Abstract
In a 4‐year follow‐up of a randomized controlled trial, this study aimed to evaluate the longer‐term effects of a peer‐led infant feeding intervention that was delivered during the first year of life. The original intervention used monthly home visits from trained volunteers to improve infant feeding practices among a sample of low‐income mothers in two disadvantaged London boroughs. Outcome measures at follow‐up included children's eating and drinking habits, general and dental health, and BMI. Data were collected via structured face‐to‐face interviews and postal questionnaires. Of 212 women who completed the original trial, 101 took part in the follow‐up (55 intervention, 46 control). Children's mean age at follow‐up was 4 years 7 months. There is little evidence that the intervention had an important effect on children's current BMI, caries levels or consumption of fruit and vegetables. However, mothers from the intervention group had better nutritional knowledge and confidence. Intervention group children also consumed more pure fruit juice [relative risk (RR) = 1.57; 95% confidence interval (CI) 0.99, 2.49] and were more likely to never drink squash (RR = 1.76; 95% CI 1.20, 2.58). The data suggest that the original peer support intervention had a small number of positive long‐term effects.
Keywords: follow‐up, infant feeding, randomized controlled trial, social support, weaning
Introduction
Dietary exposure during critical periods in early childhood can have significant implications for a child's health and development, as well as for health in adulthood (Demmelmair et al. 2006). Well‐established are the short‐ and long‐term beneficial effects of breastfeeding (Horta et al. 2007; Ip et al. 2007). Another key issue is the timing of the first introduction of solid foods. There is evidence that early weaning is related to rapid weight gain in infancy (Morgan et al. 2004; Sloan et al. 2007), which in turn has been shown to increase the risk of subsequent obesity (Baird et al. 2005; Reilly et al. 2005). In adults, overweight and obesity are significant risk factors for coronary heart disease (WHO 2002). High salt intake is associated with raised blood pressure in children, and blood pressure tracks into adult life (He & MacGregor 2006; Chen & Wang 2008). A systematic review on the relationship between early weaning (at <4 months of age) and allergic disease showed that early feeding of solids is associated with eczema (Tarini et al. 2006). Not least, weaning practices that involve a high and frequent consumption of non‐milk extrinsic sugars, such as the use of feeding bottles for sugary drinks, are associated with an increased risk of dental caries (Hallett & O'Rourke 2002).
The results of the latest UK Infant Feeding Survey demonstrated inequalities in infant feeding, with young mothers and mothers from lower socio‐economic backgrounds being least likely to follow professional recommendations (SACN 2008). This contributes to further health inequalities when their children become adults. Effective support is needed especially for children from low‐income families to encourage good dietary habits from infancy.
In relation to breastfeeding, promising results were achieved through the provision of social support to new mothers, which in a Cochrane review was shown to be effective in reducing the cessation of exclusive breastfeeding (Britton et al. 2007). While interventions to promote breastfeeding have been extensively investigated, few good‐quality studies have evaluated programmes on recommended infant feeding practices during the weaning period and beyond (Tedstone et al. 1998; National Institute for Health and Clinical Excellence 2008). Also, due to a lack of long‐term follow‐ups, very little is known about later health outcomes of such interventions.
The only randomized controlled trial with a long‐term follow‐up, the Irish Community Mothers Programme, showed that social support by ‘community mothers’ significantly improved certain feeding practices in infants under 1 year of age from low‐income families in Dublin (Johnson et al. 1993). The 7‐year follow‐up showed sustained beneficial effects on parenting skills and maternal self‐esteem (Johnson et al. 2000).
The aim of the Infant Feeding Peer Support Trial was to design, implement and evaluate a social support intervention to promote recommended infant feeding practices in a sample of lower income mothers (Watt et al. 2009). Participants were 312 new mothers who had given birth between September 2002 and November 2003. The women were recruited at baby clinics located in the more disadvantaged areas of Camden and Islington (London, UK) where Sure Start programmes existed. Exclusion criteria were: women under 17 years old; infants diagnosed with a serious medical condition or on special diets; infants aged over 12 weeks; women or their partners from social class I. Participants were randomized into intervention (157) and control group (155), using random‐digit computer tables. Local mothers (volunteers) were trained to provide practical, non‐judgemental support on infant feeding and weaning practices. Mothers in the intervention group received monthly home visits from when the baby was 3 months old until their first birthday. Women in the control group received standard professional care. A description of the process of setting up a social support infant feeding intervention was published elsewhere (Watt et al. 2006). Nutritional data and anthropometric measurements were collected at 3 months (baseline) and when the children were 12 months (post‐intervention) and 18 months (follow‐up) old. The primary outcome, vitamin C intake from fruit, remained unaffected. But, at follow‐up, intervention group children had a higher intake of certain fruits and vegetables and were less likely to be using a baby bottle. Also, the home visits positively affected mother's feeding knowledge and confidence, and were much valued by recipients and volunteers (Watt et al. 2009).
The present study was conducted to evaluate the longer‐term impact of the original intervention.
Key messages
-
•
The peer support that was delivered during the first year of life had some measurable positive long‐term effects on children's drinking habits and mothers' nutritional knowledge and confidence.
-
•
There was little evidence of an important long‐term effect on fruit and vegetable consumption, children's BMI or dental caries.
-
•
This kind of support potentially benefits both recipients and volunteers.
-
•
Future research should aim to engage with the most vulnerable mothers.
Materials and methods
This study is a single blinded 4‐year follow‐up of a community‐based randomized controlled trial. Ethical approval was granted by the Camden and Islington Community Local Research Ethics Committee.
Participants
Potential participants were the 182 mother‐and‐child pairs who completed the original trial and gave consent to be contacted for further research. Mothers who stated that they did not want to be contacted again, and children who were now on a special diet due to medical problems or diagnosed with a serious medical condition were excluded from the current follow‐up.
With Camden and Islington being areas of high mobility, only 113 (out of 182) potential participants could be reached. Of them, 101 agreed to take part in this follow‐up. The reasons for declining to participate were time constraints or health issues. Taking into account all potential participants (182), response rate was 55%. Based on the number of those who could effectively be contacted (113), response rate was 89% (see Fig. 1 flow chart).
Figure 1.
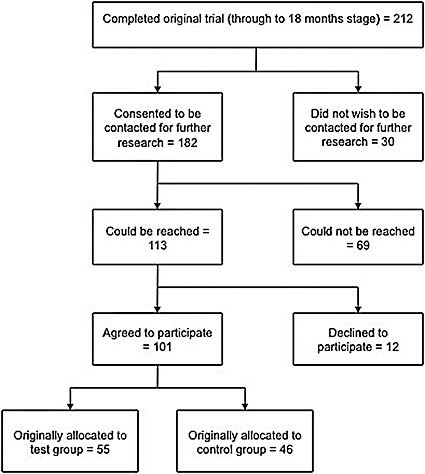
Flow diagram illustrating the identification of participants included in 4‐year follow‐up.
Outcome measures
Outcome measures were growth (height, weight, BMI), general and oral health, dietary habits, mothers' nutritional knowledge and confidence, and infant feeding practices with subsequent children. In addition, the retrospective views of the original intervention from both intervention mothers and volunteers were also assessed.
Procedures
The investigator (AS) was blinded to group allocation during data collection and entry. Data were collected mainly via structured face‐to‐face interviews during a one‐off home visit. Written consent was obtained during the visits, prior to any data collection. Where a home visit was not feasible, participants were interviewed via telephone. In these cases, height, weight and dental status could not be measured, and written consent was obtained via post. After the home visit or telephone interview, intervention group mothers were sent an additional short questionnaire about their retrospective views of the intervention. A second postal questionnaire was sent to the former volunteers, to assess the potential impact of being involved in the project on their careers or any other aspects of their lives. The data collection took place between February and July 2008.
Nutritional data
In a face‐to‐face interview, questions were asked on children's dietary habits and problems, drinks consumption, bottle use, general health problems during the past 3 months, oral‐health‐related behaviour, mother's nutritional knowledge and confidence and, if applicable, feeding practices with any subsequent children. Most questions were taken from published studies and surveys such as the ‘National Diet and Nutrition Survey (NDNS) for children aged 1½ to 4½ years’ (Gregory et al. 1995). Fruit and vegetables consumption was measured using the same 19‐item food frequency questionnaire as in the original study.
Anthropometric data
During the home visits, children's weight was measured using calibrated digital Soehnle scales, without shoes and with light clothing. Weight was recorded to the nearest 0.1 kg. Height was measured using a portable, telescopic stadiometer and recorded to the nearest 0.1 cm. The data collector was trained in accurate measurement techniques according to those used in the NDNS. For each height and weight, two measurements were taken and the mean used for the analysis.
Body mass index (BMI) was derived from mean height and weight. Overweight and obesity were determined using the UK cut‐off points as published by Chinn & Rona (2004).
Dental status
The outcome measure for dental status was the dmft index (decayed, missing and filled deciduous teeth). Children were examined while standing in front of the sitting examiner. The diagnosis was visual using a sterilized plane mouth mirror and a MAG‐LED™ Mini Maglite® torch (MAG Instrument Inc, Ontario, California, USA). Data were recorded by tooth. Teeth were coded as decayed, filled or missing according to British Association for the Study of Community Dentistry (BASCD) criteria (Pitts & Evans 1997). The data collector (AS) was a trained and registered dentist.
Statistical analysis
All analyses were carried out in Statistical Package for the Social Sciences (SPSS, version 14.0). Blinding to group allocation was maintained during data entry. Outcomes were compared between intervention and control groups. For the continuous outcomes that were normally distributed, the two groups were compared by t‐tests. Where continuous variables were not normally distributed, the Mann−Whitney U‐test was used. Categorical data were analysed using chi‐squared tests. Where the expected numbers in one or more cells of the 2 × 2 table were small, the P‐value was derived from Fisher's Exact test. Results were expressed as relative risks (RR) for binary outcomes or differences in means for continuous outcomes with a 95% confidence interval (CI). Statistical significance was defined at the 5% level. The P‐values are two‐sided. To account for differences in mother's educational attainment between the groups, binary logistic regression (for categorical outcomes) and multiple normal regression (for continuous outcomes) were carried out.
Results
Although a sample size calculation was carried out for the main trial, this was not practicable for the long‐term follow‐up; these results are, therefore, exploratory.
Of the participating mothers, 55 (54.5%) had originally been allocated to the intervention group and 46 (45.5%) to the control group. Telephone interviews were held with 13 mothers (12.9%). Children's mean age at the time of the interview was 4 years and 7 months (ranging from 4 years to 5 years 2 months). Of all children, 59 (58.4%) were boys. The mean age of the participating mothers at birth of the index child was 32 years and 29 years for those who were not followed up. About half of the mothers in this sample (51.5%) had a degree or higher qualification (32.7% for non‐responders at 18‐month stage). The groups were well‐matched regarding children's age and gender. Mother's educational attainment was lower in the intervention group, with 30.9% who never graduated from school or whose highest level of education were O‐levels or GCSE's (control group: 15.2%). All results remained unchanged when adjusting for maternal education and, hence, only unadjusted results are presented.
Eating and drinking habits
Table 1 lists the percentages of children regularly (at least once a week) consuming various types of fruit and vegetables. The intervention does not appear to have had a positive longer‐term effect on fruit and vegetable consumption. The only significant difference was that children in the control group consumed more baked beans (RR = 0.54; 95% CI 0.34, 0.85).
Table 1.
Fruits and vegetables – percentage of regular consumers (at least once a week) at age 4–5
| Intervention | Control | P‐value | RR | 95% CI | |||
|---|---|---|---|---|---|---|---|
| n/N | % | n/N | % | ||||
| Chips | 23/55 | 41.8 | 18/46 | 39.1 | 0.78 | 1.07 | 0.66, 1.72 |
| Other potatoes | 48/55 | 87.3 | 39/46 | 84.8 | 0.72 | 1.03 | 0.88, 1.21 |
| Sweet potatoes | 8/54 | 14.8 | 13/46 | 28.3 | 0.10 | 0.52 | 0.24, 1.15 |
| Carrots | 49/54 | 90.7 | 41/46 | 89.1 | 0.79 | 1.02 | 0.89, 1.16 |
| Other root vegetables | 18/55 | 32.7 | 17/46 | 37.0 | 0.66 | 0.89 | 0.52, 1.51 |
| Leafy green vegetables | 48/55 | 87.3 | 40/46 | 87.0 | 0.96 | 1.00 | 0.86, 1.17 |
| Peas | 29/55 | 52.7 | 31/45 | 68.9 | 0.10 | 0.77 | 0.56, 1.05 |
| Other green vegetables | 46/55 | 83.6 | 37/46 | 80.4 | 0.68 | 1.04 | 0.87, 1.25 |
| Baked beans | 17/55 | 30.9 | 26/45 | 57.8 | 0.007 | 0.54 | 0.34, 0.85 |
| Other beans and pulses | 18/55 | 32.7 | 16/46 | 34.8 | 0.83 | 0.94 | 0.54, 1.63 |
| Tomatoes | 46/55 | 83.6 | 37/46 | 80.4 | 0.68 | 1.04 | 0.87, 1.25 |
| Peppers | 23/55 | 41.8 | 20/46 | 43.5 | 0.87 | 0.96 | 0.61, 1.51 |
| Bananas | 41/55 | 74.5 | 40/45 | 88.9 | 0.07 | 0.84 | 0.70, 1.01 |
| Apples | 53/55 | 96.4 | 41/45 | 91.1 | 0.27 | 1.06 | 0.95, 1.17 |
| Pears | 36/55 | 65.5 | 27/45 | 60.0 | 0.57 | 1.09 | 0.80, 1.48 |
| Citrus fruits | 40/55 | 72.7 | 36/45 | 76.0 | 0.40 | 0.91 | 0.73, 1.13 |
| Soft fruit | 41/55 | 74.5 | 37/45 | 82.2 | 0.36 | 0.91 | 0.74, 1, 11 |
| Dried fruit | 26/55 | 47.3 | 27/45 | 60.0 | 0.21 | 0.79 | 0.55, 1.14 |
| Tinned fruit | 5/55 | 9.1 | 7/45 | 15.6 | 0.32 | 0.58 | 0.20, 1.71 |
The consumption of various drinks is shown in Table 2, as well as the distribution of certain drinking habits. Frequency of consumption for milk and water was similar in both groups. More intervention group children drank pure, unsweetened fruit juice on a daily basis compared with the control group (RR = 1.57; 95% CI 0.99, 2.49). It was also more likely for intervention group children never to be given squash (RR = 1.76; 95% CI 1.20, 2.58). Daily consumption of tea, fizzy drinks or ready‐to‐drink soft drinks was rare in both groups (results not shown). Outcomes relating to drinking utensils and habits were consistently more favourable among intervention group children, although the differences were not statistically significant. Fewer intervention group children used feeder beakers with a spout as their main drinking utensil, used a baby bottle after their 4th birthday or usually took a bottle into bed. No difference was found in the consumption of bedtime drinks other than water (results not shown).
Table 2.
Consumption of various drinks/drinking habits at age 4–5
| Intervention (N = 55) | Control (N = 46) | P‐value | RR | 95% CI | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Milk, at least once a day | 35 | 63.6 | 32 | 69.6 | 0.53 | 0.92 | 0.69, 1.21 |
| Plain water, at least once a day | 51 | 92.7 | 40 | 87.0 | 0.33 | 1.07 | 0.93, 1.22 |
| Pure unsweetened fruit juice, at least once a day | 30 | 54.5 | 16 | 34.8 | 0.05 | 1.57 | 0.99, 2.49 |
| Squash, never | 40 | 72.7 | 19 | 41.3 | 0.001 | 1.76 | 1.20, 2.58 |
| Usually using a feeder beaker with spout | 1 | 1.8 | 5 | 10.9 | 0.09* | 0.17 | 0.02, 1.38 |
| Still using a baby bottle at age 4 | 7 | 12.7 | 9 | 19.6 | 0.35 | 0.65 | 0.26, 1.61 |
| Usually going to bed with a baby bottle | 5 | 9.1 | 8 | 17.4 | 0.22 | 0.52 | 0.18, 1.49 |
Fisher's Exact test.
Confectionary consumption was similar in both groups. Salt was rarely added to food at the table in either group (results not shown).
Height and weight
Measurements of height and weight were obtained for 85.1% (N = 86) of the sample. Mean BMI was 16.3 (ranging from 12.3 to 25.3). According to the UK cut off points for BMI for overweight and obesity, 9.3% of all measured children were overweight and 7.0% were obese at the time of the interview. There was no significant difference in BMI or levels of overweight and obesity between the groups [mean difference (MD) = 0.42; 95% CI –0.40, 1.24].
General and dental health
Table 3 shows the percentage of children having experienced at least one health problem during the 3 months preceding the interview, as reported by the mother; and caries experience at age four. Mothers from the intervention group were less likely to report that their child experienced any health problems (RR = 0.62; 95% CI 0.43, 0.90). There was no evidence of a difference between groups regarding the consultation of medical services or whether the children were prescribed any medication.
Table 3.
Health problems during the 3 months preceding the interview, as reported by the mother/caries experience at age 4–5
| Intervention | Control | P‐value | RR | 95% CI | |||
|---|---|---|---|---|---|---|---|
| n/N | % | n/N | % | ||||
| Experienced at least one health problem | 23/55 | 41.8 | 31/46 | 67.4 | 0.01 | 0.62 | 0.43, 0.90 |
| Percentage of children with dmft > 0 | 7/44 | 15.9 | 5/41 | 12.2 | 0.62 | 1.31 | 0.45, 3.79 |
The dental examination was carried out for 84.2% of all children (N = 85). Caries had been experienced by 14.1% and mean dmft was 0.27. The intervention group had a higher risk of caries than the control group but the difference was small and based on small numbers with caries (RR = 1.31; 95% CI 0.45, 3.79). Similarly, there was no evidence of important difference regarding oral health‐related behaviour such as reported dental attendance and oral hygiene (data not shown).
Mother's nutritional knowledge and confidence
Data on mother's nutritional knowledge and confidence are presented in Table 4. In terms of knowledge, mothers from the intervention group performed better than control group mothers. They were more likely to correctly answer five or six knowledge questions out of six (RR = 1.67; 95% CI 1.06, 2.64). Intervention group mothers were also more likely to answer ‘very confident’ when asked: ‘How confident are you that you know what foods are good for your child?’ (RR = 1.59; 95% CI 1.09, 2.31).
Table 4.
Mother's nutritional knowledge and confidence
| Intervention (N = 55) | Control (N = 46) | P‐value | RR | 95% CI | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| 5 or 6 correct answers (out of six knowledge questions) | 32 | 58.2 | 16 | 34.8 | 0.02 | 1.67 | 1.06, 2.64 |
| Feels ‘very confident’ to know what foods are recommended by health professionals | 21 | 38.2 | 17 | 37.0 | 0.90 | 1.03 | 0.62, 1.71 |
| Feels ‘very confident’ to know what foods are good for child | 38 | 69.1 | 20 | 43.5 | 0.01 | 1.59 | 1.09, 2.31 |
| Feels ‘very confident’ in being able to provide these foods | 42 | 76.4 | 31 | 67.4 | 0.32 | 1.13 | 0.88, 1.45 |
Feeding practices with subsequent children
Questions were asked on breastfeeding initiation and duration, and the use of baby bottles. Only 42.6% of all children (N = 43) had at least one younger sibling. Therefore, statistical power was too low to test for differences between the groups (data not shown).
Feedback from intervention group and volunteers
Of 55 mothers originally allocated to the intervention group, 35 returned the feedback questionnaire. Feedback from the intervention mothers was predominantly positive. While 88.2% said they would recommend the peer support to a friend or relative, 57.1% found the support beneficial or very beneficial. Perceived benefits of the intervention were the practical and emotional support, reassurance and a raised awareness regarding infant nutrition. The two main criticisms were the level of the information provided, which, by some, was perceived as too basic; and the number of visits, as some mothers had received only one or two visits because of organizational problems. Some examples of mother's statements:
‘I knew most of the information she gave me. The most beneficial part of the project for me was that it made me stop and question/think about what I was feeding my child’. (Mother A)
‘I wasn't quite sure what/when to feed my growing baby (past the breastfeeding stage). I found no answer through “normal” channels. . . I felt the volunteer was a great reassurance/source of ideas and advice – it has also helped me change some of our own dietary habits’. (Mother B)
‘The volunteer's support in continuing breastfeeding when all my peers had stopped was useful’. (Mother C)
Due to the high mobility in the area, only eight volunteers (out of 16) returned the volunteer questionnaire. The volunteers were very positive overall about their participation in the study. According to the volunteers, the study had positively affected their own family's diet and nutrition and their self‐esteem. Also, volunteering had helped regarding their career and future prospects: six of them felt that their current situation was linked to their experience as a peer supporter in the study.
Two examples of volunteer's statements:
‘Many of my current roles – i.e. employee of Camden/nursing student may not have happened without the experience of the feeding project’. (Volunteer A)
‘I became motivated to further my education and become a teacher’. (Volunteer B)
Discussion
The results indicate that the original intervention had limited long‐term impact. There was, however, a suggestion of some positive effects, mainly on drinking habits. Intervention group children consumed significantly more pure fruit juice, but less squashes. There was also a tendency for intervention group children to have fewer undesirable habits such as using feeder beakers and baby bottles. Recommendations on drinks consumption and drinking utensils had indeed been a focus of the intervention. Research suggests that children who regularly consume sugar‐sweetened beverages between meals may have a greater risk of becoming overweight (Dubois et al. 2007). In addition, frequent consumption of sugary drinks is a known risk factor for dental caries in children (Wendt et al. 1996; Seow et al. 2009). Inappropriate bottle‐feeding behaviours, such as addition of sweetened liquids, sipping from the bottle during the day, sleeping with the bottle and bottle‐feeding beyond 12 months have been associated with early childhood caries (Hallett & O'Rourke 2002). The Department of Health (2007) recommends that children drink from a normal cup as soon as they are ready. Non‐spill (valved) beakers are especially not recommended as they encourage longer drinking times, which may hinder speech development and damage teeth. Mothers were also given information about pure, unsweetened fruit juice counting as one portion of fruit towards ‘five a day’ (Department of Health 2007).
Intervention mother's better knowledge and higher confidence in terms of them knowing what foods are good for their children is well in line with their written statements about feeling guided and reassured during the intervention. However, improving knowledge might not be enough to achieve behavioural changes.
The positive effects on fruit and vegetables consumption shown at the 18‐month‐stage of the original trial were not reproduced in this longer‐term follow‐up study. This may be because of the lower statistical power of the 4‐year follow‐up to detect the same difference. However, most of the estimated relative risks in this follow‐up were close to 1. Multiple statistical tests were carried out and it is therefore possible that some of the findings are spurious. In particular, less self‐reported health problems in the intervention group and a higher consumption of baked beans in the control group are hard to explain and are likely to be chance findings.
Compared with data from published surveys, the mean dmft and BMI were better than average in the control as well as the intervention group. The percentage of children in this sample who were overweight or obese was 16.3%. In comparison, the 2006 Health Survey for England found that, at the age of four to five, more than 20% of girls and nearly 30% of boys were overweight or obese (Joint Health Surveys Unit 2008). The mean dmft for all examined children in this study was 0.27, and caries had been experienced by 14.1%. The BASCD survey 2005/2006 found that in Islington, the mean dmft for 5‐year‐olds was 1.41, and caries had been experienced by 40.4% (BASCD 2007). The most obvious explanation for these discrepancies is the overall high percentage of well‐educated mothers in the follow‐up. Children from managerial and professional households are less likely to be obese (Joint Health Surveys Unit 2008), while prevalence of dental caries in young children is associated with low maternal education (Harris et al. 2004).
Obviously, children's eating and drinking habits are influenced by an array of interrelated factors. Factors such as mother's education and the family's socio‐economic background are strong predictors of these patterns and might not easily be overcome by an educational intervention.
Strengths and limitations of the study
To date, only few RCT's measured the potential long‐term effects of a peer‐led infant feeding intervention. This research used the unique opportunity of comparing intervention and control group 4 years post‐intervention, thus allowing for conclusions about the sustainability of changes and the detection of other significant longer‐term impacts of the intervention.
It was only possible to locate about 55% of the 183 mothers who consented to be contacted for a follow‐up. The relatively small sample size means that differences between the groups had to be sizable to be detected.
A major difficulty of this study was that the follow‐up sample, as well as, to a lesser extent, the original sample were not representative of the target population for whom the intervention was originally designed. In this follow‐up, the mean age of all mothers at birth of the index child was 32. In comparison, the mean age of those lost to the follow‐up was 29. Moreover, about half of the participating mothers in both intervention and control group had a degree or higher qualification (compared with a third in those who dropped out). This might have reduced the potential impact of the intervention. However, the above characteristics were similar for non‐responders in both groups. The higher percentage of mothers with low educational attainment in the intervention group also might have attenuated the results.
Some items of the questionnaire were probably prone to social desirability bias, especially as the main questionnaire was delivered in a face‐to‐face setting. Social desirability bias means that respondents tend to over‐report ‘good’ behaviour or under‐report ‘bad’ behaviour. The effects of social desirability bias might have been more pronounced among intervention group mothers as they have been educated on the subject.
Comparison with other research
Peer support interventions were shown to be effective especially in relation to breastfeeding (Britton et al. 2007). There is little research on the effects of social support on infant feeding practices during the weaning period, and long‐term follow‐ups are rare. A small‐scale (38 participants in either group) follow‐up of the Community Mothers Programme in Ireland as well demonstrated measurable positive effects after 7 years, including extended benefits to subsequent children (Johnson et al. 2000).
The high proportion of educated mothers in this study is reflected by the lower levels of caries, overweight and obesity and higher levels of fruit and vegetable consumption compared with national figures. It is known that maternal education is related to such measures (Harris et al. 2004; Joint Health Surveys Unit 2008).
Conclusion
Four years post‐intervention, the peer support that was delivered during the children's first year of life appears to have had sustained beneficial effects on children's drinking habits as well as on mother's nutritional knowledge and confidence. There was little evidence that the intervention had an important effect on levels of fruit and vegetable consumption, children's current BMI or caries levels. A major difficulty of this research was the recruitment of potentially vulnerable mothers to the original trial. It is possible that the impact of the intervention would have been greater if the sample had been more representative of the target population for whom the intervention was designed as they may have been more lacking in confidence and knowledge and thus had more to gain from the intervention. Also, considering the complexity of factors influencing infant feeding practices, educational interventions alone might not be able to largely modify engrained patterns and attitudes. The positive feedback of intervention mothers and volunteers shows that this kind of support is, however, much appreciated and indeed helpful for both sides. Bearing in mind the limitations of this research, social support interventions may still be a promising approach to reduce the existing inequalities in child nutrition.
Future research should aim to engage with the most vulnerable mothers, as it is them who are likely to benefit most from additional support and who are most in need of it.
Source of funding
The reported study was funded by UCL. No external funding was received. The original study was funded by the UK Food Standards Agency.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Acknowledgements
We would like to thank all the mothers and children who participated in this research for their time and cooperation.
This research was performed at the Department of Epidemiology and Public Health, UCL, 1‐19 Torrington Place, London WC1E 6BT, UK.
References
- Baird J., Fisher D., Lucas P., Kleijnen J., Roberts H. & Law C. (2005) Being big or growing fast: systematic review of size and growth in infancy and later obesity. British Medical Journal 331, 929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Association for the Study of Community Dentistry (2007) Dental Caries Experience of 5‐year‐old Children in Great Britain 2005/2006. Available at: http://www.bascd.org/viewdocpool.php?id=72 (accessed October 2008).
- Britton C., McCormick F.M., Renfrew M.J., Wade A. & King S.E. (2007) Support for breastfeeding mothers. Cochrane Database of Systematic Reviews 2007, Issue 1, CD001141. DOI: 10.1002/14651858.CD001141.pub3. [DOI] [PubMed] [Google Scholar]
- Chen X. & Wang Y. (2008) Tracking of blood pressure from childhood to adulthood. Circulation 117, 3171–3180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chinn S. & Rona R.J. (2004) Re: international definitions of overweight and obesity for children: a lasting solution? Annals of Human Biology 31, 695–696. [DOI] [PubMed] [Google Scholar]
- Demmelmair H., Von Rosen J. & Koletzko B. (2006) Long‐term consequences of early nutrition. Early Human Development 82, 567–574. [DOI] [PubMed] [Google Scholar]
- Department of Health (2007) Birth to Five: 2007 Edition. Department of Health: London. [Google Scholar]
- Dubois L., Farmer A., Girard M. & Peterson K. (2007) Regular sugar‐sweetened beverage consumption between meals increases risk of overweight among preschool‐aged children. Journal of the American Dietetic Association 107, 924–934. [DOI] [PubMed] [Google Scholar]
- Gregory J.R., Collins D.L., Davies P.S.W., Hughes J.M. & Clarke P.C. (1995) National Diet and Nutrition Survey: Children Aged 1½ to 4½ Years. Vol. 1: Report of the Diet and Nutrition Survey. HMSO: London. [Google Scholar]
- Hallett K.B. & O'Rourke P.K. (2002) Early childhood caries and infant feeding practice. Community Dental Health 19, 237–242. [PubMed] [Google Scholar]
- Harris R., Nicoll A.D., Adair P.M. & Pine C.M. (2004) Risk factors for dental caries in young children: a systematic review of the literature. Community Dental Health 21 (Suppl. 1), 71–85. [PubMed] [Google Scholar]
- He F.J. & MacGregor G.A. (2006) Importance of salt in determining blood pressure in children. Hypertension 48, 861–869. [DOI] [PubMed] [Google Scholar]
- Horta B.L., Bahl R., Martines J. & Victora C. (2007) Evidence on the Long‐term Effects of Breastfeeding: Systematic Reviews and Meta‐analyses. WHO: Geneva. [Google Scholar]
- Ip S., Chung M., Raman G., Chew P., Magula N., DeVine D. et al. (2007) Breastfeeding and maternal and infant health outcomes in developed countries. Evidence Report/Technology Assessment No. 153, Agency for Healthcare Research and Quality. [PMC free article] [PubMed]
- Johnson Z., Howell F. & Molloy B. (1993) Community mothers programme: randomised controlled trial of a non‐professional intervention in parenting. British Medical Journal 306, 1449–1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson Z., Molloy B., Scallan E., Fitzpatrick P., Rooney B., Keegan T. et al. (2000) Community mothers programme – seven year follow up of a randomised controlled trial on non‐professional intervention in parenting. Journal of Epidemiology and Community Health 51, 299–303. [DOI] [PubMed] [Google Scholar]
- Joint Health Surveys Unit (2008) Obesity and other risk factors in children In: Health Survey for England 2006, Vol 2 (eds Craig R. & Mindell J.), pp 19–30. The Information Centre: Leeds. [Google Scholar]
- Morgan J.B., Lucas A. & Fewtrell M.S. (2004) Does weaning influence growth and health up to 18 months? Archives of Disease in Childhood 89, 728–733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence (2008) Improving the Nutrition of Pregnant and Breastfeeding Mothers and Children in Low‐income Households. NICE: London. [Google Scholar]
- Pitts N.B. & Evans D.J. (1997) British Association for the Study of Community Dentistry (BASCD) co‐ordinated National Health Service surveys of caries prevalence 1985/6–1995/6. Community Dental Health 14 (Suppl 1), 1–5. [PubMed] [Google Scholar]
- Reilly J.J., Armstrong J., Dorosty A.R., Emmett P.M., Ness A., Rogers I. et al. (2005) Early life risk factors for obesity in childhood: cohort study. British Medical Journal 330, 1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scientific Advisory Committee on Nutrition (2008) Infant Feeding Survey 2005: A Commentary on Infant Feeding Practices in the UK. The Stationery Office: London. [Google Scholar]
- Seow W.K., Clifford H., Battistutta D., Morawska A. & Holcombe T. (2009) Case‐control study of early childhood caries in Australia. Caries Research 43, 25–35. [DOI] [PubMed] [Google Scholar]
- Sloan S., Gildea A., Stewart M., Sneddon H. & Iwaniec D. (2007) Early weaning is related to weight and rate of weight gain in infancy. Child: Care, Health and Development 34, 59–64. [DOI] [PubMed] [Google Scholar]
- Tarini B.A., Carroll A.E., Sox C.M. & Christakis D.A. (2006) Systematic review of the relationship between early introduction of solid foods to infants and the development of allergic disease. Archives of Pediatrics & Adolescent Medicine 160, 502–507. [DOI] [PubMed] [Google Scholar]
- Tedstone A., Dunce N., Aviles M., Shetty P. & Daniels L. (1998) Effectiveness of Interventions to Promote Healthy Feeding in Infants under One Year of Age: A Review. Health Education Authority: London. [Google Scholar]
- Watt R.G., McGlone P., Russell J.J., Tull K. & Dowler E. (2006) The process of establishing, implementing and maintaining a social support infant feeding programme. Public Health Nutrition 9, 714–721. [DOI] [PubMed] [Google Scholar]
- Watt R.G., Dowler E., Hardy R., Kelly Y., McGlone P., Molloy B. et al. (2009) Effectiveness of a social support intervention on infant feeding practices. Journal of Epidemiology and Community Health 63, 156–162. [DOI] [PubMed] [Google Scholar]
- Wendt L.K., Hallonsten A.L., Koch G. & Birkhed D. (1996) Analysis of caries‐related factors in infants and toddlers living in Sweden. Acta Odontologica Scandinavica 54, 31–137. [DOI] [PubMed] [Google Scholar]
- World Health Organization (2002) The World Health Report 2002. Reducing Risks, Promoting Healthy Life. WHO: Geneva. [Google Scholar]


