Abstract
According to the World Health Organization (WHO), 46% of adult females in Egypt are obese. This research was aimed at documenting obesity trends and identifying the populations most at risk for obesity. Using data from the 1995 and 2005 Egyptian Demographic and Health Surveys a linear model was employed to seek associations between household wealth, urban/rural residence, governorate of residence, employment status, parity and age and increases in body mass index (BMI) among married Egyptian women between the ages of 15–49. Between 1995 and 2005, the mean BMI of women of reproductive age in Egypt increased from 26.31 to 28.52. Although there was an overall trend towards greater obesity between 1995 and 2005, older women residing in rural, poor households became obese at a faster rate than younger women residing in richer, urban households. Studies have shown that household wealth is a key determinant of food consumption patterns. Rising obesity rates among the poor in developed countries are linked to the relatively cheap price of high‐calorie, nutrient‐poor foods. One factor that may be contributing to the rapid increases in obesity among the rural poor in Egypt is the subsidisation of high‐energy, low‐nutritive value foods that form a larger part of the diet of poor, rural populations.
Keywords: maternal obesity, food subsidies, public health interventions, Egypt
Introduction
Overweight status and obesity have been widely associated with an increased risk of disease and mortality (Ezzati et al. 2004). As the Middle East and North African countries have become more affluent and urbanised, obesity has been increasing dramatically, particularly among women. The prevalence of obesity is increasing globally, although the distribution of obesity among and within countries varies widely (Chopra et al. 2002; Mendez et al. 2005; WHO 2007). The biological determinants of obesity are a combination of over‐consumption of calories and lower caloric expenditures (less exercise or physical activity), although more distal factors such as the globalisation of food markets, economic growth and urbanisation have also been linked to the global obesity epidemic (Drewnowski 2003, 2004, 2007; Drewnowski & Specter 2004; Drewnowski & Darmon 2005). Trends towards obese status have also been related to individual‐ and household‐level factors, such as socio‐economic status (SES), that directly influence food consumption patterns (Drewnowski 2003, 2004, 2007; Galal 2003; Drewnowski & Specter 2004; Drewnowski & Darmon 2005; Hawkes 2005, 2006; Craven & Hawks 2006; Candib 2007; Ebrahim et al. 2007; Wang & Beydoun 2007; Wang et al. 2007; Ward et al. 2007).
Literature reviews on the association between SES and obesity have shown that inverse relationships between SES and obese and overweight status were limited to high‐income countries. In contrast, poorer and less developed countries had a positive association between increasing SES and increases in overweight and obese status (Sobal & Stunkard 1989). More recent studies have shown that although this trend continues, the strength of the positive association between increased SES and overweight/obese status in countries with medium and low levels of development has weakened (Mendez et al. 2005; McLaren 2007).
According to the World Health Organization (WHO), 46% of adult females in Egypt are obese. Egypt currently has the fifth highest percentage of obese women over the age of 15 in its population, with only Tonga, Samoa, Cook Islands and Nauru having higher rates of obesity (74.9%, 66.3%, 65.7% and 60.5%, respectively) (WHO 2008). This research is aimed at better understanding the drivers of the obesity epidemic among Egyptian women using two cross‐sectional data series. This study endeavours to identify the populations who bear the greatest burden of obesity in Egypt and to explore the socio‐demographic distribution of the obesity burden among women in Egypt. Identifying populations most at risk for becoming obese may provide policymakers with targeted interventions to combat the future costs of treating obesity‐related morbidities.
Key messages
-
•
Between 1995 and 2005 the mean Body Mass Index (BMI) of women of reproductive age in Egypt increased from 26.31 to 28.52.
-
•
Although there was an overall trend towards greater obesity between 1995 and 2005, older women residing in rural, poor households became obese at a faster rate than younger women residing in richer, urban households.
-
•
One factor that may be contributing to the rapid increases in obesity among the rural poor in Egypt is the subsidization of high‐energy, low‐nutritive value foods that form a larger part of the diet of poor, rural populations.
Data and methods
Data
These analyses utilise the unlinked 1995 and 2005 Egyptian Demographic and Health Survey (EDHS) data. There were different criteria for collecting anthropometric measurements in the two EDHS surveys. In 1995, the anthropometric collection was limited to married mothers between the ages of 15 and 49 who had live birth in the 5 years preceding the survey's interview date. In 2005, anthropometric data were collected for all ever‐married mothers between the ages of 15 and 49, regardless of recent fertility.
In order to have comparable data between the two survey years, the sample was restricted using the following criteria: women who were married at the time of the survey, who had a live birth in the 5 years preceding the interview date (7305 women were excluded from the 2005 data as they had not given births in the 5 years preceding the survey). Only a small number of eligible participants were missing height and weight data for both survey years. Three per cent of the 1995 eligible sample in 1995 and 0.9% of the 2005 eligible sample did not have anthropometric data collected as participants were not home when the EDHS measurer visited (El‐Zanaty et al. 1996; El‐Zanaty & Way 2006). Women who were pregnant at the time of the survey (n = 1340 for both survey years) or who were less than 2 months post‐partum (n = 361) were excluded from these analyses. Twenty‐four women in 1995 and four women in 2005 were deleted because they had unreasonably high body mass index (BMI) scores of 99.8. This resulted in a total sample size of 6432 women for 1995 and 8507 women for 2005.
Measurement of variables
The dependent variable used in this analysis was a continuous variable: BMI. BMI was calculated by dividing the weight in kilograms by the square of the height in meters (kg/m2). Data on height and weight for both survey years were collected using standardised tools and protocols. The measuring boards used for the collection of the height data were specially produced by Shorr Productions for use in survey settings. Weight data were obtained using lightweight, bathroom‐type scales with a digital screen designed and manufactured under the authority of the United Nations Children's Fund (El‐Zanaty et al. 1996; El‐Zanaty & Way 2006).
Age was defined as a continuous variable in the analyses, as the data showed a consistent and strong direct linear relationship between increasing age (in years) and increases in BMI.
The EDHS Wealth Quintiles were used in this analysis to construct a variable to capture household wealth. The Demographic and Health Surveys use a methodology of principal component analysis to weight a variety of indicator variables (such as household possessions and/or number of sleeping rooms in a dwelling). These indicator variables are then standardised, using factor analysis, to calculate coefficient scores. The indicator variables are then summed to produce a household index value. The resulting score is standardised, with a mean of zero and a standard deviation of one. Wealth Quintiles are then created using the distribution of household population (Rutstein & Johnston 2004).
Urban status was coded as ‘1’, and rural status was coded as ‘0’.
The employment variable was initially created as an attempt to proxy caloric expenditure. Women were categorised according to reported employment: unemployed (coded ‘0’), non‐physical labour (coded ‘1’), household/domestic labour (coded ‘2’) and physical labour (coded ‘3’). It was theorised that unemployed women would have the lowest caloric expenditures, while women who were working in physical labour would have the highest caloric expenditures. In 2005, there were no women in category ‘1’ or non‐physical labour. As a result, the categories were collapsed into a dichotomous variable: women who were unemployed (coded ‘0’) and women who were employed (coded ‘1’).
Any level of literacy (coded ‘1’) vs. total illiteracy (coded ‘0’) was used to assess the educational level of the participants.
Finally, as all of the women in the sample selection had given birth in the 5 years preceding the survey, children ever born was grouped into four categories (1, 2, 3 and 4+ children ever born, coded as 1–4, respectively).
Regional differences were considered at the governorate level. Urban governorates were used as the reference group. Coefficients for Lower Egypt, Upper Egypt and the Frontier Governorates are interpreted relative to the urban governorate reference group.
Methodology
Analysis was conducted using the SURVEYMEANS and SURVEYREG procedures in SAS V9 (SAS Institute Inc., Cary, NC, USA) for the descriptive, univariate and multivariate analyses. The EDHS sample was collected using a three‐stage probability sample, based on data from the Egyptian Central Agency for Public Mobilization and Statistics. The SURVEYMEANS and SURVEYREG procedures in SAS V9 are used to adjust for complex survey sample designs, including designs with stratification, clustering and unequal weighting (2004, Deaton 1997). In adjusting for the clustering, stratification and sample weights, the standard errors for the final model are slightly larger than those achieved using the parallel PROC MEANS and PROC REG statements that do not adjust for sampling design, although neither the significance nor the direction of the results changes.
Descriptive statistics were created, and then each of the independent variable was regressed individually on BMI for both 1995 and 2005.
For the final model, the 1995 and 2005 data sets were concatenated. A dummy variable representing the year of the survey was created to assess SES differences in nutritional status between the 2 years (1995 was coded ‘0’ and 2005 was coded ‘1’). The final model included interactions terms to assess whether trends in BMI increase were uniform in 1995 and 2005.
Results
Analysis of the EDHS reveals that between 1995 and 2005, the mean BMI of women of reproductive age in Egypt increased significantly (pooled two‐sample t‐test, P < 0.0001) from 26.31 to 28.52 (El‐Zanaty et al. 1996; El‐Zanaty & Way 2006). It has been argued that increases in BMI are protective in countries where under nutrition is prevalent. In Egypt, this is not the case. Using WHO‐defined cut points for underweight status (BMI < 18.5), there were very few women who fell into the underweight category. (1995: n = 130 or 2% of the total sample; 2005: n = 60 or 0.71% of the total sample). In Egypt's case, increases in BMI are not bringing women into normal weight categories but instead are moving women into the higher risk, overweight and obese WHO‐defined categories. Using the WHO's definition of obesity (BMI ≥ 30), obesity prevalence in Egypt increased from 8.41% to 19.02%, while the population of women who fall into the ‘normal’ weight category (BMI 18.5–24.99) fell from 50% of the population in 1995 to only 29% of the population in 2005. The data suggest that obesity is a substantial health problem for women in Egypt and that the trend is towards even higher levels of obesity, with the most recent 2008 data showing a mean BMI of 29.2 for women between the ages of 15 and 49 (El‐Zanaty & Way 2009).
Perhaps most alarming is the rapidity of the epidemic: population‐based means for BMI have moved significantly into the overweight category (BMI ≥ 25) in the short time span of 10 years. Figure 1 depicts the population distribution of BMI scores for 1995 and 2005. The distribution of BMI scores shift towards higher BMI scores between 1995 and 2005. Additionally, relative to 1995, the BMI distribution scores are significantly farther from the mean, with a higher proportion of women falling into the overweight/obese category in 2005.
Figure 1.
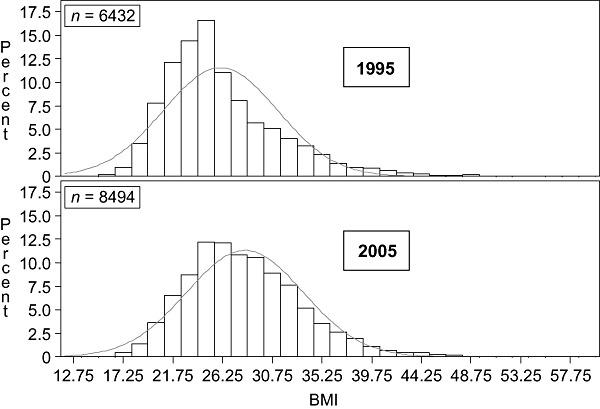
Distribution of maternal BMI in 1995 and 2005 with normal curves. BMI, body mass index.
Descriptive statistics and mean BMI scores were calculated for each of the independent variables. Per cent increases in mean BMI between 1995 and 2005 for each category of the predictor variables were calculated. Table 1 shows the distribution of mean BMI scores, by year, for each of the variables considered in these analyses. Relative to 1995, mean BMI scores are higher in 2005 in every category and, when each year is viewed individually, the trend of increasing BMI appears to be associated with increasing age, wealth, urban residence, literacy, parity and residence in an urban governorate. At the aggregate level, the trends in BMI support the literature, in that greater wealth, urban residence and higher levels of education are associated with higher BMI scores among women in Egypt (Sobal & Stunkard 1989; Monteiro et al. 2004; McLaren 2007).
Table 1.
Distribution of mean BMI by background characteristic 1995 and 2005*
| Characteristic | 1995 | 2005 | ||||
|---|---|---|---|---|---|---|
| n | Mean | SD | n | Mean | SD | |
| Age group | ||||||
| 15–19 | 246 | 24.05 | 4.55 | 307 | 25.47 | 2.22 |
| 20–24 | 1205 | 24.9 | 5.90 | 1835 | 26.83 | 1.04 |
| 25–29 | 1782 | 25.88 | 6.75 | 2560 | 27.94 | 0.96 |
| 30–34 | 1496 | 26.88 | 6.58 | 1874 | 29.32 | 1.04 |
| 35–39 | 1048 | 27.66 | 7.77 | 1277 | 30.05 | 1.33 |
| 40–44 | 486 | 27.84 | 7.50 | 540 | 31.86 | 2.30 |
| 45+ | 169 | 27.15 | 6.50 | 115 | 31.56 | 4.82 |
| Wealth quintile | ||||||
| 1 (lowest) | 1558 | 24.07 | 0.39 | 1988 | 26.78 | 1.19 |
| 2 | 1238 | 25.13 | 5.98 | 1795 | 27.65 | 1.04 |
| 3 | 1288 | 26.09 | 6.10 | 1669 | 28.54 | 1.19 |
| 4 | 1180 | 27.55 | 7.90 | 1602 | 29.76 | 1.26 |
| 5 | 1168 | 28.88 | 8.54 | 1454 | 29.9 | 1.26 |
| Residence | ||||||
| Rural | 3896 | 25.1 | 7.49 | 5242 | 27.85 | 0.74 |
| Urban | 2536 | 27.93 | 9.57 | 3266 | 29.58 | 0.96 |
| Education | ||||||
| Illiterate | 3481 | 25.33 | 7.67 | 3166 | 27.85 | 0.96 |
| Literate | 2951 | 27.38 | 8.69 | 5328 | 28.89 | 0.74 |
| Employment | ||||||
| Unemployed | 5247 | 26.06 | 9.42 | 6888 | 28.48 | 0.74 |
| Employed | 1185 | 26.92 | 7.23 | 1620 | 28.66 | 1.26 |
| Children born in the past 5 years | ||||||
| 1 | 1017 | 25.26 | 6.06 | 1749 | 27.12 | 1.04 |
| 2 | 1245 | 26.29 | 7.76 | 2226 | 28.11 | 1.04 |
| 3 | 1146 | 26.69 | 7.11 | 1839 | 29.04 | 1.19 |
| 4+ | 3024 | 26.55 | 8.80 | 2694 | 29.5 | 1.04 |
| Region | ||||||
| Frontier governorates | 550 | 24.84 | 6.57 | 395 | 31.16 | 2.37 |
| Upper Egypt | 3037 | 24.96 | 11.02 | 4315 | 27.22 | 0.96 |
| Lower Egypt | 1861 | 26.81 | 7.77 | 2469 | 29.16 | 0.96 |
| Urban governorates | 984 | 28.06 | 7.84 | 1329 | 30.18 | 1.41 |
| Total | 6432 | 26.31 | 9.62 | 8508 | 28.52 | 0.59 |
SD, standard deviation; BMI, body mass index. *Married mothers 15–45, 2+ months post‐partum, who had a live birth in the 5 years preceding the survey, adjusted for the sampling design.
Although there are no data for 1995, comparing the 2005 data on women who had, and had not had a live birth yielded some interesting differentials. Women who had not had a live birth in the 5 years preceding the survey were significantly more obese, older, wealthier, literate and rural relative to women who had a live birth in the 5 years preceding the survey (Table 2).
Table 2.
Differentials among women who had given birth/had not given birth* in the 5 years preceding the 2005 Egyptian Demographic and Health Survey
| Characteristic | No births | 1 + Births | P‐value † | Trend ‡ | ||
|---|---|---|---|---|---|---|
| n | % | n | % | |||
| BMI category | ||||||
| Normal/underweight | 936 | 12.81 | 2473 | 29.07% | ||
| Overweight | 2151 | 29.45 | 3192 | 37.52% | ||
| Obese | 4218 | 57.74 | 2843 | 33.42% | <0.0001 | <0.0001 |
| Age | ||||||
| 15–19 | 0 | 0.00 | 307 | 3.61 | ||
| 20–24 | 30 | 0.41 | 1835 | 21.57 | ||
| 25–29 | 283 | 3.87 | 2560 | 30.09 | ||
| 30–34 | 848 | 11.61 | 1874 | 22.03 | ||
| 35–39 | 1635 | 22.38 | 1277 | 15.01 | ||
| 40–44 | 2125 | 29.09 | 540 | 6.35 | ||
| 45–49 | 2384 | 32.64 | 115 | 1.35 | <0.0001 | <0.0001 |
| Wealth quintile | ||||||
| 1 (Lowest) | 1466 | 20.07 | 1988 | 23.37 | ||
| 2 | 1356 | 18.56 | 1795 | 21.10 | ||
| 3 | 1287 | 17.62 | 1669 | 19.62 | ||
| 4 | 1397 | 19.12 | 1602 | 18.83 | ||
| 5 (Highest) | 1799 | 24.63 | 1454 | 17.09 | <0.0001 | <0.0001 |
| Residence | ||||||
| Urban | 3894 | 53.31 | 5242 | 61.61 | ||
| Rural | 3411 | 46.69 | 3266 | 38.39 | <0.0001 | <0.0001 |
| Education | ||||||
| Literate | 3744 | 51.25 | 3166 | 37.21 | ||
| Illiterate | 3548 | 48.57 | 5328 | 62.62 | <0.0001 | <0.0001 |
| Region | ||||||
| Frontier governorates | 290 | 3.97 | 395 | 4.64 | ||
| Upper Egypt | 3015 | 41.27 | 4315 | 50.72 | ||
| Lower Egypt | 2391 | 32.73 | 2469 | 29.02 | ||
| Urban governorates | 1609 | 22.03% | 1329 | 15.62 | <0.0001 | <0.0001 |
| Total | 7305 | 100 | 8508 | 100 | ||
BMI, body mass index. *Women 2+ months post‐partum and who were not pregnant at the time of the interview. †Chi‐Square. ‡Cochran‐Armitage trend test.
Table 3 presents the per cent increases in mean BMI between 1995 and 2005 (using the data in Table 1). When stratified by age, mean BMI increased by over 16% among women over the age of 45 between 1995 and 2005, whereas it increased by only 6% among women under the age of 20. Further desegregation shows that mean BMI scores had higher ratios of increase among poor, rural, illiterate women who were unemployed and who had higher parities. The descriptive statistics present a marked increase in BMI among the entire population between 1995 and 2005, with higher increases found among older, poorer, illiterate, rural women with four or more children who reside in the Frontier Governorates. Viewed independently, increased BMI was significantly associated with increases in wealth, parity, literacy and urban status in both 1995 and 2005. Despite this, the increases in obesity between 1995 and 2005 were not uniform. While earlier studies (Sobal & Stunkard 1989; McLaren 2007) have shown that obesity in developing countries was concentrated among high SES populations, the burden of obesity in Egypt appears to be increasing more rapidly among older, poorer and rural populations.
Table 3.
Per cent increase in mean BMI between 1995 and 2005 by background characteristic*
| Characteristic | Difference | % Increase |
|---|---|---|
| Age group | ||
| 15–19 | 1.42 | 5.90 |
| 20–24 | 1.93 | 7.75 |
| 25–29 | 2.06 | 7.96 |
| 30–34 | 2.44 | 9.08 |
| 35–39 | 2.39 | 8.64 |
| 40–44 | 4.02 | 14.44 |
| 45+ | 4.41 | 16.24 |
| Wealth quintile | ||
| 1 (lowest) | 2.71 | 11.26 |
| 2 | 2.52 | 10.03 |
| 3 | 2.45 | 9.39 |
| 4 | 2.21 | 8.02 |
| 5 | 1.02 | 3.53 |
| Residence | ||
| Rural | 2.75 | 10.96 |
| Urban | 1.65 | 5.91 |
| Education | ||
| Illiterate | 2.52 | 9.95 |
| Literate | 1.51 | 5.51 |
| Employment | ||
| Unemployed | 2.42 | 9.29 |
| Employed | 1.74 | 6.46 |
| Children born in the past 5 years | ||
| 1 | 1.86 | 7.36 |
| 2 | 1.82 | 6.92 |
| 3 | 2.35 | 8.80 |
| 4+ | 2.95 | 11.11 |
| Region | ||
| Frontier governorates | 6.32 | 25.44 |
| Upper Egypt | 2.26 | 9.05 |
| Lower Egypt | 2.35 | 8.75 |
| Urban governorates | 2.12 | 7.54 |
| Total | 2.21 | 8.40 |
BMI, body mass index. *Married mothers 15–45, 2+ months post‐partum, who had a live birth in the 5 years preceding the survey, adjusted for the sampling design.
In Table 4, each of the variables was regressed individually on BMI for 1995 and 2005. Comparing 2005 with 1995 (Table 4), the unadjusted associations between increasing wealth and employed status and increased BMI scores were not as strong in 2005 when compared with 1995. Additionally, residence in the Frontier Governorates was significantly associated with lower BMI scores in 1995 and higher BMI scores in 2005 when compared with the other governorates.
Table 4.
Univariate analysis of the association between individual predictor variables and BMI by year*
| Predictor variables | 1995 | 2005 | ||||
|---|---|---|---|---|---|---|
| Estimate | SE | P‐value | Estimate | SE | P‐value | |
| Age | 0.17 | 0.01 | <0.0001 | 0.24 | 0.01 | <0.0001 |
| Wealth quintile | ||||||
| 1 (lowest) | −4.80 | 0.29 | <0.0001 | −3.11 | 0.23 | <0.0001 |
| 2 | −3.75 | 0.30 | <0.0001 | −2.25 | 0.21 | <0.0001 |
| 3 | −2.79 | 0.29 | <0.0001 | −1.4 | 0.23 | <0.0001 |
| 4 | −1.33 | 0.32 | <0.0001 | −0.2 | 0.23 | 0.3888 |
| 5 (ref) | 0 | 0 | 0 | |||
| Literacy | 2.05 | 0.19 | <0.0001 | 1.01 | 0.015 | <0.0001 |
| Births in past 5 years | ||||||
| 1 | −1.30 | 0.23 | <0.0001 | −2.34 | 0.18 | <0.0001 |
| 2 | −0.26 | 0.24 | 0.2723 | −1.36 | 0.18 | <0.0001 |
| 3 | 0.14 | 0.22 | 0.5352 | −0.46 | 0.19 | 0.0180 |
| 4+ (ref) | 0 | 0 | ||||
| Urban residence | 2.82 | 0.22 | <0.0001 | 1.72 | 1.56 | <0.0001 |
| Employment | 0.76 | 0.21 | 0.0004 | 0.17 | 0.18 | 0.3513 |
| Region | ||||||
| Urban governorate | 3.22 | 0.38 | <0.0001 | −0.98 | 0.37 | 0.0074 |
| Lower Egypt | 1.97 | 0.33 | <0.0001 | −1.98 | 0.34 | <0.0001 |
| Upper Egypt | 0.12 | 0.35 | 0.7239 | −3.94 | 0.34 | <0.0001 |
| Frontier governorates (ref) | 0 | 0 | ||||
BMI, body mass index; SE, standard error. *Married mothers 15–45, 2+ months post‐partum, who had a live birth in the 5 years preceding the survey, adjusted for the sampling design.
In the adjusted models (Table 5), Model 1 shows that controlling for age, wealth, literacy, parity, employment status and residence, women in 2005 had significantly higher BMIs than women in 1995. The coefficient for year in Model 1 (2.36) is very similar to the 2.38 increase in mean BMI found in the descriptive statistics. Model 2, which includes the interaction terms, shows that although overall BMI increased among older, wealthier, urban women who were literate, unemployed, had higher parities and resided in the urban governorates, the increases were not universal. BMI increased significantly less (but still increased) between 1995 and 2005 for those in urban areas (relative to rural areas) and those who possess more wealth. Adding up the total effects: 1.30 (urban residence) minus 0.03 on the year 2005 and subtracting 0.73 on the urban*year interaction term means that on average (conditional on everything else), the BMI increased by only 0.51 in urban areas in 2005, whereas in 1995, the effect of urban residence was 1.30. Similarly, when comparing the poorest to the wealthiest, the total 2005 effect is positive (adjusted coefficient = 0.46), whereas in 1995, the effect was negative (adjusted coefficient = −1.23). While poverty was associated with lower levels of BMI in 1995, by 2005, being in the lowest wealth quintile compared with the wealthiest quintile was significantly associated with increases in BMI. The starkest increases in BMI between 1995 and 2005 were found in the Frontier Governorates. Exploring the SES differentials between 1995 and 2005 in the Frontier Governorate shows (Table 6) no significant differences in education, urban residence, employment status or parity. Despite this, women in 2005 who resided in the Frontier Governorates were significantly older and wealthier than their 1995 counterparts. This older and wealthier population residing in the Frontier Governorate in 2005 had significantly higher BMI scores relative to the 1995 population. In 1995, residence in the Frontier Governorates was associated with lower BMI (adjusted coefficient −2.16); by 2005, residence in the Frontier Governorates had a positive net effect on BMI (adjusted coefficient 1.52) (Table 5). In sum, Model 2 in Table 5 shows that while BMI is increasing for everyone, it is increasing significantly more quickly for poor, rural women residing in the Frontier Governorates.
Table 5.
Adjusted linear regression models modelling maternal BMI as a continuous variable †
| Parameter | Model 1 | Model 2 | ||||
|---|---|---|---|---|---|---|
| Estimate | SE | P‐value | Estimate | SE | P‐value | |
| Intercept | 22.82 | 0.45 | <0.0001 | 24.18 | 0.58 | <0.0001 |
| Age | 0.16 | 0.01 | <0.0001 | 0.12 | 0.01 | <0.0001 |
| Wealth quintile | ||||||
| 1 (Lowest) | −2.37 | 0.23 | <0.0001 | −3.37 | 0.33 | <0.0001 |
| 2 | −1.70 | 0.21 | <0.0001 | −2.68 | 0.31 | <0.0001 |
| 3 | −1.14 | 0.20 | <0.0001 | −1.99 | 0.30 | <0.0001 |
| 4 | −0.28 | 0.20 | 0.1586 | −0.93 | 0.33 | 0.0045 |
| 5 (Highest) (ref) | 0.00 | 0.00 | . | 0.00 | 0.00 | . |
| Urban | 0.86 | 0.18 | <0.0001 | 1.30 | 0.27 | <0.0001 |
| Region | ||||||
| Frontier Governorates | 0.20 | 0.37 | 0.5819 | −2.16 | 0.41 | <0.0001 |
| Upper Egypt | −1.25 | 0.23 | <0.0001 | −0.68 | 0.37 | 0.0691 |
| Lower Egypt | 0.36 | 0.22 | 0.1066 | 0.84 | 0.36 | 0.0197 |
| Urban Governorates (ref) | 0.00 | 0.00 | . | 0.00 | 0.00 | . |
| Literacy | 0.50 | 0.12 | <0.0001 | 0.44 | 0.12 | 0.0002 |
| Births | ||||||
| 1 | −1.18 | 0.18 | <0.0001 | −1.16 | 0.18 | <0.0001 |
| 2 | −0.72 | 0.16 | <0.0001 | −0.74 | 0.16 | <0.0001 |
| 3 | −0.30 | 0.15 | 0.045 | −0.36 | 0.15 | 0.0163 |
| 4+ (ref) | 0.00 | 0.00 | . | 0.00 | 0.00 | . |
| Employment | −0.43 | 0.13 | 0.0009 | −0.49 | 0.13 | 0.0001 |
| Year | ||||||
| 1995 | 2.36 | 0.13 | <0.0001 | 0.00 | 0.00 | . |
| 2005 | −0.03 | 0.66 | 0.9677 | |||
| Age*year | 0.07 | 0.02 | <0.0001 | |||
| Year*wealth quintile | ||||||
| Year*1 | 1.72 | 0.43 | <0.0001 | |||
| Year*2 | 1.65 | 0.41 | <0.0001 | |||
| Year*3 | 1.47 | 0.39 | 0.0002 | |||
| Year*4 | 1.15 | 0.40 | 0.0043 | |||
| Year*5 (ref) | 0.00 | 0.00 | . | |||
| Urban*year | −0.76 | 0.35 | 0.03 | |||
| Region*year | ||||||
| Year*frontier governorates | 3.71 | 0.55 | <0.0001 | |||
| Year*upper Egypt | −0.97 | 0.46 | 0.0346 | |||
| Year*lower Egypt | −0.78 | 0.44 | 0.0771 | |||
| Year*Urban governorates (ref) | 0.00 | 0.00 | . | |||
| R2 = 0.20 F‐Test P < 0.0001 | R2 = 0.21 F‐Test P < 0.0001 | |||||
BMI, body mass index. †Married mothers 15–45, 2+ months post‐partum, who had a live birth in the 5 years preceding the survey, adjusted for the sampling design.
Table 6.
Differentials in the frontier governorate samples 1995 and 2005
| 1995 | 2005 | ||
|---|---|---|---|
| (n = 550) | (n = 395) | ||
| Mean age* | 29.91 | 30.8 | 0.034 |
| % in wealth quintile † | |||
| 1 (Lowest) | 21.09% | 28.35% | |
| 2 | 6.55% | 16.71% | |
| 3 | 21.09% | 15.44% | |
| 4 | 29.09% | 15.95% | |
| 5 (Highest) | 22.18% | 23.54% | <0.0001 |
| Percent urban † | 60.00% | 60.00% | 0.8216 |
| Percent literate † | 60.18% | 64.81% | 0.1480 |
| Births † | |||
| 1 | 17.82% | 15.95% | |
| 2 | 22.73% | 20.25% | |
| 3 | 18.36% | 23.29% | |
| 4+ (ref) | 41.09% | 40.51% | 0.2756 |
| Percent employed † | 24.91% | 21.52% | 0.2253 |
*Paired t‐test. †Chi‐square test.
Discussion
Egypt currently faces an epidemic of obesity among women of reproductive age. The fact that the population mean BMI has shifted significantly upwards in the short period of 10 years is alarming, particularly in light of the ill‐health outcomes associated with overweight status and obesity. While the entire population of women of reproductive age is shifting towards higher BMI scores, populations that may be more vulnerable, such as older, poor, rural populations residing in the Frontier Governorates appear to be at higher risk of becoming overweight and obese, when compared with their wealthier, younger and urban counterparts.
Increasing age, as well as obesity, is associated with the risk of non‐communicable disease (Ezzati et al. 2004). Non‐communicable disease risk is increased by poverty and rural residence as those may play a role in an individual's ability to access health care services, either because of lack of funds or to limited proximity to services. The combination of these factors may result in excessive non‐communicable disease burden among already at‐risk groups. Given the projected costs of treating obesity‐related disorders, Egypt is faced with a looming economic burden.
Globally, the vast majority of obesity interventions have been targeted at treating the individual, although most experts agree that environmental factors are driving the obesity epidemic (Jain 2005; Swinburn and Egger 2002). In his 1985 paper, Geoffrey Rose advocated a population‐based approach, rather than an individual approach to improving health (Rose 1985). Twenty years later, Doyle et al. found that while individual and population‐based approaches to health are both needed, population‐based approaches that change norms are more effective in protecting the most vulnerable populations (Doyle et al. 2006). For example, surgery has been found to be an effective treatment of severe obesity in individuals, but drug treatments and lifestyle interventions have not yielded clinically significant permanent weight loss results (Jain 2005; Swinburn and Egger 2002). In light of this, public health interventions aimed at curbing obesity must be broad‐based and incorporate macro‐level factors such as food prices and availability that may ultimately be influencing caloric consumption (Popkin 2009).
One of the main causes of obesity is caloric over‐consumption. Several studies in the United States have found that the relatively inexpensive price of high‐calorie foods has contributed to the higher rates of obesity among the poor, whose dietary choices are often constrained by price (Drewnowski 2003, 2004, 2007; Drewnowski & Specter 2004; Drewnowski & Darmon 2005; Powell & Chaloupka 2009; Drewnowski 2009). It has also been suggested that the food stamp programme in the United States has contributed to obesity among the poor through the subsidisation of high‐calorie, low‐nutritive foods (Zagorsky & Smith 2009). Drewnowski (2007, page 160) argues that ‘obesity has been linked repeatedly to consumption of low‐cost foods. . . . The fact that energy‐dense foods (megajoules/kilogram) cost less per megajoule than do nutrient‐dense foods means that energy‐dense diets are not only cheaper but may be preferentially selected by the lower income consumer. The low cost of dietary energy (dollars/megajoule), rather than specific food, beverage, or macronutrient choices, may be the main predictor of population weight gain’ (Drewnowski 2007). Empirical evidence from Egypt supports the association between the food subsidy system and the prevalence of obesity. Asfaw (2007a) found that maternal BMI was inversely related to the price of subsidised foods. Afsaw's analysis, based on the 1997 International Food Policy Research Institute (IFPRI) Egyptian Integrated household survey, suggests that the current food subsidy system contributes to the current obesity epidemic by lowering the direct costs of becoming obese (Asfaw 2007a).
Results from a 1997 International Food Policy Research Institute study found that subsidised foods accounted for over 30% of the overall per capita calorie availability in Egypt (Adams 2000). Although subsidised foods contributed a slightly lower percentage to overall calorie availability in rural Egypt (31.6% vs. 33.8% for urban areas), the total number of subsidised calories was slightly higher in rural areas. Additionally, the contribution of subsidised calories decreased with increasing wealth. People from both urban and rural areas from lower expenditure quintiles received a higher proportion of their calories from subsidised foods.
Perhaps contributing to the unequal distribution of subsidised calories, the per capita distribution of subsidised foods is also unequally distributed. For example, in 1997, the per capita number of bakeries producing the subsidised baladi bread was much higher in the Frontier Governorates (55 per 100 000 population) than in urban areas (23 per 100 000 population). Additionally, rural, Frontier Governorates had some of the highest per capita distribution of subsidised cooking oils and sugar (in kg per person) (Ahmed et al. 2001).
In recent years, there has been a marked increase in the average Egyptian's caloric consumption. Between 1990–1992 and 2000–2002, the estimates of food consumption (kcal/person/day) rose from 3090 calories to 3230 (FAO 2011). Based on 7716 kcal/kg, this daily increase of 140 kcal/person/day results in an average weight gain of 6.62 kg/person/year. It is important to note that the per capita availability of calories in Egypt is quite high, even among the poorest sectors of its population, relative to other parts of the world. Table 7 presents global and regional comparisons of per capita food consumption (WHO). In spite of this, anaemia rates among Egyptian women increased from 28% in 2000 to 39% in 2005 (El‐Zanaty & Way 2001, 2006). One factor that may be driving the overall increase in caloric consumption and concurrent declines in micronutrient nutritional status may be the Egyptian food subsidy system that experienced marked changes between 1995 and 2005.
Table 7.
Global and regional per capita food consumption (calories per capita per day) 1997–1999
| Region | Per capita kcal |
|---|---|
| World | 2803 |
| Developing countries | 2681 |
| Near East and North Africa | 3006 |
| Sub‐Saharan Africa | 2195 |
| Latin America and the Caribbean | 2824 |
| East Asia | 2921 |
| South Asia | 2403 |
| Industrialised countries | 3380 |
| Transition countries | 2906 |
The current food subsidy system in Egypt has its roots in World War II rationing programmes. In order to provide the Egyptian population with essentials, food, as well as other products, was rationed. The entire Egyptian population benefited from the ration system; it was not aimed at targeting the poor. Developed in 1941, the ration system has evolved into the current‐day Egyptian food subsidy system. Food subsidy costs in Egypt remained relatively low until the 1970s when the system expanded to include additional foods such as frozen meat, chicken and fish as well as beans and lentils. As a result of these changes, food subsidies accounted for almost 17% of the total government expenditures by 1975. By the 1980s, over 18 foods were subsidised and available in monthly rations to any Egyptian who had a ration card, providing almost universal subsidies in Egypt (Ahmed et al. 2001).
In 1981, a systematic reduction in food subsidies started. Under the Mubarak government, there was also a reduction in the number and variety of subsidised goods. Meat, fish, chicken and other foods were removed from the subsidy system between 1990 and 1992, and subsidies on Fino (Fino bread is made from flour milled at a 72% extraction rate) bread and 76% extraction flour for Shami bread were eliminated in 1992 and 1996. Since 1996, only four food commodities have been subsidised: Baladi bread (coarse brown loaf milled at a 82% extraction rate), unfortified wheat flour, edible oils and sugar (Adams 2000; Ahmed et al. 2001).
Nutritionally related health patterns in the Middle East and Egypt have changed significantly during the last two decades. Egypt has evolved from a country with high levels of undernutrition to a country that currently has a high dietary surplus. The Egyptian food subsidy programme, which lowers the relative prices of energy‐dense, nutrient‐poor food items, may be one of the contributors to the co‐emergence of overweight/obese and micronutrient‐deficient mothers in the country (Galal 2003; Asfaw 2007b). There have been several studies focused on policy recommendations for the Egyptian food subsidy system (Gutner 1999; Adams 2000; Ahmed et al. 2001). These policies have been aimed at targeting food subsidies towards the neediest populations and reducing waste and leakage. Focusing the food subsidy system so that it efficiently targets the neediest population is crucial, but examining the nutritional quality of the foods being subsidised would also protect vulnerable populations from nutritional declines. Subsidising nutritive, low‐energy foods instead of oil, sugar and unfortified wheat products may be one intervention that would impact household food consumption patterns, particularly among populations whose dietary choices and options are shaped by financial constraints.
The role of food prices should be evaluated in light of the uneven distribution of the trends towards obese status. Poor and rural populations receive a high proportion of their caloric intake from the energy‐dense, micronutrient‐poor foods provided by the Egyptian food subsidy system, and the per capita distribution of subsidised foods is highest among the Frontier Governorates. Increasing the quality of subsidised foods may minimise the proportion of the Egyptian diet that is based on energy‐dense food sources and expand the consumption of fruits, vegetables and proteins.
Study limitations
While overall caloric consumption has increased in recent years, the composition of those calories has changed a little in the same period (FAO 2011). Unfortunately, the Food and Agriculture Organization does not provide any disaggregated data on the distribution of calories consumed, nor the distribution of the type of food groups that constitute those calories. It is not possible to discern whether the increase in calories has been universal in Egypt. It is also impossible to determine from this data whether all segments of the Egyptian population have experienced consistent changes in the distribution of their dietary composition.
Although this study did not address the quality of the excess calories that are driving the obesity trend in Egypt, other studies have shown that overweight and obese status is not necessarily indicative of quality nutrition. Using the IFPRI 1997 Egyptian Integrated Household survey, Afsaw (Asfaw 2007b) found that the odds of being overweight /obese are 81% higher for micronutrient‐deficient mothers compared to non‐deficient mothers. The 1995 EDHS provides no information on the prevalence of micronutrient deficiencies, but the 2005 survey presents a high level of anaemia (40%) among women of reproductive age, pointing to some level of micronutrient deficiency. There is very little data on the joint effects of micronutrient malnutrition and obesity or the extent to which obesity as a risk factor for non‐communicable disease is modified by micronutrient malnutrition. This is an area for further research.
The exceptionally large increase in mean BMI among the Frontier Governorates is puzzling. There were no significant differences in urban/rural residence, literacy rates or in parity between 1995 and 2005 samples. The only significant difference found in the Frontier Governorates between 1995 and 2005 was that there were distributional differences in wealth quintiles and that women in 2005 were significantly older (Table 6).
Additionally, there was selection bias. The EDHS studies only collected data for married or ever‐married women, although marriage is nearly universal in Egypt. Only 1.7% of women aged 45–49 have never been married (El‐Zanaty & Way 2006). Additionally, only women who had given birth in the 5 years preceding the interview date were anthropometrically measured. When restricting the analysis to the 2005 data and comparing women who had and had not had a birth in the 5 years preceding the survey date, it appears that the sample used in this analysis presents an underestimate of the rates of obesity (Table 2). Because of data limitations, it is impossible to discern whether this is also the situation with the 1995 data.
This study did not have access to any information on the actual consumption of calories nor was there any information available on the activity levels among women in this population. While this study endeavoured to look at the environmental factors that may be contributing to the epidemic of obesity in Egypt, the fact that this data analysed cross‐sectional data means that it is impossible to infer causality between the predictors and the obesity trends in Egypt.
Source of funding
No institutional or departmental funding was provided for this research.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
AMA designed and conducted the research, analyzed the data and wrote the paper. WWF and AGH assisted in writing the paper, selecting the variables and advising during the research development. All authors read and approved the final manuscript.
Acknowledgements
The authors would like to thank Dr. David Canning for thoughtful comments.
References
- Adams R.H. (2000) Self‐targeted subsidies: the distributional impact of the Egyptian food subsidy system. Economic Development and Cultural Change 49, 115–136. [Google Scholar]
- Ahmed A.U., Bouis H., Gutner T. & Lofgren H. (2001) The Egyptian Food Subsidy System: Structure, Performance, and Options for Reform. Research Report 119. International Food Policy Research Institute: Washington, DC. [DOI] [PubMed] [Google Scholar]
- Asfaw A. (2007a) Do government food price policies affect the prevalence of obesity? Empirical evidence from Egypt. World Development 35, 687–701. [Google Scholar]
- Asfaw A. (2007b) Micronutrient deficiency and the prevalence of mothers' overweight/obesity in Egypt. Economics and Human Biology 5, 471–483. [DOI] [PubMed] [Google Scholar]
- Candib L.M. (2007) Obesity and diabetes in vulnerable populations: reflection on proximal and distal causes. Annals of Family Medicine 5, 547–556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chopra M., Galbraith S. & Darnton‐Hill I. (2002) A global response to a global problem: the epidemic of overnutrition. Bulletin of the World Health Organization 80, 952–958. [PMC free article] [PubMed] [Google Scholar]
- Craven K.L. & Hawks S.R. (2006) Cultural and western influences on the nutrition transition in Thailand. Promotion & Education 13, 14–20. [PubMed] [Google Scholar]
- Deaton A. (1997) The Analysis of Household Surveys: A Microeconometric Approach to Development Policy. Johns Hopkins University Press: Baltimore, MD. [Google Scholar]
- Doyle Y.G., Furey A. & Flowers J. (2006) Sick individuals and sick populations: 20 years later. Journal of Epidemiology and Community Health 60, 396–398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drewnowski A. (2003) Fat and sugar: an economic analysis. The Journal of Nutrition 133, 838S–840S. [DOI] [PubMed] [Google Scholar]
- Drewnowski A. (2004) Obesity and the food environment: dietary energy density and diet costs. American Journal of Preventive Medicine 27, 154–162. [DOI] [PubMed] [Google Scholar]
- Drewnowski A. (2007) The real contribution of added sugars and fats to obesity. Epidemiologic Reviews 29, 160–171. [DOI] [PubMed] [Google Scholar]
- Drewnowski A. (2009) Obesity, diets, and social inequalities. Nutrition Reviews 67 (Suppl. 1), S36–S39. [DOI] [PubMed] [Google Scholar]
- Drewnowski A. & Darmon N. (2005) The economics of obesity: dietary energy density and energy cost. The American Journal of Clinical Nutrition 82, 265S–273S. [DOI] [PubMed] [Google Scholar]
- Drewnowski A. & Specter S.E. (2004) Poverty and obesity: the role of energy density and energy costs. The American Journal of Clinical Nutrition 79, 6–16. [DOI] [PubMed] [Google Scholar]
- Ebrahim S., Garcia J., Sujudi A. & Atrash H. (2007) Globalization of behavioral risks needs faster diffusion of interventions. Preventing Chronic Disease 4, A32. [PMC free article] [PubMed] [Google Scholar]
- El‐Zanaty F. & Way A.A. (2001) Egypt Demographic and Health Survey 2000. Ministry of Health and Population [Egypt], National Population Council and ORC Macro: Calverton, MD. [Google Scholar]
- El‐Zanaty F. & Way A.A. (2006) Egypt Demographic and Health Survey 2005. Ministry of Health and Population, National Population Council, El‐Zanaty and Associates, and ORC Macro: Cairo. [Google Scholar]
- El‐Zanaty F. & Way A.A. (2009) Egypt Demographic and Health Survey 2008. Ministry of Health, El‐Zanaty and Associates, and Macro International: Cairo. [Google Scholar]
- El‐Zanaty F., Hussein E.M., Shawky G.S., Way A.A. & Kishor S. (1996) Egypt Demographic and Health Survey 1995. National Population Council [Egypt] and Macro International Inc: Calverton, MD. [Google Scholar]
- Ezzati M., Vanderhoorn S., Rodgers A., Lopez A.D., Mathers C.D. & Murray C.J.L. (2004) Potential health gains from reducing multiple risk factors In: Comparative Quantification of Health Risks: Global and Regional Burden of Disease Attributable to Selected Risk Factors (eds Ezzati M., Lopez A.D., Rodgers A. & Murray C.J.L.), pp 2167–2190. World Health Organization: Geneva. [Google Scholar]
- FAO (2011) Food Security Statistics. Available at: http://www.fao.org/fileadmin/templates/ess/documents/food_security_statistics/FoodConsumptionNutrients_en.xls. [Google Scholar]
- Galal O. (2003) Nutrition‐related health patterns in the Middle East. Asia Pacific Journal of Clinical Nutrition 12, 337–343. [PubMed] [Google Scholar]
- Gutner T. (1999) The Political Economy of Food Subsidy Reform in Egypt. International Food Policy Research Institute: Washington D.C. Available at: http://www.ifpri.org/sites/default/files/pubs/divs/fcnd/dp/papers/dp77.pdf. [Google Scholar]
- Hawkes C. (2005) The role of foreign direct investment in the nutrition transition. Public Health Nutrition 8, 357–365. [DOI] [PubMed] [Google Scholar]
- Hawkes C. (2006) Uneven dietary development: linking the policies and processes of globalization with the nutrition transition, obesity and diet‐related chronic diseases. Globalization and Health 2, 4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jain A. (2005) Treating obesity in individuals and population. BMJ (CLINICAL RESEARCH ED.) 331, 1387–1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaren L. (2007) Socioeconomic status and obesity. Epidemiologic Reviews 29, 29–48. [DOI] [PubMed] [Google Scholar]
- Mendez M.A., Monteiro C.A. & Popkin B.M. (2005) Overweight exceeds underweight among women in most developing countries. The American Journal of Clinical Nutrition 81, 714–721. [DOI] [PubMed] [Google Scholar]
- Monteiro C.A., Moura E.C., Conde W.L. & Popkin B.M. (2004) Socioeconomic status and obesity in adult populations of developing countries: a review. Bulletin of the World Health Organization 82, 940–946. [PMC free article] [PubMed] [Google Scholar]
- Popkin B.M. (2009) What can public health nutritionists do to curb the epidemic of nutrition‐related noncommunicable disease? Nutrition Reviews 67 (Suppl. 1), S79–S82. [DOI] [PubMed] [Google Scholar]
- Powell L.M. & Chaloupka F.J. (2009) Food prices and obesity: evidence and policy implications for taxes and subsidies. The Milbank Quarterly 87, 229–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose G. (1985) Sick individuals and sick populations. International Journal of Epidemiology 14, 32–38. [DOI] [PubMed] [Google Scholar]
- Rutstein S.O. & Johnston C.H. (2004) The DHS Wealth Index. DHS Comparative Reports No. 6. ORC Macro: Calverton, MD. [Google Scholar]
- Sobal J. & Stunkard A. (1989) Socioeconomic status and obesity: a review of the literature. Psychological Bulletin 105, 260–275. [DOI] [PubMed] [Google Scholar]
- Swinburn B. & Egger G. (2002) Preventive strategies against weight gain and obesity. Obesity Reviews 3, 289–301. [DOI] [PubMed] [Google Scholar]
- Wang Y. & Beydoun M.A. (2007) The obesity epidemic in the United States – gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta‐regression analysis. Epidemiologic Reviews 29, 6–28. [DOI] [PubMed] [Google Scholar]
- Wang M.C., Kim S., Gonzalez A.A., Macleod K.E. & Winkleby M.A. (2007) Socioeconomic and food‐related physical characteristics of the neighbourhood environment are associated with body mass index. Journal of Epidemiology and Community Health 61, 491–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ward H., Tarasuk V. & Mendelson R. (2007) Socioeconomic patterns of obesity in Canada: modeling the role of health behaviour. Applied Physiology, Nutrition, and Metabolism 32, 206–216. [DOI] [PubMed] [Google Scholar]
- WHO (2007) WHO Statistical Information System (WHOSIS). Available at: http://www.who.int/whosis/whostat2007.pdf.
- WHO (2008) WHO Statistical Information System (WHOSIS) WHO. Available at: http://www.who.int/whosis/whostat/EN_WHS08_Full.pdf.
- Zagorsky J.L. & Smith P.K. (2009) Does the U.S. Food Stamp Program contribute to adult weight gain? Economics and Human Biology 7, 246–258. [DOI] [PubMed] [Google Scholar]


