Abstract
Progress towards reducing mortality and malnutrition among children <5 years of age has been less than needed to achieve related Millennium Development Goals (MDGs). Therefore, several international agencies joined to ‘reposition children's right to adequate nutrition in the Sahel’, starting with an analysis of current activities related to infant and young child nutrition (IYCN). The main objectives of the situational analysis are to compile, analyse, and interpret available information on infant and child feeding, and the nutrition situation of children <2 years of age in Chad, as one of the six targeted countries. These findings are available to assist in identifying inconsistencies and filling gaps in current programming. Between June and October of 2008, key informants responsible for IYCN‐related activities in Chad were interviewed, and 53 documents were examined on the following themes: the promotion of optimal breastfeeding and complementary feeding practices, prevention of micronutrient deficiencies, management of acute malnutrition, prevention of mother‐to‐child transmission of human immunodeficiency virus (HIV), food security, and promotion of good hygienic practices. Chad is not on track to reaching the MDGs of reducing mortality by two‐thirds and malnutrition by half among children <5 years of age between 1990 and 2015. Most of the key IYCN topics were addressed in a national policy to combat malnutrition and micronutrient deficiencies. No national nutrition policy was yet ratified in Chad, so the target of many documents reviewed was the malnourished child. Researchers have identified some barriers to optimal feeding practices. However, the majority of these surveys were small scale, so they do not necessarily provide information relevant to the general population. Expanded surveys would be needed for developing evidence‐based educational messages targeted to local needs. Reviewed training materials and related programmes being implemented in Chad provide specific guidance for nearly all of the key IYCN topics, except for appropriate feeding choices for the prevention of mother‐to‐child transmission of HIV. Some of the programmes were intended for national coverage, but we could not confirm whether these programmes were actually implemented nationally. Monitoring and evaluation reports were available for some small‐scale programmes, but few of these evaluated whether IYCN‐specific programme components were implemented as designed and none evaluated whether participants adopted the promoted feeding practices. Establishment of the policy and programme framework has commenced for improving IYCN practices. Formative research is needed to guide the development of evidence‐based training materials and programmes to address the nutritional needs of infants and children. Once more directed programmes are established, there is a further need for rigorous monitoring and evaluation to ensure that training is adequate, programmes are implemented as designed, and effective programmes are identified for expansion nationally. Evaluations are also needed to determine where human and institutional capacity building is needed to carry out these activities as they are implemented. National and international support will be required to complete these enhancements, and thus improve the health and nutritional status of infants and young children in Chad.
Keywords: infant and young child nutrition, national policies, nutrition programmes, monitoring and evaluation, West Africa, Chad
Background
Chad is a landlocked country of 1.2 million square kilometres bordered by Libya to the north, Sudan to the east, Central African Republic to the south, and Cameroon, Nigeria, and Niger to the west. Chad is divided into 22 administrative regions and 61 departments within these regions. Among the 10 million inhabitants, 47% are <15 years of age (2009 estimates (1)). The estimated per capita gross domestic product was US$1600 in 2008. Natural resources in Chad include petroleum, uranium, natron, kaolin, fish (Lake Chad), gold, limestone, sand/gravel, and salt. Extensive humanitarian aid is provided to the numerous refugee camps established in Chad for the hundreds of thousands of persons fleeing the conflict in Sudan (Fig. 1).
Figure 1.
Chad – map of country borders. Map courtesy of United Nations Office for the Coordination of Humanitarian Affairs (OCHA), West and Central Africa regional office.
In Chad, the rainy season lasts from about May to September. The climate in Chad ranges from the northern Saharan region with <200 mm annual rainfall to the south‐western tip of Chad that receives 1000–1200 mm annual rainfall. Lake Chad is the fourth largest lake in Africa, but has shrunk from 25 000 km2 in 1963 to just 1350 km2 (2009 estimate) due to increased population water use and decreased rainfall. As with other countries across the Sahel, agriculture is particularly vulnerable to annual fluctuations in rainfall. Subsistence farming and livestock provide the livelihood for more than 80% of Chad's population (1). Less than 3% of Chad's land mass is considered arable, with less than 1% devoted to permanent crops [2005 (1)]. The main crops include cotton, groundnuts, rice, other cereals, and dates (2).
No progress has been reported in Chad towards achieving Millennium Development Goals (MDGs) 1.8: to halve the prevalence of underweight among children <5 years of age (Fig. 2), and MDG 4.1: to reduce mortality among children <5 years by two‐thirds (Fig. 3).
Figure 2.
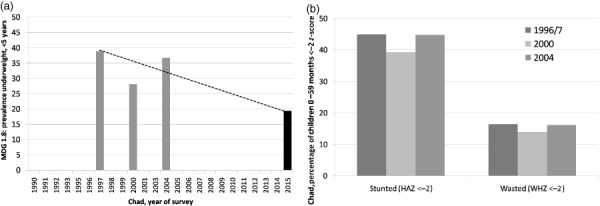
Progress towards Millennium Development Goal (MDG) 1.8 to halve underweight among children <5 years between 1990 and 2015, and trends in stunting and wasting among children <5 years of age. (a) Trend towards MDG 1.8, underweight. Dotted line indicates MDG 1.8 target trajectory: to halve hunger between 1990 and 2015, as measured by underweight among children <5 years of age, assumes 1996/7 value as baseline. (b) Trends in stunting and wasting. Underweight = weight‐for‐age <−2 z‐score; stunting = height‐for age <−2 z‐score (HAZ); wasting = weight‐for‐height <−2 z‐score (WHZ) (or <−2 SD); DHS, Demographic and Health Survey, data for 1996/7, 2000 and 2004 as reported at Macro International Inc, 2009. MEASURE DHS STAT compiler. http://www.measuredhs.com, accessed 18 February 2009.
Figure 3.
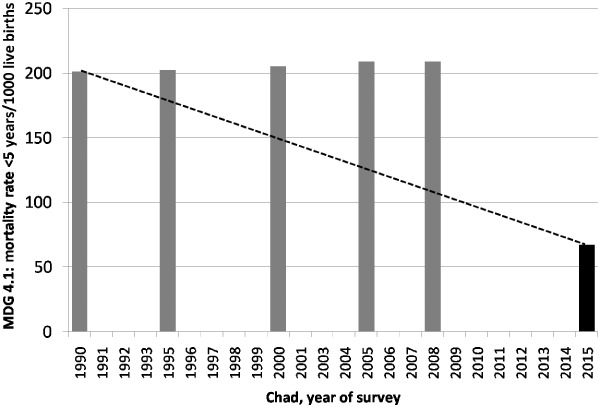
Chad – progress towards Millennium Development Goal (MDG) 4.1, to reduce child <5 years mortality rate/1000 births by two‐thirds. Dotted line indicates MDG target trajectory. Estimates from UNICEF: http://www.unicef.org/statistics/index_countrystats.html, 13 February 2009; 2015 goal is 1/3 1990 estimate.
The lack of progress towards improving these nutrition and health indicators demonstrates the continued and critical need to improve available nutritional and other health‐related activities, and fill identified gaps in these activities for infants and young children in Chad.
The main objectives of the situational analysis were to compile, analyse, and interpret available information on infant and young child feeding, and the nutrition situation of children <2 years of age in the six target countries (Burkina Faso, Chad, Mali, Mauritania, Niger, Senegal). Additional aims were to identify inconsistencies with international recommendations and gaps in programme activities, and to provide recommendations based on these findings to guide the development of more effective infant and young child nutrition (IYCN)‐related programmes and activities.
Methods
Between June and October 2008, the in‐country coordinator of this situational analysis contacted organizations known to be involved in IYCN‐related activities. Key informants from participating organizations completed a questionnaire regarding their IYCN activities and shared 53 pertinent documents that we reviewed for this analysis (see Supporting Information Appendix S1). Unfortunately, documents were not available for some relevant activities. Therefore, the analyses are limited to those documents we were able to obtain. Because it would have been beyond the scope of these analyses to include all documents regarding human immunodeficiency virus (HIV), food security, and hygiene; we focused on respective activities that targeted infants and young children with available tracking of indicators.
The documents obtained include information on (i) national policies, strategies, and plans of action; (ii) formative research studies related to barriers and beliefs concerning IYCN‐related behaviours and peer‐reviewed research relevant to programme development; (iii) training materials and programme protocols; (iv) programmes implemented with the intended and actual programme coverage; and (v) programme monitoring and evaluation reports, including available survey results. The topics reviewed in these documents included the promotion of optimal breastfeeding and complementary feeding practices, prevention of micronutrient deficiencies, the prevention and treatment of acute malnutrition, appropriate feeding practices to reduce the risk of mother‐to‐child transmission of HIV, food security, and the promotion of good hygiene. The criteria for comparison with internationally recognized recommendations are outlined in the review paper in this issue (3). Reported activities and gaps in information are discussed in the following sections by feeding practices or other nutrition‐related activities. Summary tables of additional activities and documents identified are listed in supplementary online tables by type of document reviewed. These tables provide brief summaries of the sponsors, sites of intervention, IYCN topics discussed and some key findings reported (see Supporting Information Appendix S1).
Results
The findings of our analyses are summarized in Table 1 by feeding practice promoted and by other nutrition‐related activities (rows), and by type of document reviewed with programme coverage and some related national statistics (columns). The section on breastfeeding (Promotion of optimal infant and young child feeding practices) provides examples on how to interpret the information provided in Table 1, and the contents are further explained in the table footnotes. The majority of activities identified in our review are joint activities between the relevant governmental agencies and international or national non‐governmental organizations (NGOs) and/or United Nations agencies. We found little information on the actual human and institutional resources available to implement these programmes, how well individual educational messages were promoted by facility staff, or whether participants were applying messages received.
Table 1.
Chad – summary of actions documented with respect to key infant and young child feeding practices (explanations found at the end of the table)
| Key practice promoted and related activities* | Summarized findings by type of document reviewed, with selected national‐level findings † | |||||||
|---|---|---|---|---|---|---|---|---|
| Policies | Formative research | Training materials | Programmes | Intended programme coverage | Actual programme coverage | Programme monitoring | Evaluation | |
| Promotion of optimal feeding practices | ||||||||
| Timely introduction of BF, 1 h | ✓ | ✓ | ✓ | ✓ | National | Sub‐national | (✓) | 34% ‡ |
| EBF to 6 months | ✓ | ✓ | ✓/–✓ | ✓/–✓ | National | Sub‐national | (✓) § | 2% ¶ |
| Continued BF to 24 months | ✓ | ✓ | ✓ | ✓ | National | Sub‐national | (✓) | 65%** |
| Introduce CF at 6 months | ✓ | N/I | –✓/✓ | ✓/–✓ | National | Sub‐national | (✓) | 76% †† |
| Nutrient‐dense CF | ✓ | (✓) | ✓ | ✓ | National | Sub‐national | (✓) | 19% §§ |
| Responsive feeding | N/I | N/I | N/I | N/I | N/I | N/I | N/I | N/I |
| Appropriate frequency/consistency | ✓ | N/I | ✓ | ✓ | National | Sub‐national | (✓) | N/I |
| Dietary assessments to evaluate consumption | N/I | N/I | N/I | N/I | N/I | N/I | N/I | (✓) ¶¶ |
| Prevention of micronutrient deficiencies | ||||||||
| Vitamin A supplements young children | –✓ | N/I | ✓ | ✓ | National | 32%*** | (✓) | N/I |
| Post‐partum maternal vitamin A supplementation | ✓ | N/I | –✓/(✓) | (✓) | National | N/I | (✓) | 18% ††† |
| Zinc to treat diarrhoea | N/I | N/I | ✓ | ✓ | National | Sub‐national | (✓) | N/I |
| Prevention of zinc deficiency | N/I | N/I | N/I | N/I | N/I | N/I | N/I | N/I |
| Anaemia prevention (malaria, parasites) | N/I | N/I | ✓ | ✓ | N/I | Sub‐national | 56% ‡‡‡ | N/I |
| Anaemia prevention (iron/folic acid in pregnancy) | ✓ | N/I | ✓ | ✓ | N/I | Sub‐national | 2% §§§ | N/I |
| Assessment of iron deficiency anaemia | N/I | ✓ | (✓) ¶¶¶ | (✓) | N/I | N/I | N/I | N/I |
| Iodine programmes | ✓ | ✓ | ✓ | ✓ | National | Sub‐national | 56%**** | N/I |
| Special circumstances | ||||||||
| Management of malnutrition | ✓ | ✓ | ✓ | ✓ | National | Sub‐national | (✓) | 16% WHZ 34% WAZ 45% HAZ †††† |
| Prevention MTCT HIV/AFASS | N/I | N/I | N/I | N/I | N/I | N/I | 48% ‡‡‡‡ | N/I |
| Food security | N/I | N/I | N/I | ✓ | National | Sub‐national | ✓ §§§§ | N/I |
| Hygiene and food safety | ✓ | N/I | (✓) | (✓) | (National) | Sub‐national | 4% ¶¶¶¶ | N/I |
| Related tasks | ||||||||
| IEC/BCC in programmes | N/I | N/I | ✓ | ✓ | National | Sub‐national | ✓ | N/I |
EXPLANATION OF TABLE HEADERS AND MARKINGS:
Confirmed documentation of actions specific to these key practices.
N/I
No documentation of the activity was provided or identified.
(✓)
Actions more generally related to the key practices, but without referencing the practice specifically.
Practice that is addressed but that is not specifically consistent with international norms – e.g. in case of anaemia: haemoglobin assessments are used and these cannot distinguish the cause of the anaemia, but treatments only address iron deficiency anaemia.
n/a
Not applicable.
* KEY PRACTICES AND RELATED ACTIVITIES AS OUTLINED IN TEXT BOX 1 OF THE DETAILED METHODS PAPER IN THIS ISSUE (3) .
Timely introduction of BF, 1 h: commencement of breastfeeding within the first hour after birth.
Exclusive breastfeeding (EBF) to 6 months: with no other food or drink other than required medications until the infant is 6 months of age.
Continued BF to 24 months: continuation of any breastfeeding until at least 24 months of age as complementary foods (CFs) are consumed.
Initiation of CF at 6 months: gradual commencement of CF at 6 months of age.
Nutrient‐dense CF: promotion of CF that are high in nutrient density particularly animal source foods and other foods high in vitamin A, iron, and zinc.
Responsive feeding: encouragement to assist the infant or child to eat and to feed in response to hunger cues.
Appropriate frequency/consistency: encouragement to increase the frequency of CF meals or snack as the child ages (two meals for breastfed infants 6–8 months, three meals for breastfed children 9–23 months, four meals for non‐breastfed children 6–23 months, ‘meals’ include both meals and snacks, other than trivial amounts, and breast milk), and to increase the consistency as teeth erupt and eating abilities improve.
Dietary assessments to evaluate consumption: indicates whether dietary assessments are being conducted particularly those that move beyond food frequency questionnaires.
Vitamin A supplements young children: commencement of vitamin A supplementation at 6 months of age and repeated doses every 6 months.
Post‐partum maternal vitamin A: vitamin A supplement to mothers within 6 weeks of birth.
Zinc to treat diarrhoea: 10 mg/day for 10–14 days for infants and 20 mg/day for 10–14 days for children 12–59 months.
Prevention of zinc deficiency: provision of fortified foods or zinc supplements to prevent the development of zinc deficiency among children >6 months.
Anaemia prevention (malaria, parasites), iron/folate supplementation during pregnancy, insecticide‐treated bed nets (ITNs) for children and women of child‐bearing years, anti‐parasite treatments for children and women of child‐bearing years.
Assessment of iron‐deficiency anaemia: any programme to go beyond the basic assessment of haemoglobin or haematocrit to assess actual type of anaemia such as use of serum ferritin or transferrin receptor to assess iron‐deficiency anaemia.
Iodine programmes: promotion of the use of iodized salt; universal salt iodization or other universal method of providing iodine with programmes to control the production and distribution of these products.
Management of malnutrition: diagnosis of the degree of malnutrition, treatment at reference centres/hospitals for severe acute malnutrition and appropriate follow‐up in the community, or local health centre, or community‐based treatment programmes for moderately malnourished children.
Prevention MTCT HIV/acceptable, feasible, affordable, sustainable, and safe (AFASS): appropriate anti‐retroviral treatments for HIV‐positive women during and following pregnancy to avoid transmission to the infant, EBF to 6 months, breast milk substitutes only when EBF is not possible. Substitutes should be AFASS, weaning should be gradual, or EBF should be followed by partial breastfeeding depending on the risk factors (see Text Box 4 of the detailed methods paper in reference (3)).
Food security: programmatic activities with impact on infant and young child nutrition including agency response to crises, tracking markers of food security, and food aid distributions.
Hygiene and food safety: all aspects of appropriate hand washing with soap, proper storage of food to prevent contamination, and environmental cleanliness, particularly appropriate disposal of human wastes (latrines, toilets, burial).
† CATEGORIES OF ACTIONS UNDER WHICH THE KEY PRACTICES WERE CORRECTLY ADDRESSED.
Policies: nationally written and ratified policies, strategies, or plans of action.
Formative research: studies that specifically assess barriers and beliefs among the target population regarding each topic and/or bibliographic survey of published studies related to programme development as identified through PubMed search of ‘nutrition’, plus either ‘child’ or ‘woman’, plus the name of the country, and/or by key informant.
Training/curricula: programme protocols, university or vocational school curricula, or other related curricula that specifically and correctly addresses each desired practice; these include pre‐ and in‐service training manuals.
Programmes: documented programmes that are functioning at some level that are intended to specifically address each key practice listed.
Intended programme coverage: the level at which the programme is meant to be implemented according to programme roll‐out plans.
Actual programme coverage: the extent of programme implementation that was confirmed in one of the received documents.
Programme monitoring: monitoring activities that are conducted for a given programme that specifically quantify programme coverage, training, activities implemented, whether messages are retained by caregivers and result in change.
Surveys and evaluations: studies that have been conducted to evaluate changes in specific population indicators in response to a programme and/or cross‐sectional surveys.
ADDITIONAL INFORMATION
DHS, demographic and health surveys; MTCT, mother‐to‐child transmission of HIV; HIV, human immunodefiency virus; BCC, behaviour change communication; IEC, information, education, and communication.
Percentage of infants put to breastfeeding within the first hour after birth among children born in the previous 5 years, DHS 2004.
§ Evaluated the counselling received regarding breastfeeding.
Percentage of infants still exclusively breastfeeding at 4–5 months of age, DHS 2004.
Percentage of children 20–23 months who are still breastfeeding, DHS 2004.
Percentage of infants at 6–7 months consuming complementary foods, DHS 2004.
Percentage of infants at 6–7 months consuming meat, fish, or eggs, no other nutrient‐dense foods included in DHS 2004.
Dietary consumption data collected in DHS 2004 include the groups of food consumed the previous 24 h, but no quantities.
Percentage of children 6–59 months reportedly, or by health record, who received vitamin A supplements in the past 12 months, 2004 DHS.
††† Percentage of women reporting night blindness during their last pregnancy in the previous 5 years, DHS 2004.
‡‡‡ Percentage of households in which all children are sleeping under a bed net (no report of use of ITNs), DHS 2004.
Percentage of women reporting consuming at least 60 days of iron–folic acid supplements during their last pregnancy in the previous 5 years (did not report consumption for at least 90 days), DHS 2004.
¶¶¶ Haemoglobin assessment of general anaemia, but no assessments to distinguish iron deficiency.
Percentage of homes tested with iodized salt containing ≥15 ppm iodine, DHS 2004.
Percentage of children 0–59 months <−2 z‐score, weight‐for‐height (WHZ), weight‐for‐age (WAZ), height‐for‐age (HAZ), DHS 2004 adapted for 2005 World Health Organization Growth Standards.
‡‡‡‡ Percentage of women reporting understanding that HIV can be transmitted mother‐to‐child, DHS 2004.
§§§§ In refugee camps.
¶¶¶¶ Percentage of households reporting access to method disposing of human wastes in a hygienic manner (toilet, improved latrine), DHS 2004 (no report of how children's excrements are disposed).
Promotion of optimal infant and young child feeding practices
Breastfeeding
National policies
All three key breastfeeding practices are promoted in the 1998 National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies (4). This is the only ratified national nutrition‐related policy. The Global Strategy for Infant and Young Child Feeding (5) is also used as a resource in developing nutrition programme protocols, but is not officially ratified. The check marks in the three cells for breastfeeding in Table 1 under the column for ‘policies’ indicate the promotion of these feeding practices in this policy. No other nutrition policies or strategies were ratified at the time of our analyses.
Formative research
Findings of four small surveys of barriers related to breastfeeding were reported in locally produced documents 6, 7, 8. Reported beliefs among respondents included that colostrum is ‘dirty’, so should not be provided to newborns, breast milk alone cannot quench the infant's thirst, and pregnant women should not breastfeed. Although these findings were not representative of the entire population, they provide some information for development of educational messages. Thus, the respective cells under ‘formative research’ in Table 1 are filled with check marks. However, further research is needed to clarify whether these findings are widespread and how to best counteract the suboptimal breastfeeding practices observed among most infants in Chad (see Surveys and monitoring and evaluation under Breastfeeding).
Training materials and programme documents
National‐level training documents that promote optimal breastfeeding practices are the 2007 National Protocol for the Management of Malnutrition (9) and the National Vitamin A Supplement Distribution Guidelines (10). Therefore, these cells in Table 1 under both ‘training materials’ and ‘programmes’ are filled with check marks. Because some older documents are still in circulation, which recommend exclusive breastfeeding to just 4–6 months instead of 6 months, there is also a check mark preceded by a negative sign in the row for exclusive breastfeeding. Breastfeeding is promoted in six other training documents that are either intended for use in certain regions, or the coverage was not specified 7, 8, 11, 12, 13, 14. However, there were no comprehensive guides to promote all three key breastfeeding practices for use at the national or regional level beyond the management of malnutrition protocols.
The United Nations Children's Fund (UNICEF)‐Chad cooperative programme also promotes the Baby Friendly Hospital Initiative in three hospitals [2005, denominator not provided (15)]. The three cells for breastfeeding under ‘intended programme coverage’ are filled with ‘national’ in Table 1 because all three practices are promoted in at least one programme intended for national coverage. However, we could not confirm whether these programmes were implemented beyond certain regions, therefore the ‘actual coverage’ is listed as ‘sub‐national’. The nationally mandated Minimum Packet of Activities for health centres includes the management or treatment of malnutrition but does not yet include activities to prevent malnutrition such as the promotion of optimal breastfeeding practices (16). Behaviour change communication (BCC)/information education communication (IEC) techniques are discussed in four of the government supported training documents reviewed 9, 10, 13, 14, and country contacts indicated that BCC/IEC activities play a central role in a new breastfeeding promotion programme that did not yet have any documentation for review.
Surveys and monitoring and evaluation
In the following, ‘surveys’ refer to cross‐sectional data collection among a selected subset of the population. These surveys are not necessarily related to a programme or study. ‘Monitoring’ refers to studies that evaluate the implementation of a specific programme and whether it is implemented according to protocol. ‘Evaluation’ refers to findings regarding the outcomes or impact of a programme. We identified several surveys or programme evaluations that assessed the status of breastfeeding practices. Because none of these collected data on breastfeeding practices at both baseline and follow‐up, the effectiveness of programme interventions could not be confirmed. A survey in 2007 conducted in four regions and among internally displaced persons (17) found that 9.2% of infants were exclusively breastfed at 4–5 months. This appears to be much higher than the <1% reported in the 1997 and 2004 national surveys 18, 19, but still extremely low. Due to the lack of standard errors, these surveys cannot easily be compared across time, and the regions reported in the national surveys are not necessarily the same as in the regional survey.
There appears to have been an increase in the use of complementary foods that was somewhat matched by a reduction in the use of non‐milk liquids among infants <6 months of age between the 1997 and 2004 Demographic and Health Surveys (DHS) reports (Fig. 4) 18, 19. At this same age, about 52% and 37% of infants were receiving just water in addition to breast milk (1997, 2004, respectively). The use of water and complementary foods prior to 6 months of age remains high. Analyses of the similarity between questionnaires and training methods are needed to clarify how much of the reported differences are due to methodological differences or to actual changes in feeding practices. Researchers have demonstrated associations between non‐exclusive breastfeeding and increased prevalence of diarrhoea and respiratory infections among young infants 20, 21, 22, 23. Therefore, there is great potential for improving the health and well‐being of infants in Chad by increasing rates of exclusive breastfeeding.
Figure 4.
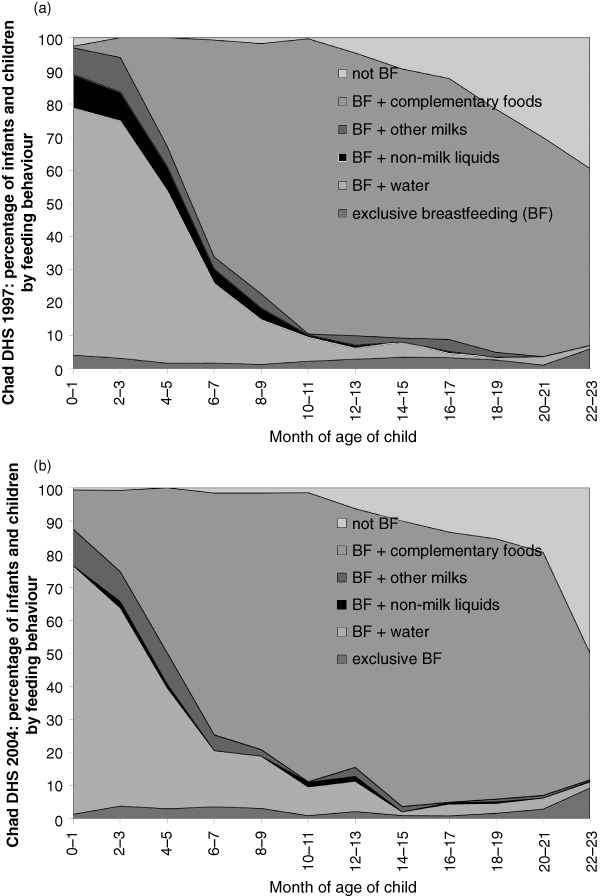
Chad – breastfeeding (BF) practices by age according to Demographic and Health Survey (DHS) reports (1997, 2004) 18, 19. (a) 1997 DHS. (b) 2004 DHS. Figure courtesy of UNICEF West and Central Africa Regional Office.
The data collected in the 2004 DHS are adequate to calculate the three core breastfeeding indicators currently recommended by the World Health Organization (WHO) to evaluate the status of infant breastfeeding practices in large populations (24). Some additional analyses of the data would be required to present the data in the recommended format for comparison with future surveys and across countries.
Summary of findings – breastfeeding
-
•
The 1998 National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies provides high‐level support for the key breastfeeding practices. This is the most recent national nutrition‐related policy or strategy.
-
•
Breastfeeding rates are low, but about 80% of infants are reportedly breastfed through 21 months of age.
-
•
There was an apparent increase in the prevalence of exclusive breastfeeding in certain regions between 2004 and 2007, but we found no programme monitoring and evaluation reports to confirm which programme may have been involved. We also found no programme monitoring to confirm whether national protocols are implemented as designed.
Recommendations – breastfeeding
-
•
Policy makers should consider developing a national nutrition policy to promote optimal IYCN practices to prevent and not just combat malnutrition.
-
•
Outdated training materials and programme documents should be replaced with national‐level protocols and guidelines that reflect current internationally recommended breastfeeding practices for the general population. These should be guidelines for primary health care providers beyond the emphasis on treating malnourished children.
-
•
The new BCC/IEC programme provides an excellent opportunity to implement rigorous monitoring and evaluation to confirm whether the programme is having expected impacts on improving breastfeeding practices, and if effective, how best to expand this programme.
-
•
Programme evaluations should also be designed to identify critical information on how to adapt breastfeeding programmes to increase their impact such as addressing negative beliefs expressed by participants during education sessions and identification of family decision makers who must be reached by IEC.
Complementary feeding
National policies, strategies, and plans of action
The National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies (4) addresses three of the four key complementary feeding practices: commencement at 6 months of age, use of nutrient‐dense complementary foods, and adequate frequency of meals. The fourth key practice is not included in this document: ‘responsive feeding’ by assisting the infant/child to eat and responding to hunger cues. This gap is identified in Table 1 with ‘N/I’ to indicate this component of complementary feeding was not addressed in any of the documents reviewed. We also evaluated whether there was any support for assessing the dietary adequacy of young children's diets. Because we found no recommendations to evaluate dietary intakes of young children beyond intake of some food groups in national surveys, this row is also mostly filled with ‘N/I’ in Table 1.
Formative research
A local survey conducted in one region (16) identified several complementary feeding practices and beliefs reported by mothers that could be addressed in educational messages: (i) infants commence eating food from the family plate starting at 6 months of age, but the consistency of these foods is not altered to the infant's eating abilities; (ii) alternative foods, such as porridges, were not prepared due to inadequate time and resources such as lack of sugar or oil to add to a porridge; and (iii) mothers were unaware that porridge would be a more age‐appropriate food for infants than the family meal. A positive finding was that some women add peanut paste to the infant's food when finances allow. These findings are limited to small groups of individuals, but they provide information that could be clarified in expanded surveys for use in developing appropriate programme approaches and educational messages.
Training materials and programme documents
As with breastfeeding promotion, the national‐level guidelines for the promotion of complementary feeding comes through the National Protocol for the Management of Malnutrition (9). This document emphasizes the importance of commencing complementary foods at 6 months of age, using nutrient‐dense complementary foods, providing complementary foods frequently enough to meet young children's needs, and assisting children with feeding during illness. It was not clear how or whether this protocol was being used to promote complementary feeding beyond the management of malnutrition. Several older programme documents are still in circulation, which promote commencing complementary foods by 4–5 months of age. We found no current programme‐related documents for the promotion of complementary feeding in the general population.
Surveys and monitoring and evaluation
As with breastfeeding, none of the identified programme evaluations assessed complementary feeding practices at baseline and following the implementation of the programme. The 1997 and 2004 DHS reported that more than half of children over 12 months of age had consumed meat, eggs, or fish as an iron‐rich food source during the 24 h prior to the survey. Although this is higher than many other countries in the region, these intakes are still low, and about 23% of infants 6–9 months of age reportedly did not consume any complementary foods during the day prior to the survey. Information on reasons for not providing foods to children ≥6 months of age would be useful in developing educational materials such as how to feed infants and children during illness and the importance of commencing complementary foods at 6 months of age.
The data collected in the 1997 and 2004 DHS are only adequate to calculate one of the five core complementary feeding indicators recommended by WHO (24), the percent of infants 6–9 months who are consuming complementary foods. In order to calculate all indicators, future surveys must include the consumption of the seven selected food groups and the numbers of meals and snacks consumed during the previous day.
A 2007 UNICEF/World food Programme food security and nutrition survey (17) reported data on the type of complementary foods consumed by young children in the Ouaddaï, Wadi Fira, Guera, and Kanem regions. The most often consumed iron‐rich food was beef (consumed by 27% of children), and the most often consumed food that was specified as a vitamin A source was fruits (consumed by 6% of children). Leaves were consumed by 14% of children, but the bioavailability of vitamin A from leaves is about half that of fruits; therefore, larger quantities of leaves are necessary to provide the same amount of vitamin A (25). The quantities consumed of each food were not reported.
Although no detailed national dietary analyses are available in Chad, the Food and Agriculture Organization of the United Nations collects data annually on the available national food supply (26). Their estimations indicate that the diet in Chad is mainly plant based, with 60% of available calories coming from high‐phytate cereals such as millet and sorghum, from which iron and zinc are not very bioavailable. Only 16% of available protein comes from animal products, which are the most bioavailable sources of many micronutrients, such as zinc, iron, and vitamin A, and just 21% of calories come from fat. Young children who consume mainly plant‐based diets, which, as these findings indicate, may be the case in Chad, are not likely to meet their micronutrient needs unless their diets are enriched through the addition of animal‐source foods, through dephytinization and/or through food fortification to increase the biavailability of minerals (27). Furthermore, if children consume low amounts of dietary fat, the bioavailability of plant‐based vitamin A precursors could be low. Fats also provide concentrated energy for young children who cannot consume large quantities to meet their caloric needs.
Summary of findings – complementary feeding
-
•
The National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies and the National Protocols for the Management of Malnutrition address most of the key complementary feeding practices. These are the only identified national‐level programme and policy promoting complementary feeding.
-
•
Findings from national nutrition surveys indicate that iron‐rich foods are provided to about half of children 12–24 months (1998 and 2004 national DHS).
-
•
Surveys identified barriers to appropriate complementary feeding as inadequate knowledge of appropriate nutrient‐rich complementary foods and inadequate household resources for providing these foods.
Recommendations – complementary feeding
-
•
There is a need to develop IYCN programmes that include the promotion of complementary feeding beyond the scope of treating malnutrition.
-
•
More detailed dietary analyses are needed to confirm in a nationally representative sample of children and caregivers: (i) whether dietary intakes are sufficient to meet young children's nutritional needs; (ii) whether it is possible for families to provide young children with complementary foods that meet these needs, given available household resources; and (iii) how best to address these needs, such as through improved education on use of available foods, production, and distribution of fortified and phytate‐reduced complementary foods or point‐of‐use fortified foods.
-
•
More rigorous monitoring and evaluation are needed to identify programmes that are effective at promoting optimal complementary feeding practices.
Prevention and treatment of micronutrient deficiencies
Vitamin A
National policies, strategies, and plans of action
The National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies (4) and the National Action Plan for Vitamin A Supplementation (VAS) (28) recommend semi‐annual VAS for children 6–59 months and VAS for women early post‐partum. The recommended time period for post‐partum supplementation is clarified as within 8 weeks in the policy document, which is slightly longer than the international recommendations of within 6 weeks post‐partum. This document correctly promotes the currently recommended doses of vitamin A for infants 6–11 and 12–59 months as 100 000 and 200 000 IU, respectively.
Formative research, training materials, and programme documents
No research articles related to vitamin A were identified by PubMed search or through informant interviews. Vitamin A supplements are disseminated by the government with support from the United Nations and international NGOs through semi‐annual national campaigns, in health centres, and in refugee camps 9, 10. The orientation guide for VAS was the only programme‐related document that addressed the consumption of vitamin A‐rich foods (10). It was not clear how this might have been used in participant education.
Surveys and monitoring and evaluation
Between 2001 and 2006, the reported coverage of VAS to children 6–59 months was >80% during 10 of the 12 semi‐annual national campaigns (29). This coverage exceeded that of most of the other countries in the region. Despite these efforts, the 2004 national DHS (18) and the 2007 WFP/UNICEF regional nutrition survey (17) found that just 32% and 60% of children 6–59 months of age, respectively, had reportedly received VAS during the previous 6 months. Some of these discrepancies are likely due to differences in data collection or timing of surveys, but it would be useful to clarify the reasons for these differences to identify whether the most nutritionally vulnerable children are also those missed with VAS campaigns. In addition, the 2007 WFP/UNICEF regional nutrition survey found that just 23% of women had received vitamin A supplements post‐partum, and the 2004 DHS and 2007 regional nutrition survey found that 18% and 37% of women, respectively, reported night blindness during their last pregnancy. These data indicate that, despite national campaigns and programmes, the risk of vitamin A deficiency is still a public health concern in Chad.
Zinc
National policies, strategies, and plans of action
We found no national‐level policies to evaluate or prevent the risk of zinc deficiency. Recent reports indicate that national policies now promote the use of zinc supplements in the treatment of diarrhoea (30).
Formative research, training materials, and programme documents
The national protocol for the management of diarrhoea, as found in the Integrated Management of Childhood Illness (IMCI) (31), recommends providing zinc in the treatment of diarrhoea. Training on these protocols was conducted in at least two health regions, but the full coverage of this programme was not available. We found no interventions aimed at preventing zinc deficiency among young children and no zinc‐related research.
Surveys and monitoring and evaluation
The prevalence of zinc deficiency has not been evaluated in Chad. However, due to high rates of stunting (45%, 2004 DHS), the International Zinc Nutrition Consultative Group considers that there is a high risk of zinc deficiency in Chad requiring commencement of preventive activities, while more specific assessments of zinc status are evaluated (32). The provision of therapeutic zinc in the treatment of diarrhoea, through IMCI, was not yet evaluated to confirm whether this component was being implemented as designed.
Iron and anaemia
National policies, strategies, and plans of action
The strategies to reduce anaemia that are recommended in the The National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies (4) are to provide iron–folic acid supplements to high‐risk populations of women and children ≥6 months of age, to fortify foods with iron, and to diversify diets to include iron‐rich foods such as liver. This 1998 national policy also recommends that all moderately malnourished children receive weekly iron (200 mg) and folic acid (40 mg) supplements during stays at health centres and rehabilitation centres. This policy has not been updated to the new recommendations to evaluate iron status prior to providing iron to young children and to provide infection control when providing this iron in malaria‐endemic regions such as against malaria in Chad's malaria‐endemic regions (33).
Formative research
We identified one research study from 1994 that identified iron deficiency among about one‐fourth of infants with anaemia, as reported in one region among 144 infants (34). The finding that three‐fourths of the infants with anaemia were not iron deficient could be a concern in the light of the new international recommendations to avoid giving iron supplements to iron‐replete infants and children, particularly because malaria was found in 45% of these infants.
Training materials and programme documents
Anaemia prevention activities that are promoted in the national‐level protocol for the management of malnutrition (9) include the use of insecticide‐treated bed nets (ITNs), systematic deworming for women and children ≥12 months of age, the consumption of iron‐rich foods, and the assessment of haemoglobin concentrations to evaluate anaemia (9). This was the only identified national‐level programme promoting activities to prevent anaemia or iron deficiency. The PDAOK agriculture development project (Projet de Développement Agricole des Ouadïs du Kanem) training module, promoted in one region between at least 1999 and the early 2000s with national and regional governmental support, promoted iron–folic acid during pregnancy and nutrient‐dense foods, but did not include other relevant recommendations to prevent anemia (8).
Surveys and monitoring and evaluation
We found no surveys reporting the prevalence of anaemia or iron deficiency among children or women in Chad beyond the findings of the 1994 study mentioned above (34). The 2004 DHS reported that 56% of children were sleeping under bed nets, and just 2% of women consumed at least 60 days of iron supplements during their previous pregnancy (18). Thus, few children and almost no women were utilizing these methods of preventing anaemia. Population‐based surveys are needed to identify why there is a low usage of currently promoted methods of preventing anaemia and iron deficiency, and what other methods might be successfully promoted. For example, considering that 86% of women give birth at home and half of those births are attended solely by family members (2004 DHS), alternatives such as delayed cord clamping would only likely be effective on a broad scale if successfully promoted beyond health centre staff.
Iodine
National policies, strategies, and plans of action
Governmental control of the level of iodine in domestic and imported salt commenced in the early 1990s (35), and the 1998 National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies (4) continues this support. In the case of severe iodine deficiency or lack of access to iodized salt, capsules of iodized oil are also prescribed.
Formative research, training materials, and related programmes
A 1996 survey found that goitre prevalence ranged from 25% in the capital of N'Djamena to 70% in the Sudan zone (36) and urinary iodine was very low (<20 µg L−1) in 33% of the population surveyed in the Sudan zone, indicating high prevalence of iodine deficiency. The 2004 DHS reported that salt was adequately iodized (≥15 ppm) in 56% of homes where salt was tested.
The iodized salt promotion programme (37) reported that key barriers to the use of iodized salt included lack of availability of iodized salt in markets, lack of understanding about the link between iodized salt in preventing iodine deficiency disorders and their consequences, and the difficulty of regulating the importation of iodized salt particularly in the region bordering Sudan.
This 18‐month (2007–2008) government supported programme was initiated to promote the control and use of iodized salt in the Ouaddaï and Wadi Fira regions to combat these problems (37). The baseline study found wide variations across villages in the percent of households with iodized salt ranging from none to 100%. There was no follow‐up study available when we collected data for these analyses.
Summary of findings – prevention of micronutrient deficiencies
-
•
A variety of methods are promoted in Chad to prevent micronutrient deficiencies such as VAS, regular deworming, iron–folic acid supplementation during pregnancy, the use of iron‐rich foods and iron fortification, and universal salt iodization. However, the only relevant national‐level programme identified, beyond the promotion of VAS and zinc supplements in the treatment of diarrhoea, was for the management of malnutrition. We could not confirm the coverage of these activities and educational messages beyond reported VAS.
-
•
The most recent surveys indicate that despite national efforts, the risk of deficiencies in vitamin A, iron, and iodine remain a public health concern, and zinc deficiency is also likely a public health concern. The current prevalence of these micronutrient deficiencies is unknown.
-
•
National protocols are in place to promote the therapeutic use of zinc supplements in treating diarrhoea, but the prevention of zinc deficiency is not yet addressed in any policies or programme‐related activities.
-
•
Although about half of salt tested nationally was adequately iodized at the household level, there is a large difference in access to iodized salt across regions.
Recommendations – prevention of micronutrient deficiencies
-
•
There is a need to develop national‐scale nutrition programmes to promote the prevention of micronutrient deficiencies among the general public beyond the management of malnutrition.
-
•
Evaluations of current programme activities are needed to determine why use of available methods of preventing micronutrient deficiencies is so low, so that programme activities can find ways to fill these gaps such as improving access to VAS, increasing use of ITNs and iron–folic acid during pregnancy, ensuring access to adequately iodized salt and so on.
-
•
The risk of zinc and iron deficiency should be evaluated among young children to guide policy and programme development to address these deficiencies among high‐risk populations.
-
•
If not yet completed, the impact of the 2007–2008 programme to increase the use of iodized salt should be evaluated and effective activities should be continued and expanded as appropriate.
Other nutritional support: management of acute malnutrition, prevention of mother‐to‐child transmission of HIV, food security, and hygiene
Management of acute malnutrition
National policies, strategies, and plans of action
The 1998 National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies (4) emphasizes the need to screen for malnutrition. Recommended methods of diagnosing malnutrition include the identification of marasmus, kwashiorkor, and/or low weight‐for‐age or height‐for‐age. Mid‐upper arm muscle circumference (MUAC) is not included as a possible screening method. This policy clearly promotes most of the key infant and young child feeding practices as described in the sections above, and these feeding practices would assist caregivers in preventing relapses once the child is treated and released.
Formative research
The findings of Renaudin (38) conducted among 1050 hospitalized children in 1992–1993, identified lack of education and poor feeding practice, particularly poor breastfeeding practices, as the highest risk factors for developing malnutrition. They suggested that improved education would be the most cost‐efficient method of fighting undernutrition and mortality among this study group.
Due to the high prevalence of malnutrition in the Kanem region, the PDAOK project conducted a baseline survey to identify the principal causes of malnutrition (7). Identified causes were neglect, ignorance of appropriate breastfeeding and weaning practices, poor hygiene, and inadequate growth monitoring.
Training materials and programme documents
The recent National Protocol for the Management of Malnutrition (9) encourages community screening for malnutrition in addition to screening in health centres. The screening criteria for severe acute malnutrition include (i) bilateral oedema, (ii) MUAC <110 mm for children 6–59 months, and/or (iii) weight‐for‐height <70%. Screening criteria for moderate acute malnutrition (MAM) include (i) MUAC ≥ 110 and <125 mm and/or (ii) weight‐for‐height between 70–80%. Referral to the reference centre was recommended with SAM or when MAM was accompanied by complications. This 2007 document was written prior to recommendations to change the MUAC cut‐off for severe acute malnutrition to 115 mm (39). The growth standards for calculating weight‐for‐height were not included in this protocol document, so the decision on which standards NCHS (National Center for Health Statistics) Reference or WHO Child Growth Standards) to use might not yet have been decided. We could not confirm where these guidelines were implemented beyond certain sites, such as in refugee camps.
Based on the PDAOK baseline survey findings (Formative research under Management of acute malnutrition), the training modules for the PDAOK project were developed to educate caregivers on the causes of malnutrition and what they could do to avoid it through appropriate feeding practices, proper hygiene, and growth monitoring. These training documents were the only ones identified that were developed to address previously identified local needs. Unfortunately, this programme was only conducted in one region and we found no evidence that the concept was extended to other regions.
Surveys and monitoring and evaluation
Most of the identified surveys and monitoring and evaluation reports collected data on height, weight, and/or MUAC, but none of these evaluated the impact of malnutrition treatment programmes. Laevens (16) monitored the capacities of health centres in one region to conduct malnutrition programme activities. The data collected included: whether staff used approved guidelines, adequacy of available human resources, available equipment, participation in programmes, and where there was a need for additional centres. The author identified serious gaps in human and institutional capacities to carry out these activities. Since programme protocols incorporate other nutrition‐related activities, as described in previous sections, it is likely that there are also gaps in capacities to carry out other nutrition‐related activities.
Summary of findings – management of acute malnutrition
-
•
The management of malnutrition is promoted through the 1998 National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies and the 2007 national protocol to manage malnutrition in addition to some region‐level programmes and training documents. The actual coverage of these activities was not reported.
-
•
These documents also provide guidance on screening for malnutrition. This 2007 document does not indicate which growth standards to use, but it appears that the new WHO 2006 standards have not yet been adopted.
-
•
The PDAOK project provides an example of developing evidence‐based training materials for a project aimed at reducing malnutrition. Unfortunately, there were no impact evaluations to confirm whether the project was successful and the concept does not appear to have been copied in other regions.
Recommendations – management of acute malnutrition
-
•
When national protocols are updated, the reference cut‐offs for screening malnutrition should be updated to utilize the WHO Child Growth Standards and the new internationally recommended MUAC cut‐offs for screening severe acute malnutrition.
-
•
There is a need for improved monitoring and evaluation to ensure these programmes are carried out as designed, reaching malnourished children and having the desired impact on preventing and/or successfully treating malnutrition.
-
•
Human and institutional capacities must be expanded to adequately carry out the management of malnutrition and other nutrition‐related services.
Prevention of mother‐to‐child transmission of HIV (PMTCT)
National policies, strategies, and plans of action
We did not identify any national policies addressing the PMTCT. The National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies (4) promotes exclusive breastfeeding among all women, except women with chronic diseases, but the case of HIV was not identified.
Formative research, training materials, and programme‐related documents
One identified research article reported on the cost‐effectiveness of activities to prevent mother‐to‐child transmission of HIV (MTCT) in Chad (40). The authors found that 17% of MTCT could be avoided by anti‐retroviral therapy (ART) and encouragement to avoid breastfeeding. However, they acknowledged that there are other health risks associated with not receiving breast milk. Because very few women in Chad provide exclusively breast milk to infants <6 months of age, the authors could not evaluate the difference between exclusive and non‐exclusive breastfeeding among young infants in their assessments. None of the identified training manuals addressed infant feeding methods to reduce MTCT.
Surveys and monitoring and evaluation
The prevalence of HIV was not available, but in 2009, reportedly 32 000 people received and needed ART in Chad (41)), which is <1% of the estimated 10 million population. In addition, 989 pregnant women with HIV received ART ((41), denominator not provided). The 2004 DHS reported that one‐third to one‐half of surveyed women understood that HIV could be transmitted during pregnancy (48%), birthing (41%), or breastfeeding (36%). Only 17% of respondents knew that HIV was not transmitted by mosquitoes and could not be contracted by sharing a meal with an infected individual. These findings highlight the need for population‐based education to clarify methods of HIV transmission and prevention. Considering that nearly all Chadian infants commence liquids other than breast milk shortly after birth, and non‐exclusive breastfeeding is a risk for MTCT during the first 6 months of life, the promotion of exclusive breastfeeding could have a positive impact on reducing MTCT among infants of HIV‐positive women in Chad.
Summary and recommendations – PMTCT
-
•
Very little national‐level guidance is available to promote methods of PMTCT. Programmes and training materials should be updated to fill this gap.
-
•
As these policies and programmes are updated, they should incorporate the most recent international recommendations to reduce MTCT through ART and exclusive breastfeeding 42, 43.
Food security
A complete review of food security activities in Chad is beyond the scope of this paper. Due to the importance of food security on the health and nutritional status of young children, we reviewed relevant activities incorporated in IYCN‐related documents and general food security tracking that is taking place in Chad. We did not identify any national policies, research activities, or programmes specifically related to food security for infants and young children beyond a discussion in relation to the management of malnutrition. The PDAOK project, mentioned previously, was a development project that included support for agricultural activities and appropriate use of water resources, with a goal of promoting food security and thus reducing malnutrition. The impact of the programme was not evaluated.
USAID‐FEWS NET conducts nearly quarterly surveys of Chad's various livelihood zones and collects data on planting and harvest seasons, average monthly rainfall, and risk factors related to each livelihood (44). These risk factors are collected to guide the implementation of programmes that work with the needs of these households. Other identified surveys collected different data to evaluate the food security situation, thus comparisons across surveys are not always possible. For example, the 2007 WFP/UNICEF survey, which was conducted in four regions and among internally displaced persons, evaluated food security and vulnerability with multiple indicators of sex of the head of household, animal stocks, monthly food expenditures per capita, per capita consumable cereal stocks, presence of shocks, and management strategies for shocks.
According to the 2007 WFP/UNICEF survey, half of households in high‐risk zones were still experiencing food insecurity following the 2005 crisis. This report also described one region where the population had doubled due to refugee immigration. Multiple aid agencies provide support for these refugees, but the influx is reportedly an added strain on the Chadian health care infrastructure. More recent estimates of the food security situation by USAID‐FEWS NET predicted, correctly, that the food security situation would worsen in 2010 (45).
Summary of findings and recommendations – food security
-
•
The role of food security in preventing malnutrition is recognized in relevant documents, but programmes focus on household level or broader activities.
-
•
The USAID‐FEWS NET system tracks the food security situation in Chad on a quarterly basis, and other tracking systems are also in place. The indicators used across surveys are not necessarily similar, so comparisons are not always possible.
-
•
Food insecurity is a chronic problem in Chad that was not resolved following the 2005 crisis, and the situation worsened in 2010. As appropriate, national policies should incorporate methods to support household livelihoods and food security in the support of adequate nutrient‐dense complementary foods for infants and young children.
-
•
Food security interventions in Chad continue to be essential to address the fundamental problems that perpetuate food insecurity, and the resulting impact on childhood health and nutritional status.
Hygiene
As with food security, a complete review of the promotion of proper hygiene in Chad was beyond the scope of this paper so we focused on activities included in IYCN‐related documents.
The importance of proper hygiene was included in the National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies (4) and in the National Protocol for the Management of Malnutrition (9).
We found no national‐level nutrition programmes that incorporated proper hygiene, such as hand washing with soap, or methods of preparing safe drinking water. These practices, including chlorination of water, were promoted in the PDAOK project, which was conducted in one region between at least 1999 and 2000 7, 8, but subsequent activities were not reported.
Hand washing was apparently evaluated in the 2007 nutrition survey in the Ouaddaï, Wadi Fira, Guera, and Kanem regions (17), but the results were not included in the report. Other data reported in this survey are that latrines or toilets were used to dispose of human wastes in just 32% of households, and potable water was available in 37% of households. According to the 2004 DHS (18), about 36% of households nationally had access to potable water, which indicates there was likely no change between 2004 and 2007. If other activities are being conducted beyond IYCN‐related activities, it does not appear that they are having an impact on improving these resources and practices nationally, based on these survey results.
Summary of findings and recommendations – hygiene
-
•
The importance of proper hygiene is discussed in the national policy and protocol for the management of malnutrition. The PDAOK project included more extensive guidelines, but the status of this project was not available.
-
•
Only about one‐third of households nationally and in certain regions had access to potable water and/or used appropriate methods to dispose of human wastes according to surveys in 2004 (18) and 2007 (17).
-
•
Where appropriate, programmes promoting IYCN should be enhanced to promote appropriate hygienic practices in food preparation and household environments.
-
•
Research may be needed to identify how to remove barriers and/or to improve access to potable water and utilization of other hygienic practices to reduce the transmission of disease.
Summary
Most of the key IYCN practices are promoted in the 1998 National Policy to Combat Protein‐Energy Malnutrition and Micronutrient Deficiencies, which is the only ratified national nutrition policy or strategy. The key IYCN practices and related activities that are not addressed in this policy include: the prevention and treatment of zinc deficiency, the diagnosis of iron deficiency vs. other causes of anaemia, and specific feeding methods to reduce the risk of mother‐to‐child transmission of HIV. Various agency representatives were cooperative and interested in providing information for our analyses, but we found no functioning nationally supported nutrition group to coordinate, promote, and implement nutrition‐related activities in Chad.
Despite the identified IYCN activities, little progress has been made towards reducing malnutrition and mortality among young children in Chad, and national surveys demonstrate that few infants and children benefit from optimal feeding practices.
We found very little formative research for developing country‐specific training materials. One exception was the PDAOK project in 1999–2000, which commenced with baseline surveys to guide the development of evidence‐based locally applicable training materials. Unfortunately, we found no impact evaluations to confirm whether the PDAOK project was successful in its goal of reducing malnutrition in the region where it was implemented or whether this concept had been expanded to other regions.
Although most of the key infant and young child feeding practices are promoted in the national‐level programme to manage malnutrition, we found no general nutrition programmes promoting these practices nationally. A review of the malnutrition programmes in one region identified serious gaps in human and institutional resources to carry out required activities. Adequate resources are essential to ensure that nutrition programmes are implemented as designed, and that evaluations are rigorous enough to identify effective programmes. We found very little monitoring and evaluation of available nutrition programmes to guide national policies and programme development activities. The chronic state of food insecurity, complicated by the added strain of refugees, demonstrates the critical need for continuous support for all nutrition programmes in Chad.
Supporting information
Table S1. Chad – organizations and summary of work in infant and young child nutrition (IYCN), with reported areas of IYCN activities and promotion.
Table S2. Chad – documents of national policies, strategies, and plans of action related to infant and young child nutrition (IYCN) that were identified, with summaries of key IYCN practices and activities included in each document.
Table S3. Chad – documents reporting surveys that collected data regarding barriers and beliefs surrounding infant and young child nutrition.
Table S4. Chad – research articles related to infant and young child nutrition identified by PubMed search.
Table S5. Chad – protocols, training manuals, and curricula related to infant and young child nutrition.
Table S6. Chad – programs related to infant and young child nutrition, as identified in relevant training, programmatic or monitoring and evaluation documents.
Table S7. Chad – surveys, monitoring, and evaluation activities regarding activities related to infant and young child nutrition programmes and situation.
Supporting info item
Financial support, in alphabetical order: Food and Agriculture Organization of the United Nations, Helen Keller International, Save the Children, Micronutrient Initiative, United Nations Children's Fund, United Nations World Food Programme, and the World Health Organization.
References
- 1. Central Intelligence Agency of the United States of America (2009) The World Factbook. Available at: https://www.cia.gov/library/publications/the-world-factbook/countrylisting.html
- 2. United States Agency for International Development (USAID), Famine Early Warning System Network (FEWS NET) (2009) FEWSNET – Livelihoods. Available at: http://www.fews.net/Pages/livehome.aspx
- 3. Wuehler S.E., Hess S.Y. & Brown K.H. (2011) Accelerating improvements in nutritional and health status of young children in the Sahel region of sub‐Saharan Africa: review of international guidelines on infant and young child feeding and nutrition. Matern & Child Nutrition 7 (Suppl. 1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. République du Tchad, Ministère de la Santé Publique – Tchad, Ministère de l'Action Sociale et de la Famille. (1998) Politique Nationale de Lutte Contre la Malnutrition Proteino‐énergique et les Carences en Micro Nutriments. [Google Scholar]
- 5. WHO, UNICEF (2003) Global Strategy for Infant and Young child Feeding [Electronic]. World Health Organization: Geneva. Available at: http://www.who.int/nutrition/topics/global_strategy/en/index.html [Google Scholar]
- 6. Ngoïdi S.N.D., Franco‐Joseph N., Ali A.D., Katir N. & Yomadji O. (n.d.) Le lait maternel peut‐il être de mauvaise qualité? Ndjaména.
- 7. Domay E.D. & Daliam A. (1999) Module de formation des agents de bases du P.D.A.O.K, infirmiers et sages femmes en éducation nutritionnelle.
- 8. Domay E.D., Daliam A. & Adef A. (2000) Module de formation des groupes de nutrition de la zone du PDAOK et hors zone 1. la consultation pré natale (CPN), 2. la consultation prévention de l'enfant (CPE).
- 9. République du Tchad, Ministère de la Santé Publique – Tchad, Fonds des Nations Unis pour l'Enfance (UNICEF), Organisation Mondial de la Santé (OMS) (2007) Protocole national de prise en charge de la malnutrition.
- 10. Ministère de la Santé Publique – Tchad, Direction Générale, Direction des Activités Sanitaires, Division Santé Maternelle et Infantile, Centre Nationale de Nutrition et de Technologie Alimentaire (1998) Supplémentation en vitamine A, fiche d'orientation.
- 11. Lacsala R. (n.d.) Formation en technique de production artisanale de farine de sevrage (Kanem).
- 12. Gaya F. (2007) Mission d'orientation de mise en place des relais communautaires dans le District de Gounou‐Gaya.
- 13. Dogoro Z.M.‐S. & M Abakar M.T. (2007) Rapport de formation des agents socio sanitaires et des réseaux communautaires dans la délégation régionales sanitaire du Guera.
- 14. Yomadjioutengar O., Ministère de la Santé Publique – Tchad . S'informer pour mieux s'alimenter.
- 15. Republique du Tchade, Fonds des Nations Unis pour l'Enfance (UNICEF) (2005) Programme de coopération Tchad‐UNICEF (2001–2005). Revue annuelle 2005. Rapport final.
- 16. Laevens A. (2007) Rapport d'évaluation sur la situation nutritionnelle et sanitaire au Kanem, Tchad.
- 17. United Nations Children's Fund (UNICEF), United Nations World Food Programme (WFP) (2007) Enquête de suivi de la situation alimentaire et nutritionnelle au Tchad.
- 18. Ouagadjio B., Nodjimadji K., Bagamla T., Madnodji R., Sibaye Tokindang J., Ngakoutou N. et al (2004) Enquête Démographique et de Santé Tchad 2004. INSEED et ORC Macro: Calverton, MD. [Google Scholar]
- 19. Ouagadjio B., Nodjimadji K., Ngoniri J.N., Ngakoutou N., Ignégongba K., Tokindang J. et al (1998) Enquête Démographique et de Santé, Tchad 1996–1997. Bureau Central du Recensement et Macro International Inc.: Calverton, MD. [Google Scholar]
- 20. Quigley M.A., Kelly Y.J. & Sacker A. (2007) Breastfeeding and hospitalization for diarrheal and respiratory infection in the United Kingdom Millennium Cohort Study. Pediatrics 119, e837–e842. [DOI] [PubMed] [Google Scholar]
- 21. Koyanagi A., Humphrey J.H., Moulton L.H., Ntozini R., Mutasa K., Iliff P. et al (2009) Effect of early exclusive breastfeeding on morbidity among infants born to HIV‐negative mothers in Zimbabwe. The American Journal of Clinical Nutrition 89, 1375–1382. [DOI] [PubMed] [Google Scholar]
- 22. Mihrshahi S., Oddy W.H., Peat J.K. & Kabir I. (2008) Association between infant feeding patterns and diarrhoeal and respiratory illness: a cohort study in Chittagong, Bangladesh. International Breastfeed Journal 3, 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Mihrshahi S., Ichikawa N., Shuaib M., Oddy W., Ampon R., Dibley M.J. et al (2007) Prevalence of exclusive breastfeeding in Bangladesh and its association with diarrhoea and acute respiratory infection: results of the multiple indicator cluster survey 2003. Journal of Health, Population, and Nutrition 25, 195–204. [PMC free article] [PubMed] [Google Scholar]
- 24. World Health Organization (WHO) United Nations Children's Fund (UNICEF), International Food Policy Research Institute (IFPRI), University of California Davis – Program in International and Community Nutrition (UCDavis), Food and Nutrition Technical Assistance (FANTA), Academy for Educational Development (AED) et al (2008) Indicators for Assessing Infant and Young Child Feeding Practices: Part I Definitions. Geneva. Available at: http://www.who.int/nutrition/publications/infantfeeding/9789241596664/en/index.html
- 25. de Pee S. & Bloem M.W. (2007) The bioavailability of (pro) vitamin A carotenoids and maximizing the contribution of homestead food production to combating vitamin A deficiency. International Journal for Vitamin and Nutrition Research 77, 182–192. [DOI] [PubMed] [Google Scholar]
- 26. Food and Agriculture Organization of the United Nations (FAO) (2010) FAOSTAT. Rome. Available at: http://faostat.fao.org/site/368/DesktopDefault.aspx?PageID=368#ancor
- 27. Gibson R.S., Bailey K.B., Gibbs M. & Ferguson E.L. (2010) A review of phytate, iron, zinc, and calcium concentrations in plant‐based complementary foods used in low‐income countries and implications for bioavailability. Food and Nutrition Bulletin 31 (Suppl. 2), S134–S146. [DOI] [PubMed] [Google Scholar]
- 28. Republique du Tchad, Primature, Ministère de la Santé Publique – Tchad, Secrétariat Général, Direction Générale des Activités Sanitaires, Direction de la Santé Préventive et de la Lutte Contre la Maladie et al (2005) Grandes lignes du plan d'action 2005–2007 pour la Supplémentation en vitamine A.
- 29. Aguayo V.M., Garnier D. & Baker S.K. (2007) Drops of life: Vitamin A Supplementation for Child Survival. Progress and Lessons Learned in West and Central Africa: UNICEF Regional Office for West and Central Africa, Dakar. [Google Scholar]
- 30. Zinc Task Force (2010) Country Updates and Experiences: World Map on Progress of Zinc in Diarrhea Treatment. Available at: http://izincg.org/treatment/country-exp
- 31. République du Tchad (2007) Nouveau protocole pour la prise en charge de la diarrhée, Atelier d'intégration de nouveaux protocoles dans le livret de tableau PCIME.
- 32. Hess S.Y., Lonnerdal B., Hotz C., Rivera J.A. & Brown K.H. (2009) Recent advances in knowledge of zinc nutrition and human health. Food and Nutrition Bulletin 30 (Suppl. 1), S5–S11. [DOI] [PubMed] [Google Scholar]
- 33. World Health Organization Secretariat on behalf of the participants to the Consultation (2007) Conclusions and recommendations of the WHO Consultation on prevention and control of iron deficiency in infants and young children in malaria endemic areas, Lyon, France, 12–14 June 2006. Food and Nutrition Bulletin 28, S621–S627. [DOI] [PubMed] [Google Scholar]
- 34. Renaudin P. & Lombart J.P. (1994) Anemia in infants less than 1 year old in Moundou, Chad: prevalence and etiology. Medicine Tropical (Mars) 54, 337–342. [PubMed] [Google Scholar]
- 35. Lantum D., Mutamba J. & Nyamandi T. (1999) IDD control in some African countries: Chad. ICCIDD Newsletter [serial on the Internet]. 15 Available at: http://www.iccidd.org/media/IDD%20Newsletter/1991-2006/feb1999.htm#a1 [Google Scholar]
- 36. Wyss K., Guiral C., Ndikuyeze A., Malonga G. & Tanner M. (1996) Prevalence of iodine deficiency disorders and goitre in Chad. Tropical Medicine & International Health 1, 723–729. [DOI] [PubMed] [Google Scholar]
- 37. République du Tchade . Lutte contre les troubles dus à la carence en iodé dans les régions du Ouaddaï et du Wadifira par la promotion du sel iodé. Plan du projet, Annexe A.
- 38. Renaudin P. (1997) Evaluation of the nutritional status of children less than 5 years of age in Moundou, Chad: correlations with morbidity and hospital mortality. Medicine Tropical (Mars) 57, 49–54. [PubMed] [Google Scholar]
- 39. World Health Organization (WHO), United Nations Children's Fund (UNICEF) (2009) WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: A Joint Statement by the World Health Organization and the United Nations Children's Fund. Geneva. Available at: http://www.who.int/nutrition/publications/severemalnutrition/9789241598163/en/index.html [PubMed]
- 40. Hutton G., Wyss K. & N'Diekhor Y. (2003) Prioritization of prevention activities to combat the spread of HIV/AIDS in resource constrained settings: a cost‐effectiveness analysis from Chad, Central Africa. The International Journal of Health Planning and Management 18, 117–136. [DOI] [PubMed] [Google Scholar]
- 41. The Joint United Nations Programme on HIV/AIDS (UNAIDS) (2010) UNAIDS Report on the Global AIDS Epidemic: UNAIDS. Available at: http://www.unaids.org/globalreport/Global_report.htm.
- 42. World Health Organization (WHO) (2009) Rapid Advice: Antiretroviral Therapy for HIV Infection in Adults and Adolescents. World Health Organization: Geneva. Available at: http://www.who.int/hiv/pub/arv/advice/en/ [Google Scholar]
- 43. World Health Organization (WHO) (2009) Rapid Advice: Revised WHO Principles and Recommendations on Infant Feeding in the Context of HIV. Available at: http://www.who.int/child_adolescent_health/documents/9789241598873/en/index.html
- 44. United States Agency for International Development (USAID), Famine Early Warning System Network (FEWS NET) (2005) Chad Livelihood Profiles. Available at: http://www.fews.net/docs/Publications/td_profile_en.pdf
- 45. United States Agency for International Development (USAID), Famine Early Warning System Network (FEWS NET) (2010) Tchad: Mise à jour de la sécurité alimentaire, janvier‐juin. Available at: http://www.fews.net/docs/Publications/Chad_OL_2009_12_fr.pdf
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Chad – organizations and summary of work in infant and young child nutrition (IYCN), with reported areas of IYCN activities and promotion.
Table S2. Chad – documents of national policies, strategies, and plans of action related to infant and young child nutrition (IYCN) that were identified, with summaries of key IYCN practices and activities included in each document.
Table S3. Chad – documents reporting surveys that collected data regarding barriers and beliefs surrounding infant and young child nutrition.
Table S4. Chad – research articles related to infant and young child nutrition identified by PubMed search.
Table S5. Chad – protocols, training manuals, and curricula related to infant and young child nutrition.
Table S6. Chad – programs related to infant and young child nutrition, as identified in relevant training, programmatic or monitoring and evaluation documents.
Table S7. Chad – surveys, monitoring, and evaluation activities regarding activities related to infant and young child nutrition programmes and situation.
Supporting info item


