Abstract
| Table of Contents | |
|---|---|
| Summary | 86 |
| 1. Background | 88 |
| 1.1 History and development of growth monitoring programmes | 88 |
| 1.2 Objectives of growth monitoring | 89 |
| 2. Expected benefits of growth monitoring and growth promotion | 90 |
| 3. Objectives of this review | 91 |
| 4. Methodology | 91 |
| 5. Evidence of effectiveness of growth monitoring programmes | 91 |
| 5.1 Nutritional status and mortality of young children | 91 |
| 5.1.1 Studies before 1990 | 91 |
| 5.1.2 Studies since 1990 | 96 |
| 5.2 Utilization of primary health services | 103 |
| 6. Quality of implementation | 104 |
| 7. Caregivers' knowledge and understanding of growth charts | 105 |
| 8. Empowerment and community mobilization | 106 |
| 9. Coverage and attendance | 107 |
| 10. Potential consequences if withdrawn | 108 |
| 11. Feasibility and conditions under which growth monitoring and promotion can be expected to work | 108 |
| 12. Cost‐effectiveness | 109 |
| 13. Potential adverse consequences | 109 |
| 14. Policy considerations and recommendations | 110 |
| References | 113 |
Summary
The rationale for growth monitoring and promotion is persuasive but even in the 1980s the appropriateness of growth monitoring programmes was being questioned. The concerns centred largely around low participation rates, poor health worker performance and inadequacies in health system infrastructure that constrained effective growth‐promoting action. More recently there has been a call for a general review of the impact of large‐scale growth monitoring and promotion programmes to determine if the investments are justified. The launch of the new World Health Organization growth standard and charts has been a timely reminder of this debate. It is within this context that this review has been undertaken: the main purpose is to analyse the evidence that growth monitoring programmes are effective in conferring measurable benefits to the children for whom growth charts are kept. The benefits considered here are improved nutritional status, increased utilization of health services and reductions in mortality.
There is evidence from small‐scale studies in Nigeria, Jamaica, India (Narangwal and Jamkhed), and from large programmes in Tanzania (Iringa), India (Tamil Nadu Integrated Nutrition Project), Madagascar and Senegal that children whose growth is monitored and whose mothers receive nutrition and health education and have access to basic child health services have a better nutritional status and/or survival than children who do not. There is tentative evidence from a large‐scale programme in Brazil (Ceara) that participation in growth monitoring confers a significant benefit on nutritional status independent of immunization and socio‐economic status. There is evidence from India (Integrated Child Development Services) and Bangladesh (Bangladesh Rural Advancement Committee and Bangladesh Integrated Nutrition Project) that growth monitoring has little or no effect on nutritional status in large‐scale programmes with weak nutrition counselling. There is evidence from Tamil Nadu in a randomized trial that when mothers are visited fortnightly at home and have unhurried counselling, no additional benefit accrues from the visual depiction of growth on a chart. There is some evidence that growth monitoring can improve utilization of health services.
Although there is no unequivocal evidence that growth monitoring is beneficial per se, it was perceived to be beneficial by the investigators of several of the studies described in this review. Growth monitoring can provide an entry point to preventive and curative health care and was an integral part of programmes that were associated with significant reductions in malnutrition and mortality. Good nutrition counselling is paramount for growth promotion and is often done badly. Effort must be made to improve this and provide age‐appropriate advice to achieve exclusive breastfeeding and appropriate complementary feeding, irrespective of decisions about growth monitoring. This review highlights the paucity of rigorous trials to determine the impact of growth monitoring separately from the impact of growth promotion. There is no controversy about the need for growth‐promotion activities, and weighing children is desirable to assess health and nutrition status. The debatable question is whether weights need to be monitored monthly and plotted on a chart. Even if there is a policy for growth monitoring, if a child has grown well in the first year of life then it would appear that little is gained by monitoring weight beyond the age of 12 months, and that the time spent monitoring older children might be better spent improving the counselling given to caregivers of infants.
Growth monitoring may not be the best use of limited resources in countries with weak economies and inadequate health budgets: a limited package of health and nutrition interventions including good nutrition counselling may be preferable, aiming for good coverage and effective health worker performance, and prioritizing infants and children <18 months of age. Two of the potential strengths of growth monitoring are that it provides frequent contact with health workers and a conduit to child health interventions. Taking into account the evidence from recent nutrition education interventions in India and Peru that used multiple delivery channels within routine health services, possible options to consider for the future are:
-
•
If growth monitoring is not in place, then focus efforts on growth‐promotion activities and consider counselling caregivers intensively at all child health contacts and through home visits by community health workers or volunteers. Where possible chart weights at birth, immunization (6, 10, 14 weeks and 9 months), vitamin A distribution and sick‐child visits. Follow up and counsel any whose weight is faltering and those with a weight‐for‐age <−2 SD.
-
•
Where growth monitoring exists but the coverage is low or there is little potential for improvement, then consider abandoning it and re‐focus efforts on growth‐promotion activities as described above.
-
•
Where growth monitoring and promotion programmes currently exist and there is potential for improvement, then maximize their potential, strengthen the nutrition counselling elements, combine growth monitoring with other health intervention channels such as immunization for the convenience of caregivers, and ensure consistent message delivery. Target younger children and use the time gained to improve services. Monitor weight until 12 months of age. If there are episodes of growth faltering, continue to monitor until 18 months. Where cultural traditions and conditions are favourable, use growth monitoring additionally for community mobilization to address underlying socio‐economic and other causes of poor nutrition and health.
Scaling up from successful small‐scale growth monitoring and promotion programmes to effective national programmes will require political commitment, investment, extensive capacity building and strengthening of health systems. Training, supervision and support will need to be improved if health workers are to be equipped with the necessary knowledge and communication skills to promote healthy growth. Impact will be related to coverage, intensity of contact, health worker performance, adequacy of resources and the ability and motivation of families to follow advice.
Keywords: growth monitoring, growth promotion, programme effectiveness, nutritional status, child survival
1. Background
1.1 History and development of growth monitoring programmes
Growth monitoring, particularly of infants and young children, is widely regarded as an essential element of primary health care and in a recent survey 154 of 178 Ministries of Health (88%) reported that they monitor child growth (de Onis et al. 2004). The potential of growth monitoring lies in its use as a diagnostic tool for identifying a child with a nutritional or health problem, thus enabling action to be taken before the child's nutritional status is seriously jeopardized. Most growth monitoring programmes use weight charts to provide a graphic representation of a child's weight‐for‐age. An undernourished or sick child will have a slower rate of weight gain than a well‐nourished, healthy child. Monitoring growth by plotting a child's weight at regular intervals and comparing the pattern of growth to reference curves of healthy children permits early detection of growth faltering. It provides an early warning signal and a trigger for early action.
Growth monitoring has a long history. Regular weighing of infants was advocated by Guillot in the 1850s for assessing the adequacy of lactation in neonates, and in the 1870s Cnopf in Nuremberg was the first to weigh infants systematically beyond the perinatal period, while Russow in St Petersburg was the pioneer of growth standards and of the idea that growth reflects an infant's well‐being (Tanner 1991). In 1899 in St Helens, England, regular child weighing and practical advice were provided by volunteers of the Infant Welfare Movement (Williams 1986) and by the mid‐1920s there was a nationwide network of welfare centres that were organized around child weighing. The first growth reference was introduced in England in 1906 (Tanner 1991). Dr Cicely Williams reported that as early as 1910 mothers in Jamaica were weighing their babies (Rohde 1988).
In 1961 the use of growth charts was recommended by a joint committee of the Food and Agriculture Organization and World Health Organization (WHO) (WHO 1962). The name ‘Road‐to‐Health chart’ originated in Malawi, but much of the pioneering work and advocacy for monitoring growth in developing countries was by Dr David Morley and colleagues at Ilesha, Nigeria (Cuthbertson & Morley 1962; Morley 1962). Over the years many different types of growth chart have been designed: many additionally serve as child health records showing illness episodes, immunization status etc. and provide advice, for example on child feeding, oral rehydration, and care‐seeking. The direction of the child's line is emphasized, that is, whether rising in parallel to the reference curve (good), or flat (early warning) or falling (danger sign). In the 1970s growth monitoring was implemented in several developing countries in Africa, Asia, Latin America and the Near East both by governments and by agencies, notably the Catholic Relief Services and the United States Agency for International Development (Griffiths 1981). Many systems emerged and WHO coordinated efforts to develop a standard weight chart and published guidelines for its use in health services (WHO 1978).
Support for growth monitoring and promotion grew considerably in the 1980s and the United Nations Children's Fund (UNICEF) was an enthusiastic advocate. It was a key component of UNICEF's selective primary health‐care strategy that promoted growth monitoring, oral rehydration, breastfeeding and immunization (GOBI). UNICEF also championed community involvement in health care: the approach was to make low‐cost, simple technologies available to improve health of all children at risk (Grant 1984). UNICEF provided countries with weighing scales and supported the local production of growth charts. Sufficient funds to build local capacity to make the programmes work effectively, however, were not allocated. Although growth promotion had always been envisaged as an integral part of growth‐monitoring procedures, promotive actions were often eclipsed by weighing and charting. The term ‘growth monitoring and promotion’ was therefore introduced to make growth promotion an explicit component (Pearson 1995).
In 1990, Samir Basta, then Director of the UNICEF Evaluation Office, initiated an evaluation of UNICEF‐supported growth‐monitoring activities in seven countries. This revealed low coverage, poor understanding of the causes of malnutrition, and few growth‐promotion actions (Pearson 1995). Although the Report concluded that UNICEF had invested insufficient funds to make the programmes work, many took the Report to mean that growth‐monitoring activities were ineffective (Shrimpton et al. 2003). The Report led to discussions that reshaped UNICEF's policies and strategies and in the 1990s there was disinvestment in community‐based nutrition programmes and a notable shift in expenditure away from growth monitoring towards breastfeeding promotion, immunization and micronutrients, especially vitamin A and iodine.
Limitations encountered in disease‐specific child health programmes led to the development of the current WHO/UNICEF strategy of Integrated Management of Childhood Illness (IMCI), which was first introduced at country level in 1996 with the aim of reducing child mortality. The three main elements are improving health worker skills, improving health systems and improving family practices so as to prevent disease and improve care‐seeking (Bryce et al. 2005). Within IMCI, growth charts are used to classify a child's weight‐for‐age to guide decisions on follow‐up and referral. Emphasis is given to nutrition counselling at every sick‐child contact rather than on regular growth monitoring.
1.2 Objectives of growth monitoring
The main aims of growth monitoring, as originally conceived, are to:
-
1
Provide a diagnostic tool for health and nutrition surveillance of individual children and to instigate effective action in response to growth faltering.
-
2
Teach mothers, families and health workers how diet and illness can affect child growth and thereby stimulate individual initiative and improved practices.
-
3
Provide regular contact with primary health‐care services, and so facilitate their utilization.
The underlying logic is that if growth faltering is detected early and is made visible to health workers and families, then families can respond by changing their child‐care practices, provided they are offered proper motivation, given clear, feasible alternatives, and given a role in deciding what practices they will try to change (Griffiths 1981).
Subsequent objectives of growth monitoring that have developed include:
-
4
Community mobilization: Growth monitoring can serve as an entry point for community mobilization and social action, especially when growth monitoring data are aggregated and used for community‐level assessment and analysis of child malnutrition. The premise is that caregivers' participation in growth monitoring will lead to increased awareness of factors that detrimentally affect children's health and that they will influence community leaders and citizens to take collective and effective action to address underlying socio‐economic causes of poor health and promote social and economic equity. This is in keeping with the Alma Ata Declaration of 1978 which emphasizes the need for community and individual participation in primary health care.
-
5
Targeting supplementary feeding: The weight chart is widely used to determine eligibility for entry to supplementary feeding programmes. The criterion is usually a weight‐for‐age below one of the reference curves on the weight chart, equivalent to ‘moderate’ underweight. This invariably shifts the focus of growth monitoring towards identifying children who meet this criterion, rather than intervening at the first sign of growth faltering. Consequently no action is taken until the child is significantly underweight. As health workers choose who should receive assistance, the collaborative involvement of families in decision‐making is lost, as well as any educational benefit of regular growth monitoring. Using weight charts in this way is thus contrary to the precept of growth monitoring. Anecdotal reports suggest that once enrolled in supplementary feeding programmes and approaching the exit criterion, some children may be purposely underfed so as to remain beneficiaries. Although supplementary feeding programmes may have their place in offsetting food shortage, growth faltering is often the result of poor feeding practices, which can still prevail even among beneficiaries of food distribution programmes.
-
6
Reporting prevalence of underweight: Governments and agencies may require health workers to provide information on the extent of underweight in their locality, or the number of children failing to grow in a given month. Currently over 50% of countries transfer information obtained from growth monitoring to higher levels (de Onis et al. 2004). In some countries time‐consuming procedures are devised, with information systems spanning village, district, provincial and national levels. In Vietnam, for example, it takes several days each month at district level to collect and aggregate village data in order to report to higher authorities the prevalence of underweight and coverage of child weighing (Shrimpton 2003). Weights may be recorded in logbooks and never plotted, and the growth chart may be used simply to determine if a child is underweight, sometimes at a later date instead of in the mother's presence. Thus, the promotive aims of growth monitoring are surrendered. Furthermore, the information submitted may not permit meaningful analysis and interpretation so that even the nutrition status surveillance objective may not be achieved.
2. Expected benefits of growth monitoring and growth promotion
The main anticipated benefits in developing countries are:
-
•
reductions in undernutrition, morbidity and mortality among young children.
Linked benefits are:
-
•
early intervention when growth faltering is more easily remedied;
-
•
improved knowledge about the effect of diet and illness on growth;
-
•
families motivated and enabled to take effective action;
-
•
nutrition and health counselling tailored to individual needs;
-
•
opportunity to assess remedial actions;
-
•
greater self‐reliance and self‐esteem;
-
•
greater utilization of preventive health‐care services;
-
•
fewer referrals for curative care; cost savings; and
-
•
communities mobilized to address underlying socio‐economic causes of poor health.
3. Objectives of this review
The logic behind the advocacy of growth monitoring and promotion is persuasive but even in the 1980s the appropriateness of growth monitoring programmes was being questioned. The concerns centred largely around low participation rates, technical problems related to the weighing process, and operational problems that constrained effective action stemming from poor health worker performance and/or inadequacies in health system infrastructure (Editorial 1985; Gopalan & Chatterjee 1985; Nabarro & Chinnock 1988; Gerein & Ross 1991). More recently there has been a call for a general review of the impact of large‐scale growth monitoring and promotion programmes to determine if the investments are justified (Save the Children UK 2003; Hossain et al. 2005). The launch of the new WHO growth standard and new growth charts that can be used to assess children everywhere regardless of ethnicity has added to this debate (WHO Multicentre Growth Reference Study Group 2006). It is within this context that this review has been undertaken. The purpose is to go beyond the commonsense appeal and analyse critically the evidence that growth monitoring programmes are effective in conferring measurable benefits to the children for whom growth charts are kept. The benefits considered here are improved nutritional status, increased utilization of health services and reductions in mortality. In addition, the quality of implementation and conditions for success are addressed, together with possible consequences of withdrawing growth monitoring activities.
4. Methodology
Database searches included Medline, Popline, PubMed, CAB Abstracts and the Cochrane Library. The main search term was child growth monitoring, which identified 1575 articles. Excluded were studies in developed countries and of growth monitoring for obesity, and interventions where growth monitoring was an outcome related to treatment (e.g. giving growth hormones). Further searching was performed using related terms, together with hand searching of related articles and authors' references. Published and unpublished reports were sought in the archives of the London School of Hygiene and Tropical Medicine, and several reports were kindly provided by Dr Nune Mangasaryan (UNICEF).
5. Evidence of effectiveness of growth monitoring programmes
The potential effectiveness of growth monitoring programmes would be suggested by a demonstration of either that:
-
•
growth monitoring can improve nutritional status and/or survival of young children (Hypothesis 1)
or that:
-
•
growth monitoring can improve utilization of health services (Hypothesis 2) and young children with improved health service utilization have better nutritional status and/or survival (Hypothesis 3).
This is shown in Fig. 1.
Figure 1.
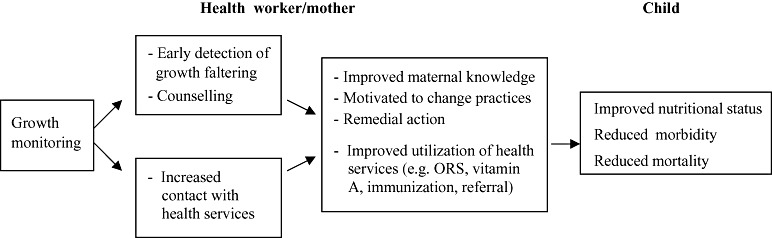
Framework for analysing the effectiveness of growth monitoring programmes. ORS, oral rehydration salts.
The following section focuses on the evidence for a benefit of growth monitoring programmes on nutritional status and mortality. Later, Section 5.2 will examine evidence related to utilization of health services.
5.1 Nutritional status and mortality of young children
Hypothesis 1: Studies were examined for evidence that growth monitoring can improve nutritional status and/or survival of young children.
5.1.1 Studies before 1990
The initial enthusiasm for growth monitoring was influenced by the impressive reductions in mortality and malnutrition from early studies reported from Nigeria, Jamaica and India. In the 1980s larger programmes in Tanzania and India were implemented. These and other studies are described below: all included growth monitoring but the growth‐promotion components varied and these are identified in the respective tables.
(i) Imesi, Nigeria
At Imesi, where there was growth monitoring at the under‐5 clinic, infant mortality was 57 per 1000 live births compared with 91 per 1000 in the control village Oke Mesi (Cunningham 1978; Gwatkin et al. 1980). Differences in 1–4‐year mortality were even more striking (18 vs. 51 per 1000, P < 0.001), and children in Imesi on average were 300–400 g heavier and 1.5–3 cm taller than control children (P < 0.01 in each case). Growth was similar up to age 6 months. Immunization coverage was 90% at Imesi compared with 45% in Oke Mesi, indicating good uptake of health services at Imesi. Evaluations that compare just two villages, however, are not methodologically robust and growth monitoring was accompanied by other health interventions (Table 1) that were likely to reduce mortality or improve growth.
Table 1.
Comparison of mortality and prevalence of underweight in Imesi (intervention village) and Oke Mesi (control village). Data are for 1966–67
| Nigeria (Cunningham 1978; Gwatkin et al. 1980) | Infant mortality rate per 1000 live births | 1–4‐year mortality rate per 1000 | Weight‐for‐age <80% median |
|---|---|---|---|
| a) Imesi under‐5 clinic, available 7 h day−1, 6 days week−1, and staff always on call. Attendees seen with minimum of delay. Coverage 95% | a) 57 (15/262) | a) 18 (16/887) | a) 38% (399/1038) |
| Growth monitoring + Nutrition education + Immunizations + Medications according to standing orders + Malaria prophylaxis | |||
| b) Control village Oke Mesi had no clinic | b) 91 (33/361) | b) 51 (52/1015) | b) 50% (482/971) |
(ii) Hanover, Jamaica
A young child nutrition programme, which comprised growth monitoring and nutrition education delivered by community health aides, started in July 1973 in the eastern half of the Parish of Hanover, and in July 1974 in the western half. This allowed a time‐series comparison of mortality in one of Jamaica's 14 Parishes (Alderman et al. 1978; Gwatkin et al. 1980). Table 2 shows that mortality in children aged 1–48 months fell by at least half in each region concurrently with the intervention. There was no comparable reduction in mortality in other Parishes. There was also a concurrent halving in the prevalence of underweight. In this programme, those not malnourished were weighed at field clinics every 2 months. Those <75% weight‐for‐age were weighed monthly, and visited at home weekly where the aides instructed parents in food preparation and child nutrition. The basic message was that diet was a critical determinant of growth and development. A similar intervention in south Trelawny, Jamaica, noted a 34% decrease in prevalence of underweight coincident with the introduction of growth monitoring at home by community health volunteers, compared with a 13% decrease for the Parish as a whole, but the sample size was small (∼100) (Melville et al. 1995).
Table 2.
Comparison of mortality and prevalence of underweight (weight‐for‐age <75% of median) in East and West Hanover. Data are for 1971–76
| Jamaica (Alderman et al. 1978; Gwatkin et al. 1980) | 1–48‐month mortality rate per 1000 (actual number of deaths) | Prevalence of underweight (%) | ||||
|---|---|---|---|---|---|---|
| Year | East | West | East | West | ||
| Intervention: Home visits by community health aides (1 aide per ∼43 children) | 71–72 | 13.7 (46) | 12.7 (42) | |||
| 72–73 | 15.4 (52) | 17.6 (58) | July 73 | 11 | – | |
| 73–74 | 5.6* (19) | 13.3 (44) | July 74 | 6* | 13 | |
| Growth monitoring + Nutrition education + Hygiene education (Some medications and occasionally dried milk packets) Control: Time series | 74–75 | 7.4* (25) | 5.7* (19) | July 75 | 6* | 7* |
| 75–76 | 5.6* (19) | 5.7* (19) | ||||
Denotes the years with the intervention. Differences between pre‐ and post‐intervention were statistically significant for mortality (P < 0.001) and underweight (P < 0.0001).
The results of the Hanover study are methodologically more robust than the Imesi study, but the key question is whether the process of growth monitoring per se had a benefit. The view of the project workers was reportedly that ‘mothers learned so much about the relation between diet and health by watching their child's growth pattern that this alone led to dietary improvements’ (Griffiths 1981). To put this to the test would require a randomized trial of the home‐visiting education intervention with and without growth monitoring.
(iii) Narangwal, India
Despite marked increases in agricultural productivity in Ludhiana District during the ‘green revolution’, malnutrition and infant mortality remained high, and it was within this context that the Narangwal Nutrition Project was designed. The aim was to assess the effectiveness of nutrition and health interventions, singly and in combination, delivered at home by family health workers. Ten villages were assigned to one of four groups (nutrition; medical; nutrition+medical; and control) (Kielmann et al. 1978; Gwatkin et al. 1980). The nutrition component comprised growth monitoring, food supplements for underweight children under 3 years old and nutrition education. Growth monitoring was the entry point for individual counselling and targeting supplementation. All three types of service were associated with lower infant and young child mortality (Table 3). The nutrition component was associated with significantly lower 1–3‐year mortality compared with control villages (P < 0.025). Medical care had a greater impact than nutrition care on infant mortality. At 17 months of age onwards, children in villages with a nutrition component were 500–600 g heavier and 1–3 cm taller than control children (P < 0.05 in each case): from 6 months of age, their haemoglobin concentration was also significantly higher than controls, the mean difference at 12–18 months being about 15 g L−1. There was a greater proportional benefit from all services on the weight of low caste children.
Table 3.
Comparison of infant and young child mortality in Narangwal, India, according to intervention group. Data are for 1970–73
| India (Kielmann et al. 1978; Gwatkin et al. 1980) | Infant mortality rate per 1000 live births | 1–3‐year mortality rate per 1000 |
|---|---|---|
| Intervention: Weekly home visits lasting 5–7 min by paramedics. | ||
| a) Nutrition intervention (n = 3 villages) Growth monitoring + Nutrition education + 2 meals per day at village centre if underweight | 89 | 10 |
| b) Medical intervention (n = 2 villages) Immunization and medical treatment | 70 | 11 |
| c) Combined interventions (n = 3 villages) | 81 | 13 |
| d) Control (n = 2 villages). Basic health services | 129 | 19 |
Although widely quoted in the 1980s in support of growth monitoring, none of these three studies provides unequivocal evidence that growth monitoring per se confers a benefit, as it is not possible to disentangle the effect of other inputs.
(iv) Calcutta, Jamkhed and Haiti
Three other growth monitoring programmes (Gwatkin et al. 1980; Chaudhuri 1988; Genece & Rohde 1988) that were often highlighted in the 1980s are shown in Table 4. Although improvements in nutritional status and survival were substantial, growth monitoring was part of a wider primary health‐care package.
Table 4.
Nutritional status and mortality before and after implementing a growth‐monitoring package in India and Haiti.
| India (Gwatkin et al. 1980; Chaudhuri 1988), Haiti (Genece & Rohde 1988) | Indicator | Outcome | ||
|---|---|---|---|---|
| Intervention | Non‐project area (concurrent with post‐) | |||
| Pre‐ | Post‐ | |||
| Intervention: Growth monitoring + Primary health care | ||||
| Calcutta, India (Chaudhuri 1988) | % <75% weight‐for‐age | 32 | 18 | 32 |
| Jamkhed, India (Gwatkin et al. 1980) | Infant mortality per 1000 | 97 | 39 | 90 |
| % immunized | <1 | 84 | 15 | |
| Haiti (Genece & Rohde 1988) | Infant mortality per 1000 | 125 | 80 | |
| 1–4‐year mortality rate per 1000 | 25 | 12 | ||
| % immunized (measles) | <1 | 68 | ||
(v) Ghana and Lesotho
Nine clinics in each country were graded as high, medium or low according to their use of growth charts (Pielemeier 1978). Grading was based on: (1) the number of growth‐related teaching sessions; (2) whether the chart was used as an educational tool or simply as a clinic record; (3) whether mothers had growth charts in their possession; (4) whether growth was discussed with the mother; and (5) whether advice was given to mothers and, if so, the quality of that advice. Over 3000 children were weighed: those <80% weight‐for‐age in the high, medium and low‐rated clinics were respectively 33%, 34% and 37% in Ghana and 31%, 19% and 23% in Lesotho. No clear pattern of improved nutritional status emerged with better chart use.
(vi) Thailand
The weight of pre‐school children was monitored over a 6‐month period following introduction of growth charts in remote villages (Viravaidhya et al. 1981). Village health volunteers and village health communicators were responsible for nutrition surveillance and education. In three villages, monthly growth monitoring was combined with an active programme of nutrition education, and two other villages received growth monitoring alone. In the two control villages with no growth monitoring, the proportion of children <75% weight‐for‐age decreased by 1 percentage point over the 6‐month period: the corresponding decrease in underweight was 2 percentage points in villages with growth charts alone, and 9 percentage points (a 60% decrease) in villages where growth monitoring was combined with nutrition education (Table 5). In one village where growth monitoring and education was provided at home, the decrease was 76%. Unfortunately no villages received nutrition education alone so it is not possible to ascertain whether growth monitoring contributed to the success of the nutrition education programme by motivating mothers to change their child‐care practices. Growth monitoring alone, without linked activities, was largely ineffective, as would be expected.
Table 5.
Change in weight‐for‐age distribution in rural villages in Thailand after introducing growth monitoring with and without an active education programme. Data are for 1980–81.
| Thailand (Viravaidhya et al. 1981) | Distribution by weight‐for‐age (% of pre‐school children) | |||||
|---|---|---|---|---|---|---|
| Growth charts + education (n = 447) | Growth charts (n = 219) | No charts (n = 218) | ||||
| Initial | After 6 months | Initial | After 6 months | Initial | After 6 months | |
| Weight‐for‐age (% of median of Thai reference) | ||||||
| ≥90% | 44 | 56 | 55 | 53 | 47 | 49 |
| 75–89% | 41 | 38 | 35 | 39 | 45 | 44 |
| <75% | 15 | 6 | 10 | 8 | 8 | 7 |
(vii) JNSP Iringa, Tanzania
In 1980, WHO and UNICEF initiated Joint Nutrition Support Programmes (JNSP) in several countries including Tanzania, with funding from the Italian Government (Government of the United Republic of Tanzania et al. 1989; UNICEF 1993). The programme started in Iringa and drew heavily on the Triple‐A process of assessment, analysis and action. Aggregated growth‐monitoring data were used for community‐level assessment and analysis of child malnutrition, the main target actions identified being increased feeding frequency, use of energy‐dense foods and reduced women's workload. Village Health Committees met with parents of children with poor growth to activate the Triple‐A cycle at the household level. Few details are reported of the methodology for the evaluation analysis but the findings indicate reductions in the prevalence of underweight associated with the programme (Table 6). The enabling components included community mobilization and participation in planning actions, capacity building at various levels, a multifaceted holistic approach unique to each village and prioritizing attention to those most in need. Immunization coverage was reported as 92% in 1987–88. The impact on infant and child mortality was not reported because of incomplete data. Knowledge of the growth chart was good, but no significant association was found between caregivers' understanding and child nutritional status. Most of the programme's activities were linked to improving child nutrition and health, so the role of growth monitoring per se cannot be disaggregated.
Table 6.
Percentage of underweight children in 168 project villages and 442 non‐project villages in Iringa. Data from project villages are for 1984 baseline (n = 30 600) and 1987 post‐intervention (n = 37 054)
| Iringa, Tanzania (Government of the United Republic of Tanzania et al. 1989) | Indicator | % underweight | ||
|---|---|---|---|---|
| Intervention | Non‐project area (concurrent with post‐) | |||
| Pre‐ | Post‐ | |||
| Intervention: Growth monitoring + Maternal and child health + Immunizations + Water and sanitation + Household food security + Child care and development + Income generation | <80% weight‐for‐age | 55.9 | 37.9 | 50.0 |
| <60% weight‐for‐age | 6.3 | 1.7 | 5.6 | |
The success experienced in Iringa led to rapid expansion to other regions of Tanzania, but the JNSP was weakened by health sector reform and community mobilization was considered too slow. Consequently the emphasis shifted to vertical micronutrient programmes and the decline in malnutrition was halted (Gillespie et al. 2003).
(viii) TINP India
The Tamil Nadu Integrated Nutrition Project (TINP) started in 1980 in parallel with Iringa and received World Bank support until 1989. In contrast to Iringa, TINP was a vertical programme with predefined inputs and little community participation. Inputs for children included growth monitoring, targeted nutrition counselling and supplementary feeding if growth faltered, immunization, deworming, vitamin A and basic health care. Pregnant women received iron and folate supplements. Discrepancies in midterm and final evaluations based on different data sets led to a re‐analysis of data from the pilot Kotampatti block (Shekar 1991; Shekar & Latham 1992). Project children aged 6–25 months were significantly heavier (P < 0.001) and more likely to have been immunized, dewormed and given vitamin A than children measured at baseline (P < 0.01 in each case). A secular trend was thought unlikely. The difference in weight, however, was apparent at age 6 months and then sustained (Table 7), thus any impact may be associated with better maternal or early post‐natal nutrition. Birth weights are unavailable.
Table 7.
Mean bodyweights of children in TINP project areas. Data are for November 1980 baseline (n = 114 children) and November 1986 (n = 308 children)
| TINP, India (Shekar 1991) | Child age | Mean bodyweight (g) | P | ||
|---|---|---|---|---|---|
| Baseline Nov. 1980 | Nov. 1986 | Difference (g) | |||
| Intervention: Growth monitoring + Nutrition and health education + Targeted supplementary feeding + Immunizations + Vitamin A + Deworming + Basic health care | 6 months | 5157 | 5915 | +758 | 0.006 |
| 12 months | 6906 | 7298 | +392 | 0.04 | |
| 18 months | 7452 | 8101 | +649 | 0.005 | |
| 24 months | 8189 | 8853 | +664 | 0.06 | |
TINP, Tamil Nadu Integrated Nutrition Project.
5.1.2 Studies since 1990
There have been few evaluation studies in the last two decades, probably reflecting the shift in emphasis away from growth monitoring and towards vertical interventions such as immunization and micronutrients.
(ix) BRAC Bangladesh
The Bangladesh Rural Advancement Committee (BRAC) has included growth monitoring in its package of primary health‐care activities since 1987. Within 4 years, 1322 growth‐monitoring centres were established and around 20 000 children were weighed each month (Karim et al. 1994). Mothers of children with faltering growth were instructed to give them more food. Those with children <60% weight‐for‐age were visited at home by a BRAC doctor and advised about feeding. Children who were ill and needed treatment were referred to a health facility. A small evaluation was conducted in 1990 in which 496 children aged 6–23 months were located and characterized as participating or not‐participating in the growth monitoring programme and were weighed (Table 8). No benefit on weight‐for‐age was apparent by participating in growth monitoring, but as participants and non‐participants may have differed in important ways, no firm conclusions can be drawn.
Table 8.
Comparison of the nutritional status of children aged 6–23 months who participated in growth monitoring (n = 188) vs. non‐participants (n = 308) in rural Bangladesh
| Bangladesh (Karim et al. 1994) | Distribution by weight‐for‐age | |
|---|---|---|
| Grade | % | |
| a) Intervention: Health and nutrition education delivered by BRAC health workers with support from village volunteers. Average consultation 5 min | a) | n = 188 |
| >75 | 52.1 | |
| 60–75 | 46.3 | |
| <60 | 1.6 | |
| Growth monitoring + Nutrition and health education + Primary health‐care package | ||
| b) Non‐participants: Primary health‐care package | b) | n = 308 |
| >75 | 51.0 | |
| 60–75 | 45.2 | |
| <60 | 3.8 | |
BRAC, Bangladesh Rural Advancement Committee.
(x) Tamil Nadu, India
The most methodologically robust study to date is that of George and colleagues in south India (George et al. 1993). Twelve non‐adjoining villages in KV Kuppam block were paired with respect to caste composition, access to a main road, cropping patterns and distance from rural clinics. One of each pair was then randomly allocated to receive monthly growth monitoring at home, while the other received no growth monitoring. All villages had a functioning primary health‐care system, which provided immunizations, deworming, antenatal care, curative care and family planning services, and all villages received a health and nutrition education intervention, delivered by a village health worker twice a month at home. The village health workers were local mothers with 2 months of training. In the intervention villages these health workers also delivered the growth‐monitoring component. The aim of the study was to test if ‘good’ growth monitoring in conjunction with an intensive education intervention conferred any additional benefit on weight and height gain compared with the education intervention alone. During the 30‐month study period, the education intervention was associated with improved nutritional status to a similar extent in both sets of villages (Table 9). This apparent lack of benefit of growth monitoring led the authors to conclude that mothers do not seem to need a visual depiction of growth to motivate them to take action. If fortnightly home visits, however, result in a ‘ceiling’ effect for the education intervention, then any additional benefit of growth monitoring may not be discernible, leaving open the possibility as to whether growth monitoring might improve the quality of counselling in less intensive settings. Bentley and colleagues also cautioned that chance differences between the two groups, especially as the growth‐monitoring villages appeared more ‘traditional’, might have obscured a real intervention effect (Bentley et al. 1993).
Table 9.
Comparison of mean weight‐for‐age z‐scores of children aged 3–23 months measured at baseline (July 1987) and at the end of the study period (December 1989) in Tamil Nadu
| Tamil Nadu, India (George et al. 1993) | Mean weight‐for‐age z‐score for children aged 3–23 months | |||
|---|---|---|---|---|
| Baseline July 1987 | Dec. 1989 | Difference | ||
| 12 villages with primary health care: immunization, deworming, curative care, antenatal care, family planning services randomized to intervention and control | ||||
| Intervention (6 villages): | n = 515 | n = 558 | ||
| Health and nutrition education twice a month + growth monitoring delivered at home monthly by village health workers | Harijan | −2.20 | −1.82 | +0.38 |
| Other castes | −2.27 | −1.97 | +0.30 | |
| Control (6 villages): | n = 505 | n = 535 | ||
| Health and nutrition education twice a month delivered at home by village health workers | Harijan | −2.24 | −1.88 | +0.36 |
| Other castes | −1.98 | −1.78 | +0.20 | |
(xi) Ceara, Brazil
An ecological study was carried out in 140 of the 184 municipalities in the State of Ceara in north‐east Brazil (de Souza et al. 1999). Growth monitoring is a state‐wide activity but the percentage of infants and children participating in growth monitoring varies among the municipalities, ranging from 42% to 100%. The prevalence of inadequate weight gain also varies among municipalities, as does access to health services. This study examined the relative contribution of growth‐monitoring participation and nine other variables (exclusive breastfeeding, immunization, antenatal care, water supply, sanitation, female literacy, family income, gross municipality product and urbanization) to variations in the prevalence of inadequate weight gain. As might be anticipated, municipalities with poorer socio‐economic status and poorer access to primary health‐care services had a higher prevalence of inadequate weight gain. Multiple linear regression analysis was used to find the independent effect of each variable. In the final predictive model, a 10% increase in growth‐monitoring participation was associated with a 4.7% decrease in the prevalence of inadequate weight gain among infants aged 0–11 months, and a 2.9% decrease in prevalence of inadequate gain in those aged 12–23 months (P < 0.0001 in each case). The only other significant determinants were urbanization (both age groups) and female illiteracy (12–23 month age group). These variables accounted for 38% of the variance in the prevalence of inadequate weight gain in infants, and 26% of the variance in children.
The analysis pertained to municipalities, not individual children, and both the weight gain data and the participation data were obtained from routine information relayed monthly by community health workers to supervisors in the municipality. Inadequate weight gain was defined as no weight gain, or a fall in weight, between two consecutive measurements, and the proportions with inadequate gains each month were averaged over 30 months. The authors considered that the results may be evidence of the effectiveness of growth monitoring, but it is difficult to exclude reverse causation. For example, if community health workers in a given municipality opt to select poorly growing children for regular monitoring, then this will cause the participation rate to be low (rather than low participation leading to inadequate weight gain). Although the findings are suggestive of a growth‐monitoring effect, they must be considered as tentative.
(xii) ICDS, India
The Integrated Child Development Services (ICDS) scheme was launched in 1975 and is the largest nutrition programme in India, serving many millions of children, adolescents, and pregnant and lactating mothers. The programme provides a package of health and nutrition services and pre‐school education, delivered by honorary anganwadi workers and helpers (Avsm et al. 1995; Kapil & Pradhan 1999). The nutrition component includes monthly growth monitoring for children <3 years, a ready‐to‐eat meal, iron and folic acid, and vitamin A every 6 months. There have been marked improvements in anthropometric status since 1975, which have been attributed to the programme (Kapil & Pradhan 1999), but these might reflect a secular trend. Comparisons of ICDS and non‐ICDS blocks show statistically significant differences in moderate and severe malnutrition, although the differences from a public health perspective are small (Table 10), the proportions <75% weight‐for‐age being 27% and 30% for ICDS and non‐ICDS blocks respectively (Avsm et al. 1995). In an evaluation of 3704 rural children whose mothers were largely illiterate, analysis of covariance was used to control for socio‐economic status and other programme services, and showed that growth monitoring did not have an impact on weight‐for‐age or morbidity (Gopaldas et al. 1990). Weaknesses in ICDS programme delivery, including incorrect weighing and plotting (Kapil et al. 1996), failure to identify children with growth faltering and lack of nutrition counselling, have been reported (Gopaldas 1988; Lalitha & Standley 1988; Gopaldas et al. 1990) and might explain the programme's lack of impact. Also participating children tended to be older than 18 months and thus had passed the critical period when interventions to prevent growth faltering are most effective (Shrimpton et al. 2001). In a joint initiative by the Bihar State Government and UNICEF, known as the Dular strategy, efforts are underway to enhance the effectiveness of ICDS by strengthening community participation and support systems, including greater emphasis on the training of anganwadi workers and volunteers, and establishing District Support Teams.
Table 10.
Comparison of the nutritional status of children aged 2–6 years in ICDS project areas (n = 22 333) and non‐ICDS areas (n = 13 854) in India
| ICDS, India (Avsm et al. 1995) | Distribution by weight‐for‐age | |
|---|---|---|
| Grade | % | |
| a) Intervention: Health and nutrition education delivered by anganwadi workers with support from village volunteers | a) | n = 22 333 |
| >75 | 73.4 | |
| Growth monitoring + Nutrition and health education + Supplementary food + Primary health‐care package | 60–75 | 20.3 |
| <60 | 6.3 | |
| b) Non‐ICDS: Basic health care | b) | n = 13 854 |
| >75 | 70.0 | |
| 60–75 | 21.8 | |
| <60 | 8.2 | |
ICDS, Integrated Child Development Services.
(xiii) Senegal and Madagascar
In 1994 and 1996, respectively, the governments of Madagascar and Senegal contracted out delivery of large‐scale community nutrition projects to non‐governmental organizations (NGOs) and civil society groups. The services comprised monthly growth monitoring, weekly nutrition and health education, food supplements for underweight children, referral of sick or severely malnourished children to health facilities, home visits, and either improved access to water supplies (Senegal) or income generation (Madagascar) (Marek et al. 1999). Children were allowed to stay in the programme for 4 months in Madagascar and 6 months in Senegal. Substantial reductions in the percentage underweight were reported over time, and during their period of participation (Table 11). Nationwide malnutrition rates in 2004 were 17% in Senegal compared with 23% in 1992, and 34% in Madagascar compared with 39% in 1997 (Sall & Sylla 2005). These reductions contrast with the rising trend seen in sub‐Saharan Africa.
Table 11.
Percentage of children underweight (<80% weight‐for‐age) before and after implementing community nutrition projects in Madagascar and Senegal. Data are for 1994–97 Madagascar and 1996–98 Senegal
| Madagascar, Senegal (Marek et al. 1999) | % <80% weight‐for‐age | ||
|---|---|---|---|
| Intervention: Community nutrition services delivered by private sector Growth monitoring + Nutrition and health education + Food supplements + Referral if sick or malnourished | a) Madagascar (data are for project beneficiaries) | ||
| District | Baseline | Sep. 1997 | |
| Talanolo | Jan. 1994 25% | 7% | |
| Soameva | Nov. 1994 23% | 6% | |
| Tantely | Nov. 1995 30% | 10% | |
| Vonon | Nov. 1996 35% | 16% | |
| b) Senegal (data are for project beneficiaries) | |||
| 4 cohorts | At enrolment | After 5 months | |
| 60–70% | 20–30% | ||
| c) Senegal (beneficiaries and non‐beneficiaries) | |||
| Entire neighbourhoods | Baseline | After 17 months | |
| 28% | 24% | ||
The reductions in malnutrition rates were accompanied by improvements in health indicators. Infant mortality fell from 86 to 61 per 1000 live births between 1986 and 2005 in Senegal, and child mortality fell from 199 to 121 per 1000. In Madagascar, between 1997 and 2003, under‐5 child mortality fell from 168 to 126 per 1000. In both countries, the Prime Ministers have direct control for child nutrition and health through a multisectoral approach and donor financing (Sall & Sylla 2005). Project managers were reported as believing that the impact on malnutrition rates was due to improved care provided by mothers through regular growth monitoring and promotion as only a small amount of the food supplement was consumed by the target children (average 25 g day−1). A rapid ripple effect was surmised, with mothers learning from each other so that whole communities gained from the programme (T. Marek, personal communication).
(xiv) BINP Bangladesh
The Bangladesh Integrated Nutrition Project (BINP) was established in 1996 and funded by a loan of $60 million from the World Bank. Initially the project served a population of around 15 million in 59 thanas, before being expanded nationally in 2002 and renamed as the National Nutrition Project. At monthly growth‐monitoring sessions held at community nutrition centres, children aged 0–23 months are weighed and caregivers counselled on young child feeding, health, hygiene and family planning. Supplementary feeding is available for those <−2 SD weight‐for‐age. In 2002, the project was evaluated by comparing three of the first six thanas to be established with three matched thanas from non‐project areas (Hossain et al. 2005). The selected thanas were similar in socio‐economic and demographic variables. The nutritional status of children aged 6–23 months in the project areas did not differ significantly from those in non‐project areas (Table 12), the proportions <−2 SD weight‐for‐age being 47% and 48%, respectively, and the mean SD score was −1.92 in both groups. Their similarity was confirmed in a multiple regression analysis as there was no association between living in a project area and weight‐for‐age: the significant factors were child age, socio‐economic status, maternal body mass index and maternal education. Karim and colleagues also found no significant difference between BINP and non‐BINP areas in their end‐line evaluation (Karim et al. 2003; The World Bank 2005).
Table 12.
Comparison of weight‐for‐age distribution in children aged 6–23 months in BINP project and non‐project areas in Bangladesh. Data are for 2002
| BINP, Bangladesh (Hossain et al. 2005) | Distribution by weight‐for‐age (% of children aged 6–23 months) | |
|---|---|---|
| Project area (n = 1598) | Non‐project area (n = 790) | |
| Intervention: Growth monitoring + Nutrition and health education + Food supplements if underweight | ||
| Weight‐for‐age (SD score) | ||
| ≥−2 | 53.4 | 51.6 |
| −2 to −3 | 35.2 | 36.3 |
| <−3 | 11.4 | 12.1 |
BINP, Bangladesh Integrated Nutrition Project.
There was no significant difference in exclusive breastfeeding but project mothers reported significantly better complementary feeding practices than non‐project mothers. The difference was 8 percentage points (i.e. 56% vs. 48% gave complementary foods at 5–6 months, P < 0.0001) (Save the Children UK 2003). Only 7% of project mothers understood the growth chart and only 22% of severely underweight children were enrolled for supplementary feeding. Of those severely underweight who were enrolled, 49% were still severely underweight at completion, 4 months later (Save the Children UK 2003). The competence of community nutrition workers was questioned both in their ability to weigh children satisfactorily and as educators. The supplementary feeding component had a high opportunity cost as beneficiaries were expected to attend daily for 3–4 months and the ration was modest (150 kcal day−1 if moderately underweight, and 300 kcal day−1 if severe). Sharing and substitution were common: 67% of mothers reported that they used the supplement to replace the normal meal, rather than as an addition. Lack of effect may thus be due to weaknesses in programme delivery rather than to any inherent ineffectiveness of growth monitoring as an intervention.
(xv) AIN‐C, Honduras
The Atención Integral a la Ninez‐Comunitaria (AIN‐C) programme (Community‐Based Integrated Child Care) is a preventive health and nutrition programme of the Ministry of Health, assisted by BASICS (Basic Support for Institutionalizing Child Survival). It relies primarily on volunteers to mobilize families and communities in growth monitoring and promotion activities for children under 2 years and in 2003 operated in approximately 1800 communities in 42 health areas and had high coverage (92%) (Fielder 2003). The programme largely follows the IMCI approach for the facility‐based component but with an added growth‐promotion community‐based component. BASICS has helped develop an AIN implementation guide and curriculum for Ministry of Health personnel, a practice‐oriented curriculum and manual for community volunteers, and counselling cards with specific feeding messages. In the mid‐term evaluation, improvements in child‐care knowledge, attitudes and practices were documented (van Roekel et al. 2002), and evaluation studies of impact on child health are in progress. This is regarded as a model programme and is being replicated in other Latin American countries and in sub‐Saharan Africa.
Table 13 collates the information regarding 12 of the growth‐monitoring studies mentioned above.
Table 13.
Summary of the impact of growth‐monitoring interventions
| Study country | Provider | Location | Contact time (min) | Intended frequency | Understanding of chart | PHC available | Benefit of programme | Benefit of chart |
|---|---|---|---|---|---|---|---|---|
| Imesi (Cunningham 1978; Gwatkin et al. 1980) Nigeria | Nurse/Midwife | Clinic | 5 | Monthly | Good | Yes | 1–4 year MR ↓ MN↓ | ? |
| Hanover (Alderman et al. 1978) Jamaica | Community health aides | Home | NR | Weekly if underweight | Good | Partial | 1–48mMR ↓ MN ↓ | Highly likely |
| Narangwal India (Kielmann et al. 1978) | Paramedics | Home | 5–7 | Weekly | NR | In some villages | Infant MR ↓ 1–3 year MR↓ | ? |
| Thailand (Viravaidhya et al. 1981) | VHVs | Central site | NR | Monthly | NR | No | MN ↓ | ? |
| Iringa (UNICEF 1993) Tanzania | VHWs | Home/health day | NR | Monthly | Good | Yes | MN ↓ | ? |
| TINP (Shekar 1991) India | CNWs | Nutrition centre | NR | Monthly | Good | Yes | MN ↓ | ? |
| BRAC (Karim et al. 1994) Bangladesh | HWs + volunteers | Central site | 7 | Monthly | Modest | Partial | No | ? |
| Tamil NaduIndia India (George et al. 1993) | VHWs | Home | 30 | Twice monthly | Good | Yes | MN ↓ | No |
| Ceara Brazil (de Souza et al. 1999) | CHWs | Home | NR | Monthly | NR | Yes | Inadequate weight gain ↓ | ? |
| ICDS India (Gopaldas et al. 1990; Avsm et al. 1995) | VHWs | Central site | NR | Monthly | Poor | Yes | No | ? |
| Madagascar Senegal (Marek et al. 1999) | CNWs | Central site | NR | Monthly | NR | NR | MN↓ | ? |
| BINP (Hossain et al. 2005) Bangladesh | CNWs | Nutrition centre | NR | Monthly | Poor | No | No | ? |
PHC, primary health care; MR, mortality rate; MN, malnutrition; NR, not reported; VHW, village health worker; VHV, village health volunteer; CHW, community health worker; CNW, community nutrition worker.
In summary, there is evidence from small‐scale studies in Nigeria, Jamaica, India (Narangwal and Jamkhed), and from large programmes in Tanzania (Iringa), India (TINP), Madagascar and Senegal that children whose growth is monitored and whose mothers receive nutrition and health education and have access to basic health care have a better nutritional status and/or survival than children who do not. There is tentative evidence from a large‐scale programme in Brazil (Ceara) that participation in growth monitoring confers a significant benefit on nutritional status independent of immunization and socio‐economic status. There is evidence from India (ICDS) and Bangladesh (BRAC and BINP) that growth monitoring has little or no effect on nutritional status in large‐scale programmes with weak nutrition counselling. There is evidence from Tamil Nadu in a randomized trial that when mothers are visited fortnightly at home and have unhurried counselling, no additional benefit accrues from the visual depiction of growth on a chart. In the Cochrane Systematic Review of growth monitoring in relation to preventing death, morbidity or malnutrition, only the last mentioned study met the inclusion criterion of randomized or quasi‐randomized studies (Panpanich & Garner 1999; Garner et al. 2000).
5.2 Utilization of primary health services
Studies were sought for evidence that growth monitoring can improve utilization of health services (Hypothesis 2) and young children with improved health service utilization have better nutritional status and/or survival (Hypothesis 3).
Hypothesis 2: First, studies were examined for evidence that growth monitoring can improve utilization of health services. Little robust evidence was located regarding growth monitoring per se, but the hypothesis is plausible. Greater maternal awareness of child health problems and increased frequency of contact with health staff as a result of engaging in growth monitoring can be expected to increase the utilization of preventive and curative primary health services, although this may not be true if, for example, utilization involves user fees, or families lack confidence in the health system (Victora et al. 2003, 2004).
In Bangladesh, participants in the BRAC growth monitoring programme had higher rates of immunization, oral rehydration solutions (ORS) and vitamin A supplementation than non‐participants (Karim et al. 1994). For immunization it was 56% and 42% for participants and non‐participants, respectively, for ORS it was 38% and 28% and for vitamin A it was 64% and 54% respectively. These differences in uptake are quite modest. In India, uptake in ICDS blocks was also modest. For vitamin A it was 35% and for iron and folate it was 16%, compared with 20% and 17% respectively in non‐ICDS blocks (Avsm et al. 1995). More impressive uptakes were found in Nigeria (Cunningham 1978), India (Chaudhuri 1988) and Haiti (Genece & Rohde 1988) (Table 4). Easier access is likely to increase health service utilization and communities with village‐based growth monitoring are reported to demand immunizations, ORS, deworming, contraceptive resupply, vitamin A and simple curative care, thus bringing health services out of the clinic into the community (Rohde & Northrup 1988).
In Casamance, rural Senegal, growth monitoring and promotion sessions within a highly available, smoothly functioning health system were regarded as an important incentive for mothers to bring their young children to the dispensaries. The sessions were used to detect and treat illnesses, deliver nutrition and health education, and distribute chloroquine. Average coverage of growth monitoring was ∼90% for children aged 3–24 months, and average attendance at the monthly sessions was 71% (Pinchinat et al. 2004). Over a 30‐year period of growth monitoring there was a substantial decline in under‐5 mortality (from 312 to 127 per 1000) and a reported decrease in severe malnutrition, although there was no change in mean weight‐for‐age. These data are suggestive of a benefit of growth monitoring in terms of improved utilization of health services, but comparative data from dispensaries with no growth monitoring would be needed for a robust conclusion.
Hypothesis 3: Evidence that young children with improved health service utilization have better nutritional status and/or survival was not rigorously sought as this is generally accepted as true if the health sector delivers effective child survival interventions such as oral rehydration therapy, breastfeeding and complementary feeding (Bryce et al. 2003; Jones et al. 2003). Two examples are given below as illustration. In India, in a randomized effectiveness trial of an educational intervention to improve infant and young child feeding delivered through routine health service contacts, children in the intervention communities had better linear growth than controls and the number of caregiver contacts with nutrition counselling channels was significantly related to improved breastfeeding and complementary feeding practices and to energy intake (2003, 2004, 2005). The main counselling channels were anganwadi workers at home visits and at growth‐monitoring sessions, and auxiliary nurse midwives at immunization sessions. In the intervention communities, the percentage of caregivers reported as receiving nutrition counselling from any channel at 3, 6 and 9 months post‐partum was 62%, 53% and 70% respectively compared with 2%, 1% and 1% in the control communities. In the Narangwal nutrition study, duration of illness episodes and infant mortality were inversely related to the number of service contacts (Kielmann et al. 1978). These and other studies support Hypothesis 3, namely that young children with improved health service utilization have better nutritional status and survival.
In summary, there is some supportive evidence from a number of countries to suggest that growth monitoring can improve utilization of health services (Hypothesis 2). It is also generally accepted that young children with improved health service utilization have better nutritional status and survival.
6. Quality of implementation
There are five main activities linked to growth monitoring and growth promotion: (1) weighing accurately; (2) plotting on a growth chart; (3) interpreting the growth curve; (4) discussing options with the caregiver and agreeing on future action; and (5) evaluating the child's response. Even though simple in concept, difficulties abound. Only 35 of 178 countries (20%) contacted in 1998–2000 reported having no problems with the use of growth charts (de Onis et al. 2004), which is similar to the proportion (22%) in 1978 among health personnel contacted in 50 countries (O'Brien 1978).
In 1985 at the request of WHO, Gopalan & Chatterjee (1985) reviewed global experience in the utilization of growth charts for promoting child nutrition, including experience from large‐scale programmes in India, Indonesia and the Philippines. They concluded that growth data were often inaccurate due to deficiencies in the technical aspects of weighing and charting, but the greatest difficulties lay in interpreting growth charts and in initiating appropriate action. Little time was available for teaching mothers, and growth monitoring programmes were often conducted in isolation, instead of being part of an integrated package of other low‐cost health and nutrition interventions. They warned that growth monitoring will be wholly futile in situations where the basic infrastructure for remedial or promotive measures is non‐existent or inadequate, and that over‐enthusiastic promotion of growth monitoring could result in a backlash of disillusionment. Nabarro & Chinnock (1988) provided further analysis of problems encountered and they too questioned the appropriateness of promoting growth monitoring if infrastructural inadequacies constrain effective action. They concluded that effective growth‐monitoring activities are not easily implemented and that local realities are often not considered when making decisions about inclusion of growth monitoring in national programmes. Likewise Gerein & Ross (1991) concluded that the introduction of growth monitoring into under‐resourced and poorly managed health systems is likely to be a costly and relatively fruitless exercise.
The problems identified by Gopalan and Chaterjee appear pervasive and enduring. In Papua New Guinea none of the key activities was performed adequately: 21% of children were misdiagnosed and interaction with mothers was rare (Cape 1988). Low coverage and limited counselling were reported in large‐scale growth monitoring programmes in India (Gopaldas et al. 1990) and in programmes supported by UNICEF in China, Ecuador, Indonesia, Malawi, Thailand, Zaire and Zambia (Pearson 1995). In Burkina Faso, Niger and Mozambique fewer than 30% of mothers were counselled (Jelley & Madeley 1983; Hampshire et al. 2004). In Costa Rica, lack of essential supplies and an unsupportive health system were said to demotivate community health workers leading to unsatisfactory growth‐monitoring practices (Valadez et al. 1995).
The limited time available for interaction with caregivers continues to constrain effective action in many countries: in growth‐monitoring clinics in Lusaka, Zambia, the mean contact time was 30 s (Msefula 1993), and in three child health programmes in rural Zaire, 64% of mothers attending growth‐monitoring sessions received <2 min consultation time, and 43% received no advice at all (Gerein & Ross 1991). Health workers were reasonably good at weighing and charting, but lacked nutrition knowledge and communication skills, with the result that advice, if given, comprised brief, standardized directives. Constant repetition of the same message, such as ‘feed the child more greens’ understandably exasperated some mothers (Cape 1988; Gerein & Ross 1991). Cowan (1988), working in Ludhiana, reported that 10–15 min is needed for a meaningful contact with mothers and to elicit the needs and problems of the family.
There appears to be a widespread lack of recognition at all levels of the health system of the importance of giving feedback to caregivers and for interactive communication (Hendrata & Rohde 1988). It is not just a shortcoming of community‐level health workers, but also of their supervisors and managers. A study of perceptions of growth monitoring and promotion among 19 District Medical Officers from 17 countries in South America, Africa and Asia revealed a very restrictive interpretation of the concept of growth monitoring and a disregard for involving caregivers in decision making (Roberfroid et al. 2005). Clearly there is a need to re‐orientate senior managers and others who have responsibility for implementing growth monitoring programmes about the centrality of the communication process in growth promotion and the need to improve communication skills of health workers.
Inadequate training of health workers, especially in equipping and enabling them to provide effective counselling, contributes to poor quality of implementation. Among the studies reviewed in Section 5.1, there is a notable difference in the training of health workers. Little time was spent training in the poorly performing programmes – 3 days in BRAC (Karim et al. 1994) and no growth‐monitoring training for anganwadi workers in some projects in ICDS (Kapil et al. 1996). In contrast, those with good outcomes spent a considerable time training and supervising their health workers. In Jamaica (Alderman et al. 1978) and Tamil Nadu (George et al. 1993), where intensive nutrition counselling was associated with improved nutritional status, health workers were trained for 8 weeks and supervisory visits were frequent. Training and supervision were also emphasized in the projects in Nigeria (Cunningham 1978) and Narangwal (Kielmann et al. 1978). In Madagascar and Senegal (Marek et al. 1999), performance was closely supervised: the indicators used were: (1) percentage of cohort children weighed monthly; (2) percentage of cohort caregivers attending weekly education sessions; and (3) percentage of cohort children who are malnourished. In Senegal, if performance targets were not met, the supervisor was dismissed after a warning period.
Ideally, the counselling should address the specific needs of each mother and her child, which is impossible if health workers lack the necessary knowledge, skills and insight to analyse the situation and deduce appropriate action. In a survey of training courses in Lusaka, weighing, plotting and interpreting the growth curve were adequately taught, but none taught counselling or follow‐up action (Msefula 1993). Too often there is insufficient investment in nutrition training. In the IMCI training, the nutrition component is sometimes reduced or not attempted because of time constraints, and so IMCI clinic staff may not be equipped for growth promotion.
7. Caregivers' knowledge and understanding of growth charts
A basic premise of growth charts is that it makes growth faltering visible to caregivers and is an educational tool. Thus caregivers must be able to interpret growth charts and understand their use. Although there are reports of good comprehension by mothers, including those who are illiterate (Wray 1978; Griffiths 1981; Arole 1988; George et al. 1993; Karim et al. 1994), some have questioned mothers' ability to comprehend their meaning or purpose (Rawlinson 1977; Forsyth 1983; Gopaldas et al. 1990; Owusu & Lartey 1992).
To test whether growth charts increase the impact of nutrition education on maternal learning, mothers attending each of nine health centres in Lesotho were sequentially assigned to one of three groups: either to one of two types of growth chart (n = 756) or to no charts (n = 268) (Ruel & Habicht 1992). The programme offered was similar in all other respects, that is, monthly growth monitoring, individual counselling and group education. Maternal knowledge about complementary feeding and diarrhoea management was tested at baseline and 4 months later. There was a 76% response rate as not all enrolled mothers were tested. Large improvements in knowledge were found, but the group with growth charts scored only slightly higher overall than those without (77% and 75% respectively). The differences were significant for mothers with underweight children (P < 0.02) regarding knowledge of diarrhoea management. The authors conclude that mothers of well‐nourished children learn equally well, with or without growth charts, but that mothers of underweight children learn better when they are taught with growth charts.
8. Empowerment and community mobilization
It is envisaged that growth monitoring can be a stimulus that will lead to collaborative involvement of the family and the community to improve health and well‐being. Williams (1986) has pointed to the similarity between current growth monitoring and promotion activities in developing countries and those in England in the early years of the Infant Welfare Movement, and to an empowering and mobilizing role of regular weighing and advice. In England, maternity benefit legislation in 1913 was spearheaded by the Women's Cooperative Guild, which was closely allied with health workers and community volunteers involved in growth monitoring and promotion. The Guild had the slogan ‘Save the Babies’ and also influenced the enactment of the Maternal and Child Welfare Act of 1918, and successfully advocated for the establishment of a Ministry of Health.
In the outreach programme of the Child in Need Institute, Calcutta, transfer of growth monitoring to communities enabled more frequent participation by all mothers and empowered women's groups (mahila mandals) to take a more central and deciding role in health and nutrition activities. This resulted in a demand for improved water supplies, child‐care activities, home gardens, poultry raising and income generation (Chaudhuri 1988). Where growth‐monitoring programmes are community‐based, villagers are reported to demand better health‐care services locally, rather than their being entirely facility‐based (Victora et al. 2004).
High‐quality village‐based delivery, however, is difficult to achieve at scale. This was the case in the Indonesian Family Nutrition Improvement Programme, which was a national intersectoral GOBI intervention focusing on nutrition education through growth monitoring, delivered by volunteer village women (kaders). Weaknesses in training (too brief and not practice‐oriented) meant that kaders had neither the knowledge nor skills to communicate effectively with caregivers. Better selection of kaders, with more emphasis on their potential as agents of community motivation and behaviour change, and better training with more role‐plays and active participation, were recommended (Hill et al. 1983).
In Zimbabwe in 1981, grass root village committees helped implement a nutrition programme whereby underweight children (screened by mid‐upper arm circumference) were fed a daily high‐energy meal of maize, beans, groundnuts and oil, cooked by mothers at over 2000 community feeding points. Through community discussions it was agreed that communal farming plots should be established to sustain the nutrition programme and this was achieved with technical support from agricultural extension officers. By the late 1980s there were ∼3000 food plots nationwide. Many of the feeding points developed into comprehensive health centres, which provided immunization, health education, growth monitoring, oral rehydration therapy and treatment for malaria and pneumonia. Between 1980 and 1988 the infant mortality rate halved (from 110 to 53 per 1000) and the percentage of children severely underweight fell from 18% to 1% (Werner & Sanders 1997). Although the impact of growth monitoring per se cannot be deduced, this example does illustrate how a community‐based participatory programme grew from a single activity into a large intersectoral programme that encompassed health and agriculture and provided preferential benefits to those in greatest need. Community‐based growth monitoring has also been the entry point for agricultural and income‐generating projects in South Africa (Faber et al. 2003), Haiti (Genece & Rohde 1988), India (Arole 1988) and Vietnam (Wollinka et al. 1997). In Narangwal, communities involved in growth monitoring provided food for the child‐feeding centres and gave donations of food to the landless at harvest time (Kielmann et al. 1983).
‘Hearth’ programmes often operate in conjunction with growth monitoring. The concept of positive deviance is used to identify feeding, caregiving and health‐seeking practices associated with good child growth, and the process is considered to provide social support and motivation, and build self‐efficacy (Wollinka et al. 1997). Growth monitoring is used to identify malnourished children and positive‐deviant families, and to motivate caregivers to sustain improved feeding behaviours. Caregivers of malnourished children then gather in small groups to feed positive‐deviant foods each day for 2 weeks. This approach was tested in a randomized trial in 12 rural communes in north Vietnam (Dickey et al. 2002; Schroeder et al. 2002). Intervened children aged 5–25 months (mean age 15 months) had better dietary intakes but did not show significantly better growth than controls, although there was a transient benefit in a small subsample of moderately underweight children aged <15 months. Attendance rates (50%) and message delivery (20%) were lower than expected.
9. Coverage and attendance
Experience shows that many mothers fail to attend regularly if weighing necessitates a lengthy visit to a clinic, especially if attendance entails economic losses, either as opportunity costs or transport costs, or if attendance results in neglect of other family responsibilities (Scrimshaw 1974; Zachariah et al. 1980; Jelley & Madeley 1983; Gopaldas et al. 1990). Those most at risk of malnutrition tend to attend least often (Jelley & Madeley 1983; Chopra & Sanders 1997). In Zaire, mothers waited 2–6 h for their children to be weighed, and for themselves to attend a 10 min group education session, and have a perfunctory consultation (Gerein & Ross 1991). ‘Lines of flow’ at Imesi clinic facilitated a quick throughput and high coverage, but in Indonesia, although flow was rapid the advice proffered was brief and ineffectual. Mobile clinics have been tried but are costly (Kimmance 1970). In the large‐scale UNICEF programmes reviewed by Pearson (1995) and the large‐scale ICDS (Avsm et al. 1995) and BRAC (Karim et al. 1994) programmes in India and Bangladesh, low coverage and attendance were seen as major weaknesses. Home visits and community‐based growth monitoring can improve coverage but any practical benefit depends on the correct interpretation of the growth chart, the appropriateness of any advice given, the motivation and resources of mothers to take action, and the availability of oral rehydration salts, drugs, vaccines etc. In Senegal, attendance was much higher where growth monitoring was provided by NGOs than at government facilities (72% of children attended monthly vs. 35%) ‘because they were welcomed properly’ (Marek et al. 1999). In South Africa, where growth monitoring is part of the Integrated Nutrition Programme, community‐based delivery achieved 90% coverage and 64% of infants had at least five weighings in the first year (Faber et al. 2003). Caregivers enjoyed having their children weighed at the home‐based growth‐monitoring points, were pleased that they understood the link between growth and health, and felt empowered. They were unhappy with growth monitoring from the mobile clinic as staff were perceived as ‘hostile and unhelpful’ and failed to explain the purpose of growth monitoring. Caregivers will not participate if they are disrespected or receive poor services.
How to scale up effective interventions and achieve high coverage especially among the poor is a difficulty faced for all preventive interventions in child health (Gwatkin et al. 2004). Clearly the quality of the service and its proximity are important, but the perceived benefit and hence demand for health services are also factors. Medications are more valued than preventive services such as nutrition counselling. Several Latin American countries have attempted to boost demand through direct cash transfers to poor families on condition that they use specific preventive health‐care interventions such as immunization and growth monitoring. One such programme operates in Honduras through an Inter‐American Development Bank loan. In a randomized controlled trial, conditional payments were made to families and coverage of growth monitoring increased significantly by 15–21 percentage points compared with control municipalities, and immunization started in a more timely fashion (Morris et al. 2004a). Improved coverage, however, was not accompanied by reductions in the prevalence of wasting or stunting (S. Morris, personal communication). In municipalities that were randomized to receive a cash injection to strengthen health centre services including a community‐based growth‐monitoring programme (AIN‐C), coverage did not increase significantly (Morris et al. 2004a). Only partial implementation of the service package, however, was achieved, which could have limited its effectiveness. In Brazil, conditional cash transfers were associated with slightly improved growth‐monitoring attendance, with 3.8 visits during a 6‐month period compared with 3.4 visits for non‐beneficiaries (P < 0.027) (Morris et al. 2004b), but again there was no accompanying improvement in growth. In Mexico, where cash transfers were larger than in Honduras and multimicronutrient supplements were also provided and beneficiaries were suspended if they did not attend, increased coverage of growth monitoring was accompanied by improved growth and fewer illness episodes (Behrman & Hoddinott 2002).
10. Potential consequences if withdrawn
If growth monitoring were withdrawn, health workers and mothers would lose:
-
•
a point of reference as to whether a child's weight is following the expected trajectory;
-
•
an early warning of a health or nutrition problem;
-
•
a visible portrayal of a health or nutrition problem; and
-
•
a visible response to corrective actions.
They might also lose:
-
•
frequent, regular contact;
-
•
the opportunity to intervene before a child's condition deteriorates;
-
•
a focal point for integrating synergistic interventions;
-
•
an entry point for timely discussion about child feeding, tailored to individual needs;
-
•
an entry point for other preventive and curative services;
-
•
satisfaction and motivation from seeing tangible responses to corrective actions; and
-
•
an advocacy tool for community mobilization to address underlying causes of poor health.
Governments and communities may also lose the conduit and driving force for delivering a package of community‐based nutrition, health and poverty‐reduction interventions. The issue is whether better delivery of key interventions (e.g. interventions to improve breastfeeding and complementary feeding) and maintaining regular contact (e.g. with home visits from community health workers) might lead to improved behaviours without recourse to growth monitoring as was found in Tamil Nadu (George et al. 1993), or whether growth monitoring might assist health staff and programmes to function more effectively.
11. Feasibility and conditions under which growth monitoring and promotion can be expected to work
Growth monitoring is clearly a waste of time and money if it is not linked with actions that promote good growth. As poor growth is often linked with poor infant feeding practices, an important action is nutrition counselling. This was perfunctory and of poor quality in all poorly performing programmes examined for this review. Health workers lack adequate knowledge and communication skills. Poor performance stems in part from inadequate training: lack of supervision adds to the problem. In some situations a weak infrastructure further constrains the actions that can be taken. These problems are compounded, however, by the conceptual confusion surrounding growth monitoring in primary care settings (Chopra & Sanders 1997), with the result that its purpose is diversified. Thus growth monitoring was used for community mobilization in Iringa (Tanzania), for targeting supplementary feeding in Tamil Nadu (TINP, India), for targeting and guiding nutrition education in the Dominican Republic, and for no apparent purpose in Colombian day‐care centres (Pelletier & Shrimpton 1994). This conceptual confusion may be exacerbated if growth charts become a child rights' instrument. Possession of a growth chart with a minimum of five recorded weights in the first year has been adopted by some governments as showing their commitment to the right of a child to have the highest attainable standard of health. The risk is that setting numerical targets may further divert attention from the growth chart as an educational tool for promoting healthy growth.
The conditions that favour good growth monitoring and growth promotion include:
-
•
well organized, functioning health system;
-
•
clear objectives as to the purpose of growth monitoring;
-
•
integration of growth monitoring with preventive/curative health services and intersectoral linkages;
-
•
integration of nutrition education into all paediatric services;
-
•
high coverage of children at risk; high degree of implementation;
-
•
trained health workers with good communication skills and knowledge;
-
•
adequate time allowed for nutrition counselling;
-
•
experiential and observational learning techniques to promote behavioural change;
-
•
regular support and supervision of health workers to maintain good performance over time;
-
•
induction and training of new staff;
-
•
service delivered locally, at convenient times;
-
•
caregivers having good access to attend, or being visited at home; and
-
•
formative research used to develop key messages that are actionable, feasible, memorable and used at all points of contact.
The essential tenets of growth monitoring and promotion are described in The World Bank Nutrition Toolkit.
12. Cost‐effectiveness
Cost‐effectiveness was examined in a growth‐promotion intervention in Trujillo, Peru, that included nutrition education and growth monitoring (Waters et al. 2006). The intervention was facility‐based and used routine health services. Children were followed from birth until 18 months of age and age‐appropriate messages aimed at improving complementary feeding were promoted at immunization clinics, growth‐monitoring sessions and sick‐child contacts. The trial was randomized at the site level and controlled (Penny et al. 2005; 2006, 2007). Children in the intervention areas made 17.6 visits to health facilities during the first 18 months of life compared with 14.1 visits by control children (P < 0.001). The prevalence of stunting in the intervention and control groups was 5% and 16% respectively (P = 0.018). The marginal cost of the intervention, which included costs for training, health education materials, and travel and equipment was US$6.12 per child reached and US$55.16 per case of stunting averted. The estimated marginal cost per death averted was US$1952.
Provision of supplementary food along with growth monitoring for targeting beneficiaries was included in the strategies examined by the WHO Choosing Interventions that are Cost Effective (CHOICE) Team in relation to achieving Millennium Development Goal 4 (Edejer et al. 2005). This strategy was the least cost‐effective of the eight strategies examined because of the high cost of providing ready‐to‐eat food supplements.
Cost analyses have been made of the Honduras Community‐Based Integrated Child Care programme (AIN‐C), which relies primarily on volunteer monitoras to mobilize families and communities in growth monitoring and promotion activities for children under 2 years (Karim et al. 2003). The average time spent per monitor per month was: monthly weighing sessions 4.5 h, monthly home visits 5 h, curative care visits 1.5 h, community meetings 0.4 h and health centre meetings 3.5 h. Annual recurrent costs per child were apportioned as personnel 51%, medicines 27%, per diems 16%, materials and supplies 3%, transportation 3%. The average annual recurrent cost per participating child was US$6.82, comprising $5.41 for the preventive component and $1.41 for curative care. If fixed costs are subtracted (i.e. costs that would need to be paid even if there were no programme), the annual incremental cost per participating child is reduced to US$4.00.
13. Potential adverse consequences
Few adverse consequences of growth monitoring and promotion have been reported, but when implemented poorly it is a waste of limited resources. Also, for caregivers, transport and opportunity costs may be considerable if growth monitoring is performed at a health facility far from their home. If caregivers feel their time is being wasted they may be discouraged from participating in other health‐care activities (Nabarro & Chinnock 1988).
In Pelotas, Brazil, where there was considerable involvement of mothers in growth monitoring, the visual representation of their child's growth led some mothers to become rather obsessed by their child's position on the chart and they strove to move it higher, even though it was in the normal range (Behague 1993). As a consequence, some mothers were reported to move away from exclusive breastfeeding to less desirable practices.
14. Policy considerations and recommendations
Malnutrition contributes to 50–60% of all deaths among children under 5 years so child mortality cannot be reduced or Millennium Development Goal 4 reached without addressing the problem of malnutrition. Prevention of malnutrition is imperative, and thus growth‐promotion activities are essential. Growth monitoring and promotion programmes have the potential to achieve improved breastfeeding and complementary feeding, which are two of the main child survival interventions, but this potential remains unfulfilled in many growth monitoring and promotion programmes.
Table 14 summarizes three recently published randomized controlled trials of different approaches to delivering nutrition counselling. The trial in Brazil (Santos et al. 2001) used IMCI medical consultations and these tended to be few (mean < 2) during the 6‐month study period, thus exposure to improved counselling in the intervention group was limited. Children were stunted rather than wasted but no significant improvement was found in linear growth during infancy. The trials in India (2003, 2004, 2005) and Peru (Penny et al. 2005; 2006, 2007) were birth cohorts followed to age 18 months. They too used routine health services but included multiple channels, including growth monitoring and promotion. In Peru, caregiver exposure and caregiver recall of key messages were significantly related to improved feeding behaviours. Caregivers were also counselled about providing psychosocial stimulation for their children, and they practised this at group growth‐monitoring sessions. Both trials achieved significant improvements in feeding practices and in linear growth. Frequent, regular exposure to uniform age‐appropriate messages appears to be important for behaviour change: growth‐monitoring contacts provide a mechanism for such exposure, as does regular home visiting. On the other hand, the IMCI approach of emphasizing nutrition counselling at sick‐child contacts may provide insufficient exposure, and it may be more difficult to reverse detrimental feeding behaviours once they have occurred than it is to adopt beneficial behaviours from the outset. Also coverage may be low as only some children will attend for curative care.
Table 14.
Three recent randomized controlled trials (RCTs) of nutrition education
| Study | Age group (months) | Intervention delivery channel | Intervention | Difference compared with controls |
|---|---|---|---|---|
| Brazil (Santos et al. 2001) RCT n = 28 health centres | First 12–13 patients <18 months visiting 33 doctors, followed for 6 months (n = 424) | Government health centres (service delivered by doctors) 20 h training on nutrition counselling | • 5 age‐appropriate feeding messages | No significant difference in length gain or % stunted or energy intake from CF Significant differences in: ↑ Recommended foods ↑ Weight gain, WAZ gain, and WLZ gain if enrolled at 12–17 months |
| India (2003, 2004, 2005) RCT n = 8 communities | Birth cohort followed to 18 months (n = 1115) Average BW 2.7 kg | Multiple contacts by: anganwadi workers – at home monthly – GMP Auxiliary midwife at immunization clinic 3‐day training (IMCI) | • 9 age‐appropriate feeding messages • Hand washing • Community activities to promote good CF | No significant differences in % stunted or weight gain Significant differences in: ↑ % EBF at 3 months ↓ Diarrhoea at 3 months and 6 months ↑ Length gain 6–12 months (equivalent to 0.18 SD) ↑ Energy intake from CF ↑ Recommended foods |
| Peru (Penny et al. 2005; 2006, 2007) RCT n = 12 health posts/centres, community hospitals | Birth cohort followed to 18 months (n = 377) Average BW 3.4 kg | Government health facilities – immunization clinic – GMP (minimum target 5 per year) – sick‐child contacts Training + follow‐up visits. Accreditation scheme | • 3 age‐appropriate feeding messages • Food preparation practice • Recipe fliers • GMP one‐to‐one discussion • Group GMP and child development activities | Significant differences in: ↑ WAZ, ↑ LAZ ↑ Length gain (on average 1 cm taller and 199 g heavier at 18 months) ↓ % stunted (5% vs. 16%) ↑ Energy intake from CF ↑ Recommended foods |
IMCI, Integrated Management of Childhood Illness; CF, complementary foods; EBF, exclusive breastfeeding; BW, birthweight; GMP, growth monitoring and promotion; WAZ, mean weight‐for‐age z‐score; WLZ, weight‐for‐length z‐score; LAZ, mean length‐for‐age z‐score.
There is no unequivocal evidence that growth monitoring is beneficial per se, but it was perceived to be beneficial by the authors of several of the studies described in this review, and was an integral part of programmes that were associated with significant reductions in malnutrition and mortality. Nevertheless, there is evidence from the randomized controlled trial in Tamil Nadu that significant reductions in malnutrition can be achieved through intensive health and nutrition education and basic health care without growth monitoring. Good nutrition counselling is paramount for growth promotion and is often performed badly. Effort must be made to improve this, irrespective of growth monitoring. Timely support is also important in achieving exclusive breastfeeding and appropriate complementary feeding.
Key messages:
-
•
To be effective in reducing child malnutrition and mortality, growth monitoring must be accompanied by community‐based health and nutrition interventions
-
•
Growth monitoring and promotion programmes should prioritise infants and children aged 0–18 m and utilise all child health contacts for nutrition counselling
-
•
Training, supervision and support for health workers must be improved if they are to be effective counsellors in growth promotion programmes
-
•
Impact is dependent on coverage, intensity of contact, health worker performance, and adequacy of resources.
When considering growth monitoring programmes, three operational questions include: (1) what age group should be included; (2) how frequently should children attend; and (3) should all children be monitored or just the most vulnerable?
Age group to be monitored: Recent data from 39 nationally representative surveys in developing countries indicate that mean weight falters between 3 and 15 months and length between 0 and 21 months of age. Thereafter mean weight and length increments follow international norms (Shrimpton et al. 2001). In Brazil, anthropometric status at 11 months of age was a very strong predictor of a child's status at 2 and 4 years (Huttly et al. 1991). Morbidity affects nutritional status largely in the first year, and poor feeding practices prevail until around 18 months of age. Focusing growth‐monitoring efforts on the first 12–18 months of life would thus seem appropriate. Growth monitoring could be stopped at 12 months for children with ≤1 episodes of faltering in the first year. The time gained by not monitoring older children could then be used to provide better nutrition‐counselling services.
Frequency of measurements: The recommended interval is monthly, which enables early identification of faltering, but growth can occur in spurts and sporadic faltering is normal (Martorell & Shekar 1994) so criteria for faltering need to be carefully defined to minimize false positives. Local circumstances and resources are best taken into account when determining the frequency of monitoring (Habicht & Pelletier 1990). If growth monitoring is combined with other services such as immunization, then the burden on caregivers is reduced and regular attendance may become more feasible. Sufficient staff and time, however, need to be provided at combined sessions to permit adequate counselling.
Targeted or universal monitoring: Henry and colleagues proposed that targeting children in the lower portion of the weight distribution at 6 months could be used to identify high‐risk children (Henry et al. 1989). They found that in Bangladesh and St Lucia, weight at 9, 12, 15 and 18 months of age was more highly correlated with weight at 6 months than with the previous 3‐month weight gain. In St Lucia, the correlation coefficient between weight at 6 months and weight at 18 months was 0.79. Most children in the study populations, however, were not exclusively breastfed so there was an opportunity for the consequences of poor feeding or contaminated environments to be manifest by 6 months of age. This would not be so in communities where infants are exclusively breastfed for 6 months, so the age for identifying high‐risk children might need to be later in such communities.
Ross & English (2005) have proposed that routine weighing should be confined to low‐birthweight infants and sick infants presenting at clinic. They came to this conclusion because in their birth cohort of 2210 Kenyan babies, neither attained weight at 6 weeks nor rate of weight gain from birth to 6 weeks, or gain between 6 and 10 weeks was a good predictor of illness episodes or death in the subsequent 4–8 weeks. This targeted pragmatic approach did not perform any better than weighing all children, but it involved 72% fewer weighings so took less staff time. The cohort was not studied beyond 14 weeks of age and nutrition counselling was provided only if staff were available, so the findings cannot be extrapolated to later infancy when faltering may be more likely.
Possible policy options: This review highlights the paucity of rigorous trials to answer the key question as to whether growth monitoring confers any measurable benefit to the children for whom growth charts are kept. Two of the potential strengths of growth monitoring are that it provides frequent contact with health workers and a conduit to child health interventions and action, but this review has shown that weaknesses in programme delivery often restrict these opportunities. Thus growth monitoring has been ineffective where coverage has been low, or health workers have lacked time, knowledge or communication skills, or where infrastructural weaknesses constrained child health services. Growth monitoring may not be the best use of limited resources in countries with weak economies and inadequate health budgets: a limited package of health and nutrition interventions including good nutrition counselling may be preferable, aiming for good coverage and effective health worker performance, and prioritizing infants and children <18 months of age.
Taking into account the evidence from recent nutrition education interventions that used multiple delivery channels within routine health services, possible options to consider for the future are:
-
1
If growth monitoring is not in place, then focus efforts on growth‐promotion activities and consider counselling caregivers intensively at all child health contacts and through home visits by community health workers or volunteers. Where possible chart weights at birth, immunization (6, 10, 14 weeks and 9 months), vitamin A distribution and sick‐child visits. Follow up and counsel any whose growth is faltering and those with a weight‐for‐age <−2 SD.
-
2
Where growth monitoring exists but the coverage is low or there is little potential for improvement, then consider abandoning it and re‐focus efforts on growth promotion activities as in (1).
-
3
Where growth monitoring and promotion programmes currently exist and there is potential for improvement, then maximize their potential, strengthen the nutrition counselling elements, combine growth monitoring with other health intervention channels such as immunization for the convenience of caregivers, and ensure consistent message delivery. Target younger children and monitor weight until 12 months of age. If there are episodes of growth faltering, continue to monitor until 18 months. Where cultural traditions and conditions are favourable, use growth monitoring additionally for community mobilization to address underlying socio‐economic and other causes of poor nutrition and health
Scaling up from successful small‐scale growth monitoring and promotion programmes to effective national programmes will require political commitment, investment, extensive capacity building and strengthening of health systems. Training, supervision and support will need to be improved if health workers are to be equipped with the necessary knowledge and communication skills to promote healthy growth. Impact will be related to coverage, intensity of contact, health worker performance, adequacy of resources, and the ability and motivation of families to follow advice.
Conflicts of interest
The authors have declared no conflicts of interest.
References
- Alderman M.H., Wise P.H., Ferguson R.P., Laverde H.T. & D'Souza A.J. (1978) Reduction of young child malnutrition and mortality in rural Jamaica. Journal of Tropical Pediatrics 24, 7–11. [DOI] [PubMed] [Google Scholar]
- Arole M. (1988) A comprehensive approach to community welfare: growth monitoring and the role of women in Jamkhed, Indian Journal of Pediatrics 55 (Suppl.), S100–S105. [DOI] [PubMed] [Google Scholar]
- Avsm Y.S., Gandhi N., Tandon B.N. & Krsihnamurthy KS. (1995) Integrated Child Development Services Scheme and nutritional status of Indian children. Journal of Tropical Pediatrics 41, 123–128. [DOI] [PubMed] [Google Scholar]
- Behague D. (1993) Growth monitoring and the promotion of breastfeeding. Social Science and Medicine 37, 1565–1578. [DOI] [PubMed] [Google Scholar]
- Behrman J.R. & Hoddinott J. (2002) Program evaluation with unobserved heterogeneity and selective implementation: the Mexican PROGRESA impact on child nutrition. PIER Working Paper 02‐006. University of Pennsylvania, Philadelphia, PA. [Google Scholar]
- Bentley M.E., Stoltzfus R.J. & Caulfield L.E. (1993) Growth monitoring (Letter). Lancet 342, 749. [PubMed] [Google Scholar]
- Bhandari N., Bahl R., Mazumder S., Martines J., Black R.E., Bahn M.K. et al (2003) Effect of community based promotion of exclusive breast feeding on diarrhea illnesses and growth – a cluster randomized controlled trial. Lancet 361, 1418–1423. [DOI] [PubMed] [Google Scholar]
- Bhandari N., Mazumder S., Bahl R., Martines J., Black R.E., Bahn M.K. et al (2004) An educational intervention to promote appropriate complementary feeding improves child feeding practices and physical growth in infants and young children in rural Haryana, India. Journal of Nutrition 134, 2342–2348. [DOI] [PubMed] [Google Scholar]
- Bhandari N., Mazumder S., Bahl R., Martines J., Black R.E. & Bhan M.K. (2005) Use of multiple opportunities for improving feeding practices in under‐twos within child health programmes. Health Policy Plan 20, 328–336. [DOI] [PubMed] [Google Scholar]
- Bryce J., El Arifeen S., Pariyo G., Lanata C.F., Gwatkin D., Habicht J.‐P. & The Multi‐Country Evaluation of IMCI Study Group (2003) Reducing child mortality: can public health deliver? Lancet 362, 159–164. [DOI] [PubMed] [Google Scholar]
- Bryce J., Victora C.G., Habicht J.‐P., Black R.E. & Scherpbier R.W. (2005) Programmatic pathways to child survival: results of a multi‐country evaluation of Integrated Management of Childhood Illness. Health Policy Plan 20 (Suppl.S1), i5–i17. [DOI] [PubMed] [Google Scholar]
- Cape N. (1988) Growth charts: help or hindrance? Health Policy Plan 3, 167–170. [Google Scholar]
- Chaudhuri S.N. (1988) Growth monitoring in the evolution of clinic based health care through a community based action program. Indian Journal of Pediatrics 55 (Suppl.), S84–S87. [DOI] [PubMed] [Google Scholar]
- Chopra M. & Sanders D. (1997) Growth monitoring – is it a task worth doing in South Africa? South African Medical Journal 87, 875–878. [PubMed] [Google Scholar]
- Cowan B. (1988) Growth monitoring as a critical means to provide primary health care. Indian Journal of Pediatrics 55 (Suppl.), S74–S77. [DOI] [PubMed] [Google Scholar]
- Cunningham N. (1978) The under fives clinic – what difference does it make? Journal of Tropical Pediatrics 24, 237–334. [PubMed] [Google Scholar]
- Cuthbertson W.F.J. & Morley D. (1962) A health and weight chart for children from birth to five. West Africa Medical Journal 11, 237–240. [PubMed] [Google Scholar]
- Dickey V.C., Pachón H., Marsh D.R., Lang T.T., Claussenius D.R., Dearden K.A. et al (2002) Implementation of nutrition education and rehabilitation programs (NERPs) in Viet Nam. Food and Nutrition Bulletin (23 (4 Suppl.), 75–82. [PubMed] [Google Scholar]
- Edejer T‐T., Aikins M., Black R., Wolfson L., Hutubessy R. & Evans D.B. (2005) Cost effectiveness analysis of strategies for child health in developing countries. British Medical Journal 331, 1177. Epub doi:10.1136/bmj.38652.550278.7C (published November 10). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Editorial (1985) Growth monitoring: intermediate technology or expensive luxury? Lancet 2, 1337–1338. [DOI] [PubMed] [Google Scholar]
- Faber M., Phungula M.A.S., Kvalsvig J.D. & Benadé A.J.S. (2003) Acceptability of community‐based growth monitoring in a rural village in South Africa. Food and Nutrition Bulletin 24, 350–359. [DOI] [PubMed] [Google Scholar]
- Fielder J.L. (2003) A cost analysis of the Honduras Community‐Based Integrated Child Care Program. HNP Discussion Paper. World Bank, Washington, DC. [Google Scholar]
- Forsyth S.J. (1983) Nutrition education: lack of success in teaching Papua New Guinea mothers to distinguish ‘good’ from ‘not good’ weight development charts. Food and Nutrition Bulletin 6, 22–26. [Google Scholar]
- Garner P., Panpanich R. & Logan S. (2000) Is routine growth monitoring effective? A systematic review of trials. Archives of Disease in Childhood 82, 197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Genece E. & Rohde J.E. (1988) Growth monitoring as an entry point for primary health care. Indian Journal of Pediatrics 55 (Suppl.), S78–S83. [DOI] [PubMed] [Google Scholar]
- George S.M., Latham M.C., Abel R., Ethirajan N. & Frongillo E.A. (1993) Evaluation of effectiveness of good growth monitoring in south Indian villages. Lancet 342, 348–352. [DOI] [PubMed] [Google Scholar]
- Gerein N.M. & Ross D.A. (1991) Is growth monitoring worthwhile? An evaluation of its use in three child health programmes in Zaire. Social Science and Medicine 32, 667–675. [DOI] [PubMed] [Google Scholar]
- Gillespie S., McLachlan M. & Shrimpton R. (eds) (2003) Combating Malnutrition: Time to Act. Human Development Network Health, Nutrition, and Population Series. The World Bank: Washington, DC. [Google Scholar]
- Gopalan C. & Chatterjee M. (1985) Use of Growth Charts for Promoting Child Nutrition: A Review of Global Experience. Nutrition Foundation of India: Delhi. (Special publication series no. 2). [Google Scholar]
- Gopaldas T. (1988) Field level health worker's skill in detection of growth retardation and faltering in young children. Indian Journal of Pediatrics 55 (Suppl.), S55–S58. [DOI] [PubMed] [Google Scholar]
- Gopaldas T., Christian P.S., Abbi R.D. & Gujral S. (1990) Does growth monitoring work as it ought to in countries of low literacy? Journal of Tropical Pediatrics 36, 322–327. [DOI] [PubMed] [Google Scholar]
- Government of the United Republic of Tanzania, WHO, UNICEF (1989) The Joint WHO/UNICEF Nutrition Support Programme in Iringa, Tanzania 1983–1988 Evaluation Report. Dar es Salaam. [Google Scholar]
- Grant J.P. (1984) The State of the World's Children 1984. Oxford University Press: New York. [Google Scholar]
- Griffiths M. (1981) Growth Monitoring. American Public Health Association: Washington, DC. (Primary health care issues, series 1, no. 3). [Google Scholar]
- Gwatkin D.R., Wilcox J.R. & Wray J.D. (1980) Can Health and Nutrition Interventions Make a Difference? Overseas Development Council: Washington DC. Monograph no. 13. [Google Scholar]
- Gwatkin D.R., Bhuiya A. & Victora C.G. (2004) Making health systems more equitable. Lancet 364, 1273–1280. [DOI] [PubMed] [Google Scholar]
- Habicht J.P. & Pelletier D.L. (1990) The importance of context in choosing nutritional indicators. Journal of Nutrition 120, 1519–1524. [DOI] [PubMed] [Google Scholar]
- Hampshire R.D., Aguayo V.M., Harouna H., Roley J.A., Tarini A. & Baker S.K. (2004) Delivery of nutrition services in health systems in sub‐Saharan Africa: opportunities in Burkina Faso, Mozambique and Niger. Public Health Nutrition 7, 1047–1053. [DOI] [PubMed] [Google Scholar]
- Hendrata L. & Rohde J.E. (1988) Ten pitfalls of growth monitoring and promotion. Indian Journal of Pediatrics 55 (Suppl.), S9–S15. [DOI] [PubMed] [Google Scholar]
- Henry F., Briend A. & Cooper E. (1989) Targeting nutritional interventions: is there a role for growth monitoring. Health Policy Plan 4, 295–300. [Google Scholar]
- Hill T.M., Florentino R. & D'Agnes L. (1983) The Indonesian National Family Nutrition Improvement Programme (UPGK): analysis of programme experience. Report to UNICEF, Jakarta, Indonesia.
- Hossain S.M.M., Duffield A. & Taylor A. (2005) An evaluation of the impact of a US$60 million nutrition programme in Bangladesh. Health Policy Plan 20, 35–40. [DOI] [PubMed] [Google Scholar]
- Huttly S.R.A., Victora C.G., Barros F.C., Teixeira A.M.B. & Vaughan J.P. (1991) The timing of nutritional status determination: implications for interventions and growth monitoring. European Journal of Clinical Nutrition 45, 85–95. [PubMed] [Google Scholar]
- Jelley D. & Madeley R.J. (1983) Preventive health care for mothers and children. A study in Mozambique. Journal of Tropical Medicine and Hygiene 86, 229–236. [PubMed] [Google Scholar]
- Jones G., Steketee R.W., Black R.E., Bhutta Z.A., Morris S.S. & The Bellagio Child Survival Study Group (2003) How many child deaths can we prevent this year? Lancet 362, 65–71. [DOI] [PubMed] [Google Scholar]
- Kapil U. & Pradhan R. (1999) Integrated Child Development Services Scheme (ICDS) and its impact on nutritional status of children in India and recent initiatives. Indian Journal of Public Health 43, 21–25. [PubMed] [Google Scholar]
- Kapil U., Saxena N., Nayar D. & Gnanasekaran N. (1996) Status of growth monitoring activities in selected ICDS projects of Rajasthan. Indian Pediatrics 33,949–952. [PubMed] [Google Scholar]
- Karim F., Huq N., Brown L. & Chowdhury A.M.R. (1994) Growth monitoring in the context of a primary health care programme. Food and Nutrition Bulletin 15, 192–199. [Google Scholar]
- Karim R., Lamstein S.A., Akhtaruzzaman M., Rahman K.M. & Alam N. (2003) The Bangladesh Integrated Nutrition Project: Endline Evaluation of the Community Based Nutrition Component. Institute of Nutrition and Food Sciences, University of Dhaka, Bangladesh, and the Friedman School of Nutrition Science and Policy, Tufts University, USA.
- Kielmann A.A., Taylor C.E. & Parker R.L. (1978) The Narangwal Nutrition Study: a summary review. American Journal of Clinical Nutrition 31, 2040–2052. [DOI] [PubMed] [Google Scholar]
- Kielmann A.A., Taylor C.E., DeSweemer C., Parker R.L., Chernichovsky D., Reinke W.A. et al (1983) Child and Maternal Health Services in Rural India. The Narangwal Experiment, Vol. 1. Integrated nutrition and health care. Johns Hopkins University Press: Baltimore, MD. [Google Scholar]
- Kimmance K.J. (1970) Evaluation of the work of a mobile outpatient unit in Swaziland. Journal of Tropical Pediatrics 16, 62–67. [DOI] [PubMed] [Google Scholar]
- Lalitha N.V. & Standley J. (1988) Training workers and supervisors in growth monitoring: looking at ICDS. Indian Journal of Pediatrics 55 (Suppl.), S44–S54. [DOI] [PubMed] [Google Scholar]
- Marek T., Diallo I., Ndiaye B. & Rakotosalama J. (1999) Successful contracting of prevention services: fighting malnutrition in Senegal and Madagascar. Health Policy Plan 14, 382–389. [DOI] [PubMed] [Google Scholar]
- Martorell R. & Shekar M. (1994) Growth‐faltering rates in California, Guatemala, and Tamil Nadu: implications for growth‐monitoring programmes. Food and Nutrition Bulletin 15, 185–191. [Google Scholar]
- Melville B., Fidler T., Mehan D., Bernard E. & Mullings J. (1995) Growth monitoring: the role of community health volunteers. Public Health 109, 111–116. [DOI] [PubMed] [Google Scholar]
- Morley D. (1962) A medical service for children under five years of age in West Africa. Transactions of the Royal Society of Tropical Medicine and Hygiene 57, 79–93. [Google Scholar]
- Morris S.S., Flores R., Olinto P. & Medina J.M. (2004a) Monetary incentives in primary health care and effects on use and coverage of preventive health care interventions in rural Honduras: cluster randomised trial. Lancet 364, 2030–2037. [DOI] [PubMed] [Google Scholar]
- Morris S.S., Olinto P., Flores R., Nilson E.A.F. & Figueiró A.C. (2004b) Conditional cash transfers are associated with a small reduction in the rate of weight gain of preschool children in northeast Brazil. Journal of Nutrition 134, 2336–2341. [DOI] [PubMed] [Google Scholar]
- Msefula D. (1993) How can growth monitoring and special care of underweight children be improved in Zambia? Tropical Doctor 23, 107–112. [DOI] [PubMed] [Google Scholar]
- Nabarro D. & Chinnock P. (1988) Growth monitoring – inappropriate promotion of an appropriate technology. Social Science and Medicine 26, 941–948. [DOI] [PubMed] [Google Scholar]
- O'Brien H.B. (1978) Communication of Innovation in Health Care. MSc Thesis. London School of Hygiene & Tropical Medicine: London. [Google Scholar]
- De Onis M., Wijnhoven T.M.A. & Onyango A.W. (2004) Worldwide practices in child growth monitoring. Journal of Pediatrics 144, 461–465. [DOI] [PubMed] [Google Scholar]
- Owusu W.B. & Lartey A. (1992) Growth monitoring: experience from Ghana. Food and Nutrition Bulletin 14, 97–100. [Google Scholar]
- Panpanich R. & Garner P. (1999) Growth monitoring in children. Cochrane Database of Systematic Reviews issue 4, CD001443. doi:10.1002/14651858. [DOI] [PubMed]
- Pearson R. (1995) Thematic Evaluation of UNICEF Support to Growth Monitoring. Evaluation and Research Working Paper Series No. 2. UNICEF: New York. [Google Scholar]
- Pelletier D.L. & Shrimpton R. (1994) The role of information in the planning, management and evaluation of community nutrition programmes. Health Policy Plan 9, 171–184. [DOI] [PubMed] [Google Scholar]
- Penny M.E., Creed‐Kanashiro H.M., Robert R.C., Narro M.R., Caulfield L.E. & Black R.E. (2005) Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: a cluster‐randomised controlled trial. Lancet 365, 1863–1872. [DOI] [PubMed] [Google Scholar]
- Pielemeier N.R. (1978) Use of the Child's Growth Chart as an Educational Tool. Office of Nutrition Development Support Bureau Agency for International Development: Washington, DC. [Google Scholar]
- Pinchinat S., Enel C., Pison G., Duthé G., Lagarde E., Simondon F. et al (2004) No improvement in weight‐for‐age of young children in southern Senegal, 1969–1992, despite a drastic reduction in mortality. Evidence from a growth monitoring programme. International Journal of Epidemiology 33, 1202–1208. [DOI] [PubMed] [Google Scholar]
- Rawlinson R. (1977) Health and nutrition concepts in uneducated highland women. Papua New Guinea Medical Journal 20, 117–121. [PubMed] [Google Scholar]
- Roberfroid D., Lefèvre P., Hoerée T. & Kolsteren P. (2005) Perceptions of growth monitoring and promotion among an international panel of District Medical Officers. Journal of Health, Population, and Nutrition 23, 207–214. [PubMed] [Google Scholar]
- Robert R.C., Gittelsohn J., Creed‐Kanashiro H.M., Penny M.E., Caulfield L.E., Narro M.R. et al (2006) Process evaluation determines the pathway of success for a health center‐delivered, nutrition education intervention for infants in Trujillo, Peru. Journal of Nutrition 136, 634–641. [DOI] [PubMed] [Google Scholar]
- Robert R.C., Gittelsohn J., Creed‐Kanashiro H.M., Penny M.E., Caulfield L.E., Narro M.R. et al (2007) Implementation examined in a health center‐delivered, educational intervention that improved infant growth in Trujillo, Peru: successes and challenges. Health Education Research 22, 318–331. [DOI] [PubMed] [Google Scholar]
- Van Roekel K., Plowman B., Griffiths M., De Alvarado V.V., Matute J. & Calderón M. (2002) BASICS II Midterm Evaluation of the AIN Program in Honduras, 2000. Survey Report, BASICS II/USAID.
- Rohde J.E. (1988). Editorial. Indian Journal of Pediatrics 55 (Suppl.): S1–S2. 3391655 [Google Scholar]
- Rohde J.E. & Northrup R.S. (1988) Feeding, feedback and sustenance of primary health care. Indian Journal of Pediatrics 55 (Suppl.), S110–S123. [DOI] [PubMed] [Google Scholar]
- Ross A. & English M. (2005) Early infant growth monitoring – time well spent? Tropical Medicine and International Health 10, 404–411. [DOI] [PubMed] [Google Scholar]
- Ruel M.T. & Habicht J.‐P. (1992) Growth charts only marginally improved maternal learning from nutrition education and growth monitoring in Lesotho. Journal of Nutrition 122, 1772–1780. [DOI] [PubMed] [Google Scholar]
- Sall M. & Sylla J. (2005) African Prime Ministers take lead in child survival. Lancet 366, 1988–1989. [DOI] [PubMed] [Google Scholar]
- Santos I., Victora C.G., Martines J., Gonçalves H., Gigante D.P., Valle N.J. et al (2001) Nutrition counseling increases weight gain among Brazilian children. Journal of Nutrition 131, 2866–2873. [DOI] [PubMed] [Google Scholar]
- Save the Children UK (2003) Thin on the Ground: Questioning the Evidence Behind World Bank Funded Community Nutrition Projects in Bangladesh, Ethiopia and Uganda. Save the Children UK: London. Available at: http://www.savethechildren.org.uk (accessed September 2006). [Google Scholar]
- Schroeder D.G., Pachón H., Dearden K.A., Ha T.T., Lang T.T. & Marsh D.R. (2002) An integrated child nutrition intervention improved growth of younger, more malnourished children in northern Viet Nam. Food and Nutrition Bulletin 23 (4 Suppl.), 50–58. [PubMed] [Google Scholar]
- Scrimshaw N.S. (1974) Myths and realities in international health planning. American Journal of Public Health 64, 792–798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shekar M. (1991) The Tamil Nadu Integrated Nutrition Project: a review of the project with special emphasis on the monitoring and information system. Cornell Food and Nutrition Policy Program Working Paper 14.
- Shekar M. & Latham M.C. (1992) Growth monitoring can and does work! An example from the Tamil Nadu Integrated Nutrition Project in rural south India. Journal of Pediatrics 59, 5–15. [DOI] [PubMed] [Google Scholar]
- Shrimpton R. (2003) Growth monitoring and evaluation activities in Vietnam. Report to UNICEF.
- Shrimpton R., Victora C.G., De Onis M., Lima R.C., Blössner M. & Clugston G. (2001) Worldwide timing of growth faltering: implications for nutritional interventions. Pediatrics 107, e75. [DOI] [PubMed] [Google Scholar]
- Shrimpton R., Macleod J., Metz P. & Belbase K. (2003) UNICEF Nutrition Portfolio Review (1980–1999): A Contribution to the World Bank/UNICEF Nutrition Assessment. UNICEF: New York. [Google Scholar]
- De Souza A.C., Peterson K.E., Cufino E., Gardner J., Craveiro M.V.A. & Ascherio A. (1999) Relationship between health services, socioeconomic variables and inadequate weight gain among Brazilian children. Bulletin of the World Health Organization 77, 895–905. [PMC free article] [PubMed] [Google Scholar]
- Tanner J.M. (1991) Auxology In: History of Pediatrics 1850–1950 (eds Nichols B.L., Ballabriga A. & Kretchmer N.), pp 147–57. Raven Press: New York. (Nestlé Nutrition Workshop Series v.22). [Google Scholar]
- The World Bank (2005) Bangladesh Integrated Nutrition Project. Project performance assessment report. Operations Evaluation Department, Report No. 32563. [Google Scholar]
- The World Bank . Promoting the Growth of Children. What Works. Nutrition Toolkit Tool #4. Available at: http://www.worldbank.org/nutritiontoolkit [Google Scholar]
- UNICEF (1993) We Will Never Go Back. UNICEF: New York. [Google Scholar]
- Valadez J.J., Brown L.D., Vargas W.V. & Morley D. (1995) Using Lot Quality Assurance Sampling to assess measurements for growth monitoring in a developing country's primary health care system. International Journal of Epidemiology 25, 381–387. [DOI] [PubMed] [Google Scholar]
- Victora C.G., Wagstaff A., Schellenberg J.A., Gwatkin D., Claeson M. & Habicht J.‐P. (2003) Applying an equity lens to child health and mortality: more of the same is not enough. Lancet 362, 233–241. [DOI] [PubMed] [Google Scholar]
- Victora C.G., Hanson K., Bryce J. & Vaughan J.P. (2004) Achieving universal coverage with health interventions. Lancet 364, 1541–1548. [DOI] [PubMed] [Google Scholar]
- Viravaidhya K.V., Tima K.N. & Merrill H.D. (1981)Impact of Age/Weight Charts Maintained in the Home and Nutrition Education on Nutritional Status of Infants and Pre‐school Children. Nutrition Division, Ministry of Public Health, Royal Thai Government: Bangkok. [Google Scholar]
- Waters H.R., Penny M.E., Creed‐Kanashiro H.M., Robert R.C., Narro R., Willis J. et al (2006) The cost‐effectiveness of a child nutrition education programme in Peru. Health Policy Plan 21, 257–264. [DOI] [PubMed] [Google Scholar]
- Werner D. & Sanders D. (1997) Questioning the Solution: The Politics of Primary Health Care and Child Survival. Healthwrights: Palo Alto. [Google Scholar]
- WHO (1962) Joint FAO/WHO Expert Committee on Nutrition, Sixth Report. WHO Technical Report Series 245. World Health Organization: Geneva. [Google Scholar]
- WHO (1978) A Growth Chart for International Use in Maternal and Child Health Care: Guidelines for Primary Health Care Personnel. World Health Organization: Geneva. [Google Scholar]
- WHO Multicentre Growth Reference Study Group (2006) WHO child growth standards based on length/height, weight and age. Acta Paediatrica 95 (Suppl.450), 76–85. [DOI] [PubMed] [Google Scholar]
- Williams G. (1986) Save the babies. World Health Forum 7, 391–398. [Google Scholar]
- Wollinka O., Keeley E., Burkhalter B.R. & Bashir N. (eds) (1997) Hearth Nutrition Model: Applications in Haiti, Vietnam and Bangladesh. BASICS: Arlington. [Google Scholar]
- Wray J.D. (1978) Direct nutrition intervention and the control of diarrheal diseases in preschool children. American Journal of Clinical Nutrition 31, 2073–2082. [DOI] [PubMed] [Google Scholar]
- Zachariah P.S., Cowan B. & Dhillion H. (1980) Limitations of the under‐fives' clinics in a comprehensive health care programme. Journal of Tropical Pediatrics 26, 144–149. [DOI] [PubMed] [Google Scholar]


