Abstract
Vitamin D deficiency is associated with poor bone health, colorectal cancer, type 1 diabetes and multiple sclerosis. Two national health‐related societies in Canada have made recommendations for vitamin D supplementation, yet little research has been reported on the vitamin D status of Canadians. Lifestyle changes, such as sunscreen use, spending less time outdoors and insufficient intake of vitamin D‐containing foods as well as northern latitude, may be affecting human vitamin D status. A cross‐sectional analysis of 25‐hydroxyvitamin D [25‐(OH)D] was conducted in pregnant women, newborns (umbilical cord blood) and children. Samples were analysed by liquid chromatography mass spectrometry. Published ranges for 25‐(OH)D were used to determine vitamin D status. The prevalence of 25‐(OH)D deficiency for the three groups studied revealed most concentrations in the 25‐(OH)D deficiency or insufficiency ranges. There were significant differences in all groups studied between seasons, with the exception of maternal blood and female cord blood samples. 25‐(OH)D insufficiency was common in all groups for winter and summer, more so in winter. 25‐(OH)D insufficiency was common in the three groups studied. The Newfoundland and Labrador population may be at increased risk for vitamin D insufficiency because of factors such as northern latitude and lifestyle issues. Further research on the vitamin D status of this population is important, considering the potential adverse health‐related outcomes and the recommendations on supplementation being made.
Keywords: vitamin D insufficiency, pregnancy, newborns, children, Newfoundland and Labrador
Introduction
Vitamin D insufficiency and deficiency have been associated with many diseases, including multiple sclerosis, cancer (Garland et al. 2006; Holick 2006), type 1 diabetes (Hypponen 2004), psychiatric illness (Gloth III et al. 1999) and cardiovascular disease (Krause et al. 1998). Two national health‐related societies in Canada have recently made recommendations for vitamin D supplementation. The Canadian Pediatric Society recommended 2000 IU of vitamin D daily to pregnant and lactating women, especially during the winter months (Canadian Pediatric Society 2007). The Canadian Cancer Society recommended 1000 IU vitamin D daily for adults during the fall and winter to prevent cancer (Canadian Cancer Society 2007). These recommendations have been made despite scant research on the vitamin D status of Canadians.
The vitamin D status of people living in Newfoundland and Labrador (NL) (latitudes 46°N and 53°N), Canada, has not been previously studied. We measured 25‐hydroxyvitamin D [25‐(OH)D] concentrations in three groups of individuals hypothesizing that vitamin D insufficiency may be common because of Newfoundland's northern latitude and other lifestyle issues.
Subjects and methods
The study was approved by the Human Investigations Committee of Memorial University (in accordance with the Declaration of Helsinki). An anonymous cross‐sectional analysis of serum 25‐(OH)D in three patient groups was conducted. Approximately equal numbers of unmatched samples were taken at the end of summer (September 2005) and the end of winter (March 2006). The three groups included: group 1, pregnant women undergoing routine prenatal blood work collected from the provincial public health laboratory; group 2, umbilical cord blood samples, taken routinely at the time of birth and group 3, paediatric samples collected from children ages 0–14 years that presented to the children's hospital and had blood work [complete blood count (CBC or electrolytes)] performed. Leftover blood was sampled. A laboratory records review was performed on the paediatric samples searching for elevated glucose, glycosylated hemoglobin (A1C) or thyroid stimulating hormone (TSH), to exclude patients with diabetes or hypothyroidism, conditions which could be associated with vitamin D insufficiency. All samples came from individuals residing on the Avalon Peninsula of NL. We did not ascertain the ethnic background of patients; it is highly likely that the vast majority were Caucasian (98% of residents are documented as English or Irish descent) (Rahman et al. 2003).
Definitions of 25‐(OH)D status were based on published guidelines; however, international cut‐offs for insufficiency or deficiency have not been established. Therefore, we presented the results using several cut‐offs (including those used by two Canadian studies: Rucker et al. 2002 and Roth et al. 2005): deficiency <25 nmol L−1, deficiency <50 nmol L−1, insufficiency 25–75 nmol L−1 and sufficiency >75 nmol L−1 (Dawson‐Hughes et al. 2005; Holick 2007).
Vitamin D
The 25‐(OH)D3 analysis was performed at the provincial tertiary care hospital. Aliquots of 1 mL were taken from the samples, centrifuged to remove contaminating red blood cells, and the supernatant was frozen and stored at −70°C. Patient sera or quality control samples (250 µL) were added to 25 µL of D6‐26,27‐(OH)D3 for an internal standard in methanol (200 nmol L−1 final concentration) (Alvarez & DeMazancourt 2001). Briefly, the samples containing internal standard were incubated at 37°C for 2 h in the dark in 1.5‐mL microfuge tubes, and then 200 µL of 95% ethanol was added and the samples were vortexed for 1 min. Samples were then extracted once by adding 1 mL of hexane : dichloromethane (90:10 v/v), vortexing for 1 min, and centrifuged. The upper organic layer was transferred to a fresh vial and evaporated to dryness under a stream of nitrogen. The residue was reconstituted in 100 µL of methanol and 20 µL was injected and analysed by LC‐MS/MS (liquid chromatography‐mass spectrometry) on a Waters Symmetry C8 3.5 µm (2.1 mm × 50 mm) column and separated in a solvent system containing methanol and 0.05% formic acid in water (Maunsell et al. 2005). Liquid chromatography was carried out on a Waters High Performance Liquid Chromatography System (2795 Separation module) and detection and quantification by positive ion electrospray ionization on a Micromass Quattro Ultima PT mass spectrometer. The instrument was operated in multiple reaction monitoring mode with monitoring of the transitions 401.6 > 159.1 and 401.6 > 365.3 for 25‐(OH)D3, and 407.7 > 371.3 and 407.7 > 389.5 for D6‐26,27‐(OH)D3.
Statistical analysis
Descriptive statistics were conducted on the 25‐(OH)D concentrations (mean, standard deviation). Independent sample's t‐tests were used to compare 25‐(OH)D concentrations for seasonal differences in each group. spss 14.0 was used for analyses. An α of 0.05 was used for statistical significance.
Results
The prevalence of 25‐(OH)D deficiency for the three groups studied is shown in Table 1. Most samples had concentrations in the 25‐(OH)D deficiency or insufficiency ranges (Table 1). The mean 25‐(OH)D concentrations for winter and summer seasons are shown in Table 2. There were significant differences in all groups studied between seasons, with the exception of maternal blood and female cord blood samples (Table 2). The prevalence of 25‐(OH)D deficiency, insufficiency and sufficiency are shown in Fig. 1 by season. Insufficiency is common in all groups for both seasons, more so in winter.
Table 1.
Prevalence of 25‐hydroxyvitamin D [25‐(OH)D] deficiency (<25 nmol L−1 or <50 nmol L−1), insufficiency (25–75 nmol L−1) and sufficiency (>75 nmol L−1) (winter and summer combined)
| 25‐(OH)D (nmol L−1) | Children | Maternal Blood* | Cord Blood | |||
|---|---|---|---|---|---|---|
| n = 48 | n = 50 | n = 51 | ||||
| n | % | n | % | n | % | |
| <25 | 0 | 0 | 1 | 2.0 | 2 | 3.9 |
| <50 | 17 | 35.4 | 21 | 42.0 | 18 | 35.3 |
| 25–75 | 37 | 77.1 | 39 | 78.0 | 41 | 82.4 |
| >75 | 11 | 22.9 | 10 | 20.0 | 8 | 15.7 |
1st trimester sample.
Table 2.
25‐hydroxyvitamin D [25‐(OH)D] concentrations per sample by season
| Sample | n | Mean 25‐(OH)D (nmol L−1) | Standard deviation | P‐value |
|---|---|---|---|---|
| Children | ||||
| Winter | 24 | 52.6 | 14.3 | 0.002 |
| Summer | 24 | 67.7 | 17.1 | |
| Male | ||||
| Winter | 14 | 50.4 | 12.0 | 0.042 |
| Summer | 13 | 63.2 | 17.8 | |
| Female | ||||
| Winter | 10 | 55.7 | 17.1 | 0.028 |
| Summer | 11 | 72.8 | 15.5 | |
| Maternal blood | ||||
| Winter | 25 | 51.9 | 17.9 | 0.075 |
| Summer | 25 | 61.1 | 17.8 | |
| Cord blood | ||||
| Winter | 24 | 48.6 | 17.5 | 0.002 |
| Summer | 27 | 63.3 | 13.5 | |
| Male | ||||
| Winter | 12 | 46.7 | 18.3 | 0.008 |
| Summer | 16 | 65.3 | 14.1 | |
| Female | ||||
| Winter | 12 | 50.6 | 17.3 | 0.128 |
| Summer | 11 | 60.5 | 12.6 | |
Figure 1.
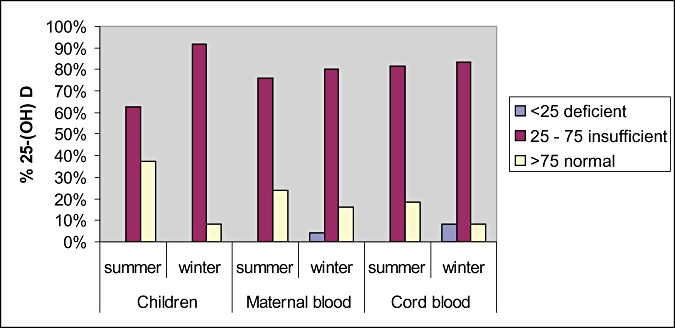
Prevalence of 25‐hydroxyvitamin D [25‐(OH)D] deficiency (<25 nmol L−1), insufficiency (25–75 nmol L−1) and sufficiency (>75 nmol L−1) by sample and season.
Discussion
Our study has shown that vitamin D insufficiency is common among three groups sampled.
Reporting vitamin D status on populations is not straight‐forward as there are no international consensus guidelines on the definitions of vitamin D status (Holick 2007). Some studies have used a cut‐off of <25 nmol L−1 to define deficiency, as this correlates clinically with rickets and osteomalacia. Controversy exists with the lower limit of normal (suggesting a sufficiency concentration). Research suggests that >75 nmol L−1 makes physiological sense, as at this level parathyroid hormone concentrations begin to level off, and intestinal calcium transport increases. Higher concentrations (>90 nmol L−1 or >100 nmol L−1) have been suggested by some for optimal health outcomes (Bischoff‐Ferrari et al. 2006). We presented our results using multiple cut‐offs to allow for comparison with other studies.
We have documented vitamin D deficiency and insufficiency in pregnant women and cord blood samples. Vitamin D insufficiency or deficiency in pregnancy or during the neonatal period may have important negative health consequences. A recent study of northern US black and white pregnant women and neonates revealed high levels of vitamin D deficiency and insufficiency, despite a high compliancy rate of prenatal vitamins containing vitamin D (Bodnar et al. 2007b). These authors found maternal vitamin D deficiency to be an independent risk factor for pre‐eclampsia (Bodnar et al. 2007a). Maternal vitamin D status may also have a significant impact on newborn bone mineral content and developing foetal bone (Namgung & Tsang 2000).
There are two published studies on the vitamin D status of Canadians. A pediatric study in Edmonton, Alberta (52°N) at the end of winter reported a mean 25‐(OH)D concentration of 47.2 nmol L−1 (95% CI 43.8–50.8 nmol L−1). Thirty‐four per cent of participants had vitamin D insufficiency (<40 nmol L−1) and 6% were deficient (<25 nmol L−1) (Roth et al. 2005). An adult study from Calgary, Alberta (51°N) also reported a high prevalence of vitamin D insufficiency [25‐(OH)D < 40 nmol L−1; 34% were deficient at least once out of the four sampling times] (Rucker et al. 2002). Our study revealed higher mean concentrations of 25‐(OH)D which may be due to differences in latitude. Both Canadian studies were consistent with our results; vitamin D insufficiency is common.
Other worrisome evidence of vitamin D insufficiency exists for Canadians. There have been 104 confirmed cases of rickets in Canada between 2002 and 2004 [serum 25‐(OH)D <27.5 nmol L−1], suggesting that high‐risk babies may not be receiving the recommended supplementation of vitamin D, or that the recommended amounts are insufficient (Ward et al. 2007).
St John's is the capital city of NL (47°N) and is one of the foggiest, snowiest and cloudiest of Canadian cities (Government of Canada 2004b). Less sunlight may mean a lower cutaneous synthesis of vitamin D. Human skin exposed to sunlight on cloudless days in Boston (42°N) in winter produced no previtamin D3. In Edmonton (52°N), this ineffective period extended from October through March (Webb et al. 1988).The latitude of St John's (47°N) is in between these geographic locations; however, more northern regions of NL may be worse off (Labrador City 52°N, Happy Valley‐Goose Bay 53°N, St Anthony 51°N). For long stretches of winter in NL, endogenous vitamin D production is likely very minimal to none. Fewer hours outdoors, use of sunscreen and advice to keep babies and children out of the sun may also be affecting vitamin D synthesis.
Newfoundland residents may not be consuming enough calcium in their diet, and as a result, not consuming enough vitamin D‐fortified food. A nutrition survey conducted in 2003 found that 92% of randomly selected NL residents were not consuming adequate levels of calcium (Roebothan 2003). The same study revealed that only 24% of NL residents took vitamin–mineral supplements (Roebothan 2003). Routine administration of vitamin D supplementation is recommended for exclusively breastfed infants (Government of Canada 2004a); however, a recent survey found that only 34% of babies in NL were given vitamin supplements (Twells et al. 2007). Other changes in diet, such as eating farmed salmon (75% less vitamin D than the wild variety), may be another contributing factor (Lu et al. 2007).
Our results are important as vitamin D insufficiency may be a significant health issue for NL residents and further study is required, including research on mother–baby pairs and associated health outcomes.
Key Messages
-
•
Vitamin D insufficiency is common in NL pregnant women, newborns and children.
-
•
Lifestyle changes may be contributing to vitamin D insufficiency.
-
•
Pregnant women, newborns and children may be at risk for adverse health outcomes because of vitamin D insufficiency.
-
•
Further study to assess vitamin D insufficiency and health outcomes is warranted.
-
•
Further study to assess the appropriateness of current vitamin D supplementation recommendations is needed.
Contributors
All of the authors made substantial contributions to the conception and design, acquisition of data or analysis and interpretation of data, drafted the article or revised it critically for important intellectual content and gave final approval of the version to be published.
Competing interests
None declared.
Acknowledgements
The Janeway Research Foundation funded this study. Thank you to Dr S. Ratnam, Dr Cindy Whitman and staff of the NL Public Health and Health Sciences laboratories, especially Ms Florence Stead, Mr Ahmed Mostafa and Ms June Hynes. The Janeway Research Foundation funded this study.
References
- Alvarez J.C. & De Mazancourt P. (2001) Rapid and sensitive high‐performance liquid chromatographic method for simultaneous determination of retinol, alpha‐tocopherol, 25‐hydroxyvitamin D3 and 25‐hydroxyvitamin D2 in human plasma with photodiode‐array ultraviolet detection. Journal of Chromatograph. B, Biomedical Sciences and Applications 755, 129–135. [DOI] [PubMed] [Google Scholar]
- Bischoff‐Ferrari H.A., Giovannucci E., Willett W.C., Dietrich T. & Dawson‐Hughes B. (2006) Estimation of optimal serum concentrations of 25‐hydroxyvitamin D for multiple health outcomes. The American Journal of Clinical Nutrition 84, 18–28. [DOI] [PubMed] [Google Scholar]
- Bodnar L.M., Catov J.M., Simhan H.N., Holick M.F., Powers R.W. & Roberts J.M. (2007a) Maternal vitamin D deficiency increases the risk of preeclampsia. Journal of Clinical Endocrinology and Metabolism 92, 3517–3522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bodnar L.M., Simhan H.N., Powers R.W., Frank M.P., Cooperstein E. & Roberts J.M. (2007b) High prevalence of vitamin D insufficiency in black and white pregnant women residing in the Northern United States and their neonates. The Journal of Nutrition 137, 447–452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Cancer Society (2007) Vitamin D Recommendation. Canadian Cancer Society: Toronto, ON. Available at: http://www.cancer.ca/ccs/internet/mediareleaselist/0,3208,3172_1613121606_1997621989_langId-en,00.html. [Google Scholar]
- Canadian Pediatric Society (2007) Vitamin D supplementation: recommendations for Canadian mothers and infants. Paediatrics & Child Health 12, 583–589. [PMC free article] [PubMed] [Google Scholar]
- Dawson‐Hughes B., Heaney R.P., Holick M.F., Lips P., Meunier P.J. & Vieth R. (2005) Estimates of optimal vitamin D status. Osteoporosis International 16, 713–716. [DOI] [PubMed] [Google Scholar]
- Garland C.F., Garland F.C., Gorham E.D., Lipkin M., Newmark H., Mohr S.B. et al (2006) The role of vitami D in cancer prevention. American Journal of Public Health 96, 252–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gloth F.M. III, Alam W. & Hollis B. (1999) Vitamin D vs. broad spectrum phototherapy in the treatment of seasonal affective disorder. The Journal of Nutrition, Health and Aging 3, 5–7. [PubMed] [Google Scholar]
- Government of Canada (2004a) Vitamin D for breastfed infant 2004 Health Canada Recommendation. Health Canada: Canada. Available at: http://www.healthcanada.ca/nutrition. [Google Scholar]
- Government of Canada (2004b) Yearly Hours of Sunshine in Canada. Environment Canada: Canada. Available at: http://www.atl.ec.gc.ca/climate/nfld.html. [Google Scholar]
- Holick M.F. (2006) Calcium plus vitamin D and the risk of colorectal cancer. The New England Journal of Medicine 354, 2287–2288. [DOI] [PubMed] [Google Scholar]
- Holick M.F. (2007) Vitamin D deficiency. The New England Journal of Medicine 357, 266–281. [DOI] [PubMed] [Google Scholar]
- Hypponen E. (2004) Micronutrients and the risk of type 1 diabetes: vitamin D, vitamin E, and nicotinamide. Nutrition Reviews 62, 340–347. [DOI] [PubMed] [Google Scholar]
- Krause R., Buhring M., Hopfenmuller W., Holick M.F. & Sharma A.M. (1998) Ultraviolet B and blood pressure. Lancet 352, 709–710. [DOI] [PubMed] [Google Scholar]
- Lu Z., Chen T.C., Zhang A., Persons K.S., Kohn N., Berkowitz R. et al (2007) An evaluation of the vitamin D3 content in fish: Is the vitamin D content adequate to satisfy the dietary requirement for vitamin D? The Journal of Steroid Biochemistry and Molecular Biology 103, 642–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunsell Z., Wright D.J. & Rainbow S.J. (2005) Routine isotope‐dilution liquid chromatography‐tandem mass spectrometry assay for simultaneous measurement of the 25‐hydroxy metabolites of vitamins D2 and D3. Clinical Chemistry 51, 1683–1690. [DOI] [PubMed] [Google Scholar]
- Namgung R. & Tsang R.C. (2000) Factors affecting newborn bone mineral content: in utero effects on newborn bone mineralization. The Proceedings of the Nutrition Society 59, 55–63. [DOI] [PubMed] [Google Scholar]
- Rahman P., Jones A., Curtis J., Bartlett S., Peddle L., Fernandez B. et al (2003) The Newfoundland population: a unique resource for genetic investigation of complex diseases. Human Molecular Genetics 12, R167–R172. [DOI] [PubMed] [Google Scholar]
- Roebothan B. (2003) Nutrition Newfoundland and Labrador: The Report of a Survey of Residents of Newfoundland and Labrador. Department of Health and Community Services: Province of NL, NL, Canada. [Google Scholar]
- Roth D.E., Martz P., Yeo R., Rosser C., Bell M. & Jones A.B. (2005) Are national vitamin D guidelines sufficient to maintain adequate blood levels in children? Canadian Journal of Public Health 96, 443–449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rucker D., Allan J., Fick G. & Hanley D. (2002) Vitamin D insufficiency in a population of healthy western Canadians. Canadian Medical Association Journal 166, 1517–1524. [PMC free article] [PubMed] [Google Scholar]
- Twells L., Day S. & Newhook L.A. (2007) Does breastfeeding protect preschool children from obesity? Atlantic Networks for Prevention Research Conference. St John's, NL, Canada (Abstract).
- Ward L.M., Gaboury I., Ladhani M. & Zlotkin S. (2007) Vitamin D‐deficiency rickets among children in Canada. Canadian Medical Association Journal 177, 161–166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb A.R., Kline L. & Holick M.F. (1988) Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. The Journal of Clinical Endocrinology and Metabolism 67, 373–378. [DOI] [PubMed] [Google Scholar]


