Abstract
Progress towards reducing mortality and malnutrition among children <5 years of age has been less than needed to achieve related Millennium Development Goals (MDGs). Therefore, several international agencies joined to ‘Reposition children's right to adequate nutrition in the Sahel’, starting with an analysis of current activities related to infant and young child nutrition (IYCN). The main objectives of the situational analysis are to compile, analyse and interpret available information on infant and child feeding and the nutrition situation of children <2 years of age in Senegal, as one of the six targeted countries. These findings will be used to assist in identifying inconsistencies and filling gaps in current programming. Between August and December 2008, key informants responsible for conducting IYCN‐related activities in Senegal were interviewed, and 157 documents were examined on the following themes: optimal breastfeeding and complementary feeding practices, prevention of micronutrient deficiencies, prevention of mother‐to‐child transmission of HIV, management of acute malnutrition, food security and hygienic practices. Nearly all of the key IYCN topics were addressed, specifically or generally, in national policy documents. Senegal reported substantial improvements since the 1990s towards reducing infant and young child mortality and underweight, and increasing exclusive breastfeeding among infants <6 months of age (34%). Senegal is one of the few countries in the region that is nearly on track for reaching related MDGs. Notable activities that may have played a role include: (1) vitamin A supplementation was expanded to nearly semi‐annual national campaigns starting in 1994; (2) the Ministry of Health partnered with several national and international agencies to scale up child survival activities under the umbrella of the Basic Support for Institutionalizing Child Survival (1994–2006); (3) a national nutrition division was developed to support a national nutrition strengthening programme; (4) the national nutrition counsel was organized to coordinate nutritional activities across various organizations and governmental sectors, involving representatives from health, agriculture and surveillance; and (5) an integrated communications programme was developed to support harmonized behaviour change communication tools for the health and nutrition sectors. Along with these activities, a number of programme evaluations were conducted to ensure that programmes obtain desired results. Although useful, these evaluations were not rigorous enough to identify effective programmes that contributed to the mentioned reductions in the prevalence of underweight and mortality, and increases in exclusive breastfeeding. The policy and programme framework is well established for support of optimal IYCN practices in Senegal. Despite the recent improvements in infant and young child nutritional status indicators, there is still much to do. Greater resources and continued capacity building are needed to: (1) conduct necessary research for adapting training materials and programme protocols to programmatic needs; (2) improve and carry out monitoring and evaluation that identify effective programme components; and (3) apply these findings in developing, expanding and improving effective programmes.
Keywords: infant and young child nutrition, national policies, nutrition programmes, monitoring and evaluation, West Africa, Senegal
Background
Senegal covers 196 722 sq km of the west coast of Africa, surrounded by Mauritania to the north, Mali to the east, and Guinea and Guinea Bissau to the south (1), and is divided into 11 administrative regions. Among the 13.7 million inhabitants (July 2009 estimate (1)), 42% are less than 15 years of age. The gross domestic product per capita was estimated at US$1600 in 2008, with 48% unemployment rate estimated for 2007 (1). The country is mostly semi‐arid savannah. About 13% of the land mass is considered arable, with less than 1% devoted to permanent crops. Agricultural and livestock production includes peanuts, millet, corn, sorghum, rice, cotton, tomatoes, green vegetables, cattle, poultry, pigs and fish. Senegal's main exports are fish, groundnuts (peanuts), petroleum products, phosphates and cotton. Industries in Senegal include agricultural and fish processing, phosphate mining, fertilizer production, petroleum refining; iron ore, zircon and gold mining; there is also the production of construction materials, and ship construction and repair (Fig. 1).
Figure 1.
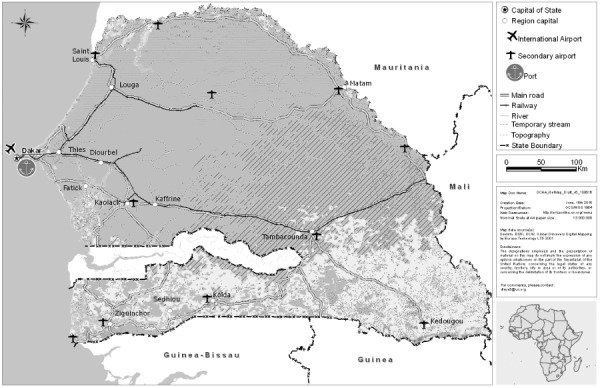
Map of Senegal. Map courtesy of United Nations Office for the Coordination of Humanitarian Affairs, Central and West Africa Regional Office.
The average rainy season in Senegal lasts from May to September. In the north, rain only falls 20–30 days of each year, with average annual rainfall of 300–350 mm. Rainfall is more frequent in the south, averaging 1000–1500 mm across an average of 60–90 days of rainfall each year (2). The short rainy season across Senegal and the low annual rainfall in the north can lead to large fluctuations in the food security situation.
The Millennium Development Goals (MDGs) most related to infant and young child nutritional status are MDG 1, Target 1.C (to halve, between 1990 and 2015, the proportion of people who suffer from hunger) and MDG 4, Target 4.A (reduce by two thirds, between 1990 and 2015, the under‐5 mortality rate). Two monitoring indicators for these MDGs that are regularly collected and reported globally are indicator 1.8 (the prevalence of underweight children under‐5 years of age) and indicator 4.1 (the under‐5 mortality rates). Senegal is on track for halving by 2015 the proportion of children <5 years that are underweight (Fig. 2a). Reductions have also been achieved in the rates of stunting among children less than 5 years of age (Fig. 2b), a measure of chronic malnutrition.
Figure 2.
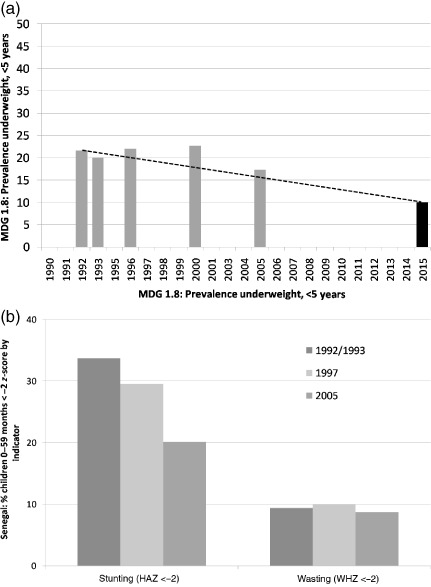
Trends in underweight compared to Millennium Development Goal (MDG) for 2015 (a), and stunting and wasting (b) in infants and children <5 years, ∼1990–2015; dotted line indicates target for MDG indicator 1.8: to reduce underweight by half between 1990 and 2015. Underweight = weight‐for‐age z‐score <‐2, HAZ = height‐for‐age z‐score; WHZ = weight‐for‐height z‐score. Data sources: WHO 2006 Child Growth Standards data from MEASURE DHS STAT compiler at http://measuredhs.com 19 February 2009. (a) 2015 goal is 1/2 of 1992 value (3).
Senegal is not quite on target for reaching MDG 4.1, to reduce mortality rates by two thirds among infants and children less than 5 years of age (Fig. 3). However, among the Sahelian countries included in this situational analysis, Senegal is the second closest to being on target, next to Niger.
Figure 3.
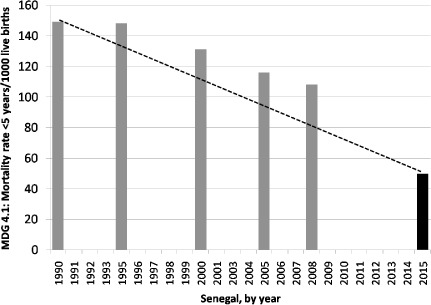
Under‐5 mortality rate, 1990 estimate; 1992/1993, 1997 and 2005 DHS; 2015 Millennium Development Goal (MDG), dotted line indicates target trajectory for MDG indicator 4.1: to reduce mortality rates by 2/3 (4). Data source http://www.childmortality.org/; 2015 goal is 1/3 of 1990 estimate.
The development and implementation of nutrition‐related activities in Senegal are positioned within a multi‐sectorial unit composed of ministries and organizations with the common goal of reducing malnutrition. This ‘Unit to combat malnutrition’ (Cellule de Lutte contre la Malnutrition – CLM) was established by a legislative decree in 2001, which places this unit under the authority of the Prime Minister (5). Participants include representatives from the Prime Minister; the President of the Republic; the Minister of Economy and Finances; the Minister of the Interior; the Minister of Education; the Minister of Social Development and National Solidarity; the Minister of Mines, Energy and Hydraulics; the Minister of Agriculture and Livestock; the Minister of Youth, the Environment and Public Hygiene; the Minister of Families and Infancy; the Minister of Technical Education, Professional Training, Literacy and National Languages; the Minister of Health and Prevention; the Minister delegate charged with Local Collectives; non‐governmental organizations; and the Association of Senegalese Mayors (5).
Since 2002, the CLM, under the leadership of the National Executive Office, has managed the Nutrition Reinforcement Program (PRN). This programme replaced a community nutrition project and focuses on improving the nutritional status of children and pregnant and lactating women, along with the development of community resources and of institutional and organizational capacities to carry out and evaluate nutrition programmes. The Food, Nutrition and Child Surveillance Division (DANSE in French) directs the programmes of the Ministry of Health, such as the packet of integrated nutrition activities (PAIN in French), which combined the minimum packet of nutrition activities, a community nutrition surveillance programme, and the Integrated Management of Childhood Illness (IMCI), which now includes community outreach.
The University Cheikh Anta Diop provides master and doctoral degrees in nutrition (6). The enrolments are currently limited to 12 students in the master's programme, and there are currently two doctoral students.
The main objectives of this situational analysis are to compile, analyse and interpret available information on infant and child feeding, and the nutrition and health situation of children <2 years of age in the six target countries (Burkina Faso, Chad, Mali, Mauritania, Niger, Senegal). Additional aims were to identify inconsistencies with international recommendations and gaps in programme activities, and to provide recommendations based on these findings to guide the development of more effective infant and young child nutrition (IYCN)‐related programmes and activities.
Methods and data collection
Between August and October 2008, the local project coordinator of this situational analysis contacted organizations known to be involved in nutrition and health‐related activities in Senegal, as identified through the Regional Food Security and Nutrition Working Group and Ministry of Health nutrition focal points. Twenty‐one organizations completed a questionnaire regarding their IYCN activities and shared 157 pertinent documents that we reviewed for inclusion in this analysis (see Supporting Information Appendices). Unfortunately, we were not able to obtain all relevant documents from agencies contacted and some activities conducted by these organizations might not have been documented in formal reports. Therefore, the analyses are limited to those documents we were able to obtain during this general time period. It would have been beyond the scope of these analyses to include all documents and activities regarding HIV, food security and hygiene. Therefore, we focused on respective activities that targeted infants and young children. We found few of these programmes with specific activities targeted at young children. Because the family's food security status has an impact on the health and nutritional status of young children, we provide a brief overview of food security tracking that is taking place in‐country.
The documents obtained include information on: (i) national policies, strategies and plans of action; (ii) research studies related to barriers and beliefs concerning IYCN‐related behaviours; (iii) other formative research; (iv) training materials, programme protocols and curricula; (v) programmes implemented, with the intended and actual programme coverage, where available; and (vi) programme monitoring and evaluation reports, including available survey results. In the following, ‘surveys’ refer to cross‐sectional data collected among a selected subset of the population. These surveys are not necessarily related to a programme or study. ‘Monitoring’ refers to studies that evaluate the implementation of a specific programme and whether it is implemented according to protocol. ‘Evaluation’ refers to findings regarding the outcomes or impact of a programme.
The topics we reviewed in these documents included: promotion of breastfeeding and complementary feeding practices, prevention of micronutrient deficiencies, management of acute malnutrition, prevention of mother‐to‐child transmission of HIV, food security and hygienic practices. The criteria for comparison, with international recommendations, are outlined in Table 1 and in the introductory chapter in this issue (7). Reported activities and gaps in information are discussed in the following sections by feeding practices or other related activities, in the order found in Table 1. Because of the number of activities and documents reviewed, we were only able to discuss the most relevant activities in this publication. Summary tables of additional activities and documents identified are listed in supplementary online tables by type of document reviewed (see Supporting Information Appendices).
Table 1.
Summary of actions documented with respect to key infant and young child feeding practices in Senegal
| Key practice* | Summarized findings by type of document reviewed, with selected national‐level findings† | |||||||
|---|---|---|---|---|---|---|---|---|
| Policies | Formative research | Protocols/training | Programmes | Intended programme coverage | Actual programme coverage | Programme monitoring | Surveys and evaluation | |
| Promotion of optimal feeding practices | ||||||||
| Timely introduction BF, 1 h | ✓ | ✓ | ✓ | ✓ | National | National | ✓(BFHI ‡ ) | 23% § |
| EBF to 6 months | ✓ | ✓ | ✓/–✓ | ✓/–✓ | National | National | (✓) | 15%, 4–5 months, 34%, <6 months ¶ |
| Continued BF to 24 months | ✓ | ✓ | ✓ | ✓ | National | National | (✓) | 42%** |
| Introduce CF at 6 months | ✓ | ✓ | ✓ | ✓ | National | Sub‐national | (✓) | 50% †† |
| Nutrient dense CF | ✓ | N/I | ✓ | ✓ | National | Sub‐national | (✓) | 23% VA‐FV 29% MFPE ‡‡ |
| Responsive feeding | N/I | N/I | ✓ | ✓ | National | Sub‐national | N/I | N/I |
| Appropriate frequency/consistency | ✓ | N/I | ✓ | ✓ | National | Sub‐national | N/I | 49% §§ |
| Dietary assessments | N/I | (FRAT ¶¶ ) | N/I | N/I | N/I | (National) ¶¶ | N/I | N/I |
| Prevention of micronutrient deficiencies | ||||||||
| Vitamin A supplements young children | ✓ | ✓ | ✓ | ✓ | National | 75%*** | (✓) | N/I |
| Post‐partum vitamin A | (✓) | N/I | ✓ | ✓ | National | 27% ††† | (✓) | 13% ‡‡‡ |
| Zinc to treat diarrhoea | ✓ | N/I | ✓ | ✓ | National | Sub‐national | (✓) | N/I |
| Prevention of zinc deficiency | N/I | N/I | N/I | N/I | N/I | N/I | N/I | N/I |
| Anaemia prevention (malaria, parasites) | ✓ | ✓ | ✓ | ✓ | National | N/I | 10% ITN §§§ 10% ITN ¶¶¶ | 83% anaemia**** |
| Anaemia prevention (iron–folic acid in pregnancy/post‐partum) | ✓ | ✓ | ✓ | ✓ | National | Sub‐national | 40% FAF †††† | 59% anaemia ‡‡‡‡ |
| Assessment of iron deficiency anaemia | N/I | N/I | N/I | N/I | N/I | N/I | N/I | N/I |
| Iodine programmes | ✓ | ✓ | ✓ | ✓ | National | N/I | 35% §§§§ 23% ¶¶¶¶ | N/I |
| Other nutrition support | ||||||||
| Management of malnutrition | ✓ | ✓ | ✓ | ✓ | National | Sub‐national | ✓ | 9% WHZ 15% WAZ 20% HAZ***** |
| Prevention MTCT HIV/AFASS | (✓) | (✓) | ✓ | ✓ | National | Sub‐national | ✓ ††††† , (8) 61% ‡‡‡‡‡ | (✓) §§§§§ , (9) |
| Food security | ✓ | N/I | N/I | N/I | vulnerable | vulnerable | (✓) | ✓/VAM |
| Hygiene and food safety | ✓ | N/I | ✓ | ✓ | National | Sub‐national | 77% ¶¶¶¶¶ | |
| Related tasks | ||||||||
| IEC/BCC in programmes† | ✓ | N/I | ✓ | ✓ | National | Sub‐national | 62%******, (10) | N/I |
EXPLANATION OF TABLE HEADERS AND MARKINGS:
✓ Confirmed documentation of actions specific to these key practices.
N/I No documentation of the activity was provided or identified.
(✓) Actions more generally related to the key practices, but without referencing the practice specifically.
–✓ Practice that is addressed but that is not specifically consistent with international norms – e.g. in case of anaemia: haemoglobin assessments are used and these cannot distinguish the cause of the anaemia, but treatments only address iron deficiency anaemia.
n/a Not applicable.
*KEY PRACTICES AND RELATED ACTIVITIES AS OUTLINED IN THE DETAILED METHODS PAPER IN THIS ISSUE (7) , TEXTBOX 1.
Timely introduction of breastfeeding 1 h, commencement of breastfeeding within the first hour after birth.
EBF to 6 months, exclusive breastfeeding, with no other food or drink, other than required medications, until the infant is 6 months of age.
Continued BF to 24 months, continuation of any breastfeeding until at least 24 months of age as complementary foods (CFs) are consumed.
Initiation of CF at 6 months, gradual commencement of CF at 6 months of age.
Nutrient dense CF, promotion of CFs that are high in nutrient density, particularly animal source foods and other foods high in vitamin A, iron, zinc.
Responsive feeding, encouragement to assist the infant or child to eat and to feed in response to hunger cues.
Appropriate frequency/consistency, encouragement to increase the frequency of CF meals or snack as the child ages (two meals for breastfed infants 6–8 months, three meals for breastfed children 9–23 months, four meals for non‐breastfed children 6–23 months; ‘meals’ include both meals and snacks, other than trivial amounts, and breast milk), and to increase the consistency as teeth erupt and eating abilities improve.
Dietary assessments to evaluate consumption, indicates whether dietary assessments are being conducted, particularly those that move beyond food frequency questionnaires.
Vitamin A supplements young children, commencement of vitamin A supplements (VAS) at 6 months of age and repeated doses every 6 months.
Post‐partum maternal vitamin A, VAS to mothers within 6 weeks of birth.
Zinc to treat diarrhoea, 10 mg day−1 for 10–14 days for infants and 20 mg day−1 for 10–14 days for children 12–59 months.
Prevention of zinc deficiency, provision of fortified foods or zinc supplements to prevent the development of zinc deficiency among children >6 months.
Anaemia prevention (malaria, parasites), iron/folate supplementation during pregnancy, insecticide‐treated bed nets (ITN) for children and women of childbearing years, anti‐parasite treatments for children and women of childbearing years.
Assessment of iron deficiency anaemia, any programme to go beyond the basic assessment of haemoglobin or hematocrit to assess actual type of anaemia, such as use of serum ferritin or transferrin receptor to assess iron deficiency anaemia.
Iodine programmes, promotion of the use of iodized salt; universal salt iodization or other universal method of providing iodine with programmes to control the production and distribution of these products.
Management of malnutrition, diagnosis of the degree of malnutrition, treatment at reference centres/hospitals for severe acute malnutrition and appropriate follow‐up in the community, or local health centre; or community‐based treatment programmes for moderately malnourished children.
Prevention of MTCT HIV/AFASS, appropriate antiretroviral treatments for HIV+ women during and following pregnancy to avoid transmission to the infant, exclusive breastfeeding to 6 months, breast milk substitutes only when exclusive breastfeeding is not possible. Substitutes should be acceptable, feasible, affordable, sustainable and safe, weaning should be gradual or EBF should be followed by partial breastfeeding depending on the risk factors (see Textbox 4 of the detailed methods paper in reference (7)).
Food security, programmatic activities with impact on infant and young child nutrition (IYCN), including agency response to crises, tracking markers of food security and food aid distributions.
Hygiene and food safety, all aspects of appropriate hand washing with soap, proper storage of food to prevent contamination and environmental cleanliness, particularly appropriate disposal of human wastes (latrines, toilets, burial).
CATEGORIES OF ACTIONS.
Policies, nationally written and ratified policies, strategies or plans of action.
Formative research; studies that specifically assess barriers and beliefs among the target population regarding each topic and bibliographic survey of published studies identified through PubMed search of ‘nutrition’ plus either ‘child’ or ‘woman’ plus the name of the country and/or by key informant.
Training/curricula, programme protocols, university or vocational school curricula or other related curricula that specifically and correctly addresses each desired practice, these include pre‐ and in‐service training manuals.
Programmes, documented programmes that are functioning at some level that are intended to specifically address each key practice listed.
Intended programme coverage, the level at which the programme is meant to be implemented, according to programme documentation/plans.
Actual programme coverage, the extent of programme implementation that was confirmed in one of the received documents.
Programme monitoring, monitoring activities that are conducted for a given programme that specifically quantify programme coverage, training, activities implemented, whether messages are retained by caregivers.
Surveys and evaluations, studies that have been conducted to evaluate changes in specific population indicators in response to a programme and/or cross‐sectional surveys.
ADDITIONAL INFORMATION
BFHI = Baby Friendly Hospital Initiative implemented at specified hospitals and health centres and adherence to the international Code of the marketing of breast milk substitutes.
§ Per cent of infants reportedly put to the breast within one hour of birth, DHS 2005.
¶ Per cent of infants reportedly consuming exclusively breast milk the day prior to the survey, DHS 2005.
Per cent of children 20–23 months still consuming breast milk; calculated as 100% – the percentage NOT consuming breast milk, DHS 2005.
Per cent of infants 6–7 months reportedly consuming complementary foods (beyond liquids) the day prior to the survey, DHS 2005.
Per cent of children <3 years consuming vitamin A fruits and vegetables (VA‐FV), or animal source foods (MFPE = meat, fish, poultry, eggs), DHS 2005.
Per cent of children 6–23 months who reportedly consumed the minimum number of meals during the day prior to the survey, DHS 2005.
¶¶ FRAT survey to assess the frequency and quantity of consumption of selected possible food vehicles for fortification programmes, 2006.
Per cent of children 6–59 months who reportedly received vitamin A supplement during the previous 6 months, DHS 2005.
††† Per cent of women who received vitamin A supplement early post‐partum following the last pregnancy occurring in the prior 5 years, DHS 2005.
‡‡‡ Per cent of women who reported night blindness during the last pregnancy that occurred within the prior 5 years, DHS 2005.
§§§ Per cent of children who slept under an insecticide treated bed net the night before the survey, DHS 2005.
¶¶¶ Per cent of pregnant women who slept under an insecticide treated bed net the night before the survey, DHS 2005.
Per cent of children 6–59 months with haemoglobin concentration <11.0 g dL−1, DHS 2005.
Per cent of women who reported taking iron–folic acid supplements ≥90 days during the last pregnancy occurring in previous 5 years, DHS 2005.
Per cent of women 15–49 years with haemoglobin concentration <11.0 g dL−1, DHS 2005.
Per cent of children <5 years living in households with adequately iodized salt (≥15 ppm), DHS 2005.
Per cent of tested households in which the salt was adequately iodized (≥15 ppm), DHS 2005.
Per cent of children <5 years < −2 z‐score, weight‐for‐height (WHZ), weight‐for‐age (WAZ), height‐for‐age (HAZ), by WHO Child Growth Standards, DHS 2005.
Reports using evaluations from the first phase of a malnutrition prevention programme in enhancing the second phase, CAMA‐MBOUR project, (8).
Per cent of women 15–49 years reporting knowledge that HIV can be transmitted by breastfeeding, DHS 2005.
Very limited survey of infant feeding choices of six HIV‐positive mothers, (9).
¶¶¶¶¶ Per cent of households with access to toilet or latrine for disposal of human wastes (use for disposal of children's wastes not included), DHS 2005.
Per cent of participation in weekly education sessions during 6‐month intervention in a community nutrition programme, (10).
Results
The wide range of the activities reported in identified documents demonstrates the Senegalese government's keen awareness of the existing nutritional problems and its substantial commitment to implement appropriate actions to improve the health and nutritional status of Senegalese infants and young children.
The following sections present the findings of the situational analyses. These findings are summarized in Table 1 by feeding practice or other nutrition‐related activities (rows) and by type of document reviewed and identified programme coverage (columns). The section on breastfeeding provides examples on how to interpret the information provided in Table 1, and the contents are further explained in the table's footnotes.
Promotion of optimal feeding practices
Breastfeeding
National policies, strategies, plans of action
All three key breastfeeding practices (Table 1) were clearly addressed in at least one of the national nutrition policies, strategies and plans of action that were reviewed, as noted with check marks in the first column ‘policies’ for the first three rows on breastfeeding in Table 1. In addition, there is a Senegalese code for the marketing of breast milk substitutes, and the Baby Friendly Hospital Initiative is being promoted. Although at one time 36 hospitals were certified, in 2002 just three hospitals were still certified as Baby Friendly, according to a representative from DANSE. The government also mandates work release for breastfeeding women early post‐partum.
Formative research
Eight identified surveys included questions regarding beliefs and barriers associated with breastfeeding practices in selected sites in Senegal. Positive beliefs that were identified include: (i) early introduction of breastfeeding speeds the cleansing of the infant's bowels following birth 8, 9, 10, 11, 12, 13, 14; and (ii) malnourished children benefit from breastfeeding (15). Potentially negative beliefs include: (i) the mother should be bathed before allowing breastfeeding to commence 8, 9, 10, 11, 12, 13, 14; (ii) the first thing introduced into the infants' mouth should be the sacred water or ‘l'eau bénite’8, 9, 10, 11, 12, 13, 14; (iii) breastfeeding is fatiguing (16); (iv) infants require extra water beyond breast milk (16); and (v) colostrum can provoke diarrhoea (17). Among these is a series of surveys across five regions of Senegal, as reported in 2007 8, 9, 10, 11, 12, 13. These surveys provide more population‐representative data for programme development than the others listed, which were smaller in scale.
Another series of studies reported findings related to breastfeeding and complementary feeding in the Niakhar Population and Health Project in 1989–1998 15, 18, 19, 20, 21, 22, 23, 24. Project documents were not available beyond these identified research articles. One of these articles by Simondon et al. (17) reported reasons for weaning or continuing breastfeeding among 485 children in rural Senegal, as collected during two rounds of structured interviews when the children were 18–28 months and 23–33 months of age. The authors reported that the main reasons for weaning prior to 2 years (n = 244 children) included that the child ate well from the family plate (60%), that the child was ‘tall and strong’ (46%) or that the mother was again pregnant (35%). The main reasons for weaning later than the age of 2 were because of perceived weakness or small size of the child (33%), food shortage (25%), illness of the child (24%) and refusal by the child to eat family meals (14%, n = 120). Thus, in this study, older breastfed children may have been more sick or malnourished than non‐breastfed ones.
These findings are indicated with checkmarks in the respective cells of the column on formative research in Table 1. The Basic Support for Institutionalizing Child Survival (BASICS) project (http://www.basics.org) also reportedly conducted a series of surveys and interviews nationally to identify key barriers to optimal feeding practices for use in developing educational messages. Unfortunately, the BASICS survey findings were not available for review.
Training manuals and protocols
Most of the identified training materials and protocols (16 of 27 documents) addressed some aspect of breastfeeding. Just four of these documents clearly addressed all three of the key breastfeeding practices indicated in Table 1. Two of these were older documents which still recommended continuing exclusive breastfeeding to just 4–6 months of age 25, 26. The respective cell in Table 1, under training materials, includes a check mark for those documents which correctly promote exclusive breastfeeding to 6 months of age, and a second check mark preceded by a negative sign for the documents that still promote exclusive breastfeeding to just 4–6 months. Two of these training manuals reported that barriers and beliefs to optimal practices were an integral part of the training process 25, 27, and nearly all of the reviewed training materials incorporated some guidance on information education communication (IEC).
Programmes
The three key breastfeeding practices are promoted in the national PRN and the PAIN, and these programmes are reportedly intended to be implemented nationally. The national breastfeeding promotion week commenced in 1995 and is hosted in different regions each year (28). The selected themes reflect the World Breastfeeding Week themes (http://www.worldbreastfeedingweek.net/wbw2009/themes.htm). The intended coverage of programmes promoting the three key breastfeeding practices, in Table 1, is listed as ‘national’ for intended and actual coverages of the national breastfeeding promotion week in all regions.
Surveys and monitoring and evaluation reports
Senegal has recently reported substantial progress toward improving several nutrition indicators of infant and young child health. Rates of breastfeeding within the first hour after birth doubled between 1992 and 2005 (Fig. 4). However, even with this increase, less than a quarter of infants were put to the breast in the first hour after birth.
Figure 4.
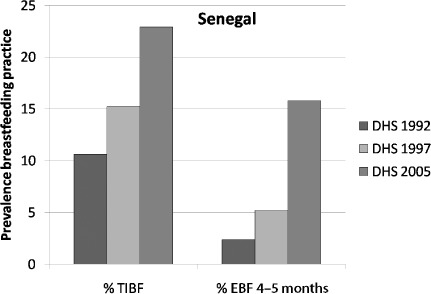
Senegal – Per cent of infants put to the breast in the first hour after birth (TIBF), exclusive breastfeeding (EBF) among infants 4–5 months of age, according to maternal report. Data courtesy of UNICEF West and Central Africa Regional Office from Demographic and Health Surveys (DHS) (29, 30, 31).
The duration of exclusive breastfeeding to 6 months and appropriate introduction of complementary foods at 6 months also increased dramatically in the same period of time (Fig. 5). The prevalence of exclusive breastfeeding among infants 4–5 months increased from 2% (1992/1993) to 14% (2005). These are notable improvements, but optimal breastfeeding is still well below desirable prevalances.
Figure 5.
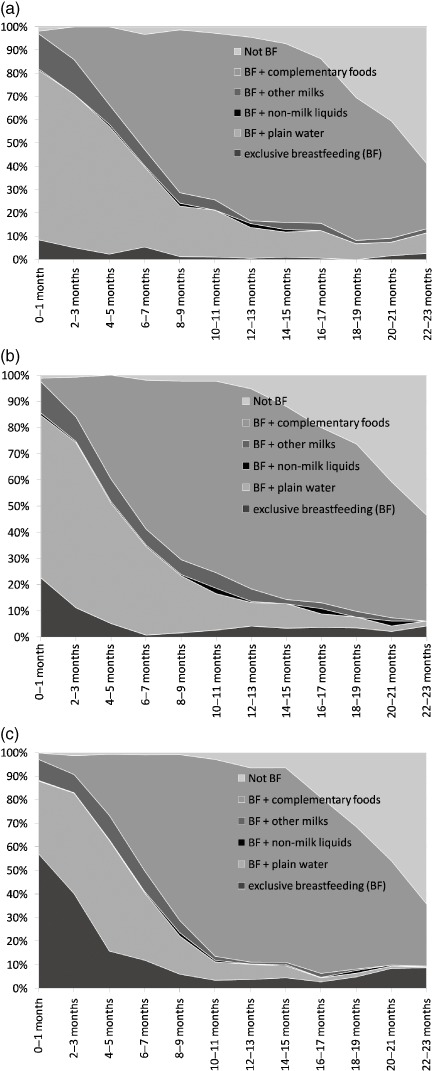
Senegal – Per cent of children by breastfeeding practice and age in months. (a) 1992/1993 DHS (31); (b) 1997 DHS (32); (c) 2005 DHS (33).
As of 2006, the PRN reportedly was reaching 50% of the population in the 11 regions across Senegal (32). However, none of the identified programme monitoring confirmed which programme components were being implemented in each region and impact evaluations were not conducted. Therefore, we could not confirm which programmes were most likely to have contributed to the improvements in breastfeeding practices just noted.
Improvements in breastfeeding practices, as compared with baseline surveys, were reported in one community where the community‐based growth promotion component of the BASICS project was being implemented (33) and in 10 villages of the CANAH project region where promotion of health care and appropriate feeding choices included grandmothers along with mothers (34). However, analyses compared changes in relation to the situation at baseline in these intervention sites, but not in comparison to changes in non‐intervention sites. Therefore, the analyses were not rigorous enough to confirm whether the intervention contributed to the reported improvements in breastfeeding practices.
Summary of findings – breastfeeding
-
•
National policies, programmes and training protocols clearly address all three of the key breastfeeding practices. The training materials identified were not specific to the national programmes with nutrition components (PRN/PAIN/IMCI), so we could not always confirm which components are being addressed in each programme.
-
•
National campaigns promoting various themes on breastfeeding have been taking place annually since 1995.
-
•
Surveys, small‐scale and nearly national, have inquired into barriers to optimal breastfeeding practices and beliefs that influence these practices.
-
•
Most training materials incorporate aspects of IEC into methods promoted for disseminating nutrition messages.
-
•
The national prevalence of exclusive breastfeeding among infants < 6 months increased between 1992 and 2005 (DHS findings). However, programme evaluations were not rigorous enough to confirm which programmes had a positive impact on improving these practices. Despite these notable increases, overall prevalence is still low.
-
•
Some monitoring and evaluation surveys reported on the logistics of programme implementation, such as supervision and available facilities that would be useful in improving programme activities. We could not confirm how these reports were used to improve programme activities or how many programme components are being implemented in various sites.
Recommendations – breastfeeding
-
•
Support of breastfeeding promotion should continue to ensure that recent improvements are maintained and expanded.
-
•
Rigorous programme evaluations are necessary to determine which programmes have been successful in promoting these successes, how well programmes are being implemented, and how to best adapt programmes to continue to improve breastfeeding practices nationally.
-
•
These monitoring and evaluation activities could also include better mapping of in‐service training and impact evaluations to facilitate tracking of programme implementation and to confirm which regions are not yet being reached compared to identified needs. Based on these findings, programmes can be expanded more effectively to optimize their impact.
Complementary feeding
National policies, strategies and plans of action
We identified national policies and strategies that promoted three of the four key complementary feeding practices outlined in Table 1, namely: (i) the introduction of complementary foods at 6 months of age; (ii) the importance of introducing nutrient‐dense complementary foods; and (iii) gradually increasing the frequency of meals and the consistency of complementary foods. The importance of being responsive to the needs of infants and young children when providing food by following hunger cues was not included.
Research
As mentioned previously, Simondon et al. (15) found that respondents in a programme evaluation reported that children who were growing well could be weaned earlier than sick children. Thus, healthy children in this study group could be put at risk by weaning from breastfeeding too early. Additional findings from this programme evaluation (23) among 522 infants followed from 2–3 months of age until 6–10 months of age were that infants who consumed complementary foods early, commencing between 2–3 months of age, had lower weight‐for‐age, length‐for‐age and mid‐upper arm circumference at 6–10 months of age than those who initiated complementary feeding at 4–5 or 6–7 months of age. These findings support current international recommendations, to delay the introduction of complementary foods until 6 months of age, and could be used to demonstrate to mothers the importance of exclusive breastfeeding during the infant's first 6 months of life.
Training materials, programme protocols and related programmes
The 2003–2004 guidelines for the community‐level IMCI (C‐IMCI) promoted all four key complementary feeding practices 26, 35, 36. The C‐IMCI is intended to be implemented nationally, but we could not confirm the actual coverage of training and implementation of this approach. None of the more recent nutrition training materials reviewed included any guidance on complementary feeding practices.
Surveys, monitoring and evaluation reports
As seen in Figure 5, reported consumption of complementary foods among infants at 6–7 months increased from 30% (1992/1993) to 50% for the day prior to the 2005 DHS survey (31). Only about half of the children 12–23 months of age reportedly consumed vitamin A‐rich foods during the day prior to the survey, and slightly more reportedly consumed iron‐rich foods (57–65%). These reports are higher than reports from national surveys of most other countries included in this issue's situational analyses. However, the total amount consumed of these foods is not collected for DHS reports.
We found no dietary analyses from which to determine the total nutritional quality of complementary foods consumed by young children in Senegal. Further, there is no data on whether nutritionally adequate complementary foods are available or affordable among the most food‐insecure populations.
There is still considerable room for improvement, particularly considering the high prevalence of anaemia among children <5 years of age [83% (31)]. These feeding indicators contribute information towards calculating the currently recommended infant and young child feeding indicators (37). Most data required for these indicators were not yet available from previous national surveys, but UNICEF recently published estimates (38).
Summary of findings – complementary feeding
-
•
National policies/strategies, training materials and programmes promote most of the optimal complementary feeding practices, but most support for complementary feeding is found in older documents.
-
•
Among the documents reviewed, the community IMCI protocols (26) provide the most comprehensive training on practices that constitute optimal complementary feeding, but we could not confirm the coverage of these programme activities. Other documents that address complementary feeding are less specific, leaving doubt regarding what are considered optimal complementary feeding practices.
-
•
We found no programme monitoring or evaluations confirming whether programmes currently address any identified barriers to optimal complementary feeding practices, actually implement protocols to provide appropriate counselling on complementary feeding or have an impact on improving complementary feeding practices.
-
•
About half of children 12–24 months are reportedly consuming vitamin A‐rich foods and about two‐thirds are consuming iron‐rich foods nationally (31), but the quantities consumed are unknown.
-
•
No dietary analyses were adequate to evaluate whether the types and amounts of complementary foods consumed are adequate to meet nutritional needs or whether poor families are able to afford and provide ample quantities of nutrient‐dense complementary foods to young children.
Recommendations – complementary feeding
-
•
There is a need to ensure that new nutrition programmes that promote IYCN do not neglect the promotion of optimal feeding practices beyond breastfeeding.
-
•
Monitoring and evaluation activities should be conducted to confirm (i) which programmes are most effective at promoting the appropriate complementary feeding behaviours reported in national surveys, and (ii) whether pertinent activities are being implemented as necessary in all regions, particularly in regions where the highest nutritional vulnerability is identified.
-
•
Based on these findings, effective programmes should be expanded to increase their impact.
-
•
There is also a need for qualitative studies of dietary intakes to identify gaps in the nutrient quality and adequacy of complementary foods. These findings should be used in developing educational messages and guide the development of interventions to ensure that children have access to and are consuming adequate amounts of nutrient‐dense complementary foods such as targeted fortified complementary foods, point of use fortificants, supplements and/or dietary modification.
Prevention and treatment of micronutrient deficiencies
Vitamin A
National policies, strategies and plans of action
National policies, strategies and/or directives target the prevention of vitamin A deficiency through the promotion of semi‐annual vitamin A supplements (VAS) for children 6–59 months of age and VAS for women early post‐partum 29, 40.
In 2006, the strategic plan for food fortification with micronutrients (41) was accepted and activities are moving forward for oil fortification with vitamin A. This fortification is now mandatory.
Formative research and training materials and related programmes
The 2005 FRAT survey (42) reported on the consumption of cooking oil across various regions in Senegal. This survey was instrumental in selecting oil as the vehicle for the mass vitamin A fortification programme, commencing in 2010. It is expected that half of children 12–59 months of age would consume more than half of their vitamin A needs and half of women 15–45 years would consume at least 140% of their recommended daily intake of vitamin A through fortified oil 42, 43. However, the intakes vary widely across regions. It is expected that the primary benefit of this fortified oil for children in families with limited resources would be through breast milk.
VAS are provided nationally through semi‐annual campaigns and micronutrient promotion days (44), the C‐IMCI 35, 36, 45, PRN (46) and PAIN (47), and programmes managing malnutrition and HIV 46, 48, 49, 50. In addition, the C‐IMCI and PAIN promote the use of vitamin A‐rich foods.
Financial responsibility for the VAS campaigns began with international support and is gradually being transferred to the national and district levels. Reports of progress towards this transfer are favourable and the programme should be fully supported by government resources by 2015 (51).
Surveys, monitoring and evaluation
VAS was reportedly reaching three fourths of children 6–59 months in 2005 (31) and more than 80% of children in more recent years 51, 52. However, only about one‐fourth of women early post‐partum were reached with VAS (31), indicating a need for additional support for VAS through other post‐natal contacts. The per cent of infants who commenced VAS at 6 months of age was not reported. However, if relying mainly on semi‐annual national campaigns, very few infants will commence VAS right at 6 months of age.
In 1993, nearly three‐fourths of 281 children 6–59 months had vitamin A deficiency (serum retinol <0.7 umol L−1) in a rural location of Senegal at the end of the lean season (53). The presence of infection, which can affect serum retinol levels, was not reported. More recent surveys are not available. We did not identify any baseline and follow‐up surveys of vitamin A status indicators that were specific to programme interventions.
Zinc
National policies, strategies and plans of action
The national policy for infant and young child feeding promotes the use of zinc supplements for the treatment of diarrhoea (54). National legislation does not yet address the possible risk of zinc deficiency.
Formative research, training materials and related programmes
We found no studies evaluating zinc status of young children or the use of zinc in treating diarrhoea. One study on local barriers and beliefs did report that participants believed that oral rehydration solution (ORS) is not sufficient to treat children with diarrhoea and they seek further interventions (55). The introduction of zinc supplements in diarrhoea therapy may fill the need identified by these caretakers for something more than just ORS (56).
The national PRN programme promotes the provision of zinc supplements to children during the treatment of diarrhoea, when authorized by a doctor 46, 55. More recent documents were not available to confirm whether this is now expanded to other health staff. No programmes yet promote the prevention of zinc deficiency. As described next, zinc is currently added to the premix to fortify wheat flour in Senegal. Because only the iron and folic acid fortificants are mandated, it is not certain whether manufacturers will continue to purchase premix that includes zinc.
Surveys, monitoring and evaluation
In the absence of data on the prevalence of zinc deficiency, the International Zinc Nutrition Consultative Group estimates the national risk of zinc deficiency to be a public health concern if the national prevalence of stunting among children <5 years of age (height‐for‐age < −2 z‐score) is >20%. The national prevalence of stunting in Senegal was 20.1% in 2005 [using the WHO growth reference standards for DHS 2005 (31)], but the prevalence varied widely across regions. Thus, zinc deficiency is likely a public health risk in many regions of Senegal.
An evaluation of the Project Health‐Community Health, completed in 2007, reported that 52–99% staff in 7 of the 11 regions of Senegal had been trained on the proper use of zinc supplements in the treatment of diarrhoea (14). Impact evaluations were not yet available. In 2008, a national situational analysis, in preparation for the use of zinc supplements in the treatment of diarrhoea (55), found that although community health workers were conversant with recommended management of diarrhoea with ORS: (i) the general populace is not applying the messages received during health education activities; (ii) health centres lack resources, such as health cards and counselling cards, to support information education; and (iii) current household management of diarrhoea is not in compliance with recommendations from health centres. They did not report on the quality of the educational messages. Thus, there is a need to improve programme monitoring to identify the reasons whether educational messages were provided as designed and why participants are not applying recommendations. Oral rehydration solution was distributed to health centres through traditional essential medication methods at the time of the study, so the authors considered that stock‐outs would be possible thus impeding its distribution.
Iron and anaemia
National policies, strategies and plans of action
National policies, strategies and/or directives target the prevention of anaemia and iron deficiency through promotion of iron–folic acid supplements during pregnancy (54) and the consumption of iron‐rich foods (57).
The Strategic plan for food fortification with micronutrients (41), mentioned previously, also promotes fortification of wheat flour with iron and folic acid. This fortification is now mandatory.
Formative research, training materials and related programmes
Training manuals and protocols addressed the key practices to reduce the risk of anaemia related to iron deficiency, malaria and parasite infections.
The reproductive health services protocols (58) include an additional recommendation to delay cord clamping until the pulse decreases, as one method of reducing the risk of anaemia in the infant.
Programmes to prevent anaemia and iron deficiency include the promotion of iron–folic acid supplements during pregnancy, anti‐parasites, and the use of insecticide‐treated bed nets (ITNs) for children and pregnant women. These promotions occur during national VAS campaigns (46) and through other national and regional programmes 27, 46, 48, 59, 60, 61. No policies or programmes identify the need to differentiate iron deficiency from other causes of anaemia in Senegal, where malaria is endemic. However, protocols only recommend providing iron supplements to young children through malnutrition programmes.
According to estimates based on a FRAT survey of intakes of wheat flour and the currently recommended levels of micronutrients, once these programmes reach universal fortification, the fortified wheat flour would provide recommended amounts of iron (3–4 mg day−1) to 27–46% of children 12–59 months of age, and about half or more of the recommended amount of zinc and iron to 39–71% of women in childbearing years, varying by region 42, 62. Although these theoretical intakes should have an impact on the iron status of children who consume the expected amount of wheat flour, it is not certain whether these levels of iron through a fortified product will be adequate to have an impact on the prevalence of anaemia as a result of iron deficiency among young children.
Surveys, monitoring and evaluation
Despite high prevalences of anaemia among young children and women in childbearing years reported in 2005 [83% of children 6–59 months and 59% of women 15–49 years with haemoglobin concentrations < 11.0 g dL−1 (31)], methods of preventing anaemia were used infrequently: ITNs were reportedly used in just 10% of households with young children, and just 40% of pregnant women consumed at least 90 days of iron–folic acid supplements during the most recent pregnancy (during the previous 5 years). As mentioned previously, more than half of children 6–23 months reported consuming an iron‐rich animal source food the day prior to the 2005 DHS, but the amount consumed was not quantified. The prevalence and linked risks of iron deficiency among young children, with or without anaemia, is unknown. This information could assist programme developers in identifying methods of reducing iron deficiency and anaemia.
Following two rounds of integration of deworming into the national VAS campaign, a small survey found anaemia among 48% of the 121 children 11–59 months of age surveyed in the Tambacounda region of Senegal in 2007 (63). No baseline data were collected, but the DHS data in 2005 in this region reported 88% anaemia among children 6–59 months of age. Although the observed difference in the prevalence of anaemia could be due to multiple factors, including the season of the survey or differences in sample selection, these findings are encouraging.
Iodine
National legislation mandates iodization of salt (document not available) and the use of iodized salt is promoted nationally by the PRN and PAIN programmes 46, 60. However, in 2005, just 35% of households with children <5 years and 36% of households of women of childbearing years had adequately iodized salt available (31).
Surveys, monitoring and evaluation
A 2007 survey evaluated the impact of salt iodization in Tambacounda and Kolda regions, where the prevalence of goitre was previously highest (63). There was an increase in the percentage of households in which adequately iodized salt (≥15 ppm iodine) was found, from 39 and 24% in 2005 (31), respectively, in these two regions, to 95 and 63% in 2007 (63), respectively. The prevalence of goitre reportedly decreased from 40 to 5% in these regions. However, in 2007 they also found that 38% of tested children had urinary iodine concentrations <100 µg L−1, indicative of inadequate iodine status (63).
Summary of findings – prevention of micronutrient deficiencies
-
•
National policies, training materials, programmes and research address most of the key methods promoted to prevent micronutrient deficiencies. However, there are no specific recommendations to prevent zinc deficiency and methods are not available to distinguish between general anaemia and iron deficiency in Senegal where malaria is endemic.
-
•
Recent surveys indicate that VAS are reaching >80% of children 6–59 months, but <30% of women early post‐partum (31). The proportion of infants who receive VAS commencing at 6 months of age is not reported.
-
•
Currently, the costs of VAS campaigns are being successfully transferred from mostly external donors to national and district‐level governmental budgets.
-
•
There are no surveys of the risk of zinc deficiency in Senegal in children. Based on the prevalence of stunting, there is an elevated public health risk of zinc deficiency in Senegal, particularly in certain regions.
-
•
Despite fairly high reported consumption of iron‐rich foods among young children and the national promotion of methods to reduce anaemia and iron deficiency, the prevalence of anaemia is very high among young children (83% of children 6–59 months) and women (59% of women 15–49 years). There are no activities to define the prevalence of iron deficiency in guiding intervention programmes.
-
•
The implementation of the national mandate to fortify cooking oil with vitamin A and wheat flour with iron and folic acid is moving forward. The micronutrient premix for floor also currently includes zinc and some other vitamins.
-
•
National policies also mandate universal iodization of salt produced in Senegal, but surveys indicate this is not yet occurring and iodine deficiency disorders are still a health risk in Senegal.
Recommendations – prevention of micronutrient deficiencies
-
•
National policies should be updated to include the prevention of zinc deficiency and there is a need to evaluate the risk of zinc deficiency among high‐risk populations of young children and women in childbearing years to guide possible prevention programmes.
-
•
Training on the introduction of zinc supplements in the treatment of diarrhoea should be extended to all health care facilities and, as this expands there is a need to confirm that caregivers are providing ORS and supplements as recommended.
-
•
As flour and oil fortification programmes are implemented, researchers should evaluate the impact of these programmes to confirm whether there is an impact on anaemia and vitamin A deficiency. Possible targeted programmes for at‐risk populations not reached by these fortified products should also be considered, particularly among young children.
-
•
Research is needed to define the causes of anaemia, to identify why available methods of preventing anaemia are not used and how to increase accessibility and use of these methods.
-
•
Programmes to ensure universal salt iodization must be strengthened. If this is not possible, more expensive alternative methods of preventing iodine deficiency disorder may be necessary among populations with the highest risk of iodine deficiency.
Other nutritional support: management of acute malnutrition, prevention of mother‐to‐child transmission of HIV, food security and hygiene
Management of acute malnutrition
National policies, strategies and plans of action
National legislation promotes community‐ and facility‐based screening and management of acute malnutrition and growth monitoring 54, 64, 65.
Formative research
We identified eight research articles conducted in Senegal that addressed topics related to malnutrition. Notable findings from these research articles include: (i) in a cross‐sectional study, 30% of 1731 evaluated hospitalized children were malnourished and the main associated illnesses were diarrhoea (51%), pneumonia (30%) and malaria (7%) (66); (ii) among 70 severely malnourished children who entered one study, those who were randomly assigned to receive a solid peanut‐based ready‐to‐use food supplement consumed more calories, gained relatively more weight and completed the rehabilitation phase more rapidly than those randomized to receive the usual F100 milk‐based liquid supplemental food (67); and (iii) rates of stunting and iron deficiency anaemia were still significantly higher 5 years after recovery from severe acute malnutrition (24 children) than among 24 similarly aged siblings and 19 age‐matched controls who had never been severely malnourished (68). The first study provides useful information in developing educational messages to prevent malnutrition. The second study was small, but has reportedly been used to advocate for improved methods of managing malnutrition.
One study that could have an impact internationally, if confirmed in other settings, was reported by Donnen et al. (69). They evaluated the impact of randomly assigned low‐dose (5000 IU) or high‐dose (100 000 IU for infants and 200 000 IU for children 12+ months of age) VAS to 1214 hospitalized malnourished children. They found a lower incidence of respiratory infection among children on the low‐dose vitamin A, compared with those on the high‐dose vitamin A; and among children with oedema upon admission, mortality was lower among those who were randomized to receive the low‐dose supplement, compared with those who received the high‐dose supplement. If confirmed in other settings, this could have an impact on international recommendations for VAS provided to malnourished children, particularly those with oedema.
Training materials and protocols
The 2008 national training manual for the management of malnutrition (50) provides guidance on screening, diagnosing and treating children with malnutrition. Recommended treatments for malnourished children, depending on the phase of treatment, included: (i) VAS, if none were received in the prior month; (ii) iron–folic acid supplements; and (iii) anti‐parasites, in addition to the usual supplemental food regime. This guide did not yet apply the current international recommendations to evaluate iron status prior to providing iron supplements in malaria‐endemic regions (70), such as Senegal.
This manual also promoted exclusive breastfeeding among malnourished infants less than 6 months. Counselling guidelines did not include promotion of high nutritional quality and adequate quantities of complementary foods for children ≥6 months of age to prevent relapses once recovered from malnutrition.
Programmes
Programmes to manage malnutrition are incorporated in the national PRN (46) and two older regional projects 16, 48. The national strategy plan for the PRN (46) indicated that the PRN was reaching 50% of the Senegalese population, but it did not specify whether the malnutrition component was implemented in all sites. One objective of this PRN strategy was to reinforce the capacity of community agents to monitor children's growth and improve negotiations with mothers and other care‐givers on health care and feeding options for their children. Home visits by community agents are also encouraged for mothers of children who do not participate in the clinic activities and/or whose children have experienced 2 or more months of growth faltering.
Surveys and monitoring and evaluation reports
Several evaluations of the impact of programmes on preventing malnutrition were identified. The findings appeared to be promising and could identify programmes linked to reducing the prevalence of underweight in Senegal. However, none of the assessments statistically compared changes in intervention sites with changes in non‐intervention sites to confirm the impact, most did not include comparison sites and the programme components that were most likely to have contributed to these changes were not identified. For example, an impact evaluation comparing randomly selected intervention and non‐intervention villages following implementation of the PRN in three regions between 2004 and 2006 (71) found that the decrease in the prevalence of wasting observed in the intervention villages was larger than the decrease observed in the non‐intervention villages, but analyses did not compare these decreases to determine whether there was a statistical difference between sites. The CAMA project (48) reported in 2006 that the prevalence of malnutrition decreased from 26.9% at baseline, to 8.3% after 12 months of intervention during the first phase of the project (indicator not defined), but there were no non‐intervention sites for comparison. The prevalence of malnutrition in the surrounding region was 13% at about the same time, according to DHS 2005. The reported lessons learned during the first phase of the CAMA project (48) included: (i) that behaviour change requires buy‐in by the caregiver's support system (grandmothers, fathers, community leaders, other women); (ii) reinforcement of the capacities of community organizations facilitates the appropriation of health‐ and nutrition‐related resources, such as the dissemination of ITNs; and (iii) the distribution of small grants to promote small revenue‐generating activities is an important motivator for community organizations to take responsibility for health and nutrition activities. The authors reporting on the AGETIP programme assessed the prevalence of malnutrition (weight‐for‐age < 89 percentile, NCHS), in four different cohorts of children who were evaluated as the programme expanded between 1996 and 1998. The prevalence of malnutrition decreased from about 60–70% at baseline to about 20% after 6 months of intervention in these four cohorts (72). Again, no comparison sites were evaluated.
Summary of findings – management of acute malnutrition
-
•
National policies, training materials and related programmes address methods of preventing and treating acute malnutrition among young children.
-
•
Programme monitoring is not available to confirm the extent to which malnutrition prevention and treatment activities are implemented in available programmes.
-
•
Several studies contributed information for guiding the development of malnutrition treatment programmes, and programme evaluations identified possible positive impacts of nutrition programmes on reducing the prevalence of malnutrition. These programmes may have contributed to the reported reductions in underweight since 1990. However, programme evaluations generally did not include control sites. When control sites were available, the changes in the control sites were not compared statistically to changes in intervention sites to confirm the impact of the intervention beyond other changes in the region.
Recommendations – management of acute malnutrition
-
•
There is a need to improve programme monitoring and evaluation to confirm the implementation of programme activities and the impact of these programmes, thus facilitating decisions on whether to continue or change programmes to treat and prevent malnutrition.
Prevention of mother‐to‐child transmission of HIV
National policies, strategies and plans of action
HIV is addressed in two national policies 73, 74. These policies were developed prior to the current international recommendations for feeding and antiretroviral therapy recommended to reduce the risk of mother‐to‐child transmission of HIV 75, 76.
Formative research
A baseline survey was conducted in 2006 (77) in Dakar, the capital of Senegal, and in Ziguinchor region to evaluate the knowledge, attitudes and practices of persons living with HIV and the staff members who would be implementing the upcoming HIV‐related nutrition programme. Some of the key findings were the need to: increase relevant staff training, improve interpersonal communication between staff and participants with the development of visual aids, and take into account the nutritional needs of the children of persons with HIV. No follow up to this survey was identified.
A World Health Organization Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality (78) used data from Senegal and five other countries to evaluate the risk of mortality as a result of illness among infants of HIV‐positive women, based on their breastfeeding status. This analysis included previous data from Senegal [1983–1986 study (79)] to evaluate the risks associated with lack of breastfeeding and led to the development of recommendations to promote exclusive breastfeeding among infants <6 months of age, including when the mother is HIV positive. No other research was identified related to infants or young children and HIV.
Training materials and related programmes
Several identified national‐level 26, 35, 36, 48, 58, 80, 81 and regional‐level (61) training guides provide guidance on preventing HIV transmission, including a 2005 guidebook for participants (82). Feeding methods for the prevention of mother‐to‐child transmission (PMTCT) of HIV are only addressed in general 25, 58, 83. These guidelines were all written prior to the recent international recommendations to promote exclusive breastfeeding for all infants <6 months of age in combination with antiretroviral therapy to prevent mother‐to‐child transmission (MTCT) of HIV (75).
The national coverage of the implementation and training on these guidelines was not available. In addition to the programmes linked to the said training guides, the national programme for the PMTCT of HIV (84) and the PRN (46) also promote methods of reducing transmission of HIV.
Surveys and monitoring and evaluation reports
A review of the PMTCT programme among 13 hospitals and clinics, reported in 2007 (84), evaluated counselling, screening, staff training and the available resources to carry out these activities in these centres. Those interviewed reported a general lack of adequately trained staff and some facilities lacked the infrastructure to carry out PMTCT activities. This review also included a very small evaluation of infant‐feeding choices among six HIV‐positive women in which women reported that social image was more a factor in selecting feeding practices than financial concerns. This type of survey should be repeated in a more representative sample of women to guide the development of educational messages for PTMTC.
Female participants in the 2005 DHS survey (31) identified condoms (75%), fidelity and limiting sexual partners (91%), and abstinence from sexual relations (86%) as primary methods of preventing HIV transmission. The MTCT of HIV was not addressed in this survey.
Summary of findings – PMTCT of HIV
-
•
National policies, training materials and programmes promoting the PMTCT address a variety of methods, but do not include the infant feeding guidelines recommended to reduce the risk of MTCT.
-
•
Comprehensive training and counselling materials, including a handbook for the participant, are available to aid in counselling persons living with HIV. These provide guidance on: (i) methods of reducing the risk of transmission; (ii) maintaining optimal health status when affected by HIV; and (iii) the previous recommendations on selecting feeding options for infants of HIV‐positive mothers.
Recommendations – PMTCT of HIV
-
•
National policies, training materials and programme documents should be updated to incorporate the latest recommendations regarding infant feeding and antiretroviral therapy to prevent MTCT of HIV.
-
•
Surveys among a representative population of HIV‐positive women with infants and of healthcare providers are needed to identify barriers that may be encountered in implementing the new recommendations for feeding and antiretroviral therapy among infants of mothers with HIV, including health workers, participants, possible supply‐chain issues.
Food security
We found no programmes specifically addressing the risk of food security among infants and young children. Household‐level programmes and situation tracking are beyond the scope of these analyses, but are discussed briefly here because of the potential impact on young children's feeding patterns.
The World Food Programme's Senegal Country Program includes a component for the prevention of food crises, in addition to providing support for the government's efforts to prevent malnutrition (85). Other documents identified food security‐related activities, including a national household vulnerability analysis and mapping survey conducted in 2003 (86) that was used to identify the poorest and most vulnerable regions for food security interventions (Fatick, Kaolack, Kolda, Tambacounda and Ziguinchor), a second national household survey in 2004 (87), a national food balance assessment in 2006 (88) and a food security evaluation in 2007–2008 (89). Key informants identified the need to implement food security interventions which support household livelihoods, to ensure positive and sustainable impacts.
The 2003 vulnerability study demonstrated that the highest structural vulnerability and indicators of the poorest household diets were observed in the south and south‐east of Senegal. The situation appeared to be more secure moving north or closer to the region surrounding the capital of Dakar (86). In a 2008 food security evaluation (89), the mapping of rural community vulnerability demonstrated that rural community vulnerability was more widespread than the structural vulnerability and lack of dietary diversity demonstrated in 2003. Similar surveys were not available to view changes in vulnerability indicators over time.
Recommendations – food security
-
•
There is a need to evaluate the impact of household food security interventions to ensure that the impact is maximized, particularly for preventing malnutrition among young children.
-
•
Harmonized indicators across food security‐related surveys are needed to allow tracking of the situation over time, and thus, more effectively identify vulnerable populations for targeting interventions.
Hygiene and sanitary practices
As with food security, we searched for activities promoting proper hygiene within the context of infant and young child feeding practices. Additional activities are likely available that are not covered in these analyses.
The promotion of safe water, hand washing and other hygienic practices is addressed in the national strategic plan for child survival (64). Personal and environmental hygiene were addressed in the C‐IMCI training materials 35, 36, 45, including the promotion of environmental sanitation surrounding homes, use of latrines and hand washing. This programme is intended for national dissemination. The extent of coverage of these components of the C‐IMCI was not available. Additional national programmes that promoted optimal hygienic practices include the packet of essential actions for child survival (90), and the Norms and Protocols for Nutrition Services (25). No identified programmes addressed the importance of sanitary practices when preparing foods, particularly for infants and young children.
The PRN Phase II strategic plan (46) reported that access to potable water increased from 78 to 90% in urban areas and from 56 to 64% in rural areas between 2000 and 2004, but access to potable water was still as low as 22% in some regions. The reported changes were not necessarily linked to the programme interventions so the programme impact was not clarified.
The DHS 2005 indicated that while 49–67% of households had access to water, soap or a basin for hand washing, only 35% had all three available at the time of the survey. Further, only 47% of households disposed of children's stools in toilets, latrines or by burying them.
Recommendations – hygiene
-
•
There is a need to continue to support current activities promoting personal and environmental hygiene and sanitation.
-
•
The importance of proper hygienic practices in nutritional outcomes should be emphasized through the integration of the promotion of personal and environmental hygiene into health and nutrition promotion activities, as appropriate. For example, when discussing the introduction of complementary foods at 6 months of age, educational messages should also include how to ensure that these foods are safe for consumption.
General findings
Several global programme evaluations were identified among documents collected for Senegal. Identified topics included: factors influencing the nutritional status of young children (17); experiences, progress and lessons learned while implementing the IMCI (80); the status of the PAIN programme's implementation of the minimum packet of activities (47); the status of the marketing of breastmilk substitutes (91); the satisfaction of beneficiaries of the PRN (92); a compendium of national policies, programmes and practices related to infant and young child feeding (93); knowledge, practices and coverage of the PRN programme (32); health centre management of children less than 5 years of age (94); a national nutrition profile conducted in 2007 (95); a summary of the Project health‐community health surveys conducted in five regions where the project was implemented (14); a survey of the BASICS programme implementation (33); and the status of the implementation of integrating zinc supplements into the treatment of diarrhoea in 7 of 11 regions (55). The number of surveys and monitoring and evaluation reports identified in Senegal surpassed all other countries included in these situational analyses 96, 97, 98, 99, 100. As mentioned previously, few of the programme and training documents identified how the findings of these surveys were utilized, but key informants reported that at least some of the identified surveys were utilized in developing programme messages and training materials, and the interpersonal communication component of Senegalese programmes (101) provides guidelines for behaviour change communication. Unfortunately, documentation of these activities was generally difficult to obtain. There is a need for a central repository of nutrition‐related documents to provide support for future activities.
Summary
Senegal is one of the few countries in the region that is nearly on track to reaching the MDGs of reducing mortality and underweight among children less than 5 years of age by 2015. The prevalence of exclusive breastfeeding among infants less than 6 months of age has increased substantially, but is still below 40%. In addition, the CLM, which is the multi‐sector coordinating organization developed by the Senegalese government, provides an example for other countries of a governmentally supported multi‐sector unit to promote collaborative nutrition‐related activities.
Despite the notable number of evaluations that have been conducted to evaluate nutrition programmes in Senegal, including a number of large‐scale evaluations (see ‘General findings’), none included statistical analyses that were adequate to confirm the impact of the related programme. Therefore, we could not confirm which programmes contributed to the reported progress towards nutrition‐related MDGs and increases in the prevalence of exclusive breastfeeding since the early 1990s. Nevertheless, these evaluations likely contributed to implementing effective nutrition programmes in Senegal. In addition, large‐scale surveys of local barriers to optimal feeding practices were conducted, and the results were used in developing training materials. However, the extent to which these training materials are being used to provide educational messages is not documented.
Breastfeeding practices are supported through a number of older and more recent national activities. Documents in support of appropriate complementary feeding practices tend to be older and provide fewer details than for breastfeeding. Thus, there is a need to reinforce the integration of proper feeding practices in IYCN programmes. Although 60–70% of young children reportedly consumed iron‐rich complementary foods the day prior to the 2005 DHS, the prevalence of anaemia is high (83%). Dietary analyses of home‐available complementary foods are needed to understand whether currently consumed complementary foods are adequate to meet nutritional requirements. These analyses will also allow assessing whether, given available resources, it is feasible for caregivers to provide local complementary foods of adequate nutritional value to infants and young children.
Financial responsibility for semi‐annual VAS campaigns are being successfully transferred from international organizations to national and regional Senegalese budgets. About two‐thirds of the costs are now covered at the national or district level.
Although a considerable number of documents are available regarding IYCN activities in Senegal, there is no central repository of all this nutrition programme‐related information and some documents were no longer available. There is a need for more ready access and storage of the extensive documentation of nutrition‐related activities being conducted in Senegal to facilitate their use in developing subsequent policies, programmes and related documents.
Continued support is needed to ensure that: (i) national‐level and multi‐sector coordination of nutrition activities continue; (ii) research and survey findings are used in developing and improving programme guidelines; (iii) monitoring and evaluation reports are rigorous enough to identify well‐implemented programmes that are effective at improving the nutritional status of infants and young children; and (iv) these programme evaluations are used in improving and expanding the reach of effective programmes.
Supporting information
Appendix S1. Senegal summary data
Supporting info item
Financial support, in alphabetical order: Food and Agriculture Organization of the United Nations, Helen Keller International, Micronutrient Initiative, Save the Children, United Nations Children's Fund, United Nations World Food Program and the World Health Organization.
References
- 1. Central Intelligence Agency of the United States of America (2009) The World Factbook. 9 April 2009 [cited 2009 19 April]; Available at: https://www.cia.gov/library/publications/the-world-factbook/countrylisting.html
- 2. British Broadcasting Company (BBC) (2009) BBC Weather, Country Guide, Senegal. [cited 3 August 2009]; Available at: http://www.bbc.co.uk/weather/world/country_guides/results.shtml?tt=TT000530
- 3. United States Agency for International Development (USAID) from the American People (2008) DHS Statcompiler. [cited 2008 accessed 17 March 2008]; [Demographic and Health Survey]. Available at: http://www.statcompiler.com/
- 4. United Nations Children's Fund (UNICEF) (2009) Childinfo: Monitoring the Situation of Children and Women, Infant feeding patterns by country. December 2008 [cited 2009 2 February]; Available at: http://www.childinfo.org/breastfeeding_infantfeeding.html
- 5. République du Sénégal (2001) Décret n°2001‐770 du 05/10/2001 Relatif à la Cellule de Lutte contre la Malnutrition.
- 6. Université Cheikh Anta Diop de Dakar – Sénégal, Faculté des Sciences et Techniques, Département de Biologie Animale, Laboratoire de Nutrition (2009) Master en nutrition et alimentation humaine, Plan stratégique (2009–2015).
- 7. Wuehler S.E., Hess S.Y. & Brown K.H. (2011) Accelerating improvements in nutritional and health status of young children in the Sahel region of Sub‐Saharan Africa: review of international guidelines on infant and young child feeding and nutrition. Maternal & Child Nutrition 7 (Suppl. 1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gartner A., Maire B., Kameli Y., Traissac P. & Delpeuch F. (2006) Process evaluation of the Senegal‐Community Nutrition Project: an adequacy assessment of a large scale urban project. Tropical Medicine & International Health 11, 955–966. [DOI] [PubMed] [Google Scholar]
- 9. Le Groupement IPS‐Helite, République du Sénégal, Ministère de la Santé et de la Prévention Médicale – Sénégal, United States Agency for International Development (USAID) from the American People, Programme Santé‐ Santé Communautaire, Christian Children's Fund (CCF) et al (2007) Evaluation de base du Projet Santé– Santé Communautaire de L'USAID Rapport de synthese regionale – Région de Kaolak.
- 10. Le Groupement IPS‐Helite, République du Sénégal, Ministère de la Santé et de la Prévention Médicale – Sénégal, United States Agency for International Development (USAID) from the American People, Programme Santé‐ Santé Communautaire, Christian Children's Fund (CCF) et al (2007) Evaluation de base du Projet Santé– Santé Communautaire de L'USAID Rapport de synthese regionale – Région de Kolda.
- 11. Le Groupement IPS‐Helite, République du Sénégal, Ministère de la Santé et de la Prévention Médicale – Sénégal, United States Agency for International Development (USAID) from the American People, Programme Santé– Santé Communautaire, Christian Children's Fund (CCF) et al (2007) Evaluation de base du Projet Santé– Santé Communautaire de L'USAID Rapport de synthese regionale – Région de Louga.
- 12. Le Groupement IPS‐Helite, République du Sénégal, Ministère de la Santé et de la Prévention Médicale – Sénégal, United States Agency for International Development (USAID) from the American People, Programme Santé‐ Santé Communautaire, Christian Children's Fund (CCF) et al (2007) Evaluation de base du Projet Santé– Santé Communautaire de L'USAID Rapport de synthese regionale – Région de Thies.
- 13. Le Groupement IPS‐Helite, République du Sénégal, Ministère de la Santé et de la Prévention Médicale – Sénégal, United States Agency for International Development (USAID) from the American People, Programme Santé‐ Santé Communautaire, Christian Children's Fund (CCF) et al (2007) Evaluation de base du Projet Santé– Santé Communautaire de L'USAID Rapport de synthese regionale – Région de Ziguinchor.
- 14. Le Groupement IPS‐Helite, République du Sénégal, Ministère de la Santé et de la Prévention Médicale – Sénégal, United States Agency for International Development (USAID) from the American People, Programme Santé‐ Santé Communautaire, Christian Children's Fund (CCF) et al (2007) Evaluation de base du Projet Santé– Santé Communautaire de L'USAID Rapport National, Juillet.
- 15. Simondon K.B., Costes R., Delaunay V., Diallo A. & Simondon F. (2001) Children's height, health and appetite influence mothers' weaning decisions in rural Senegal. International Journal of Epidemiology 30, 476–481. [DOI] [PubMed] [Google Scholar]
- 16. Guiro A.T., Mbacké M., AGETIP . (1994) Etude des habitudes alimentaires des populations cibles du Projet de Nutrition Communautaire au Sénégal.
- 17. Guiro A.T., Diop B., United Nations Children's Fund (UNICEF), Université Cheikh Anta Diop de Dakar – Sénégal. Evaluation de la situation nutritionnelle et al (1990) imentaire du jeune enfant Sénégalais (0–5 ans). Influence des facteurs socio économiques et culturels. Rapport final.
- 18. Garenne M., Maire B., Fontaine O. & Briend A. (2006) Distributions of mortality risk attributable to low nutritional status in Niakhar, Senegal. Journal of Nutrition 136, 2893–2900. [DOI] [PubMed] [Google Scholar]
- 19. Simondon K.B., Delaunay V., Diallo A., Elguero E. & Simondon F. (2003) Lactational amenorrhea is associated with child age at the time of introduction of complementary food: a prospective cohort study in rural Senegal, West Africa. The American Journal of Clinical Nutrition 78, 154–161. [DOI] [PubMed] [Google Scholar]
- 20. Simondon K.B., Diallo A. & Simondon F. (2000) Breastfeeding and growth in rural Senegalese toddlers. Advances in Experimental Medicine and Biology 478, 173–181. [DOI] [PubMed] [Google Scholar]
- 21. Simondon K.B., Simondon F., Simon I., Diallo A., Benefice E., Traissac P. et al (1998) Preschool stunting, age at menarche and adolescent height: a longitudinal study in rural Senegal. European Journal of Clinical Nutrition 52, 412–418. [DOI] [PubMed] [Google Scholar]
- 22. Mane N.B., Simondon K.B., Diallo A., Marra A.M. & Simondon F. (2006) Early breastfeeding cessation in rural Senegal: causes, modes, and consequences. The American Journal of Public Health 96, 139–144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Simondon K.B. & Simondon F. (1997) Age at introduction of complementary food and physical growth from 2 to 9 months in rural Senegal. European Journal of Clinical Nutrition 51, 703–707. [DOI] [PubMed] [Google Scholar]
- 24. Ntab B., Simondon K.B., Milet J., Cisse B., Sokhna C., Boulanger D. et al (2005) A young child feeding index is not associated with either height‐for‐age or height velocity in rural Senegalese children. Journal of Nutrition 135, 457–464. [DOI] [PubMed] [Google Scholar]
- 25. Commission National de Lutte Contre la Malnutrition (CNLCM), Ministère de la Santé et de la Prévention – Sénégal, Programme de Renforcement de la Nutrition (PRN) (2001) Normes et protocoles des services de nutrition.
- 26. République du Sénégal, Ministère de la Santé et de la Prévention – Sénégal, Direction de la Santé– Sénégal, World Health Organization (WHO), United States Agency for International Development (USAID) from the American People, BASICS II – Programme Sénégal et al (2003) Prise en charge intégrée des maladies de l'enfant: Conseiller la mère.
- 27. Christian Children's Fund (CCF), United States Agency for International Development (USAID) from the American People, CANAH II project (n.d.) Rapport global d'exécution du projet CANAH II.
- 28. Ministère de la Santé et de la Prévention Médicale – Sénégal (2001) Préparation à la semaine mondiale de l'allaitement maternel, note technique.
- 29. Ministère de l'Economie des Finances at du Plan, Direction de la Prévention et de la Statistique (1993) Enquête Demographique et de la Santé au Sénégal (EDS II) 1992/3. Macro International Inc.: Calverton, MD. [Google Scholar]
- 30. Ministère de l'Economie des Finances at du Plan – Sénégal, Direction de la Prévention et de la Statistique – Sénégal, Division des Statistiques Démographiques – Sénégal, Demographic and Health Surveys, Macro International Inc. , Ndiaye S. et al (1997) Enquête Demographique et de la Santé au Sénégal (EDS III). Macro International Inc : Calverton, MD. [Google Scholar]
- 31. République du Sénégal, Ministère de la Santé et de la Prévention Médicale – Sénégal, Centre de Recherche pour le Développement Humain , Ndiaye S., Ayad M., ORC Macro (2005) Enquête Démographique et de la Santé Sénégal. ORC Macro.
- 32. Primature – Cellule de Lutte contre la Malnutrition. Programme de Renforcement de la Nutrition (PRN) (2006) Synthèse des résultats des enquêtes sur les connaissances, pratiques et couverture (CPC) des zones d'intervention du Programme de Renforcement de la Nutrition. Juin.
- 33. United States Agency for International Development (USAID) from the American People, BASICS – Programme Sénégal (2007) USAID/BASICS SENEGAL PROGRAM (1994–2006).
- 34. Aubel J., Touré I., Diagne M., Projet CANAH, Christian Children's Fund (CCF), Ministère de la Santé et de l'Action Sociale – Sénégal (2002) La stratégie d'éducation nutritionnelle avec les grands‐mères draft.
- 35. Republique du Sénégal, Ministère de la Santé et de la Prevention Médicale – Sénégal, Direction de la Santé– Sénégal, Division de l'Alimentation de la Nutrition et de la Survie de l'Enfant (DANSE) (2004) Formation en PCIME – C (Prise en Charge Intégrale des Maladies de l'Enfant au niveau Communautaire): Guide du facilitateur pour la formation des relais, avril 2004, version 1.
- 36. Republique du Sénégal, Ministère de la Santé et de la Prevention Médicale – Senegal, Direction de la Santé– Sénégal, Division de l'Alimentation de la Nutrition et de la Survie de l'Enfant (DANSE) (2004) Cahier du relais PCIME – C (Prise en Charge Intégrale des Maladies de l'Enfant au niveau Communautaire).
- 37. World Health Organization (WHO), United Nations Children's Fund (UNICEF), International Food Policy Research Institute (IFPRI), University of California Davis – Program in International and Community Nutrition (UCDavis), Food and Nutrition Technical Assistance (FANTA), Academy for Educational Development (AED) et al (2008) Indicators for assessing infant and young child feeding practices: Part I Definitions. Geneva.
- 38. World Health Organization (WHO), United Nations Children's Fund (UNICEF), International Food Policy Research Institute (IFPRI), University of California Davis – Program in International and Community Nutrition (UCDavis), Food and Nutrition Technical Assistance (FANTA), Academy for Educational Development (AED) et al (2010) Indicators for assessing infant and young child feeding practices, Part III Country Profiles. Geneva.
- 39. République du Sénégal, Ministère de la Santé et de la Prévention – Sénégal, Direction de la Santé (DS) – Sénégal (2004) Directives pour l'administration de la vitamine A en routine.
- 40. Cisse D., Helen Keller International (HKI), United Nations Children's Fund (UNICEF) (2005) Opérationnalisation des directives pour l'administration de la vitamine A en routine (Elaboration de plans de mise en œuvre de la routine au Sénégal).
- 41. République du Sénégal, Comité Sénégalais pour la fortification des aliments en micronutriments (2006) Plan Stratégique pour la Fortification des Aliments en Micronutriments au Sénégal (PSFAMS) 2006–2011.
- 42. Institute Technologie Alimentaire (ITA), Université Cheikh Anta Diop de Dakar Faculté des Sciences et Techniques Laboratoire de Physiologie‐Département de Biologie Animale, Helen Keller International (HKI), Micronutrient Initiative (MI) (2006) Rapport d'étude FRAT (Sénégal) Etude d'identification des aliments vecteurs susceptible d'être enrichis à grande échelle en micronutriments au Sénégal.
- 43. World Health Organization (WHO), Food and Agriculture Organization of The United Nations (FAO) (2004) Vitamin and mineral requirements in human nutrition. 2nd edn. World Health Organization: Geneva. [Google Scholar]
- 44. République du Sénégal, Ministère de la Santé et de la Prévention – Sénégal, Direction de la Santé– Sénégal, Division de l'Alimentation de la Nutrition et de la Survie de l'Enfant (DANSE), Programme National de Lutte Contre le Paludisme (PNLCP) (2008) Compte rendu reunion evaluation des JLS, JSE et MILDA, 24 juillet.
- 45. République du Sénégal, Ministère de la Santé de l'Hygiène et de la Prévention (MSHP) – Sénégal (2003) Guide du facilitateur (draft/post test) Manuel de formation des relais en PCIME‐C.
- 46. Primature – Cellule de Lutte contre la Malnutrition. Programme de Renforcement de la Nutrition (PRN) (2006) Plan stratégique phase II. 2007–2011.
- 47. BASICS II – Programme Sénégal (2004) Evaluation rapide du Paquet d'Activité Intégrées de Nutrition ‘PAIN’ et de la Prise en Charge des Maladies de l'Enfant.
- 48. Christian Children's Fund (CCF) (2006) Community Actions against Malnutrition I. Action Communautaire contre la Malnutrition à Mbour CAMA – MBOUR.
- 49. Primature – Cellule de Lutte contre la Malnutrition. Programme de Renforcement de la Nutrition (PRN) (2006) Rapport d'achèvement phase I (2002–2006).
- 50. République du Sénégal, Ministère de la Santé de l'Hygiène et de la Prévention (MSHP) – Sénégal, Division de l'Alimentation de la Nutrition et de la Survie de l'Enfant (DANSE) .(2008) Protocole de prise en charge de la malnutrition aiguë.
- 51. Cisse D., Baker S.K., Flach M., Gueye A.L., Gaye Y., Guidetti F. et al (2009) Shifting financial support for the vitamin a supplementation (VAS) program from external donors to national sources did not reduce coverage in Senegal. Micronutrient Forum. Beijing.
- 52. Aguayo V.M., Garnier D. & Baker S.K. (2007) Drops of Life: Vitamin A Supplementation for Child Survival. Progress and Lessons Learned in West and Central Africa. UNICEF Regional Office for West and Central Africa: Dakar.
- 53. Rankins J., Green N.R., Tremper W., Stacewitcz‐Sapuntzakis M., Bowen P. & Ndiaye M. (1993) Undernutrition and vitamin A deficiency in the Department of Linguere, Louga Region of Senegal. The American Journal of Clinical Nutrition 58, 91–97. [DOI] [PubMed] [Google Scholar]
- 54. République du Sénégal, Ministère de la Santé et de la Prévention Médicale – Sénégal, Direction de la Santé (DS) – Sénégal, Division de l'Alimentation de la Nutrition et de la Survie de l'Enfant (DANSE), Programme National de Nutrition – Sénégal (2006) Politique nationale pour l'alimentation du nourrisson et du jeune enfant.
- 55. République du Sénégal, Ministère de la Santé et de la Prévention – Sénégal, Division de l'Alimentation de la Nutrition et de la Survie de l'Enfant (DANSE), Université Cheikh Anta Diop de Dakar Faculté des Sciences et Techniques Laboratoire de Physiologie – Département de Biologie Animale (UCAD), Groupe Institut de Pédiatrie Sociale et Institut de Population Développement et de Santé de la Reproduction (GIPS‐IPDSR), United Nations Children's Fund (UNICEF) et al (2008) Analyse situationnelle pour l'introduction des nouvelles directives (SRO‐NF et Zinc) dans la prise en charge de la diarrhee au Sénégal, Rapport final.
- 56. Ellis A.A., Winch P., Daou Z., Gilroy K.E. & Swedberg E. (2007) Home management of childhood diarrhoea in southern Mali – implications for the introduction of zinc treatment. Social Science & Medicine 64, 701–712. [DOI] [PubMed] [Google Scholar]
- 57. Ministère de la Santé et de la Prévention – Sénégal, Division de l'Alimentation de la Nutrition et de la Survie de l'Enfant (DANSE). (n.d.) Stratégie Nationale IEC sur la Survie de l'Enfant/Plan Intégré de Communication (PIC).
- 58. République du Sénégal, Ministère de la Santé– Sénégal, Division de la Santé de la Reproduction (DSR) – Sénégal, United Nations Population Fund (UNFPA) (2007) Protocoles de services de la santé de la réproduction.
- 59. Wone I., Plan International – Sénégal (2008) Evaluation final du Projet Survie de l'Enfant PLAN PLAN/NNO dans le district sanitaire de Louga.
- 60. Ministère de la Santé de l'Hygiène et de la Prévention (MSHP) – Sénégal, Direction de la Santé (DS) – Sénégal, Division de l'Alimentation et de la Nutrition – Sénégal, BASICS II – Programme Sénégal, United States Agency for International Development (USAID) from the American People (2002) Le Paquet d'Activités Intégrées de Nutrition (P.A.I.N.) (Document d'orientation).
- 61. Helen Keller International (HKI) , Tendeng C.A. (n.d.) Protocole de réhabilitation nutritionnelle des PVVIH malnutries avec le Plumpy Nut.
- 62. Fortitech Strategic Nutrition (2006) Réponse à l'appel d'offre pour la livraison de prémixe de micronutriments avec assistance technique en Afrique de l'Ouest Francophone commençant l'enrichissement des farines de céréales (Response to the bid for the supply of micronutrient premix with technical assistance in Francophone West Africa embarking on cereal flour fortification).
- 63. Université Cheikh Anta Diop de Dakar Faculté des Sciences, Techniques Laboratoire de Physiologie – Département de Biologie Animale , Sall M.G., Diarra D.Z. (2007) Evaluation de l'impact de l'iodation du sel sur la prevalence des T.D.C.I. et l'impact du deparasitage sur la prévalence de l'anémie dans les régions de Tambacounda et de Kolda Sénégal.
- 64. République du Sénégal, Ministère de la Santé et de la Prévention Médicale – Sénégal, United Nations Children's Fund (UNICEF), World Health Organization (WHO) (2007) Plan stratégique pour la survie de l'enfant (2008–2015).
- 65. République du Sénégal (2008) Stratégie Nationale de Sécurité Alimentaire du Sénégal, document principal, janvier.
- 66. Sylla A., Diouf S., Sall M.G., Ndiaye O., Moreira C. & Kuakuvi N. (2002) [Epidemiology and management of malnutrition in hospitalized children 0–5 years of age in Dakar]. Archives of Pediatrics 9, 101–102. [DOI] [PubMed] [Google Scholar]
- 67. Diop E.H.I., Dossou N.I., Ndour M.M., Briend A. & Wade S. (2003) Comparison of the efficacy of a solid ready‐to‐use food and a liquid, milk‐based diet for the rehabilitation of severely malnourished children: a randomized trial. The American Journal of Clinical Nutrition 78, 302–307. [DOI] [PubMed] [Google Scholar]
- 68. Idohou‐Dossou N., Wade S., Guiro A.T., Sarr C.S., Diaham B., Cisse D. et al (2003) Nutritional status of preschool Senegalese children: long‐term effects of early severe malnutrition. The British Journal of Nutrition 90, 1123–1132. [DOI] [PubMed] [Google Scholar]
- 69. Donnen P., Sylla A., Dramaix M., Sall G., Kuakuvi N. & Hennart P. (2007) Effect of daily low dose of vitamin A compared with single high dose on morbidity and mortality of hospitalized mainly malnourished children in Senegal: a randomized controlled clinical trial. European Journal of Clinical Nutrition 61, 1393–1399. [DOI] [PubMed] [Google Scholar]
- 70. World Health Organization Secretariat on behalf of the participants to the Consultation. (2007) Conclusions and recommendations of the WHO Consultation on prevention and control of iron deficiency in infants and young children in malaria endemic areas, Lyon, France, 12–14 June 2006. Food and Nutrition Bulletin 28, S621–S627. [DOI] [PubMed] [Google Scholar]
- 71. République du Sénégal, Primature du Sénégal, Cellule de Lutte contre la Malnutrition (CLM) – Sénégal (2007) Etude d'impact rapport final, février.
- 72. Marek T., Diallo I., Ndiaye B. & Rakotosalama J. Successful contracting of prevention services: fighting malnutrition in Senegal and Madagascar. Health Policy Plan 1999; 14, 382–389. [DOI] [PubMed] [Google Scholar]
- 73. Ministère de la Santé de l'Hygiène et de la Prévention – Sénégal, Direction de la Santé (DS) – Sénégal, Division SIDA/IST – Sénégal, Conseil National de Lutte Contre le SIDA (CNLS) – Sénégal (2005) Politique Nationale de Prévention de la transmission Mère‐Enfant au VIH au Sénégal. Juillet.
- 74. Ministère de la Santé de l'Hygiène et de la Prévention (MSHP) – Sénégal, Division de la Santé de la Reproduction (DSR) – Sénégal (2007) Politiques et normes de services de la santé de la reproduction.
- 75. World Health Organization (WHO) (2009) Rapid Advice: Antiretroviral Therapy for HIV Infection in Adults and Adolescents. World Health Organization: Geneva. [Google Scholar]
- 76. World Health Organization (WHO) (2009) Rapid advice: revised WHO principles and recommendations on infant feeding in the context of HIV.
- 77. République du Sénégal, Ministère de la Santé et de la Prévention Médicale – Sénégal, Conseil National de Lutte Contre le SIDA (CNLS) – Sénégal, United States Agency for International Development (USAID) from the American People, Catholic Relief Services (CRS), Helen Keller International (HKI) (2006) Enquête de base sur les connaissance et pratiques nutritionnelles des PVVIH et des prestataires impliqués dans la prise en charge au niveau des structures sanitaires et communautaires, Synthèse des résultats en direction des agences d'exécution.
- 78. WHO Collaborative Study Team on the Role of Breastfeeding on the Prevention of Infant Mortality (2000) Effect of breastfeeding on infant and child mortality due to infectious diseases in less developed countries: a pooled analysis. Lancet 355, 451–455. [PubMed] [Google Scholar]
- 79. Garenne M. & Fontaine O. (eds) (1986) Assessing Probable Causes of Deaths Using a Standardized Questionnaire: A Study in Rural Senegal. Clarendon Press: Oxford. [PMC free article] [PubMed] [Google Scholar]
- 80. République du Sénégal, Ministère de l'Hygiène et de la Prévention – Sénégal, Division de l'Alimentation de la Nutrition et de la Survie de l'Enfant (DANSE) (2004) Documentation de la PCIME: experiences, progres et lecons apprises au Sénégal Draft.
- 81. Ministère de la Santé de l'Hygiène et de la Prévention (MSHP) – Sénégal, Direction de la Santé– Sénégal, Division SIDA/IST – Sénégal, Conseil National de Lutte contre le SIDA (CNLS) – Sénégal, Family Health International (FHI), United States Agency for International Development (USAID) from the American People (2005) Prévention de la transmission mère‐enfant au VIH au Sénégal.
- 82. Ministère de la Santé de l'Hygiène et de la Prévention – Sénégal, Direction de la Santé (DS) – Sénégal, Division SIDA/IST – Sénégal, Conseil National de Lutte Contre le SIDA (CNLS) – Sénégal, United States Agency for International Development (USAID) from the American People, Family Health International (FHI) (2005) Cours de formation en Counseling Dépistage volontaire Anonyme et Counseling Prévention Transmission Mére‐Enfant. Guide du Participant.
- 83. United States Agency for International Development (USAID) from the American People, Catholic Relief Services (CRS), Counterpart, ‘fhi’ Family Health International, OPAIS Sénégal, Division SIDA/IST – Sénégal et al (n.d.) Paquet Intégré de Services Essentiels de Nutrition pour les PVVIH (PISEN) Aide mémoire pour le prestataires.
- 84. Ministère de la Santé et de la Prévention Médicale – Sénégal, Division SIDA/IST – Sénégal, SANNI , Dia S., Wane Y., World Fund et al (2007) Rapport de la revue du programme national de prevention de la transmission mère‐enfant du VIH.
- 85. World Food Programme of the United Nations (WFP) (2006) Country Programme Senegal (2007–2011).
- 86. République du Sénégal, Vulnerability Analysis and Mapping Unit of the World Food Programme of the United Nations (2003) La vulnérabilité structurelle à l'insécurité alimentaire en milieu rural Sénégal (Vulnerability Analysis and Mapping – VAM).
- 87. République du Sénégal, Ministère de l'Economie des Finances – Sénégal, Direction de la Prévention et de la Statistique – Sénégal (2004) Rapport de synthèse de la deuxième Enquête Sénégalaise Auprès des Ménages (ESAM‐II).
- 88. République du Sénégal, Ministère du Développement Rural et de l'Agriculture – Sénégal, Direction de l'Analyse de la Prévision et des Statistiques – Sénégal, Division des Statistiques Documentation et Information Agricole – Sénégal (2007) Bilan alimentaire 2006.
- 89. République du Sénégal, Direction de l'Analyse de la Prévision et des Statistiques – Sénégal, Direction de l'Elevage le Commissariat à la Sécurité Alimentaire du Ministère de la Famille – Sénégal, Agence Nationale de la Statistique et de la Démographie du Ministère des Finances – Sénégal, Centre de Suivi Ecologique du Ministère de l'Environnement – Sénégal, Secrétariat Exécutif du Conseil National de Sécurité Alimentaire (SE/CNSA) et al (2008) Evaluation sur la Sécurité Alimentaire au Sénégal – Rapport Final.
- 90. Paquet Intégré de Conseil (PIC), Agir pour Sauver, Ministère de la Santé et de la Prévention Médicale – Sénégal, United States Agency for International Development (USAID) from the American People, BASICS II – Programme Sénégal, Helen Keller International (HKI) et al (n.d.) Paquet d'Actions Essentielles pour la Survie de l'Enfant: Aide mémoire pour les agents de santé.
- 91. République du Sénégal, MSAS – Sénégal, Ministère du Commerce et de l'Artisanat (MCA) – Sénégal (2004) Analyse/Arrête interministériel fixant les conditions de commercialisation des substituts ou lait maternel. No 005969/ MSAS/ MCA.
- 92. Sarr F., Primature – Cellule de Lutte contre la Malnutrition. Programme de Renforcement de la Nutrition (PRN) (2005) Etude sur la satisfaction des bénéficiaires. Rapport final. Juin 2005.
- 93. République du Sénégal, Ministère de la Santé– Sénégal, Direction de la Santé– Sénégal, Division de l'Alimentation de la Nutrition et de la Survie de l'Enfant (DANSE) (2005) L'Alimentation du Nourrisson et du Jeune Enfant (ANJE) Evaluation nationale des pratiques, des politiques et des programmes.
- 94. République du Sénégal, Ministère de la Santé et de la Prevention Médicale – Sénégal, Direction de la Santé– Sénégal, Division de l'Alimentation de la Nutrition et de la Survie de l'Enfant (DANSE), World Health Organization (WHO), Management Sciences for Health (MSH) et al (2007) Rapport de l'évaluation de la qualité de la prise en charge des enfants de moins de cinq ans dans les structures de santé de premier niveau au Sénégal.
- 95. République du Sénégal, Food and Agriculture Organization of the United Nations (FAO) (2007) Profil nutritionel de pays: République du Sénégal Draft.
- 96. Wuehler S.E. & Ouedraogo A.W. (2011) Situational analysis of infant and young child nutrition‐related activities in Burkina Faso. Maternal & Child Nutrition 7 (Suppl. 1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Wuehler S.E. & Djasndibye N. (2011) Situational analysis of infant and young child nutrition‐related activities in Chad. Maternal & Child Nutrition 7 (Suppl. 1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Wuehler S.E. & Coulibaly M. (2011) Situational analysis of infant and young child nutrition‐related activities in Mali. Maternal & Child Nutrition 7 (Suppl. 1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Wuehler S.E. & Ould Dehah C.M.E.H. (2011) Situational analysis of infant and young child nutrition‐related activities in Mauritania. Maternal & Child Nutrition 7 (Suppl. 1), this issue. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Wuehler S.E., Biga Hassoumi A., Hess S.Y. & Brown K.H. (2010) Situational analysis of infant and young child nutrition‐related activities in Niger. Maternal & Child Nutrition 7 (Suppl. 1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Primature du Sénégal, Cellule de Lutte contre la Malnutrition (CLM) – Sénégal (2007) Programme de Renforcement de la Nutrition (PRN). Communication Interpersonnelle (CIP) Cahier illustré du relais.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Senegal summary data
Supporting info item


