Abstract
A high prevalence of vitamin D deficiency has been reported in non‐Western immigrants in Norway. Our objective was to test whether written information about how to improve vitamin D status could improve the vitamin D status in immigrants mothers attending child health clinics. In this cluster randomized controlled trial in eight child health clinics in Oslo, mothers aged 18–43 years with Pakistani, Turkish, or Somali background were included when their infants were 6 weeks old. The public health nurses gave the intervention group a brochure with information on how to improve vitamin D status, written in their native language. They were compared with a control group receiving usual care, consisting of oral information only. The principal outcome measure was increase in serum 25‐hydroxyvitamin D [s‐25(OH) D] in mothers 7 weeks later. Forty‐four mothers completed the study. Mean baseline s‐25(OH) D was 29.1 (14.8) nmol l−1 in the intervention and 19.4 (9.2) in the control group. There was no significant increase in s‐25(OH) D from baseline to follow‐up in the intervention [6.3 (95%CI: −1.9, 14.4) nmol l−1)] or in the control group [2.9 (95% CI [confidence interval]: −1.2, 7.0) nmol l−1]. When adjusting for baseline s‐25(OH) D concentration the mean difference in increase between the intervention and control group was 1.4 (95% CI: −18.7, 21.4) nmol l−1 (P = 0.87). Adjustment for ethnicity, season and mother's educational background did not alter the results. In sum, providing immigrant mothers with written information about how to improve their vitamin D status did not have an effect on the mothers' vitamin D status.
Keywords: randomized controlled trial, vitamin D, nutrition education, immigrant mothers, maternal nutrition, lactation
Introduction
Vitamin D is important for bone mineralization by regulating calcium metabolism (Holick 2006) and severe vitamin D deficiency can cause rickets in children and osteomalacia in adults (Heaney 2003). In addition, recent research suggests that vitamin D deficiency may be related to a variety of other diseases (Sowers & Lachance 1999; Chan 2000; Holick 2003; Jacobs et al. 2004; VanAmerongen et al. 2004). In areas with temperate climate, vitamin D is synthesized in the skin upon solar ultraviolet B (UVB) exposure during the summer half of the year (Webb et al. 1988). Vitamin D may also be obtained from a limited number of dietary sources such as fatty fish and food fortified with vitamin D, and from dietary supplements.
Unless vitamin D intake is increased, vitamin D status will likely deteriorate when people migrate from developing countries with prevalent vitamin D deficiency (Atiq et al. 1998; Andiran et al. 2002) to Norway or other countries at northern latitude where UVB radiation is not sufficient for vitamin D synthesis in the skin for many months of the year. In Norway, a high prevalence of serious vitamin D deficiency (s‐25(OH)D below 12.5 mol l−1) among immigrant adults have been reported (Henriksen et al. 1995; Meyer et al. 2004; Holvik et al. 2005). In spite of this, an effective nutrition intervention strategy among immigrant populations in Norway has not been in place. However, oral information on vitamin D‐related issues is given at the Child Health Clinics, and intake of vitamin D supplements to infants and mothers is encouraged by public health nurses. The objective of this study was to test whether written information about how to improve vitamin D status, written in the study subject's native language, could improve the vitamin D status in immigrants mothers attending child health clinics in Norway.
Key messages
-
•
In this cluster‐randomized trail among non‐Western immigrant mothers, the great majority had low s‐25(OH) D concentrations both at baseline and at follow‐up.
-
•
Written health education messages on vitamin D provided to intervention group did not have an effect on their vitamin D status.
-
•
Vitamin D determinants such as use of vitamin D supplements, fatty fish, fortified milk, butter, margarine and sun exposure did not change from baseline to follow‐up in the intervention group.
-
•
Effective strategies to improve vitamin D status in non‐Western immigrants should be developed.
Methods and materials
The study is part of a cluster randomized trial conducted between March 2004 and February 2006 in infants with immigrant background and their mothers. As published previously, free supply of vitamin D drops to 6‐week‐old infants together with tailor‐made information handouts significantly improved the vitamin D status of the infants (Madar et al. 2009a). In this paper, we report the results of the intervention in the mothers.
Participants
Mothers with Pakistani, Turkish, or Somali background who came for a routine 6 weeks check‐up of their infants were recruited from Child Health Clinics in Oslo. All participants provided written and translated informed consent. For those who declined to participate, the reasons for not participating were noted. The main reasons for non‐participation were plans of moving back to their countries of origin, frequent moving within the city, having sick children and poor communication skills.
Study design
As described elsewhere (Madar et al. 2009a) 12 Child Health Clinics in Oslo with the highest proportions of immigrant clients were invited to participate, and the eight clinics agreed to participate. They were then paired based on estimates of the number of children with immigrant background belonging to each clinic in order to ensure approximately equal numbers of eligible children in each group. Within each pair, the names of both child health clinics were placed in a box and one was drawn by an independent person. Each clinic drawn was allocated to the intervention group (Fig. 1). We chose to randomize at the Child Health Clinics level in order to avoid any potential practical problems which would have influenced the implementation of the study. If we had randomized at the individual level a couple of issues would have posed problem to the implementation of the study. First, to randomize at the individual level would have been problematic as the public health nurses would then have to carry out both the intervention and usual care at the same time. Secondly, such an allocation procedures could easily lead to a situation with two mothers coming to the Child Health Clinic at the same time allocated to different groups with only one of them receiving free vitamin D drops for their infant. The third issue would have been the possible information exchange between mothers in the intervention group and the control group (relationship or neighbouring). Mothers who came to the intervention Child Health Clinics received a small brochure specially designed for this intervention study, translated to Pakistani, Turkish and Somali. It included simple illustrations and information about the importance of vitamin D and its sources (fatty fish, fortified food available in the Norwegian market, vitamin D supplements and sun exposure). The brochure was intended to aid the public health nurses in providing information to the mothers about vitamin D.
Figure 1.
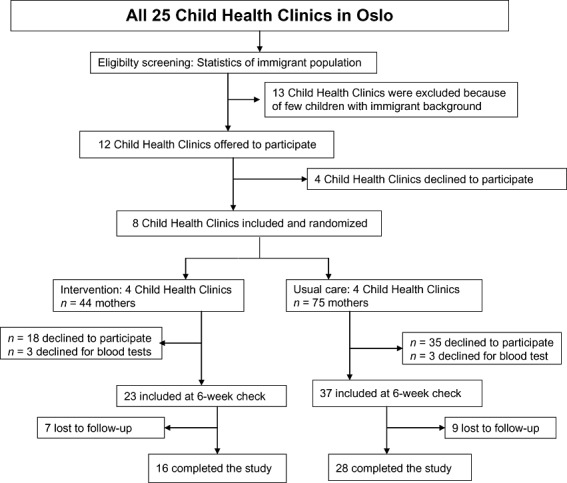
Flowchart of subject progress.
Mothers attending control clinics received usual care consisting of general information about various health issues including recommendation of vitamin D supplementation to their infants from their public health nurses during the first visit after delivery.
Sample size
A priori, we calculated that 18 persons in each group would give the study an 80% power at the 5% significance level to detect a 15 mol l−1 difference in increase in s‐25(OH) D between the two groups given a standard deviation of 16 nmol l−1.
Taking into account that the randomization took place at the Child Health Clinics, we estimated that a study with 48 participants distributed at eight Child Health Clinics corresponded to an individually randomized study with 36 participants given an intraclass correlation of 0.05 (Hanley et al. 2003).
Data collected at baseline and follow‐up
Background information about the mothers including age, number of years living in Norway, height, weight, education, time spent outdoor, clothing habits, vitamin/mineral supplementation and use of foods containing vitamin D was collected by the public health nurses at baseline and at follow‐up using structured questionnaires. The food frequency questions included were piloted among Turkish and Pakistani mothers at the pilot child health clinic (see later).
Blood was drawn from the participating mothers at baseline (when their child was 6 weeks old) and 7 weeks later (3 months check‐up of the child).
The blood was centrifuged after coagulation in room temperature and serum specimens were frozen at −70°C until analysed. S‐25(OH) D2 and s‐25(OH) D3 were determined as previously described (Madar et al. 2009a) by high‐performance liquid chromatography‐ atmospheric pressure chemical ionization at AS VITAS. All samples were analyzed in two batches (one for baseline samples and one for follow‐up samples)
Outcome variable
The main outcome was the individual change in s‐25(OH) D concentration (the sum of s‐25(OH) D2 and s‐25(OH)D3) from baseline to follow‐up.
Statistical analysis
Descriptive analyses for all variables were calculated. We tested the increase of s‐25(OH) D concentration in the intervention group, control group and the pilot study, respectively, by paired sample t‐test. We then tested if change in s‐25(OH) D in the mothers from baseline to follow‐up differed between the intervention and control group by analysis of covariance (ANCOVA). Adjustment was made for baseline s‐25(OH) D (Vickers & Altman 2001). As the randomization was made at the health clinic level, we performed multilevel analyses. Although the test of variation in random intercept was not significant (P = 0.25), the estimated intraclass correlation was 0.43 suggesting a clustering effect. The results reported are thus from multilevel analyses.
We chose a significance level of 0.05. An additional analysis adjusting for ethnicity, mother's education and season [season was defined as winter (October–March) and summer (April–September)] was also conducted. In addition, data on all subjects who were randomly assigned were analysed on an intention to treat basis (mothers with no follow‐up data had their missing values replaced with baseline s‐25(OH) D concentration). The main analyses were executed by a statistician unaware of the grouping of the participants, and who was not otherwise involved in the study. The analyses were performed with SPSS version 11.0 (SPPS, Chicago, IL, USA).
Pilot study
Before the inception of the main study, a pilot study was conducted at one Child Health Clinic in Drammen, a town nearby Oslo, where more than 80% of the attending mothers are non‐Western immigrants. From December 2003, mothers with immigrant background who came for routine 6‐week check‐up of their infants were included. Background data and blood samples were collected both from the mothers and their infants at baseline and follow‐up. The pilot study went very well and did not lead to any modification of materials or procedures in the protocol. We decided to continue to include mothers at the pilot study Child Health Clinic in order to use the data later if needed. Twenty‐one mothers with Turkish and Pakistani immigrant background were included and 19 mothers completed the study. All were given the same intervention as the intervention group in the main study and there was no control group. The follow‐up data from the pilot study was not analysed before the main study.
Ethical clearance
The study was recommended by the Regional Committees for Medical Research Ethics (reference number S‐03196), and approved by the data inspectorate.
Results
A total of 60 mothers (41 Pakistani, 9 Turkish and 10 Somali) were included in the study (Fig. 1). Seventy‐three percent of the participants completed the study; 70% (16/23) in the intervention group and 76% (28/37) in the control group. Background information of the study subjects are presented in Table 1. The three ethnic groups were equally distributed in the intervention and control group. There were some differences between the intervention and control group in baseline characteristics with a larger proportion of women with low education in the control group (Table 1). Baseline s‐25(OH) D was also somewhat lower in the control group (Table 2). A small amount of the total s‐25(OH) D came from S‐25(OH) D2 (5% and 8% for the intervention and control group, respectively).
Table 1.
Baseline information in mothers in the intervention and control group who completed the study
| Intervention n = 16 | Control n = 28 | |
|---|---|---|
| Age (years)* | 31 (6.7) | 28 (5.0) |
| Education <10 years [%, (n)] | 31.3 (5) | 53.6 (15) |
| Time lived in Norway (years)* | 11.8 (7.4) | 9.1 (6.5) |
| BMI (kg m−2)* | 28.9 (4.5) | 26.1 (4.3) |
| Daily vitamin D‐supplements [%, (n)] | 37 (6) | 25 (6) |
| Butter/margarine on bread or for cooking daily [%, (n)] | 86 (12) | 87 (21) |
| Usual fatty fish intake, at least twice a week [%, (n)] | 70 (7) | 50 (10) |
| Use of fortified low fat milk daily [%, (n)] | 25 (4) | 4 (1) |
| Time spent outdoors >1 h daily in the summer [%, (n)] | 38 (6) | 57 (16) |
| Covered head, hands and legs with clothes [%, (n)] | 44 (7) | 50 (14) |
BMI, body mass index; *Mean (SD).
Table 2.
Levels of s‐25(OH) D in the intervention and control groups at baseline and follow‐up in immigrant mothers
| Mean s‐25(OH) D [nmol l−1 (SD)] | |||
|---|---|---|---|
| Baseline | Follow‐up | Δ (change from baseline to follow‐up) | |
| Intervention group (n = 16) | |||
| S‐25(OH) D | 29.1 (14.8) | 35.4 (21.9) | 6.3 (15.3) |
| Control group (n = 28) | |||
| S‐25(OH) D | 19.4 (9.2) | 22.3 (12.7) | 2.9 (10.6) |
Effect of intervention
The mean increase in s‐25(OH) D levels from baseline to follow‐up was 6.3 [95% CI (confidence interval): −1.9, 14.4] nmol l−1 in the intervention group and 2.9 (95% CI: −1.2, 7.0) nmol l−1 in the control group, but none of these changes were statistically significant (Table 2). When adjusting for baseline s‐25(OH) D, the mean difference in increase between the two groups was 1.4 (95% CI: −18.7, 21.4) nmol l−1 (P = 0.87).
Statistical adjustment for season, body mass index, education and ethnic background did not materially alter the estimates (data not shown). When we included the 16 subjects who did not provide the follow‐up blood sample by imputing a follow‐up value equal to the baseline value, the mean difference in increase between the two groups was 1.8 (95% CI:−9.5, 13.1) nmol l−1.
Vitamin D status at baseline and follow‐up
At baseline, 13% and 25% of mothers in intervention and control group, respectively, had s‐25(OH) D below 12.5 nmol l−1, while around 90% of mothers in both groups had s‐25(OH) D concentrations below 50 nmol l−1. Similar figures were found at follow‐up.
Observed change in other factors of interest
Self‐reported use of vitamin D supplements, fatty fish, fortified milk, butter and margarine, and sun exposure did not change from baseline to follow‐up in the intervention group (data not shown). At baseline, six mothers in each group reported using vitamin D containing supplements daily. At follow‐up, the same six mothers in intervention group and four mothers in the control group reported using vitamin D supplements daily. However, these six mothers who reported taking vitamin D supplements did not have a different increase in their s‐25(OH) D levels than the other mothers in the intervention group. Although many mothers in both groups reported spending more than one hour per day outdoors during the summer, around half of them reported to cover their body totally while outside.
Result from the pilot study
Women in the pilot study had a similar proportion with low education (57%) as women in the control group. Mean s‐25(OH) D increased by 2.9 nmol l−1 (P = 0.15) from 22.8 nmol l−1 at baseline to 25.7 nmol l−1 at follow‐up among the mothers completing the study at the pilot Child Health Clinic (n = 19). Including the data from the pilot study in the intervention group did not change the main finding from our study; the mean difference in increase was 2.5 (95% CI: −13.5, 18.5) nmol l−1 between the extended intervention group and the control group after adjustment for baseline s‐25(OH) D levels.
Discussion
The mothers in the intervention group in this study were given a specific informational brochure explaining the importance and sources of vitamin D. Public health nurses handed out the brochures and explained the objectives and content of the brochure to the mothers. We found no benefit of this intervention in improving vitamin D status. These results are supported by the findings from the pilot study showing no effect of the intervention. It is important to note that neither usual care with standard information concerning vitamin D nor the extra effort made in the intervention group lead to any notable change in 25(OH) D in these vitamin D deplete immigrant women.
We have previously demonstrated that the same informational brochure, combined with free provision of vitamin D drops to the infants, significantly improved the vitamin D status of the infants of the participating mothers (Madar et al. 2009a). The lack of change in vitamin D status in the mothers shows that the intervention did not lead to any notable increased intake of vitamin D supplements, foods rich in vitamin D, or in sun exposure.
We are not aware of any similar intervention studies conducted among immigrant mothers. However, a small study conducted in pregnant Pakistani women in Norway, consisting of free samples of vitamin D supplements (10 µg day−1) combined with information, failed to reduce vitamin D deficiency due to poor compliance (Henriksen et al. 1995). In the present study, we did not provide free vitamin D supplement to the mothers, as we did to their infants. We had anticipated that the information provided would enhance the awareness regarding vitamin D and its importance among these mothers.
It is well known that dietary intake of vitamin D increases s‐25(OH) D levels. However, studies that assessed the effect of vitamin D intake on s‐25(OH) D levels have produced different results (Byrne et al. 1995). One reason for this might be that the effect of a given dose is larger at low compared to high baseline levels of s‐25(OH) D (Natri et al. 2006). We have previously shown that 10 µg of vitamin D supplements per day over a 4‐week period produced a mean elevation of s‐25(OH) D of 32–36 nmol l−1 (Holvik et al. 2007). Similar increase in s‐25(OH) D has also been demonstrated in an intervention study conducted in Pakistani immigrants living in Denmark (Andersen et al. 2008). Based on these studies we estimated that in order to achieve an increase of 15 nmol l−1 in s‐25(OH)D, the intervention mothers should on average increase their vitamin D intake by 5 µg day−1[assuming that 1 µg per day of vitamin D raises the s‐25(OH) D by 3 nmol l−1]. If the mothers had adhered to the recommendation in the brochure, this amount of vitamin D would have been achievable through exogenous and endogenous sources.
In Norway, the recommendation for vitamin D intake is 7.5 µg day−1 for individuals between 2 and 60 years. Furthermore, the health and nutrition information messages have been for the most part given in channels directed towards the population in general and not specifically for an immigrant population. In this study, the information was given to the mothers during the 6 weeks check‐up of their infant. Although most of the mothers in this study reported that they were literate and had been resident in Norway for many years (11 years), the tailor‐made written information, failed to produce the desired affect. The lack of effect of the intervention can have multiple explanations. Mothers might have been more concerned about the wellbeing of their infants and put less emphasis on their own health and diet. A second explanation might be that the intervention and public health nurses were focusing on the infant and did not to sufficient degree pay attention to the needs of the mothers. In addition, the source of information to these mothers might not necessarily be the health workers, but rather other people important to these mothers (Imams and elderly people).
This study suggests that written information in the native language alone is insufficient in order to improve vitamin D status among young women from Pakistan, Turkey and Somalia living in Norway. To ensure adequate vitamin D intake of these mothers, we have to consider developing more comprehensive nutrition intervention strategies to reach ethnic minorities.
The strength of this study is that we have measured the effect of the intervention directly by measuring s‐25(OH) D concentrations and not relied on the results from self‐reported information. Furthermore, the information material was specially designed for the target group and translated to their respective languages.
A possible limitation is the relatively large number of mothers lost to follow‐up– reducing the generalizability of the results. However, comparison of the education levels of the participating mothers with data from Statistics Norway (2001) suggests that the mothers included in this study are representative of mothers with Pakistani, Turkish and Somali background living in Norway. Although many mothers reported that they ate fatty fish and used fortified butter/margarine in their diet and that more than a quarter daily used vitamin D supplement, they were low in 25(OH)D. As previously discussed this puts in question the applicability of these questions (Madar et al. 2009b).
One can also argue that perhaps the changes that can realistically be achieved in diet and sun exposure with an intervention such as ours are too small to be detectable with the given sample size. In addition, the number of women in the intervention group completing the study was lower than given by the power calculation, and the 95% CI for the difference in change in 25(OH) D between the two groups was −18.7–21.4 nmol l−1 thus including 15 nmol l−1. On the other hand, the results from the 19 mothers completing the pilot study support our finding, and none of the groups had a significant increase in s‐25(OH) D during the study.
Conclusion
There was no observed effect of tailor‐made information handouts on vitamin D status of mothers with immigrant background. Also results from the pilot study indicate the same result. The fact that almost all the mothers in the study had low s‐25(OH) D concentrations at baseline and follow‐up confirms the need to develop effective strategies to improve the vitamin D status in immigrants.
Source of funding
The study was funded by the Directorate for Health and Social Affairs.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Acknowledgements
We thank all mothers, public health nurses and members of the study advisory group Kirsten Berge, Leif Brunvand, Aud Haugen and Else‐Karin Grøholt for their help with the study. Kristin Berge is also acknowledged for her contribution as the Child Health Clinics coordinator. We also thank Magne Thoresen, University of Oslo for help with the statistical analyses.
Contributors: Ahmed Madar carried out the data collection, performed data analysis and prepared the manuscript. Professor Haakon Meyer developed the study protocol, secured initial funding and assisted in the analysis of the data. Professor Knut‐Inge Klepp and Professor Haakon Meyer supervised the study. All authors commented on the draft, contributed to the interpretation of the findings and approved the final version of the manuscript. The authors declare no conflict of interest with regard to this paper.
Trial registration number: ISRCTN78298308.
References
- Andersen R., Molgaard C., Skovgaard L.T., Brot C., Cashman K.D., Jakobsen J. et al. (2008) Effect of vitamin D supplementation on bone and vitamin D status among Pakistani immigrants in Denmark: a randomised double‐blinded placebo‐controlled intervention study. The British Journal of Nutrition 100, 197–207. [DOI] [PubMed] [Google Scholar]
- Andiran N., Yordam N. & Ozon A. (2002) Risk factors for vitamin D deficiency in breast‐fed newborns and their mothers. Nutrition 18, 47–50. [DOI] [PubMed] [Google Scholar]
- Atiq M., Suria A., Nizami S.Q. & Ahmed I. (1998) Maternal vitamin‐D deficiency in Pakistan. Acta Obstetricia et Gynecologica Scandinavica 77, 970–973. [PubMed] [Google Scholar]
- Byrne P.M., Freaney R. & McKenna M.J. (1995) Vitamin D supplementation in the elderly: review of safety and effectiveness of different regimes. Calcified Tissue International 56, 518–520. [DOI] [PubMed] [Google Scholar]
- Chan T.Y. (2000) Vitamin D deficiency and susceptibility to tuberculosis. Calcified Tissue International 66, 476–478. [DOI] [PubMed] [Google Scholar]
- Hanley J.A., Negassa A., Edwardes M.D. & Forrester J.E. (2003) Statistical analysis of correlated data using generalized estimating equations: an orientation. American Journal of Epidemiology 157, 364–375. [DOI] [PubMed] [Google Scholar]
- Heaney R.P. (2003) Long‐latency deficiency disease: insights from calcium and vitamin D. The American Journal of Clinical Nutrition 78, 912–919. [DOI] [PubMed] [Google Scholar]
- Henriksen C., Brunvand L., Stoltenberg C., Trygg K., Haug E. & Pedersen J.I. (1995) Diet and vitamin‐D status among pregnant Pakistani women in Oslo. European Journal of Clinical Nutrition 49, 211–218. [PubMed] [Google Scholar]
- Holick M.F. (2003) Vitamin D: a millenium perspective. Journal of Cellular Biochemistry 88, 296–307. [DOI] [PubMed] [Google Scholar]
- Holick M.F. (2006) Vitamin D In: Modern Nutrition in Health and Disease (ed. Shils ME, Shike M, Ross AC, Caballero B. & Cousins RJ.) pp 376–395. Lippincott Williams & Wilkins: Philadelphia. [Google Scholar]
- Holvik K., Madar A.A., Meyer H.E., Lofthus C.M. & Stene L.C. (2007) A randomised comparison of increase in serum 25‐hydroxyvitamin D concentration after 4 weeks of daily oral intake of 10 microg cholecalciferol from multivitamin tablets or fish oil capsules in healthy young adults. The British Journal of Nutrition 98, 620–625. [DOI] [PubMed] [Google Scholar]
- Holvik K., Meyer H.E., Haug E. & Brunvand L. (2005) Prevalence and predictors of vitamin D deficiency in five immigrant groups living in Oslo, Norway: the Oslo Immigrant Health Study. European Journal of Clinical Nutrition 59, 57–63. [DOI] [PubMed] [Google Scholar]
- Jacobs E.T., Giuliano A.R., Martinez E.M., Hollis B.W., Reid M.E. & Marshall J.R. (2004) Plasma levels of 25‐hydroxyvitamin D, 1,25‐dihydroxyvitamin D and the risk of prostate cancer. Journal of Steroid Biochemistry 89–90, 533–537. [DOI] [PubMed] [Google Scholar]
- Madar A.A., Klepp K.I. & Meyer H.E. (2009a) Effect of free vitamin D(2) drops on serum 25‐hydroxyvitamin D in infants with immigrant origin: a cluster randomized controlled trial. European Journal of Clinical Nutrition 63, 478–484. [DOI] [PubMed] [Google Scholar]
- Madar A.A., Stene L.C. & Meyer H.E. (2009b) Vitamin D status among immigrant mothers from Pakistan, Turkey and Somalia and their infants attending child health clinics in Norway. British Journal of Nutrition 101, 1052–1058. [DOI] [PubMed] [Google Scholar]
- Meyer H.E., Falch J.A., Sogaard A.J. & Haug E. (2004) Vitamin D deficiency and secondary hyperparathyroidism and the association with bone mineral density in persons with Pakistani and Norwegian background living in Oslo, Norway, The Oslo Health Study. Bone 35, 412–417. [DOI] [PubMed] [Google Scholar]
- Natri A.M., Salo P., Vikstedt T., Palssa A., Huttunen M., Karkkainen M.U. et al. (2006) Bread fortified with cholecalciferol increases the serum 25‐hydroxyvitamin D concentration in women as effectively as a cholecalciferol supplement. The Journal of Nutrition 136, 123–127. [DOI] [PubMed] [Google Scholar]
- Sowers M. & Lachance L. (1999) Vitamins and arthritis. The roles of vitamins A, C, D, and E. Rheumatic Diseases Clinics of North America 25, 315–332. [DOI] [PubMed] [Google Scholar]
- Statistics Norway . (2001) Persons 30‐44 years, by level of education, gender, immigrant category and country background. Available at: http://www.ssb.no/english/subjects/04/01/utinnv_en/tab-2003-02-26-01-en.html
- VanAmerongen B.M., Dijkstra C.D., Lips P. & Polman C.H. (2004) Multiple sclerosis and vitamin D: an update. European Journal of Clinical Nutrition 58, 1095–1109. [DOI] [PubMed] [Google Scholar]
- Vickers A.J. & Altman D.G. (2001) Statistics notes: analysing controlled trials with baseline and follow up measurements. British Medical Journal 323, 1123–1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb A.R., Kline L. & Holick M.F. (1988) Influence of season and latitude on the cutaneous synthesis of vitamin D3: exposure to winter sunlight in Boston and Edmonton will not promote vitamin D3 synthesis in human skin. The Journal of Clinical Endocrinology and Metabolism 67, 373–378. [DOI] [PubMed] [Google Scholar]


