Abstract
This paper provides an overview of the current knowledge relating to the nutritional requirements and corresponding recommended nutrient intake values of children and adolescents for micronutrients and specificities related to these requirements in the course of childhood and adolescence in Europe. Aspects that can influence micronutrient requirements, such as physiological requirements and bioavailability of the nutrients in the organism, are discussed. The methodology used to obtain the data and also the main knowledge gaps regarding these concepts are emphasized. Methodological critical points in achieving the data and physiological aspects of children and adolescents are important in order to standardize the reference values for micronutrients among Europe for these stages of life.
Keywords: children, adolescents, micronutrient, requirement, growth, development, Europe and EURRECA
Background
Childhood can be considered to extend from 1 year of age to the beginning of adolescence. Early childhood (1–5 years) is an extremely sensitive period to the presence of appropriate nutrition (Rai & Larson 2009) and can be considered as a vulnerable population group. Adolescence is a time of dramatic change as the relatively uniform growth of childhood is suddenly altered by an increase in growth velocity. Changes in growth are linked with hormonal, cognitive and emotional features (Rickert 1996). In addition to the nutritional demand of growth and development, changes in lifestyle and food habits may also justify special nutrient needs, e.g. for those who participate in sports, become pregnant, diet excessively or consume alcohol and drugs (Rickert 1996). Research has indicated that inadequate intake of various nutrients may cause impaired or accelerated growth affecting overall health (Suskind 2009). Adequate nutrition during this vulnerable period of life is therefore important to support general health during adulthood (Serra‐Majem & Aranceta 2004). There exists a significant knowledge gap on the relation among nutrient intake, nutrient status and various health outcomes related to growth and development.
Monitoring intakes and reference values in population groups can help to assure an adequate health status in the present and in the future. However, important limitations exist with respect to deriving adequate reference values for nutrient intakes for children and adolescents because of a lack of consensus in definitions for population groups across Europe. Reference intakes values for children and adolescents are estimated by extrapolation from data established for adults and for young infants. Usually, they are based on body weight or body surface area, or on observed nutrient intakes of groups of children and adolescents in apparently good health (Koletzko 2008a). When they are based on body weight or on body surface area, differences in substrate absorption, metabolism, deposition in tissues during growth and renal or other excretion may affect the tolerable upper level (UL) of nutrient intakes. The extrapolation made from adults and for young infants does not have a scientifically valid basis and may lead to inappropriate values, as was recently emphasized by the Scientific Committee on Food of the European Commission with respect to extrapolation of UL (Koletzko 2008a).
Unfortunately, only a few food consumption surveys have been performed among children and adolescents to enable more direct assessment of recommended values for nutrient intake. With this approach, it is assumed that the children in these surveys are healthy and are achieving their full genetic potential, and that their diets are appropriate and free from adverse long‐term effects, which is difficult to assume with a cross‐sectional design (Koletzko 2008b).
The European Society for Paediatric Gastroenterology, Hepatology and Nutrition (ESPGHAN) Committee on Nutrition, which is an European professional and scientific body that seeks to influence the standards of medical care for patients and their families, also stated that the reference nutrient intakes ‘are designed for specialists and must be interpreted carefully’ (Aggett et al. 1997). Therefore, intake recommended values for every micronutrient are established for nutrition experts, but medical interpretation should be individualized. Given these limitations, reference values established by various expert committees (e.g. German Nutrition Society, Austrian Nutrition Society, Swiss Society for Nutrition Research, Swiss Nutrition Association) can only provide some first guidance on an appropriate supply for a child, taking into account that the needs of the individual may greatly differ from these reference intakes (Koletzko 2008a).
In order to establish micronutrient recommendations, a range of intakes between what is clearly inadequate leading to clinical deficiency and what is in excess leading to signs of toxicity had to be taken into account. Between these two extremes, there is a level of intake that is adequate for normal health and the maintenance of metabolic integrity, and a series of more precisely definable levels of intake that are adequate to meet specific criterion and may be used to determine requirements and appropriate levels of intake (Prentice et al. 2004; Bender 2008).
The EURopean RECcommendations Aligned (EURRECA) European Network of Excellence (Ashwell et al. 2008) attempts to consolidate the basis for the definition of micronutrient requirements across Europe with special focus on vulnerable groups. Diverse national recommendations across Europe are confusing for policy‐makers, health professionals, industry and consumers. Difficulties also arise when attempts are made to compare reference values across Europe, as population segmentation differs between countries (Ortega, 2004; Ashwell et al. 2008). For example, the number of age categories that relate to childhood and adolescence varies between four and six, with different age cut‐off points being used by different European countries (Doets et al., 2008a). The EURRECA network will review the micronutrient recommendations for children and adolescents and the methodological approaches that were used throughout Europe in order to achieve their harmonization.
This paper provides an overview on the current knowledge of the nutritional requirements of children and adolescents for micronutrients with specificities, methodologies and limitations related to the criterion used to determine and apply them in Europe.
Key messages
-
•
Childhood and adolescence are nutritional critical points due to rapid growth and development.
-
•
Data on methods to obtain micronutrient reference values in children and adolescents are often scarce and moreover they usually have important limitations. Most of the time, they are extrapolated from infants and adult data.
-
•
High disparity in micronutrient reference values in childhood and adolescence exists among European countries and committees.
Methods used for establishing dietary reference values
Factors modifying nutritional recommendations
Physiological requirement
During childhood, the velocity of growth slows down considerably compared with infancy. Excluding the first year of life, the largest peak of growth is observed during adolescence. Childhood and adolescence are characterized by an increase in cell number and a concerted and coordinated change in cell/tissue/organ characteristics and functions. Longitudinal growth of the skeleton is the most obvious feature accompanied by the growth and maturation of the muscles, the internal organs, the reproductive system and the central nervous system. Physical activity, as well as the consumption of a balanced diet, ensures this coordinated growth pattern. If the intake of one or more of the essential nutrients is not adequate, growth abnormalities can occur (Berdanier & Zempleni 2009). The greatest nutritional requirements are required in adolescence, not only because of increased metabolism, but also because the habits acquired at this stage of life are those that can be consolidated into adulthood. Consideration is also required of the physiological factors that lead to differences in nutritional requirements between the sexes, such as menarche, because nutritional needs are more related to the stage of development than with chronological age (Moreno et al. 2008).
A definition of a physiological requirement is the amount and chemical form of a nutrient that is systematically needed to maintain normal health and development without disturbance of the metabolism of any nutrient. The corresponding dietary requirement would be the intake sufficient to meet the physiological requirement (Aggett et al. 1997). Advances in knowledge of food composition, the availability of consumers' data and increasing scientific evidence of the influences of nutrition on health have enabled the establishment of reference intake values to maintain the physiological needs. The formulation of reference values are based on the requirements for an individual in good health status and needs to take into account differences between them. After their formulation, physiological requirements have to be translated into the amount of nutrients that individuals have to ingest daily (Prentice et al. 2004).
Bioavailability
Bioavailability is an important factor to consider when determining the reference nutrient intake values of selected micronutrients (King & Garza 2007). Bioavailability is the proportion of a nutrient in a given food that is absorbed and utilized. Bioavailability is used considering the mechanisms of absorption, distribution, metabolism and excretion in the human body. The application of the bioavailability factor is widely used for populations with low nutrient status (developing countries) or population groups that have increased requirements because of the physiologic status, such as in childhood and adolescence (Hunt 1996).
Several nutrients have a low bioavailability from common diets, attributed principally to composition of the diet, the chemical form of the nutrient, the nutritional status of the individual concerning this nutrient and the physiological age of the individual. In this sense, it is important to mention the metabolic adaptation that occurs at different stages of life. For example, the absorption of many minerals increases and their excretion decreases during puberty, in order to maintain the rapid growth and development characteristic of the stage (Prentice et al. 2004). A poor nutritional status or a trace elements deficiency can negatively affect the absorption of other nutrients (Sandstrom 2001).
Physical activity
A child's participation in physical activity is an essential part of the growth and development process. Physical activity helps prevent several diseases such as obesity, diabetes and hypertension, and offers children the opportunity for leisure, social integration and development of their aptitude, leading to enhanced self‐esteem and confidence.
Regular physical training, or even the involvement in everyday relatively moderate physical activities, together with other environmental variables, influences the establishment of a genetically determined growth pattern. Their action on muscles and bones is an important factor for the increase in bone mass peak during adolescence and, consequently, for the prevention of osteoporosis in adulthood (Rizzoli et al. 2009). Regular physical activity is important for controlling ponderal index and has been associated with the reduction of fat mass and increase in lean mass (Rizzoli et al. 2009).
It is important that physically active children and adolescents consume enough energy and nutrients to meet their needs in terms of growth, tissue maintenance and performance of their intellectual and physical activities.
It is remarkable that only some eastern countries in Europe, e.g. Lithuania, Latvia, Poland, Romania and Slovakia, provide recommendations for different levels of physical activity. This could be because, in general, these countries are more active than the western ones (Doets et al. 2008a).
Methods used to estimate recommendations and reference values for children and adolescents
One of the reasons why nutrient recommendations across Europe differ is because the methods used to estimate them are different. In spite of the sophistication of these methods, they have important limitations that should be taken into account (Martin 2001; Food and Nutrition Board (FNB) 2005). The main methods used to estimate micronutrient requirements are presented below.
The factorial approach consists of dividing total requirements into those for maintenance and those for growth. Maintenance requirements are estimated through the losses of the body (urine, faeces, sweat, menstrual blood, semen, etc.) in a steady‐state situation. For growth, the requirements are based on data on body composition and body content of nutrients (Prentice et al. 2004). Possible variations in recommendations on micronutrients using this method reflect differences of opinion about the limits of individual physiological adaptation and the allowance needed to account for bioavailability and mandatory losses (Prentice 2002).
Balance studies are difficult to carry out in children because the subject must to be in a steady state according to the nutrient in question. Moreover, at the commencement of the study, the subject is considered to be in balance regarding the observed nutrient. The intake should be regulated to equal losses. This is difficult for children because of their high velocity of growth and because they also use nutrients for accretion (Prentice et al. 2004). Efforts in collecting biosamples over a long period of time and for ethical reasons can also represent a problem with carrying out this method. It is also criticized because of the physiological adaptability; the estimated micronutrient requirement at balance generally matches intake and thus gives little indication of the sufficiency values (Martin 2001; Prentice 2002; Food and Nutrition Board (FNB) 2005).
Measures based on functional outcomes are based on the detection of an impaired biological function attributed to a nutrient. In spite of the well‐known tasks of nutrients in body functions, we are still far from understanding the effect of specific nutrients or from defining nutritional reference values on these bases. This is the main limitation of this method (Prentice et al. 2004).
Extrapolation consists of calculating recommended values for children and adolescents from the values obtained for infants or for adults older than 19 years because of a lack of data in these group ages. In the 1‐ to 3‐year‐old age group, this approach is the most frequently used because in these young children it is very difficult to measure and collect the required information (Prentice et al. 2004). Internationally accepted standards for growth, body size and body composition should be applied, and inclusion of appropriate adjustments (metabolic efficiency, weight change or physical activity) should be performed in this method (Atkinson & Koletzko 2007).
Most of the countries in Europe have followed similar methodologies to establish their own recommendations. Studies on new ways of classification taking into account the scientific evidence are currently under development, which also aim to assess the reliability of the established recommendations (Baladia & Basulto 2008).
Micronutrient intake distribution in healthy children and adolescents
In population studies, collection of self‐reported data [24‐h recalls (24HR), diet records or food frequency questionnaires (FFQs)] is the most common means of gathering information. Self‐reporting is subject to a number of inaccuracies and biases that have been discussed in several publications (Gibson 2005). When evaluating nutrient intake data in children and adolescents, the most accurate data collections will be those that follow the recommendations described by Ortiz‐Andrellucchi et al. (2009). When there is insufficient scientific information to estimate the distribution of nutrient requirements, nutrient intake data obtained from experimental studies conducted in small samples or those of observational studies from nationwide surveys can be of use. For this purpose, the information on nutrient intake should be as accurate as possible.
Children may not have fully developed the cognitive skills required to self‐report food intake and may not have adequately acquired the concept of time. Moreover, they lack memory retention and attention span, as well as knowledge of the names of foods and experiences in and knowledge of food preparation. Undoubtedly, they need the assistance of adults for dietary reporting (Livingstone et al. 2004). As they grow older, their food habits undergo considerable changes, especially when their parents have less control and supervision over their diet, and children can make choices and be responsible for their own food intake. When children are around 9–10 years old, they should be interviewed by themselves without the intervention of parents when conducting diet data collection (Livingstone et al. 2004).
Almost all the studies dealing with the validity and reliability of dietary data collection in children younger than 9 years included adult assistance in the provision of information on the child's intake. Little data on the effect of gender, race or ethnicity on instrument validity were found. In general, the studies concluded that children generally have difficulty estimating portion sizes (Ortiz‐Andrellucchi et al. 2009). This problem is even more magnified in low‐income populations that are particularly vulnerable in terms of inadequate intakes. Low motivation, low literacy and possible mental or physical disabilities markedly increase biases in estimating intake (Vucic et al. 2009). There are few studies conducted in adolescents that have validated food records, either weighed or estimated, or diet histories (Andersen et al. 2004; Livingstone et al. 2004).
The appropriate way to assess dietary intake in children and adolescents will depend on the purpose of the study, the age of the population sample and the nutrient under study. Regarding the estimation of energy intake, diet records and 24HR and, to a lesser extent, a diet history may provide accurate estimates (Livingstone et al. 2004).
A systematic review conducted by Ortiz‐Andrellucchi addressing the validity of food intake assessment methods in children and adolescents revealed that in children aged 2 to 5 years, FFQs had adequate correlation coefficients (≥0.5) when compared with multiple 24HR for estimating the intake of potassium, magnesium, calcium, iron, vitamin B6, vitamin C, thiamin, riboflavin, vitamin E, folate and niacin; estimated diet records (EDR) for estimating calcium intake; weighed diet records (WDR) for estimating vitamin A, vitamin D, riboflavin and thiamine, and calcium intake; and to biomarkers for estimating the intake of vitamin C (Ortiz‐Andrellucchi et al. 2009). In children aged 6 to 12 years, the FFQ showed adequate correlation coefficients (≥0.5) for assessing the intake of vitamin C, calcium and magnesium when using multiple 24HR as a gold standard for comparison; for assessing vitamin C and beta‐carotene intake when compared with EDR; for assessing vitamin C, potassium, calcium and magnesium intake when using WDR as comparison tool (Ortiz‐Andrellucchi et al. 2009). Moreover, in adolescents aged 13 to 18 years, the intake of retinol, riboflavin, vitamin B6, folate, calcium, phosphorus, copper, iron, zinc, thiamin and vitamin E was adequately correlated when comparing the FFQ to the estimation based on multiple 24HR; and the intake of riboflavin, thiamin, phosphorus, calcium and iron showed a good correlation when compared with the WDR (Ortiz‐Andrellucchi et al. 2009).
Current micronutrient recommendations for children and adolescents in Europe
Methodological aspects
To investigate differences and similarities in the current micronutrient recommendations in Europe, we performed a comparison of reference values for a selection of micronutrients. Furthermore, we aimed to identify differences in methodological aspects underlying these reference values. An aim of the EURRECA network is to develop tools that could improve transparency on the approaches used for deriving nutrient recommendations that vary from country to country.
Data collection
A questionnaire was developed to obtain a comprehensive overview of current micronutrient recommendations in European countries and methods used to derive and apply them. The questions aimed at obtaining information on the process of setting recommendations, the type of evidence used and the translation of recommendations into nutrition policies. For each European country, region or organization, providing micronutrient recommendations, we identified key informants that were involved in the process of setting micronutrient recommendations. These key informants were asked to fill out the questionnaire and return if before the end of September 2007, concurrently providing the latest report(s) on nutrient recommendations. A more detailed description of the contents of the questionnaire and its distribution is described elsewhere (Doets et al., 2008a).
Both the completed questionnaires and the recommendation reports were used to extract micronutrient recommendations on phosphorus, calcium, zinc, iron, vitamin B12, folate, vitamin D and vitamin C for children and adolescents. Furthermore, for each micronutrient of interest, we extracted information on methodological aspects including the type of reference value, the origin of the reference values (derived de novo or adopted from another country/organization), methods used to define reference values, health end points considered for evaluating adequacy of intakes and the type of scientific evidence considered. As described elsewhere (Doets et al. 2008a), it appeared that only the European Community (EC), the UK, France, Latvia, the Netherlands, the German‐speaking countries (Germany, Austria and Switzerland), the Nordic countries (Norway, Denmark, Sweden, Finland and Iceland) and the World Health Organization/Food and Agriculture Organization (WHO/FAO) provided recommendations that had been derived de novo. Other countries defined recommendations by adopting values from at least one other country or institution sometimes after slight modification.
Recommendations were entered onto a database, and a user‐friendly software tool on current recommendations was developed. The description of this EURRECA NutriReQuest tool and its main applications are described elsewhere (Cavelaars et al. 2010).
Comparison of micronutrient recommendations
As micronutrient recommendations are expressed in many different ways, we defined standardization procedures to enable comparison of the recommendations. In the case of multiple recommendations for one population group, e.g. for different activity levels, the mean of all presented values was included in the comparison. In case a recommendation was expressed as a range of acceptable intakes, the mid value was included in the comparison. If recommendations were not expressed in the most common unit, e.g. IU instead of µg, values were converted. Finally, all recommendations included in the comparison were rounded to two decimals. Standardized recommendations on phosphorus, calcium, zinc, iron, vitamin B12, folate, vitamin D and vitamin C were compared per sex for ages 5, 10 and 15 years. There was a large variance in the number of age categories during childhood and adolescence; therefore, we selected three ages that refer to important developmental stages. To identify differences in methodological aspects between European countries/organizations, we compared their own reports on aspects that could be related to the variation between the recommendations.
Results
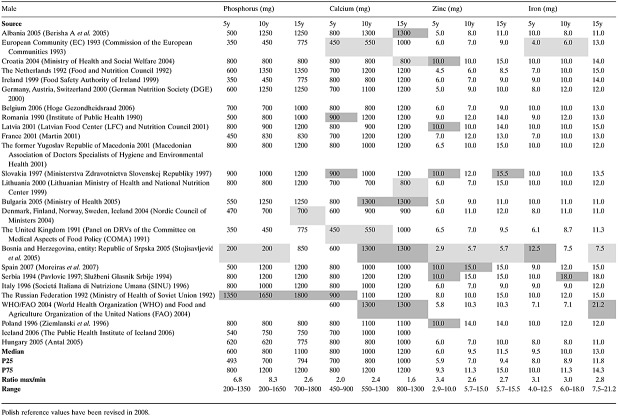
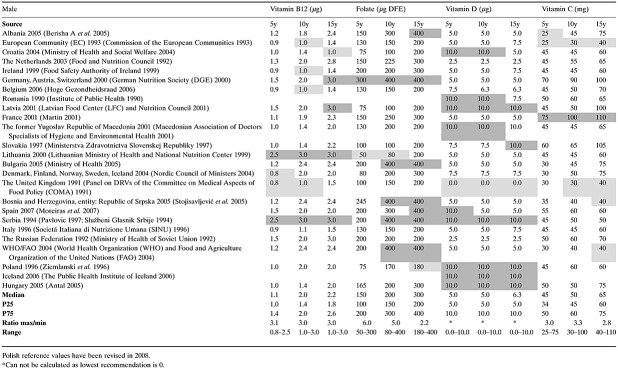
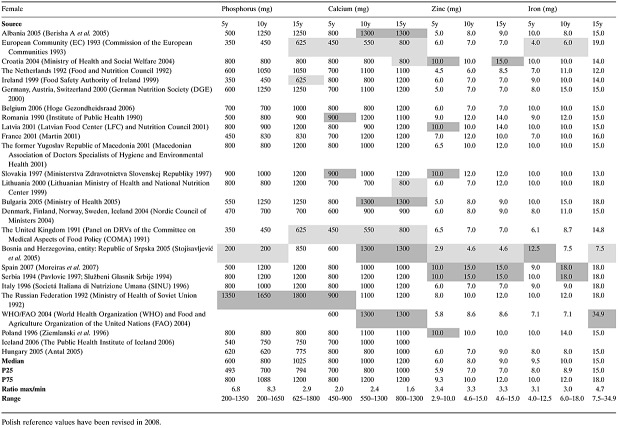
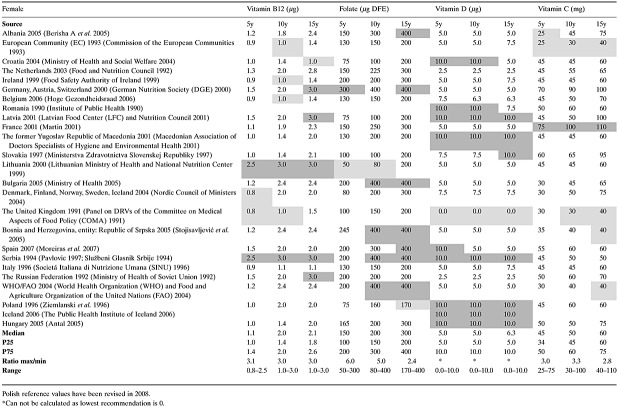
1, 2, 3, 4 illustrate the variability in the micronutrient reference values for selected micronutrients at 5, 10 and 15 years in all European countries divided by gender. Apart from single values given by each country or committee, the lowest (in yellow) and highest (in green) values for each micronutrient have been calculated to understand the high variation between countries. In case of multiple recommended values for a population group, the mean of the given values was used. Values are also distributed in 25th and 75th percentiles. As reference values are expressed in a variety of ways, e.g. as single values, multiple values, ranges, etc., Doets et al. (2008b) defined standardization procedures to enable comparison.
Table 1.
Comparison of minerals intake recommendations for selected age groups
Table 2.
Comparison of vitamin intake recommendations for selected age groups
Table 3.
Comparison of mineral intake recommendations for selected age groups
Table 4.
Comparison of micronutrient recommendation for selected population groups
The method used to approach the reference value in each country is often scarce. The most likely reason is because questions were not clearly formulated (Doets et al. 2008a). Therefore, most of the European countries have expressed that their recommendations are based on ‘general health’ and ‘prevention of deficiency’ concepts.
Phosphorus
‘The calcium/phosphorus ratio of 1 or 1.3’ (Belgium, the Netherlands, the Nordic countries), ‘maintenance of a serum phosphate level’ (the DACH countries, the Nordic countries and France) and ‘compensation for daily losses via urine, faeces and skin’ (France) were the criterion used for adequacy requirement in contrast to the general rule of ‘prevention of deficiency’ and ‘general health’ given by Hungary, Italy, Latvia, Lithuania, Romania and the Russian Federation. All reports include a recommended daily allowance (RDA) for phosphorus, except the Netherlands that provides an acceptable range. The means of these acceptable ranges are higher than the median of European values for ages 10 and 15 years.
Calcium
Besides ‘general health’ and ‘prevention of deficiency’ (Italy, Latvia, Lithuania, Romania, the Russian Federation), other end points for adequacy mentioned are ‘optimal bone mass’ (Belgium, Italy), ‘compensation for losses via skin, faeces and urine’ and ‘increments for skeleton consolidation’ (the Netherlands, EC and France), ‘calcium balance’ and ‘intake required to maintain skeletal integrity’ (the Nordic countries and WHO/FAO). All reports include an RDA for calcium, except Bulgaria and the Netherlands that provide an adequate intake (AI). These AIs are higher than the median of European values for ages 10 and 15 years (only Bulgaria). For calcium, the values recommended for boys are higher than for girls in the EC report, the Netherlands, Romania and the UK.
Zinc
Other end points for adequacy mentioned are ‘zinc balance’, ‘compensation for losses via faeces and urine, skin, semen and menses’ and ‘the maintenance of a reserve’ (Belgium, the Netherlands, the Nordic countries, the DACH countries, the UK, WHO/FAO and EC) apart from ‘prevention of deficiency’ and ‘general health’. All reports include an RDA for zinc, except the Netherlands that provides an acceptable range. The mean of these acceptable ranges are lower than the median of European values. The values for zinc differ between genders in most of the countries at age 15 years and in some countries also at age 10 years. Only in the EC report, Croatia, the Netherlands, Romania, Latvia, Spain and Serbia are the values at age 15 years the same for boys and girls.
Iron
Besides ‘general health’ and ‘prevention of deficiency’, other end points for adequacy mentioned are ‘compensation for losses via skin, urine and faeces’ and ‘the maintenance of a certain haemoglobin level in the blood’ (Belgium, the Netherlands, the Nordic countries, Italy, the DACH countries, the UK, WHO/FAO, the EC and France). Furthermore, all reports take into account compensation for growing body tissues and expanding red cell mass. For 15‐year‐old girls, additional menstrual losses are estimated. The estimated losses and absorption rate of iron corresponds well between reports. All reports include an RDA for iron, except the Netherlands that provides an AI. This AI is at 5 years below the median, at 10 years equal to (males) or higher than the median and at 15 years higher than the median of European values. Iron values are higher in boys than in girls at age 15 years in the Netherlands, Slovakia and in the WHO/FAO report. In this last report, the values are in general much higher than in other countries. For 10 year olds, values for iron are higher in females than in males in the Netherlands, the DACH countries, Bulgaria, Spain and Poland. In Croatia, the Netherlands, Ireland, Latvia, Slovakia, Bosnia and Herzegovina and Serbia, female values for iron are lower than in boys for 15 year olds.
Vitamin B12 (Cobalamin)
Most recommendations are based on the amount needed to cure macrocitic/pernicious anaemia. Other end points for adequacy mentioned are ‘plasma vitamin B12 concentrations’ (the DACH countries, the Netherlands, Italy and WHO/FAO), ‘bilio‐digestive losses’ and ‘other haematological parameters’ (DACH countries, the Netherlands). The levels of bioavailability taken into account vary by 40–50% between reports. All reports include an RDA for vitamin B12 intake, except the report of the Netherlands that includes an AI. This AI is somewhat higher than the median of recommendations at ages 5 and 15 years. The vitamin B12 recommendations for both genders are almost the same. Only in Italy is the value for boys at 15 years slightly higher than for girls.
Folate
Besides ‘general health’ and ‘preventing of deficiencies’, ‘optimal reduction of plasma homocysteine’ (DACH, not specified, France: <10 µmol L−1, WHO/FAO: <7 µmol L−1) was also mentioned as a criteria for adequacy. Furthermore, ‘red cell folate’ (the Netherlands: <140 ng mL−1, WHO/FAO: >150 µg L−1, EC: not specified) and ‘other biochemical parameters reflecting adequate folate status’ were reported (the Netherlands, Nordic countries, Belgium). All countries present an RDA for folate intake, except France and the Netherlands that present an AI. These AIs are close or equal to the European median. Only in Italy are the values for boys lower than for girls at 10 and 15 years.
Vitamin D
Criteria for adequacy in all country reports are based on the vitamin D requirements to prevent biochemical deficiency assessed by the serum value of 25‐hydroxyvitamin D (25‐OH‐D). Most countries provide an RDA for vitamin D, except for Belgium, France and the Netherlands (AI), the EC and Croatia (acceptable range). These AIs and the means of the acceptable ranges are not higher than the RDAs. There are no differences between genders in reference values for this vitamin.
More research is needed on the definition of optimal vitamin D status in childhood/adolescence because it is the micronutrient with the highest variations across Europe. This is because, at least in part, of the differences in ideas about the effect of sunlight on vitamin D endogenous synthesis. The values for children and adolescents are often the same as those given for young adults (Prentice et al. 2004).
Vitamin C
Besides ‘general health’ and ‘prevention of deficiency’, other end points for adequacy mentioned are ‘plasma vitamin C concentrations’ mostly in relation to risk for cardiovascular disease and all‐cause mortality (the DACH countries, France, the Nordic countries, WHO/FAO) and ‘maintenance of body storage’ (Belgium: 1500 mg, the Netherlands: 1500 mg, EC: body pool 900 mg, WHO/FAO: unspecified). All reports include an RDA for vitamin C intake, except the Netherlands that provides an AI. This AI is equal or close to the median of European values. Vitamin C recommendations differ between the sexes at 15 years in Romania, the Yugoslav Republic of Macedonia, Slovakia and Bulgaria.
Conclusion
Childhood and adolescence are important periods in life because of the various implications for long‐term health. The number of studies on micronutrient requirements in children and adolescents is very scarce given all the implications of micronutrients in processes related to growth and development. For this reason, the EURRECA Network of Excellence wishes to align recommendations on micronutrients in Europe for children and adolescents.
The method used in different countries to determine their reference values are not always the same, but many of them are based on extrapolation of data from young adults and infants or on the consumption of apparently healthy children and adolescents. However, these approaches have several limitations. First, long‐term consequences of this consumption are not known; second, this information has been obtained from different countries with different dietary patterns; and third, this depends on the quality of the surveys considered.
In this paper, we presented current daily recommendations and AI values for European countries. The publication date of the values range from 1990 (Romania) to 2007 (Spain), but this variation does not seem to be related to the level of the recommendation.
Terminology also substantially differs among countries, but all the terms were re‐categorized as three basic concepts: RDA, AI (as defined by Institute of Medicine) and the acceptable range (a range of intake to avoid deficiencies and toxic effects). In Tables 1 to 4, the differences in recommended daily values are shown for selected micronutrients. The differences are particularly expressed in recommendations for phosphorus, with the range from 200 mg (Bosnia and Herzegovina, entity Republic of Srpska) to 1350 and 1650 mg daily (Russian Federation) for 5‐ and 10‐year‐old children, respectively. The ratio between maximal and minimal daily recommended values is also very high for folate (6.0), where the range is from 50 µg (Lithuania) to 300 µg daily for 5‐year‐old children (DACH countries). For all other micronutrients, the max/min−1 ratio is from 1.6 to 3.4, which is still unacceptably high and clearly demonstrates the need to harmonize all micronutrient daily recommendations throughout Europe. This wide range of values is derived in a major part from differences in the criteria for adequacy in requirements chosen. Micronutrients have multiple sites of action in metabolism, and therefore, misapprehension of some parameters of body function can occur in favour of others. In addition to the risk of insufficient intake of vitamins and minerals and the possible consequences mentioned above, excessive intake of micronutrients could also be harmful (fat‐soluble vitamins, iron, etc.). For these reasons, it is very important to establish unique and evidence‐based daily recommendations for micronutrient intake, which will meet all the specific requirements for children and adolescent population group. In this sense, the EURRECA toolkit attempts to provide harmonized best practice guidance for assessing micronutrient requirements that can be used for food/nutrition policies such as the development of dietary guidelines and food fortification and enrichment programmes. For this dietary guidance, it would be important to consider the food sources of the micronutrients, which may be emphasized to the population to prevent future health problems. The best practice guidance includes the determination of the best way to segment the population groups, clarification of the method to approach the real physiological requirement and evaluation of the best dietary reference intake (DRI) concept to assure the physiological needs of a micronutrient. To meet this point, it would be important that inter‐individual variability and the determinants of micronutrient requirements will be studied in depth as well as data on good biomarkers for the intake of micronutrients. It is also necessary for an overseeing committee to periodically review the new data to better communicate the use of DRIs and to apply them more rapidly.
Source of funding
The work report herein has been carried out within the EURRECA Network of Excellence (http://www.eurreca.org), which is financially supported by the Commission of the European Communities, specific Research Technology and Development (RTD) Programme Quality of Life and Management of Living Resources, within the Sixth Framework Programme, contract no. 036196.
Conflict of interest
This report does not necessarily reflect the Commission's views or its future policy in this area. The authors declare no conflict of interest.
Acknowledgements
The authors would like to thank the persons involved in data collation, entry, analyses in the context of RA1.3 and RA1.4: Liesbeth S. de Wit, Rosalie A.M. Dhonukshe‐Rutten, Adriënne E.J.M. Cavelaars, Anna Brzozowska Trudy M.A. Wijnhoven, UNU/SCN Network for Capacity Development in Nutrition in Central and Eastern Europe (http://www.srbnutrition.info/?page=Network), Torunn Holm Totland, Lene F. Andersen, Jiri Ruprich, Lisette C.P.G.M. de Groot (Leader RA1.4 Current Recommendations for population groups), Pieter van't Veer (Leader RA1.3 Concepts and Definitions).
References
- Aggett P.J., Bresson J., Haschke F., Hernell O., Koletzko B., Lafeber H.N. et al (1997) Recommended dietary allowances (RDAs), recommended dietary intakes (RDIs), recommended nutrient intakes (RNIs), and population reference intakes (PRIs) are not ‘recommended intakes’. Journal of Pediatric Gastroenterology and Nutrition 25, 236–241. [DOI] [PubMed] [Google Scholar]
- Andersen L.F., Lande B., Trygg K. & Hay G. (2004) Validation of a semi‐quantitative food‐frequency questionnaire used among 2‐year‐old Norwegian children. Public Health Nutrition 7, 757–764. [DOI] [PubMed] [Google Scholar]
- Antal M. (2005) Tápanyagtáblázat (New Food Composition Tables). Rodler I, Medicina Publishing Comp., Budapest.
- Ashwell M., Lambert J.P., Alles M.S., Branca F., Bucchini L., Brzozowska A. et al (2008) How we will produce the evidence‐based EURRECA toolkit to support nutrition and food policy. European Journal of Nutrition 47 (Suppl 1), 2–16. [DOI] [PubMed] [Google Scholar]
- Atkinson S.A. & Koletzko B. (2007) Determining life‐stage groups and extrapolating nutrient intake values (NIVs). Food and Nutrition Bulletin 28, S61–S76. [DOI] [PubMed] [Google Scholar]
- Baladia E. & Basulto J. (2008) Sistema de clasificación de los estudios en función de la evidencia científica. Dietética y Nutrición Aplicada Basadas en la Evidencia (DNABE): una herramienta para el dietista‐nutricionista del futuro. Act Diet 12, 11–19. [Google Scholar]
- Bender D. (ed.) (2008) Introduction to Nutrition and Metabolism, 4th edn. CRC Press Taylor and Francis Group: Boca Raton, FL. [Google Scholar]
- Berdanier C. & Zempleni J. (eds) (2009) Advanced Nutrition: Macronutrients, Micronutrients and Metabolism. CRC Press Taylor and Francis Group: Boca Raton, FL. [Google Scholar]
- Berisha A., Bader E., Deligia C. & Claude Dop M. (2005) Nutrition country profile Republic of Albania. Food and Nutrition Division, Food and Agricultural Organization of the United Nations (FAO).
- Cavelaars A.E., Kadvan A., Doets E.L., Tepsic J., Novakovic R., Dhonukshe‐Rutten R. et al (2010) Nutri‐RecQuest: a web‐based search engine on current micronutrient recommendations. European Journal of Clinical Nutrition 64 (suppl. 2), S43–S47. [DOI] [PubMed] [Google Scholar]
- Commission Of The European Communities (1993) Nutrient and energy intakes for the European Community. Reports of the Scientific Committee for Food. Thirty first series. Luxembourg.
- Doets E.L., De Wit L.S., Dhonukshe‐Rutten R.A., Cavelaars A.E., Raats M.M., Timotijevic L. et al (2008a) Current micronutrient recommendations in Europe: towards understanding their differences and similarities. European Journal of Nutrition 47 (suppl. 1), 17–40. [DOI] [PubMed] [Google Scholar]
- Doets E.L., De Wit L.S., Dhonukshe‐Rutten R.A., Cavelaars A.E., Raats M.M., Timotijevic L. et al (2008b) Current micronutrient recommendations in Europe: towards understanding their differences and similarities. European Journal of Nutrition 47 (suppl. 1), 17–40. [DOI] [PubMed] [Google Scholar]
- Food And Nutrition Board (FNB), I. O. M. I. (ed.) (2005) Dietary Reference Intakes for Energy, Carbohydrate, Fiber, Fat, Fatty Acids, Cholesterol, Protein and Amino Acids. National Academy Express: Washington DC. [DOI] [PubMed] [Google Scholar]
- Food and Nutrition Council (1992) Nederlandse normen 1989/Dutch dietary reference values 1989, 2nd edn. The Hague. [Google Scholar]
- Food Safety Authority of Ireland (1999) Recommended Dietary Allowances for Ireland. Dublin.
- German Nutrition Society (DGE) (2000) Referenzwerte fur die Nahrstoffzufuhr/reference values for nutrient intake. German Nutrition Society (DGE) , Austrian Nutrition Society (ÖGE) , Swiss Society for Nutrition Research (SGE) & Swiss Nutrition Association (SVE) ), 1st edn. Umschau/Braus: Frankfurt/Main. [Google Scholar]
- Gibson R.S. (ed.) (2005) Principles of Nutritional Assessment. Oxford University press: New York. [Google Scholar]
- Hoge Gezondheidsraad (2006) Voedingsaanbevelingen voor Belgie herziening 2006, HGR dossiernummer: 7145‐2 .
- Hunt J.R. (1996) Bioavailability algorithms in setting recommended dietary allowances: lessons from iron, applications to zinc. The Journal of Nutrition 126, 2345S–2353S. [DOI] [PubMed] [Google Scholar]
- Institute of Public Health (1990) Recommended amounts Romania.
- King J.C. & Garza C. (2007) Harmonization of nutrient intake values. Food and Nutrition Bulletin 28, S3–S12. [DOI] [PubMed] [Google Scholar]
- Koletzko B. (2008a) Basic concepts in nutrition: Nutritional needs of children and adolescents. e-SPEN 3, e179–e184. [Google Scholar]
- Koletzko B. (2008b) General Aspects of Childhood Nutrition In Paediatric Nutrition in Practice (ed. Karger Ag B.), pp. 27–30. Universitat Munchen: Muenchen, Germany. [Google Scholar]
-
Latvian Food Center (LFC) & Nutrition Council
(2001) Leteicamās
 un uzturvielu devas Latvijas iedzivotājiem / recommended intake of energy and nutrients for Latvians.
un uzturvielu devas Latvijas iedzivotājiem / recommended intake of energy and nutrients for Latvians.
- Lithuanian Ministry of Health & National Nutrition Center (1999) Recommended dietary allowances for Lithuanian population (energy, protein, fat, carbohydrate, vitamins and minerals). Valstybės žinios / Official Gazette, No. 102–2936.
- Livingstone M.B., Robson P.J. & Wallace J.M. (2004) Issues in dietary intake assessment of children and adolescents. The British Journal of Nutrition 92 (suppl. 2), S213–S222. [DOI] [PubMed] [Google Scholar]
- Macedonian Association of Doctors Specialists of Hygiene and Environmental Health (2001) Fiziološki Normi Za Ishrana Na Naselenieto Vo Republika Makedonija/Pysiological recommendations for population of Republic of Macedonia.
- Martin, A. (2001) The ‘Apports nutritionnels conseillés’ (ANC) for the French population. Agence Française de Securité Sanitaire des Aliments. Tec & Doc Lavoisier, 3rd edn.: Paris.
- Ministerstva Zdravotnictva Slovenskej Republiky (1997) Vestnik. Odporúčané výživové dávky pre obyvatelstvo Slovenska. Bulletin of Ministry of Health.
- Ministry of Health (2005) Ordinance No. 23 from 19 July 2005 for physiological normative requirement (DRI) for nutrition of the population. State Gazete 63.
- Ministry of Health and Social Welfare (2004) Ordinance on food for particular nutritional needs. Croatian National Official Gazzette 81.
- Ministry of Health of Soviet Union (1992) Recommended dietary allowances for nutrients and energy for several population groups. Voprosy Pitanija 2, 6–15. [Google Scholar]
- Moreiras O., Carbajal A., Cabrera L. & Cuadrado C. (2007) Tablas de composición de alimentos. Ediciones Pirámide (Grupo Anaya, SA). 11a edición revisada y ampliada. Ingestas recomendadas de energía y nutrientes para la población española (chapter) .
- Moreno L.A., Gonzalez‐Gross M., Kersting M., Molnar D., De Henauw S., Beghin L. et al (2008) Assessing, understanding and modifying nutritional status, eating habits and physical activity in European adolescents: the HELENA (Healthy Lifestyle in Europe by Nutrition in Adolescence) Study. Public Health Nutrition 11, 288–299. [DOI] [PubMed] [Google Scholar]
- Nordic Council of Ministers (2004) Nordic Nutrition Recommendations: Integrating Nutrition and Physical Activity, Nord 2004:13, 4th edn. Nordic Council of Ministers: Copenhagen. [Google Scholar]
- Ortega R.M. (ed.) (2004) La composición de los alimentos:herramienta básica para la valoración nutricional. Editorial Complutense: Madrid. [Google Scholar]
- Ortiz‐Andrellucchi A., Henríquez‐Sánchez P., Sánchez‐Villegas A. & Al E. (2009) Dietary Assessment Methods (DAME) for micronutrient intake in infants, children and adolescents: a systematic review. The British Journal of Nutrition 102 (Suppl.1), S87–S117. [DOI] [PubMed] [Google Scholar]
- Panel on DRVS of the Committee on Medical Aspects of Food Policy (COMA) (1991) Dietary reference values (DRVs) for food energy and nutrients for the UK. Report on Health and Social Subjects 41. [PubMed]
- Pavlovic M. (ed.) (1997) Ishrana dece predškolskog uzrasta/Nutrition for Preschool Children, Manual for Implementation of the Recommendations. Subotica, Zavod za zas̆titu zdravlja: Serbia. [Google Scholar]
- Prentice A. (2002) What are the dietary requirements for calcium and vitamin D? Calcified Tissues International 70, 83–88. [DOI] [PubMed] [Google Scholar]
- Prentice A., Branca F., Decsi T., Michaelsen K.F., Fletcher R.J., Guesry P. et al (2004) Energy and nutrient dietary reference values for children in Europe: methodological approaches and current nutritional recommendations. The British Journal of Nutriton 92 (suppl. 2), S83–S146. [DOI] [PubMed] [Google Scholar]
- Rai D. & Larson B. (2009) Driving research in infant and children's nutrition: a perspective on industry. The American Journal of Clinical Nutrition 89, 1530S–1532S. [DOI] [PubMed] [Google Scholar]
- Rickert V.I. (ed.) (1996) Adolescent Nutrition Assessment and Management. Chapman & Hall: New York. [Google Scholar]
- Rizzoli R., Bianchi M.L., Garabedian M., Mckay H.A. & Moreno L.A. (2009) Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone 46, 294–305. [DOI] [PubMed] [Google Scholar]
- Sandstrom B. (2001) Micronutrient interactions: effects on absorption and bioavailability. The British Journal of Nutrition 85 (suppl. 2), S181–S185. [PubMed] [Google Scholar]
- Serra‐Majem L. & Aranceta J. (eds) (2004) Nutrición infantil y juvenil. Estudio enKid. Masson: Barcelona. [Google Scholar]
- Službeni Glasnik Srbije (1994) Pravilnik o normativima društvene ishrane dece u ustanovama za decu/Recommendations for collective nutrition of children 50/94, in State Gazette RS.
- Societá Italiana Di Nutrizione Umana (SINU) (1996) Livelli di Assunzione Raccomandati di Energia e Nutrienti per la Popolazione Italiana (LARN).
- Stojisavljević D., Danojević D., Bojanić J. & Jandrić L. (2005) Dietary guidelines with reference values for all micronutrients. No 1. Public Health Institute of the Republika of Srpska.
- Suskind D.L. (2009) Nutritional deficiencies during normal growth. Pediatric clinics of North America 56, 1035–1053. [DOI] [PubMed] [Google Scholar]
- The Public Health Institute of Iceland (2006) Ráðleggingar um mataræði og næringarefni fyrir fullorðna og börn frá tveggja ára aldri. Reykjavík.
- Vucic V., Glibetic M., Novakovic R., Ngo J., Ristic‐Medic D., Tepsic J. et al (2009) Dietary assessment methods used for low‐income populations in food consumption surveys: a literature review. The British Journal of Nutrition 101 (suppl. 2), S95–S101. [DOI] [PubMed] [Google Scholar]
- World Health Organization (WHO) & Food and Agriculture Organization of the United Nations (FAO) (2004) Vitamin and mineral requirements in human nutrition. Second edition of report of a joint FAO/WHO expert consultation, Bangkok, Thailand . Geneva.
- Ziemlanski S., Bulhak‐Jachymczyk B., Budzynska‐Topolowska J., Panczenko‐Kresowska B. & Wartanowicz M. (1996) Recommended dietary allowances for Polish population (energy, protein, fat, vitamins and minerals). New Medicine 3, 1–27. [Google Scholar]