Abstract
The objective of this study was to review how accurately micronutrient intakes in infants, children, and adolescents were assessed with validated food frequency questionnaires (FFQs) to which study quality criteria had been applied. The methodology and the analysis presented were based on several research activities carried out within the European Micronutrient Recommendation Aligned Network of Excellence. The analysis was limited to vitamin D, vitamin C, vitamin B12, folate, selenium, iron, zinc, iodine, calcium, and copper. A search strategy was defined in MEDLINE and EMBASE literature for studies validating FFQs that estimated intakes of micronutrients being evaluated. Identification of at least three validation studies per micronutrient was required to be included in the analysis. A total score for each nutrient was calculated from the mean of the correlation coefficients weighted by the quality of the study, which included a quality score that was based on sample size, statistics used, data collection procedure, consideration of seasonality and supplement use, an adjustment/weighting of the correlation coefficient according to the quality score, and a rating of the adjusted/weighted correlation. When the mean weighted correlation coefficient was equal to or higher than 0.5, micronutrient intake was considered as adequately estimated. Sufficient validation studies were identified for vitamin C, vitamin D, vitamin B12, iron, zinc, and calcium for infants and pre‐school children, and vitamin C, calcium, and iron for older children and adolescents. Results showed that the FFQ was a good instrument for estimating intake of vitamin C, vitamin D, calcium, zinc and iron in infants and pre‐school children, and for estimating calcium and vitamin C in children and adolescents.
Keywords: EURRECA, food frequency questionnaire, validity, infants, children, adolescents
Introduction
The study of the relationship between diet and health relies on the estimation of energy and nutrient intakes in a given population. The assessment of food intake is challenging and prone to reporting errors, especially among the population groups of infants, children, and adolescents (Livingstone et al. 2004; Ortiz‐Andrellucchi et al. 2009). Certain aspects linked to the characteristics of the population group assessed (cognitive aspects, intake patterns, etc.) and to methodological issues (validity of the method, food composition table used, estimation of supplement use, etc.) constitute factors to consider when evaluating nutrient intake. To overcome these hurdles, it is critical to choose the best dietary intake method available for estimating food and nutrient intake. The selection of a method previously validated for the population and the nutrients under study is essential. The absence of a gold standard to use as the reference when validating methods to estimate food intake necessitates the use of other existing methods of dietary assessment to conduct calibration or correlation studies. Regarding biomarkers, they are considered as good indicators of intake, but only for those nutrients where a recovery marker is available and also when the temporal correlation between intake and biomarker measurements is taken into account (Willett & Hu 2006). This is essential considering that the FFQ may assess the diet of the previous year or a longer period of time. When conducting validation studies, apart from showing results that compare the data obtained by both methods (estimated intake and the intake measured by the reference method), a further analysis of other aspects of the study methodology such as the selection of the subjects, sequence and spacing of the study, the sample size, statistics used for comparison, etc., will contribute to the rigour of the results obtained (Serra‐Majem et al. 2009).
When the aim of the study is to estimate the risk of inadequacy in a given population, an estimation of long‐term average intake is needed to attenuate the intraindividual variability (Carriquiry 1999). Irrespective of the method used to estimate food intake in the population, all dietary methods should be validated using a reference dietary method or a biomarker that has been selected according to the study objectives. When using diet recalls or registers, an appropriate number of repeated recalls and records on each stratum of the population group will allow the estimation of usual intake by applying statistical methods (Hoffmann et al. 2002). In the case of food frequency questionnaire (FFQ) administration, the validation of the method will compensate for the likely overestimation of usual intake by this instrument (Sempos 1992; Liu 1994; Carroll et al. 1996; Serdula et al. 2001).
The purpose of this study was to review which micronutrients were more accurately assessed with an FFQ in infants, children, and adolescents based on the results of an in‐depth review of the validation studies conducted in these population groups, taking into account the quality of the studies included. The methodology applied and the results shown are based on the results obtained from research carried out as part of the European Micronutrient Recommendation Aligned (EURRECA) Network of Excellence (Ortiz‐Andrellucchi et al. 2009; Serra‐Majem et al. 2009).
Key messages
-
•
Assessment of food intake is challenging and prone to reporting errors, especially among infants, children, and adolescents.
-
•
The FFQ is a suitable tool to assess vitamin C, vitamin D, calcium, zinc and iron intake in infants and pre‐school children, and for estimating calcium and vitamin C in children and adolescents.
-
•
More research is needed to assess specific concerns related to FFQ validation in infants, pre‐schoolers,children, and adolescents, particularly with regard to irregular patterns of intake (small portions, snacking) that is prevalent in these population groups.
Materials and methods
A search was conducted within the context of the EURRECA Network of Excellence focusing on studies conducted to validate methods assessing micronutrient intake specifically in infants, children and adolescents published up to June 2008. The search strategy and inclusion and exclusion criteria have been previously explained (Ortiz‐Andrellucchi et al. 2009). In brief, three search stages were applied, the first one consisting of the identification of articles in MEDLINE and EMBASE using MeSH terms (nutritional assessment, diet, nutritional status, dietary intake, food intake, validity, validation study, reproducibility, replication study, correlation coefficient, and correlation study) and keywords [infants (1–23 months), pre‐school child (2–5 years), children (6–12 years), adolescents (13–18 years), dietary assessment, dietary intake, nutrition assessment, diet quality, reliability, reproducibility, validit* and correlate*]. The second stage comprised the evaluation of titles and abstracts by two independent reviewers, applying specific exclusion criteria (studies describing the content of foods in nutrients, additives, or contaminants; studies exclusively focused on diseased or institutionalized persons; articles presenting reference values for food consumption, nutrient intake, biochemical markers and anthropometric measurements; articles establishing associations between food consumption, nutrient intake, biological variables, biochemical markers, and anthropometric measurements; studies relating diseases to food consumption or nutrient intake; intervention studies and other therapeutic studies with nutrients or drugs related to the metabolism of these nutrients; calibration studies and those discussing statistical methods; studies evaluating the physiological effects of foods and nutrients and in relation to their genetic determinants; studies in animals; and studies written in other languages than English, Spanish, French, Italian, Portuguese, and German and those without abstract). At stage 3, studies selected from stage 2 that fulfilled the inclusion criteria (i.e. population group) were analysed for relevance to the research question (‘is the FFQ reliable for the assessment of micronutrient intake in infants, children and adolescents?’). The population groups defined for the analysis were infants and pre‐school children (1 month to 5 years), and children and adolescents (6–18 years). The selected studies were then classified into three different categories according to the reference method used for comparison: (1) short‐term intake methods [repeated 24‐h dietary recall (24HR), estimated dietary records, and weighted dietary records for less than 7 days of registration]; (2) long‐term intake methods (7 days or more of registered intake); and (3) the use of biomarkers as the reference method.
Moreover, the different studies selected were evaluated according to a quality scoring system that was developed following a EURRECA consensus‐based methodology (Serra‐Majem et al. 2009), which took into account the study sample (homogeneity and sample size), statistics applied to assess validity (comparisons between methods' means, medians or difference; type of correlation coefficient used: crude, energy adjusted, deattenuated or intraclass; statistics to assess agreement or misclassification), data collection (personal interview), consideration of seasonality and the evaluation of supplement intake. The possible quality scores obtained ranged from 0.5 to 7.0. The correlation coefficient for the relative validity of micronutrient intake estimates from each study was multiplied by its quality score. The sum of the weighted correlations was then divided by the sum of the quality scores for the group of studies assessing each micronutrient, thus obtaining the mean quality‐weighted correlation coefficient. The analysis was conducted for the EURRECA micronutrients of interest (vitamin D, vitamin C, vitamin B12, folate, selenium, iron, zinc, iodine, calcium, and copper). In addition, the analysis was limited to those micronutrients for which at least three validation studies were available for every population group and time category analysed. The intake method was rated as ‘good’ when the mean correlation coefficient weighted by the quality criteria score was at least 0.5.
Results
The search strategy identified 9085 articles. After applying the selection criteria by reading the title and abstract, 141 articles were selected. Further examination of full papers permitted a final selection of 26 articles.
Table 1 shows the number of studies identified for each of the EURRECA priority vitamins and minerals for infants and pre‐school children, children, and adolescent population groups. For the infant and pre‐school children population group, the vitamins and minerals with sufficient identified studies to be included in the analysis were vitamin B12 (Blum et al. 1999; 2008a, 2008b), vitamin C (Blum et al. 1999; Williams & Innis 2005; 2008a, 2008b), vitamin D (Marshall et al. 2003; 2008a, 2008b), iron (Blum et al. 1999; Williams & Innis 2005; 2008a, 2008b), zinc (Blum et al. 1999; 2008a, 2008b), and calcium (Stein et al. 1992; Taylor & Goulding 1998; Blum et al. 1999; Marshall et al. 2003; Williams & Innis 2005; Huybrechts et al. 2006; 2008a, 2008b), and in which short‐term intakes constituted the validation reference time category. The number of studies using a long‐term intake method as the reference (two studies identified for vitamins C and D, iron, and calcium) or using a biomarker (one study identified for vitamins C and D and iron) as a reference to validate that the FFQ was not sufficient to be included in the analysis (2003, 2004; Parrish et al. 2003; Williams & Innis 2005). In addition, no studies were identified for folate and copper. The articles identified had a calculated quality score ranging from 2.5 to 3.5 for vitamin B12, from 2.5 to 5 for vitamin C, from 3.5 to 4 for vitamin D, from 2.5 to 5 for iron, from 2.5 to 3.5 for zinc, and from 2.5 to 5.5 for calcium.
Table 1.
Characteristics and calculated quality score of the studies identified
| Author/year pub/country | Age group (n) | FFQ characteristics | Reference method | Micronutrient | Quality score | Study correlation coefficient |
|---|---|---|---|---|---|---|
| Blum et al. 1999, USA | 1–5 years (233) | Past 4‐week intakes; 84 food items + 19 items on supplements, food habits. Completed by the child's parent or guardian (self‐administered). Mean of two FFQs 1 month apart. | 3 × 24HR at 7–10‐day intervals between 1st and 2nd FFQ. Two recalls on weekdays and one recall on weekend. Interviewer‐administered by telephone or in person. | vit C, vit B12, Ca, Zn, Fe | 2.5 | vit C (0.58); vit B12 (0.47); Ca (0.6); Fe (0.51); Zn (0.31) |
| Marriott et al. 2008a, UK | 6 months (50) | Previous 7‐day intake; 34 items (including 10 categories of commercial baby foods). Portion size estimated using household measures. Interviewer‐administered | 4‐day WDR (within 15 days following FFQ completion). For breast‐fed infants, the length of each feeding was recorded. | vit D, vit B12, vit C, Ca, Fe, Zn | 3.5 | Energy adjusted: vit D (0.83); vit B12 (0.74); vit C (0.67); Ca (0.78); Fe (0.78); Zn (0.83) |
| Marriott et al. 2008b, UK | 12 months (50) | Previous 28‐day intake; 78 items. Portion size estimated using household measures. Interviewer‐administered. | 4‐day WDR (within 15 days following FFQ completion) | vit D, vit B12, vit C, Ca, Fe, Zn | 3.5 | Energy adjusted: vit D (0.4); vit B12 (0.24); vit C (0.47); Ca (0.61); Fe (0.50); Zn (0.48) |
| Marshall et al. 2003, USA | 6–12 months, 3–5 years (240) | Quantitative beverage FQ; self‐administered. Seven food items or groups described. Intakes in preceding week: at 6 and 12 months, parents reported average daily intake; at 3 and 5 years, average number of servings per week and usual serving size for each beverage | 3‐day WDR (two weekdays and one weekend day); intakes from food and beverages (reported here) as well as beverages only (similar results) analysed | vit D, Ca | 4 | 6 months: vit D (0.80, P < 0.001); Ca (0.64, P < 0.001); 12 months: vit D (0.60, P < 0.001); Ca (0.67, P < 0.001); 3 years: vit D (0.74, P < 0.001); Ca (0.74, P < 0.001); 5 years: vit D (0.63, P < 0.001); Ca (0.64, P < 0.001) |
| Stein et al. 1992, USA | 44–60 months (224) | Past 6‐month intake. Completed by the child's parent. Mean of two FFQs completed at 6‐month intervals. Reference portion sizes adapted for children. Interviewer‐administered. | 4 × 24HR Interviewer‐administered prior to each FFQ. 3D food models | Ca | 5.5 | Adjusted for energy (male 0.54, female 0.47); adjusted for energy intake and intraindividual variability (male 0.65, female 0.57) |
| Taylor & Goulding 1998, New Zealand | 3–6 years (41 female; 26 male) | Past 12‐month intake; 35 food and drink items | 4‐day EDR | Ca | 2.5 | 0.52 |
| Williams & Innis 2005, Canada | 8–26 months (148) | Previous 2‐week intake; 191 foods. Include supplements. Interviewer‐administered. | (i) 3‐day EDR (three consecutive weekdays and one weekend day). Household measuring utensils provided. Completed 1 week before food records. (ii) Biomarkers: serum markers of iron status (ferritin, haemoglobin) | vit C, Ca, Fe | 5 | vit C (0.64); Ca (0.75); Fe (0.64) |
| Andersen et al. 1995, Norway | 17–18 years (49) | Past 12‐month intake; 190 food items. Portion size in household measures, variable portion sizes included. | 7‐day WDR; four consecutive days, 1‐week interval and three consecutive days (five week days and two weekend days). Completed 2–3 months after FFQ. | vit C | 3 | Energy adjusted (0.37) |
| Arnold et al. 1995, Canada | 7–12 years (707 female) | Intakes in past year; 160 food items. Standard reference portions. Interviewers reviewed responses. | 2 × 7‐day EDR | vit C | 3.5 | 0.57 |
| Bellùet al. 1995, Italy | 9–12 years (49 female; 39 male) | 116 food items. Reference portion sizes Self‐administered | 7d EDR; 3D‐ food models. Completed after FFQ | vit C | 3.5 | raw nutrient 0.45; nutrient density 0.53 |
| Field et al. 1999, USA | 4th to 7th grade students (109) | Past 12‐month intake; 97 food items, standard reference portions used. Self‐administered. | 4 × 24HR (non‐consecutive days approximately 3 months apart) Interviewer‐administered prior to FFQ. Portion size in household measures or using colour photographs. | vit C, Ca, Fe | 4 | vit C (crude 0.19, deattenuated 0.32); Ca (crude 0.27, deattenuated 0.39); Fe (crude 0.20, deattenuated 0.28) |
| Harnack et al. 2006, USA | 11–14 years (248) | Past month's intake; 10 items. Portion size alternatives included. Self‐administered. | 3 × 24HR by phone subsequent to FFQ. 2D food model; visual aids mailed | Ca | 2.5 | 11–12 years (ICC: 0.52); 14–18 years (ICC: 0.57) |
| Jenner et al. 1989, Australia | 11–12 years (225) | Previous 7‐day intake; 175 items. Meal‐based reporting. Six frequency categories. No portions on FFQ (average portions from records applied). Administered separately to (i) children and (ii) parents. A subset of the first one to three diet records were also used as an alternative intake estimate. | 14 × 24HR completed over 3‐month period after FFQ. | Ca | 3.5 | FFQ completed by children (0.20). FFQ completed by parents (0.31). |
| Lietz et al. 2002, UK | 11–13 years (n = 50, biomarker n = 27) | Past 12‐month intake; 130 items. Nine frequency categories. Standard reference portions used. Interviewer‐administered. | 7‐day WDR. After FFQ. Food photographs. | Ca | 3.5 | Energy adjusted: 0.47 (P < 0.01) |
| Mølgaard et al. 1998, Denmark | 13–14 years (23) | Past 1‐month intake; 88 food items. Portion size in household measures. Self‐administered together with their parents | 3‐day WDR completed after FFQ, Two weekdays, one weekend day. | Ca | 2 | 0.62 |
| Moore et al. 2007, Canada | 9–12 years and 14–16 years (162 male) | 32 items. Included supplements. Visual aids to approximate portion size. Interviewer‐administered. | Single 24HR | Ca | 4.5 | 9–12 years (ICC: 0.46); 14–16 years (ICC: 0.43) |
| Magkos et al. 2006, Greece | 11.9 years (189 female; 162 male) | Past 12‐month intake; 30‐item; self‐administered. Standard reference portions. | Single multipass 24HR. Interviewer‐administered subsequent to FFQ. Standard household measures. | Ca | 3 | 0.63 (P < 0.001) |
| Rockett et al. 1997, USA | 9–18 years (261) | Past 12‐month intake; 131 items; standard reference portions. Mean of two questionnaires administered approximately 1.5 years apart. Self‐administered. | 3 × 24HR at approximately 5‐month intervals, with detailed probing. Administered between 1st and 2nd FFQ. | vit C, Ca, Fe | 3.5 | 9–13 years vit C (0.61); Ca (0.52); Fe (0.47); 14–18 years: vit C (0.45); Ca (0.57); Fe (0.59) |
| Slater et al. 2003, Brazil | 14–18 years (79) | Past 6‐month intake; 76 food items. Single reference portion sizes listed. Use of interviewers not reported. | 3 × 24HR. At intervals of 45 days prior to FFQ administration | vit C, Ca, Fe | 4 | Energy adjusted: vit C (0.47; P < 0.01); Ca (0.51, P < 0.01); Fe (0.17) |
FFQ, food frequency questionnaire; WDR, weighed dietary record; EDR, estimated dietary record; 24HR, 24‐h diet recalls; DH, diet history; vit, vitamin; ICC, intraclass coefficient; 3D, three‐dimensional; 2D, two‐dimensional.
For the children and adolescent population group, the vitamins and minerals with a sufficient number of studies to be included in the analysis were vitamin C (Andersen et al. 1995; Arnold et al. 1995; Bellùet al. 1995; Rockett et al. 1997; Field et al. 1999; Slater et al. 2003) and calcium (Jenner et al. 1989; Rockett et al. 1997; Mølgaard et al. 1998; Taylor & Goulding 1998; Field et al. 1999; Slater et al. 2003; Harnack et al. 2006; Magkos et al. 2006; Moore et al. 2007) for both short‐ and long‐term reference methods used as comparison and iron for the short‐term intake reference method (Rockett et al. 1997; Field et al. 1999; Slater et al. 2003). For vitamin B12, folate, vitamin D, zinc, and copper, only one study for each micronutrient was identified in the children and adolescent population group (Andersen et al. 1995; Rockett et al. 1997). In the same population group, only one study using biomarkers of intake as a reference was identified for validating intakes of vitamin B12, vitamin C and folate (Byers et al. 1993; Green et al. 1998). No studies were identified for iodine and selenium in either population group. The quality score for the articles identified ranged from 3.0 to 4.0 for vitamin C, from 3.5 to 4.0 for iron, and from 2.5 to 4.5 for calcium.
Table 2 shows the EURRECA micronutrients that were adequately estimated by an FFQ. The mean correlation coefficient weighted by the quality score was 0.48 for vitamin B12, 0.6 for vitamin C, 0.62 for vitamin D, 0.62 for iron, 0.56 for zinc, and 0.65 for calcium in the infant and pre‐school children group and for the short‐term comparison methods. In the older population group, the results were as follows: for the short‐term dietary intake reference method, 0.61 for vitamin C, 0.51 for calcium and 0.38 for iron; for the long‐term dietary intake reference method, 0.5 for vitamin C, 0.47 for calcium and 0.37 for iron.
Table 2.
Mean of correlation coefficients weighted by the quality score for the FFQ validation studies per EURRECA micronutrients and population group analysed
| Nutrient | Infants and pre‐school children | Children and adolescents | ||||
|---|---|---|---|---|---|---|
| Short‐term intake (<7 days) | Long‐term intake (≥7 days) | Biomarkers | Short‐term Intake (<7 days) | Long‐term intake (≥7 days) | Biomarkers | |
| Vit B12 | 0.48 (3 studies) | NA | NA | NA | NA | NA |
| Folate | NA | NA | NA | NA | NA | NA |
| Vit C | 0.60 (4 studies) | NA | NA | 0.61 (3 studies) | 0.50 (3 studies) | NA |
| Vit D | 0.62 (3 studies) | NA | NA | NA | NA | NA |
| Calcium | 0.65 (8 studies) | NA | NA | 0.51 (8 studies) | 0.47 (5 studies) | NA |
| Iron | 0.62 (4 studies) | NA | NA | 0.38 (3 studies) | NA | NA |
| Zinc | 0.56 (3 studies) | NA | NA | NA | NA | NA |
| Copper | NA | NA | NA | NA | NA | NA |
FFQ, food frequency questionnaire; EURRECA, European Micronutrient Recommendation Aligned; vit, vitamin; NA, not available, less than three studies found.
1, 2 show the mean correlation coefficients weighted by the study quality score for the EURRECA top 10 vitamins and minerals for infant/pre‐schoolers and children/adolescents population groups. The results for the infant/pre‐schoolers group (Fig. 1) showed that the micronutrients with a mean weighted correlation coefficient of at least 0.50 were as follows: vitamin D (0.62), vitamin C (0.6), calcium (0.65), zinc (0.56), and iron (0.62) when using a short‐term reference method to validate the FFQ. For the children/adolescents population group (Fig. 2), calcium (0.51) had a good mean weighted correlation coefficient for the studies validating the FFQ against short‐term intake methods, but not for those comparing the FFQ against long‐term intake methods. Vitamin C had good mean weighted correlation coefficients for studies evaluating the validity of the FFQ compared with short‐term (0.61) and long‐term (0.5) intake methods. When using short‐term intake methods, the mean correlation coefficient weighted by the study quality score for iron was below 0.50.
Figure 1.
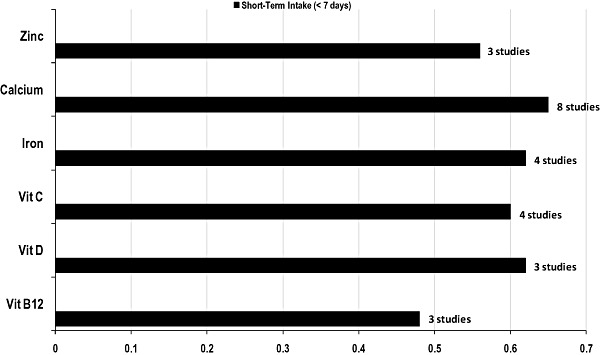
Mean of correlation coefficients weighted by the study quality score for infants and pre‐school children. Mean of correlation coefficients weighted by the study quality score (Serra‐Majem et al. 2009).
Figure 2.
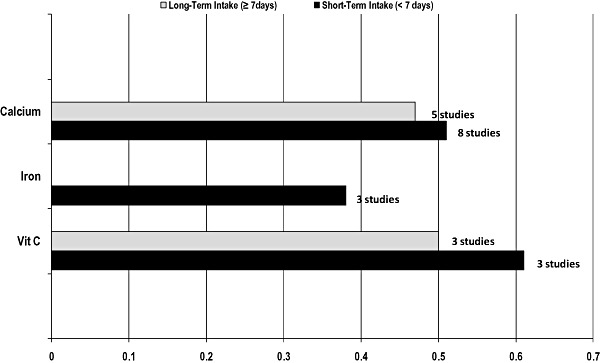
Mean of correlation coefficients weighted by study quality score for children and adolescents. Mean of correlation coefficients weighted by the study quality score (Serra‐Majem et al. 2009).
Discussion
The FFQ was shown to be adequate for estimating intakes for a number of EURRECA micronutrients. In the population group of infants and pre‐school children, FFQs yielded adequate assessments for vitamin C, vitamin D, calcium, zinc and iron, but marginally inadequate assessments for vitamin B12. In the children and adolescent population group, assessments based on FFQs were adequate for calcium and vitamin C, but not for iron. There was not enough information to draw conclusions regarding the validity of intake assessments based on FFQs for folate, copper, iodine, and selenium in the population group of infants and pre‐school children, or for vitamin D, vitamin B12, folate, zinc, copper, iodine, and selenium in the children and adolescent population group. This analysis not only took into account the correlation coefficients obtained, but also certain aspects of the methodology that should be addressed when validating FFQs: adequate sample size, seasonality, data collection methodology such as the use of interviewers vs. self‐administered questionnaires, inclusion of supplement use, and whether the statistics applied for validating the method adjusted for factors such as energy intakes. Pooled correlation coefficients were weighted to account for these factors, giving higher weight to studies with superior methodology (Serra‐Majem et al. 2009). The results of relative validation studies comparing FFQs with estimates based on repeated 24‐h recalls or food diaries suggest that carefully designed and validated FFQs may be adequate for estimating intakes of several important micronutrients in children of different ages. The importance of ensuring that FFQs have been adequately validated has received substantial attention in recent publications. This arose as a consequence of several studies reporting significant diet–disease relationships based on intakes estimated with food diaries or biomarkers, but not using FFQs (2003, 2008; Freedman et al. 2006). Most of these studies have focused on dietary fats, and several studies suggest that bias in FFQ‐based reporting may be particularly acute for fat intakes, in comparison with protein and micronutrients such as potassium (Heitmann & Lissner 1995; Heerstrass et al. 1998; Subar et al. 2003). However, a recent study reported associations between ischemic heart disease and biomarker‐ or diary‐based (but not FFQ‐evaluated) intake estimates of vitamin C and fruits and vegetables, raising concern about poor micronutrient intake estimation using FFQs (Bingham et al. 2008). Further study is needed to better understand how FFQ‐based estimates of micronutrients perform relative to diaries, recalls and biomarkers in studies targeting both adults and children.
The lack of sufficient data to assess the ability of the FFQ to provide valid intake estimates for many of the micronutrients of interest is an issue of concern. Very few studies provided data on the majority of EURRECA priority nutrients: a minimum of three studies were available for only 6 of the 10 priority nutrients in children under 5 years, and data were available for only three of these nutrients in older children (1, 2). Very few of these validation studies in children incorporated biomarkers, which may provide an objective measure of intakes for some nutrients, reducing the problem of correlated errors when the reference method is also based on self‐reports (Day et al. 2004). However, it is worth qualifying again that the problem of correlated errors seems to be greater for dietary fat than for micronutrients such as vitamin C (Day et al. 2004).
Regardless of the ability of FFQ‐based estimates to rank subjects according to levels of intake, the validity of FFQs for estimating absolute intakes and the prevalence of inadequacy remains an important and separate concern (Román‐Viñas et al. 2009). As shown in several studies, there may be substantial disparities in absolute estimates of intakes based on FFQs vs. other instruments despite high correlations indicating adequate ability for ranking intakes (Lietz et al. 2002). For example, intakes of dietary fat and calcium based on weighed diet records were 76.5 g and 813 mg, respectively, differing substantially from the FFQ estimates of 98.0 g (28% lower) and 1016 mg (25% higher) (Freedman et al. 2006).
Conclusions
The FFQ is a suitable tool to assess nutrient intake adequacy for the following EURRECA micronutrients: vitamin C, vitamin D, calcium, zinc and iron. More research is needed to assess specific concerns related to FFQ validation in infants, pre‐schoolers, children, and adolescents, such as portion size estimation, irregular pattern of intake (small portions, snacking), probing questions for specific input, and the usefulness of new technologies such as computer‐assisted interviews to enhance data collection and address problems such as the cost of collecting and processing data using methods such as 24‐h recalls or diaries (Van Horn et al. 1990; Vereecken et al. 2005. This is especially relevant given the irregular pattern of intake (small portions, snacking, etc.) in these population groups. Sufficient evidence is lacking to evaluate the validity of the FFQ for assessing intake adequacy of vitamin B12, folate, selenium, iodine, and copper in these population groups.
Source of funding
The work reported here has been carried out within the EURRECA Network of Excellence (http://www.eurreca.org) that is financially supported by the Commission of the European Communities, specific Research Technology and Development (RTD) Programme Quality of Life and Management of Living Resources, within the Sixth Framework Programme, contract no. 036196. This report does not necessarily reflect the Commission's views or its future policy in this area.
Conflict of interest
The authors declare no conflict of interest.
Acknowledgements
English editing support provided by Joy Ngo, RD, is gratefully acknowledged.
References
- Andersen L.F., Nes M., Lillegaard I.T., Sandstad B., Bjørnebow G.E. & Drevon C.A. (1995) Evaluation of a quantitative food frequency questionnaire used in a group of Norwegian adolescents. European Journal of Clinical Nutrition 49, 543–554. [PubMed] [Google Scholar]
- Andersen L.F., Lande B., Arsky G.H. & Trygg K. (2003) Validation of a semi‐quantitative food‐frequency questionnaire used among 12‐month‐old Norwegian infants. European Journal of Clinical Nutrition 57, 881–888. [DOI] [PubMed] [Google Scholar]
- Andersen L.F., Lande B., Trygg K. & Hay G. (2004) Validation of a semi‐quantitative food‐frequency questionnaire used among 2‐year‐old Norwegian children. Public Health Nutrition 7, 757–764. [DOI] [PubMed] [Google Scholar]
- Arnold J.E., Rohan T., Howe G. & Leblanc M. (1995) Reproducibility and validity of a food‐frequency questionnaire designed for use in girls age 7 to 12 years. Annals of Epidemiology 5, 369–377. [DOI] [PubMed] [Google Scholar]
- Bellù R., Ortisi M.T., Riva E., Banderalli M.D., Cuccome M.D., Giovannini M.M.D. et al (1995) Validity assessment of a food frequency questionnaire for school‐age children in Northern Italy. Nutrition Research 15, 1121–1128. [Google Scholar]
- Bingham S.A., Luben R., Welch A., Wareham N., Khaw K.T. & Day N. (2003) Are imprecise methods obscuring a relation between fat and breast cancer? Lancet 362, 212–214. [DOI] [PubMed] [Google Scholar]
- Bingham S., Luben R., Welch A., Low Y.L., Khaw K.T., Wareham N. & Day N. (2008) Associations between dietary methods and biomarkers, and between fruits and vegetables and risk of ischaemic heart disease, in the EPIC Norfolk Cohort Study. International Journal of Epidemiology 37, 978–987. [DOI] [PubMed] [Google Scholar]
- Blum R.E., Wei E.K., Rockett H.R., Langeliers J.D., Leppert J., Gardner J.D. et al (1999) Validation of a food frequency questionnaire in Native American and Caucasian children 1 to 5 years of age. Maternal and Child Health Journal 3, 167–172. [DOI] [PubMed] [Google Scholar]
- Byers T., Trieber F., Gunter E., Coates R., Sowell A., Leonard S. et al (1993) The accuracy of parental reports of their children's intake of fruits and vegetables: validation of a food frequency questionnaire with serum levels of carotenoids and vitamins C, A, and E. Epidemiology 4, 350–355. [PubMed] [Google Scholar]
- Carriquiry A.L. (1999) Assessing the prevalence of Nutrient inadequacy. Public Health Nutrition 2, 23–33. [DOI] [PubMed] [Google Scholar]
- Carroll R.J., Freedman L.S. & Hartman A.M. (1996) Use of semiquantitative food frequency questionnaires to estimate the distribution of usual intake. The American Journal of Epidemiology 143, 392–404. [DOI] [PubMed] [Google Scholar]
- Day N.E., Wong M.Y., Bingham S., Khaw K.T., Luben R., Michels K.B. et al (2004) Correlated measurement error – implications for nutritional epidemiology. International Journal of Epidemiology 33, 1373–1381. [DOI] [PubMed] [Google Scholar]
- Field A.E., Peterson K.E., Gortmaker S.L., Cheung L., Rockett H., Fox M.K. et al (1999) Reproducibility and validity of a food frequency questionnaire among fourth to seventh grade inner‐city school children: implications of age and day‐to‐day variation in dietary intake. Public Health Nutrition 2, 293–300. [DOI] [PubMed] [Google Scholar]
- Freedman L.S., Potischman N., Kipnis V., Midthune D., Schutzkin A., Thompson F.E. et al (2006) A comparison of two dietary instruments for evaluating the fat‐breast cancer relationship. International Journal of Epidemiology 35, 1011–1021. [DOI] [PubMed] [Google Scholar]
- Green T.J., Allen O.B. & O'Connor D.L. (1998) A three‐day weighed food record and a semiquantitative food‐frequency questionnaire are valid measures for assessing the folate and vitamin B‐12 intakes of women aged 16 to 19 years. The Journal of Nutrition 128, 1665–1671. [DOI] [PubMed] [Google Scholar]
- Harnack L.J., Lytle L.A., Story M., Galuska D.A., Schmitz K., Jacobs D.R. Jr. et al (2006) Reliability and validity of a brief questionnaire to assess calcium intake of middle‐school‐aged children. Journal of the American Dietetic Association 106, 1790–1795. [DOI] [PubMed] [Google Scholar]
- Heerstrass D.W., Ocké M.C., Bueno‐de‐Mesquita H.B., Peeters P.H. & Seidell J.C. (1998) Underreporting of energy, protein and potassium intake in relation to body mass index. International Journal of Epidemiology 27, 186–193. [DOI] [PubMed] [Google Scholar]
- Heitmann B.L. & Lissner L. (1995) Dietary underreporting by obese individuals – is it specific or non‐specific? British Medical Journal 311, 986–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann K., Boeing H., Dufour A., Volatier J.L., Telman J., Virtanes M. et al (2002) Estimating the distribution of usual dietary intake by short‐term measurements. European Journal of Clinical Nutrition 56 (Suppl. 2), S53–S62. [DOI] [PubMed] [Google Scholar]
- Huybrechts I., De Bacquer D., Matthys C., De Bacquer G. & De Henauw S. (2006) Validity and reproducibility of a semi‐quantitative food‐frequency questionnaire for estimating calcium intake in Belgian preschool children. The British Journal of Nutrition 95, 802–816. [DOI] [PubMed] [Google Scholar]
- Jenner D.A., Neylon K., Croft S., Beilin L.J. & Vandongen R. (1989) A comparison of methods of dietary assessment in Australian children aged 11–12 years. European Journal of Clinical Nutrition 43, 663–673. [PubMed] [Google Scholar]
- Lietz G., Barton K.L., Longbottom P.J. & Anderson A.S. (2002) Can the EPIC food‐frequency questionnaire be used in adolescent populations? Public Health Nutrition 5, 783–789. [DOI] [PubMed] [Google Scholar]
- Liu K. (1994) Statistical issues related to semiquantitative foodfrequency questionnaires. The American Journal of Clinical Nutrition 59 (Suppl.), S262–S265. [DOI] [PubMed] [Google Scholar]
- Livingstone M.B., Robson P.J. & Wallace J.M. (2004) Issues in dietary intake assessment of children and adolescents. The British Journal of Nutrition 92 (Suppl. 2), S213–S222. [DOI] [PubMed] [Google Scholar]
- Magkos F., Manios Y., Babaroutsi E. et al (2006) Development and validation of a food frequency questionnaire for assessing dietary calcium intake in the general population. Osteoporosis International 17, 304–312. [DOI] [PubMed] [Google Scholar]
- Marriott L.D., Robinson S.M., Poole J. et al (2008a) What do babies eat? Evaluation of a food frequency questionnaire to assess the diets of infants aged 6 months. Public Health Nutrition 11, 751–756. [DOI] [PubMed] [Google Scholar]
- Marriott L.D., Inskip H.M., Borland S.E. et al (2008b) What do babies eat? Evaluation of a food frequency questionnaire to assess the diets of infants aged 12 months. Public Health Nutrition 12, 967–972. [DOI] [PubMed] [Google Scholar]
- Marshall T.A., Eichenberger Gilmore J.M., Broffitt B. et al (2003) Relative validation of a beverage frequency questionnaire in children ages 6 months through 5 years using 3‐day food and beverage diaries. Journal of the American Dietetic Association 103, 714–720. [DOI] [PubMed] [Google Scholar]
- Mølgaard C., Sandström B. & Michaelsen K.F. (1998) Evaluation of a food frequency questionnaire for assessing of calcium, protein and phosphorus intakes in children and adolescents. Scandinavian Journal of Nutrition 42, 2–5. [Google Scholar]
- Moore M., Braid S., Falk B. et al (2007) Daily calcium intake in male children and adolescents obtained from the rapid assessment method and the 24‐hour recall method. Nutrition Journal 6, 24–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ortiz‐Andrellucchi A., Henríquez‐Sánchez P., Sánchez‐Villegas A., Peña‐Quintana L., Mendez M. & Serra‐Majem L. (2009) Dietary Assessment Methods for microNutrient intake in infants, children and adolescents: a systematic review. The British Journal of Nutrition 102, s87–s117. [DOI] [PubMed] [Google Scholar]
- Parrish L.A., Marshall J.A., Krebs N.F. et al (2003) Validation of a food frequency questionnaire in preschool children. Epidemiology 14, 213–217. [DOI] [PubMed] [Google Scholar]
- Rockett H.R., Breitenbach M., Frazier A.L. et al (1997) Validation of a youth/adolescent food frequency questionnaire. Preventive Medicine 26, 808–816. [DOI] [PubMed] [Google Scholar]
- Román‐Viñas B., Serra‐Majem L., Ribas‐Barba L. et al (2009) Overview of methods used to evaluate the adequacy of Nutrient intakes for individuals and populations. The British Journal of Nutrition 101 (Suppl. 2), S6–S11. [DOI] [PubMed] [Google Scholar]
- Sempos C.T. (1992) Some limitations of semiquantitative food frequency questionnaires. The American Journal of Epidemiology 135, 1127–1132. [Google Scholar]
- Serdula M.K., Alexander M.P., Scanlon K.S. & Bowman B.A. (2001) What are preschool children eating? A review of dietary assessment. Annual Review of Nutrition 21, 475–498. [DOI] [PubMed] [Google Scholar]
- Serra‐Majem L., Frost Andersen L., Henríquez P. et al (2009) Evaluating the quality of dietary intake validation studies. The British Journal of Nutrition 102, s3–s9. [DOI] [PubMed] [Google Scholar]
- Slater B., Philippi S.T., Fisberg R.M. et al (2003) Validation of a semi‐quantitative adolescent food frequency questionnaire applied at a public school in São Paulo, Brazil. European Journal of Clinical Nutrition 57, 629–635. [DOI] [PubMed] [Google Scholar]
- Stein A.D., Shea S., Basch C.E. et al (1992) Consistency of the Willett semiquantitative food frequency questionnaire and 24‐hour dietary recalls in estimating Nutrient intakes of preschool children. The American Journal of Epidemiology 15, 667–677. [DOI] [PubMed] [Google Scholar]
- Subar A.F., Kipnis V., Troiano R.P. et al (2003) Using intake biomarkers to evaluate the extent of dietary misreporting in a large sample of adults: the OPEN study. The American Journal of Epidemiology 158, 1–13. [DOI] [PubMed] [Google Scholar]
- Taylor R.W. & Goulding A. (1998) Validation of a short food frequency questionnaire to assess calcium intake in children aged 3 to 6 years. European Journal of Clinical Nutrition 52, 464–465. [DOI] [PubMed] [Google Scholar]
- Van Horn L.V., Gernhofer N., Moag‐Stahlberg A. et al (1990) Dietary assessment in children using electronic methods: telephones and tape recorders. Journal of the American Dietetic Association 90, 412–416. [PubMed] [Google Scholar]
- Vereecken C.A., Covents M., Matthys C. et al (2005) Young adolescents' Nutrition assessment on computer (YANA‐C). European Journal of Clinical Nutrition 59, 658–667. [DOI] [PubMed] [Google Scholar]
- Willett W.C. & Hu F.B. (2006) Not the time to abandon the food frequency questionnaire: point. Cancer Epidemiology, Biomarkers & Prevention 15, 1757–1758. [DOI] [PubMed] [Google Scholar]
- Williams P.L. & Innis S.M. (2005) Food frequency questionnaire for assessing infant iron nutrition. Canadian Journal of Dietetic Practice and Research 66, 176–182. [DOI] [PubMed] [Google Scholar]


