocial stress and the frequency of illness, and innate and adaptive immune function in children . Brain, Behavior, and Immunity 22 , 933 – 940 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Checkley W. , Buckley G. , Gilman R.H. , Assis A.M. , Guerrant R.L. , Morris S.S. et al . ( 2008. ) Multi‐country analysis of the effects of diarrhoea on childhood stunting . International Journal of Epidemiology 37 , 816 – 830 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng D. , Schwarz E.B. , Douglas E. & Horon I. ( 2009. ) Unintended pregnancy and associated maternal preconception, prenatal and postpartum behaviors . Contraception 79 , 194 – 198 . [DOI] [PubMed] [Google Scholar]
- Coker A.L. , Smith P.H. , Bethea L. , King M.R. & Mckeown R.E. ( 2000. ) Physical health consequences of physical and psychological intimate partner violence . Archives of Family Medicine 9 , 451 – 457 . [DOI] [PubMed] [Google Scholar]
- Davies P.T. , Sturge‐Apple M.L. , Cicchetti D. & Cummings E.M. ( 2008. ) Adrenocortical underpinnings of children's psychological reactivity to interparental conflict . Child Development 79 , 1693 – 1706 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devries K. , Watts C. , Yoshihama M. , Kiss L. , Schraiber L.B. , Deyessa N. et al . ( 2011. ) Violence against women is strongly associated with suicide attempts: evidence from the WHO multi‐country study on women's health and domestic violence against women . Social Science & Medicine (1982) 73 , 79 – 86 . [DOI] [PubMed] [Google Scholar]
- Ellsberg M. , Pena R. , Herrera A. , Liljestrand J. & Winkvist A. ( 2000. ) Candies in hell: women's experiences of violence in Nicaragua . Social Science & Medicine (1982) 51 , 1595 – 1610 . [DOI] [PubMed] [Google Scholar]
- Ellsberg M. , Heise L. , Pena R. , Agurto S. & Winkvist A. ( 2001. ) Researching domestic violence against women: methodological and ethical considerations . Studies in Family Planning 32 , 1 – 16 . [DOI] [PubMed] [Google Scholar]
- Ellsberg M. , Jansen H.A. , Heise L. , Watts C.H. & Garcia‐Moreno C. ( 2008. ) Intimate partner violence and women's physical and mental health in the WHO multi‐country study on women's health and domestic violence: an observational study . Lancet 371 , 1165 – 1172 . [DOI] [PubMed] [Google Scholar]
- Erel O. & Burman B. ( 1995. ) Interrelatedness of marital relations and parent‐child relations: a meta‐analytic review . Psychological Bulletin 118 , 108 – 132 . [DOI] [PubMed] [Google Scholar]
- Faruque A.S. , Ahmed A.M. , Ahmed T. , Islam M.M. , Hossain M.I. , Roy S.K. et al . ( 2008. ) Nutrition: basis for healthy children and mothers in Bangladesh . Journal of Health, Population, and Nutrition 26 , 325 – 339 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernald L.C. & Grantham‐Mcgregor S.M. ( 2002. ) Growth retardation is associated with changes in the stress response system and behavior in school‐aged Jamaican children . The Journal of Nutrition 132 , 3674 – 3679 . [DOI] [PubMed] [Google Scholar]
- Flury M. , Nyberg E. & Riecher‐Rossler A. ( 2010. ) DV against women: definitions, epidemiology, risk factors and consequences . Swiss Medical Weekly: Official Journal of the Swiss Society of Infectious Diseases, the Swiss Society of Internal Medicine, the Swiss Society of Pneumology 140 , w13099 . [DOI] [PubMed] [Google Scholar]
- Forte J.A. , Franks D.D. & Rigsby D. ( 1996. ) Asymmetrical role‐taking: comparing battered and nonbattered women . Social Work 41 , 59 – 73 . [DOI] [PubMed] [Google Scholar]
- Frith A.L. ( 2006. ) The Influence of Maternal Nutritional Interventions and Stress on Maternal‐infant Interaction in Bangladesh. PH.D. CORNELL UNIVERSITY .
- Garcia‐Moreno C. , Jansen H.A. , Ellsberg M. , Heise L. & Watts C.H. ( 2006. ) Prevalence of intimate partner violence: findings from the WHO multi‐country study on women's health and domestic violence . Lancet 368 , 1260 – 1269 . [DOI] [PubMed] [Google Scholar]
- Hasselmann M.H. & Reichenheim M.E. ( 2006. ) Parental violence and the occurrence of severe and acute malnutrition in childhood . Paediatric and Perinatal Epidemiology 20 , 299 – 311 . [DOI] [PubMed] [Google Scholar]
- Herrenkohl T.I. , Sousa C. , Tajima E.A. , Herrenkohl R.C. & Moylan C.A. ( 2008. ) Intersection of child abuse and children's exposure to domestic violence . Trauma Violence Abuse 9 , 84 – 99 . [DOI] [PubMed] [Google Scholar]
- Hibel L.C. , Granger D.A. , Blair C. & Cox M.J. ( 2009. ) Intimate partner violence moderates the association between mother–infant adrenocortical activity across an emotional challenge . Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43) 23 , 615 – 625 . [DOI] [PubMed] [Google Scholar]
- Jesmin A. , Yamamoto S.S. , Malik A.A. & Haque M.A. ( 2011. ) Prevalence and determinants of chronic malnutrition among preschool children: a cross‐sectional study in Dhaka City, Bangladesh . Journal of Health, Population, and Nutrition 29 , 494 – 499 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnston H.B. & Naved R.T. ( 2008. ) Spousal violence in Bangladesh: a call for a public‐health response . Journal of Health, Population, and Nutrition 26 , 366 – 377 . [PMC free article] [PubMed] [Google Scholar]
- Karamagi C.A. , Tumwine J.K. , Tylleskar T. & Heggenhougen K. ( 2007. ) Intimate partner violence and infant morbidity: evidence of an association from a population‐based study in eastern Uganda in 2003 . BMC Pediatrics [Electronic Resource] 7 , 34 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kitzmann K.M. , Gaylord N.K. , Holt A.R. & Kenny E.D. ( 2003. ) Child witnesses to domestic violence: a meta‐analytic review . Journal of Consulting and Clinical Psychology 71 , 339 – 352 . [DOI] [PubMed] [Google Scholar]
- Krug E.G. , Dahlberg L.L. , Mercy J.A. , Zwi A.B. & Lozano R. ( eds ) ( 2002. ) World Report on Violence and Health . World Health Organization; : Geneva, Switzerland . [Google Scholar]
- Lau Y. & Chan K.S. ( 2007. ) Influence of intimate partner violence during pregnancy and early postpartum depressive symptoms on breastfeeding among Chinese women in Hong Kong . Journal of Midwifery & Women's Health 52 , e15 – e20 . [DOI] [PubMed] [Google Scholar]
- Levendosky A.A. & Graham‐Bermann S.A. ( 2000. ) Trauma and parenting in battered women: an addition to an ecological model of parenting . Journal of Aggression, Maltreatment & Trauma 3 , 25 – 35 . [Google Scholar]
- Levendosky A.A. & Graham‐Bermann S.A. ( 2001. ) Parenting in battered women: the effects of domestic violence on women and their children . Journal of Family Violence 16 , 171 – 192 . [Google Scholar]
- Levendosky A.A. , Huth‐Bocks A.C. , Shapiro D.L. & Semel M.A. ( 2003. ) The impact of domestic violence on the maternal–child relationship and preschool‐age children's functioning . Journal of Family Psychology: JFP: Journal of the Division of Family Psychology of the American Psychological Association (Division 43) 17 , 275 – 287 . [DOI] [PubMed] [Google Scholar]
- Martin S.G. ( 2002. ) Children exposed to domestic violence: psychological considerations for health care practitioners . Holistic Nursing Practice 16 , 7 – 15 . [DOI] [PubMed] [Google Scholar]
- Mccaw B. , Golding J.M. , Farley M. & Minkoff J.R. ( 2007. ) Domestic violence and abuse, health status, and social functioning . Women & Health 45 , 1 – 23 . [DOI] [PubMed] [Google Scholar]
- Mead H.K. , Beauchaine T.P. & Shannon K.E. ( 2010. ) Neurobiological adaptations to violence across development . Development and Psychopathology 22 , 1 – 22 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller E. , Decker M.R. , Mccauley H.L. , Tancredi D.J. , Levenson R.R. , Waldman J. , Schoenwald P. & Silverman J.G. ( 2010. ) Pregnancy coercion, intimate partner violence and unintended pregnancy . Contraception 81 , 316 – 322 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moraes C.L. , De Oliveira A.S. , Reichenheim M.E. & Lobato G. ( 2011. ) Severe physical violence between intimate partners during pregnancy: a risk factor for early cessation of exclusive breast‐feeding . Public Health Nutrition 24 , 1 – 8 . [DOI] [PubMed] [Google Scholar]
- National Institute of Population Research and Training (NIPORT), Mitra and Associates, & Macro International ( 2009. ) Bangladesh Demographic and Health Survey 2007 . NIPORT, Mitra and Associates, and Macro International: Dhaka, Bangladesh and Calverton, MD .
- Naved R.T. & Akhtar N. ( 2008. ) Spousal violence against women and suicidal ideation in Bangladesh . Women's Health Issues: Official Publication of the Jacobs Institute of Women's Health 18 , 442 – 452 . [DOI] [PubMed] [Google Scholar]
- Olivan G. ( 2003. ) Catch‐up growth assessment in long‐term physically neglected and emotionally abused preschool age male children . Child Abuse & Neglect 27 , 103 – 108 . [DOI] [PubMed] [Google Scholar]
- Pasricha S.R. & Biggs B.A. ( 2010. ) Undernutrition among children in South and South‐East Asia . Journal of Paediatrics and Child Health 46 , 497 – 503 . [DOI] [PubMed] [Google Scholar]
- Rahman A. & Chowdhury S. ( 2007. ) Determinants of chronic malnutrition among preschool children in Bangladesh . Journal of Biosocial Science 39 , 161 – 173 . [DOI] [PubMed] [Google Scholar]
- Ribeiro W.S. , Andreoli S.B. , Ferri C.P. , Prince M. & Mari J.J. ( 2009. ) Exposure to violence and mental health problems in low and middle‐income countries: a literature review] . Revista Brasileira de Psiquiatria (Sao Paulo, Brazil: 1999) 31 ( Suppl. 2 ), S49 – S57 . [DOI] [PubMed] [Google Scholar]
- Rico E. , Fenn B. , Abramsky T. & Watts C. ( 2011. ) Associations between maternal experiences of intimate partner violence and child nutrition and mortality: findings from Demographic and Health Surveys in Egypt, Honduras, Kenya, Malawi and Rwanda . Journal of Epidemiology and Community Health 65 , 360 – 367 . [DOI] [PubMed] [Google Scholar]
- Rosen D. , Seng J.S. , Tolman R.M. & Mallinger G. ( 2007. ) Intimate partner violence, depression, and posttraumatic stress disorder as additional predictors of low birth weight infants among low‐income mothers . Journal of Interpersonal Violence 22 , 1305 – 1314 . [DOI] [PubMed] [Google Scholar]
- Scarborough A.A. , Lloyd E.C. & Barth R.P. ( 2009. ) Maltreated infants and toddlers: predictors of developmental delay . Journal of Developmental and Behavioral Pediatrics: JDBP 30 , 489 – 498 . [DOI] [PubMed] [Google Scholar]
- Shah P.S. & Shah J. ( 2010. ) Maternal exposure t domestic violence and pregnancy and birth outcomes: a systematic review and meta‐analyses . Journal of Women's Health 19 , 2017 – 2031 . [DOI] [PubMed] [Google Scholar]
- Shay‐Zapien G. & Bullock L. ( 2010. ) Impact of intimate partner violence on maternal child health . MCN. The American Journal of Maternal Child Nursing 35 , 206 – 212 . [DOI] [PubMed] [Google Scholar]
- Shroff M. , Griffiths P. , Adair L. , Suchindran C. & Bentley M. ( 2009. ) Maternal autonomy is inversely related to child stunting in Andhra Pradesh, India . Maternal & Child Nutrition 5 , 64 – 74 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverman J.G. , Decker M.R. , Reed E. & Raj A. ( 2006. ) Intimate partner violence around the time of pregnancy: association with breastfeeding behavior . Journal of women's health 15 , 934 – 940 . [DOI] [PubMed] [Google Scholar]
- Silverman J.G. , Decker M.R. , Gupta J. , Kapur N. , Raj A. & Naved R.T. ( 2009. ) Maternal experiences of intimate partner violence and child morbidity in Bangladesh: evidence from a national Bangladeshi sample . Archives of Pediatrics & Adolescent Medicine 163 , 700 – 705 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobkoviak R.M. , Yount K.M. & Halim N. ( 2012. ) Domestic violence and child nutrition in Liberia . Social Science & Medicine 74 , 103 – 111 . [DOI] [PubMed] [Google Scholar]
- Stephenson R. , Koenig M.A. , Acharya R. & Roy T.K. ( 2008. ) Domestic violence, contraceptive use, and unwanted pregnancy in rural India . Studies in Family Planning 39 , 177 – 186 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Children's Fund (UNICEF) ( 2000. ) Domestic violence against women and girls . United Nations Children's Fund: Florence, Italy . [PMC free article] [PubMed]
- United Nations Children's Fund (UNICEF) ( 2010. ) Bangladesh Statistics Available at: http://www.unicef.org/infobycountry/bangladesh_bangladesh_statistics.html#74 (Accessed 11 February 2011 ).
- United States Agency for International Development (USAID) ( n.d.), Measure DHS: quality Information to Plan, Monitor, and Improve Population, Health, and Nutrition Programs Available at: http://www.measuredhs.com/Who-We-Are/upload/MEASURE_DHS_Brochure.pdf (Accessed 22 January 2011 ).
- Weisz A. , Meuli G. , Thakwalakwa C. , Trehan I. , Maleta K. & Manary M. ( 2011. ) The duration of diarrhea and fever is associated with growth faltering in rural Malawian children aged 6–18 months . Nutrition Journal 10 , 25 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization Multicentre Growth Reference Study Group ( 2006. ) WHO Child Growth Standards: Length/Height‐for‐age, Weight‐for‐age, Weight‐for‐length, Weight‐for‐height and Body Mass Index‐for‐age: Methods and Development . World Health Organization; : Geneva, Switzerland . [Google Scholar]
- Wyman P.A. , Moynihan J. , Eberly S. , Cox C. , Cross W. , Jin X. et al . ( 2007. ) Association of family stress with natural killer cell activity and the frequency of illnesses in children . Archives of Pediatrics & Adolescent Medicine 161 , 228 – 234 . [DOI] [PubMed] [Google Scholar]
- Yount K.M. , Digirolamo A.M. & Ramakrishnan U. ( 2011. ) Impacts of domestic violence on child growth and nutrition: a conceptual review of the pathways of influence . Social Science & Medicine (1982) 72 , 1534 – 1554 . [DOI] [PubMed] [Google Scholar]


