Abstract
The World Health Organization and UNICEF define non‐oedematous severe acute malnutrition (SAM) either by a mid‐upper arm circumference (MUAC) less than 115 mm or by a weight‐for‐height z‐score (WHZ) less than –3. The objective of this study was to assess whether there was any benefit to identify malnourished children with a high risk of death to combine these two diagnostic criteria. Data of a longitudinal study examining the relationship between anthropometry and mortality in rural Senegal and predating the development of community‐based management of SAM were used for this study. First, the receiver operating characteristic (ROC) curves of MUAC and of WHZ to predict mortality were drawn, and then the points corresponding to WHZ less than –3 and/or MUAC less than 115 mm were positioned in relation to these curves. MUAC had the highest ROC curve, which indicates that it identifies high‐risk children better than WHZ. Both points representing WHZ less than –3 and/or MUAC less than 115 mm were below the MUAC ROC curve. It is concluded that to identify high‐risk malnourished children, there is no benefit in using both WHZ less than –3 and/or MUAC less than 115 mm, and that using MUAC alone is preferable.
Keywords: severe acute malnutrition, mid‐upper arm circumference, weight‐for‐height, risk of death
The World Health Organization (WHO) and UNICEF propose to use two independent criteria for diagnosing non‐oedematous severe acute malnutrition (SAM) in children aged 6–60 months, viz. mid‐upper arm circumference (MUAC) less than 115 mm and weight‐for‐height z‐score (WHZ) based on WHO growth standard less than −3 (WHO & UNICEF 2009). WHZ has been used for years in clinical settings for diagnosing SAM (WHO 1999), but the use of MUAC was introduced more recently with the development of community‐based management of SAM (WHO & UNICEF 2007). In practice, large‐scale programmes increasingly use MUAC as single diagnostic criteria as it is closely related to the risk of dying and is easy to implement at the community level after minimum training by health workers or even by volunteers (Myatt et al. 2006). MUAC and WHZ, however, do not identify the same set of children as having malnutrition (Berkley et al. 2005), and using only one of the diagnostic criteria proposed by WHO may potentially leave some high‐risk children untreated.
To clarify how using one or two diagnostic criteria is effective in diagnosing children at risk of dying if left untreated, old data exploring the relationship between anthropometry and mortality and pre‐dating the development of community‐based management of SAM are invaluable. This study used an old data set from Senegal to examine the risk of dying of children having either a low MUAC or a low WHZ or a combination of both in the absence of treatment. The specific objective was to test whether combining both MUAC less than 115 mm and WHZ less than −3 would improve the identification of high‐risk children.
Key messages
-
•
MUAC is better than WHZ to identify high‐risk children in the community.
-
•
Using both WHZ less than −3 AND MUAC less than 115 mm increases specificity but decreases sensitivity to identify high‐risk children.
-
•
Using both WHZ less than −3 OR MUAC less than 115 mm increases sensitivity but decreases specificity to identify high‐risk children.
-
•
There is no advantage for programmes in combining WHZ and MUAC to identify high‐risk children.
Methods
This analysis was based on a data set collected in 1983 and 1984 in the area of Niakhar, in rural Senegal, to examine the relationship between anthropometry and mortality. This study has been described in detail elsewhere (Garenne & Cantrelle 1997; 2000, 2006). In brief, we followed an open cohort of about 5000 children, comprising all under 5 living in 30 villages. We visited the children four times at 6‐month intervals in May and November of 1983 and 1984. At each visit, comprehensive anthropometric measurements were taken (weight, height, head circumference, arm circumference, triceps skin fold and subscapular skin fold). All measures were taken by the researchers themselves (BM and OF) after careful standardization and using state‐of‐the‐art equipment: Beam scales with a precision of 10 g (SECA France, Semur en Auxois, France) and length/height boards with a precision of 1 mm (Holtain Ltd, Crymych, UK). Survival within 6 months was monitored for all children by a demographic surveillance system. The Niakhar study was conducted with the approval of the Ministry of Health of Senegal.
For this analysis, the data from all children aged 6–59 months at the time of anthropometric assessment were used. WHZ was calculated using the WHO growth standards (WHO 2006). Receiver operating characteristic (ROC) curves (sensitivity vs. 1‐specificity) were calculated for WHZ and for MUAC using death within 6 months as outcome. Only the part of the curve with a percentage of false positive less than 5% was explored as these indicators are always used in a context of limited treatment capacity, and a high specificity is required. The anthropometric index with the highest ROC was considered as more adapted to identify high‐risk children (Bairagi 1981). Specificity and sensitivity of ‘MUAC less than 115 mm AND WHZ less than −3’ and also for ‘MUAC less than 115 mm OR WHZ less than −3’ were also estimated and positioned in relation to the ROC curve of MUAC and WHZ.
Results
In total, 12 638 measures were made on 5751 children, and 303 deaths occurred within 6 months of the nutritional assessment. ROC curves of MUAC and WHZ are shown in Fig. 1. The MUAC ROC curve is above the WHZ curve. The criteria ‘WHZ less than −3 AND MUAC less than 115’ had a specificity of 99.0% and a sensitivity of 5.9%. For ‘MUAC less than 115 mm OR WHZ less than −3’, the specificity was 96.9% and the sensitivity was 13.2%. Both points combining WHZ less than −3 and MUAC less than 115 mm were positioned above the WHZ ROC curve but below the MUAC curve.
Figure 1.
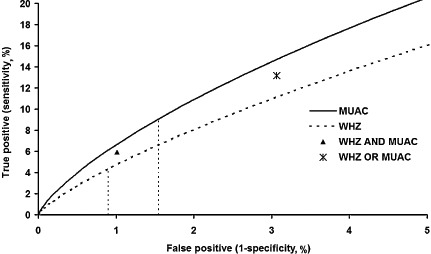
Receiver operating characteristic curves of MUAC and WHZ and combinations of WHZ ≤−3 and/or MUAC <115 mm. The two vertical dotted lines represent WHZ = −3 (left) and MUAC = 115 mm (right). MUAC, mid‐upper arm circumference; WHZ, weight‐for‐height z‐score.
For a MUAC, the threshold of 112 mm had a specificity of 99.1, comparable with the specificity observed for ‘MUAC less than 115 AND WHZ less than −3’. However, the sensitivity of MUAC 112 mm was 6.0%, slightly higher than for these two indices combined.
For a MUAC of 119 mm, the specificity was 96.9%, comparable with the specificity of ‘WHZ less than −3 OR MUAC less than 115 mm’. However, the sensitivity was higher at 14.9%.
Discussion
This study confirms that MUAC has a better ability than WHZ to assess the risk of dying. This is consistent with a previous analysis of the same data set, which showed that MUAC was superior to weight‐for‐height (percentage of the National Center for Health Statistics median) to identify high‐risk children (Briend et al. 1989). This is also consistent with other reports from the literature. In a previous review of the predictive ability of different anthropometric indicators, it was found that the most consistent observation across studies was that weight‐for‐height was the less effective predictor of mortality in community settings using a follow‐up above 6 months (Pelletier 1994).
In addition to confirming previous findings, this study also shows that using WHZ ≤−3 and MUAC ≤115 mm together did not improve the identification of high‐risk children. The position of two possible combinations of WHZ <−3 and/or MUAC ≤115 mm compared with the MUAC ROC curve suggests that using the two indices together may lead to poorer results than using MUAC alone. Arguably, using WHZ ≤−3 AND MUAC ≤115 mm increases the specificity, but this can be obtained by using a lower MUAC cut‐off (112 mm) with a greater sensitivity. Conversely, using WHZ ≤−3 OR MUAC ≤115 mm increases sensitivity, but it also decreases the specificity. Using a MUAC cut‐off of 119 mm, with the same specificity as WHZ ≤−3 OR MUAC ≤115 mm, will result in a higher sensitivity.
Several explanations have been given to explain the apparent superiority of MUAC to assess the risk of dying. A first hypothesis is that MUAC, which grows continuously with age, selects younger children with a higher risk of dying when used with a cut‐off not adjusted for age. Another explanation might be that MUAC is closely related to muscle mass (Briend et al. 1989). A close association between MUAC and muscle mass has been suggested by corresponding measures of body composition by Dual energy X‐ray absorptiometry (Brambilla et al. 2000). The underappreciated metabolic role of muscle both in health and disease may explain its association with survival (Wolfe 2006). These two explanations, however, are not incompatible, as the proportion of muscle in total body mass increases with age (FAO et al. 1985), making a malnourished wasted child with a low muscle mass comparable with a younger child in terms of body composition. Finally, it has been shown that WHZ differences are largely influenced by leg length, unrelated to the nutritional status of the child, which may also decrease its ability to identify high‐risk children (Myatt et al. 2009).
This study was based on MUAC data carefully collected by skilled investigators. Its findings may not be extrapolated to other settings where these conditions are not met. Appropriate training of field workers and standardization of measures are probably needed to use successfully MUAC in field conditions to identify high‐risk children (Cogill 2003). The use of colour‐banded MUAC straps could also help to minimize measurement errors (Myatt et al. 2006).
In conclusion, this study shows that there is no benefit for programmes in using both MUAC ≤115 mm and/or WHZ ≤−3 to identify high‐risk children. If a higher sensitivity is required for programmatic reasons, for instance to take into account a poor food security, it seems preferable to increase the MUAC cut‐off rather than combine it with WHZ. In the same way, if a higher specificity is required, in case of limited treatment capacity, lowering the MUAC cut‐off should be preferable.
Source of funding
The original Niakhar study was supported by the European Union, DG‐XII, Grant No. TDR‐36. This re‐analysis was supported by institutional funds (Institut Pasteur, IRD, University of Tampere).
Conflicts of interest
The authors declare that they have no conflicts of interest.
Contributions
MG was the principal investigator of the original Niakhar study. All other authors were co‐investigators. AB proposed the present analysis and wrote the first draft of this article. MG did the statistical analysis. BM and OF commented and revised the manuscript.
References
- Bairagi R. (1981) On validity of some anthropometric indicators as predictors of mortality. The American Journal of Clinical Nutrition 34, 2592–2594. [DOI] [PubMed] [Google Scholar]
- Berkley J., Mwangi I., Griffiths K., Ahmed I., Mithwani S., English M. et al (2005) Assessment of severe malnutrition among hospitalized children in rural Kenya: comparison of weight for height and mid upper arm circumference. JAMA: the Journal of the American Medical Association 294, 591–597. [DOI] [PubMed] [Google Scholar]
- Brambilla P., Rolland‐Cachera M.F., Testolin C., Briend A., Salvatoni A., Testolin G. et al (2000) Lean mass of children in various nutritional states. Comparison between dual‐energy X‐ray absorptiometry and anthropometry. Annals of the New York Academy of Sciences 904, 433–436. [DOI] [PubMed] [Google Scholar]
- Briend A., Garenne M., Maire B., Fontaine O. & Dieng K. (1989) Nutritional status, age and survival: the muscle mass hypothesis. European Journal of Clinical Nutrition 43, 715–726. [PubMed] [Google Scholar]
- Cogill B. (2003) Anthropometric Indicators Measurement Guide. FANTA: Washington, DC. Available at: http://www.fantaproject.org/downloads/pdfs/anthro_1.pdf [Google Scholar]
- FAO , WHO & UNU (1985) Energy and protein requirements. WHO Technical Report Series 724, 1–112. [PubMed] [Google Scholar]
- Garenne M. & Cantrelle P. (1997) Three decades of research on population and health: the ORSTOM experience in rural Senegal: 1962–1991 In: Prospective Community Studies in Developing Countries (eds Das Gupta M. & Garenne M.), pp 233–252. Oxford University Press: Oxford. [Google Scholar]
- Garenne M., Maire B., Fontaine O., Dieng K. & Briend A. (2000) Risques de décès associés à différents états nutritionnels chez l'enfant d'age préscolaire. Etudes du CEPED no. 17. CEPED: Paris. [Google Scholar]
- Garenne M., Maire B., Fontaine O. & Briend A. (2006) Distributions of mortality risk attributable to low nutritional status in Niakhar, Senegal. The Journal of Nutrition 136, 2893–2900. [DOI] [PubMed] [Google Scholar]
- Myatt M., Khara T. & Collins S. (2006) A review of methods to detect cases of severely malnourished children in the community for their admission into community‐based therapeutic care programs. Food and Nutrition Bulletin 27, S7–23. [DOI] [PubMed] [Google Scholar]
- Myatt M., Duffield A., Seal A. & Pasteur F. (2009) The effect of body shape on weight‐for‐height and mid‐upper arm circumference based case definitions of acute malnutrition in Ethiopian children. Annals of Human Biology 36, 5–20. [DOI] [PubMed] [Google Scholar]
- Pelletier D.L. (1994) ) The relationship between child anthropometry and mortality in developing countries: implications for policy, programs and future research. The Journal of Nutrition 124, 2047S–2081S. [DOI] [PubMed] [Google Scholar]
- WHO (1999) Management of severe malnutrition: a manual for physicians and other senior health workers. World Health Organization: Geneva. [Google Scholar]
- WHO (2006) WHO Child Growth Standards: Methods and development: Length/height‐for‐age, weight‐for‐age, weight‐for‐length, weight‐for‐height and body mass index‐for‐age. World Health Organization: Geneva. [Google Scholar]
- WHO & UNICEF (2007) Community‐based management of severe acute malnutrition. World Health Organization: Geneva. [Google Scholar]
- WHO & UNICEF (2009) WHO child growth standards and the identification of severe acute malnutrition in infants and children. World Health Organization: Geneva. [PubMed] [Google Scholar]
- Wolfe R.R. (2006) The underappreciated role of muscle in health and disease. The American Journal of Clinical Nutrition 84, 475–482. [DOI] [PubMed] [Google Scholar]


