Abstract
Background
Urbanisation has been associated with temporal and geographical differences in asthma prevalence in low-income and middle-income countries (LMICs). However, little is known of the mechanisms by which urbanisation and asthma are associated, perhaps explained by the methodological approaches used to assess the urbanisation-asthma relationship.
Objective
This review evaluated how epidemiological studies have assessed the relationship between asthma and urbanisation in LMICs, and explored urban/rural differences in asthma prevalence.
Methods
Asthma studies comparing urban/rural areas, comparing cities and examining intraurban variation were assessed for eligibility. Included publications were evaluated for methodological quality and pooled OR were calculated to indicate the risk of asthma in urban over rural areas.
Results
Seventy articles were included in our analysis. Sixty-three compared asthma prevalence between urban and rural areas, five compared asthma prevalence between cities and two examined intraurban variation in asthma prevalence. Urban residence was associated with a higher prevalence of asthma, regardless of asthma definition: current-wheeze OR:1.46 (95% CI:1.22 to 1.74), doctor diagnosis OR:1.89 (95% CI:1.47 to 2.41), wheeze-ever OR:1.44 (95% CI:1.15 to 1.81), self-reported asthma OR:1.77 (95% CI:1.33 to 2.35), asthma questionnaire OR:1.52 (95% CI:1.06 to 2.16) and exercise challenge OR:1.96 (95% CI:1.32 to 2.91).
Conclusions
Most evidence for the relationship between urbanisation and asthma in LMICs comes from studies comparing urban and rural areas. These studies tend to show a greater prevalence of asthma in urban compared to rural populations. However, these studies have been unable to identify which specific characteristics of the urbanisation process may be responsible. An approach to understand how different dimensions of urbanisation, using contextual household and individual indicators, is needed for a better understanding of how urbanisation affects asthma.
PROSPERO registration number
CRD42017064470.
Keywords: urbanisation, asthma, urban and rural areas, LMICs
Key messages.
What is the key question?
The effects of urbanisation on asthma prevalence in low-income and middle-income countries (LMICs).
What is the bottom line?
Asthma prevalence is greater in urban than rural populations in LMICs, but the mechanisms by which urbanisation affects asthma are not clear, explained probably by the methods used to measure urbanisation.
Why read on?
Our systematic review provides evidence that urban residence and urbanisation are important determinants of asthma prevalence although such studies to date have used inadequate methodological approaches to identify the causal factors involved.
Introduction
The prevalence of asthma and related allergic disorders (RAD) has been increasing over the past four decades.1 However, recent evidence indicates that the prevalence may have reached a plateau in high-income countries (HICs) with a high prevalence, but continues to increase in lower prevalence LMICs, particularly among urban populations.2 3 The factors that underlie such temporal and geographical trends in asthma prevalence are poorly understood, but are likely to reflect a complex interplay of biologic, environmental and social factors.4
It has been hypothesised that the urbanisation process could be in part responsible for the temporal and geographical variations of asthma prevalence in both HICs and LMICs.5–7 This hypothesis has received support mainly by three observations. First, studies on wheezing or asthma in different regions of the world have regularly shown a lower asthma prevalence in rural settlements compared with cities.5 8 9 Second, the low asthma prevalence in rural areas has been explained by possible protection provided by traditional rural exposures such as farming.6 7 However, recent studies have shown that allergic disorders could be increasing in rural areas, reducing the urban–rural gap in asthma prevalence.10–12 Third, exposures relating to environmental and lifestyle changes that originate from the urbanisation process have been identified as risk factors for asthma including changes in diet, sedentarism, reductions in childhood infections, smaller families, use of antibiotics, environmental pollution and migration.6 13
Epidemiological studies have provided invaluable information about the relationship between urbanisation and asthma through use of diverse methods and indicators of urbanisation. However, studies evaluating the effects of urbanisation on asthma are complex and face several conceptual and methodological limitations. First, there is no standard definition of urbanisation. Urbanisation is a highly complex process that affects all levels of human activity and no single definition can fully describe the multidimensional nature of this process.14 Second, there is no universally accepted definition of what constitutes an urban area. Different countries use different definitions for urban areas mainly based on demographic, political or economic characteristics of their populations.15 Third, there is no agreed definition of asthma for research purposes, so different studies use different definitions such as doctor diagnosis, presence of clinical symptoms and bronchial hyper-responsiveness.16 17
In LMICs, the specific features and mechanisms by which urbanisation affects asthma are not clear. Part of this problem may lie in the methods used by asthma studies to assess the effects of urbanisation on asthma. The aim of this systematic review is to provide a general overview of how epidemiological studies have assessed the relationship between asthma prevalence and urbanisation in LMICs.
In this review, we addressed the following research objectives:
To examine the methods used to evaluate the effects of urbanisation on asthma.
To examine rural ⁄urban differences in asthma prevalence.
Methods
We performed a systematic review of the scientific literature to identify studies that have assessed the relationship between asthma and urbanisation in LMICs following Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.18
Inclusion criteria
Population and context
Subjects of all ages living in urban or rural areas of LMICs. We excluded populations living in HICs. LMICs were defined using the list of countries of the World Bank (https://datahelpdesk.worldbank.org) based on the year in which each study was conducted.
Study designs
Cross-sectional, case–control, cohort and ecological studies. We excluded intervention, experimental and genetic studies. Studies that lacked essential data for calculating ORs were also excluded.
Exposure
Urban areas or urban environments defined by demographic, socioeconomic, administrative or other indicators associated to the urbanisation process. We excluded studies evaluating the effects of air pollution on asthma.
Outcomes
Prevalence of asthma measured by wheeze/asthma in the last 12 months, clinical symptoms, doctor’s diagnosis, questionnaire data and pulmonary function tests.
Search strategy
A literature search was done in PubMed, ScienceDirect and Scielo databases in February 2017 (online supplementary figure 1). To include all available evidence, past reviews, letters to the editor and publications discussing the relationship between urbanisation and asthma were also evaluated. Further, no restrictions were imposed regarding sample size, age, sex and publication date. Articles in English, Spanish and Portuguese were included in the search. The search process concluded on July 2017.
thoraxjnl-2018-211793supp001.pdf (574.5KB, pdf)
Paper selection and retrieval process
Publications were grouped by three methods: (a) studies comparing the prevalence of asthma between rural and urban areas, (b) studies comparing the prevalence of asthma between cities of the same country or across countries and (c) studies examining variations in the prevalence of asthma within cities.19 Titles and abstracts of the articles identified with the initial search were screened by AR. Full-text papers were retrieved and classified based on the previously mentioned categories. Retrieved texts were evaluated by two reviewers (AR and PC) and a final decision on their inclusion or exclusion was made based on the criteria previously outlined. In case of any doubts and uncertainties, a third author was consulted (LR). Non-systematic review papers and letters to the editor were included to provide a general overview of the topic and as a reference source only and did not provide primary data. A flow chart of the selection process is shown in figure 1.
Figure 1.
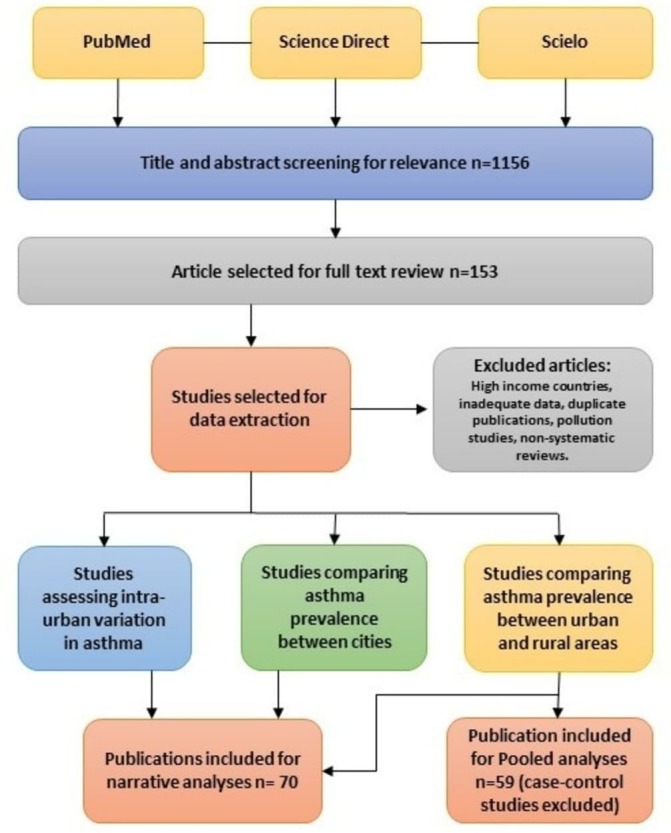
Flow chart of publication selection process.
Data extraction
A working database was designed using SPSS V.20 including relevant characteristics of the publications: authors(s) name, title, publication year, country, region, gross national income, study design, study approach, area description, age range, sample size, indicators of urbanisation, urban area definition, asthma definition, urban–rural asthma prevalence, unadjusted OR and P value for the urban–rural difference. For studies using more than one category for urban or rural settings (eg, urban and periurban, or rural and perirural), those categories were grouped into either urban or rural area as appropriate.
Study quality assessment
Study quality was assessed using Strengthening the Reporting of Observational Studies in Epidemiology guidelines,20 and ‘Critical Appraisal of Health Research Literature: Prevalence or Incidence of a Health Problem’.21 Seven criteria were considered (setting description, population description, sample method, sample size, urban definition, asthma definition and adequate response rate) to classify study quality as high, medium or low. High-quality studies were those providing complete information for these criteria while medium quality studies lacked information for one criterion. Studies lacking information on more than one criterion were considered to be of low quality.
Statistical analysis
A descriptive analysis was done based on the relevant characteristics of included publications. For cross-sectional studies comparing urban and rural areas, forest plots and unadjusted ORs were used to explore the association between asthma prevalence and area of residence. Because of the large degree of heterogeneity, studies were analysed by asthma definition. A single descriptive pooled OR (and 95% CI) was estimated for each definition using a random-effects model as a synthesis of available information. Results of individual studies were entered into the Cochrane Collaboration Review Manager V.5 and analysed using Metaview V.5. The I2 test was used to evaluate heterogeneity between studies. Funnel plots were used to detect bias or systematic heterogeneity by asthma definition groups.
Results
Literature search
From 1156 titles and abstracts identified for eligibility in the three databases, 153 articles were selected for a full text review. Seventy articles met our inclusion criteria after full-text review (figure 1). We found two manuscripts with information for two locations in the same publication,22 23 and two publications comparing asthma studies in the same location but at two different times.10 11 These articles were included in our analysis considering each location (survey) as an independent study. We identified eleven asthma studies that used several categories to define urban and rural - these were re-categorised into a dichotomous urban versus rural classification for inclusion (online supplementary table 1).10 24–33 Although we did not consider non-systematic review articles for data extraction, eleven non-systematic review articles addressing the relationship between urbanisation and asthma in LMICs were identified in the literature search.5 7 8 34–42 Eighty-three articles were excluded because they were conducted in HICs, studies that lacked data to estimate ORs and duplicate publications.
thoraxjnl-2018-211793supp002.pdf (77.2KB, pdf)
Narrative analysis
Seventy articles published between 1979 and 2017 met the inclusion criteria (table 1). Sixty-three publications compared asthma prevalence between urban and rural areas, five compared asthma prevalence between cities or rural settlements of the same country or among countries and two studied intraurban variations in asthma prevalence. Latin America (LA), Africa and Asia presented a similar number of publications (n=22, n=23, n=24, respectively) (figure 2). Current wheeze was the most used asthma definition (44 publications). Fifty-two publications studied age groups ≤18 years including studies of children (0–12 years), adolescents (12–18 years) or both (0–18 years).
Table 1.
Characteristics of publications included in the systematic review
| Variables and categories | n (%) |
| Study approach | |
| Comparing urban vs rural areas | 59 (89) |
| Comparing cities or settlements | 5 (8) |
| Comparing intraurban variation | 2 (3) |
| Region | |
| Asia | 22 (33) |
| Africa | 22 (33) |
| Latin America | 21 (32) |
| Easter Europe | 1 (2) |
| Study design | |
| Cross-sectional | 58 (88) |
| Ecologic | 7 (10) |
| Cohort | 1 (2) |
| Methodology | |
| ISAAC | 34 (52) |
| Other | 32 (48) |
| Asthma definition* | |
| Wheezing ever | 19 (16) |
| Current wheeze | 42 (35) |
| Doctor diagnosis | 24 (20) |
| Exercise challenge test | 10 (8) |
| Self-report asthma | 15 (12) |
| Questionnaire diagnosis | 11 (9) |
| Age category (years) | |
| Children (0–12) | 15 (23) |
| Adolescent12–18 | 13 (18) |
| Children and adolescent (0–18) | 21 (34) |
| Adult (>18) | 9 (14) |
| All ages | 7 (11) |
| Year of the publication | |
| Before 1990 | 2 (3) |
| 1990–1999 | 6 (9) |
| 2000–2009 | 23 (35) |
| 2010–2017 | 35 (53) |
*Some studies used two or three asthma definitions, so percentages were calculated using the total number of definitions as denominator.
ISAAC, International Study of Asthma and Allergies in Childhood.
Figure 2.
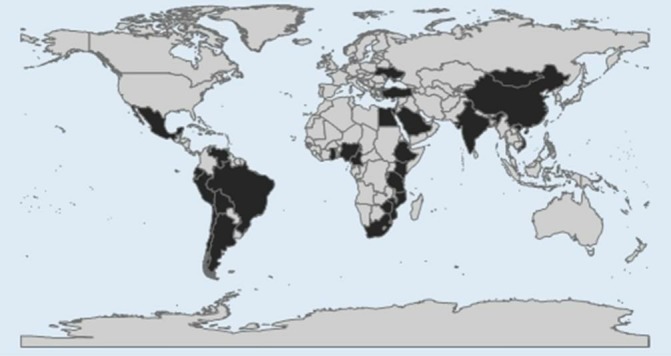
Map of countries in which studies on asthma and urbanisation have been done (countries in black).
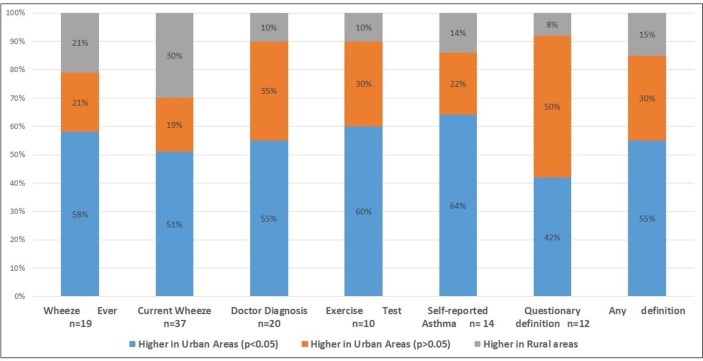
Asthma studies comparing rural and urban areas
We found 58 cross-sectional studies, 4 case–control studies conducted in 32 different countries of Africa,10 23 25 27 28 31 32 43–57 Asia,11 29 30 33 58–73 LA22 24 26 74–91 and Eastern Europe.92 Figure 3 shows differences in asthma prevalence between urban and rural areas of these countries. Asthma prevalence was generally higher in urban areas. However, proportions of studies showing greater prevalence in urban compared with rural areas varied by asthma definition (figure 4): current wheeze 19/37 studies were statistically significant, wheezing ever 11/19 studies were significant, doctor diagnosis 11/20 studies were significant, exercise challenge test 6/10 studies were significant, self-reported asthma 9/14 were significant and questionnaire diagnosis 5/12 of which five were significant. Complete data are shown in online supplementary table 2.
Figure 3.
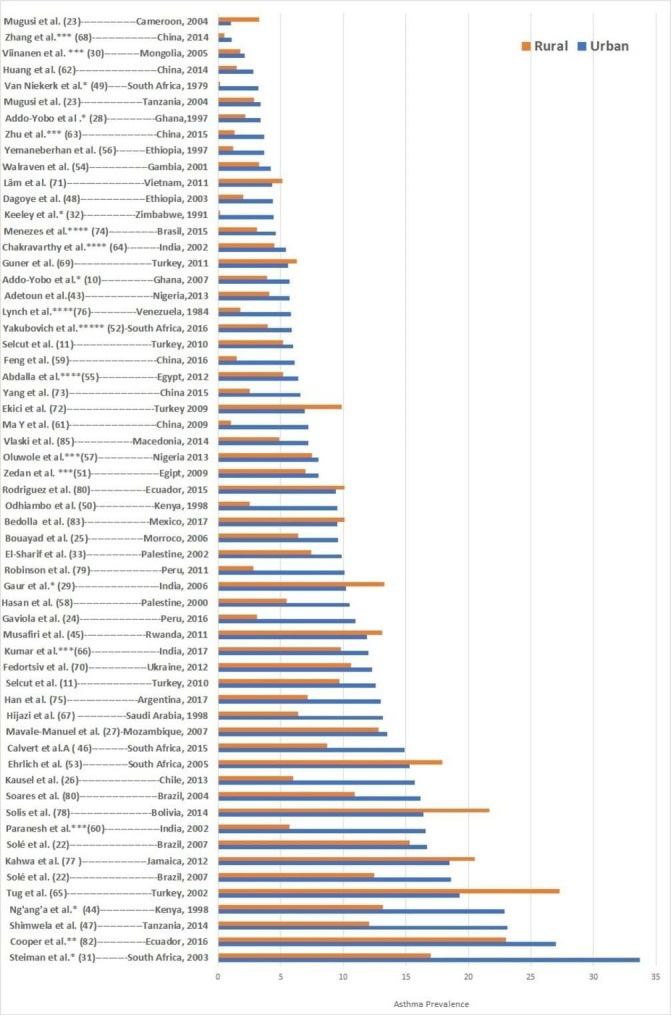
Urban–rural gradient in asthma prevalence in low-income and middle-income countries. asthma definition: (*) exercise challenge test, (**) wheeze ever, (***) asthma questionnaire, (****) doctor diagnosis. All other studies were defined using current wheeze.
Figure 4.
Proportions of studies showing greater prevalence of asthma in urban compared with rural areas by asthma definition.
Pooled unadjusted ORs and forest plots for urban versus rural comparisons of asthma prevalence by asthma definition are shown in figures 5–7. Pooled ORs were: current wheeze, OR: 1.46 (95% CI 1.22 to 1.74); doctor diagnosis, OR: 1.89 (95% CI 1.47 to 2.41); wheeze ever, OR: 1.44 (95% CI 1.15 to 1.81); self-reported asthma, OR: 1.77 (95% CI 1.33 to 2.35); questionnaire-defined asthma, OR: 1.52 (95% CI 1.06 to 2.16); and exercise-induced asthma OR: 1.96 (95% CI 1.32 to 2.91). A high statistical heterogeneity was found (I2 >60) for all definitions. Additionally, we calculated pooled unadjusted ORs and forest plots for urban versus rural comparisons of asthma prevalence by age groups, list of countries by national gross income and regions. (Data is shown in online supplementary figures 3-6). Pooled ORs were: age group 0–12 years, OR 1.70 (95% CI 1.37 to 2.11); age group 13–18, OR: 2.09 (95% CI 1.49 to 2.93); low-income countries: OR: 1.48 (95% CI 1.13 to 1.93); lower-middle-income countries, OR: 1.41 (95% CI 1.06 to 1.88); and upper-middle-income countries, OR: 1.70 (95% CI 1.34 to 2.15); Africa, OR 1.56 (95% CI 1.24 to 1.95), Asia, OR 1.62 (95% CI 1.19 to 2.20) and LA, OR 1.52 (95% CI 1.22 to 1.90).
Figure 5.
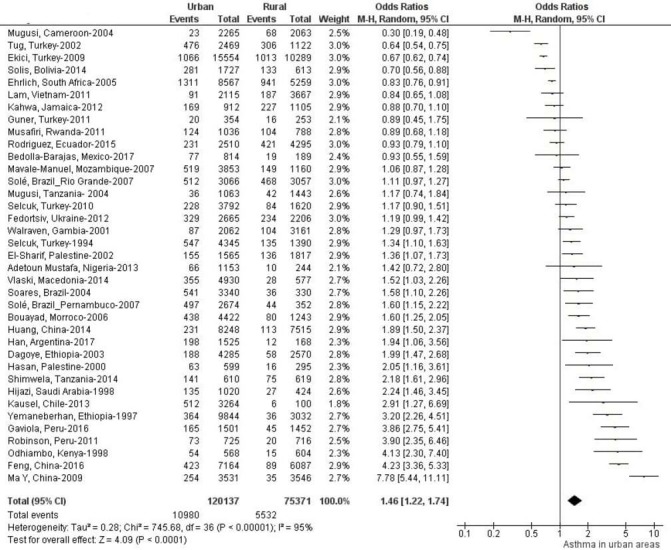
Forest plot and unadjusted ORs for studies using current wheeze to define asthma comparing populations living in urban versus rural areas.
Figure 6.
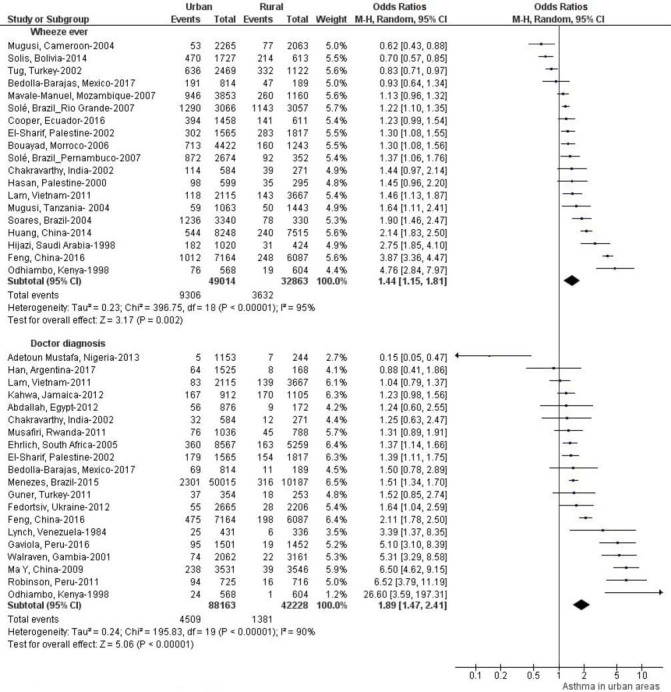
Forest plots and unadjusted ORs for studies using wheezing ever and doctor diagnosis to define asthma comparing populations living in urban versus rural areas.
Figure 7.
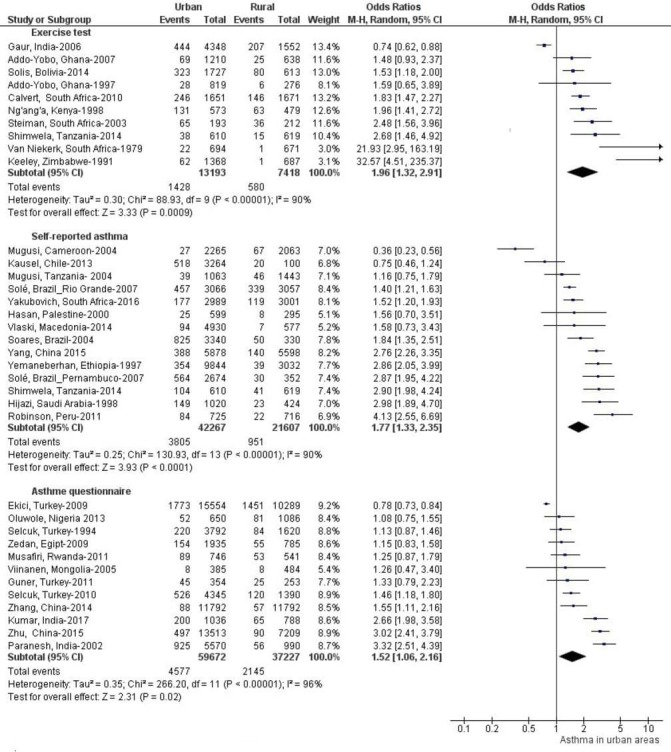
Forest plots and unadjusted ORs for studies using exercise challenge test, self-reported asthma and asthma questionnaire to define asthma comparing populations living in urban versus rural areas.
Asthma studies comparing cities
Publications in this group used ecological designs to compare different urban characteristics between cities of the same country or across countries to infer effects of the urban environment on asthma (table 2). However, this approach was also used to compare other types of settlements as rural communities with other rural communities. In general, five studies were included in this group. The first evaluated associations between asthma prevalence and 11 health and socioeconomic indicators in 20 Brazilian cities and showed that indicators related to urban poverty and inequality were associated with a greater asthma prevalence.85 The second evaluated 59 rural communities in Ecuador and correlated community asthma prevalence with different indices constructed to represent the process of urbanisation in the communities.86 The study showed that greater levels of urbanisation, particularly with respect to lifestyle and socioeconomic indices, were positively associated with asthma prevalence. The third compared the prevalence of asthma between 31 urban centres across LA using several socioeconomic and environmental indicators.87 This study found that social inequalities between cities could be a central determinant of the geographical variation in asthma prevalence within LA. A fourth study conducted in Brazil used 266 municipalities with more than 100 000 inhabitants as the unit of analysis.88 This study correlated indicators of socioeconomic factors and violence with the rate of hospital admissions for asthma. The study found a direct correlation between indicators of violence and rates of admission due to asthma, and an inverse correlation with indicators of development. The final study evaluated the effect of urbanisation on hospital admissions and death rates from asthma in 5505 municipalities in Brazil using time series analysis in which urbanisation was defined as the proportion of people living in urban areas by municipality.89 The study showed that urban population growth by municipality was associated with a rise in hospital admissions and death rates from asthma in children and young adults.89
Table 2.
Publications comparing asthma prevalence among cities and publication comparing intraurban variation in asthma within cities
| Publication | Methodology | Asthma definition | Urban indicators | Findings |
| Cunha et al, 2007 85 |
|
Current wheezing |
|
Asthma prevalence increased with poorer sanitation and with higher infant mortality, GINI index and external mortality. Poverty and inequality seems to be related with asthma prevalence in urban areas of Brazil. |
| Rodriguez et al, 2011 86 |
|
Current wheezing |
|
Lifestyle and socioeconomic indicators had stronger overall effects on asthma prevalence than infrastructure indicators. Higher asthma prevalence was present in communities with a higher socioeconomic level and a more urbanised lifestyle. |
| Fattore et al, 2014 87 |
|
Current wheezing |
|
Income inequality, lack of adequate sanitation, less crowding households, greater reduction in the infant mortality rates and high homicide rates were determinants of asthma symptoms in Latin American urban children. |
| Tabalipa et al,2015 88 |
|
Hospital rate admissions (doctor diagnosis) |
-Index of Youth Vulnerability to Violence: Injury from external causes, incidences of homicides, traffic accidents, education, involvement in crime, poverty and unemployment. | Direct correlation between indicators of violence and rates of admission due to asthma, and an inverse correlation with indicators of development. |
| Ponte et al,2016 89 |
|
Hospital rate admissions (doctor diagnosis) |
|
An increase in urban population by municipality was associated with lower odds for reduced hospital admissions and death rates from asthma in children and young adults. |
| Antunes et al, 2014 90 |
|
Hospital rate admissions (doctor diagnosis) |
Socioeconomic indicators: Income, education, household crowding, presence of slums, GINI Index, sanitation, garbage collection. | Areas of Salvador whose population had lower levels of education and income had higher risk of hospitalisation for respiratory diseases, particularly for asthma and pneumonia. |
| Dias et al, 2016 91 |
|
Hospital rate admissions (doctor diagnosis) |
-Health Vulnerability Index: Inadequate water supply, sanitary sewage and inadequate garbage collection, housing, illiterate population, per capita income, race and ethnicity. | Hospital admissions for asthma were higher in areas of greater social vulnerability, suggesting that social and environmental factors may be determinants of variation in asthma prevalence in urban areas. |
GINI, Measure of Inequality; HDI, Human Development Index.
Asthma studies examining intraurban variations within cities
We found two studies describing the spatial distribution of asthma and their relationships with social and health determinants in two Brazilian cities.90 91 Both publications were ecological studies using census wards as the unit of analysis evaluating how living in a particular spatial setting within a city might be associated with asthma. The first study found that areas of Salvador whose population had lower levels of education and income, had a higher risk of hospitalisation for respiratory diseases, particularly for asthma and pneumonia.90 The second study conducted in Belo Horizonte found that hospital admissions for asthma were higher in areas of greater social vulnerability, suggesting that social and environmental factors may be determinants of variations in asthma prevalence.91
Study quality
Information on study quality is provided in online supplementary table 3. There was considerable variation in methodological quality between studies. Of the 66 studies included in this systematic review, 26 were considered of low methodological quality. Although most studies used schools as the unit of analysis (comparing urban and rural schoolchildren), the methods by which schools were selected were variable and generally not random but based on convenience samples (n=16). Twenty-three studies provided no information on response rates. Most studies used population size and administrative criteria to define urban and rural areas, comparing populations living in cities with those in rural towns or cities versus communities or villages. However, fifteen studies did not provide general information about the settings in which they were done (n=12). For studies comparing urban and rural areas, sample sizes ranged between 405 and 60 000 subjects. In the case of ecological studies sample size ranged between 20 and 5505 units of analysis.
Discussion
In this systematic review, we assessed how epidemiological studies conducted in LMICs have addressed the relationship between urbanisation and asthma. We compared also the reported prevalence of asthma in the urban and rural settings studied. Our analyses showed that almost all publications addressing the relationship between asthma and urbanisation come from studies comparing asthma prevalence between urban and rural populations. Few studies from LMICs have used more complex approaches to assess the relationship between urbanisation and asthma. This review provides evidence for an urban–rural gradient in asthma prevalence in LMICs, showing that the risk of asthma is higher in urban compared with rural areas, findings that were consistent irrespective of the asthma definition used. However, any interpretation of these data needs to be cautious because of the high level of heterogeneity between studies.
The study of urbanisation in asthma research has used different methodological approaches to measure the effects of urban areas and urban environments on asthma occurrence, of which the most widely used is comparison urban and rural populations. Although this approach have been useful to identify differences between environmental and social factors that could explain the urban–rural gradient in asthma prevalence,6 93 they have limited usefulness understanding the multidimensional nature of urbanisation. Issues such as diverse dimensions of urban environments, differences in lifestyle between populations, distinct levels of urbanisation between urban centres and changes over time, cannot be properly addressed using this approach. For example, in our review, 13 studies reported a similar or a higher prevalence of asthma in rural compared with urban areas. It is likely that differences in lifestyle between urban and rural population may be responsible for these findings. Indeed, a non-systematic review of urban–rural comparisons of asthma prevalence showed only minimal differences, particularly where socioeconomic and environmental factors were comparable between urban and rural populations.42 Thus, rural and urban populations that share similar living conditions and socioeconomic factors are likely to have comparable asthma risks. Such a situation is commonly found in HICs where rural and urban populations have similar lifestyles and standards of living, but also in LMICs where many urban (and periurban) localities may have similar living conditions to more rural settings, and in the case of urban slums living conditions may be worse than many rural settings.94 This is important because of the frequent misconception in asthma studies that urban populations in LMICs live in cleaner and healthier environment.95
A second common approach has been to compare asthma prevalence or asthma hospitalisation rates by different urban characteristics of cities, municipalities or communities—such as infrastructure, socioeconomic indicators, level of violence, urban services, health indicators, among others—to identify features of the urbanisation process that could be related to asthma prevalence. In studies comparing cities, a higher prevalence of asthma was observed in those cities with poor sanitation, high infant mortality, social inequalities and elevated levels of violence. Overall, these studies indicate that social deprivation in cities could contribute to asthma risk. In agreement with this, cross-sectional studies from the USAnited States and LA have observed associations between asthma risk and poverty and lack of basic services in urban areas.42 96 97 In the Ecuadorian study comparing rural communities, indices representing different domains of the urbanisation process as socioeconomic, lifestyle, urban infrastructure and a summary urbanisation derived from representative variables of each of these, were associated with asthma prevalence. While significant heterogeneity was observed in the level of urbanisation between rural communities, the community prevalence of asthma increased with greater levels of urbanisation, especially with indices representing lifestyle and socioeconomic factors. These findings mirror those of other studies done in LMICs.24 26 30 33 For example, a cross-sectional study from Mongolia compared the prevalence of asthma and RAD in localities with different levels of urbanisation: city, urban town and villages. The study showed an increasing prevalence of allergic diseases with greater level of urbanisation.30 It is important to highlight that comparing cities (or other urban areas) in the same country offer a relative solution to the lack of a general definition of urbanisation present in asthma studies comparing urban and rural areas from diverse parts of the world. The city comparison approach within the same country is based on (1) urban area definition is the same for all settlements, and (2) urban characteristics of the cities are more comparable within a country than between countries, especially because factors such as climate, culture and other characteristic are likely to be similar. Likewise, comparisons between rural localities allow the study of urbanisation processes and urban sprawl in transitional societies where changes in lifestyle and environmental factors occur more rapidly. A weakness of studies using cities or settlements as the unit of analysis is the assumption that aggregate behaviours or characteristics at the city level are equally important for all residents. This ecologic fallacy requires a cautious interpretation of findings from such studies.98
Intraurban studies evaluate how living in a particular area of a city may be associated with asthma outcomes. Such studies tend to use spatial groupings of individuals, commonly represented by neighbourhoods or census wards, to assess the effect of place of residence within an urban area on community or individual health.19 These studies often require spatial and socioeconomic information in these localities at individual and contextual levels, commonly provided by censuses and other publicly available data sources. For asthma research, this approach would be appropriate for addressing questions related to identifying the characteristics of areas within cities that may be associated with asthma. However, few such studies have been done in LMICs.
Limitations of this review
Studies evaluating specific characteristics of the urban environment, such as air pollution or distance to an urban location,99 were not included. In the case of air pollution, there is a large literature and this topic may be better dealt with separately. We considered only studies done in LMICs because these countries share historical and developmental processes determining the evolution of the urban environment that are distinct from those that have occurred in HICs.100 Other ecological studies, especially those related to the International Study of Asthma and Allergies in Childhood, were not included here because they use populations from both LMICs and HICs.101–103 Because of the large degree of heterogeneity between studies (different study setting, population age, asthma definitions, urban–rural definitions) and variable methodological quality, pooled ORs estimated by asthma definition need to be interpreted with caution. Finally, although we carried out a thorough search of the literature and produced funnel plots to investigate potential publication bias (see online supplementary figure 2), the plots were not suggestive of publication bias, but we cannot completely exclude the possibility that studies that do not show a positive association are less likely to be published.
Conclusions
This systematic review analysed the effects from the published literature of urbanisation on the prevalence of asthma in LMICs. Published epidemiological studies addressing this issue have mostly used one of three methodological approaches; comparisons of asthma prevalence between urban and rural areas, comparisons of cities within and between countries, and comparisons of areas within cities. Similarly, published studies have used a variety of definitions to define asthma. However, despite such heterogeneity in asthma definitions a number of consistent patterns emerged in this systematic review: (1) irrespective of the asthma definitions used, the prevalence of asthma was greater in urban than rural areas in most but not all studies; (2) indicators of social deprivation, inequality and or poverty within or between cities were associated with the prevalence of asthma or hospitalisation rates for asthma; and (3) even at the rural level, indicators of urbanisation, particularly lifestyle and socioeconomic factors, were associated with asthma prevalence. Overall, these findings provide evidence that urban residence and urbanisation are important determinants of asthma prevalence but do not permit us to identify which aspects of the urbanisation process are most important as determinants of risk due to most of the studies exploring the effects of urbanisation on asthma have used the simple urban–rural approach. Such method does not allow us to consider the multifactorial dimensions of the urbanisation process and cannot identify specific factors or conditions associated with asthma risk. We need to start thinking about more complex chains of causation in urban studies and asthma. An important issue for studies of the effects of urbanisation and asthma is a lack of an adequate conceptual model for how social, psychological and biological determinants within urbanisation processes interact to affect asthma risk. A better understanding of how such processes operate is likely to lead to a better understanding of asthma causation and potential strategies to the primary prevention of this important debilitating disease. We believe that studies addressing the multifactorial dimensions of the urbanisation process using the city comparison and the intraurban comparison approaches will help to generate more closely specified causal models which also help to clarify the distinction between confounding and intervening variables. Additionally, there is a clear need for an accurate standardised operational definition of asthma and a clearer and more precise definitions of ‘urbanisation’ and ‘urban areas’. This would facilitate aetiological research, comparisons between locations (especially in international studies) and estimations of asthma prevalence in epidemiological studies.
Acknowledgments
We thank all authors who kindly sent us their manuscripts upon request during the retrieval and selection process. We also thank Ecuadorian Institute of Educational Credit (IECE) and the Ecuadorian Ministry of Higher Education, Science, Technology and Innovation (SENESCYT).
Footnotes
Contributors: Study design: AR, PJC, LCR. Data collection; AR, PJC, LCR. Data analysis: AR. Draft manuscript: AR, PJC. Manuscript review: AR, EB, RN, PJC, MLB.
Funding: The research was supported by grants from the Wellcome Trust (072405/Z/03/Z and 088862/Z/09/Z). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available upon reasonable request.
References
- 1. Asher I, Pearce N. Global burden of asthma among children. Int J Tuberc Lung Dis 2014;18:1269–78. 10.5588/ijtld.14.0170 [DOI] [PubMed] [Google Scholar]
- 2. Beasley R. Worldwide variation in prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and atopic eczema: Isaac. The Lancet 1998;351:1225–32. 10.1016/S0140-6736(97)07302-9 [DOI] [PubMed] [Google Scholar]
- 3. Pearce N, Aït-Khaled N, Beasley R, et al. Worldwide trends in the prevalence of asthma symptoms: phase III of the International study of asthma and allergies in childhood (Isaac). Thorax 2007;62:758–66. 10.1136/thx.2006.070169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Castro-Rodriguez JA, Forno E, Rodriguez-Martinez CE, et al. Risk and protective factors for childhood asthma: what is the evidence? J Allergy Clin Immunol Pract 2016;4:1111–22. 10.1016/j.jaip.2016.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Weinberg EG. Urbanization and childhood asthma: an African perspective. J Allergy Clin Immunol 2000;105:224–31. 10.1016/S0091-6749(00)90069-1 [DOI] [PubMed] [Google Scholar]
- 6. von Hertzen L, Haahtela T. Disconnection of man and the soil: reason for the asthma and atopy epidemic? J Allergy Clin Immunol 2006;117:334–44. 10.1016/j.jaci.2005.11.013 [DOI] [PubMed] [Google Scholar]
- 7. Platts-Mills TAE, Cooper PJ. Differences in asthma between rural and urban communities in South Africa and other developing countries. J Allergy Clin Immunol 2010;125:106–7. 10.1016/j.jaci.2009.10.068 [DOI] [PubMed] [Google Scholar]
- 8. Nicolaou N, Siddique N, Custovic A. Allergic disease in urban and rural populations: Increasing prevalence with increasing urbanization. Allergy 2005;60:1357–60. 10.1111/j.1398-9995.2005.00961.x [DOI] [PubMed] [Google Scholar]
- 9. Cooper PJ, Rodrigues LC, Cruz AA, et al. Asthma in Latin America: a public Heath challenge and research opportunity. Allergy 2009;64:5–17. 10.1111/j.1398-9995.2008.01902.x [DOI] [PubMed] [Google Scholar]
- 10. Addo-Yobo EOD, Woodcock A, Allotey A, et al. Exercise-induced bronchospasm and atopy in Ghana: two surveys ten years apart. PLoS Med 2007;4:e70–60. 10.1371/journal.pmed.0040070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Selcuk ZT, Demir AU, Tabakoglu E, et al. Prevalence of asthma and allergic diseases in primary school children in Edirne, Turkey, two surveys 10 years apart. Pediatr Allergy Immunol 2010;21:e711–7. 10.1111/j.1399-3038.2010.01008.x [DOI] [PubMed] [Google Scholar]
- 12. Kolokotroni O, Middleton N, Nicolaou N, et al. Temporal changes in the prevalence of childhood asthma and allergies in urban and rural areas of Cyprus: results from two cross sectional studies. BMC Public Health 2011;11 10.1186/1471-2458-11-858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rodriguez A, Vaca MG, Chico ME, et al. Rural to urban migration is associated with increased prevalence of childhood wheeze in a Latin-American City. BMJ Open Resp Res 2017;4 10.1136/bmjresp-2017-000205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Germani G. Modernization, urbanization, and the urban crisis. Transaction Publishers, 1973. [Google Scholar]
- 15. Vlahov D, Urbanization GS. urbanicity, and health. J Urban Health 2002;79:S1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sá-Sousa A, Jacinto T, Azevedo LF, et al. Operational definitions of asthma in recent epidemiological studies are inconsistent. Clin Transl Allergy 2014;4 10.1186/2045-7022-4-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Pekkanen J, Pearce N. Defining asthma in epidemiological studies. Eur Respir J 1999;14:951–7. 10.1034/j.1399-3003.1999.14d37.x [DOI] [PubMed] [Google Scholar]
- 18. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015;4 10.1186/2046-4053-4-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Galea S, Vlahov D. Handbook of urban health: populations, methods, and practice. Springer Science & Business Media 2006.
- 20. Von EE, Altman DG, Egger M, et al. guidelines for reporting observational studies Strengthening the reporting of observational studies in epidemiology (STROBE) statement : guidelines for reporting observational studies. Br Med J 2007;335:19–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Loney PL, Chambers LW, Bennett KJ, et al. Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Dis Can 1998;19:170–6. [PubMed] [Google Scholar]
- 22. Solé D, Cassol VE, Silva AR, et al. Prevalence of symptoms of asthma, rhinitis, and atopic eczema among adolescents living in urban and rural areas in different regions of Brazil. Allergol Immunopathol 2007;35:248–53. 10.1157/13112991 [DOI] [PubMed] [Google Scholar]
- 23. Mugusi F, Edwards R, Hayes L, et al. Prevalence of wheeze and self-reported asthma and asthma care in an urban and rural area of Tanzania and Cameroon. Trop Doct 2004;34:209–14. 10.1177/004947550403400408 [DOI] [PubMed] [Google Scholar]
- 24. Gaviola C, Miele CH, Wise RA, et al. Urbanisation but not biomass fuel smoke exposure is associated with asthma prevalence in four resource-limited settings. Thorax 2016;71:154–60. 10.1136/thoraxjnl-2015-207584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Bouayad Z, Aichane A, Afif A, et al. Prevalence and trend of self-reported asthma and other allergic disease symptoms in Morocco: Isaac phase I and III. Int J Tuberc Lung Dis 2006;10:371–7. [PubMed] [Google Scholar]
- 26. Kausel L, Boneberger A, Calvo M, et al. Childhood asthma and allergies in urban, semiurban, and rural residential sectors in Chile. The Scientific World Journal 2013;2013:1–4. 10.1155/2013/937935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mavale-Manuel S, Joaquim O, Macome C, et al. Asthma and allergies in schoolchildren of Maputo. Allergy 2007;62:265–71. 10.1111/j.1398-9995.2006.01251.x [DOI] [PubMed] [Google Scholar]
- 28. Addo Yobo EO, Custovic A, Taggart SC, et al. Exercise induced bronchospasm in Ghana: differences in prevalence between urban and rural schoolchildren. Thorax 1997;52:161–5. 10.1136/thx.52.2.161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gaur SN, Gupta K, Rajpal S, et al. Prevalence of bronchial asthma and allergic rhinitis among urban and rural adult population of Delhi. Indian J Allergy Asthma Immunol 2006;20:90–7. [Google Scholar]
- 30. Viinanen A, Munhbayarlah S, Zevgee T, et al. Prevalence of asthma, allergic rhinoconjunctivitis and allergic sensitization in Mongolia. Allergy 2005;60:1370–7. 10.1111/j.1398-9995.2005.00877.x [DOI] [PubMed] [Google Scholar]
- 31. Steinman HA, Donson H, Kawalski M, et al. Bronchial hyper-responsiveness and atopy in urban, peri-urban and rural South African children. Pediatr Allergy Immunol 2003;14:383–93. 10.1034/j.1399-3038.2003.00062.x [DOI] [PubMed] [Google Scholar]
- 32. Keeley DJ, Neill P, Gallivan S. Comparison of the prevalence of reversible airways obstruction in rural and urban Zimbabwean children. Thorax 1991;46:549–53. 10.1136/thx.46.8.549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. El-Sharif N, Abdeen Z, Qasrawi R, et al. Asthma prevalence in children living in villages, cities and refugee camps in Palestine. Eur Respir J 2002;19:1026–34. 10.1183/09031936.02.01832001 [DOI] [PubMed] [Google Scholar]
- 34. Schröder PC, Li J, Wong GWK, et al. The rural-urban enigma of allergy: what can we learn from studies around the world? Pediatr Allergy Immunol 2015;26:95–102. 10.1111/pai.12341 [DOI] [PubMed] [Google Scholar]
- 35. Urbanisation AMI. Asthma and allergies. Thorax 2011;66:1025–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Cullinan P. Asthma in African cities. Thorax 1998;53:909–10. 10.1136/thx.53.11.909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Awotedu AA. Urban-rural dicothomy in asthma. S Afr Fam Pr 2003;45:50–1. [Google Scholar]
- 38. Naleway AL. Asthma and atopy in rural children: is farming protective? Clin Med Res 2004;2:5–12. 10.3121/cmr.2.1.5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wong GWK, Chow CM. Childhood asthma epidemiology: insights from comparative studies of rural and urban populations. Pediatr. Pulmonol. 2008;43:107–16. 10.1002/ppul.20755 [DOI] [PubMed] [Google Scholar]
- 40. Pal R, Dahal S, Pal S. Prevalence of bronchial asthma in Indian children. Indian J Community Med 2009;34 10.4103/0970-0218.58389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Lim A, Asher MI, Ellwood E, et al. How are ‘urban’ and ‘rural’ defined in publications regarding asthma and related diseases? Allergologia et Immunopathologia 2014;42:157–61. 10.1016/j.aller.2013.02.009 [DOI] [PubMed] [Google Scholar]
- 42. Malik HU-R, Kumar K, et al. Minimal difference in the prevalence of asthma in the urban and rural environment. Clin Med Insights Pediatr 2012;33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Adetoun Mustapha B, Briggs DJ, Hansell AL. Prevalence of asthma and respiratory symptoms in children in a low socio-economic status area of Nigeria. int j tuberc lung dis 2013;17:982–8. 10.5588/ijtld.12.0434 [DOI] [PubMed] [Google Scholar]
- 44. Ng'ang'a LW, Odhiambo JA, Mungai MW, et al. Prevalence of exercise induced bronchospasm in Kenyan school children: an urban-rural comparison. Thorax 1998;53:919–26. 10.1136/thx.53.11.919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Musafiri S, van Meerbeeck J, Musango L, et al. Prevalence of atopy, asthma and COPD in an urban and a rural area of an African country. Respir Med 2011;105:1596–605. 10.1016/j.rmed.2011.06.013 [DOI] [PubMed] [Google Scholar]
- 46. Calvert J, Ascaris BP. Atopy, and exercise-induced bronchoconstriction in rural and urban South African children. J Allergy Clin Immunol 2015;125:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Shimwela M, Mwita JC, Mwandri M, et al. Asthma prevalence, knowledge, and perceptions among secondary school pupils in rural and urban coastal districts in Tanzania. BMC Public Health 2014;14 10.1186/1471-2458-14-387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Dagoye D, Bekele Z, Woldemichael K, et al. Wheezing, allergy, and parasite infection in children in urban and rural Ethiopia. Am J Respir Crit Care Med 2003;167:1369–73. 10.1164/rccm.200210-1204OC [DOI] [PubMed] [Google Scholar]
- 49. Van Niekerk CH, Weinberg EG, Shore SC, et al. Prevalence of asthma: a comparative study of urban and rural Xhosa children. Clin Allergy 1979;9:319–24. 10.1111/j.1365-2222.1979.tb02489.x [DOI] [PubMed] [Google Scholar]
- 50. Odhiambo JA, Ng'ang'a LW, Mungai MW, et al. Urban–rural differences in questionnaire-derived markers of asthma in Kenyan school children. Eur Respir J 1998;12:1105–12. 10.1183/09031936.98.12051105 [DOI] [PubMed] [Google Scholar]
- 51. Prevalence of bronchial asthma among Egyptian school. Egypt J Bronchol 2009;3:124–30. [Google Scholar]
- 52. Yakubovich AR, Cluver LD, Gie R. Socioeconomic factors associated with asthma prevalence and severity among children living in low-income South African communities. S Afr Med J 2016;106:404–12. 10.7196/SAMJ.2016.v106i4.10168 [DOI] [PubMed] [Google Scholar]
- 53. Ehrlich RI, White N, Norman R, et al. Wheeze, asthma diagnosis and medication use: a national adult survey in a developing country. Thorax 2005;60:895–901. 10.1136/thx.2004.030932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Walraven GEL, Nyan OA, Van Der Sande MAB, et al. Asthma, smoking and chronic cough in rural and urban adult communities in the Gambia. Clin Exp Allergy 2001;31:1679–85. 10.1046/j.1365-2222.2001.01094.x [DOI] [PubMed] [Google Scholar]
- 55. Abdallah A, Sanusy K, Said W, et al. Epidemiology of bronchial asthma among preparatory school children in Assiut district. Egypt J Pediatr Allergy Immunol 2012;10:109–17. [Google Scholar]
- 56. Yemaneberhan H, Bekele Z, Venn A, et al. Prevalence of wheeze and asthma and relation to atopy in urban and rural Ethiopia. The Lancet 1997;350:85–90. 10.1016/S0140-6736(97)01151-3 [DOI] [PubMed] [Google Scholar]
- 57. Oluwole O, Arinola OG, Falade GA, et al. Allergy sensitization and asthma among 13-14 year old school children in Nigeria. Af Hlth Sci 2013;13 10.4314/ahs.v13i1.20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Hasan MMS, Gofin R, Bar-Yishay E. Urbanization and the risk of asthma among schoolchildren in the Palestinian authority. Journal of Asthma 2000;37:353–60. 10.3109/02770900009055459 [DOI] [PubMed] [Google Scholar]
- 59. Feng M, Yang Z, Pan L, et al. Associations of early life exposures and environmental factors with asthma among children in rural and urban areas of Guangdong, China. Chest 2016;149:1030–41. 10.1016/j.chest.2015.12.028 [DOI] [PubMed] [Google Scholar]
- 60. Paramesh H. Epidemiology of asthma in India. Indian J Pediatr 2002;69:309–12. 10.1007/BF02723216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Ma Y, Zhao J, Han ZR, et al. Very low prevalence of asthma and allergies in schoolchildren from rural Beijing, China. Pediatr. Pulmonol. 2009;44:793–9. 10.1002/ppul.21061 [DOI] [PubMed] [Google Scholar]
- 62. Huang DM, Xiao XX, SM F, et al. Incidence of wheezing and chronic cough in children aged 3-14 years in rural and urban areas of Zhongshan, China: a questionnaire survey. Chinese J Contemp Pediatr 2014;16:734–9. [PubMed] [Google Scholar]
- 63. Zhu W-J, Ma H-X, Cui H-Y, et al. Prevalence and treatment of children's asthma in rural areas compared with urban areas in Beijing. Chin Med J 2015;128:2273–7. 10.4103/0366-6999.163381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Chakravarthy S, Singh RB, Swaminathan S, et al. Prevalence of asthma in urban and rural children in Tamil Nadu. Natl Med J India 2002;15:260–3. [PubMed] [Google Scholar]
- 65. Tug T, Acik Y. Prevalence of asthma, asthma-like and allergic symptoms in the urban and rural adult population in eastern Turkey. Asian Pacific J Allergy Immunol 2002;20:209–15. [PubMed] [Google Scholar]
- 66. Kumar N, Kumar N, Sharma P. Prevalence of bronchial asthma among school children in urban and rural areas and associated risk factors: a cross sectional study from western Uttar Pradesh, India. IJMSCI 2017;4;(41):2538–43. 10.18535/ijmsci/v4i2.02 [DOI] [Google Scholar]
- 67. Hijazi N, Abalkhail B, Seaton A. Asthma and respiratory symptoms in urban and rural Saudi Arabia. Eur Respir J 1998;12:41–4. 10.1183/09031936.98.12010041 [DOI] [PubMed] [Google Scholar]
- 68. Zhang W, Chen X, Ma L, et al. Epidemiology of bronchial asthma and asthma control assessment in Henan Province, China. Transl Respir Med 2014;2:5–7. 10.1186/2213-0802-2-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Guner SN, Gokturk B, Kilic M, et al. The prevalences of allergic diseases in rural and urban areas are similar. Allergologia et Immunopathologia 2011;39:140–4. 10.1016/j.aller.2010.05.004 [DOI] [PubMed] [Google Scholar]
- 70. Fedortsiv O, Brozek GM, Luchyshyn N, et al. Prevalence of childhood asthma, rhinitis, and eczema in the Ternopil region of Ukraine--results of BUPAS study. Adv Med Sci 2012;57:282–9. 10.2478/v10039-012-0034-6 [DOI] [PubMed] [Google Scholar]
- 71. Lâm HT, Rönmark E, Tu'ò'ng NV, et al. Increase in asthma and a high prevalence of bronchitis: results from a population study among adults in urban and rural Vietnam. Respir Med 2011;105:177–85. 10.1016/j.rmed.2010.10.001 [DOI] [PubMed] [Google Scholar]
- 72. Ekici A, Ekici M, Kocyigit P, et al. Prevalence of self-reported asthma in urban and rural areas of turkey. J Asthma 2012;49:522–6. 10.3109/02770903.2012.677893 [DOI] [PubMed] [Google Scholar]
- 73. Yang Z, Zheng W, Yung E, et al. Frequency of Food Group consumption and risk of allergic disease and sensitization in schoolchildren in urban and rural China. Clin Exp Allergy 2015;45:1823–32. 10.1111/cea.12532 [DOI] [PubMed] [Google Scholar]
- 74. Menezes AMB, Wehrmeister FC, Horta B, et al. Prevalência de diagnóstico médico de asma em adultos brasileiros : Pesquisa Nacional de Saúde, Prevalence of asthma medical diagnosis among Brazilian adults : National Health Survey, 2013. Rev Bras Epidemiol 2015:204–13. [DOI] [PubMed] [Google Scholar]
- 75. Han Y-Y, Badellino HA, Forno E, et al. Rural residence, farming environment, and allergic diseases in Argentinean adolescents. Pediatr Pulmonol. 2017;52:21–8. 10.1002/ppul.23511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Lynch NR, Medouze L, Di Prisco-Fuenmayor MC, et al. Incidence of atopic disease in a tropical environment: partial independence from intestinal helminthiasis. J Allergy Clin Immunol 1984;73:229–33. 10.1016/S0091-6749(84)80012-3 [DOI] [PubMed] [Google Scholar]
- 77. Kahwa EK, Waldron NK, Younger NO, et al. Asthma and allergies in Jamaican children aged 2–17 years: a cross-sectional prevalence survey. BMJ Open 2012;2:e00113 10.1136/bmjopen-2012-001132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78. Solis Soto MT, Patiño A, Nowak D, et al. Prevalence of asthma, rhinitis and eczema symptoms in rural and urban school-aged children from Oropeza Province - Bolivia: a cross-sectional study. BMC Pulm Med 2014;14 10.1186/1471-2466-14-40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Robinson CL, Baumann LM, Romero K, et al. Effect of urbanisation on asthma, allergy and airways inflammation in a developing country setting. Thorax 2011;66:1051–7. 10.1136/thx.2011.158956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80. Rodriguez A, Vaca MG, Chico ME, et al. Lifestyle domains as determinants of wheeze prevalence in urban and rural schoolchildren in Ecuador: cross sectional analysis. Environ Health 2015;14 10.1186/1476-069X-14-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81. Maia JGS, Marcopito LF, Amaral AN, et al. Prevalência de asma E sintomas asmáticos em escolares de 13 E 14 anos de idade. Rev. Saúde Pública 2004;38:292–9. 10.1590/S0034-89102004000200020 [DOI] [PubMed] [Google Scholar]
- 82. Cooper PJ, Chico ME, Amorim LD, et al. Effects of maternal geohelminth infections on allergy in early childhood. Journal of Allergy and Clinical Immunology 2016;137:899–906. 10.1016/j.jaci.2015.07.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Bedolla-Barajas M, Javier Ramírez-Cervantes F, Morales-Romero J, et al. A rural environment does not protect against asthma or other allergic diseases amongst Mexican children. Allergol Immunopathol 2017. [DOI] [PubMed] [Google Scholar]
- 84. Endara P, Vaca M, Platts-Mills TAE, et al. Effect of urban vs. rural residence on the association between atopy and wheeze in Latin America: findings from a case-control analysis. Clin Exp Allergy 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. da Cunha SS, Pujades-Rodriguez M, Barreto ML, et al. Ecological study of socio-economic indicators and prevalence of asthma in schoolchildren in urban Brazil. BMC Public Health 2007;7 10.1186/1471-2458-7-205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Rodriguez A, Vaca M, Oviedo G, et al. Urbanisation is associated with prevalence of childhood asthma in diverse, small rural communities in Ecuador. Thorax 2011;66:1043–50. 10.1136/thoraxjnl-2011-200225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Fattore GL, Santos CAT, Barreto ML. Social determinants of childhood asthma symptoms: an ecological study in urban Latin America. J Community Health 2014;39:355–62. 10.1007/s10900-013-9769-7 [DOI] [PubMed] [Google Scholar]
- 88. Tabalipa FdeO, Daitx RB, Traebert JL, et al. Indicators of violence and asthma: an ecological study. Allergology International 2015;64:344–50. 10.1016/j.alit.2015.04.003 [DOI] [PubMed] [Google Scholar]
- 89. Ponte EV, Cruz AA, Athanazio R, et al. Urbanization is associated with increased asthma morbidity and mortality in Brazil. Clin Respir J 2015;2016:1–8. [DOI] [PubMed] [Google Scholar]
- 90. Antunes FP, Costa MdaCN, Paim JS, et al. Social determinants of intra-urban differentials of admissions by respiratory diseases in Salvador (BA), Brazil. Rev Bras Epidemiol 2014;17(suppl 2):29–38. 10.1590/1809-4503201400060003 [DOI] [PubMed] [Google Scholar]
- 91. Dias C, Dias M, Friche A, et al. Temporal and spatial trends in childhood asthma-related hospitalizations in Belo Horizonte, Minas Gerais, Brazil and their association with social vulnerability. Int J Environ Res Public Health 2016;13 10.3390/ijerph13070704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92. Vlaski E, Lawson JA. Urban-rural differences in asthma prevalence among young adolescents: the role of behavioural and environmental factors. Allergol Immunopathol 2015;43:131–41. 10.1016/j.aller.2013.09.016 [DOI] [PubMed] [Google Scholar]
- 93. Von Hertzen LC, Haahtela T. Asthma and atopy - the price of affluence? Allergy 2004;59:124–37. 10.1046/j.1398-9995.2003.00433.x [DOI] [PubMed] [Google Scholar]
- 94. Awumbila M. Linkages between urbanization, Rural–Urban migration and poverty outcomes in Africa. Int Organ Migr 2014:3–24. [Google Scholar]
- 95. Platts-Mills TAE, Erwin E, Heymann P, et al. Is the hygiene hypothesis still a viable explanation for the increased prevalence of asthma? Allergy 2005;60(Suppl 7):25–31. 10.1111/j.1398-9995.2005.00854.x [DOI] [PubMed] [Google Scholar]
- 96. Cooper PJ, Vaca M, Rodriguez A, et al. Hygiene, atopy and wheeze-eczema-rhinitis symptoms in schoolchildren from urban and rural Ecuador. Thorax 2014;69:232–9. 10.1136/thoraxjnl-2013-203818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Barreto ML, Cunha SS, Fiaccone R, et al. Poverty, dirt, infections and non-atopic wheezing in children from a Brazilian urban center. Respir Res 2010;11 10.1186/1465-9921-11-167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Kawachi I, Berkman LF. Neighborhoods and health. Oxford University Press, 2003. [Google Scholar]
- 99. D'Amato G, D’Amato G. Environmental urban factors (air pollution and allergens) and the rising trends in allergic respiratory diseases. Allergy 2002;57:30–3. 10.1034/j.1398-9995.57.s72.5.x [DOI] [PubMed] [Google Scholar]
- 100. Fox S, Goodfellow T. Cities and development. 2nd edn Cities and Development, 2016: 1–340. [Google Scholar]
- 101. Asher MI, Stewart AW, Mallol J, et al. Which population level environmental factors are associated with asthma, rhinoconjunctivitis and eczema? review of the ecological analyses of Isaac phase one. Respir Res 2010;11 10.1186/1465-9921-11-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Stewart AW, Mitchell EA, Pearce N, et al. The relationship of per capita gross national product to the prevalence of symptoms of asthma and other atopic diseases in children (Isaac). Int J Epidemiol 2001;30:173–9. 10.1093/ije/30.1.173 [DOI] [PubMed] [Google Scholar]
- 103. Foliaki S, Nielsen SK, Björkstén B, et al. Antibiotic sales and the prevalence of symptoms of asthma, rhinitis, and eczema: the International study of asthma and allergies in childhood (Isaac). Int J Epidemiol 2004;33:558–63. 10.1093/ije/dyh031 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
thoraxjnl-2018-211793supp001.pdf (574.5KB, pdf)
thoraxjnl-2018-211793supp002.pdf (77.2KB, pdf)