Abstract
The baby‐led weaning philosophy proposes that when solids are introduced, infants should be encouraged to self‐feed with solid food, as opposed to spoon‐feeding purees. We used data from the Gateshead Millennium Study (GMS) to define the range of ages at which infants reach out for and eat finger foods and related this to developmental status. GMS recruited infants shortly after birth and followed them prospectively using postal questionnaires. Of the 923 eligible children, 602 had data on when they first reached out for food, and 340 (56%) had done so before age 6 months, but 36 (6%) were still not reaching for food at age 8 months. Infants who had not reached out for food by 6 months were less likely to be walking unaided at age 1 year (85 out of 224, 38%) compared with those who did (155 out of 286, 54%; P < 0.001). For the 447 parents who completed a diary of the first five occasions when their child ate finger foods, the first finger food eaten was before age 6 months for 170 (40%) and before age 8 months for 383 (90%); foods offered were mainly bread, rusks or biscuits. Of the 604 with information at age 8 months about current intake, all but 58 (9.6%) were having some finger foods at least daily, but only 309 (51%) were having them more than once per day. Baby‐led weaning is probably feasible for a majority of infants, but could lead to nutritional problems for infants who are relatively developmentally delayed.
Keywords: infant nutrition, complimentary feeding, solid feeding, child development, epidemiology
Introduction
The age at which weaning solids should start had been much debated, but the World Health Organization (WHO) recommendation that this should be 6 months (World Health Organization 2002) has resulted in a reduction in the proportion of infants in the UK starting solids very early, although the proportion waiting until 6 months remains low (Bolling et al. 2007). However, there is now a new debate about the manner in which first solids should be offered, spearheaded in the UK by the baby‐led weaning (BLW) movement (Rapley & Murkett 2008), which recommends that first solids should be offered as solid ‘finger foods’, and that the infant be encouraged to self‐feed from the outset. This approach argues that the use of spoon feeding and purees is an adaptation to the introduction of solids at an inappropriate and un‐physiological age. They suggest that the later age at weaning now recommended by the WHO coincides with developmental readiness to reach out for and chew food. This is, in many ways, an attractive concept, but it does assume that developmental readiness will reliably coincide with the nutritional need for complementary solids. The BLW approach argues that the baby can continue to rely largely on breast milk until the baby has learnt the skills necessary to take nutritionally useful amounts, on average at around the age of 8 months (Rapley & Murkett 2008). However, published evidence does suggest that the majority of infants need solids by the age of 6 months, when increasing nutritional vulnerability outweighs the immune protective value of continued exclusive breastfeeding (Committee on Medical Aspects of Food 1994; Mehta et al. 1998; World Health Organization 2002). A further potential conflict with this approach is the suggestion that delaying introduction of solids risks missing a critical developmental window, leading to later feeding problems (Illingworth & Lister 1964). However, there is little research evidence to support this; one large study found that infants who started lumpy solids later (10 months or older) were more difficult to feed than those introduced earlier (Northstone et al. 2001), but the authors of that study point out that there is little else to suggest that the period before 6 months is a critical window for introducing solids (Northstone et al. 2001). We have previously described the pattern of introduction of solids in the Gateshead Millennium Study cohort and found little evidence that there was an effect of age of introduction on the ease with which they were accepted, although this was within a very narrow age range (4–6 months).
There is only limited published evidence on when children do begin to reach out for foods, or the age at which finger feeding usually becomes established (Northstone et al. 2001; Carruth & Skinner 2002; Carruth et al. 2004; Hetzner et al. 2009). Within the cohort described above, we have this information, so the aim of this paper is to describe the range of ages at which infants first reach out for food and how these relate to other aspects of development, to parental provision of finger foods and socio‐economic status.
Key messages
-
•
The baby‐led weaning philosophy proposes that when solids are introduced, infants should be encouraged to self‐feed with solid food, as opposed to spoon‐feeding purees. This approach has never been formally tested.
-
•
Previous studies in the UK and the USA suggest widely differing norms for the age when finger‐feeding skills are acquired, suggesting that this may be culturally determined.
-
•
We aimed to establish whether infants from a historic UK cohort would have been developmentally ready to self‐feed by age 6 months, when complementary feeding should start.
-
•
Most infants in the cohort started reaching out for food and eating finger foods between the ages of 4 and 7 months. Despite this, for many children, self‐feeding was still not a routine part of their meals at the age of 8 months.
-
•
Baby‐led weaning might be feasible for a majority of infants but could lead to nutritional problems for infants who were relatively developmentally delayed. A policy of promoting self‐feeding and family meals in parallel with spoon feeding might be more realistic.
Method
The Gateshead Millennium Study is a population‐based cohort that recruited infants shortly after birth in 1999–2000 (Parkinson et al. 2010), at which point baseline socio‐demographic data were collected. Families completed postal questionnaires at intervals in the first year, covering a range of topics mainly related to feeding. Ethical approval was granted by Gateshead and South Tyneside Local Research Ethics Committee.
At 6 weeks, 4 and 8 months families were asked whether they had started complementary solids (Wright et al. 2004). At 8 months, among other feeding questions, parents were asked, ‘When did your baby start reaching out for foods?’. They were also asked, ‘When was your baby first given finger foods?’ and ‘How often does your baby eat finger foods?’. Finger foods were defined for parents as ‘food your child can pick up and feed to themselves’. Parents were also asked whether their child partially or fully self‐fed or was fully fed by parent at meals. The questionnaire at 12 months included questions about development (see Table 1).
Table 1.
Age reached out for food and developmental stage at age 12 months
| Walking (N = 510*) | Words with meaning (N = 506*) | ||||||
|---|---|---|---|---|---|---|---|
| No | Round furniture | Without support | P (χ 2) | No | Yes | P (χ 2) | |
| All | 61 (12%) | 209 (41%) | 240 (47%) | 210 (41%) | 296 (59%) | ||
| Children without feeding data (N = 67) | 9 (13%) | 25 (37%) | 33 (49%) | 0.83 | 24 (36%) | 42 (64%) | 0.51 |
| Age reached out for food (months) | |||||||
| 4–5 | 8% (8) | 25% (26) | 67% (70) | 32% (33) | 68% (70) | ||
| 5–6 | 10% (18) | 43% (79) | 47% (85) | 44% (80) | 56% (102) | ||
| 6–7 | 10% (15) | 46% (69) | 44% (65) | 38% (55) | 62% (91) | ||
| 7–8 | 24% (10) | 52% (22) | 24% (10) | 57% (24) | 43% (18) | ||
| >8 | 30% (10) | 39% (13) | 30% (10) | <0.001 † | 54% (18) | 46% (15) | 0.013 † |
Total with that variable plus response for when reached out for food;
P, chi‐squared linear.
Infants born before 37 completed weeks of gestation were excluded, as were 33 infants from Haredi Jewish families as they had been found to have very different growth patterns that appeared to be associated with deferred and restricted complementary feeding practices (Wright et al. 2010).
Families in the study were issued with a parent‐held child record that included a finger‐feeding diary. Parents were asked to complete this on the first five occasions the child was given a finger food. For each occasion, the parents recorded the date, recorded the amount taken (none, hardly any, a mouthful, more than a mouthful) and described the type of food and how the child responded as free text. The diary was then either returned with the next postal questionnaire or retrieved from the record by survey staff when the child was brought for a health check at age 13 months. The food types were subsequently coded into food categories, and the age the finger foods were given was calculated.
The family post code was used to allocate their family's residential area (ED) to a deprivation quintile using Townsend scores compared with the deprivation levels for the Northern region (Wright et al. 2006). Families lacking one or more of three amenities (own home, wage earner in household, own car) were defined as deprived. The analysis was undertaken using SPSS v15 (IBM, Chicago, IL, USA). Associations between variables were explored using Spearman's non‐parametric correlations and chi‐squared analysis.
Results
Demographic and developmental characteristics
After exclusions (see Fig. 1), there were 609 with feeding data at 8 months; of these infants, 336 (57%) had been breastfed at some time, but only 124 (21%) had been breastfed for more than 4 months. The detailed demographic characteristics of the cohort have been described elsewhere (Wright et al. 2006; Parkinson et al. 2010). Of those returning the 8‐month questionnaire, all quintiles of the area‐based deprivation measure were reasonably represented, but more deprived families were slightly underrepresented, and the more affluent slightly overrepresented compared with the Northern region (most affluent, 21.4%; least affluent, 14.4%). Only 131 (23%) had received higher education, and 229 (37%) were classified as deprived using the individual measure. At age 12 months, 510 of the parents with earlier feeding data reported whether their child was yet walking, and 506 reported whether they were saying words with meaning (Table 1).
Figure 1.
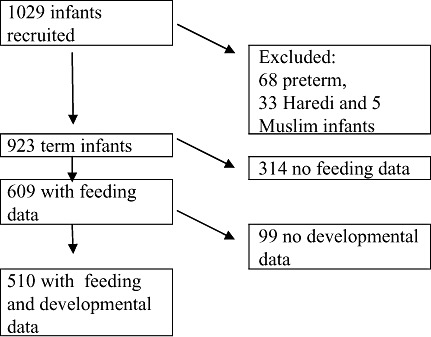
Flow chart for study participants.
What age did children reach out for food?
In the 8‐month questionnaire, 602 parents reported when their child started reaching out for food, and of these, 340 (56%) had done so before the age of 6 months, with 36 (6%) still not reaching out at the age of 8 months (Fig. 2). The age a child first reached out for food was unrelated to whether breastfed and to its duration. It was weakly, although significantly, correlated with the age they first had complementary solids (Spearman's r = 0.14, P < 0.001). The age a child reached out for food was related to developmental stage at age 12 months, with those infants who were already walking and saying words with meaning significantly more likely to have reached out for food at a younger age (see Table 1). Although age of first solids was weakly related to individual (Spearman's r = 0.15, P < 0.001) and area‐based deprivation (Spearman r with Townsend score quintile = 0.14, P < 0.001) as described in a previous paper (Wright et al. 2004), there was no association between age reached out for food and either individual (Spearman's r = 0.04, P = 0.35) or area‐based deprivation (Spearman's r with Townsend score quintile = −0.03, P = 0.43).
Figure 2.
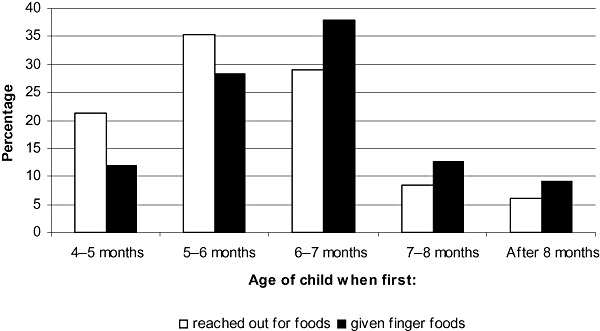
Frequency distribution of number of infants in cohort who first reached out for food and were given finger foods at different ages.
What age did children eat finger foods?
In the 8‐month questionnaire, 599 parents reported when they first offered finger foods; for 242 (40%), this was before the age of 6 months (Fig. 2). This was consistent with the diaries, which had been completed by 447 of the mothers, where 170 (40%) recorded their first diary finger food offer before age 6 months; 383 (90%) had done so by age 8 months, and all but one by the age of a year. In the diaries, the mean (standard deviation) age of first finger food was 6.35 (1.4) months, and the fifth was 6.85 (1.5) weeks. The commonest foods offered were bread, rusks or biscuits in some form, although by the fifth offer, 20% were fruit or vegetables, but only 2% were meat and 5% were confectionery (Table 2).
Table 2.
Types of first finger foods offered and amount eaten. Values are percentages unless otherwise stated
| Offer number | First | Second | Third | Fourth | Fifth |
|---|---|---|---|---|---|
| Food type | |||||
| Number responding | 447 | 431 | 414 | 397 | 380 |
| Bread or toast | 38.9 | 30.9 | 34.3 | 32.7 | 31.1 |
| Rusk or biscuit | 43.4 | 34.3 | 31.9 | 28.2 | 31.6 |
| Fruit/veg | 11.0 | 19.5 | 18.1 | 20.2 | 20.0 |
| Confectionery | 1.8 | 3.5 | 3.9 | 5.3 | 4.7 |
| Crisps | 2.0 | 3.7 | 4.1 | 4.0 | 4.7 |
| Meat | 1.1 | 0.7 | 1.4 | 2.3 | 1.8 |
| Teething stick | 0.2 | 1.2 | 0.2 | 0.0 | 0.0 |
| Other | 1.6 | 6.3 | 6.0 | 7.3 | 6.1 |
| Amount eaten | |||||
| Number responding | 445 | 431 | 416 | 396 | 379 |
| None | 5.8 | 3.9 | 2.2 | 3.0 | 1.1 |
| More than mouthful | 42.0 | 48.0 | 60.6 | 68.2 | 73.6 |
At 8 months, 604 parents reported their current intake of finger foods, and all but 58 (9.6%) were having some at least daily. However, only 309 (51%) were having them more than once per day, and 215 (35%) infants were still described as needing to be fully fed at meal times. The frequency finger foods were offered was inversely correlated with the age when the child first reached out for food (Spearman's r = −0.24, P < 0.001). However, of the 340 children who had been reaching out for food since before the age of 6 months, 18 (5%) were still being not offered finger foods on a daily basis, 124 (36%) were being offered them only once per day and 92 (27%) were regarded as unable to feed themselves at meal times.
Discussion
These results suggest that about half the infants in the cohort were reaching out for food and beginning to eat finger foods by the age of 6 months and the majority by age 8 months. There was a wide range of ages when this milestone was acquired, also described in other studies (Carruth et al. 2004), and the less developmentally advanced infants did so later on average. Our results seem quite in keeping with one UK survey that reported that 43% children were eating toast and 27% were eating biscuits before the age of 6 months (Northstone et al. 2001). However, they seem strikingly different from findings from US surveys. One large US telephone survey (Carruth et al. 2004) found that although 68% of 4–6‐month‐old children had begun grasping foods, only 53% of 7–8‐month‐old children were able to eat food that needed chewing. Another much smaller prospective study by the same author (Carruth & Skinner 2002) found mean age for ‘eating finger foods without gagging’ was 8.44 (range 6–12) months, although the mean age for ‘feeds self cracker or cookie’ was 7.7 (4–14) months. Both these studies also collected information on developmental milestones, but appear not to have related them to feeding skills within individuals. Another large US survey found that only 15% of mothers had ‘introduced finger foods’ before the age of 6 months (Hetzner et al. 2009), while a retrospective study comparing infants with major surgical problems with normal controls found that on average, the controls only started to ‘self‐feed finger foods’ at 10 months (Khan et al. 2009). These quite large differences suggest that there is a cultural, as well as developmental, influence on age of finger feeding. The age at which these skills are acquired depends greatly upon being given the opportunity to learn as well as developmental readiness. It is already recognized that age at ‘readiness’ for weaning is strongly culturally determined, but it seems likely that the same applies for finger foods.
A limitation in comparing our study with others is that each study has used a slightly different form of question regarding self‐feeding and finger foods, so that we cannot be sure that mothers' answers are directly comparable. A strength of our study is that the questionnaire data, which rely on recall, are underpinned by data from the feeding diaries that were collected contemporaneously. Although available for a smaller proportion of infants, the contemporaneous diaries are consistent with the questionnaire data. These data were collected 10 years ago, so they may not be fully generalizable to infants today, as in the intervening period the age at commencement of solids has increased and also possibly the duration of breastfeeding. However, this also means that these infants were studied well before the BLW approach began to be advocated, so that we can be sure that none of the mothers were influenced in their behaviour by that philosophy.
There has been very little formal research as yet into BLW. One study has attempted to explore the correlates of BLW using a web survey about weaning practice, targeted at mothers of infants aged 6–12 months, a majority of whom were at least familiar with BLW (Brown & Lee 2010). Not surprisingly, this suggested that mothers adopting the BLW feeding style breastfed for longer periods and were more affluent and highly educated. The survey did not ask specifically about finger feeding, but mothers reported that the first complementary food (given at a mean age of 5.1 months) was in solid as opposed to puree form for 52%, which contrasts with our cohort where 92% gave commercially produced purees of some kind (Wright et al. 2004). No study has yet examined the safety or nutrient sufficiency of BLW, but equally there have as yet been no case reports of adverse outcomes, although the number of members (2811) of a BLW web forum suggests that it is already widely used (Baby Led Weaning Forum 2010).
Given the high proportion still not self‐feeding at 6 months, it may seem unrealistic to suggest that most children could rely on self‐feeding from start of solid feeding. However, as argued above, the age when finger foods are taken depends at least partially on maternal expectations and when finger foods are actually offered. In this cohort, there was a substantial discrepancy between an apparent capacity to self‐feed and being given the opportunity to do so. Even among those children who reached out earliest and had been spontaneously reaching out for foods for 2 months, less than two‐thirds were offered finger foods more than once per day, and a quarter were described by their parents as not able to feed themselves at mealtimes. While this may genuinely reflect a lack of skill, it also suggests a low parental expectation of self‐feeding.
Our data would suggest that there might be risk in this method for children with relatively slower development. The BLW guidelines do advise against using this method in infants born preterm, or children known to be developmentally delayed. However, mild developmental delay is not usually recognized until the second year of life, and even children at the bottom of the normal range could be vulnerable if the method was applied too slavishly. Parents should probably be advised that BWL is only realistic so long as their child is reaching out for and mouthing objects by the age of 6 months.
The BLW approach also has the merit that it introduces a social and varied meal pattern at an early stage, in contrast to purees that usually require a separate meal and different food from the rest of the family. Indeed, feeding children purees is not without its problems. In the developing world, early solids are usually delivered as a puree or paste either poured into the infant's mouth or by hand feeding. There has been growing recognition that this style of feeding is commonly coercive, and that it may lead to food refusal as well as delaying the acquisition of feeding and social skills (Aboud et al. 2008; Aboud et al. 2009). It must also be born in mind that purees are of very low nutrient density, so that the small amounts taken in the early weeks after solids have started will contribute relatively little to meeting an infant's requirements. In contrast, finger foods are very nutrient dense, so a child who may appear to be eating little when self‐feeding may actually be meeting their requirements. In an observational study nested within this cohort, 15‐month‐old infants eating a finger‐fed meal took 50% longer to eat only just over half the weight of food eaten at a comparison spoonable meal, but the average energy intake at both meals was the same (Parkinson et al. 2004).
Probably the most pragmatic approach would be to adopt what is good about BLW without going to extremes: promoting the use of self‐feeding of finger foods and participation at family meals at an early stage, while recognizing the need to also co‐feed with spoonable foods, at least in the early weeks.
Conclusions
Most infants in the cohort started reaching out for food and eating finger foods between the ages of 4 and 7 months, but for many children, self‐feeding was still not a routine part of their meals at the age of 8 months. BLW might be feasible for a majority of infants but could lead to nutritional problems for infants who were relatively developmentally delayed. A more pragmatic partial BLW approach would probably be the wisest option.
Source of funding
This cohort was established with funding from Henry Smith Charity and Sport Aiding Research in Kids (SPARKS).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Acknowledgements
The study would not have been possible without the invaluable support of the midwives at the Gateshead and Newcastle maternity units, the health visitors of Gateshead and the loyal participation of all the parents.
References
- Aboud F.E., Moore A.C. & Akhter S. (2008) Effectiveness of a community‐based responsive feeding programme in rural Bangladesh: a cluster randomized field trial. Maternal & Child Nutrition 4, 275–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aboud F.E., Shafique S. & Akhter S. (2009) A responsive feeding intervention increases children's self‐feeding and maternal responsiveness but not weight gain. The Journal of Nutrition 139, 1738–1743. [DOI] [PubMed] [Google Scholar]
- Baby Led Weaning Forum. (2010) Available at: http://babyledweaning.com/forum/
- Bolling K., Grant C., Hamlyn B. & Thornton A. (2007) Infant Feeding 2005. NHS Information Centre for Health and Social Care: London.
- Brown A. & Lee M. (2010) A descriptive study investigating the use and nature of baby led weaning in a UK sample of mothers. Maternal & Child Nutrition (in press). [DOI] [PMC free article] [PubMed]
- Carruth B.R. & Skinner J.D. (2002) Feeding behaviors and other motor development in healthy children (2–24 months). Journal of the American College of Nutrition 21, 88–96. [DOI] [PubMed] [Google Scholar]
- Carruth B.R., Ziegler P.J., Gordon A. & Hendricks K. (2004) Developmental milestones and self‐feeding behaviors in infants and toddlers. Journal of the American Dietetic Association 104, s51–s56. [DOI] [PubMed] [Google Scholar]
- Committee on Medical Aspects of Food (1994) Weaning and the weaning diet. Health and social subjects. Department of Health, 45. HMSO: London. [PubMed]
- Hetzner N.M., Razza R.A., Malone L.M. & Brooks‐Gunn J. (2009) Associations among feeding behaviors during infancy and child illness at two years. Maternal and Child Health Journal 13, 795–805. [DOI] [PubMed] [Google Scholar]
- Illingworth R.S. & Lister J. (1964) Critical or sensitive period with special reference to certain feeding problems in infants + children. The Journal of Pediatrics 65, 839–848. [DOI] [PubMed] [Google Scholar]
- Khan K.M., Krosch T.C., Eickhoff J.C., Sabati A.A., Brudney J., Rivard A.L. et al (2009) Achievement of feeding milestones after primary repair of long‐gap esophageal atresia. Early Human Development 85, 387–392. [DOI] [PubMed] [Google Scholar]
- Mehta K., Specker B., Bartholmey S., Giddens J. & Ho M. (1998) Trial on timing of introduction to solids and food type on infant growth. Pediatrics 102, 569–573. [DOI] [PubMed] [Google Scholar]
- Northstone K., Emmett P., Nethersole F. & ALSPAC Study Team . (2001) The effect of age of introduction to lumpy solids on foods eaten and reported feeding difficulties at 6 and 15 months. Journal of Human Nutrition and Dietetics 14, 43–54. [DOI] [PubMed] [Google Scholar]
- Parkinson K.N., Wright C.M. & Drewett R.F. (2004) Mealtime energy intake and feeding behaviour in children who fail to thrive: a population‐based case‐control study. Journal of Child Psychology and Psychiatry 45, 1030–1035. [DOI] [PubMed] [Google Scholar]
- Parkinson K.N., Pearce M.S., Dale A., Reilly J.J., Drewett R.F., Wright C.M. et al (2010) Cohort profile: the Gateshead Millennium Study. International Journal of Epidemiology doi:10.1093/ije/dyq015. [DOI] [PubMed]
- Rapley G. & Murkett T. (2008) Baby‐Led Weaning. Vermilion: London. [Google Scholar]
- World Health Organization (2002) Report of the expert consultation on the optimal duration of exclusive breastfeeding. Department of Nutrition for Health and Development and of Child and Adolescent Health and Development, World Health Organization: Geneva.
- Wright C.M., Parkinson K.N. & Drewett R.F. (2004) Why are babies weaned early? Data from a prospective population based cohort study. Archives of Disease in Childhood 89, 813–816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright C.M., Parkinson K.N. & Drewett R.F. (2006) The influence of maternal socioeconomic and emotional factors on infant weight gain and weight faltering (failure to thrive): data from a prospective birth cohort. Archives of Disease in Childhood 91, 312–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright C.M., Stone D. & Parkinson K.N. (2010) Undernutrition in British Haredi infants within the Gateshead Millennium Cohort Study. Archives of Disease in Childhood 95, 630–633. [DOI] [PubMed] [Google Scholar]


