Abstract
Although exclusive breastfeeding for the first 6 months of infant life is recommended in the UK, there is little information on the extent of exclusive breastfeeding. This study has taken the 1996 and 2003 World Health Organization (WHO) definitions of breastfeeding and investigated breastfeeding rates in the first 6 months of life in infants born to mothers enrolled in a longitudinal, representative, population‐based cohort study – the Avon Longitudinal Study of Parents and Children (ALSPAC). Information about breastfeeding and introduction of solids was available for 11 490 infants at 6 months of age (81% of live births). Exclusive breastfeeding declined steadily from 54.8% in the first month to 31% in the third, and fell to 9.6% in the fourth month mainly due to the introduction of solids to the infants. In the first 2 months, complementary feeding (breastmilk and solid/semi‐solid foods with any liquid including non‐human milk) was used in combination, and declined from 22% in the first month to 16.8% in the second due to a switch to exclusive commercial infant formula feeding. Replacement feeding (exclusive commercial infant formula or combined with any liquid or solid/semi‐solid food but excluding breastmilk) increased steadily from 21.9% in the first month to 67.1% by the seventh. This obscured the change from exclusive commercial infant formula feeding only to commercial infant formula feeding plus solids/semi‐solids, a change which started in the third month and was complete by the fifth. Using categories in the 1996 and 2003 WHO definitions, such as complementary feeding and replacement feeding, presented difficulties for an analysis of the extent of breastfeeding in this population.
Keywords: exclusive breastfeeding, longitudinal cohort study, infant feeding, child health, child nutrition, targeted interventions
Introduction
Recent changes in World Health Organization (WHO) advice on the optimum period of exclusive breastfeeding have been incorporated into the Department of Health (DH) policy (2003). The DH advice states,
Exclusive breastfeeding is recommended for the first 6 months (26 weeks) of an infant’s life.
Six months is the recommended age for the introduction of solid foods for infants.
Breastfeeding (and/or breastmilk substitutes, if used) should continue beyond the first six months, along with appropriate types and amounts of solid foods.
By emphasizing the practice of exclusive breastfeeding, the new advice draws attention to the limited information available on the nature of breastfeeding practice and the extent of exclusive breastfeeding in the UK (Yngve & Sjostrom 2001a, 2001b; Sachs 2002; Watt & Kelly 2005). In this study, we present data from a longitudinal cohort study of parents and children in the south‐west of England, describing the extent of exclusive breastfeeding throughout the first 6 months of infant life in the early 1990s. Our aim is to assess the WHO recommendation against the feeding practice of a representative UK cohort in the 1990s, and to complement the other Avon Longitudinal Study of Parents and Children (ALSPAC) publications relevant to infant nutrition (North et al. 2000; Noble et al. 2001; Northstone et al. 2001).
The total duration period of breastfeeding is correlated with a number of factors – maternal age, maternal occupation and working conditions, socio‐economic status, household smoking patterns, co‐sleeping and the use of dummies or pacifiers (Sjölin et al. 1979; Ford et al. 1994; Pérez‐Escamilla et al. 1995; Victoria et al. 1997; Yngve & Sjostrom 2001a, 2001b; Hamlyn et al. 2002; Watt & Kelly 2005). There is also evidence demonstrating that an increased total duration period of breastfeeding and exclusive breastfeeding during the first 6 months of life increases the positive health and development benefits to children (Saarinen & Kajosaari 1995; Horwood & Fergusson 1998). In light of this evidence, women are now advised to breastfeed exclusively for the first 6 months of life, and to continue breastfeeding up to 24 months or beyond while complementing breastmilk with nutritionally appropriate and adequate foods (WHO 2001).
There appears to be a process of evolution with regard to 1996, 2003) of exclusive breastfeeding, complementary feeding and replacement feeding. Many studies have included in the category of exclusive breastfeeding infants who have received one or more of the following – ritual foods, formula feeds, semi‐solids and water. This makes for great difficulty when trying to gauge the extent of the exclusive breastfeeding population at any one moment in time (de Carvalho et al. 1982; Butte et al. 1985; Hillervik‐Lindquist et al. 1991; Michaelsen et al. 1994; Yngve & Sjostrom 2001a, 2001b).
Patterns of breastfeeding
The 1996 definitions used by the WHO in making their recommendations make a distinction between infants who are exclusively breastfed and those who are predominantly breastfed. However, this distinction is missing from the glossary in ‘Infant and Young Child Feeding: A Tool for Assessing National Practices, Policies and Programmes’ (WHO 2003); as is the definition of breastfeeding. For the purposes of this study, we have used the 1996 WHO definitions for breastfeeding and predominate breastfeeding (see Table 1).There is no difference between the 1996 and 2003 definitions for exclusive breastfeeding.
Table 1.
Definitions used: ‘Global Data Bank on Breastfeeding’ (WHO 1996); and ‘Infant and Young Child Feeding: A Tool for Assessing National Practices, Policies and Programmes’ (WHO 2003)
| Requires infant to receive | Allows infant to receive | Does not allow infant to receive | |
|---|---|---|---|
| Breastfeeding (WHO 1996) | Breastmilk including expressed breastmilk – any food or liquid including non‐human milk | Any food or liquid including non‐human milk or breastmilk via a bottle | _ |
| Exclusive breastfeeding (WHO 2003) | Breastmilk including expressed breastmilk | Drops/syrups – vitamins and minerals | Anything else |
| Predominate breastfeeding (WHO 1996) | Breastmilk including expressed breastmilk | Liquids, ritual fluids, drops and syrups | Anything else (especially non‐human milk and food‐based fluids) |
| Complementary feeding (WHO 2003) | Breastmilk and solid/semi‐solid foods | Any food or liquid including non‐human milk | _ |
| Replacement feeding (WHO 2003) | Commercial infant formula | Any liquid or semi‐solid food | Does not include breastmilk or expressed breastmilk |
Exclusive breastfeeding refers to babies and infants who receive breastmilk or expressed breastmilk, syrup/drops, vitamins, minerals and medicines but nothing else. With predominate breastfeeding, babies receive breastmilk as before and other non‐milk liquids or ritual fluids, as well as syrups/drops and medicines but not solids. These two definitions contrast with the definition for breastfeeding, where an infant may receive breastmilk and any other food or liquid, including milk via a bottle. These definitions are useful in that they categorize the diverse range of infant feeding practices that take place at any one moment in time, but they do not separate expressed breastmilk from suckled breastmilk. This is important because of the effect of expressing breastmilk on maternal lactation physiology, the subsequent maintenance of maternal milk supplies and the immunological differences in breastmilk that arise from expressing breastmilk rather than breastfeeding directly (Labbok & Krasovec 1990). Unfortunately, such data are not available in the UK, and it is an area for consideration in further inquiry into breastfeeding practice in the UK.
With regard to babies who do not receive breastmilk, we have used the 2003 WHO definition of replacement feeding. This refers to ‘the use of a suitable breast‐milk substitute’ within the first 6 months of life, which is augmented after this time with ‘suitable complementary foods’ (WHO 2003, p. 117). However, one of the problems with this definition is that it does not allow for the differentiation of babies fed exclusively on commercial infant formula from those babies receiving complementary feeding before 6 months. Similarly, the definition of complementary feeding does not allow those babies who are only fed with commercial infant formula and complementary foods to be distinguished from babies who are only fed breastmilk and complementary foods. For the purposes of this study, we have used replacement feeding to refer to babies who are being fed exclusively on commercial infant formula with or without complementary foods but not receiving breastmilk during the period of inquiry; and complementary feeding to refer to babies fed on breastmilk with complementary foods and/or commercial infant formula.
The research questions that we set out to answer were:
-
•
What is the extent of exclusive breastfeeding in a representative cohort of British women over the first 6 months of their babies’ life? and
-
•
What is the extent of other forms of feeding in a representative cohort of British women over the first 6 months of their babies’ life?
Methods
The sample used for this study is derived from the ALSPAC, a prospective cohort study of 14 062 children born in the south‐west of England in 1991−1992 (Golding & the ALSPAC Team 1996). The mothers were recruited during pregnancy and their progress was followed by self‐completion questionnaires before and after the birth of their children. The ALSPAC population is broadly similar to the UK population at the 1991 census, but is under‐represented in the following categories: people living in rented accommodation, people without a car, single‐parent families, unmarried cohabiting couples, and those from an ethnic minority (Golding & the ALSPAC Team 1996).
Mothers were surveyed at 4 weeks, 6 months and 15 months after the birth of their children by postal questionnaires. Information was collected at 6 months to identify the dietary groups, and 11 490 cases were available. Answers to the questionnaires at 6 months were checked against answers in a questionnaire completed when infants were 4 weeks old. There was 97% agreement regarding initiation of breastfeeding. The majority of those that were discordant had breastfed only in the first few days. In a further questionnaire at 15 months, there was 96% agreement regarding initiation with a tendency to longer estimation of the duration of breastfeeding if asked at the later date.
At each point, the questionnaires asked mothers to comment on the feeding patterns in the intervening period. These included questions on source and type of nutrition, e.g. whether they were exclusively breastfeeding, whether they gave their babies commercial infant formula, types of solid/semi‐solid food used, and the age at which changes were made to feeding practices, such as introduction of commercial infant formula and/or solid/semi‐solid food, cessation of breastfeeding. Where a mother was exclusively breastfeeding but introduced another form of feeding, e.g. commercial infant formula, for a time limited period and then reverted to exclusive breastfeeding, she was categorized as complementary feeding from the point of introducing the other form of feeding.
Data concerned with types of drinks consumed, foods and nutrient intakes, and issues around feeding difficulties have been reported elsewhere (North et al. 2000; Noble et al. 2001; Northstone et al. 2001). The main reason for missing data was mothers stating they had started a particular food/drink but failed to specify the age of starting. By 15 months, 11 077 cases were available. Any conclusions about dropout and feeding behaviour between 6 and 15 months are unlikely to be reliable due to the small numbers involved. A total of 1084 children had data at 6 months but not at 15 months, and 671 vice versa, making the net loss of 413 cases. It is unlikely that the missing children are in the exclusive breastfeeding category. For this to be true, it would require the data to be missing on the breastfeeding variable and a combination of the variables related to other forms of feeding, i.e. not started, missing on formula, other milk, other drinks and solids.
Feeding data from the questionnaires on children up to 6 months of age were used to categorize the infants according to the definitions identified earlier and summarized in Table 1. Ethical permission for the ALSPAC study was granted by the ethics committees of United Bristol Healthcare Trust, Frenchay and Southmead Healthcare Trusts, and the study is also monitored by the ALSPAC Ethics and Law Advisory Committee.
Results
Of 14 062 live births, information about breastfeeding and introduction of solids at 4 weeks, 6 months and 15 months was available for 11 490 (81%) infants. Table 2 shows the percentage of infants in each category of feeding during each month of life.
Table 2.
Percentage of babies in feeding categories by month
| 1st* month n (%) | 2nd month n (%) | 3rd month n (%) | 4th month n (%) | 5th month n (%) | 6th month n (%) | 7th month n (%) | |
|---|---|---|---|---|---|---|---|
| Exclusive breastfeeding | 5 738 (54.8) | 4 565 (43.7) | 3 249 (31.0) | 1 012 (9.6) | 165 (1.6) | 39 (0.4) | 6 (0.1) |
| Predominate breastfeeding | 129 (1.2) | 199 (1.9) | 263 (2.5) | 146 (1.4) | 33 (0.3) | 6 (0.1) | 1 (0.0) |
| Complementary feeding | 2 308 (22.0) | 1 757 (16.8) | 2 547 (21.8) | 3 927 (37.2) | 4 148 (39.3) | 3 750 (35.5) | 3 395 (32.2) |
| Replacement feeding | 2 292 (21.9) | 3 900 (37.3) | 4 668 (44.3) | 5 368 (50.9) | 6 106 (57.8) | 6 654 (63.0) | 7 089 (67.1) |
| Other | 10 (0.1) | 25 (0.2) | 39 (0.4) | 93 (0.9) | 104 (1.0) | 109 (1.0) | 67 (0.6) |
| Valid cases | 10 474 | 10 446 | 10 485 | 10 546 | 10 556 | 10 558 | 10 558 |
| Missing cases | 1 016 | 1 044 | 1 005 | 944 | 934 | 932 | 932 |
| Total | 11 490 | 11 490 | 11 490 | 11 490 | 11 490 | 11 490 | 11 490 |
Infant will be aged 1 month at the end of the first month and so on.
Exclusive breastfeeding declined steadily in the first 3 months (Table 2), then showed a dramatic drop between the third and fourth months of life. The percentage of children who were predominately breastfed was small throughout (<2.5%), and this rate also declined at 3 months of age. In the first 2 months, complementary feeding was almost always breast and formula used in combination, and the decline from 22.1% to 16.8% was due to a switch to replacement feeding and in particular, exclusive commercial infant formula feeding. From the third month, complementary feeding showed a steady rise to a peak of 39.3% in the fifth month; this was mainly due to breastfeeding mothers beginning to introduce solids.
Replacement feeding rose steadily each month from 21.8% in the first month to 67.1% at age 6 months. However, replacement feeding as a category obscures the fact that for the first 2 months, this is mainly exclusive commercial infant formula feeding (see Fig. 1). This exclusive commercial infant formula reached a peak of 30.3% in the second month, followed by a marked decline as solids were introduced.
Figure 1.
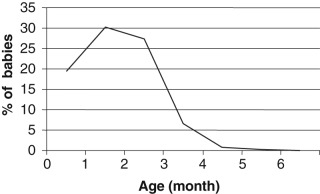
Percentage of babies who are fed exclusive commercial infant formula by month.
Discussion
This study has described the use of breastfeeding practice of a large population of British mothers in the 1990s, and categorized the sample using a range of WHO definitions from 1996 and 2003. The strengths of the study are in the broadly representative nature of the cohort and the collection of data at three time points. The main limitation is that data collection has been restricted to self‐reported questionnaires at fixed time points, and that there may be a memory effect at 6 and 15 months. This makes it difficult to pinpoint exactly the various transition points from exclusive to predominant breastfeeding and on to complementary feeding, as well as the transition from exclusive commercial infant formula feeding to replacement feeding.
Our experience of using the WHO categories was similar to that reported by Lanigan et al. (2001) in that there is no category available for infants who only receive breastmilk and solid/semi‐solid foods. In this study, we include them in complementary feeding. However, there may be differences in future health outcomes between this group and infants who receive breastmilk plus commercial infant formula and solid/semi‐solid foods. Also, there is no category available for exclusive commercial infant formula‐fed infants. Although the WHO definitions (2003) continue to evolve, there is no satisfactory WHO term to clearly describe this particular group. Here we include these infants under replacement feeding. In this paper, we have used the replacement feeding category to also include those children who are making the transition from exclusive commercial infant formula feeding to commercial infant formula feeding plus solid/semi‐solid foods, but we have highlighted the transition point from exclusive commercial infant formula fed to formula and weaning foods. Again, there may be differences in the future health experiences of these two groups, which may warrant a clearer set of definitional terms (Ong et al. 2006).
In a similar vein, the use of the 2003 WHO complementary feeding category is not helpful, as the definition is broad and ill‐defined. It may include mothers who are breastfeeding five times a day but also introducing a formula feed at night, as well as mothers who use formula milk during the day but give a breastfeed to settle their child before bed. If we only focus on exclusively and predominately breastfed children, then the extent of breastfeeding in the general population is hidden. Refined definitions may be helpful in teasing out the nuances of breastfeeding and the use of commercial infant formula in this population (McCann et al. 1994; Piwoz et al. 1996). However, there are data collection issues around the accurate recording of feed duration and frequency, and how this correlates with milk flow, energy value and nutritional composition (Hörnell et al. 1999; Aarts et al. 2000).
The proportion of children who were exclusively breastfed in the ALSPAC population ranged from 54.8% to 31% in the first 3 months, and fell down to 0.1% by the age of 6 months. Our data showed a higher proportion of women exclusively breastfeeding in the second (43.7%) and third months (31%) than was reported in Infant Feeding 1995 (Foster et al. 1997), where only 21% of women were breastfeeding during this period. This may be due to the slight bias in the ALSPAC towards more affluent families, so that the true level of breastfeeding in the general population is likely to be a little lower than this. This supposition seems to be confirmed when comparing exclusive breastfeeding rates between the ALSPAC cohort and the Millennium Cohort Study (Watt & Kelly 2005). The data from the Millennium Cohort indicate an exclusive breastfeeding rate of 34% after 1 month, falling to 3% at the fourth month and 0.3% by the sixth month.
Nevertheless, the proportion of mothers who were exclusively breastfeeding up to 6 months in ALSPAC was far below Sachs’ projection (2002) of 3% of UK babies. Infants were continuing to be breastfed into the seventh month of life, but this was more likely to be with other sources of nutrition in the form of solids, formula or other drinks from the fourth month onwards. At the time that these mothers were introducing solid/semi‐solid foods to their infants, the guidance given in Infant Feeding 1985 (Martin & White 1988) was clear about not introducing solids prior to 3 months of age. Indeed, most mothers in this study started giving solids during the third month of life. These data are in line with other recent studies in the UK which show that over 90% of women have introduced solids by month 4 (Mills & Tyler 1992; White et al. 1992; Foster et al. 1997; Thomas & Avery 1997; Hamlyn et al. 2002), and in contrast to the 56% estimated by Martin & Monk (1982).
The changes in feeding category seemed to have three phases. The first phase was between the first and second months when 16% of women changed their breastfeeding practice. The majority of women who were exclusively breastfeeding switched to complementary feeding, but few gave up the breast completely – only 1.8% of the exclusive breastfeeding group in the first month gave up by the second month. In comparison, of the mothers giving complementary feeds in the first month, 64.7% gave up breastfeeding by the second month.
The second phase ran from the second to fourth month, and was characterized by a more gradual loss of the exclusive breastfeeding population and an increase in the proportion of women who were complementary feeding. Finally, in the third phase from the fourth to sixth month exclusive breastfeeding tailed off completely, and complementary feeding started to decline gradually so that although a third of women were breastfeeding at 6 months of age, virtually none were exclusively breastfeeding. The data on complementary feeding at 6 months from this study are broadly in line with that reported by Hamlyn et al. (2002), although they report a breastfeeding prevalence rate of 22% in England in 2000. Further comparisons are difficult to make with Hamlyn et al.’s (2002) work as they do not differentiate between exclusively/predominately breastfed babies and breastfed babies who may be receiving commercial infant formula and/or solids/semi‐solids.
This study presents data from a UK longitudinal study of infant feeding practice that will help place current UK feeding practice in context. An appreciation of these patterns of feeding may have implications for the working practices of health professionals with regard to targeted interventions. This study highlights the transitions in feeding practice from exclusive/predominate breastfeeding to complementary, and from exclusive commercial infant formula feeding to replacement feeding. It provides information against which current feeding practices may be compared in the light of the DH (2003) recommendations. This study supports the notion that there are a sizeable number of breastfeeding mothers (exclusive/predominate breastfeeding, and complementary feeding) who could be targeted for education and support by midwives and health visitors in line with DH infant feeding recommendations (Sikorski et al. 2002; DH 2003). Although this study suggests that the number of women who are likely to exclusively breastfeed up to 6 months is probably small (Watt & Kelly 2005), it indicates the extent of women who breastfeed with other forms of nutrition to 6 months, and highlights the possibility of increasing this proportion.
Acknowledgements
We are extremely grateful to all the mothers who took part and to the midwives for their co‐operation and help in recruitment. The ALSPAC study team includes interviewers, computer and laboratory technicians, clerical workers, research scientists, volunteers, managers, receptionists and nurses. This study would not have been undertaken without the financial support of the Medical Research Council, the Wellcome Trust, the UK Department of Health, the Department of the Environment, a variety of medical research charities and commercial companies. While the ALSPAC study has received financial support from commercial companies, some of whom are infant food manufacturers, no funding has been received from infant food manufacturers to support the development of this paper. For further details on ALSPAC funding, please see http://www.alspac.bris.ac.uk/protocol/Section12.shtml. The authors wish to thank the MCN reviewers for their helpful comments on previous drafts of this paper.
References
- Aarts C., Kylberg E., Hornell A., Hofvander Y., Gebre‐Medhin M. & Greiner T. (2000) How exclusive is exclusive breastfeeding? A comparison of data since birth with current status data. International Journal of Epidemiology 29, 1041–1046. [DOI] [PubMed] [Google Scholar]
- Butte N., Wills C., Jean C., Smith E. & Garza C. (1985) Feeding patterns of exclusively breast fed infants during the first four months of life. Early Human Development 12, 291–300. [DOI] [PubMed] [Google Scholar]
- De Carvalho M., Robertson S., Merkatz R. & Klaus M. (1982) Milk intake and frequency of feeding in breast‐fed infants. Early Human Development 7, 155–163. [DOI] [PubMed] [Google Scholar]
- Department of Health (DH ) (2003) Infant Feeding Recommendation Available at: http://www.dh.gov.uk/assetRoot/04/09/69/99/0496999.pdf
- Ford R., Mitchell E., Scragg R., Stewart A., Taylor B. & Allen E. (1994) Factors adversely associated with breast feeding in New Zealand. Journal of Paediatrics and Child Health 30, 483–489. [DOI] [PubMed] [Google Scholar]
- Foster K., Lader D. & Cheesborough S. (1997) Infant Feeding 1995. The Stationary Office: London. [Google Scholar]
- Golding J. & the ALSPAC Team (1996) Children of the nineties: a resource for assessing the magnitude of long‐term effects of prenatal and perinatal events. Contemporary Review of Obstetrics and Gynaecology 8, 89–91. [Google Scholar]
- Hamlyn B., Brooker S., Oleinikova K. & Wands S. (2002) Infant Feeding: A Survey Conducted on Behalf of the Department of Health, the Scottish Executive, the National Assembly for Wales and the Department of Health, Social Security & Public Safety in Northern Ireland. The Stationary Office: London. [Google Scholar]
- Hillervik‐Lindquist C., Hofvander Y. & Sjölin S. (1991) Studies on perceived breast milk insufficiency. IV. Relation to the weaning process. Journal of Human Nutrition and Dietetics 4, 333–342. [Google Scholar]
- Hörnell A., Aarts C., Kylberg E., Hofvander Y. & Gebre‐Medhin M. (1999) Breastfeeding patterns in exclusively breastfed infants: a longitudinal prospective study in Uppsala, Sweden. Acta Paediatrica 88, 203–211. [DOI] [PubMed] [Google Scholar]
- Horwood L. & Fergusson D. (1998) Breastfeeding and later cognitive and academic outcome. Pediatrics 101, 1–7. [DOI] [PubMed] [Google Scholar]
- Labbok M. & Krasovec K. (1990) Toward consistency in breastfeeding definitions. Studies in Family Planning 21, 226–230. [PubMed] [Google Scholar]
- Lanigan J., Bishop J., Kimber A. & Morgan J. (2001) Systematic review concerning the age of introduction of complementary foods to the healthy full‐term infant. European Journal of Clinical Nutrition 55, 309–320. [DOI] [PubMed] [Google Scholar]
- McCann M., Bender D. & Rangel Sharpless M. (1994) Infant feeding in Bolivia: a critique of the World Health Organisation indicators applied to demographic and health survey data. International Journal of Epidemiology 23, 129–137. [DOI] [PubMed] [Google Scholar]
- Martin J. & Monk J. (1982) Infant Feeding 1980. OPCS: London. [Google Scholar]
- Martin J. & White A. (1988) Infant Feeding 1985. HMSO: London. [Google Scholar]
- Michaelsen K., Larsen P., Thomsen B. & Samuelson (1994) The Copenhagen cohort study on infant nutrition and growth: breast milk intake, human milk macronutrient content, and influencing factors. American Journal of Clinical Nutrition 59, 600–611. [DOI] [PubMed] [Google Scholar]
- Mills A. & Tyler H. (1992) Food and Nutrient Intakes of British Infants Aged 6–12 Months. HMSO: London. [Google Scholar]
- Noble S. & Emmett P. & the ALSPAC Study Team (2001) Food and nutrient intake in a cohort of 8‐month‐old infants in the South‐west of England in 1993. European Journal of Clinical Nutrition 55, 698–707. [DOI] [PubMed] [Google Scholar]
- North K., Emmett P. & Noble S. & the ALSPAC Study Team (2000) Types of drinks consumed by infants at 4 and 8 months of age: sociodemographic variations. Journal of Human Nutrition and Dietetics 13, 71–82. [DOI] [PubMed] [Google Scholar]
- Northstone K., Emmett P., Nethersole F. & the ALSPAC Study Team (2001) The effect of age of introduction to lumpy solids on foods eaten and reported feeding difficulties at 6 and 15 months. Journal of Human Nutrition and Dietetics 14, 43–54. [DOI] [PubMed] [Google Scholar]
- Ong K., Emmett P., Noble S., Ness A., The ALSPAC Study Team & Dunger D. (2006) Dietary energy intake at age 4 months predicts postnatal weight gain and childhood body mass index. Pediatrics 117, e503–e508. (10.1542/peds.2005‐1668). [DOI] [PubMed] [Google Scholar]
- Pérez‐Escamilla R., Lutter C., Segall A., Rivera A., Trevino‐Siller S. & Sanghvi T. (1995) Exclusive breast feeding duration is associated with attitudinal socio‐economic and biocultural determinants in three Latin American Countries. Journal of Nutrition 125, 2972–2984. [DOI] [PubMed] [Google Scholar]
- Piwoz E., Creed de Kanashiro H., Lopez de Romana G., Black R. & Brown K. (1996) Feeding practices and growth among low‐income Peruvian infants: a comparison of internationally recommended definitions. International Journal of Epidemiology 25, 103–114. [DOI] [PubMed] [Google Scholar]
- Saarinen U. & Kajosaari M. (1995) Breastfeeding as prophylaxis against atopic disease: prospective follow‐up study until 17 years old. Lancet 346, 1065–1069. [DOI] [PubMed] [Google Scholar]
- Sachs M. (2002) Exclusive breastfeeding. MIDIRS Midwifery Digest 12, 244–248. [Google Scholar]
- Sikorski J., Renfrew M., Pindoria S. & Wade A. (2002) Support for breastfeeding mothers [Cochrane review]. The Cochrane Library Issue 4. Oxford Update Software. [DOI] [PubMed] [Google Scholar]
- Sjölin S., Hofvander Y. & Hillervik C. (1979) A prospective study of individual courses of breast feeding. Acta Paediatrica Scandinavica 68, 521–529. [DOI] [PubMed] [Google Scholar]
- Thomas M. & Avery V. (1997) Infant Feeding in Asian Families: Early Feeding Practices and Growth. HMSO: London. [Google Scholar]
- Victoria C., Behague D., Barros F., Olinto M. & Weiderpass E. (1997) Pacifier use and short breastfeeding duration: cause, consequence, or coincidence? Pediatrics 99, 445–453. [DOI] [PubMed] [Google Scholar]
- Watt R. & Kelly Y. (2005) Breastfeeding initiation and exclusion duration at 6 months by social class – results from the Millennium Cohort Study. Public Health Nutrition 8, 417–421 (5). [DOI] [PubMed] [Google Scholar]
- White A., Freeth S. & O’Brien M. (1992) Infant Feeding 1990. HMSO: London. [Google Scholar]
- World Health Organization (1996) Global Data Bank on Breastfeeding. WHO: Geneva. [Google Scholar]
- World Health Organization (2001) 54th World Assembly. Global Strategy for Infant and Young Child Feeding: The Optimal Duration of Exclusive Breastfeeding. WHO: Geneva. [Google Scholar]
- World Health Organization (2003) Infant and Young Child Feeding: A Tool for Assessing National Practices, Policies and Programmes. WHO: Geneva. [Google Scholar]
- Yngve A. & Sjostrom M. (2001a) Breastfeeding determinants and a suggested framework for action in Europe. Public Health Nutrition 4(2B), 729–739. [DOI] [PubMed] [Google Scholar]
- Yngve A. & Sjostrom M. (2001b) Breastfeeding in countries of the European Union and EFTA: current and proposed recommendations, rationale, prevalence, duration and trends. Public Health Nutrition 4(2B), 631–645 [erratum in Public Health Nutrition 4(6), 1306]. [DOI] [PubMed] [Google Scholar]


