Abstract
| Table of Contents | |
|---|---|
| Summary | 237 |
| Introduction | 238 |
| Objectives | 238 |
| Approach and methodology for the study | 238 |
| Background to barriers to use of health services | 239 |
| Models of health service utilization | 239 |
| Mosley and Chen Child Survival framework | 239 |
| Explanatory models | 239 |
| Hierarchy of resort | 240 |
| Dimensions of access | 240 |
| Framework for categorization of barriers | 241 |
| Summary | 242 |
| Barriers to use of health services | 242 |
| Geographic access | 243 |
| Temporal access | 244 |
| Socio‐cultural access | 245 |
| Financial access | 248 |
| Quality of care | 249 |
| Discussion | 250 |
| References | 252 |
Summary
In the light of mainstreaming nutrition programs into health services, this review article approaches the issue of barriers to existing maternal child health programs from both theoretical and applied perspectives. It begins with a discussion of salient literature on models of health service utilization. The mid‐section of the paper presents the results of a review of research studies that illuminate the barriers to care. Categorical themes emerged from the review of studies in the form of barriers based on geographic factors, temporal factors, a myriad of socio‐cultural factors, financial factors and quality of care. The discussion focuses on the need to overcome existing restrictions to health services in order to facilitate initiatives to mainstream nutrition and achieve Millennium Development Goal #1.
Keywords: nutrition, barriers, health services, maternal, child, integration
Introduction
Millennium Development Goal #1 (MDG 1) seeks to reduce present levels of hunger by one‐half. Efforts are underway to incorporate the Mainstreaming Nutrition Initiative (MNI) into existing maternal, newborn, child health (MCH) programmes in order to increase the likelihood of achieving MDG 1. Reducing hunger through increased food availability is not the only component to reducing malnutrition. Nearly one‐third of the children in the developing world are malnourished in terms of acute or chronic malnutrition and micronutrient deficiency. While it can be difficult to measure, it is estimated that nearly 60% of child mortality involves malnutrition as a major underlying cause (Pelletier et al. 1995). In South Asia, the problem is even more extreme, with half of all pre‐school children suffering from stunting (UNICEF 1998). Because of high population numbers, some 70% of the world's malnourished children live in this region (UNICEF 1998).
There is persuasive evidence that programmes to improve maternal nutrition, breastfeeding and complimentary feeding, and the provision of micronutrients at appropriate times, are feasible and have the ability to reap health and economic benefits. It is also apparent that such programmes are most effective when they are comprehensive and are integrated into other MCH programmes and services. Stand‐alone feeding programmes have generally not proved to have a sustainable, long‐term impact (World Bank 2006). In some cases this is because the interventions were not effective, in other cases because the organizational and financial burden imposed on governments was beyond their capacity to sustain.
To this point, nutrition has been poorly integrated with MCH activities, but there is an emerging international consensus that the convergence of nutrition and MCH is essential. This review will focus on research involving pregnant women, infant and children. While it is generally agreed that integrating nutrition with existing MCH services is desirable, there are some additional criteria, such as ensuring that the poor have equitable access to these services that must be addressed.
Objectives
This paper is part of a larger programme of research on the issue of mainstreaming nutrition into MCH. The total initiative will generate three major outputs that together will provide both the evidence base and operational guidance for mainstreaming nutrition into MCH programmes. Within these major outputs, this paper is one component of a larger review of issues related to mainstreaming nutrition into MCH programmes. This paper sets out specifically to review barriers to services from existing MCH programmes. The paper is developed around the observation that many existing MCH services are less than fully utilized by individuals and families in developing countries, and an understanding of reasons why people refrain from seeking existing MCH services should facilitate mainstreaming nutrition into MCH services if such barriers can be overcome or avoided.
Approach and methodology for the study
The approach to be used for this study is a literature review summarizing the experience of utilization of a wide range of preventive and curative maternal, neonatal and child health services. These experiences will be predominantly from low‐income countries but will also include middle‐ and high‐income countries as needed. The services reviewed include the public and non‐state sectors to include both private providers and non‐government organizations. The full spectrum of service provider will be considered in order to illuminate barriers to appropriate care across health‐care systems and cultural norms.
This study was conducted as a literature review to present relevant examples in the vast body of literature of the barriers to accessing health services in a global context. Articles were searched for in PubMed with the primary keywords: access, barriers and health. Further, the keywords: maternal, prenatal, child, newborn and infant were run separately with each of the primary keywords. Articles were excluded if they did not discuss access or barriers to care among the MCH population. References already held by three of the reviewers (T.K., P.K.S., M.K.M.) were included in the review if they were judged appropriate. Individual studies were not evaluated for quality.
After a discussion of existing models of health service utilization and barriers to care, the paper discusses barriers to appropriate care in the following organizational structure. Within each category studies were categorized by the intended recipient of services; whether maternal, infant or child centred.
Background to barriers to use of health services
It is not difficult to relate a ‘shopping list’ of experiences of dissatisfied users, or potential users of health services across the spectrum of nations and health services. Again and again the myriad of barriers to health‐care access have been documented in population‐based surveys, focused research studies, and anecdotal reports (Pollock 2001). What is more challenging is to attempt to put these experiences into some kind of conceptual framework. This is particularly important where cultural perceptions of disease (and their causes and appropriate responses) affect the behaviour of patients and their care seekers. In the following section a brief review will be made of several useful conceptual frameworks that relate to utilization of health services or health providers.
Models of health service utilization
Mosley and Chen Child Survival framework
In 1984 Mosley and Chen published a useful framework for examining the factors that affect child survival. That framework divided five groups of factors through which socio‐economic factors influence both morbidity outcomes, including nutritional status, and mortality outcomes. The pathways operate through demographic; environmental, nutritional, injury (intentional and unintentional); and personal illness control. This framework pays little attention to the cultural aspects of interpretation of illness, and consequent choice of healer or health service provider. Indeed, the Child Survival framework does not focus on the health system to any great extent, but rather on individual behaviour and the factors underlying that.
Explanatory models
In the classic medical anthropology text, Patients and Healers in the Context of Culture (Kleinman 1980), Kleinman suggests that there are three overlapping sectors of health care: the popular sector, the folk sector and the professional sector.
As Helman explains, the popular sector tends to focus on curative care, and includes all informal options for which payment is not made, and excludes folk healers and medical practitioners (Helman 1990). This sector also includes the concept of health maintenance, the purpose of which is to avoid ill health. Correct ways to eat and drink are included here. This sector is believed to be the source of the majority of health care in both developed and developing countries, although mainly for minor illnesses.
In the folk sector, certain people specialize in forms of healing. Some are ‘secular’ or technical, repairing broken bones, for example. Others are ‘sacred’ and deal with illnesses caused by sorcery, evil eye and other mystical sources within the belief structure of the society.
Both popular and folk remedies tend to evolve from the belief that ‘health’ is a ‘balance between man and his social, natural and supernatural environments. A disturbance of any of these . . . may result in physical symptoms . . . and require the services of a sacred folk healer’ (Helman 1990).
Folk healing has several advantages over modern allopathic medicine. In addition to a shared worldview, the use of everyday language in consultations, the involvement of the family in diagnosis and treatment is highly valued. These folk healers reinforce the cultural values of the community in which they live, in contrast to Western doctors who may represent a very different social and economic background (Helman 1990, p. 61).
The professional sector generally revolves around organized modern Western scientific medicine, although in some countries, such as India and Sri Lanka, traditional medical systems have also become ‘professionalized’ to an extent (Helman 1990). Although this sector includes paramedical staff, resources are usually scarce in developing countries. But in relation to the current study, the important point is that this sector holds great power, including legal authority, over patients, and subscribes to a medical system that may often be inconsistent with the belief systems of patients.
The professional system tends to reflect the political system in which it operates. Some societies regard free (or inexpensive) health care as a basic right of all citizens; another society may see health care as a commercial product to be ‘sold’ to the patient (‘customer’). Such differences in ideology affect the likelihood of the poor, in particular, being able to access ‘professional’ sector health services.
Hierarchy of resort
According to Pelto it is important to first establish the various health service options available. When a person perceives himself/herself as ill, he/she will follow a ‘hierarchy of resort’ in seeking treatment. This hierarchy will often start with self‐treatment in the popular sector, and if not successful, will progress to professional care, sometimes through several other intermediate steps. This stepwise approach can potentially result in delays, in inappropriate treatment and in additional expense. However, on occasions the problem may be ‘cured’ before reaching the highest or final level of resort.
Pelto summarizes the steps that caregivers take in responding to episodes of illness (Pelto 2006). She argues that the family usually follows this sequence:
-
1
recognition of specific signs and symptoms,
-
2
interpretation of these signs as an indication of an illness that requires expertise that is external to the household (sometimes called ‘labelling’ of the disease),
-
3
taking an initial action to obtain care, and
-
4
maintaining a relationship with the provider and adhering to provider advice until the individual is well.
Finally, the modern allopathic health system is not regarded by all cultures as appropriate for all conditions. It has long been recognized that there are different classes of illness for which different healer systems are needed. Kendall's (1983) work in Honduras summarized this as (1) illnesses such as simple diarrhoea and acute respiratory infections (ARI) for which the formal health system is appropriate; (2) illnesses believed to be caused by evil eye for which folk practitioners are appropriate; and (3) illnesses that are believed to be incurable, like polio, cancer and tuberculosis (Pelto 2006).
A difference between traditional health systems and modern allopathic systems is the continuing relationship between patient, or their caregivers, and the provider. Pelto argues that the Western allopathic model often requires a series of repeat visits to the same provider to treat a particular illness episode, whereas the non‐Western model tends to involve a single visit to an individual provider, possibly with visits to other providers at the same time (‘simultaneous resort to care’), or to a series of providers possibly offering different forms of care (‘sequential resort’). This practice has obvious implications for compliance (or ‘adherence’), which limits the capacity of Western medicine to achieve the desired results.
Dimensions of access
Penchansky & Thomas (1981) define access as the measure of fit. The fit represents the degree of matching characteristics between the provider and the type of health services to the characteristics of the patients including patient expectations. Penchansky and Thomas outline five distinct areas or dimensions of access:
-
•
availability;
-
•
accessibility;
-
•
accommodation;
-
•
affordability; and
-
•
acceptability
Barton (2003) built upon the work of Penchansky and Thomas by categorizing barriers to access into five major groupings to include geographic barriers, physical barriers, temporal barriers, socio‐cultural barriers and financial barriers. Barton further elaborates on three important factors that affect access to health services: predisposing factors, need factors and enabling factors, which do not operate independently but in combination to influence the ability or likelihood of an individual seeking health services.
Predisposing factors include individual characteristics such as gender, ethnicity, education, age and occupation. Need factors include the perception of health status, the health beliefs and perceptions of illness. Last, enabling factors include items such as distance to care and availability of care, financial assets (insurance or cash reserve) in paying for care.
In addition to the aforementioned access conditions, it is necessary to consider the overarching framework of health systems values: cost–quality–access. It would be virtually impossible to discuss access without also focusing on cost and quality. Cost is particularly complex in that the cost of health care includes myriad of components including cross‐sector issues such as private vs. public providers (including under‐the‐table fees); family income; availability, use and structure of health insurance. Quality becomes an access issue when poor‐quality services discourage or otherwise prevent the use of proper health utilization. Quality is assessed from various perspectives including the provider, patient and the evidence base.
Framework for categorization of barriers
The barriers to use of MCH services can be categorized in various ways as discussed above. One technique for gaining appreciation of the opportunity for barriers to exist is to examine increasing degrees of aggregation from individual, household, community (village), national, to international. Within each of those administrative and cultural layers there are cross‐cutting categories such as cultural belief systems, economic and financial factors, and importantly, health systems at various levels.
-
•
Individual characteristics:
-
∘
social and demographic characteristics;
-
∘
economic status;
-
∘
cultural beliefs (operate at higher levels also);
-
∘
mobility of care seekers (may be different for different purposes, e.g. may be permitted for child care but not for socializing);
-
∘
knowledge of illnesses (symptoms, outcomes, appropriate preventive measures and curative responses);
-
∘
decision‐making authority of care seeker (operates at household and community levels also);
-
∘
knowledge of health system (location of health service providers, and how to navigate the health system); and
-
∘
family structure (availability of caretakers for other children/family members).
-
∘
-
•
Community level characteristics:
-
∘
cultural belief systems of community;
-
∘
customs such as post childbirth seclusion that limit access to services;
-
∘
availability and influence of non‐allopathic health providers in the community;
-
∘
Influence of role models in community to generate change in traditional approaches to disease control;
-
∘
commitment of community to minimizing conditions, which contribute to illness and disease, namely ensuring a hygienic environment (water supply, sanitation, etc.); and
-
∘
role of community in providing needed but unfunded services for community members.
-
∘
-
•
National health programme characteristics:
-
∘
organization of the national public health system;
-
∘
role and impact of health insurance within the nation;
-
∘
importance given to particular services (e.g. malaria, HIV, others) in terms of staff skills, budgets, allocation of medicines or vaccines;
-
∘
management information systems in place to ensure functioning services;
-
∘
aspects of health system structure that affect implementation;
-
∘
political considerations regarding relative weight given to health in relation to other ministries (political and budgetary considerations);
-
∘
licensing and regulation to minimize unauthorized unqualified service providers;
-
∘
regulation of costs of health services, and legislation to provide low cost services and/or insurance; and
-
∘
drug regulation policies to minimize access to harmful or ineffective drugs.
-
∘
-
•
International and non‐government organization health programme characteristics:
-
∘
importance given by international agencies and organizations to specific health challenges;
-
∘
availability of funds to support specific services and interventions;
-
∘
involvement of multilateral agencies or projects in provision of funds or commodities, etc.;
-
∘
involvement of non‐multilateral agencies in provision of funds or commodities, etc. (in‐kind contributions), including foundations;
-
∘
availability of data to support the need for responding to particular problems; and
-
∘
political will of international agencies to confront governments that conceal health challenges (e.g. severe acute respiratory syndrome, avian influenza).
-
∘
The hierarchy and complexity of individual, community, national health system and international issues as well as the myriad of barriers that can be put in place preventing the individual access to care can be seen in the following illustration developed by Varkevisser et al. (2003) (Fig. 1). The health systems research Model places the individual at the centre of the concentric circles, surrounded by the family, the community, the layers of public health services, all within the greater context of nation and culture. Public services including health, sanitation and agriculture appear on the right side of the model with non‐state sector services appearing on the left side of the diagram.
Figure 1.
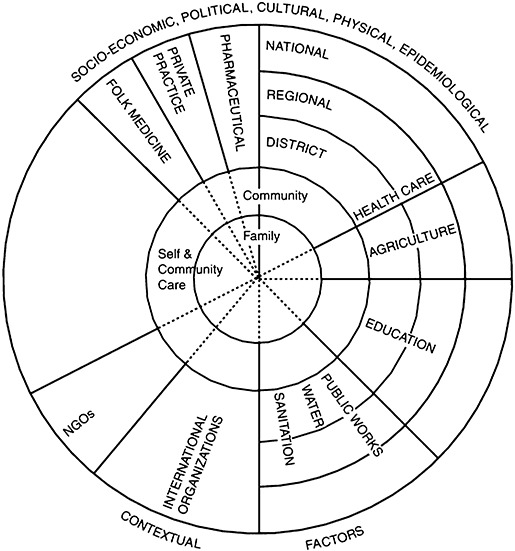
Model of a health system. From: Health Systems Research Projects, Part 1, by Varkevisser et al. (2003). NGO, non‐government organization.
Summary
Over the past 30 years a broad range of theories have been used in discussions of access to care and barriers to service utilization across the spectrum of health services. The next section of this review will apply each category of barrier to maternal, infant and child barriers.
Barriers to use of health services
This section presents global research findings that fall within each of the major barrier categories discussed in the previous section. This section is organized into geographic access, temporal access, socio‐cultural access, financial access and quality in relation to its impact on access. Each barrier is further delineated by studies that apply to maternal, infant and child health as appropriate.
Geographic access
Geographic access relies on the physical relationship between the location of the care seeker and the location of the health services and the ability to overcome that distance to seek care. There is not a single country that has achieved social equity in health care because of regional inequalities; but some countries have faired much better than others (Lassey et al. 1997). Distance, transportation and outreach are all central tenants in the consideration of geographic barriers to access. Consistent throughout the theories of health service barriers is the idea that closer access to care will increase utilization, even if closer access means lower levels of staff skills, and possible shortages of medications and other supplies. The World Health Organization's (1978) Alma‐Ata Declaration set the historic goal of Health for All by the year 2000. The declaration focused on primary health‐care services, which were ideally to be brought ‘as close as possible to where people live and work’ (World Health Organization 1978). The problem of geographic access is common across the spectrum of low‐, middle‐ and high‐income countries. As described below the problem of geographic access is occasionally addressed through outreach services.
Maternal
In Zaire the geographic accessibility of the hospital and the mother's perception of the risk status were the two most important factors determining the compliance of referral of high‐risk mothers (Dujardin et al. 1995). A 1992 study in Bangladesh found that difficult terrain and residing more than two miles from a government health facility lead to a large number of people who did not receive health services when ill (Islam 1992). A study in Cordova found that transportation difficulties were a problem regardless of women's success in obtaining care and were ranked as the top barrier by women who never tried to obtain care (Aved 1993). One example of geographic barriers to prenatal care from a high‐income country was produced by Kalmuss & Fennelly (1990) and set in the USA where lack of transportation was an important barrier. Buekens (1990) revealed that distance was an important barrier across Europe. A qualitative study in rural communities in Nigeria, Ghana and Sierra Leone identified barriers to the use of health‐care facilities when obstetric problems arise. The findings illustrated that physical and social distance between communities and facilities, as well as transportation problems, were relevant obstacles to care (Prevention of Maternal Mortality Network 1992).
Distance did not prove to be as important as other barriers in the two following studies from Central America. A study in Mexico found that the development of different types of health services in the community was not a significant predictor of utilization of prenatal services, but existence of a good road was associated with a 30% increase in probability of using medical services. However, the analysis also suggested that the policy of providing medical facilities at the community level has had little effect on the extremely disparate use of prenatal care and hospital delivery in rural Mexico (Potter 1988). A similar study that looked at obstetric needs in Guatemala revealed that improving proximity to biomedical services was unlikely to have a dramatic impact on utilization in the absence of additional changes that improve the quality of care or reduce other barriers to access (Glei et al. 2003).
Urban–rural differences are a further example of geographic barriers to care. In Haiti, the rural–urban difference in prenatal care seeking was estimated. The expected probability of using prenatal care services in rural Haiti was 77.2%, compared with 85.8% in urban Haiti. Among users of prenatal care services, mothers in rural areas made an expected number of 3.78 prenatal care visits, compared with 5.06 visits for the women in urban areas (Alexandre et al. 2005).
Infant
In The Gambia in the mid‐1980s, the Health for All initiative led to the development of Primary Health (PH) Centers in rural villages. After the establishment of the PH Centers in 1983, infant mortality in villages with PH Centers dropped from 134/1000 to 69/1000 by the period of 1992–93 whereas secular trends in non‐PH Center villages saw a drop in infant mortality from 155/1000 in 1983 to 91/1000 (Hill et al. 2000).Orubuloye & Caldwell (1975) showed that increased proximity and availability of health services has led to prompt treatment of illness and a subsequent lowering of infant and child mortality in two Nigerian villages. Similar findings based on short geographic distance to treatment were reported in Narangwal, India (Kielmann 1983).
Child
Two examples of using outreach to tackle geographic barriers to health services from Bangladesh include a reduction in the risk of a child dying from diarrhoeal diseases by 30% in a community where Oral Rehydration Solution (ORS) packets were distributed via home delivery by Primary Health Care (PHC) workers compared with a community with no ORS distribution by PHC workers (Rahaman et al. 1982). Also in Bangladesh, simple training of PHC workers to provide treatment for ARI at home or refer ARI patients to clinics reduced overall infant and child mortality by 20% (Fauveau et al. 1991). Another study in the USA explored barriers to childhood immunization and found that transportation problems were a commonly reported barrier (Yawn et al. 2000).
Temporal access
Temporal barriers to access are those barriers that relate to the time issues around an illness that would produce a care‐seeking episode. There are numerous dimensions that fall into the category of temporal barriers. First, waiting times are an issue, including the time waiting for treatment within the health facility and the time between care being initially sought or scheduled and the actual time/date of the appointment. Another issue is the hours of operation of a health facility or hours of availability of the health service provider, which may not be convenient to working hours of the care seeker or may not be available in an emergency situation. Another temporal barrier is that of requiring care for other family members who are not involved in the care‐seeking episode such as watching/caring for other children or providing meals and housekeeping services to a family during an absence. Often temporal barriers will bundle with other barriers such as the aforementioned geographic distance and transportation.
Maternal
In Europe, a health system study revealed that distance, long waiting time and lack of child care were significant barriers to the use of antenatal services (Buekens 1990). In Ghana a maternity waiting home initiative provided an important lesson. To minimize delay of transport in the event of a complication, a maternity waiting home was established in Nsawam, Ghana in 1994 and women were encouraged to move there so that they could be transferred to the hospital when labour began. Of 25 women referred to the maternity waiting home by health personnel over 12 months, only one complied, for one night. Focus group discussions with community members and hospital staff later revealed that cost and hardship of staying away from home, absence of health personnel, distance from hospital, desolate surroundings and lack of perceived need were reasons for poor utilization (Wilson et al. 1997). A study in the USA identified two major barriers to seeking prenatal care, one of which was long waiting times at the time of appointments (Beckmann et al. 2000).
Infant
Another study (Woelfel et al. 2004) identified barriers that deter parents/caretakers of infants and children enrolled in the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) from taking full advantage of the services provided by the programme. The study found that waiting too long was the most frequently cited barrier (48%). Difficulties in bringing the infant/child to re‐certify and rescheduling appointments were other key variables associated with failure to use, either pick up or cash, WIC checks. A study in New Zealand revealed that removing the 6‐week post‐partum check from a general practitioner and separating it from the immunization appointment had a deleterious effect on immunization uptake of children (Turner et al. 1999).
Child
In the USA, Yawn et al. explored the barriers to immunization services for children and found that the most commonly reported barriers were those of inconvenience. Caretakers complained of having to wait too long to be treated and of inconvenient office hours. Also, the study showed the impact of delays caused by a sick child and fear of child's reaction to the vaccination (Yawn et al. 2000). Tarrant & Gregory (2003) found similar temporal barriers in terms of time constraints in a Canada‐based study.
Socio‐cultural access
Access to care can be hindered by a variety of socio‐cultural factors. Many of these factors fall into the category of enabling factors to health care such as gender and perception of illness. Further barriers include significant variation and lack of understanding between provider and patient. Ethnicity and language are other socio‐cultural barriers.
Recognition of illness (defining severity and appropriate level of care)
Initiation of treatment and choice of treatment provider depend on recognition of illness and perceived severity of the illness following its onset. What is deemed as ‘sick’ or ‘ill’ is not the same across various subcultures. While a perception of severity of illness triggers a call for health actions in diverse settings, the term ‘severity’ does not mean the same thing to all groups of people (Mechanic 1992). Episodes of illness that are considered as severe by informed caretakers or household members may not always be recognized as severe by less well‐informed individuals. The issue of health literacy resides within this category although in general, poor women with a low level of education demonstrate greater difficulty both in perceiving illness and in judging its severity compared with their more financially established and better‐educated counterparts.
Maternal A qualitative study conducted among First Canadians explained that conceptualization of pregnancy in a spiritual context and believing it to be a healthy, natural process requiring no intervention prohibit women from taking prenatal services (Sokoloski 1995). A study in the USA found that late initiation of care was associated with patient perception of prenatal care as being less than very important [odds ratio (OR) = 4.1, 95% confidence interval (CI), 1.7–9.7] and annual income <$17 000 (OR = 2.9, 95% CI, 1.5–5.7) among other barriers. In the same study, multiparous women and women older than 35 years were more likely to perceive prenatal care as less than very important and resulted in seeking prenatal care at a later stage of pregnancy (OR = 3.9, 95% CI, 2.5–14.6 and OR = 2.9, 95% CI, 1.2–6.8 respectively) (Roberts et al. 1998). Another study identified that after controlling for social and demographic characteristics, six barriers were significant predictors of inadequate prenatal care with the most important one being that the odds of receiving inadequate care were 7.9 among women who had a poor understanding of, or attached a low value to, prenatal care compared with those who did not cite this barrier (Harvey & Faber 1993). In Nigeria, the major barriers to use of antenatal care and obstetric care services that were identified included economic and cultural factors and those related to the women's perception of their condition (Adamu & Salihu 2002). Another study in four states of India found that pregnant women from poor and uneducated backgrounds with at least one child were the least likely to receive antenatal check‐ups and services (Pallikadavath et al. 2004).
Again in Nigeria, a different study found that increased awareness of the signs of obstetric complications and the need for prompt treatment among community women and men did not result in greater utilization of emergency obstetric services at the facilities. (Gummi et al. 1997).
Infant In Bangladesh infants are taken to homeopaths at a higher rate because unlicensed village practitioners, who hold the idea that allopathic medicine is too strong for young infants, refer them to homeopathic practitioners (Stewart et al. 1994).
Child In South Asia, upon recognition of illness, a child is typically provided with home‐care. Many studies have shown that most early treatment for childhood illness occurs at home, using shop‐bought brand name drugs (Ashraf 1982; Mwabu 1986; Sauerborn et al. 1989; Nessa 1991; Bhuiya & Streatfield 1995; Ryan 1998). Use of home‐remedies is common for treatment of less severe episodes, but can be incorrect and suboptimal. Caretakers are often uninformed as to the recognition of danger signs of common illnesses (such as fever, ARI and diarrhoea) and about in what circumstances they should leave home‐remedies and seek professional care. Knowledge of germs is present in some societies but at a superficial level and often in relation to a limited number of diseases, such as dysentery, malaria and tuberculosis, and mostly among those who are educated (Ashraf 1982). Stewart et al. (1994) reported that parents who believed ARI was caused by evil spirits went to faith healers rather than to modern doctors. Similarly in Uganda, a study showed that although the perceptions of childhood diseases were high, the care‐seeking practices were poor. Most children with fever, diarrhoea and upper respiratory tract infection were treated at home and taken to health units only when they developed life‐threatening symptoms. The high costs of care, long distances to health units, poor attitude of health workers, lack of drugs at health units and limited involvement of fathers in care of the children complicated the situation and resulted in late referrals to health units (Mbonye 1998).
Gender
Women, as mothers and caregivers, may bear particular responsibility for the nursing of sick children, but they often have a subordinate position in the household and society. Their subordinate position affects use of health care during illness. In many settings, women lack decision‐making power and lack control over household resources. Female fetuses may be aborted at higher rates to meet socio‐cultural demands. Female children may receive care at a lower rate than male children under similar circumstances.
Gender bias can be seen as a common thread throughout the continuum of care, not just limited to MCH. A number of studies have illustrated the variable weights given to particular household members in terms of priority for obtaining health care. A study of the redirection of micro‐credit loans for use in medical emergencies showed that adult male income earners were most likely to be supported by such finance in times of illness. The next priority was male children, followed by female children and adult females at lowest priority. This pattern appears to be gender bias, but also incorporates economic (family or household income) considerations, and is thus potentially amenable to change through empowerment of women as generators of household income (Hashemi 1995).
Maternal A sociological enquiry based in Argentina revealed conflicting social pressures that led the women onto the path of maternal death. The men were found not to be involved in the health issues arising from pregnancy and delivery, and the reproductive process was seen to lie exclusively in the women's domain (Szmoisz et al. 1990).
Infant Lack of male involvement has also been identified as an important barrier to access to care for infants. A study among low‐income women in the USA found that women who did not have much help from the infant's father were 1.9 times more likely not to have adequate care (95% CI, 1.0–3.6) (Gazmararian et al. 1999).
Child Studies have shown a consistent pattern over three decades whereby in Bangladesh female children are less likely to be taken for curative care than male children. However, the situation now appears more subtle. For preventive services that are generally free of (financial) cost, such as immunization, girls and boys are almost equally likely to receive them. Even for curative services that involve little or no cost, gender equity is relatively good. It is only where financial costs are involved that gender differentials emerge, to the detriment of girls' health (Chen et al. 1981). Child health programmes usually target mothers in order to improve child health while the fathers are the key persons in the family health decision‐making process. Choice of health‐care provider reflects fathers' choice rather than mothers' choice because fathers have to pay the treatment costs out of their income.
Ethnicity
Ethnicity is another aspect of socio‐cultural barriers. Ethnicity, low‐caste membership and otherwise belonging to a minority population group are frequently found to be significant barriers to access to health services. Some diseases such as Tay–Sachs and sickle‐cell anaemia only affect members of certain racial and ethnic groups resulting in health needs that differ from the general population (Barton 2003). Further, ethnic population group members may face discrimination or other cultural barriers that hinder their access to health services. In Organization for Economic Cooperation and Development (OECD) member nations, much effort has gone into addressing and correcting for racial and ethnic disparities. In the USA alone an enormous body of research has been developed in the areas of barriers to care based on ethnicity and race. 1 Samples of the USA and other OECD studies will be included in the discussion below, but an emphasis will be placed on including studies about ethnicity from low‐ and middle‐income countries.
Maternal A study from the USA revealed that after controlling for important socio‐economic status and cultural characteristics, ethnicity had a strong independent effect on the number of prenatal visits and adequacy of prenatal care. Mexican‐American infants made fewer visits (8.2 vs. 9.8) and completed fewer age‐appropriate immunizations than non‐Hispanic whites (Moore & Hepworth 1994). Also, African‐American women were less likely to receive prenatal care than white women yet they were less likely to report barriers to such care (Tossounian et al. 1997). Tossounian and colleagues concluded that the cause behind this may be differing expectations from the health system. In Hawaii social variation in care‐seeking behaviour continues to exist among ethnic groups, even in the presence of universal access to care (Kogan et al. 1998).
Infant African‐American women were twice as likely as women from other ethnic groups to have babies with low birthweight, and to experience the loss of infant death (Gates‐Williams 1992).
Language and communications problems
Difficulties in communication between the care provider and the recipient introduce the possibility of increased risk or harm to the recipient of health services. Cultural barriers in the form of poor communication can increase the use of inappropriate care regardless of the patient population. Communication problems can also exist between patients and providers who speak the same native language but come from vastly different socio‐economic backgrounds. This same language gap can result in the inability to communicate effectively because of low health literacy or use of medical jargon.
Maternal A study among Turkish immigrants who received prenatal and childbirth services within the Danish health‐care system concluded that the language barrier between provider and pregnant patient resulted in the increased risk of delayed or missing obstetric interventions (Jeppesen 1993).
Child In a paediatric teaching hospital in Cape Town, South Africa, the majority of the health providers speak primarily Afrikaans or English while many of the patients and their families use Xhosa as their primary language. Parents interviewed repeatedly cited language as the greatest barrier, with 94% of respondents citing that the staff did not speak any Xhosa and that only 21% of medical interviews included any form of interpreter. The result was that 69% of the parents were dissatisfied with the care their child received and 45% expressed sincere concern about the impact that poor communication might have on their children (Levin 2006). Poor communication between caretakers and health‐care providers in New Zealand resulted in Samoan children with pneumonia presenting at the hospital with a later stage of disease and without the proper referral documentation, even when the child had seen a referring physician. The break in the continuity of care was attributed to mistrust and poor communication between parties rather than beliefs in traditional healers (Young 2001).
A USA‐based child health study found that limited English proficiency of parents was associated with triple the odds of a child having fair/poor health status and double the odds of the child having spent at least 1 day in bed for illness during the course of the previous year and significantly increased the odds of children not being brought in for needed medical care (Flores et al. 2005). A different US study surmised that the notable disadvantage among Hispanic children in access to care was the result of poor language ability (Bennett et al. 2006)
Financial access
Globally, nations engage in a diverse array of financial schemes for funding basic health‐care services. The most widely used form of financing health‐care services is compulsory public insurance (Yakoboski et al. 1994) and it has featured broadly in the rapidly industrializing regions of Central Europe and South‐East Asia and has been considered to varying degrees by some nations in Africa and in the Caribbean (Mills & Ranson 2006). Although most countries offer universal coverage, only 70–80% of health‐care expenditures are paid through public sources (Lassey et al. 1997).
Financial barriers play an important role in limiting access to care even in areas with no cost at point of service set‐ups. Is removing financial barriers to access to care enough to ensure universal care seeking? A study (Mor et al. 1995) in Hawaii suggested that removing financial barriers to access to care does not guarantee universal use of disease prevention and health promotion services. Out‐of‐pocket payments, either official or unofficial, can be very high and create a barrier to use of services.
Maternal
Financial barriers were one of the significant factors identified as barriers to the use of prenatal care in one study in Kinshasa (Khan et al. 2005). Delvaux et al. (2001) found that in 10 European countries, lack of health insurance was an important risk factor for inadequate prenatal care (OR = 30.1, 95% CI, 20.1–47.1). However, this group of uninsured women was not representative of the population in that they were more likely to be foreign nationals among other factors. Financial barriers were identified as one of the barriers to prenatal care in studies from as diverse places as Kenya, India and the USA (Kalmuss & Fennelly 1990; Beckmann et al. 2000; Pallikadavath et al. 2004; Khan et al. 2005). In particular, Pallikadavath et al. characterized the financial barrier as poverty whereas Beckman et al. and Kalmuss and Fennelly characterized the financial barrier as the ‘cost of getting care’.
Another study (Piper et al. 1994) compared outcome rates for pregnant women who enrolled in Tennessee Medicaid health insurance in the 6‐month period before presumptive eligibility was enacted with those obtained for pregnant women who enrolled in the 6‐month period after presumptive eligibility had been in effect for 5 months. The study found that women in the ‘after’ group were 40% more likely to enrol and 30% more likely to obtain prenatal care in the first trimester. They were 300% more likely to fill a prescription for prenatal vitamins in the first trimester and 16% more likely to have begun prenatal care before the third trimester. Similarly, Brown (1989) found that inadequate insurance coverage and limitations of the Medicaid programme were significant barriers for low‐income women in obtaining prenatal care.
Infant
Financial barriers that contribute to lack of utilization of one type of service can lead to barriers to use of related services. Two USA‐based studies found an association that prenatal care use, based on health insurance status, may influence the likelihood that very low‐birthweight infants will have access to neonatal intensive care (Pierson et al. 1994; Bronstein et al. 1995).
Child
Children with chronic conditions from poor families in the USA experienced substantial financial barriers to care. A study (Newacheck 1994) revealed that they were 118% more likely to be uninsured than were children from non‐poor families and 42% more likely to lack a usual source of care. Children with chronic conditions from poor families were found to use fewer ambulatory care services but more inpatient hospital care than their non‐poor counterparts.
In Bangladesh financial barriers do not involve health insurance. Women's employment and participation in economic activities are considered as tools for empowering women in the household and community by non‐government organizations and the government agencies. Their work and associated earnings are assumed to empower them, which may affect the welfare of their children. To date there is limited empirical evidence to show that children benefit more than other household members from mothers' additional household earnings (‘maternal altruism’). Women's status, particularly women's membership in credit unions and social networks in the household and community, are positively associated with use of health services for children (Levin et al. 1998; Alam 2000).
Quality of care
Operationalizing quality is a relatively new science. In 1990 the Institute of Medicine (USA) described quality as that which consists of the degree to which ‘health services for individuals and populations increase[s] the likelihood of desired health outcomes and are consistent with current knowledge’ (Lohr 1990). There is no health‐care system that is perceived as perfect by its users or by the providers who work within it (Blendon et al. 1993). Quality becomes an access issue and a barrier to care when actual or perceived poor‐quality services result in patients not receiving adequate care and/or patients refusing to utilize services when they are available.
Expanding upon the classic Donobedian model of Structure, Process and Outcome, the main components of quality of services can be viewed as efficacy of the treatment the facility offers, the availability of supplies and equipment, the characteristics of its personnel, and the nature of its management and organizational structure. Each of these components affects the utilization of health services. The public‐sector facilities in many poor countries (Mwabu 1986) are beset with numerous deficiencies: shortage of drugs, non‐availability of health staff, long waiting times for short consultations with a doctor, indifferent attitudes of health staff, poor physical environment and amenities that obviously affect the quality of services offered (Mwabu 1986; Guyon 1994; Arifeen et al. 2005).
Studies in diverse settings show that people's perceptions of the quality of care have a tremendous effect on health services use (Habib & Vaughan 1986; LaFond 1995; Rahman 2000). Low quality of modern health services deters rural people from using them in Java, Nigeria and Guatemala (Annis 1981; Murphy & Baba 1981; Young 2001). In rural Ethiopia, people by‐passed the referral system and approached the better‐equipped hospital for primary health care in spite of the larger distance involved (Kroeger 1983).
Maternal
In Ghana, Mills and Bertrand explored the role of access vs. traditional beliefs in the decision to seek obstetric care from health professionals. Among accessibility factors nurses' attitudes were a major barrier to care and traditional beliefs were less significant (Mills & Bertrand 2005). The use of primary health units and the referral hospital was considered only as a last resort in a Uganda‐based study. The study found that lack of skilled staff at primary health‐care level, complaints of abuse, neglect and poor treatment in hospital and poorly understood reasons for procedures, plus health workers' views that women were ignorant as explanation behind the unwillingness of women to deliver in health facilities and seek care for complications (Kyomuhendo 2003).
A particularly revealing study from India explored key social, economic and cultural factors influencing women's decisions to use maternal health care and the places used for child delivery. The study demonstrated that socio‐economic status was not found to be a barrier to service use when women perceived the benefits of the service to outweigh the cost. A large number of women perceived private services to be superior to those provided by the government, although cost often meant they were unable to use them. The provision of services did not ensure that women used them; they had to first perceive them to be beneficial to their health and that of their unborn child. Respondents identified the poor quality of services offered at government institutions to be a motivating factor for delivering at home (Griffiths & Stephenson 2001).
Among other barriers to prenatal care in a USA‐based study, study informants pointed to a lack of coordination between different social and health programmes and inhospitable conditions at the sites where prenatal care was delivered (Brown 1989).
The attitudes of the frontline clerical staff proved to be a significant barrier during a study based in the USA (Fallon & Fishler 1994). In this study, patient dissatisfaction with prenatal care was linked to poor attitudes about the patients, patient benefits and low recognition.
Kwast (1996) suggested that the availability of humane and functioning obstetric services and improved quality of care that takes into account both client satisfaction and provider fulfilment were prerequisites for improving access to prenatal care.
Quality of the provider and provider knowledge and the impact on access to competent prenatal care were assessed in a study based in Cameroon (Tita et al. 2005). This study explored the awareness of evidence‐based reproductive health interventions among service providers and found that this varied from 29% for the use of antenatal corticosteroids to 97% for the use of iron and folic acid supplementation during pregnancy. Their use of these interventions ranged from 10.2% for antenatal corticosteroids to 94.8% for iron and folic acid supplementation. Only 15.5% (95% CI, 11.8–20.0) of health workers were aware of four vital interventions, and only 12/312 (3.8%; 95% CI, 2.0–6.6) reported using all of them regularly. A deficiency in the education and training of health workers, especially a lack of continuing education, was commonly identified as the most important barrier to their awareness of evidence‐based practices. A lack of awareness and a lack of supplies and materials were the main barriers to high‐quality practice. Even in developed countries provider attitudes and knowledge about the cost‐effectiveness of evidence‐based interventions can be crucial in providing services. One study (Jafari et al. 1995) in the USA revealed that physicians who did not screen antenatal patients for Group B Streptococcus cited that reasons for not screening were ‘no clear guidelines’ and ‘not cost‐effective’ (52% and 39% respectively). These barriers to appropriate practice translate into barriers to high‐quality care.
Child
The use of child immunization services in Canada was deterred by a variety of factors including quality of care issues, such as traumatic immunization experiences, fear of vaccine side‐effects and sequelae, and negative interactions with health professionals (Tarrant & Gregory 2003).
Discussion
When access to health services is viewed through a theory vs. practice approach, the literature shows that most studies in this area are built around socio‐cultural barriers and financial barriers, which seem to present a myriad of challenges.
These same socio‐cultural barriers may be encountered between regular health services for MCH and MCH for mainstreaming nutrition in that the providers and the patient population will be unaccustomed to interacting in this area. In addition to overcoming the barriers to seeking modern health services, changing the predominant provider and client view of health services as strictly curative in nature to one that is both curative and preventative is highly improbable in developing countries overburdened with disease and fragile health systems. Therefore, nutritional services are best positioned as complementary to location‐based service delivery points where interventions are delivered. For example, delivery points can range from home deliveries to health facility‐based care, as well as mass promotion events and child health/immunization campaigns. Each of these delivery mechanisms can reach a population at several client contact points.
An acceptability assessment should be conducted before scaling up any new programme. Long‐standing cultural norms and beliefs will have to be overcome for the MCH population to accept nutritional services from health providers who are not a traditional source of such information. Providers must also be trained and motivated to provide a new form of services or else the financial and temporal investment of the promoting agencies may not result in a measurable increase in the use of services or health of the population (C. Larson, ICDDRB, Dhaka, pers. comm.).
Sustained health development requires people to be aware of modern scientific concepts of disease causation and to have the means to act on that knowledge (Mosley & Chen 1984). Parents' belief about the causes of illness (natural or supernatural), and the effectiveness of medicine, guides choice and use of modern medical care have a tremendous impact on the approach to care seeking for family members. If someone believes that evil spirits cause a particular disease, he/she will hardly use modern medicine to treat it. Micro‐level morbidity surveys in developing countries have documented a high prevalence of beliefs in causes of illness different from those held by modern biomedical science. Additionally, traditional nutritional beliefs will be encountered and challenged through the mainstreaming of nutrition in the public health sector.
Financial barriers were observed from a variety of approaches in health systems both with and without health insurance. In health insurance‐based systems, lack of insurance or inadequate insurance coverage played a significant barrier to access. Among those studies without health insurance, poverty and the cost of care were barriers to care.
Quality remains difficult to operationalize as a barrier to care on account of its various levels and approaches. However, in terms of limiting access to care, numerous studies demonstrated that quality was an important factor. Patient perceptions of quality, staff attitudes and providers' appropriate use of evidence‐based medicine each play a role in facilitating or hindering health service utilization. Given the diverse components of quality, any new initiative in the health system or health service delivery system should attempt to address as many as possible of the components in the planning and development phase to prevent perceptions of poor quality that inhibit future use.
Given the wide range of barriers to care that exist both in theory and in practice, research in this area would benefit greatly from the development of a rigorous typology so that more meta‐analytical review could be conducted in this area. Further, primary studies are needed to assess and evaluate the broad spectrum of barriers that are described in the background literature. More studies should also be conducted and published from low‐ and middle‐income countries.
This review suggests that a systematic review of the effectiveness of existing nutrition programmes should be conducted before embarking on a new nutrition programme venture.
It is likely that publication bias exists in the sampling of articles included in this review. The tendency among researchers, writers and editors to not pursue publication for weak or insignificant study outcomes may be present here. Few studies were found that did not address a significant barrier in access to care. It is further likely that small studies, particularly without positive results, were only used as guidance for local programmes and may only have seen publication in the form of working papers. As it stands, it is impossible to collect or to be sure that a review project has collected all of the studies or data that are available in a particular subject area (Dickersin 1990; Kleijnen & Knipschild 1992). A complete dissemination of knowledge would be helpful in forming future research in this area. Similar to the current movement to register clinical trials, there should be a mechanism by which non‐clinical research can be registered and then, that registration information can be accessed.
Incorporating nutrition initiatives into existing maternal–child health services represents a major shift both at the policy and at the programmatic level from the current focus of the health systems of many nations. The 2015 deadline for the Millennium Development Goals is rapidly approaching, which necessarily produces a sense of urgency in policy and programme development. Inclusion of a new programme into an existing system as opposed to the development of yet another stand‐alone programme bodes favourably with current thinking (Travis et al. 2004). In general key issues facing decision makers include repairing fragile health systems of developing nations rather than investing and further diverging existing financial, temporal and human resources into another vertical programme. The possibility exists that additional investment of nutrition resources into the health system could have the effect of strengthening health‐care systems. However, even if nutrition is successfully mainstreamed into existing maternal and child health services, the challenge remains that, if unchanged, the barriers to accessing existing health services could now include that of preventative and curative nutrition services.
Conflicts of interest
The authors have declared no conflicts of interest.
Footnotes
For a detailed overview of racial and ethnic barriers to care in the USA, the authors refer you to Institute of Medicine (2003).
References
- Adamu Y.M. & Salihu H.M. (2002) Barriers to the use of antenatal and obstetric care services in rural Kano, Nigeria. Journal of Obstetrics and Gynaecology 22, 600–603. [DOI] [PubMed] [Google Scholar]
- Alam N. (2000) Women, Households and Communities and the Care of Sick Children in Rural Bangladesh. Unpublished PhD Thesis. University of London: London. [Google Scholar]
- Alexandre P., Saint‐Jean G., Crandall L. & Fevrin E. (2005) Prenatal care utilization in rural areas and urban areas of Haiti. Revista Panamericana de Salud Publica 18, 84–92. [DOI] [PubMed] [Google Scholar]
- Annis S. (1981) Physical access and utilization of health services in rural Guatemala. Social Science and Medicine 15, 515–524. [DOI] [PubMed] [Google Scholar]
- Arifeen S.E., Bryce J., Gouws E., Baqui A.H., Black R.E., Hoque D.M.E. et al (2005) Quality of care for under‐fives in first‐level health facilities in one district of Bangladesh. Available at: http://www.who.int/bulletin/volumes/83/4/arifeen0405abstract/en/print.html (accessed January 2008). [PMC free article] [PubMed]
- Ashraf A., Chowdhury S. & Streefland P. (1982) Health, disease and health‐care in Bangladesh. Social Science and Medicine 16, 2041–2054. [DOI] [PubMed] [Google Scholar]
- Aved B., Irwin M., Cummings L. & Findeisen N. (1993) Barriers to prenatal care for low‐income women. Western Journal of Medicine 158, 493–498. [PMC free article] [PubMed] [Google Scholar]
- Barton P.L. (2003) Understanding the US Health Services System, 2nd edn. Health Administration Press: Washington, DC. [Google Scholar]
- Beckmann C.A., Buford T.A. & Witt J.B. (2000) Perceived barriers to prenatal care services. MCN American Journal of Maternal Child Nursing 25, 43–46. [DOI] [PubMed] [Google Scholar]
- Bennett I., Switzer J., Aguirre A., Evans K. & Barg F. (2006) ‘Breaking it down’: patient–clinician communication and prenatal care among African American women of low and higher literacy. Annals of Family Medicine 4, 334–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhuiya A. & Streatfield K. (1995) Feeding, home‐remedy practices and consultation with health care providers during childhood illness. Journal of Diarrhoea Disease Research 13, 106–112. [PubMed] [Google Scholar]
- Blendon R., Donelan K., Leitman R., Epstein A., Cantor J., Cohen A. et al (1993) Health reform lessons learned from physician in three nations. Health Affairs (Millwood) 12, 194–203. [DOI] [PubMed] [Google Scholar]
- Bronstein J.M., Capilouto E., Carlo W.A., Haywood J.L. & Goldenberg R.L. (1995) Access to neonatal intensive care for low‐birthweight infants: the role of maternal characteristics. American Journal of Public Health 85, 357–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown S. (1989) Drawing women into prenatal care. Family Planning Perspective 21, 73–80. [PubMed] [Google Scholar]
- Buekens P. (1990) Variations in provision and uptake of antenatal care. Baillieres Clinical Obstetrics and Gynaecology 4, 187–205. [DOI] [PubMed] [Google Scholar]
- Chen L., Huq E. & D'Souza S. (1981) Sex bias in family allocation of food and health care in rural Bangladesh. Population and Development Review 7, 55–70. [Google Scholar]
- Delvaux T., Buekens P., Godin I. & Boutsen M. (2001) Barriers to prenatal care in Europe. American Journal of Preventive Medicine 21, 52–59. [DOI] [PubMed] [Google Scholar]
- Dickersin K. (1990) The existence of publication bias and risk factors for its occurrence. Journal of the American Medical Association 263, 1385–1389. [PubMed] [Google Scholar]
- Dujardin B., Clarysse G., Criel B., De Brouwere V. & Wangata N. (1995) The strategy of risk approach in antenatal care: evaluation of the referral compliance. Social Science and Medicine 40, 529–535. [DOI] [PubMed] [Google Scholar]
- Fallon P.D. & Fishler L.S. (1994) Clerical staff attitudes toward patients in 19 prenatal care clinics in New York City. American Journal of Perinatology 11, 362–366. [DOI] [PubMed] [Google Scholar]
- Fauveau V., Stewart K., Khan S.A. & Chakraborty J. (1991) Effect on mortality of community‐based maternity‐care programme in rural Bangladesh. Lancet 338, 1183–1186. [DOI] [PubMed] [Google Scholar]
- Flores G., Abreu M. & Tomany‐Korman S.C. (2005) Limited English proficiency, primary language at home, and disparities in children's health care: how language barriers are measured matters. Public Health Report 120, 418–430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gates‐Williams J., Jackson M.N., Jenkins‐Monroe V. & Williams L.R. (1992) The business of preventing African‐American infant mortality. Western Journal of Medicine 157, 350–356. [PMC free article] [PubMed] [Google Scholar]
- Gazmararian J.A., Arrington T.L., Bailey C.M., Schwarz K.S. & Koplan J.P. (1999) Prenatal care for low‐income women enrolled in a managed‐care organization. Obstetrics and Gynecology 94, 177–184. [DOI] [PubMed] [Google Scholar]
- Glei D.A., Goldman N. & Rodriguez G. (2003) Utilization of care during pregnancy in rural Guatemala: does obstetrical need matter? Social Science and Medicine 57, 2447–2463. [DOI] [PubMed] [Google Scholar]
- Griffiths P. & Stephenson R. (2001) Understanding users' perspectives of barriers to maternal health care use in Maharashtra, India. Journal of Biosocial Science 33, 339–359. [DOI] [PubMed] [Google Scholar]
- Gummi F.B., Hassan M., Shehu D. & Audu L. (1997) Community education to encourage use of emergency obstetric services, Kebbi State, Nigeria. The Sokoto PMM Team. International Journal of Gynaecology and Obstetrics 59 (Suppl. 2), S191–S200. [DOI] [PubMed] [Google Scholar]
- Guyon A.B., Barman A., Ahmed J.U., Ahmed A.U. & Alam M.S. (1994) A baseline survey on use of drugs at the primary health care level in Bangladesh. Bulletin of the World Health Organization 72, 265–271. [PMC free article] [PubMed] [Google Scholar]
- Habib O.S. & Vaughan J.P. (1986) The determinants of health services utilization in southern Iraq: a household interview survey. International Journal of Epidemiology 15, 395–402. [DOI] [PubMed] [Google Scholar]
- Harvey S.M. & Faber K.S. (1993) Obstacles to prenatal care following implementation of a community‐based program to reduce financial barriers. Family Planning Perspectives 25, 32–36. [PubMed] [Google Scholar]
- Hashemi S. (1995) Disparate responses to medical emergencies in rural Bangladesh. Population Council Dhaka: Bangladesh. [Google Scholar]
- Helman, C.G. (1990) Culture, Health and Illness. Butterworth Heinemann: Oxford. [Google Scholar]
- Hill A., MacLeod W., Joof D., Gomes P., Ratcliffe A. & Walraven G. (2000) Decline of mortality in children in rural Gambia: the influence of village‐level primary health care. Tropical Medicine International Health 5, 107–118. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (2003) Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. National Academies Press: Washington, DC. [PubMed] [Google Scholar]
- Islam A. (1992) A majority remain untreated, Bangladesh. Integration 33, 46–49. [PubMed] [Google Scholar]
- Jafari H.S., Schuchat A., Hilsdon R., Whitney C.G., Toomey K.E. & Wenger J.D. (1995) Barriers to prevention of perinatal group B streptococcal disease. Pediatric Infectious Disease Journal 14, 662–667. [DOI] [PubMed] [Google Scholar]
- Jeppesen E.Z. (1993) [Obstetric health care offered to Turkish immigrant women – a quality assessment. Ugeskr Laeger 155, 3849–3854. [PubMed] [Google Scholar]
- Kalmuss D. & Fennelly K. (1990) Barriers to prenatal care among low‐income women in New York City. Family Planning Perspectives 22, 215–218, 231. [PubMed] [Google Scholar]
- Kendall C. (1983) Anthropology, communications, and health: the mass media and health practices program in Honduras. Human Organization 42, 353–360. [DOI] [PubMed] [Google Scholar]
- Khan M., Mwaku R.M., McClamroch K., Kinkela D.N. & Van Rie A. (2005) Prenatal care in Kinshasa: knowledge, beliefs, and barriers to timely care. Sante 15, 93–97. [PubMed] [Google Scholar]
- Kielmann A.A. (1983) Child and Maternal Health Services in Rural India: The Narangwal Experiment, Volume I: Integrated Nutrition and Health Care. Johns Hopkins University Press: Baltimore, MD. [Google Scholar]
- Kleijnen J. & Knipschild P. (1992) Review articles and publication bias. Azrneimittelforschung 42, 587–591. [PubMed] [Google Scholar]
- Kleinman, A. (1980) Patients and healers in the context of culture. University of California Press: Berkeley, CA. [Google Scholar]
- Kogan M.D., Alexander G.R., Mor J.M. & Kieffer E.C. (1998) Ethnic‐specific predictors of prenatal care utilisation in Hawaii. Paediatric and Perinatal Epidemiology 12, 152–162. [DOI] [PubMed] [Google Scholar]
- Kroeger A. (1983) Anthropological and socio‐medical health care research in developing countries. Social Science and Medicine 17, 147–161. [DOI] [PubMed] [Google Scholar]
- Kwast B.E. (1996) Reduction of maternal and perinatal mortality in rural and peri‐urban settings: what works? European Journal of Obstetrics, Gynecology, and Reproductive Biology 69, 47–53. [DOI] [PubMed] [Google Scholar]
- Kyomuhendo G.B. (2003) Low use of rural maternity services in Uganda: impact of women's status, traditional beliefs and limited resources. Reproduction Health Matters 11, 16–26. [DOI] [PubMed] [Google Scholar]
- LaFond A. (1995) Sustaining Primary Health Care. Save the Children, Earthscan Publications: London. [Google Scholar]
- Lassey M., Lassey W. & Jinks M. (1997) Health Care Systems around the World: Characteristics, Issues, Reforms. Prentice Hall: New Jersey. [Google Scholar]
- Levin A., Rahman M.A., Quayyum Z., Routh S. & Khuda B. (1998) Demand for Child Curative Care in Two Rural Thanas of Bangladesh: Effects of Income and Women's Employment. Operations Research Project Working Paper No. 150, International Centre for Diarrhoeal Disease Research, Bangladesh.
- Levin M. (2006) Language as a barrier to care for Xhosa‐speaking patients at a South African paediatric teaching hospital. South African Medical Journal 96, 1076–1079. [PubMed] [Google Scholar]
- Lohr K. (1990) Medicare: A strategy for Quality Assurance. National Academy Press: Washington, DC. [PubMed] [Google Scholar]
- Mbonye A.K. (1998) Prevalence of childhood illnesses and care‐seeking practices in rural Uganda. Scientific World Journal 19, 721–730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mechanic D. (1992) Health and illness behavior and patient‐practitioner relationship. Social Science and Medicine 34, 1345–1350. [DOI] [PubMed] [Google Scholar]
- Mills A. & Ranson M. (2006) The design of health systems In: International Public Health: Diseases, Programs, Systems, and Policies (eds Merson M., Mills A. & R. Black), 2nd edn, pp 513–551. Jones and Bartlett: Sudsbury, MA. [Google Scholar]
- Mills S. & Bertrand J.T. (2005) Use of health professionals for obstetric care in northern Ghana. Studies in Family Planning 36, 45–56. [DOI] [PubMed] [Google Scholar]
- Moore P. & Hepworth J.T. (1994) Use of perinatal and infant health services by Mexican‐American Medicaid enrollees. Journal of the American Medical Association 272, 297–304. [PubMed] [Google Scholar]
- Mor J.M., Alexander G.R., Kogan M.D., Kieffer E.C. & Hulsey T.C. (1995) Determinants of prenatal care use in Hawaii: implications for health promotion. American Journal of Preventive Medicine 11, 79–85. [PubMed] [Google Scholar]
- Mosley W.H. & Chen L.C. (1984) An analytical framework for the study of child survival in developing countries. Population and Development Review 10 (Suppl.), 25–44. [PMC free article] [PubMed] [Google Scholar]
- Murphy M. & Baba T.M. (1981) Rural dwellers and health care in northern Nigeria. Social Science and Medicine 15, 265–271. [DOI] [PubMed] [Google Scholar]
- Mwabu G.M. (1986) Health care decisions at the household level: results of rural health survey in Kenya. Social Science and Medicine 22, 315–319. [DOI] [PubMed] [Google Scholar]
- Nessa F., Rahman S. & Banu S. (1991) Self care in health. Bangladesh Medical Research Council Bulletin 17, 63–73. [PubMed] [Google Scholar]
- Newacheck P.W. (1994) Poverty and childhood chronic illness. Archives of Pediatrics and Adolescent Medicine 148, 1143–1149. [DOI] [PubMed] [Google Scholar]
- Orubuloye T.O. & Caldwell J.C. (1975) The impact of public health services on mortality: a study of mortality differentials in a rural area in Nigeria. Population Studies 29, 259–272. [Google Scholar]
- Pallikadavath S., Foss M. & Stones R.W. (2004) Antenatal care: provision and inequality in rural north India. Social Science and Medicine 59, 1147–1158. [DOI] [PubMed] [Google Scholar]
- Pelletier D.L., Frongillo E.A. Jr, Schroeder D.G. & Habicht J.P. (1995) The effects of malnutrition on child mortality in developing countries. Bulletin of World Health Organization 73, 443–448. [PMC free article] [PubMed] [Google Scholar]
- Pelto G.H. (2006) Socio‐cultural Determinants of Care‐seeking: Implications for Interventions. Background paper for the World Health Organization.
- Penchansky R. & Thomas J. (1981) The concept of access: definition and relationship to consumer satisfaction. Medical Care 19, 127–140. [DOI] [PubMed] [Google Scholar]
- Pierson V.H., Schramm W., Stockbauer J., Land G., Hoffman H. & Herman A. (1994) Prenatal care access and pregnancy outcomes in Missouri. Missouri Medicine 91, 624–629. [PubMed] [Google Scholar]
- Piper J.M., Mitchel E.F. Jr & Ray W.A. (1994) Presumptive eligibility for pregnant Medicaid enrollees: its effects on prenatal care and perinatal outcome. American Journal of Public Health 84, 1626–1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollock D. (2001) Barriers to health care access: what counts and who's counting? Academic Emergency Medicine 8, 1016–1018. [DOI] [PubMed] [Google Scholar]
- Potter J.E. (1988) [Use of maternal health services in rural Mexico. Salud Publica de Mexico 30, 387–402. [PubMed] [Google Scholar]
- Prevention of Maternal Mortality Network (1992) Barriers to treatment of obstetric emergencies in rural communities of West Africa. Studies in Family Planning 23, 279–291. [PubMed] [Google Scholar]
- Rahaman M.M., Aziz K.M.S., Munshi M.H., Patwari Y. & Rahman M. (1982) A diarrhoea clinic in rural Bangladesh: influence of distance, age and sex on attendance and diarrhoeal mortality. American Journal of Public Health 72, 1124–1128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahman S. (2000) Utilization of Primary Health Care Services in Rural Bangladesh: The Population and Provider Perspectives. PhD Thesis. Health Services Research Unit London School of Hygiene and Tropical Medicine: UK.
- Roberts R.O., Yawn B.P., Wickes S.L., Field C.S., Garretson M. & Jacobsen S.J. (1998) Barriers to prenatal care: factors associated with late initiation of care in a middle‐class midwestern community. Journal of Family Practice 47, 53–61. [PubMed] [Google Scholar]
- Ryan G. (1998) What do sequential behavioral patterns suggest about the medical decision‐making process?: modeling home case management of acute illness in a rural Cameroonian village. Social Science and Medicine 46, 209–225. [DOI] [PubMed] [Google Scholar]
- Sauerborn R., Nougtara A. & Diesfield H.J. (1989) Low utilization of community health workers: results from a household interview survey in Burkina Faso. Social Science and Medicine 29, 1163–1174. [DOI] [PubMed] [Google Scholar]
- Sokoloski E.H. (1995) Canadian First Nations women's beliefs about pregnancy and prenatal care. Canadian Journal of Nursing Research 27, 89–100. [PubMed] [Google Scholar]
- Stewart M.K., Parker B., Chakraborty J. & Begum H. (1994) Acute respiratory infection (ARI) in rural Bangladesh: perceptions and practices. Medical Anthropology 15, 377–394. [DOI] [PubMed] [Google Scholar]
- Szmoisz S., Vuegen S.E., Plaza A.S., Barracchini R., Checa S., Derlindati A. et al (1990) Argentina: risk factors and maternal mortality in La Matanza, Province of Buenos Aires, 1990. World Health Statistics Quarterly 48, 4–7. [PubMed] [Google Scholar]
- Tarrant M. & Gregory D. (2003) Exploring childhood immunization uptake with First Nations mothers in north‐western Ontario, Canada. Journal of Advanced Nursing 41, 63–72. [DOI] [PubMed] [Google Scholar]
- Tita A.T., Selwyn B.J., Waller D.K., Kapadia A.S. & Dongmo S. (2005) Evidence‐based reproductive health care in Cameroon: population‐based study of awareness, use and barriers. Bulletin of the World Health Organization 83, 895–903. Epub 30 January 2006. [PMC free article] [PubMed] [Google Scholar]
- Tossounian S.A., Schoendorf K.C. & Kiely J.L. (1997) Racial differences in perceived barriers to prenatal care. Maternal and Child Health Journal 1, 229–236. [DOI] [PubMed] [Google Scholar]
- Travis P., Bennett S., Haines A., Pang T., Bhutta Z., Hyder A. et al (2004) Overcoming health‐systems constrains to achieve the Millennium Development Goals. Lancet 362, 900–906. [DOI] [PubMed] [Google Scholar]
- Turner N., Hounsell D., Robinson E., Tai A. & Whittle N. (1999) Uptake of postnatal services for mothers of newborn babies up to eight weeks of age. New Zealand Medical Journal 112, 395–398. [PubMed] [Google Scholar]
- UNICEF (1998) The State of World's Children. Oxford University Press: Oxford. [Google Scholar]
- Varkevisser C., Pathmanathan I. & Brownlee A. (2003) Designing and Conducting Health Systems Research projects. Part I: Proposal Development and Fieldwork. KIT Publishers: Amsterdam. [Google Scholar]
- Wilson J.B., Collison A.H., Richardson D., Kwofie G., Senah K.A. & Tinkorang E.K. (1997) The maternity waiting home concept: the Nsawam, Ghana experience. The Accra PMM Team. International Journal of Gynaecology and Obstetrics 59 (Suppl. 2), S165–S172. [DOI] [PubMed] [Google Scholar]
- Woelfel M.L., Abusabha R., Pruzek R., Stratton H., Chen S.G. & Edmunds L.S. (2004) Barriers to the use of WIC services. Journal of the American Dietetic Association 104, 736–743. [DOI] [PubMed] [Google Scholar]
- World Bank (2006) Repositioning Nutrition as Central to Development: A Strategy for Large‐scale Action. Directions in Development. World Bank: Washington, DC. [Google Scholar]
- World Health Organization (1978) Declaration of Alma Ata. International Conference on Primary Healthcare. 12 September 1978. Available at: http://www.who.int/hpr/NPH/docs/declaration_almaata.pdf (accessed 5 May 2007).
- Yakoboski P., Ratner J. & Gross D. (1994) The effectiveness of budget targets and caps in the German ambulatory care sector. Benefits Quarterly 10, 31–37. [PubMed] [Google Scholar]
- Yawn B.P., Xia Z., Edmonson L., Jacobson R.M. & Jacobsen S.J. (2000) Barriers to immunization in a relatively affluent community. Journal of the American Board of Family Practice 13, 325–332. [PubMed] [Google Scholar]
- Young N. (2001) The pre‐hospital experiences of Samoan families who have had a child admitted to hospital with pneumonia: a qualitative investigation. Pacific Health Dialog 9, 20–28. [PubMed] [Google Scholar]


