Abstract
We assessed eight World Health Organization (WHO) core child feeding indicators for their association with stunting and underweight in Cambodia in 2000 and 2005. We compared the feeding data from the Cambodian Demographic and Health Surveys for 2000 with 2005 for 0–24 months children using the WHO feeding indicators, with stunting and underweight as outcomes. Prevalence of stunting and underweight was significantly less in 2005 than in 2000 among children aged 0–5 and 6–11 months, but stunting among children 18–23 months remained >50%. Prevalence of compliance with seven of the eight core healthy feeding indicators was higher in 2005. Exclusive breastfeeding among 0–5 months infants increased more than fivefold; among 6–11 and 12–17 months children, prevalence of feeding diversity and meeting a minimally acceptable diet, while improved, remained ≈25%. Modelling showed compliance with breastfeeding indicators was associated with reduced risk of underweight in 0–5 months infants, no association between compliance with feeding indicators and growth outcomes in other ages, and a significant association of higher relative wealth with growth outcomes overall. Between 2000 and 2005, Cambodia stabilized and focused resources on infant feeding. Prevalence of meeting the WHO feeding indicators improved, but modelling indicated that, in general, relative wealth, not feeding practices, was associated with improved growth outcomes. Yet, over 50% of children 18–23 months were stunted in 2005. Similar to the success with breastfeeding, focus on complementary feeding of 6–23 months children may reduce the risk of stunting in Cambodia.
Keywords: breastfeeding promotion, child feeding, child growth, poverty, stunting, underweight
Introduction
Maternal and child undernutrition is the principal underlying cause of 3.5 million deaths and 11% of total global disability‐adjusted life years (Bhutta et al. 2008; Black et al. 2008), making undernutrition the largest single age risk factor for global disease burden (Bryce et al. 2008). To address the crisis of undernutrition, the World Health Organization (WHO) released feeding guidance for the breastfed and non‐breastfed child (Pan American Health Organization (PAHO) 2003; Dewey et al. 2004; WHO 2005), and indicators to assess feeding patterns (WHO 2008a). The indicators and the WHO growth standards (WHO Multicentre Growth Reference Study Group 2006; WHO 2008b) provide a basis for assessing undernutrition to help improve child nutrition outcomes.
In Cambodia, undernutrition is viewed as the most important risk factor for infant mortality (Collins et al. 2007). In 1999, Cambodia participated for the first time in the Demographic and Health Surveys (DHS) and collected nationally representative data on maternal and young child health and behaviour. The results indicated high rates of undernutrition as measured by stunting 44.3% (low height for age), wasting 15.0% (low weight for height) and underweight 45.3% (low weight for age) in children less than 5 years of age (National Institute of Statistics et al. 2001). Stunting is viewed as an indicator of chronic undernutrition, wasting as an indicator of acute undernutrition, and underweight as a composite indicator, which reflects both chronic and acute undernutrition. Information on young child feeding patterns was similarly discouraging, with low compliance with the recognized WHO guidance on breastfeeding and complementary feeding (National Institute of Statistics et al. 2001; PAHO 2003; UNICEF 2008a). In 2005, Cambodia released findings from a second DHS survey that demonstrated significant improvement in undernutrition indicators: stunting 37.3%, wasting 7.3% and underweight 35.6% (National Institute of Statistics et al. 2006). In the Cambodian DHS 2000 and 2005 reports, measures of undernutrition were generated using the US National Center for Health Statistics growth standards (Victora et al. 1998).
Cambodia has undergone dramatic change in the last decade that has led to stabilization of the country and an increase in the gross domestic product from $3.7 billion in 2000 to $6.2 billion in 2005 (World Bank 2008a). This economic growth is reflected in an increase in the per capita gross national income (purchasing power parity) from 860 to 1380 (2006 US dollars), export of rice and other commodities, and foreign investments (World Bank 2008a). As a result, Cambodia increased investments in health‐service delivery (Pavignani 2006) and made strides towards implementing a national poverty reduction strategy (Cambodian Ministry of Health 2002; Lane 2007). Between 1999 and 2005, life expectancy at birth in Cambodia increased from 56.5 to 58.3 years, and under‐5‐yr mortality rates declined from 104.2 to 85.4 per 1000 children (World Bank 2008a). Also during this time, rural inequality of consumption stabilized and inequality non‐consumption measures of living standards narrowed, including access to roads, clean water, electricity, schooling and health care (Lane 2007). Nonetheless, Cambodia remains a developing country, which is included among the World Bank's 53 low‐income economies and ranks economically as 180th of 209 global countries (World Bank 2008b). In addition, the urban–rural gap in terms of access to amenities remains wide in Cambodia, and this gap is a continued target for further poverty reduction (Adams et al. 2007).
Beginning in 2003, the Cambodian Ministry of Health invested $41 million into its national plan of action on nutrition and adopted a national policy on infant and young child feeding (Dara 2003). In 2004, in partnership with the United Nations Children's Fund, the WHO, Cooperative for Assistance and Relief Everywhere, Inc. Cambodia, and the Cambodian Reproductive and Child Health Alliance, the Cambodian Ministry of Health launched a baby‐friendly community initiative that promoted exclusive breastfeeding through mother support‐group networking. This programme grew from 600 villages in 2005 to 2675 villages throughout the country by the end of 2007 (Collins et al. 2007).
The breastfeeding education campaign in Cambodia coincided with rapid national economic growth. Recent publications have underscored the association between undernutrition, based on growth indicators, and poverty (Blakely et al. 2005; Nandy et al. 2005; Gonzalez‐Cossio et al. 2006). In Mexico, measures of recommended breastfeeding and complementary feeding practices in a national, probabilistic survey were not associated with growth when economics and other factors were part of logistic regression models (Gonzalez‐Cossio et al. 2006). In contrast, recommended child feeding practices were positively associated with height for age using DHS data in seven Latin American countries, with the effect being statistically stronger for children of lower socio‐economic status (Ruel & Menon 2002). Similarly, dietary diversity measured using DHS data for 6‐to 23‐month‐old children was positively associated with height for age in 7 of 11 countries when other variables were considered (Arimond & Ruel 2004).
Van dePoel et al. (2008) recently presented an analysis of stunting and wasting (as measures of malnutrition) and socio‐economic inequalities in malnutrition in 47 developing countries. This study, which used DHS data with the recently published WHO global growth standards (WHO Multicentre Growth Reference Study Group 2006), reported that stunting and wasting ‘disproportionately affected the poor’. However, while these authors found that socio‐economic inequality in malnutrition was prevalent throughout low‐income countries, it was not related to growth measures when they considered other factors. Data from the 2000 Cambodian DHS were included in the study, and index values indicated that stunting and wasting were more concentrated in poorer children in Cambodia.
The purpose of our study was to assess the new WHO core healthy feeding indicators (WHO 2008a) with other covariates in terms of their association with the documented improvement in stunting and underweight in Cambodia using data from the DHS in 2000 and 2005. For this analysis we used the eight core WHO healthy feeding indicators (WHO 2008a) and WHO growth standards to calculate stunting and underweight as outcome measures (WHO Multicentre Growth Reference Study Group 2006). We hypothesized that improvement in the core feeding indicators would be highly associated with improvement in undernutrition in Cambodia.
Key messages
-
•
Prevalence of maternal compliance with criteria underlying each of the eight WHO core feeding indicators was significantly higher in 2005 compared with 2000 for all indicators, with the exception of currently breastfeeding at 12–15 months.
-
•
Prevalence of stunting and underweight was significantly less in 2005 than in 2000 among children aged 0–5 and 6–11 months, but stunting among children 18–23 months remained >50%.
-
•
Exclusive breastfeeding among 0–5 months infants increased more than fivefold; among 6–11 and 12–17 months children, prevalence of feeding diversity and meeting a minimally acceptable diet, while improved, remained ≈25%.
-
•
When we included data on the compliance with the eight core feeding indicators in regression models with sociodemographic variables for 2000 and 2005, we found compliance with breastfeeding indicators was associated with reduced risk of underweight in 0–5 months infants, no association between compliance with complementary feeding indicators and growth outcomes, and a significant association of higher relative wealth with growth outcomes.
-
•
The high prevalence of stunting among 18–23 months children and the low prevalence of adequate dietary diversity and meeting minimum acceptable diet criteria among 6–17 months children suggest the need for a focus on improvement in dietary quality for this age group to reduce the percent of children who are stunted in Cambodia.
Materials and methods
Survey instrument
We accessed ‘MEASURE DHS+’ data collected in Cambodia in 2000 and 2005 (Macro International Inc., Opinion Research Corporation (ORC Macro) 2007). The DHS selected nationally representative samples of women of childbearing age.
Under contract with the US Agency for International Development since 1989, ORC Macro updates the DHS basic model instrument approximately every 5 years and facilitates the conduct of the survey with in‐country nationals. The DHS model core maternal/infant questionnaire collects information on anthropometry, child feeding and child morbidity, and is paired with household and other modules depending upon the country. ORC Macro staff and in‐country staff modify specific questions and answers to be country‐ or culturally relevant, as needed.
Study sample
We accessed ‘MEASURE DHS+’ data collected in Cambodia in 2000 and 2005 that employed two different model survey instruments. We calculated the country‐specific counts for each survey and compared these counts to reports on the ORC Macro web site to ensure that full data sets were included for each survey year.
For our study, we tested the eight core indicators for assessing infant and young child feeding (WHO 2008a), and selected the youngest living child up to 24 months of age in each of the families. We excluded, from all analyses, deceased children and children for whom age information was missing. Children from one mother were only included in the analysis if the children were born at the same time (i.e. twins or triplets). As specified in each of the core indicators, we conducted separate analyses for different age groups of children. In 2000 and 2005, the Cambodia study only collected height and weight information on mothers and children for a 50% subsample. We used this subsample to calculate stunting and underweight, and in multivariate models, which tested these undernutrition indicators.
Variables
We tested eight core indicators for assessing infant and young child feeding using definitions and parameters for child feeding associated with each indicator (Table 1), and disaggregated the data by the specified age groups. Indicators for infants 0–5 months were initiation of breastfeeding in the first hour after birth and exclusive breastfeeding. Complementary feeding indicators were dietary diversity, feeding frequency, feeding iron‐fortified foods and minimum acceptable diet, which is a combination of dietary diversity and feeding frequency. Breastfeeding at 1 year (age 12–15 months) and introduction of solid, semi‐solid and soft foods (hereafter complementary foods) (age 6–8 months) were tested independently because of their unique age ranges. We scored infants whose mothers' feeding behaviour matched all of the core indicators that were relevant for their age (i.e. the breastfeeding indicators for infants under 6 months of age, and dietary diversity, feeding frequency and iron‐fortified foods for those age 6–23 months) as being compliant with all of the relevant indicators.
Table 1.
Eight core indicators for assessing infant and young child feeding
| 1. Early Initiation of breastfeeding: |
| Children born in the last 23.9 months and breastfed within 1 h of birth |
| Disaggregated and reported for live births in the last 11.9 months and live births occurring between the last 12 and 23.9 months |
| 2. Exclusive breastfeeding under 6 months: |
| Infants 0–5.9 months of age who received only breast milk during the previous day |
| Infants 0–5.9 months of age |
| Disaggregated for the following age groups: 0–1.9, 2–3.9 and 4–5.9 months |
| 3. Continued breastfeeding at 1 year: |
| Children 12–15.9 months of age who received breast milk during the previous day |
| Children 12–15.9 months of age |
| 4. Introduction of solid, semi‐solid or soft foods: |
| Infants 6–8.9 months of age who received solid, semi‐solid or soft foods during the previous day |
| Infants 6–8.9 months of age |
| 5. Minimum dietary diversity: |
| Children 6–23.9 months of age who received foods from ≥4 food groups during the previous day |
| Children 6–23.9 months of age |
| Disaggregated for age groups 6–11.9, 12–17.9 and 18–23.9 months |
| 6. Minimum meal frequency: |
| Breastfed children 6–23.9 months of age who received solid, semi‐solid or soft foods the minimum number of times or more during the previous day |
| Breastfed children 6–23.9 months of age |
| Disaggregated for age groups 6–11.9, 12–17.9 and 18–23.9 months |
| Where minimum equals: |
| two times for breastfed infants 6–8.9 months |
| three times for breastfed children 9–23.9 months |
| 7. Minimum acceptable diet: |
| Breastfed children 6–23.9 months of age who received at least the minimum dietary diversity and the minimum meal frequency during the previous day |
| Breastfed children 6–23.9 months of age |
| Disaggregated for age groups 6–11.9, 12–17.9 and 18–23.9 months |
| 8. Consumption of iron‐rich or iron‐fortified food: |
| Children 6–23.9 months of age who received an iron‐rich food, or a food that was specially designed for infants and young children and was fortified with iron, or a food that was fortified in the home with a product that included iron during the previous day |
| Children 6–23.9 months of age |
| Disaggregated for age groups 6–11.9, 12–17.9 and 18–23.9 months |
Source: Indicators for assessing infant and young child feeding practices, conclusions of a consensus meeting held 6–8 November 2007 in Washington, DC, USA (WHO 2008a).
We used logistic regression models to estimate the relationship between the feeding indicators and two outcome measures – stunting and underweight. We chose stunting and underweight because of the prominence of these two measures as health indicators for undernutrition and for assessing progress towards global development goals. We assessed stunting and underweight using the growth standards from the WHO (WHO Multicentre Growth Reference Study Group 2006; WHO 2008b) as outcome indicators for undernutrition (UN 2000; WHO 2007; Standing Committee on Nutrition 2008). Height and weight more than two z‐scores below the reference population mean were classified as stunted or underweight, respectively (WHO Multicentre Growth Reference Study Group 2006).
Analytical methods
DHS interviewers asked mothers how many times their infant consumed a liquid or complementary food in the prior 24 h. Breastfed children were classified as exclusively breastfed if they received no liquid or complementary foods in the prior 24 h. Solid food variables were recoded so any consumption was set to 1 and responses of ‘no consumption’ or ‘do not know’ were set to 0. Missing values were treated as missing.
To calculate minimum food diversity in the prior 24 h for children 6–23.9 months, reported intake of complementary foods was grouped into six (2000) or seven (2005) groups because meat and eggs were combined in the 2000 Cambodia survey. We used a report of intake of at least four food groups during the previous day as meeting the minimum dietary diversity indicator (Table 1).
We used sample weights for all analyses, taking into account the sample design information in the DHS manual (Rutstein & Rojas 2006). The sampling frame for the Cambodia 2000 and 2005 surveys was complex and included multistage, clustering, stratification and unequal probability sampling.
Statistical analysis
We used the SAS (Version 9.2; SAS Institute, Cary, NC, USA) statistical software programme (SAS Institute Inc. 2004). Standard errors were estimated using the Taylor series linearization method that incorporated sampling weights and used variance formulas appropriate for the DHS sample design using the SAS mean, t‐test and logistic procedures. We used t‐tests on weighted percentages to compare results between the 2000 and 2005 surveys.
We performed multivariate analyses separately for breastfeeding indicators (indicators 1 and 2 in Table 1) and complementary food feeding indicators (indicators 5 through 8) using the subsample for which height and weight data were available. We estimated separate models for 2000 and 2005, allowing examination of changes in the relationship between outcomes and feeding practices at each time. The models estimated the relationship between overall compliance with the feeding practice indicators and outcomes (underweight and stunting). We estimated five models:
-
•
Models 1 and 1a: These models included the entire 0–23 months study sample and examined the relationship between all age‐specific feeding indicators and outcomes. Models 1 and 1a were the same, except that Model 1a included interaction terms between infant's age and compliance (compliant and age 0–5, 6–11 and 12–23 months).
-
•
Model 2: This model included 0–5‐month‐old infants and examined the relationship between the breastfeeding‐related indicators (initiation of breastfeeding, exclusive breastfeeding) and outcomes.
-
•
Models 3 and 3a: These models included 6–23‐month‐olds. Model 3 included separate indicators for dietary diversity and feeding frequency while Model 3a included an indicator for minimum acceptable diet that combines feeding frequency and dietary diversity.
Covariates in the statistical models included measures of compliance with the feeding indicators and other variables that were relevant to the indicators. These included indicators for the age and gender of the infant, mother's age and a measure of family wealth.
The DHS does not include family income or individual income variables. These variables can be unreliable in developing countries where family income is comprised of a diversity of recompense modes and many individuals cannot estimate an annual income. Instead, the DHS includes a carefully developed asset‐based wealth index (Rutstein & Johnson 2004). We included covariates for the family's asset index quintile in our models.
Infant weight at birth was only collected in a small subset of survey participants. We therefore created a ‘healthy pregnancy index’ to provide a baseline, covariate, proxy variable for infant health status at birth. We based this index on indicators of the mother's health/status and recommended perinatal practices (Black et al. 2008), whether the mother had a body mass index (BMI) > 18.5, a height > 150 cm, antenatal care, a tetanus injection, an iron supplement, no night blindness and assistance at birth. We specified each indicator as a binary variable. The healthy pregnancy index was calculated as the number of these indicators met by the mother. The healthy pregnancy index was included as a covariate in the models estimated for 0–5‐month‐olds.
We reported odds ratios and the 95% confidence interval of odds ratios, and Wald chi‐squared tests to determine statistical significance (SAS Institute Inc. 2004).
Results
For this study, our final sample included 3027 and 3112 mother–infant pairs from the 2000 and 2005 Cambodia DHS, respectively (Table 2). As height and weight data were collected on fewer mothers, our maternal BMI sample sizes were less (1491 and 1508, respectively). Because of the age‐targeted focus of the feeding indicators, the sample size differed with each infant age group‐based subsample, and we have organized our results accordingly. The overall prevalence of demographic and lifestyle characteristics of the two DHS surveys is included in Table 2, with prevalence of underweight and stunting in Table 3, overall compliance with the age‐based breastfeeding indicators and introduction of complementary foods in Table 4, and age‐based prevalence of compliance with the complementary feeding indicators in Table 5. In Table 6, we provide a summary of logistic regression combined with age‐based indicator associations with stunting and underweight based on age, while Table 7 summarizes the regression models based on specific feeding indicators. Table 8 illustrates the variables included in the asset index.
Table 2.
Demographic and lifestyle characteristics of mothers and infants. Cambodian Demographic and Health Surveys 2000 and 2005
| Characteristic (n: 2000; 2005) | 2000 | 2005 | ||||
|---|---|---|---|---|---|---|
| Mean % (SEM) | n | Mean % (SEM) | n | |||
| Infant gender (3027; 3112) | ||||||
| Male (%) | 50.9 | (0.91) | 1438 | 50.1 | (0.90) | 1490 |
| Female (%) | 49.1 | (0.91) | 1390 | 49.9 | (0.90) | 1487 |
| Average maternal age (years) (3027; 3112) | 29.6 | 0.12 | 28.4 † | 0.12 | ||
| Mother's education (3027; 3112) | ||||||
| None (%) | 32.1 | (0.85) | 908 | 22.5 † | (0.75) | 671 |
| Primary (%) | 53.1 | (0.91) | 1502 | 59.6 † | (0.88) | 1775 |
| Secondary or higher (%) | 14.8 | (0.65) | 418 | 17.8 † | (0.68) | 531 |
| Mother working (3027; 3112) | ||||||
| Mother works (%) | 78.7 | (0.75) | 2222 | 99.6 † | (0.11) | 2956 |
| Mother works outside home (%) | 19.4 | (0.81) | 431 | 17.7 | (0.80) | 386 |
| Mother's BMI (1491; 1508) | ||||||
| Mother's mean BMI | 20.4 | 0.06 | 20.7* | 0.07 | ||
| Healthy pregnancy index (children 0–5 months) (420; 342) | ||||||
| Mothers with BMI > 18.5 (%) | 86.5 | (1.67) | 332 | 83.1 | (2.03) | 261 |
| Mothers with height > 150 cm | 71.9 | (2.20) | 277 | 65.6 | (2.57) | 206 |
| Antenatal care (%) | 2.6 | (0.77) | 10 | 75.5 † | (2.33) | 237 |
| Tetanus injection (%) | 51.7 | (2.44) | 199 | 77.9 † | (2.25) | 244 |
| Iron supplement (%) | 30.6 | (2.25) | 118 | 71.0 † | (2.46) | 223 |
| No night blindness (%) | 89.7 | (1.48) | 345 | 92.2 | (1.46) | 289 |
| Assistance at birth (%) | 2.3 | (0.73) | 9 | 53.8 † | (2.70) | 169 |
| Mean total index score | 3.4 | (0.06) | 5.2 † | (0.08) | ||
| Asset index (3027; 3112) | ||||||
| Quintile 1 | 25.9 | (0.80) | 733 | 26.4 | (0.79) | 786 |
| Quintile 2 | 22.8 | (0.76) | 644 | 21.7 | (0.74) | 647 |
| Quintile 3 | 19.2 | (0.72) | 542 | 18.4 | (0.69) | 546 |
| Quintile 4 | 19.2 | (0.72) | 542 | 16.2 † | (0.66) | 483 |
| Quintile 5 | 12.9 | (0.61) | 366 | 17.3 † | (0.68) | 514 |
SEM, standard error of the mean; BMI, body mass index (kg m2). Analyses are based on the most recent living birth and include infants age 0–23 months or other age groups as specified. *Statistically significant at P < 0.05. †Statistically significant at P < 0.01.
Table 3.
Undernutrition indicators by age. Cambodian Demographic and Health Surveys 2000 and 2005
| Age (months) | Number of children in sample | Underweight (WHO) | Stunted (WHO) | |||
|---|---|---|---|---|---|---|
| 2000 | 2005 | 2000 | 2005 | 2000 | 2005 | |
| Mean % (SEM) | Mean % (SEM) | |||||
| 0–5 | 355 | 291 | 21.5 (2.01) | 9.8* (1.63) | 27.3 (2.18) | 17.2* (2.08) |
| 6–11 | 363 | 367 | 25.8 (2.19) | 17.6* (1.95) | 33.6 (2.36) | 17.5* (1.95) |
| 12–17 | 331 | 359 | 34.0 (2.48) | 21.6* (2.14) | 40.0 (2.56) | 37.2 (2.52) |
| 18–23 | 262 | 378 | 36.8 (2.84) | 30.4 (2.34) | 54.2 (2.94) | 52.7 (2.56) |
| 12–23 | 593 | 737 | 35.3 (1.86) | 26.2* (1.60) | 46.3 (1.95) | 45.4 (1.82) |
SEM, standard error of the mean; WHO, World Health Organization. *Statistically significant at P < 0.01.
Table 4.
Prevalence of overall compliance with World Health Organization feeding indicators*. Cambodian Demographic and Health Surveys 2000 and 2005
| Breastfeeding indicators | 2000 | 2005 |
|---|---|---|
| Initiation of breastfeeding in first hour | ||
| 0–11 months | ||
| Mean % (SEM) | 11.1 (0.77) | 34.8 ‡ (1.21) |
| n | 1672 | 1542 |
| 12–23 months | ||
| Mean % (SEM) | 12.5 (0.94) | 33.8 ‡ (1.21) |
| n | 1245 | 1529 |
| Exclusive breastfeeding | ||
| 0–1 months | ||
| Mean % (SEM) | 18.0 (2.51) | 73.8 ‡ (2.93) |
| n | 234 | 226 |
| 2–3 months | ||
| Mean % (SEM) | 11.7 (1.77) | 66.4 ‡ (2.85) |
| n | 329 | 275 |
| 4–5 months | ||
| Mean % (SEM) | 5.6 (1.34) | 48.7 ‡ (3.20) |
| n | 296 | 245 |
| Currently breastfeeding | ||
| 12–15 months | ||
| Mean % (SEM) | 87.1 (1.50) | 89.6 (1.33) |
| n | 505 | 532 |
| Introduction of complementary foods | ||
| 6–8 months | ||
| Mean % (SEM) | 74.7 (2.10) | 82.4 ‡ (1.92) |
| n | 431 | 393 |
SEM, standard error of the mean. *Indicators for assessing infant and young child feeding practices, conclusions of a consensus meeting held 6–8 November 2007 in Washington, DC, USA (Working Group on Infant and Young Child Feeding Indicators 2007). ‡Statistically significant at P < 0.01.
Table 5.
Complementary feeding indicators by age. Cambodian Demographic and Health Surveys 2000 and 2005
| Age (months) | Sample size | Feeding frequency | Feeding diversity | Minimum acceptable diet | Iron‐rich and iron‐fortified foods (including formula) | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2000 | 2005 | 2000 | 2005 | 2000 | 2005 | 2000 | 2005 | 2005 | 2000 | |
| Mean % (SEM) | Mean % (SEM) | Mean % (SEM) | Mean % (SEM) | |||||||
| 6–11 | 830 | 790 | 52.1 (1.74) | 62.2* (1.73) | 20.4 (1.40) | 27.4* (1.60) | 13.9 (1.20) | 20.9* (1.45) | 52.9 (1.75) | 59.4* (1.75) |
| 12–17 | 713 | 794 | 59.9 (1.84) | 70.8* (1.62) | 21.9 (1.04) | 26.2* (1.11) | 14.5 (0.88) | 20.7* (1.02) | 41.9 (1.25) | 51.5* (1.27) |
| 18–23 | 610 | 758 | 62.1 (2.00) | 64.8 (1.74) | 44.7 (2.02) | 56.6* (1.80) | 31.2 (1.88) | 41.5* (1.80) | 84.3 (1.54) | 91.0* (1.05) |
SEM, standard error of the mean. *Statistically significant at P < 0.01.
Table 6.
Association of stunting and underweight and overall compliance with World Health Organization feeding indictors* for children of different age groups † . Cambodian Demographic and Health Survey, 2000 and 2005
| Stunting [odds ratio (95% CI)] | Underweight [odds ratio (95% CI)] | |||||||
|---|---|---|---|---|---|---|---|---|
| 2000 models | 2005 models | 2000 models | 2005 models | |||||
| Model 1 | Model 1a | Model 1 | Model 1a | Model 1 | Model 1a | Model 1 | Model 1a | |
| Age | 1.06 § | 1.07 § | 1.11 § | 1.12 § | 1.05 § | 1.06 § | 1.07 § | 1.06 § |
| (1.04, 1.08) | (1.05, 1.09) | (1.09, 1.13) | (1.09, 1.15) | (1.03, 1.07) | (1.04, 1.08) | (1.05, 1.09) | (1.03, 1.9) | |
| Infant is male | 1.21 | 1.22 | 1.64 § | 1.67 § | 1.26 | 1.26 | 1.77 § | 1.76 § |
| (0.96, 1.51) | (0.97, 1.53) | (1.28, 2.10) | (1.30, 2.13) | (0.99, 1.60) | (0.99, 1.60) | (1.34, 2.33) | (1.33, 2.32) | |
| Mother's age | 1.00 | 1.00 | 1.02 | 1.02 | 1.01 | 1.01 | 1.01 | 1.01 |
| (0.99, 1.02) | (0.99, 1.02) | (1.00, 1.04) | (1.00, 1.04) | (1.00, 1.03) | (1.00, 1.03) | (0.99, 1.03) | (0.99, 1.03) | |
| Asset index: Quintile 2 | 0.66 ‡ | 0.65 § | 0.82 | 0.82 | 0.75 | 0.75 | 1.08 | 1.07 |
| (0.48, 0.91) | (0.47, 0.90) | (0.58, 1.16) | (0.58, 1.16) | (0.54, 1.04) | (0.54, 1.04) | (0.75, 1.55) | (0.75, 1.54) | |
| Asset index: Quintile 3 | 0.60 § | 0.59 § | 0.71 | 0.71 | 0.57 § | 0.56 § | 0.55 § | 0.55 § |
| (0.43, 0.84) | (0.42, 0.83) | (0.49, 1.01) | (0.49, 1.01) | (0.39, 0.81) | (0.39, 0.81) | (0.36, 0.84) | (0.36, 0.83) | |
| Asset index: Quintile 4 | 0.82 | 0.82 | 0.62 ‡ | 0.62 ‡ | 0.78 | 0.78 | 0.71 | 0.69 |
| (0.59, 1.15) | (0.59, 1.15) | (0.43, 0.91) | (0.42, 0.91) | (0.55, 1.10) | (0.55, 1.10) | (0.47, 1.08) | (0.45, 1.06) | |
| Asset index: Quintile 5 | 0.56 § | 0.57 § | 0.30 § | 0.30 § | 0.54 § | 0.56 ‡ | 0.33 § | 0.32 § |
| (0.37, 0.84) | (0.38, 0.85) | (0.20, 0.46) | (0.20, 0.46) | (0.35, 0.84) | (0.36, 0.88) | (0.20, 0.54) | (0.20, 0.53) | |
| Compliant with all relevant indicators | 1.21 | 0.91 | 1.09 | 0.85 | ||||
| (0.92, 1.61) | (0.71, 1.17) | (0.81, 1.46) | (0.64, 1.12) | |||||
| Compliant and age 0–5 months | 2.88 § | 1.38 | 2.33 ‡ | 0.50 ‡ | ||||
| (1.50, 5.52) | (0.84, 2.27) | (1.17, 4.62) | (0.26, 0.96) | |||||
| Compliant and age 6–11 months | 0.71 | 0.33 § | 1.23 | 1.04 | ||||
| (0.36, 1.41) | (0.16, 0.71) | (0.63, 2.40) | (0.56, 1.92) | |||||
| Compliant and age 12–17 months | 1.23 | 0.87 | 1.05 | 0.89 | ||||
| (0.82, 1.85) | (0.60, 1.28) | (0.68, 1.62) | (0.58, 1.37) | |||||
| Compliant and age 18–23 months | 0.94 | 0.95 | 0.68 | 0.99 | ||||
| (0.57, 1.54) | (0.63, 1.43) | (0.40, 1.16) | (0.63, 1.55) | |||||
CI, confidence interval. Note that Model 1 includes an indicator for whether the infant was in compliance with all the age‐specific relevant feeding indicators while Model 1a includes interaction terms between age and compliance. *Indicators for assessing infant and young child feeding practices, conclusions of a consensus meeting held 6–8 November 2007 in Washington, DC, USA (Working Group on Infant and Young Child Feeding Indicators 2007). †Sample size varied with age group and indicator. See Table 3. ‡Statistically significant, P < 0.05. §Statistically significant, P < 0.01.
Table 7.
Association of stunting and underweight with WHO feeding indicators*. Cambodian Demographic and Health Surveys 2000 and 2005
| WHO feeding indicators | ||||||||
|---|---|---|---|---|---|---|---|---|
| Stunting [odds ratio (95% CI)] | Underweight [odds ratio (95% CI)] | |||||||
| 2000 models | 2005 models | 2000 models | 2005 models | |||||
| 0–5 month olds † | Model 2 | Model 2 | Model 2 | Model 2 | ||||
| Pregnancy index | 0.80 ‡ | 1.13 | 0.88 | 0.73 | ||||
| (0.64, 1.00) | (0.88, 1.46) | (0.69, 1.11) | (0.53, 1.01 | |||||
| Initiated breastfeeding in first hour | 0.94 | 1.62 | 0.82 | 2.28 | ||||
| (0.44, 2.03) | (0.85, 3.11) | (0.34, 1.97) | (0.98, 5.33) | |||||
| Exclusive breastfeeding | 3.59 § | 1.00 | 2.91 § | 0.56 | ||||
| (1.74, 7.42) | (0.49, 2.02) | (1.35, 6.29) | (0.23, 1.35) | |||||
| 6–23 month olds ¶ | Model 3 | Model 3a | Model 3 | Model 3a | Model 3 | Model 3a | Model 3 | Model 3a |
| Minimum acceptable diet | 0.99 | 0.80 | 1.01 | 1.01 | ||||
| (0.71, 1.37) | (0.60, 1.08) | (0.71, 1.42) | (0.73, 1.39) | |||||
| Dietary diversity | 0.85 | 0.75 | 1.04 | 0.93 | ||||
| (0.61, 1.17) | (0.56, 1.02) | (0.74, 1.45) | (0.67, 1.29) | |||||
| Feeding frequency | 0.94 | 1.12 | 0.95 | 1.14 | ||||
| (0.72, 1.24) | (0.83, 1.51) | (0.72, 1.27) | (0.82, 1.57) | |||||
| Iron‐fortified foods | 0.96 | 0.89 | 0.80 | 0.80 | 0.91 | 0.92 | 0.93 | 0.93 |
| (0.69, 1.36) | (0.64, 1.23) | (0.52, 1.24) | (0.52, 1.21) | (0.64, 1.31) | (0.65, 1.29) | (0.58, 1.49) | (0.59, 1.48) | |
CI, confidence interval; WHO, World Health Organization. Note that these models also included age, gender, mother's age and asset quintile as covariates. *Indicators for assessing infant and young child feeding practices, conclusions of a consensus meeting held 6–8 November 2007 in Washington, DC, USA (Working Group on Infant and Young Child Feeding Indicators 2007). †Sample size for 0–5 months models: 2000 = 956; 2005 = 1104. ‡Statistically significant, P < 0.05. §Statistically significant, P < 0.0l. ¶Sample size for 6–23 months models: 2000 = 355; 2005 = 291.
Table 8.
Household possessions and housing characteristics* included in the Cambodian Demographic and Health Surveys asset indices based on the household surveys † in 2000 and 2005
| Variable | 2000 † | 2005 † | ||
|---|---|---|---|---|
| Mean % (SEM) | Mean % (SEM) | |||
| Household possessions | ||||
| Radio | 42.3 | (0.45) | 49.6 § | (0.42) |
| Television | 32.6 | (0.42) | 55.2 § | (0.42) |
| Phone | 3.6 | (0.17) | 20.1 § | (0.34) |
| Refrigerator | 1.8 | (0.12) | 2.9 § | (0.14) |
| Wardrobe | 21.2 | (0.37) | 30.0 § | (0.38) |
| Sewing machine | 7.6 | (0.24) | 8.4 ‡ | (0.23) |
| Means of transport | ||||
| Bicycle | 52.6 | (0.45) | 68.3 § | (0.39) |
| Animal drawn cart | 27.2 | (0.40) | 24.1 § | (0.36) |
| Motorcycle/scooter | 23.2 | (0.38) | 34.7 § | (0.40) |
| Car/truck | 2.3 | (0.14) | 3.9 § | (0.16) |
| Boat with motor | 3.6 | (0.17) | 3.4 | (0.15) |
| Boat without motor | 5.3 | (0.20) | 5.4 | (0.19) |
| Has electricity | 16.6 | (0.34) | 20.5 § | (0.34) |
| Main floor material | ||||
| Earth, sand | 9.0 | (0.26) | 8.5 | (0.23) |
| Wood planks | 44.9 | (0.45) | 48.1 § | (0.42) |
| Palm, bamboo | 36.9 | (0.44) | 30.0 § | (0.38) |
| Ceramic tiles | 5.2 | (0.20) | 5.9 ‡ | (0.20) |
| Cement | 2.6 | (0.14) | 6.8 § | (0.21) |
| Roofing | ||||
| Natural roofing (palm, bamboo, thatch) | 40.8 | (0.44) | 24.5 § | (0.36) |
| Metal | 25.2 | (0.39) | 38.2 § | (0.41) |
| Tiles/cement | 33.5 | (0.43) | 37.0 § | (0.40) |
| Water source | ||||
| Piped water | 5.9 | (0.24) | 10.5 § | (0.31) |
| Well | 56.9 | (0.50) | 56.1 | (0.50) |
| Surface water | 28.0 | (0.45) | 24.2 § | (0.43) |
| Rain | 1.1 | (0.10) | 2.1 § | (0.14) |
| Tanker | 4.6 | (0.21) | 5.3 § | (0.22) |
| Bottled | 0.1 | (0.03) | 1.6 § | (0.12) |
| Other | 3.4 | (0.18) | 0.2 § | (0.02) |
| Toilet facilities | ||||
| Flush | 13.7 | (0.31) | 24.4 § | (0.36) |
| Latrine | 7.0 | (0.23) | 1.8 § | (0.11) |
| Composting toilet | 79.1 | (0.37) | 71.5 § | (0.38) |
| Type of cooking fuel | ||||
| LPG/natural gas | 3.1 | (0.16) | 7.3 § | (0.22) |
| Kerosene | 0.5 | (0.06) | 0.0 § | (0.02) |
| Charcoal | 6.6 | (0.22) | 7.9 § | (0.23) |
| Firewood | 89.7 | (0.28) | 84.4 § | (0.30) |
LPG, liquefied petroleum gas; SEM, standard error of the mean. *Item categories with mean values of less than 1% in both time periods are not reported. †Sample sizes in the household surveys: 2000 = 12 236; 2005 = 12 243. ‡Statistically significant at the 5% level, P < 0.05. §Statistically significant at the 1% level, P < 0.01.
Comparison t‐tests of data from the two surveys indicated that there were no statistical differences in the distribution of male and female children (P = 0.53) between the surveys, whereas in 2005, maternal age was significantly lower (P < 0.0001) and maternal BMI was significantly higher (P = 0.012). More mothers attained a primary or secondary level of education, and the prevalence of no education was lower in 2005 than in 2000 (P < 0.0001). More mothers reported working in 2005 than in 2000 (P < 0.0001), but there was no significant difference in the proportion of women who reported working outside the home (P = 0.157).
The overall healthy pregnancy index score was significantly higher in 2005 than in 2000 (P < 0.0001). Within the healthy pregnancy index, there was no significant difference in the proportion of mothers with a BMI ≥ 18.5, or in the proportion of mothers with a height > 150 cm (P = 0.197 and P = 0.58, respectively). However, significantly more women engaged in healthful perinatal behaviours in 2005 than in 2000: tetanus injection (P < 0.0001), iron supplement (P < 0.0001), any assistance at birth (P < 0.0001) and antenatal care (P < 0.0001). The difference in the proportion of women reporting no night blindness was not statistically significant between the two surveys (P = 0.253).
By design, the asset index was constructed so that about 20% are in each quintile (across the entire sample for the country). In our analytic sample, there was a significantly lower proportion in asset index quintile 4 in 2005 (P < 0.0001) and a significantly higher proportion in asset index quintile 5 (P < 0.0001).
Using the WHO growth standards, we found that a lower proportion of children in 2005 were underweight (age groups: 0–5, 6–11, 12–17 and 12–23 months, P < 0.01) or stunted (age group: 0–5 and 6–11 months, P < 0.01) using the age groups from the WHO indicators (Table 3). For 12–17, 18–23 and 12–23 months children, the prevalence of stunting was slightly lower in 2005, but the differences were not statistically significant. Among 18–23 months children, the prevalence of stunting remained over 50% in both periods (2000: 54.2%; 2005: 52.7%). In 2005, the prevalence of stunting for 18–23 months children was more than three times as high as for the 0–5 and 6–11 months age groups.
We show the prevalence of compliance with the breastfeeding indicators for 2000 and 2005 in Table 4. With the exception of currently breastfeeding at 12–15 months, the prevalence of compliance with each indicator for both breastfeeding and complementary food feeding among all age groups increased significantly between the 2000 and 2005 surveys (P < 0.01). Of particular note is the more than fivefold increase in prevalence of exclusive breastfeeding for children 0–5 months (P < 0.01).
The mean prevalence of the four complementary food feeding indicators increased in 2005 (P < 0.01) for all age subgroups except feeding frequency for 18–23‐month‐old indicators (Table 5). Note that in 2005, the prevalence of meeting the criteria for recommended feeding frequency (>60%) and consumption of iron‐rich/fortified foods (>50%) was relatively high for all age groups In contrast, in 2005, the prevalence of meeting the criteria for feeding diversity and the composite measure, minimum acceptable diet, remained low for younger infants (feeding diversity: 6–11 months: 27.4%; 12–17 months: 26.2%; minimum acceptable diet: 6–11 months: 20.9%; 12–17 months: 20.7%). For 18–23 months children, the prevalence of meeting complementary feeding indicator criteria improved significantly from 2000 to 2005 for feeding diversity (from 44.7 to 56.6%: P < 0.001) and for minimum acceptable diet (from 31.2 to 41.5%: P < 0.01). In 2005, among 12–23 months children, there was a statistically significant improvement in prevalence of feeding iron‐rich foods (12–17 months: ≈51.5%; 18–23 months: 91%).
As recommended in the WHO report (WHO 2008a), we included Fig. 1 that shows the prevalence of exclusive breastfeeding and complementary food intake for each month across the first 6 months of life, and further illustrates the differences between the 2000 and 2005 DHS surveys. Significantly more women exclusively breastfed their infants in each of the first 6 months of life in 2005 than in 2000 (68% vs. 18% in month 1; 33% vs. 3% in month 5, respectively). The rates of change in breastfeeding initiation between 2000 and 2005, and the decrease in breastfeeding rates between months 1 and 5 in both years were statistically significant (P < 0.0001). In contrast, complementary food feeding practices (Fig. 1) were similar across the two survey years. In both years, some mothers introduced complementary foods earlier than recommended, with 17 and 9% (2000:2005) of children receiving complementary foods in their third month of life. Also in both years, the prevalence of mothers feeding complementary foods to their babies increased dramatically in the fifth month (2000: 39%; 2005: 36%), and by the sixth month, over 50% of babies were receiving complementary foods (2000: 57.3%; 2005: 67.2%).
Figure 1.
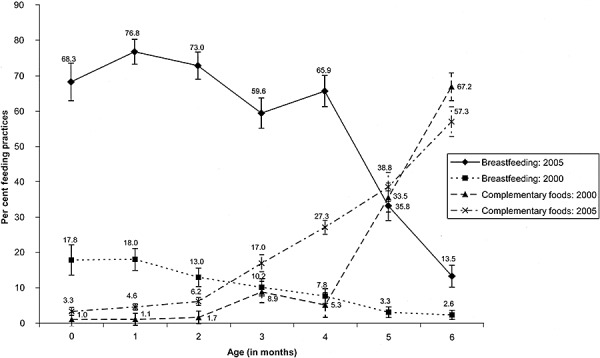
Exclusive breastfeeding and complementary foods: comparison of per cent feeding, Cambodian Demographic and Health Surveys, 2000 and 2005.
Table 6 presents the results of logistic regression models testing the association of the core feeding indicators with lowered stunting and underweight for the 2000 and 2005 DHS data. Overall compliance with all of the age‐specific indicators was not associated with any difference in the probability of being stunted or underweight (see the Model 1 columns in Table 6). However, the models (Model 1a) that examined the relationship between compliance and outcomes for specific age groups did identify some significant, although mixed, relationships between compliance with individual indicators and outcomes for specific age groups. In 2000, children aged 0–5 months whose mothers were compliant with the two breastfeeding indicators for their age group were significantly more likely to be stunted and underweight (P < 0.01 and P < 0.05, respectively). In 2005, children aged 0–5 months of compliant mothers were significantly less likely to be underweight (P < 0.05). Also, in 2005, 6–11 months children whose feeding was compliant with all core indicators for their age group were significantly less likely to be stunted (P < 0.01). There was no significant association between compliance with feeding indicators in 12−17 or 18–23 months children and either stunting or underweight.
Child age overall was significantly and positively associated with being stunted and underweight in both years (P < 0.01) and males were more likely to be both stunted and underweight in 2005 (P < 0.01). There was no association between mother's age and outcomes in either year.
Relative wealth was consistently associated with a lower probability of being both stunted and underweight. In both 2000 and 2005, those children whose families were in the highest asset quintile were significantly less likely to be stunted and also less likely to be underweight than those in the lowest quintile (which is the omitted category in these models) (P < 0.01 in all models except for underweight Model 1a in 2000, for which P < 0.05). There were also several significant coefficients for other asset index quintile variables, all of which supported the hypothesis that greater levels of wealth are associated with lower probabilities of stunting and underweight.
Table 7 shows the relationship between the age‐specific feeding indicators and the two outcome measures. There was no significant association between the initiation of breastfeeding in the first hour after birth and either outcome measures. Exclusive breastfeeding was statistically associated with a higher probability of being stunted and underweight in 2000 (both P < 0.01), but there was no association in 2005 when the prevalence of exclusive breastfeeding was much higher. None of the complementary food indicators for children ages 6 through 23 months was associated with either stunting or underweight in either years or for either models.
We disaggregated the variables that comprise the asset index to explore the changes in household wealth that occurred in Cambodia between 2000 and 2005 for each item used in the asset index (Table 8). Consistent with the profile of a country with improving economic conditions, mean values were higher in 2005 than they were in 2000 for most of the variables (P < 0.05 or P < 0.01), and, for some items in the asset index, the changes were substantial. For example, the proportion of families with a phone increased from 3.6% in 2000 to more than 20% in 2005, the proportion with a television increased from 32.6 to 55.2%, the proportion with piped water increased from 5.9 to 10.5%, and the proportion with a flush toilet increased from 13.7 to 24.4%.
Discussion
The data from the DHS in Cambodia in 2000 and in 2005 represented an assessment of feeding patterns at two distinct points in time. The results, like the focus of the feeding indicators, are highly age dependent. In 2005, there was a significantly lower prevalence of stunting and underweight in Cambodian children in age groups 0–5 and 6–11 months than in 2000. We reviewed compliance with the WHO core feeding indicators to assess the association of differences in compliance between 2000 and 2005 with stunting and underweight. Prevalence of compliance with seven of the eight WHO core healthy feeding indicators dramatically improved between 2000 and 2005. The one exception was the currently breastfeeding at 12–15 months, for which there was little change.
Overall, the healthy pregnancy index improved significantly in 2005, as did the perinatal maternal behaviours and access to health care services that comprised it. These changes may be partly the result of the investment of the Cambodian government and international organizations at the local level on reducing poverty and improving health care delivery systems in the country (Cambodian Ministry of Health 2002; Pavignani 2006; Adams et al. 2007; Lane 2007). These changes may also reflect improvements in wealth that occurred in the country between 2000 and 2005.
For compliance with the age‐specific core feeding indicators between 2000 and 2005, the largest difference was the over fivefold increase in the prevalence of exclusive breastfeeding and threefold increase in breastfeeding initiation among infants age 0–5 months. These data suggest that health educational interventions about breastfeeding in Cambodia, such as the baby‐friendly community initiative (Collins et al. 2007) and the various child and maternal health education and health support programmes instituted in Cambodia (Cambodian Ministry of Health 2002; Dara 2003; Lane 2007; UNICEF 2008b), had a positive impact on infant feeding practices, particularly exclusive breastfeeding. However, while initiation of breastfeeding within the first hour of life improved in prevalence from 2000 to 2005, only one‐third of Cambodian women in 2005 followed this practice. In contrast, in 2005, almost 90% of women in Cambodia reported continuing to breastfeed their babies through the first year of life.
When we tested the breastfeeding indicators in models that included socio‐economic attributes, maternal compliance with all relevant feeding indicators and with age‐relevant feeding indicators was not associated with reduced risk of stunting and underweight, with the exception of 0–5 months infants in 2005. We found that 0–5 months infants whose mothers were in compliance with both the exclusive breastfeeding and breastfeeding initiation indicators had a significantly lower risk of underweight in 2005 but a significantly higher risk of underweight in 2000. Compliance with breastfeeding indicators was not positively associated with a reduced risk of stunting in this same age group, perhaps reflecting the longer term chronic undernutrition that underpins stunting. Our primary finding in these models was a consistent positive association of reduction in risk of stunting and underweight associated with increases in relative wealth.
In 2005, 0–5 months males were at higher risk of being stunted and underweight than females. Factors, including higher energy requirements (Butte et al. 2000) and genetic, developmental and sociological factors (Harrison et al. 1999; Ward et al. 2000; Migeon 2006; Di Renzo et al. 2007), may dispose male infants to greater growth risks, as seen in Cambodia and elsewhere (Espo et al. 2002; Shah et al. 2003; Margai 2007).
Criteria for meeting the complementary food indicators were met by a higher per cent of mothers in 2005 than in 2000. Seventy‐five per cent of babies aged 6–8 months received solid food in 2000 compared with 82% in 2005. The mean prevalence for four of the complementary food feeding indicators (feeding frequency, feeding diversity, minimum acceptable diet, and consumption of iron‐rich and iron‐fortified foods) was significantly higher for all age subgroups in 2005 compared with 2000. However, while the prevalence for the feeding frequency and consumption of iron‐rich/fortified foods was relatively high, the prevalence of feeding diversity and the composite measure, minimum acceptable diet, remained low in 2005, particularly for the 6–11 and 12–17 months age ranges (feeding diversity: 27.4% and 26.2%; minimum acceptable diet: 20.9% and 20.7%, respectively). For the 18–23 months children, the prevalence of meeting these feeding indicators improved to 57 and 42%, respectively.
While the prevalence of meeting all of the complementary food feeding guidance indicators in 2005 for 6–23 months children was higher than in 2000, there was little evidence from our modelling analyses that these decreases in stunting and underweight were because of changes in feeding practices, at least as measured by the core feeding indicators. For 6–11 months infants, while prevalence of stunting and underweight in Cambodia significantly dropped to below 20% in 2005, meeting the overall solid food feeding indicators in this age group was associated in regression models with a significantly reduced risk of stunting in 2005, but no significant association for underweight. Among 12–17 month children, prevalence of underweight similarly dropped significantly to 16% in 2005. However, for children 18–23 months, prevalence of underweight was not significantly lower in 2005 and remained at 30%. None of the feeding indicators for 12–23 months children was associated with reduced risk of undernutrition.
Other authors have identified the high level of stunting among 12–23 months children in Cambodia as problematic (Collins et al. 2007). Prevalence of meeting a minimum acceptable diet improved to approximately 42% among 18–23 months children in 2005. However, stunting is an indicator of chronic undernutrition (WHO 2008b). Therefore, stunting in 18–23 months children may reflect individual child feeding patterns and/or repeated illness at a younger age. While this is a cross‐sectional study, the low per cent of 6–17‐month‐old children with a minimally acceptable diet may be a feeding pattern that could predispose these children to stunting at 18–23 months.
Similar to earlier studies (Nandy et al. 2005; Van dePoel et al. 2008) in Cambodia, we found an association between higher relative wealth and reduced risk of stunting and underweight. Examination of the asset index illustrated household‐level improvements in household structure, water sources, sanitation and cooking facilities that touched all aspects of family lives. Similar to other reports (Blakely et al. 2005; Nandy et al. 2005; Gonzalez‐Cossio et al. 2006; Van dePoel et al. 2008), relative reduction in poverty status led to household changes that may have been key factors in the decline in undernutrition in Cambodia.
Limitations of DHS include its cross‐sectional nature (preventing conclusions about causality) reporting and recall bias, and that the sampling scheme of population‐based clusters are not randomly spread across geographical areas (Rutstein & Johnson 2004; Rutstein & Rojas 2006). Food diversity measures combined meat and eggs in 2000, and information on the quantity of foods consumed was not collected (2001, 2006).
Our data show that increased relative wealth was associated with reduction in risk of stunting and underweight in Cambodia, and we found limited association of the WHO core feeding indicators with reduction in risk of these same outcomes. While prevalence of exclusive breastfeeding and meeting the criteria for other core feeding practices were higher in 2005 than in 2000 in Cambodia, changes in outcome measures could not be attributed to feeding practices when relative wealth was taken into consideration. In particular, while associated with relative wealth in regression modelling, overall stunting among 18–23‐month‐old children was greater than 50% in both years. Also of concern, less than 30% of women with 1–17 months infants met the criteria for meeting feeding diversity and the minimum acceptable diet.
Undernutrition in the first 2 years of life has been associated with poor later health outcomes and loss of human capital (Hoddinott et al. 2008; Victora et al. 2008). Stunting in particular has been associated with poor performance on cognitive tests in older children (Mendez & Adair 1999). The second year of life is recognized as a critical period in terms of child mortality (Black et al. 2008; Victora et al. 2008). The cross‐sectional nature of the DHS survey data makes it impossible for us to analyse the relationship between early exclusive breastfeeding and outcomes later in life for the individual infant. However, this study appears to support recent analyses that show that strategies for breastfeeding promotion can affect prevalence of feeding practices among children who are not exclusively breastfed (Black et al. 2008). However, the high prevalence of stunting in 18–23 months children coupled with paucity of women meeting the complementary feeding recommendations indicate that special attention needs to be paid to complementary feeding at the critical 6–23 months age range (Mendez & Adair 1999; Piwoz et al. 2003; Black et al. 2008; Hoddinott et al. 2008; Victora et al. 2008). These results also may imply the need to focus attention on the feeding practices targeted to the second year of life. Specifically, inclusion of quantity of food intake could enhance the dietary diversity indicator for tracking feeding changes and outcomes among young children. In addition, we envision that the Cambodian government could build on its breastfeeding education model to target its health education and health service delivery to food diversity among the 6–23 months children.
Source of funding
This project was funded by Wyeth Nutrition P.O. No. 4501241713/03 to Abt Associates, Inc.
Conflicts of interests
The authors declare that they have no conflicts of interest.
Acknowledgements
We thank Janice Abbas for the preparation of the manuscript, and Hao Nyugen for quality control of the table data and her research on gender differences in young children.
References
- Adams J.W., Porter I., Gill I.S., Agrawal N., Goh C. & Conway T. (2007) Sharing Growth: Equity and Development in Cambodia. Equity Report 2007. World Bank: Phnom Penh, Cambodia. [Google Scholar]
- Arimond M. & Ruel M.T. (2004) Dietary diversity is associated with child nutritional status: evidence from 11 demographic and health surveys. The Journal of Nutrition 134, 2579–2585. [DOI] [PubMed] [Google Scholar]
- Bhutta Z.A., Ahmed T., Black R.E., Cousens S., Dewey K., Gugliani E. (2008) Maternal and child undernutrition 3: what works? Interventions for maternal and child undernutrition and survival. Lancet 371, 41–64. [DOI] [PubMed] [Google Scholar]
- Black R.E., Allen L.H., Bhutta Z.A., Caulfield L.E., Deonis M., Ezzati M. et al. (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371, 243–260. [DOI] [PubMed] [Google Scholar]
- Blakely T., Hales S., Kieft C., Wilson N. & Woodward A. (2005) The global distribution of risk factors by poverty level. Bulletin of the World Health Organization 83, 118–126. [PMC free article] [PubMed] [Google Scholar]
- Bryce J., Coitinho D., Damton‐Hill I., Pelletier D., Pinstrup‐Andersen P. for the Maternal and Child Undernutrition Study Group (2008) Maternal and child undernutrition: effective action at national level. Lancet 371, 65–81. [DOI] [PubMed] [Google Scholar]
- Butte N.F., Wong W.W., Hopkinson J.M., Heinz C.J., Mehta N.R. & Smith E.O.B. (2000) Energy requirements derived from total energy expenditure and energy deposition during the first two years of life. The American Journal of Clinical Nutrition 72, 1558–1569. [DOI] [PubMed] [Google Scholar]
- Cambodian Ministry of Health (2002) National Poverty Reduction Strategy: 2003–2005. Kingdom of Cambodia: Phnom Penh, Cambodia. [Google Scholar]
- Collins D., Lewis E. & Steinberg K. (2007) Scaling Up Child Survival Interventions in Cambodia: The Cost of National Programme Resource Needs, Final Report. USAID, BASICS, World Health Organization: Geneva, Switzerland. [Google Scholar]
- Dara T. (2003) Cambodia: Nutrition Overview. National Nutrition Program, Ministry of Health: Phnom Penh, Cambodia. [Google Scholar]
- Dewey K.G., Cohen R.J., Rollins N.C. & Informal Working Group on Feeding of Nonbreastfed Children (2004) WHO technical background paper: feeding of nonbreastfed children from 6 to 24 months of age in developing countries. Food and Nutrition Bulletin 25, 377–402. [DOI] [PubMed] [Google Scholar]
- Di Renzo G.C., Rosati A., Sarti R.D., Cruciani L. & Cutuli A.M. (2007) Does fetal sex affect pregnancy outcome? Gender Medicine 4, 19–30. [DOI] [PubMed] [Google Scholar]
- Espo M., Kulmala T., Maleta K., Cullinan T., Salin M.L. & Ashorn P. (2002) Determinants of linear growth and predictors of severe stunting during infancy in rural Malawi. Acta Paediatrica 91, 1364–1370. [DOI] [PubMed] [Google Scholar]
- Gonzalez‐Cossio T., Rivera‐Dommarco J., Moreno‐Macias H., Monterrubio E.A. & Sepulveda J. (2006) Poor compliance with appropriate feeding practices in children under 2 yr in Mexico. The Journal of Nutrition 136, 2928–2933. [DOI] [PubMed] [Google Scholar]
- Harrison L.M., Morris J.A., Telford D.R., Brown S.M. & Jones K. (1999) The nasopharyngeal bacterial flora in infancy: effects of age, gender, season, viral upper respiratory tract infection and sleeping position. FEMS Immunology and Medical Microbiology 25, 19–28. [DOI] [PubMed] [Google Scholar]
- Hoddinott H., Maluccio J.A., Behrman J.R., Flores R. & Martorell R. (2008) Effect of a nutrition intervention during early childhood on economic productivity in Guatemalan adults. Lancet 371, 411–416. [DOI] [PubMed] [Google Scholar]
- Lane C. (2007) Scaling Up for Better Health in Cambodia. World Health Organization & Ministry of Health, Kingdom of Cambodia: Geneva, Switzerland. [Google Scholar]
- Margai F.M. (2007) Geographic targeting of risk zones for childhood stunting and related health outcomes in Burkina Faso. World Health & Population 9, 64–82. [DOI] [PubMed] [Google Scholar]
- Mendez M.A. & Adair L.S. (1999) Severity and timing of stunting in the first two years of life affect performance on cognitive tests in late childhood. The Journal of Nutrition 129, 1555–1562. [DOI] [PubMed] [Google Scholar]
- Migeon B.R. (2006) The role of X inactivation and cellular mosaicism in women's health and sex‐specific diseases. The Journal of the American Medical Association 295, 1428–1433. [DOI] [PubMed] [Google Scholar]
- Nandy S., Irving M., Gordon D., Subramanian S.V. & Smith G.D. (2005) Poverty, child undernutrition and morbidity: new evidence from India. Bulletin of the World Health Organization 83, 210–216. [PMC free article] [PubMed] [Google Scholar]
- National Institute of Statistics, Directorate General for Health [Cambodia] & ORC Macro (2001) Cambodia Demographic and Health Survey 2000. National Institute of Statistics, Directorate General for Health and ORC Macro: Phnom Penh, Cambodia, and Calverton, MD. [Google Scholar]
- National Institute of Statistics, Directorate General for Health [Cambodia] & ORC Macro (2006) Cambodia Demographic and Health Survey 2005. National Institute of Statistics, Directorate General for Health and ORC Macro: Phnom Penh, Cambodia, and Calverton, MD. [Google Scholar]
- ORC Macro (2007) Description of the Demographic and Health Surveys Individual Recode Data File, Version 1.0. Measure DHS+. ORC Macro: Calverton, MD. [Google Scholar]
- Pan American Health Organization (PAHO) (2003) Guiding Principles for Complementary Feeding of the Breastfed Child. Pan American Health Organization: Washington, DC, 40 pp. [Google Scholar]
- Pavignani E. (2006) Health Service Delivery in Post‐Conflict States. High Level Forum on the Health Millennium Development Goals (MDGs): Selected Papers, 2003–2005, World Bank & World Health Organization.
- Piwoz E.G., Huffman S.L. & Quinn V.J. (2003) Promotion and advocacy for improved complementary feeding: can we apply the lessons learned from breastfeeding? Food and Nutrition Bulletin 24, 29–44. [DOI] [PubMed] [Google Scholar]
- Ruel M.T. & Menon P. (2002) Child feeding practices are associated with child nutritional status in Latin America: innovative uses of the demographic and health surveys. The Journal of Nutrition 132, 1180–1187. [DOI] [PubMed] [Google Scholar]
- Rutstein S. & Johnson K. (2004) DHS Comparative Reports No. 6. The DHS Wealth Index. ORC Macro: Calverton, MD. [Google Scholar]
- Rutstein S.O. & Rojas G. (2006) Guide to DHS Statistics. ORC Macro: Calverton, MD. [Google Scholar]
- SAS Institute Inc . (2004) SAS/STAT9.1 Users Guide. SAS Institute Inc.: Cary, NC. [Google Scholar]
- Shah S.M., Selwyn B.J., Luby S., Merchant A. & Bano R. (2003) Prevalence and correlates of stunting among children in rural Pakistan. Pediatrics International 45, 49–53. [DOI] [PubMed] [Google Scholar]
- Standing Committee on Nutrition (2008) Recommendations from the SCN 35th Session: Accelerating the Reduction of Maternal and Child Undernutrition, Executive Summary. Available at: http://www.unsystem.org/SCN/Publications/AnnualMeeting/SCN35/35th_Session_Recommendations.pdf (accessed 17 July 2008).
- UN (2000) Millennium Development Goals. Available at: http://www.un.org/millenniumgoals/ (accessed 14 May 2008).
- UNICEF (2008a) The State of Asia‐Pacific's Children 2008: Child Survival. UNICEF: New York. [Google Scholar]
- UNICEF (2008b) Mother Support Group Network Promotes Exclusive Breastfeeding in Cambodia. Available at: http://www.unicef.org/infobycountry/cambodia_43437.html (accessed 14 May 2008).
- Van dePoel E., Hosseinpoor A.R., Speybroeck N., Van Ourti T. & Vega J. (2008) Socioeconomic inequality in malnutrition in developing countries. Bulletin of the World Health Organization 86, 282–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Victora C.G., Morris S.S., Barros F.C., De Onis M. & Yip R. (1998) The NCHS reference and the growth of breast‐ and bottle‐fed infants. The Journal of Nutrition 128, 1134–1138. [DOI] [PubMed] [Google Scholar]
- Victora C.G., Adair L., Fall C., Hallal P.C., Martorell R., Richter L. et al. (2008) Maternal and child undernutrition: consequences for adult health and human capital. Lancet 371, 340–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward M.J., Lee S.S. & Lipper E.G. (2000) Failure‐to‐thrive is associated with disorganized infant‐mother attachment and unresolved maternal attachment. Infant Mental Health Journal 21, 428–442. [Google Scholar]
- World Bank (2008a) Cambodia data profile. World Developers Indicators Database. Available at: http://web.worldbank.org/ (accessed 14 May 2008).
- World Bank (2008b) Data and Statistics: Country Classification. Available at: http://web.worldbank.org/ (accessed 14 May 2008).
- World Health Organization (WHO) (2005) Guiding Principles for Feeding Non‐Breastfed Children 6–24 Months of Age. World Health Organization: Geneva, Switzerland, 40 pp. [Google Scholar]
- World Health Organization (WHO) (2007) Ten Statistical Highlights in Global Public Health. Available at: http://www.who.int/whosis/whostat2007_10highlights.pdf (accessed 30 May 2008).
- World Health Organization (WHO) (2008a) Indicators for Assessing Infant and Young Child Feeding Practices: Conclusions of a Consensus Meeting Held 6–8 November 2007 in Washington, D.C., USA, Part 1: Definitions. World Health Organization: Geneva, Switzerland, 20 pp. [Google Scholar]
- World Health Organization (WHO) (2008b) Child Growth Standards Frequently Asked Questions. Available at: http://who.int/childgrowth/faqs/en (accessed 14 May 2008).
- World Health Organization (WHO) Multicentre Growth Reference Study Group (2006) WHO Child Growth Standards: Length/Height‐for‐Age, Weight‐for‐Age, Weight‐for‐Length, Weight‐for‐Height and Body Mass Index‐for‐Age: Methods and Development. World Health Organization: Geneva, Switzerland. [Google Scholar]


