Abstract
Choosing an infant feeding mode is complex for human immunodeficiency virus (HIV)‐infected African women. We documented infant feeding choices by 811 mothers of infants aged less than 18 months enrolled in the Chilenje Infant Growth, Nutrition and Infection Study of fortified complementary or replacement foods. We also conducted 20 interviews and 4 focus group discussions among women and nurses to explore the issues in depth. Practices of most HIV‐infected women did not closely follow national or international guidelines: 26% never initiated breastfeeding, and 55% were not breastfeeding by 6 months post partum. Women of lower socio‐economic status and those not meeting criteria for safe replacement feeding were more likely to initiate breastfeeding, to continue longer and to stop at 6 months when provided with free food within the trial. Most HIV‐negative women and women of unknown HIV status continued breastfeeding into the infant's second year, indicating limited ‘spillover’ of infant feeding messages designed for HIV‐infected women into the uninfected population. Qualitative work indicated that the main factors affecting HIV‐infected women's infant feeding decisions were the cost of formula, the advice of health workers, influence of relatives, stigma and difficulties with using an exclusive feeding mode. Rapidly changing international recommendations confused both mothers and nurses. Many HIV‐infected women chose replacement feeding without meeting criteria to do this safely. Women were influenced by health workers but, for several reasons, found it difficult to follow their advice. The recently revised international HIV and infant feeding recommendations may make the counselling process simpler for health workers and makes following their advice easier for HIV‐infected women.
Keywords: HIV, breastfeeding, infant, Zambia
Introduction
Human immunodeficiency virus (HIV)‐infected mothers in sub‐Saharan Africa face challenges at different stages of infant feeding. International HIV and infant feeding guidelines have changed rapidly (World Health Organization 1992; UNAIDS/UNICEF/WHO 1998; World Health Organization 2007b, 2009) over the years since HIV was detected in the breast milk of HIV‐positive mothers (Thiry et al. 1985) and since mother‐to‐child HIV transmission through breast milk was confirmed (Ziegler et al. 1985). Guidelines have rightly been changed in response to research findings, but it has been hard for mothers and healthcare staff advising them to keep up with and interpret changing recommendations. A review of programmatic experience by the World Health Organization (WHO)/United Nations Children's Fund found a number of shortcomings in the coverage and quality of infant feeding counselling and support in most prevention of mother‐to‐child transmission programmes (World Health Organization 2007a). Inadequate infant feeding counselling was found in programmes in Kenya, Malawi and Zambia (Chopra et al., 2009). Mothers may therefore be confused about what feeding mode is best for their infants.
Approximately a fifth of pregnant women in Zambia are infected with HIV (Central Statistical Office et al. 2009). The Baby Friendly Hospital Initiative started in the country in 1997, and exclusive breastfeeding rates in the first 6 months of life increased from 26% in 1996 to 41% in 2002 (Zambian National Food and Nutrition Commission 2007). Lusaka District Health provides primary healthcare for the capital and has been proactive in implementing changing mother‐to‐child transmission guidelines as they arise (Stringer et al., 2003). Pregnant women are provided with HIV testing and counselling as part of routine antenatal care. Provision of antiretrovirals during late pregnancy and at delivery means that the post‐natal period is the major period of HIV transmission (Breastfeeding and HIV International Transmission Study Group 2004). Midwives provide infant feeding counselling to HIV‐infected mothers. Mothers may also get infant feeding information from radio, television and pamphlets given out by health institutions. Local guidelines (Zambian National Food and Nutrition Commission 2007) are that HIV‐infected mothers should breastfeed exclusively from birth to 6 months or replace breastfeeding completely by giving formula from birth. While conducting a trial of replacement foods for infants after 6 months, the Chilenje Infant Growth, Nutrition and Infection Study (CIGNIS), we noted that breastfeeding practice of many of the HIV‐infected mothers in the study appeared far from what was recommended. Most of the women had access to the Lusaka city treated water supply, but that is not considered in itself sufficient to recommend replacement feeding from birth. Women also require adequate sanitation, sufficient finances, family support and knowledge of how to prepare alternative foods (Doherty et al., 2007; World Health Organization 2009). The study was conducted to investigate to what extent the CIGNIS women's infant feeding choices reflected the recommendations, based on socio‐economic data collected as part of the trial. In order to understand their choices in more detail and to determine interventions to improve infant feeding practices among HIV‐infected women, we conducted qualitative research related to infant feeding choices.
Key messages
-
•
Rapidly changing international guidelines regarding maternal HIV and infant feeding have confused mothers and healthcare staff, resulting in many choices that are not ideal for infant health.
-
•
Women's meeting criteria to safely replacement‐feed was not closely related to their actual feeding choices.
Materials and methods
Study site
Women were recruited to the CIGNIS trial and to the qualitative component of the current study from among mothers attending the child health section of the Chilenje government clinic on the same site as the CIGNIS project clinic in Lusaka, Zambia. Attendance for antenatal care at Lusaka government clinics is very high. Pregnant women are tested for HIV infection on the first day of attendance, and results are available on the same day, although not all mothers return for their results. Women who are HIV‐infected are counselled by midwives regarding infant feeding (Zambian National Food and Nutrition Commission 2007).
The study was approved by the ethics committees of the University of Zambia and the London School of Hygiene and Tropical Medicine. Written consent was obtained from all participants in both quantitative and qualitative components. Both components of the study were held in the project clinic, which is known as working on maternal and child nutrition, not specifically HIV, so there is little or no stigma. Interviews and focus group discussions (FGDs) were held in a private room within the clinic.
Quantitative component
We used data collected from participants in the CIGNIS study, a randomized, double‐blind, controlled trial, conducted from October 2005 to July 2009, comparing two locally made infant foods given from age 6 months to age 18 months for their effects on growth and morbidity (registered as ISRCTN37460449, http://www.controlled-trials.com/mrct). The inclusion criteria were infant aged 6 months, resident in Chilenje, mother willing to comply with study procedures including child HIV testing and informed consent. The current study includes 68 additional children who were excluded from the primary analysis of the randomized trial (Chilenje Infant Growth Nutrition and Infection (CIGNIS) Study Team, 2010).
Women and infants were recruited when infants were 6 months old and followed until the infant was 18 months. At monthly visits, women were asked if they were still breastfeeding and, if not, when they had stopped. Data on the exclusivity of early breastfeeding were not collected.
We assessed a woman's likely ability to replacement‐feed safely based on socio‐economic data collected at enrolment. Those who had at least secondary school education, either the woman or her partner was employed or self‐employed, had a private indoor or outdoor toilet, had electricity in the home and whose household water came from either a tap to the Lusaka District water supply or a borehole were considered to meet the criteria for safe replacement feeding. We also used an overall measure of socio‐economic status (SES) based on an asset index, created by combining data on possessions and housing characteristics (Filmer & Pritchett 2001). We did not have information on two other related criteria for safe replacement feeding: family support and disclosure of the woman's HIV status to her partner (Doherty et al., 2007; World Health Organization 2009).
Breastfeeding duration was evaluated using Kaplan–Meier curves, stratified by maternal HIV and by SES, and meeting the criteria for safe replacement feeding. Log‐rank tests were used to test for equality of the survivor function. Person‐years at risk was calculated from the child's date of birth until the earliest of date of stopping breastfeeding or exit from trial. For women who stopped breastfeeding before enrolment, the date of stopping was estimated based on the child's age at which they reported stopping. For women who stopped breastfeeding after enrolment, the date of stopping was estimated based on the date of the monthly visit and the number of days the woman had breastfeed in the previous month.
Qualitative component
This component was conducted in 2009 to explore further issues arising from the quantitative component. Participants in the qualitative component consisted of a purposive sample of mothers who knew their HIV test results during antenatal care. Some of the women had participated in the CIGNIS trial, and others had come to the Chilenje government clinic for child growth monitoring or family planning. Twenty in‐depth interviews were conducted with HIV‐infected mothers. Four FGDs were conducted: two with HIV‐infected mothers, one with HIV‐uninfected mothers and one with the midwives (counsellors) from the Mother and Child Health department and labour ward of the Chilenje clinic. Each FGD had 7–10 participants. Recruitment ceased when information obtained reached saturation, i.e. no new information was forthcoming.
Interviews and FGDs were conducted by two of the authors (MC and JS) who are qualified health workers and have experience in qualitative interviewing. Each interview lasted 30 to 40 min, and FGDs lasted about 1 h and 15 min. Interview guides (Box 1) were used to explore what determines infant feeding choices for HIV‐infected mothers. Open‐ended questions were used to allow participants to freely express their views. In Lusaka, many people move freely through conversation in English and the two main local languages, Nyanja and Bemba; the interviewers were fluent in all these languages.
Box 1. Topic guide for FGDs and in‐depth interviews
| Women's FGDs | Nurses' FGDs | Interviews | |
|---|---|---|---|
| What do you know about breastfeeding? | x | x | x |
| What do you know about prevention of mother‐to‐child HIV transmission? | x | x | x |
| Did you share with anyone your HIV test results? If yes, whom did you share them with? | x | x | |
| Are there mothers who are not breastfeeding, and if so, what are the reasons for not breastfeeding? | x | x | |
| What information is given about infant feeding at the clinic? | x | x | x |
| At what stage is the infant feeding counselling done? | x | x | x |
| If mothers choose not to breastfeed, what should they feed their infants? | x | x | x |
| When mothers make a choice of replacing breastfeeding, how do the health personnel follow up to find out if the replacement feeding is acceptable, feasible, affordable, sustainable and safe for them and their infants? | x |
HIV, human immunodeficiency virus; FGD, focus group discussion.
FGDs and interviews were audio‐taped and transcribed verbatim. The two interviewers then agreed translation into English of sections of the transcripts in Nyanja or Bemba. Thematic data analysis was conducted manually by the two independently (Green & Thorogood 2004). Analysis involved identifying key categories and recurrent themes. The two researchers then jointly reviewed emerging themes and debated until agreement was reached.
Results
Quantitative component
Table 1 shows demographic and some socio‐economic variables of women in the CIGNIS study, subdivided by their antenatal HIV status. Breastfeeding duration of HIV‐infected women differed greatly from that of HIV‐uninfected women and women of unknown status (Fig. 1). Twenty‐six per cent of HIV‐infected women never initiated breastfeeding, and 55% were not breastfeeding by 6 months post partum. By 12 and 18 months, respectively, only 14% and 8% of HIV‐positive mothers were still breastfeeding. The median age of stopping breastfeeding was 3 months.
Table 1.
Demographic and socio‐economic data for the CIGNIS study women
| HIV‐negative mothers | HIV‐positive mothers | HIV‐unknown mothers | |
|---|---|---|---|
| N | 564 | 177 | 70 |
| Age (years) | 25.6 (SD 5.7) | 28.3 (SD 5.4) | 26.1 (SD 5.5) |
| Body mass index (kg/m2) | |||
| <18.5 | 46 (8%) | 12 (7%) | 3 (4%) |
| 18.5–25 | 327 (58%) | 107 (60%) | 40 (57%) |
| 25–30 | 130 (23%) | 43 (24%) | 16 (23%) |
| >30 | 60 (11%) | 15 (8%) | 11 (16%) |
| Education | |||
| Primary or less | 173 (31%) | 71 (40%) | 25 (36%) |
| Secondary | 215 (38%) | 64 (36%) | 30 (43%) |
| College/university | 176 (31%) | 42 (24%) | 15 (21%) |
| Marital status | |||
| Married | 423 (75%) | 128 (72%) | 56 (80%) |
| Single | 119 (21%) | 34 (19%) | 13 (19%) |
| Divorced, separated, widowed | 22 (4%) | 15 (9%) | 1 (1%) |
| Mother's occupation | |||
| Housewife | 286 (51%) | 96 (54%) | 40 (57%) |
| Salaried employee | 111 (20%) | 36 (20%) | 14 (20%) |
| Self‐employed | 53 (9%) | 22 (12%) | 3 (4%) |
| Other | 114 (20%) | 23 (13%) | 13 (19%) |
| Father's occupation | |||
| Salaried employee | 341 (60%) | 97 (55%) | 45 (64%) |
| Self‐employed | 144 (26%) | 59 (33%) | 16 (23%) |
| Unemployed/other/no partner | 79 (14%) | 21 (12%) | 9 (13%) |
| Tertiles of socio‐economic status | |||
| Low | 178 (32%) | 71 (40%) | 22 (31%) |
| Middle | 221 (39%) | 64 (36%) | 26 (37%) |
| High | 165 (29%) | 42 (24%) | 22 (31%) |
| Household toilet type | |||
| Private indoors | 319 (57%) | 84 (47%) | 46 (66%) |
| Private outdoors | 124 (22%) | 37 (21%) | 12 (17%) |
| Other | 121 (21%) | 56 (26%) | 12 (17%) |
| Household water source | |||
| Private tap | 430 (76%) | 120 (68%) | 57 (81%) |
| Communal tap | 129 (23%) | 55 (31%) | 12 (17%) |
| Borehole | 5 (1%) | 1 (0.6%) | 1 (1%) |
| Other | 0 (0%) | 1 (0.6%) | 0 (0%) |
| Electricity in household | |||
| Yes | 87 (15%) | 27 (15%) | 11 (16%) |
| No | 477 (85%) | 150 (85%) | 59 (84%) |
CIGNIS, Chilenje Infant Growth, Nutrition and Infection Study; HIV, human immunodeficiency virus; SD, standard deviation.
Figure 1.
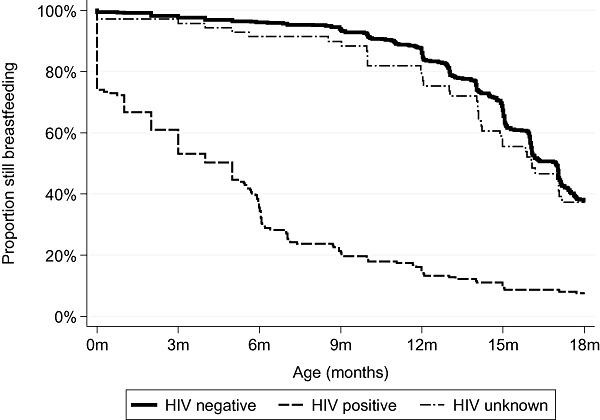
Maternal HIV status and duration of breastfeeding. HIV, human immunodeficiency virus.
In contrast, most HIV‐uninfected and HIV‐unknown women were still breastfeeding at 6 months, and the proportions of these two groups, respectively, still breastfeeding at 12 months were 86% and 79%, and at 18 months were 38% and 37%. The median age of stopping breastfeeding was 15 months among HIV‐uninfected mothers and 14 months among HIV‐unknown mothers.
Of the 177 HIV‐infected women, 76% had at least secondary school education, 92% were either employed or had an employed partner, 68% had a private toilet, 85% had electricity in the home and all but 1 had household water from either a tap to the Lusaka District water supply or a borehole. Combining these, 73 (41%) met all the specified criteria for safe replacement feeding. Women who met the criteria were more likely to have never breastfeed their child (33% vs. 21%, P = 0.08) and had a significantly shorter breastfeeding duration (P = 0.009, log‐rank test; Fig 2a). In addition, there was a significant association between breastfeeding duration and SES (P = 0.02; Fig 2b) with the women in the lowest SES tertile breastfeeding longer.
Figure 2.
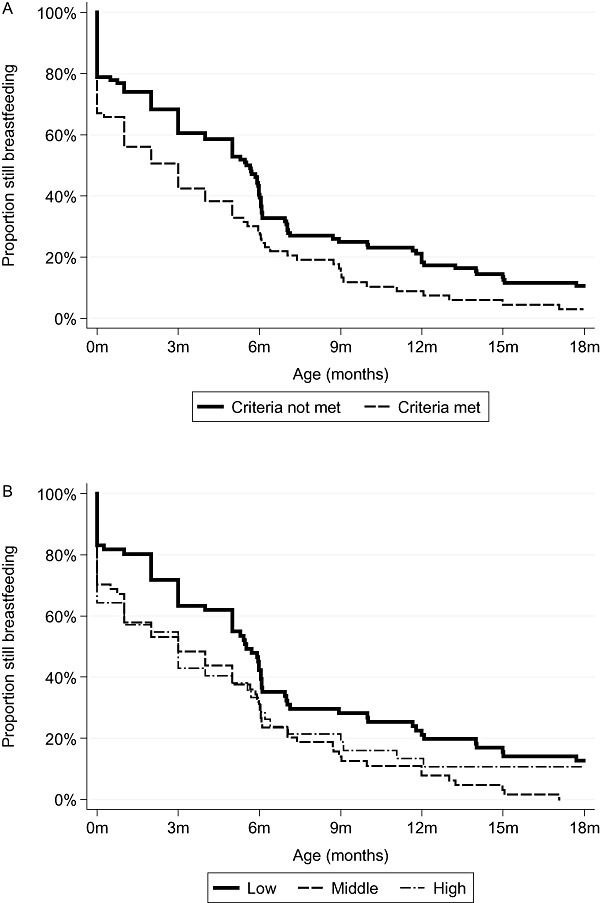
(a) Breastfeeding duration among HIV‐infected women who did (n = 73) or did not (n = 104) meet criteria for replacement feeding. (b) Duration of breastfeeding according to socio‐economic tertile of HIV‐infected mothers. Socio‐economic tertiles were derived from a principal components analysis that included all study women, irrespective of HIV status. P‐value from log‐rank test for the effect on breastfeeding duration of meeting replacement criteria was P = 0.009, and for the effect of socio‐economic tertile was P = 0.02. HIV, human immunodeficiency virus.
There is an inflection point at 6 months in the Kaplan–Meier curves for HIV‐positive women who did not meet the criteria for safe replacement feeding and those in the lowest SES tertile. This inflection indicates that our giving out free food at 6 months for the CIGNIS trial, and suggesting to HIV‐infected women that they should consider stopping breastfeeding, may have had an influence on breastfeeding duration in these subgroups.
Qualitative component
The 20 mothers who participated in interviews were aged between 18 and 36 years, and their children were aged between 9 and 24 months. The mothers reported breastfeeding duration ranging from none to 18 months. Eleven of the 13 who stopped breastfeeding before the infant was 6 months gave infant formula, and the others gave fresh milk or pasteurized commercial milk products for general home use.
All mothers had received antenatal care including HIV counselling and testing and infant feeding counselling from the Chilenje clinic. They knew that HIV could be transmitted through breast milk and knew about the perinatal antiretroviral programme. The results showed five key categories of what determines infant feeding choice for HIV‐infected mothers: cost of formula, influence from health workers, influence from relatives, stigma and not disclosing HIV results and difficulties of maintaining an exclusive feeding mode, i.e. either exclusive breastfeeding or exclusive replacement feeding.
Many mothers [6 out of 20 (30%) of those who participated in in‐depth interviews] indicated that they would have liked to give their babies formula milk as replacement feed immediately after birth but could not because of the cost, so they opted to breastfeed their babies (Box 2). Some women breastfed for more than 6 months. In trying to avoid the cost of appropriate baby formula milk, some fed their babies less nutritious foods such as tea with milk.
Box 2. Comments related to cost of formula
| ‘. . . when I was pregnant I decided that I was not going to breast feed the baby, but when he was born we did not have money (to buy formula milk). How do you stop the child from breastfeeding when you do not have money?’ (interview mother 10) |
| ‘. . . they (mothers) will say sister (nurse) I think I am just going to breastfeed because when I breastfeed the milk has all the nutrients for the baby and I will not be hardened up (bothered) with finances to start buying formula.’ (Nurse, FGD) |
| ‘The milk used to cost K28 000.00 (about $6.00) a tin, now she would finish two tins in a week, so it makes K56 000.00. . . . So we (with husband) said aah!! That is a bit expensive to continue, at least (at) 5 months you know she can eat porridge . . . that is why we stopped her from formula.’ (interview mother 5) |
| ‘. . . I did not know what to do. The father who used to help me died. I had nothing to do but just continue with breastfeeding.’ (interview mother 13). |
| ‘So when I was told that I am HIV‐positive, I chose to breastfeed the children, the first one I did not breastfeed; at a project, they provided formula milk. The second one, the project finished so I changed from milk to tea.’ (HIV‐positive mother, FGD) |
| ‘The choice depends on your health and your financial what . . . accountability . . . how financially successful are you. If you are not able, you are not financially able to buy that milk, it is better you breastfeed the first 6 months.’ (interview mother 9) |
HIV, human immunodeficiency virus; FGD, focus group discussion.
Mothers depend on the advice they get from health workers in guiding their infant feeding choices (Box 3). Health workers are thus key to prevention of mother‐to‐child transmission services. Eight (40%) of the 20 mothers who participated in the interviews demonstrated that the health workers influenced their infant feeding choice. Some counsellors advise or indeed ‘instruct’ mothers which feeding option is suitable for her child rather than just provide information for the mother to have an ‘informed choice’ herself. The rapidly changing infant feeding advice from healthcare staff was confusing to some mothers.
Box 3. Comments related to influence of health workers
| ‘Most of the time we advise them to breastfeed up to 6 months.’ (Nurse, FGD) |
| ‘That is what they told us, that it is better you don't breastfeed the baby if you are found positive.’ (interview mother 1) |
| ‘What they told us is that breast milk has the HIV. Yes that is what they told us so it is better you do not breastfeed.’ (interview mother 11) |
| ‘She said it is up to you but you have to stop breastfeeding at six months. So it is up to you if you want you can stop earlier as long as you give something.’ (interview mother 17) |
| ‘. . . after she said mixing the two is dangerous for the baby . . . so that's when I just made up my mind that let me just choose bottle feeding.’ (interview mother 5) |
| ‘Each time we would have a baby it would die. So we (with husband) decided to do what they (nurses) were teaching at the clinic and that was not to breastfeed.’ (HIV‐positive mother, FGD) |
| ‘There was a certain time when they were promoting breastfeeding here in Zambia saying that bottle (feeding) brings diseases to children. There are certain mothers who still have that in their minds, that feeding bottles bring diseases to children. So even if they are found positive and they know that for this child, I just need to breastfeed only for a certain period of time, that issue they were taught before that feeding bottles bring diseases, diarrhea comes to their mind so they breastfeed. It is confusing us, today breastfeed, tomorrow don't.’ (HIV‐positive mother, FGD) |
HIV, human immunodeficiency virus; FGD, focus group discussion.
Six (30%) of the mothers interviewed indicated that relatives or neighbours influenced their infant feeding practice. Most of the advice from these people contradicted the official recommendations from the health services (Box 4).
Box 4. Comments related to the influence of relatives and neighbours
| ‘Mum is the one who told me [to buy bonnita (pasteurized milk for general home use)] She had kept the child for her boss. They gave milk, bonnita. They never bought tinned milk, grew up with bonnita. This child has even finished school. Yes they were just giving bonnita, fresh milk. It is mum who told me, this is the milk you should give.’ (interview mother 20) |
| ‘There are some grandmothers who are stubborn, cannot be controlled, they know everything. My mother‐in‐law started the child at one week. She started giving porridge.’ (HIV‐negative mother, FGD) |
| ‘So my sister came who said she saw a child of a friend who was drinking bonnita long life. Boil it, add little water and salt. So that is what I gave.’ (HIV‐positive mother, FGD) |
| ‘Breast milk is the best, nutrients in the breast milk. If you choose breastfeeding, this is the best for her (the baby). That is what we (and husband) decided to do. We chose to breastfeed.’ (interview mother 5) |
| ‘Because neighbours will say ‘why is the baby crying? Aah it is milk, only milk – the baby is not getting enough. It is crying a lot because of hunger . . . so give porridge. Even at 1 month or 2 months. Now for HIV‐positive mother that is dangerous.’ (interview mother 5) |
HIV, human immunodeficiency virus; FGD, focus group discussion.
Stigma around HIV and fear of discrimination remain an issue. Stigma prevented HIV‐positive mothers from feeding their infants with the method they wished because choosing replacement feeding would disclose their status (Box 5). Disclosure of HIV status to the woman's partner is usually a condition for successful replacement feeding. However, disclosure of HIV‐positive status to a partner was greatly feared and was an obstacle to choosing the desired infant feeding option by the mother for fear of being victimized by the partner.
Messages about the dangers of mixing breast milk and other foods are understood by many women, but they nevertheless find it difficult to avoid mixed feeding. Both exclusive breastfeeding and exclusive replacement feeding were considered difficult to maintain (Box 6).
Discussion
Many of the HIV‐infected CIGNIS study women's breastfeeding practices were not in line with WHO recommendations. A large proportion, including a fifth of those not meeting the specified criteria for safe replacement feeding, did not initiate breastfeeding, and additional women stopped breastfeeding before the infant was 6 months. Poorer women and those not meeting criteria for safe replacement‐feeding were more likely to initiate breastfeeding and continue longer. The results reflect those found previously in South Africa (Doherty et al., 2007) and suggest confusion among either HIV‐infected women or the nurses advising them. It is good news, however, that most HIV‐uninfected women and those of unknown HIV status breastfed into the second year of the infant's life, indicating there was no major spillover of messages targeted at HIV‐infected women. It is notable that providing free food from 6 months appeared to induce some of the poorest HIV‐infected women, but not other women, to stop breastfeeding. This supports the evidence from the qualitative component that cost of replacement foods was an important consideration for women. In previous research among HIV‐untested women in the community, we showed that providing this food displaced lower quality complementary foods, not breast milk (Owino et al., 2007).
A limitation of the study is that breastfeeding duration before the recruitment to CIGNIS when infants were 6 months old means that estimation of breastfeeding duration before 6 months is less precise than after 6 months when women were seen monthly by project staff. However, we expect that women can accurately recall if they never breastfed and we knew their practice at 6 months, so this does not seem a major limitation.
We designed the qualitative component to further explore the quantitative results. HIV‐positive mothers cited many challenges to choosing an infant feeding option. Mothers understand messages saying that to minimize the chances of a child getting HIV from breast milk, they should exclusively breastfeed for a short time or not to breastfeed at all and instead use replacement feeding. However, their choices are greatly influenced by other factors than this knowledge. The main factors have been seen in other studies (Thairu et al. 2005; Doherty et al., 2006b): cost of replacement feeds, stigma associated with replacement feeding and disclosure of HIV status and influence of health workers, family and neighbours. The women also highlighted that maintaining either exclusive breastfeeding or exclusive replacement feeding is difficult to do in practice.
Most mothers trusted and relied on the information given by health workers. However, mothers reported that health workers sometimes instruct them to pick a particular feeding option that is not in keeping with counselling concepts based on ‘informed choice’. Counsellors themselves may lack sufficient knowledge to provide adequate information about the options. They may also lack counselling skills and frequently lack time to explain to women and explore the options with them. Infant feeding counsellors need to be adequately trained. Simple assessment guidelines or algorithms (Chopra et al., 2005) could be formulated to enable counsellors to offer effective and practical messages in a relatively short time.
Although stigma about HIV infection often appears to be decreasing in highly endemic countries of sub‐Saharan Africa, it remained an important factor influencing infant feeding decisions. Rates of disclosure of an HIV‐positive status remain low (Doherty et al. 2006a). The nurses and mothers confirmed that it was difficult for some mothers to share their HIV‐positive results with their spouses for fear of being stigmatized, divorced or chased from home. Having men attend with their wives for antenatal care might decrease the problem of not disclosing HIV results. In this study, as previously shown in Nigeria (Sadoh & Sadoh 2009) and Uganda (Matovu et al. 2002), mothers who disclosed their HIV status to their spouses were generally supported by their partners towards choosing an infant feeding option. However, nurses reported that mothers were also scared of joint testing with partners in case they were found to be discordant couples. Lack of disclosure to family and friends also made it difficult for women to choose and adhere to replacement feeding. Those who chose replacement feeding often gave other reasons to family and neighbours as to why they were not breastfeeding, e.g. sores on the breasts, baby refuses breast milk, when baby sucks on the breast her cheeks get swollen.
Box 5. Comments related to stigma and disclosure of HIV status
| ‘I have come across such women who would say “No, me I can afford sister (nurse), I can buy milk, I can buy formula.” Now I do not want to because my neighbour will be asking me, “why are you not breastfeeding? And why have you stopped (breastfeeding) at 6 months because nowadays most people know that if you stop at 6 months it means you are not okay (HIV positive)”.’ (Nurse, FGD) |
| ‘People will start saying that one is sick. She stopped breastfeeding. That's what people say.’ (HIV‐negative mother, FGD) |
| ‘. . . I just feel ashamed that if my friends see me giving milk to the baby they will know (my status), so it is better I breastfeed. This is what is happening most of the time to the mothers.’ (HIV‐positive mother, FGD) |
| ‘. . . especially in these types of houses we stay. You will find someone asking why you are not breastfeeding the child. These days there are (HIV) testing. They will know if I do not breastfeed, that I am infected.’ (interview mother 18) |
| ‘Like me it was difficult because my mother‐in‐law questioned the son so much about why the baby was not breastfeeding. My husband would tell her that each time the baby sucks on the breast the cheeks get swollen.’ (HIV‐positive mother, FGD) |
| ‘. . . and found to be HIV‐positive they fail to tell their husbands . . . so in the process of hiding (the results) from husbands, you find that the husband has a good job, can even manage to buy milk for the baby but because they want to hide their status from their husband you find that they will be breastfeeding the baby. So such mothers say we are protecting our marriages because if my husband gets to know I will be chased.’ (HIV‐positive mother, FGD) |
| ‘Like me I have only told my sister about this problem, so she is the only one who advises me.’ (interview mother 10) |
| ‘. . . hide the status and you breastfeed the child! Because of fear of being chased you put the child's health at risk.’ (HIV‐positive mother, FGD) |
| ‘As friends have said it is not easy to inform the husbands. It is very difficult unless nurses ask them (husbands) to come with their wives for antenatal care, so that counsel and test them together. This will help mothers, because this is what helped me.’ (HIV‐positive mother, FGD) |
| ‘Again one thing these couples are scared of is to be found discordant, . . . these (discordant couples) bring a lot of confusions because when you say go and bring your husband (for HIV testing) you will find that the husband is negative, she (wife) is positive, some do have problems.’ (Nurse, FGD) |
HIV, human immunodeficiency virus; FGD, focus group discussion.
Box 6. Comments related to difficulties with exclusive breastfeeding or exclusive replacement feeding
| ‘I had difficulties finding food to give him. It was difficult to abruptly stop him and find food to give him. In the day I was just giving him porridge but at night he used to trouble me so I would breastfeed him maybe once until he turned 1 year old and I stopped him completely.’ (interview mother 4) |
| ‘And somebody said those drugs, nevirapine, that you take, they reduce the flow of milk, that is what somebody said. I do not know how far true that was. So I could give formula milk (during) day time, in the evening breastfeed. Yes, but it was only . . . I must have mixed the two just for four days.’ (interview mother 5) |
| ‘I breastfed for 4 months without giving anything. I bought milk but he (child) did not like it. He used to refuse. I would put the baby on the breast. Yes, (I gave) milk and breastfeeding.’ (interview mother 10) |
| ‘At the beginning the child was refusing (formula) as he was not used (to it). I would feel pity and breastfeed the child.’ (interview mother 17) |
| ‘Yes I was breastfeeding and giving milk as well.’ (interview mother 20) |
| ‘. . . this practice of not giving any food (i.e. exclusive breastfeeding) is difficult, because you are not the only one handling the child . . .’ (HIV‐negative mother, FGD) |
HIV, human immunodeficiency virus; FGD, focus group discussion.
As previously found for South African women (Doherty et al. 2006b), the women in our study expressed both practical and social concerns with managing exclusive breastfeeding or exclusive replacement feeding. They had been informed of the dangers of mixed feeding but had difficulty stopping breastfeeding abruptly. There was even concern that the perinatal antiretroviral drugs given in the clinic were to help stop milk flow. Abrupt weaning is not a natural part of infant feeding and has not been shown to improve health or reduce HIV transmission (Kuhn et al. 2008). No version of the changing international HIV and infant feeding guidelines has explicitly recommended weaning abruptly. However, the rumour that this was required is widespread, apparently based on the assumption that the association between exclusive breastfeeding and lower HIV transmission risk is causal, and therefore, even a short period of mixed feeding at weaning should be avoided.
Several of the issues raised – cost of replacement feeds, stigma, difficulties with maintaining an exclusive feeding mode – should become less of a concern once the new WHO HIV and infant feeding guidelines (World Health Organization 2009) are implemented. These guidelines are responding in part to evidence that not breastfeeding is associated with increased infant illness even in relatively well‐resourced African settings and even where replacement foods are provided for free. The new guidelines recommend provision of antiretroviral therapy to the HIV‐positive mother or her infant while mothers breastfeed exclusively for 6 months and then partially to about 12 months for HIV‐exposed but uninfected infants and those of unknown HIV status. This more usual infant feeding practice will not advertise the woman's HIV‐positive status, thus reducing stigma, and will avoid difficulties of exclusive replacement‐feeding a young infant, although not difficulties of exclusive breastfeeding. Assuming that the cost of antiretroviral therapy is borne by health services or international donors, mothers will not have to worry about the cost of replacement foods. The replacement foods used by mothers in this study were often inadequate and included cheaper foods such as Bonnita (pasteurized milk meant for general use in a home; women boil it and add salt when giving it to infants), maheu (a drink made of maize flour and millet), tea or home‐made soya milk. However, scaling up of the new WHO HIV and infant feeding guidelines must consider the difficulties experienced by both health workers and mothers in adapting to the ever‐changing messages regarding infant feeding. In this study, one mother already expressed concern about what she thought were conflicting messages given by health workers regarding infant feeding. Some mothers, and even nurses, may find it difficult to trust that practices they were advised not to do a while ago (e.g. breastfeed for at least 12 months) could now be safely practised.
In conclusion, many HIV‐infected women either did not initiate breastfeeding or stopped early, although they did not meet criteria for safe replacement feeding. Women were influenced by health workers but found it difficult to follow their advice because of the cost of formula, influence from relatives, stigma and difficulties of maintaining an exclusive feeding mode. Because health workers are critical to women's infant feeding choices, they need to be educated adequately on the new infant feeding guidelines for HIV‐positive mothers. Because replacement foods are expensive, there is a need to explore ways of making more affordable replacement feeds such as milk (Bonnita) more nutritionally suitable for infants. Lastly, the government should take infant feeding for HIV‐positive mothers as one of their policy priorities.
Source of funding
The study was funded by the Bill and Melinda Gates Foundation.
Conflict of interest
The authors declare that they have no conflicts of interest.
Acknowledgements
The authors wish to thank the women who participated in interviews and FGDs, nurses Munalula Likando and Anne Kanunga for help in recruiting women for the qualitative work, and the CIGNIS study team involved in collection of the quantitative data. The CIGNIS study team comprises the following – Principal Investigator: Suzanne Filteau, London School of Hygiene and Tropical Medicine (LSHTM); Zambian Lead Investigator: Lackson Kasonka, University Teaching Hospital (UTH), Lusaka; Senior Investigators: Rosalind Gibson, University of Otago, New Zealand; Ursula Gompels, LSHTM; Shabbar Jaffar, LSHTM; Emmanuel Kafwembe, Tropical Diseases Research Centre, Ndola; Mwaka Monze, UTH; Moses Sinkala, Catholic Relief Services, Zambia; Andrew Tomkins, Institute of Child Health, University College, London; Rodah Zulu, National Institute of Science and Industrial Research, Zambia; Clinic Coordinator: Molly Chisenga; Clinical Officer: Joshua Siame; Data Manager: Hildah Banda Mabuda; Statisticians: Kathy Baisley, Helen Dale, Daniela Manno, Andrea Rehman; Research Fellows: Matthew Bates, Anne Mullen; Clinic Staff: Hellen Kangwa Bwalya, Margaret Chileshe, Priscilla Kangwa Kowa, Mabvuto Kumwenda, Munalula Likando, Sydney Mambwe, Mutinta Muzyamba, Anne Mwale, Lungowe Nyaywa; Laboratory Staff: Mirriam Kapambwe, Humphrey Bima, Laura Gosset, Louise Hackett, Abigail Jackson, Eric Njunju, Sydney Mwanza; Data Entry: Natalia Shampwaya, Concillia Kabanga; Drivers and Cleaners: John Chobo, Winford Kapumba, Charity Musonda, Philip Soko.
References
- Breastfeeding and HIV International Transmission Study Group ( 2004. ) Late postnatal transmission of HIV‐1 in breast‐fed children: an individual patient data meta‐analysis . Journal of Infectious Diseases 189 , 2154 – 2166 . [DOI] [PubMed] [Google Scholar]
- Central Statistical Office, Ministry of Health, Tropical Diseases Research Centre, University of Zambia & Macro International Inc ( 2009. ) Zambia Demographic and Health Survey 2007 . CSO and Macro International Inc; : Calveton, Maryland, USA . [Google Scholar]
- Chilenje Infant Growth Nutrition and Infection (CIGNIS) Study Team ( 2010. ) Microutrient fortification to improve growth and health of maternally HIV‐unexposed and exposed Zambian infants: a randomised controlled trial . PLoS One Available at: http://www.plosone.org/article/info%3Adoi%2F10.1371%2Fjournal.pone.0011165 . [DOI] [PMC free article] [PubMed]
- Chopra M. , Doherty T. , Jackson D. & Ashworth A. ( 2005. ) Preventing HIV transmission to children: quality of counselling of mothers in South Africa . Acta Paediatrica 94 , 357 – 363 . [DOI] [PubMed] [Google Scholar]
- Chopra M. , Doherty T. , Mehatru S. & Tomlinson M. ( 2009. ) Rapid assessment of infant feeding support to HIV‐positive women accessing prevention of mother‐to‐child transmission services in Kenya, Malawi and Zambia . Public Health Nutrition 12 , 2323 – 2328 . [DOI] [PubMed] [Google Scholar]
- Doherty T. , Chopra M. , Jackson D. , Goga A. , Colvin M. & Persson L.A. ( 2007. ) Effectiveness of the WHO/UNICEF guidelines on infant feeding for HIV‐positive women: results from a prospective cohort study in South Africa . AIDS 21 , 1791 – 1797 . [DOI] [PubMed] [Google Scholar]
- Doherty T. , Chopra M. , Nkonki L. , Jackson D. & Greiner T. ( 2006a. ) Effect of the HIV epidemic on infant feeding in South Africa: “when they see me coming with the tins they laugh at me” . Bulletin of the World Health Organization 84 , 90 – 96 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doherty T. , Chopra M. , Nkonki L. , Jackson D. & Persson L.A. ( 2006b. ) A longitudinal qualitative study of infant‐feeding decision making and practices among HIV‐positive women in South Africa . Journal of Nutrition 136 , 2421 – 2426 . [DOI] [PubMed] [Google Scholar]
- Filmer D. & Pritchett L. ( 2001. ) Estimating wealth effects without expenditure data – or tears: an application to educational enrolments in states of India . Demography 38 , 115 – 132 . [DOI] [PubMed] [Google Scholar]
- Green J. & Thorogood N. ( 2004. ) Qualitative Methods for Health Research . Sage; : London . [Google Scholar]
- Kuhn L. , Aldrovandi G.M. , Sinkala M. , Kankasa C. , Semrau K. , Mwiya M. et al . ( 2008. ) Effects of early, abrupt weaning on HIV‐free survival of children in Zambia . The New England Journal of Medicine 359 , 130 – 141 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matovu J. , Bukenya R. , Musoke P. , Kikonyogo F. & Guay L. ( 2002. ) Experience with Providing Free Formula in Uganda . In HIV and Infant Feeding: A Compilation of Programmatic Evidence ( eds Koniz‐Booher P. , Burkhalter B. , de Wagt A. , Iliff P. & Willumsen J. ), UNICEF/USAID; : Bethesda, USA . [Google Scholar]
- Owino V. , Kasonka L. , Sinkala M. , Wells J. , Eaton S. , Darch T. et al . ( 2007. ) Fortified complementary foods, with or without α‐amylase‐treatment, increase hemoglobin but do not reduce breast milk intake of 9‐month old Zambian infants . the American Journal of Clinical Nutrition 86 , 1094 – 1103 . [DOI] [PubMed] [Google Scholar]
- Sadoh W. & Sadoh A. ( 2009. ) Experiences of HIV‐positive mothers who chose not to breastfeed their babies in Nigeria . African Journal of Reproductive Health 13 , 27 – 35 . [PubMed] [Google Scholar]
- Stringer E.M. , Sinkala M. , Stringer J.S. , Mzyece E. , Makuka I. , Goldenberg R.L. et al . ( 2003. ) Prevention of mother‐to‐child transmission of HIV in Africa: successes and challenges in scaling‐up a nevirapine‐based program in Lusaka, Zambia . AIDS 17 , 1377 – 1382 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thairu L.N. , Pelto G.H. , Rollins N.C. , Bland R.M. & Ntshangase N. ( 2005. ) Sociocultural influences on infant feeding decisions among HIV‐infected women in rural Kwa‐Zulu Natal, South Africa . Maternal & Child Nutrition 1 , 2 – 10 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thiry L. , Sprecher‐Goldberger S. , Jonckheer T. , Levy J. , Van de Perre P. , Henrivaux P. et al . ( 1985. ) Isolation of AIDS virus from cell‐free breast milk of three healthy virus carriers . Lancet 2 , 891 – 892 . [DOI] [PubMed] [Google Scholar]
- UNAIDS/UNICEF/WHO ( 1998. ) HIV and Infant Feeding: Guidelines for Decision‐makers . Geneva, Switzerland .
- World Health Organization ( 1992. ) Consensus statement from the WHO/UNICEF consultation on HIV transmission and breastfeeding . Weekly Epidemiological Record 67 , 177 – 184 . 1610667 [Google Scholar]
- World Health Organization ( 2007a. ) HIV and Infant Feeding: New evidence and Programmatic Experience . Report of a technical consultation held in Geneva, Switzerland, 25–27 October, 2006. Geneva, Switzerland .
- World Health Organization ( 2007b. ) HIV and Infant Feeding: Update .
- World Health Organization ( 2009. ) New WHO Recommendations on Infant Feeding in the Context of HIV .
- Zambian National Food and Nutrition Commission ( 2007. ) Advice and information on nutrition issues in Zambia .
- Ziegler J.B. , Cooper D.A. , Johnson R.O. & Gold J. ( 1985. ) Postnatal transmission of AIDS‐associated retrovirus from mother to infant . Lancet 1 , 896 – 898 . [DOI] [PubMed] [Google Scholar]


