Abstract
As researchers increasingly focus on early infancy as a critical period of development, there is a greater need for methodological tools that can address all aspects of infant growth. Infant skinfold measures, in particular, are measurements in need of reliable reference standards that encompass all ages of infants and provide an accurate assessment of the relative fatness of a population. This report evaluates three published reference standards for infant skinfold measurements: Tanner–Whitehouse, Cambridge Infant Growth Study, and the World Health Organization (WHO) Child Growth Standards. To assess these standards, triceps skinfolds from a population of rural Kenyan infants (n = 250) and triceps skinfolds and subscapular skinfolds from infants in the National Health and Nutrition Examination Survey 1999–2002 (NHANES; n = 1197) were calculated as z‐scores from the lambda‐mu‐sigma curves provided by each reference population. The Tanner–Whitehouse standards represented both the Kenyan and US populations as lean, while the Cambridge standards represented both populations as overfat. The distribution of z‐scores based on the WHO standards fell in the middle, but excluded infants from both populations who were below the age of 3 months. Based on these results, the WHO reference standard is the best skinfold reference standard for infants over the age of 3 months. For populations with infants of all ages, the Tanner–Whitehouse standards are recommended, despite representing both study populations as underfat. Ideally, the WHO will extend their reference standard to include infants between the ages of 0 and 3 months.
Keywords: anthropometry, Kenya, National Health and Nutrition Examination Survey, body composition, infant growth
Introduction
There is increasing research interest focused on early infancy as a critical period during which later growth and health outcomes are partially programmed (Gluckman et al. 2007). While traditional indicators of nutritional status, such as height, weight and age‐based z‐scores, are widely used for developmental research, the specifics of early body composition is recognized as increasingly important to later‐life outcomes (Wells et al. 2007). Complicating studies of the development of fat deposits is the non‐linear development of fat during infancy. During the first 3–6 months of life, infants rapidly develop fat stores to as a protection against pathogen stress associated with weaning (Kuzawa 1998). After 6 months of age, fat levels decline as fat is mobilized to support brain development, growth and the developing immune system (Leonard et al. 2010).
The measurement of fat mass in infants is an imperfect, though valuable, research tool for researchers and clinicians. There are a variety of technologies available for fat measurement in laboratory settings, including bioelectrical impedance analysis, dual‐energy X‐ray absorptiometry, isotope dilution analysis, magnetic resonance imaging and others (Wells & Fewtrell 2006). In field settings, inexpensive and simple techniques such as body mass index (BMI) or skinfolds can be used to quickly assess body composition. While BMI's relationship to body composition is complex, skinfolds represent a reasonable approximation of the relative fat of an individual (Wells & Fewtrell 2006). Currently, the best use of skinfold measurements is to use raw skinfold measurement as a measure of regional fat deposits. However, because fat acquisition is not straightforward across the early postnatal period, standardizing skinfold measurements becomes important to facilitate both within and between population analyses. Fortunately, several skinfold reference standards are available to assess fat development in early infancy.
The first reference standard considered by this report are the Tanner–Whitehouse standards, which are a revision of skinfold standards originally published by the authors 15 years prior (Tanner & Whitehouse 1975). These reference standards were based on UK children and were intended to represent actual, not optimal infants and children present in the country during that time. The second reference standard, based on the Cambridge Infant Growth study (referred to as Cambridge standards throughout), was created in response to increasing criticism of the Tanner–Whitehouse standards (Paul et al. 1998). It was recognized that the Tanner–Whitehouse reference population was overfat, based largely on their reliance on formula feeding and early supplementation. The Cambridge standards were developed based on mostly white, UK infants from the Cambridge area. The final reference standard, the World Health Organization Child Growth Standards (referred to as WHO standards throughout) are the most recent reference standard available (WHO Multicentre Growth Reference Study Group 2006). The WHO standards were designed to represent a population of breastfed children that experienced ideal growth conditions in order to facilitate comparisons between diverse global populations. For all three reference standards, values for both triceps skinfold and subscapular skinfold are available.
The goal of this report is to evaluate these three reference standards using data from an undernourished Kenyan population as well as a well‐nourished US population. Z‐scores from the reference standards will be used to test the relative fatness of each standard, the distribution of each z‐scores for both populations, and the overall suitability of each standard for the available data sets. It is hoped that this paper will help researchers make informed choices about the selection of a reference standard for as they assess early infant nutritional status.
Key messages
The measurement of infant skinfolds requires reliable reference standards for within and between population comparisons.
Three available skinfold reference standards were evaluated using data from Kenyan and US populations: Tanner–Whitehouse, Cambridge Infant Growth Study and World Health Organization (WHO) Child Growth Standards.
WHO standards are recommended for infants above 3 months of age, and it is hoped that these standards will be extended to include young infants.
Materials and methods
Two study populations were used to test the three reference populations. The first population is a cross‐sectional sample of breastfeeding Kenyan infants between the ages of 0 and 24 months (n = 250). These infants experience significant nutritional stress with age (Miller & McConnell 2012), as is typical of infants in this region (Victora et al. 2010). Only triceps skinfold measurements are available for this population. The second population is a US population taken from the 1999–2002 National Health and Nutrition Examination Survey (NHANES). Infants who were between the ages of 0 and 24 months and who had both triceps and subscapular skinfold measurements available were included in the study (n = 1169). Ethical permissions for the collection of the Kenyan data were given by the Institutional Review Board at the University of Michigan; the secondary analysis of NHANES data is exempt from ethical review.
In order to transform skinfold measurements, the lambda‐mu‐sigma (LMS) values published for Cambridge and Tanner–Whitehouse were entered into SAS as equations and calculated for both US and Kenyan infants (Davies et al. 1993; Paul et al. 1998). Software provided by the WHO was used transform skinfold measurements using the WHO reference standards (who anthro 2010). The resultant z‐scores were analysed based on their mean and standard deviation (SD), their distribution, and how representative they are of the underlying study population.
Results
Means, medians and SDs of age, height, weight, triceps skinfold, subscapular skinfold and the corresponding z‐scores for the NHANES US infants and the Kenyan infants are shown in Table 1. The Tanner–Whitehouse reference standard produced mean negative triceps skinfold z‐scores for both the Kenyan and US populations. By contrast, the Cambridge reference standards gave high mean z‐scores for both populations, each scoring above +1 SD compared with the reference group. Finally, the WHO standards give intermediate, but positive, mean z‐scores for both the Kenyan and US infants. Subscapular skinfold z‐score means were positive for WHO and Tanner–Whitehouse standards and negative for the Cambridge standard for the US infant population.
Table 1.
Means, medians and SD of descriptive statistics and z‐scores
| Kenyan infants | US infants | |||||
|---|---|---|---|---|---|---|
| (n = 250) | (n = 1197) | |||||
| Mean | Median | SD | Mean | Median | SD | |
| Age (mo) | 10.6 | 10.3 | ±6.1 | 11.9 | 11.0 | ±6.2 |
| Sex (% male) | 46% | 53% | ||||
| Triceps skinfold (mm) | 9.3 | 9.2 | ±2.5 | 10.4 | 10.1 | ±2.6 |
| Subscapular skinfold (mm) | – | 7.7 | 7.4 | ±2.0 | ||
| Triceps skinfold‐for‐age z‐score | ||||||
| Tanner–Whitehouse | 0.79 | 0.79 | ±1.0 | 0.41 | 0.54 | ±1.0 |
| Cambridge | 1.19 | 1.33 | ±1.4 | 1.67 | 1.77 | ±1.5 |
| WHO Child Growth Standards | 0.42* | 0.61* | ±1.5* | 0.92 † | 0.90 † | ±1.2 † |
| Subscapular skinfold‐for‐age z‐score | ||||||
| Tanner–Whitehouse | – | 0.24 | 0.25 | ±0.91 | ||
| Cambridge | – | 0.74 | 0.78 | ±1.0 | ||
| WHO Child Growth Standards | – | 0.54 † | 0.59 † | ±1.3 † | ||
SD, standard deviation. *n = 218. † n = 1169.
Figure 1 shows the histogram z‐scores for triceps skinfolds for both Kenyan and US infants for each of the three standards. The skew and kurtosis for each histogram was calculated. All skews were between ±1 for all skinfold z‐scores across all standards, indicating that the z‐scores generated by all three standards were not overly skewed. The kurtosis for all z‐score distributions ranged between 0 and 1.5, indicating that the distributions skewed slightly more towards the tail ends of the distribution compared with a normal Gaussian distribution. Extreme values may be over‐represented in these z‐scores, although whether this is due to the sample populations or the reference populations is unclear.
Figure 1.
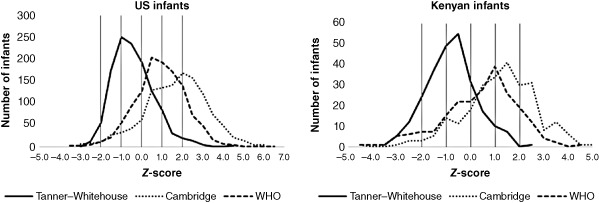
Histographs/frequency polygons of triceps skinfold‐for‐age z‐scores for US and Kenyan infants for each reference population [Tanner–Whitehouse, Cambridge, World Health Organization (WHO)].
Not all skinfold measurements could be transformed using the WHO standards, as the reference population is only available for infants three months of age and older. Using the WHO standards excluded 12.8% of the Kenyan infants (n = 32) and 2.3% of the US infants (n = 28).
Discussion
The results indicate that each reference population fit the data in a different manner. The Tanner–Whitehouse standards are relatively high fat, giving negative z‐scores to a large proportion of both the Kenyan and US populations. The Cambridge standards have the opposite problem: they are relatively lean. Both the Kenyan and the US mean triceps skinfold z‐scores were above 1, meaning that a large proportion of infants in these populations would be considered overfat. The WHO standards best represented the Kenyan population in terms of relative fatness, with the triceps z‐score mean being closest to 0. However, this growth standard excluded an eighth of the Kenyan infants, making it ultimately inappropriate for this population. It fared slightly better with the US population, excluding only 2.5% of young infants from analysis. It did represent the US population as overfat; however, this may in fact be a true representation of the nutritional status of these infants.
Each reference standard posed practical difficulties as well. The Cambridge and Tanner–Whitehouse reference standards were published as LMS values by sex for each age (in months) that must be used in LMS equations. These equations must be transcribed by hand into a software program that will calculate the resultant z‐scores. This method is time consuming and prone to mathematical errors. Equations and z‐scores should be checked for errors and for undefined numbers. By contrast, the WHO offers both their own native software (who anthro 2010) as well as macros for sas, stata, s‐plus, r and spss for calculating z‐scores. Of the three, the WHO Child Growth Standards are the most accessible and easiest to implement by nutritional researchers.
Of the three, the WHO Child Growth Standards best represents the ideal growth of a breastfed population and this standard is recommended for those who have populations of infants that are greater than 3 months of age. Ideally, the WHO would extend these reference standards to birth so that fat development in very young infants can be quantified relative to older infants. For those populations that include young infants, the Tanner–Whitehouse standards represent the pattern of infant fat development more accurately than the Cambridge standards, although they will mostly likely return skinfold z‐scores that are too low. The Cambridge standards, unfortunately, represent even undernourished Kenyan infants as very overfat, and do not represent the typical pattern of infant fat development. Based on the results of this report, the Cambridge standards cannot be recommended for population work at this time.
Source of funding
Funding for the study was from NSF DDIG (Grant Number BCS‐05750779), and the Leakey Foundation General Research Grant.
Conflicts of interest
The author has no conflict of interest to declare.
Contribution
EMM was responsible for the design, data collection and analysis, and write‐up of this report.
Acknowledgements
I would like to thank my field assistants Korea Leala, Rapheala Leado, Selena Gambare and Abdulai Khalifa for their dedicated data collection. Finally, I would like to thank the Ariaal women and infants who participated in this study.
Miller, E. M. (2015) A comparison of three infant skinfold reference standards: Tanner–Whitehouse, Cambridge Infant Growth Study, and WHO Child Growth Standards. Matern Child Nutr, 11: 1023–1027. doi: 10.1111/mcn.12111.
References
- Davies P.S., Day J.M. & Cole T.J. (1993) Converting Tanner–Whitehouse reference tricep and subscapular skinfold measurements to standard deviation scores. European Journal of Clinical Nutrition 47, 559–566. [PubMed] [Google Scholar]
- Gluckman P.D., Hanson M.A. & Beedle A.S. (2007) Early life events and their consequences for later disease: a life history and evolutionary perspective. American Journal of Human Biology 19, 1–19. [DOI] [PubMed] [Google Scholar]
- Kuzawa C.W. (1998) Adipose tissue in human infancy and childhood: an evolutionary perspective. Yearbook of Physical Anthropology 41, 177–209. [DOI] [PubMed] [Google Scholar]
- Leonard W., Snodgrass J. & Robertson M. (2010) Evolutionary perspectives on fat ingestion and metabolism in humans In: Fat Detection: Taste, Texture, and Post Ingestive Effects (eds Montmayeur J. & le Coutre J.), pp 3–18. CRC Press: Boca Raton, FL. [PubMed] [Google Scholar]
- Miller E.M. & McConnell D.S. (2012) Chronic undernutrition is associated with higher mucosal antibody levels among Ariaal infants of northern Kenya. Am J Phys Anthropol 149, 136–141. [DOI] [PubMed] [Google Scholar]
- Paul A.A., Cole T.J., Ahmed E.A. & Whitehead R.G. (1998) The need for revised standards for skinfold thickness in infancy. Archives of Disease in Childhood 78, 354–358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanner J.M. & Whitehouse R.H. (1975) Revised standards for triceps and subscapular skinfolds in British children. Archives of Disease in Childhood 50, 142–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora C.G., de Onis M., Hallal P.C., Blossner M. & Shrimpton R. (2010) Worldwide timing of growth faltering: revisiting implications for interventions. Pediatrics 125, e473–e480. [DOI] [PubMed] [Google Scholar]
- Wells J.C.K., Chomtho S. & Fewtrell M.S. (2007) Programming of body composition by early growth and nutrition. Proceedings of the Nutrition Society 66, 423–434. [DOI] [PubMed] [Google Scholar]
- Wells J.C.K. & Fewtrell M.S. (2006) Measuring body composition. Archives of Disease in Childhood 91, 612–617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- who anthro (2010) Software for assessing growth and development of the world's children. 3.2.2, 2011 edn. WHO, Geneva.
- WHO Multicentre Growth Reference Study Group (2006) WHO Child Growth Standards: Length/Height‐for‐Age, Weight‐for‐Age, Weight‐for‐Length, Weight‐for‐Height and Body Mass Index‐for‐Age: Methods and Development. World Health Organization: Geneva. [Google Scholar]


