Abstract
The objective of this study was to examine how breastfeeding behaviours, perceptions and experiences vary by race/ethnicity among a low‐income sample in the USA. Bilingual interviewers conducted a cross‐sectional telephone survey of 767 white, African American or Hispanic mothers who received the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). Rates of breastfeeding initiation and duration varied by race/ethnicity. Hispanic mothers were more likely to initiate breastfeeding than African American (91% vs. 65%) or white (61%) mothers. Hispanic mothers breastfed longer (mean 5 months) than either African American (mean 3.5 months) or white (mean 3 months) mothers. The most common reason for not breastfeeding was fear of difficulty or pain during breastfeeding (35.6%). Among mothers who did not initiate breastfeeding, African American and white mothers were more likely than Hispanic mothers to report perceptions of breastfeeding difficulty or pain, and Hispanic mothers were more likely than African American and white mothers to report perceptions of infant breast rejection. The most common reason reported for breastfeeding cessation was not having enough milk (23.4%). Hispanic mothers were more likely than African American and white mothers to cite perceptions of milk insufficiency and infant breast refusal than concerns regarding breast discomfort or pain. African American mothers were more likely than white mothers to report cessation to return to work. In conclusion, while breastfeeding initiation rates approach Healthy People 2010 goals, breastfeeding duration remains far below these goals. Race/ethnicity differences in experiences related to breastfeeding cessation suggest that culturally sensitive breastfeeding interventions are necessary.
Keywords: breastfeeding, race/ethnicity, low‐income, WIC
Introduction
The nutritional, immunological and developmental benefits of breastmilk for infants are well established (American Academy of Pediatrics Work Group on Breastfeeding et al. 2005; American Dietetic Association et al. 2005). For these reasons, the American Academy of Pediatrics (AAP) recommends exclusive breastmilk for infants during the first 6 months and continued breastfeeding for at least the first year of life (American Academy of Pediatrics Work Group on Breastfeeding et al. 2005). Although rates of breastfeeding initiation in the United States are approaching the Healthy People 2010 national goal of 75%, the rates of breastfeeding duration at 6 and 12 months postpartum are still far below the national goals of 50% and 25%, respectively (Li et al. 2005). In addition, breastfeeding rates remain lowest among African American and socio‐economically disadvantaged women (Lee et al. 2005). Mothers with higher levels of education or income are more likely to initiate breastfeeding and to breastfeed longer than women with lower levels of education or income (Kurinij et al. 1988; Forste et al. 2001; Wright 2001; Ryan et al. 2002; Li et al. 2005). Breastfeeding is most common among older, married and immigrant mothers (Kurinij et al. 1988; Wiemann et al. 1998; Forste et al. 2001; Li et al. 2005).
Much of the previous literature has focused on how national breastfeeding rates vary by race/ethnicity or socio‐economic status, although in most studies the two variables are confounded. Little is known about racial/ethnic differences within low‐income populations. The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) provides a low‐income population to examine racial/ethnic breastfeeding differences. WIC is the largest supplemental food programme in the USA, providing food, nutrition counselling and health referrals to low‐income pregnant and postpartum women, infants and children up to 5 years of age (United States Department of Agriculture 2006). To be eligible to participate in WIC, potential clients must meet income guidelines (185% of the US Poverty Income Guidelines), meet a state residency requirement, and be individually determined to be at ‘nutritional risk’ by a health professional (Committee on Scientific Evaluation of WIC Nutrition Risk Criteria Food and Nutrition Board 1996). On average, 1.95 million infants per month, or about half of all infants in the USA, receive WIC services (Ryan & Zhou 2006; United States Department of Agriculture 2006).
Data on whether breastfeeding perceptions and experiences vary by race/ethnicity are limited. Recent studies show that immigrant mothers in the USA who demonstrate close ties with their cultural traditions and practices are more likely to initiate breastfeeding than mothers who are acculturated into the mainstream culture, making it reasonable to expect higher rates of breastfeeding among Spanish‐speaking Hispanic mothers (Guendelman & Siega‐Riz 2002; Chatterji & Brooks‐Gunn 2004; Celi et al. 2005; Gibson et al. 2005) than among other low‐income mothers. Conversely, negative breastfeeding perceptions or experiences, and the need or desire to work, may have a stronger negative effect on breastfeeding initiation and duration among low‐income white and African American mothers than among low‐income Spanish‐speaking Hispanic mothers. Because breastfeeding practices are guided by ethnotheories, or beliefs about what constitutes culturally acceptable and appropriate breastfeeding practices (Harkness & Super 1994, 1996), we hypothesize that breastfeeding behaviours, perceptions and experiences vary by race/ethnicity in a low‐income US population.
Materials and methods
Procedures
A cross‐sectional study of Maryland WIC mothers and infants was conducted from July 2004 to July 2005. Maryland WIC provided the names and contact information of all WIC mothers with infants from birth through 12 months of age (n = 33 804). Recruitment was designed to achieve geographic and ethnic balance throughout the state of Maryland. Therefore, the sampling plan was designed to have adequate sample sizes for three key infant age subgroups (0–4, 5–8 and 9–12 months), equally stratified by race/ethnicity (white, African American and Hispanic) and geographic location of residence (urban/peri‐urban and suburban/rural). Using a random‐number table, a sample (n = 10 376) was selected from the stratified population. With a goal of approximately 800 study participants, contacts were made or attempted for 3285. Potential participants were ineligible if they were less than 18 years of age, had an infant aged greater than 12 months, or were not the primary caregiver at the time of contact (n = 371; Fig. 1).
Figure 1.
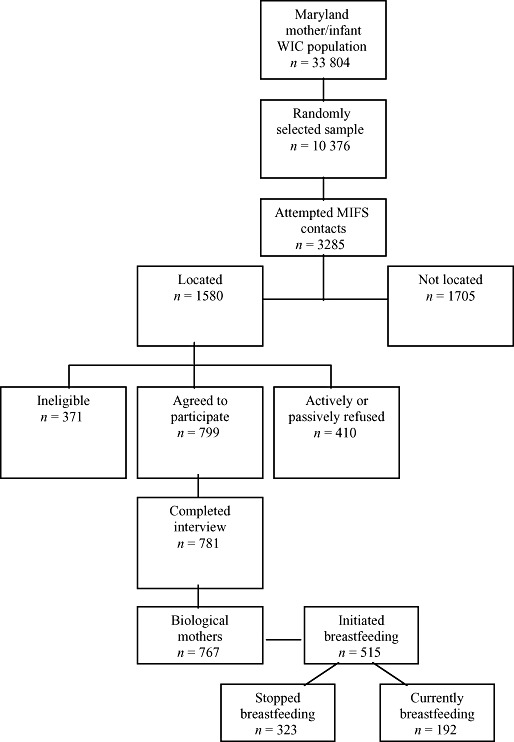
Flow diagram for the Maryland Infant Feeding Study (MIFS). WIC, Special Supplemental Nutrition Program for Women, Infants, and Children.
A brief description of the project was sent to potential participants. All materials were written in English and Spanish, and respondents were given a choice of completing the interview in either language. Six trained telephone interviewers (including three bilingual interviewers) collected data. Each interview took approximately 45 min to complete.
Despite multiple attempts, approximately 52% (n = 1705) of the randomly selected sample of WIC participants could not be located (see Fig. 1). There were no differences between participants located and not located in infant gender, maternal pre‐pregnancy weight and geographic location of residence. Of the 1209 eligible participants who were located, 65% completed the interview (n = 781), 24% refused, and 10% failed to keep scheduled appointments. There were no differences between those who did and did not participate with regard to race/ethnicity, location of residence, infant age, infant gender and maternal pre‐pregnancy weight. Data for 14 participants were eliminated because they were not the infants' biological mothers, and eight infants in their 13th month at the completion of the interview were retained, resulting in a final analytic dataset of 767 mothers and infants.
Measures
Breastfeeding initiation (n = 515) was measured by responses to the question ‘Did you ever breastfeed your infant?’‘Yes’ responses were classified as ‘ever breastfed infant’, and ‘no’ responses were classified as ‘never breastfed infant’.
Breastfeeding duration was measured by responses to two questions. For those who initiated breastfeeding but were no longer breastfeeding at the time of the interview (n = 323), the question ‘If no longer breastfeeding, when did you stop breastfeeding?’ was asked. For those who were still breastfeeding at the time of the interview (n = 192), duration was recoded as age of infant at time of interview.
Perceptions related to breastfeeding initiation were measured by open‐ended responses to the question ‘Why did you decide not to breastfeed your infant?’ Responses were coded into 12 unique and mutually exclusive categories. The first response was used for mothers who provided multiple responses (n = 9).
Experiences related to breastfeeding cessation were measured by open‐ended responses to the question ‘Why did you stop breastfeeding?’ Responses were coded into 16 unique and mutually exclusive categories. The first response was used for mothers who provided multiple responses (n = 19).
Background characteristics, including mother's age, education, employment status, parity and marital status, and infant's age, gender and birthweight, were collected during the telephone interview. Race/ethnicity data were obtained from WIC records. Ninety‐five (83%) of the Hispanic mothers preferred to complete the interview in Spanish. With the exception of lower education obtainment among mothers who preferred to complete the interview in Spanish, demographic and breastfeeding behaviours did not differ by language preference among the Hispanic mothers. In this paper, we refer to Hispanic mothers as Spanish‐speaking Hispanic mothers.
All participants were informed that participation in the study was voluntary, that responses were confidential, and that they would receive a US$10 gift certificate and a list of health and social services. Verbal consent was obtained from each respondent before proceeding with the study interview. The Maryland Department of Health and Mental Hygiene Institutional Review Board, the University of Maryland, Baltimore Institutional Review Board, and the Johns Hopkins Committee on Human Research approved all data collection instruments and procedures for the study.
Data analysis
Frequencies were computed to describe demographic characteristics of the entire sample and then by race/ethnicity. Chi‐squared test and analyses of variance were performed to assess whether the demographic characteristics differed across race/ethnicity.
Unadjusted associations between each demographic characteristic and breastfeeding initiation were estimated using a logistic regression model. A multivariate logistic regression model was used to examine the relationship between race/ethnicity and breastfeeding initiation, adjusting for potential confounding variables.
Duration of breastfeeding was computed as the time from date of breastfeeding initiation until the date of breastfeeding cessation. Data from mothers who were breastfeeding at the time of the interview were censored at that date. Survival analysis techniques were used to model time to cessation of breastfeeding. A series of Cox proportional hazards regression models were used to examine the associations between each maternal and infant demographic characteristic and breastfeeding cessation, as well as the relationship between race/ethnicity and breastfeeding cessation, adjusting for potential confounders (Grimm & Yarnold 2000). The proportionality of hazards assumption was checked for all models.
Chi‐squared tests were conducted to assess whether breastfeeding perceptions and experiences differed by race/ethnicity. A probability of P < 0.05 was considered statistically significant for all tests. Analyses were conducted using spss version 11.00 (SPSS 2001).
Results
Sample characteristics
Relevant data were available for 767 mothers; 48% (n = 365) were white, 37% (n = 285) were African American, and 15% (n = 117) were Hispanic. All socio‐economic indicators differed significantly across the three racial/ethnic groups (Table 1). Due to bilingual examiner availability, an unequal racial/ethnic distribution was obtained.
Table 1.
Demographic characteristics among 767 Maryland WIC mothers and infants overall and by race/ethnicity
| Total sample (n = 767) | African American (n = 285) | Hispanic (n = 117) | White (n = 365) | Test of significance | |
|---|---|---|---|---|---|
| Maternal characteristics | |||||
| Age (%) | |||||
| 18–20 years | 18.2 | 21.3 | 13.8 | 17.2 |
 = 7.12
† = 7.12
†
|
| 21–25 years | 33.6 | 28.4 | 37.9 | 36.3 | |
| 26+ years | 48.2 | 50.4 | 48.3 | 46.5 | |
| Education (%) | |||||
| Less than high school | 20.6 | 16.5 | 39.3 | 17.9 |
 = 31.42[Link], [Link] = 31.42[Link], [Link]
|
| High school/GED | 34.9 | 35.4 | 31.6 | 35.4 | |
| Beyond high school | 44.5 | 48.1 | 29.1 | 46.7 | |
| Employment status (%) | |||||
| Full‐time | 21.6 | 26.9 | 11.2 | 20.7 |
 = 26.29[Link], [Link] = 26.29[Link], [Link]
|
| Part‐time | 18.7 | 18.4 | 13.8 | 20.4 | |
| Unemployed | 53.6 | 45.9 | 70.7 | 54.1 | |
| Student | 6.2 | 8.8 | 4.3 | 4.7 | |
| Marital status (%) | |||||
| Not married | 60.0 | 70.9 | 63.2 | 51.0 |
 = 29.0[Link], [Link] = 29.0[Link], [Link]
|
| Married | 40.0 | 29.1 | 36.8 | 49.0 | |
| Parity of birth (%) | |||||
| Primiparous | 40.7 | 44.0 | 38.5 | 38.7 |
 = 2.12
† = 2.12
†
|
| Multiparous | 59.3 | 56.0 | 61.5 | 61.3 | |
| Infant characteristics | |||||
| Age (%) | |||||
| 0–4 months | 29.5 | 30.5 | 22.2 | 31.0 |
 = 7.60
† = 7.60
†
|
| 5–8 months | 34.7 | 36.8 | 31.6 | 34.0 | |
| 9–12 months | 35.9 | 32.6 | 46.2 | 35.1 | |
| Gender (%) | |||||
| Male | 52.7 | 56.1 | 45.3 | 52.3 |
 = 3.94
† = 3.94
†
|
| Female | 47.3 | 43.9 | 54.7 | 47.7 | |
| Birthweight (g), mean (SD) | 3272 (592) | 3171 (596) | 3341 (561) | 3329 (589) | F 2,766 = 0.01 ‡ |
GED, General Educational Development; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children. *P < 0.05 (education, P < 0.001; employment status, P < 0.001; marital status, P < 0.001). †Chi‐squared test used to test for significant differences by race/ethnicity for categorical or dichotomous variables. ‡ anova (F‐test) used to test for significant differences by race/ethnicity for continuous variables.
Breastfeeding initiation
Two‐thirds of mothers (67%) initiated breastfeeding. The unadjusted proportion of women who initiated breastfeeding varied by race/ethnicity; Hispanic mothers (91%) were more likely to initiate breastfeeding than African American (65%) or white (61%) mothers. Three sociodemographic characteristics were significantly associated with breastfeeding initiation. Mothers with less than a high school education or with only a high school diploma were half as likely to initiate breastfeeding as mothers with any college education. Increased maternal age and decreased infant age (0–4 vs. 9–12 months) were positively related to breastfeeding initiation. No statistically significant relationships were detected between breastfeeding initiation and maternal employment status, marital status, parity, or infant gender and birthweight (Table 2). After adjusting for maternal education, and maternal and infant age, African American (logistic regression: OR = 0.15, CI: 0.07–0.29, P < 0.001) and white (logistic regression: OR = 0.13, CI: 0.07–0.25, P < 0.001) mothers continued to be significantly less likely to have initiated breastfeeding than Spanish‐speaking Hispanic mothers.
Table 2.
Unadjusted associations between maternal and infant characteristics and breastfeeding initiation among Maryland WIC mothers and infants (n = 767)
| OR* (95% CI) | |
|---|---|
| Maternal characteristics | |
| Age (years) | 1.03* (1.001, 1.1) |
| Education | |
| Beyond high school | 1.0 |
| Less than high school | 0.51 † (0.34, 0.77) |
| High school/GED | 0.48 † (0.34, 0.68) |
| Employment status | |
| Unemployed | 1.0 |
| Part‐time | 0.96 (0.64, 1.40) |
| Full‐time | 0.80 (0.55, 1.20) |
| Marital status | |
| Married | 0.99 (0.97, 1.03) |
| Parity of birth | |
| Multiparous | 0.82 (0.61, 1.1) |
| Infant characteristics | |
| Age | |
| 9–12 months | 1.0 |
| 5–8 months | 0.80 (0.56, 1.1) |
| 0–4 months | 1.5 † (1.01, 2.2) |
| Gender | |
| Female | 1.1 (0.80, 1.5) |
| Birthweight (g) | 1.23 (0.96, 1.6) |
GED, General Educational Development; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children. *Logistic regression: unadjusted odds ratios (OR) and 95% confidence intervals (CI). † P < 0.05 (maternal age, P = 0.02; education, P = 0.001 and P < 0.001; infant's age, P = 0.045).
The most common reasons mothers reported for not breastfeeding included: fear of difficulty or pain during breastfeeding (35.6%), poor maternal health at delivery (15.3%), the need to return to work (9.3%), infant breast rejection (8.9%), and fear of embarrassment (6.1%). Among mothers who did not initiate breastfeeding, African American and white mothers tended to report more perceptions of breastfeeding difficulty or pain than Spanish‐speaking Hispanic mothers. However, Spanish‐speaking Hispanic mothers were more likely than African American or white mothers to report perceptions of initial infant breast rejection (Table 3).
Table 3.
Reasons why mothers decide not to breastfeed among 252 Maryland WIC participants, per cent overall and per cent stratified by race/ethnicity
| Reasons for not breastfeeding | % | |||
|---|---|---|---|---|
| Total (n = 252) | African American (n = 100) | Hispanic (n = 11) | White (n = 141) | |
| Fear of breastfeeding difficulty or pain | 35.6 | 40.0 a | 9.1 a , b | 35.0 b |
| Mother sick at birth | 15.3 | 16.7 | 9.1 | 14.3 |
| Had to return to work | 9.3 | 8.3 | 9.1 | 10.0 |
| Infant rejected breast | 8.9 | 4.2 c | 36.4 c , d | 10.0 d |
| Fear of embarrassment | 6.1 | 3.1 | 9.1 | 7.9 |
| Other reasons* | 24.7 | 28.1 | 18.2 | 22.9 |
Other reasons include: infant sick at birth (1.6%), to allow others to help (1.2%), others criticized (0.4%), had Caesarean section (1.2%), did not want to breastfeed (9.7%), mother smoked (5.7%), and others (6.9%).
Difference in Hispanic vs. African American mothers ( = 3.96, P = 0.047).
= 3.96, P = 0.047).
Differences in Hispanic vs. white mothers ( = 3.10, P = 0.08).
= 3.10, P = 0.08).
Differences in Hispanic vs. African American mothers ( = 14.80, P < 0.001).
= 14.80, P < 0.001).
Differences in Hispanic vs. white mothers ( = 6.75, P = 0.01).
= 6.75, P = 0.01).
Breastfeeding cessation
The median time to breastfeeding cessation was 4 months. Hispanic mothers breastfed longer (mean 5 months) than either African American (mean 3.5 months) or white (mean 3 months) mothers. Rates of breastfeeding cessation were higher in younger mothers and in mothers without a high school education or with only a high school diploma, than in older mothers and in mothers with any college education. Mothers who were employed full‐time or had more than one child reported higher rates of breastfeeding cessation compared with unemployed or first‐time mothers. Rates of breastfeeding cessation did not significantly differ by marital status, infant gender and infant birthweight (Table 4).
Table 4.
Unadjusted hazard ratios of breastfeeding cessation by maternal and infant characteristics of Maryland WIC mothers and infants (N = 515)
| HR* (95% CI) | |
|---|---|
| Maternal characteristics | |
| Age (years) | 0.93 a (0.91, 0.95) |
| Education | |
| Beyond high school | 1.0 |
| Less than high school | 1.87 a (1.4, 2.48) |
| High school/GED | 1.56 a (1.21, 2.02) |
| Employment status | |
| Unemployed | 1.0 |
| Full‐time | 1.42 a (1.07, 1.88) |
| Part‐time | 1.15 (0.86, 1.54) |
| Marital status | |
| Married | 1.00 (0.98, 1.03) |
| Parity of birth | |
| Multiparous | 1.52 a (1.21, 1.90) |
| Infant characteristics | |
| Age | |
| 9–12 months | 1.0 |
| 5–8 months | 1.25 (0.96, 1.63) |
| 0–4 months | 1.58 a (1.67, 2.12) |
| Gender | |
| Female | 0.88 (0.70, 1.10) |
| Birthweight (g) | 0.96 (0.88, 1.05) |
GED, General Educational Development; WIC, Special Supplemental Nutrition Program for Women, Infants, and Children. *Cox proportional hazard regression: hazard ratios and 95% confidence intervals (CI). a P < 0.05 (maternal age, P < 0.001; education, P < 0.001 and P = 0.001; employment status, P = 0.01; parity, P < 0.001; infant age, P = 0.003).
After adjusting for maternal age, education, parity, employment status and infant age, rates of breastfeeding cessation were significantly earlier among white (Cox proportional hazards: HR = 1.61, CI: 1.15–2.24, P = 0.005) and marginally earlier among African American (Cox proportional hazards: HR = 1.37, CI: 0.96–1.94, P = 0.08) mothers than Spanish‐Speaking Hispanic mothers (mean 5 months). The duration of exclusive breastfeeding (defined as infants receiving only breastmilk without additional food or drink, including water) averaged 2.1 months, dropped consistently over the first 6 months of the child's life (23% at 3 months and 2.2% at 6 months), and did not vary by race/ethnicity.
The most common reasons mothers reported for breastfeeding cessation included: not having enough milk (23.4%), breast discomfort or pain (16.9%), infant breast rejection (14.1%), having to return to work (12.8%) and maternal illness (9.3%). As compared with African American and white mothers, Spanish‐speaking Hispanic mothers were more likely to stop breastfeeding based on perceptions of decreased milk supply and infant breast refusal than concerns regarding breast discomfort or pain. African American mothers were more likely to report stopping because of the need to return to work than white mothers (see Table 5).
Table 5.
Per cent overall and per cent stratified by race/ethnicity of the reasons for breastfeeding cessation in a statewide sample of 323 Maryland WIC participants*
| Reasons for cessation | % | |||
|---|---|---|---|---|
| Total (n = 311) | African American (n = 114) | Hispanic (n = 63) | White (n = 134) | |
| Not enough milk | 23.4 | 19.5 a | 41.3 a , b | 18.4 b |
| Breast discomfort or pain | 16.9 | 23.0 c | 3.2 c , d | 18.4 d |
| Infant rejected breast | 14.1 | 11.5 e | 30.2 e , f | 8.8 f |
| Had to return to work | 12.8 | 19.5 g , h | 9.5 g | 8.8 h |
| Mother sick/taking meds | 9.3 | 8.0 | 4.8 | 12.5 |
| Other reasons † | 23.3 | 18.5 | 11 | 33.1 |
WIC, Special Supplemental Nutrition Program for Women, Infants, and Children. *Missing data on reasons for breastfeeding cessation on 12 participants.
†Other reasons include: infant sick (4.5%), infant seemed hungry (3.8%), infant irritable or not sleeping (1.0%), concerned about infant's growth (1.0%), to allow others to help (2.6%), others recommended (0.6%), infant seemed interested in other foods (2.2%), infant old enough for other liquids (2.6%), mother embarrassed (1.3%), mother smoked (1.0%) and others (3.2%).
aDifference by Hispanic vs. African American ( = 9.69, P = 0.003).
bDifference by Hispanic vs. white (
= 9.69, P = 0.003).
bDifference by Hispanic vs. white ( = 11.83, P = 0.001).
cDifference by Hispanic vs. African American (
= 11.83, P = 0.001).
cDifference by Hispanic vs. African American ( = 11.89, P < 0.001).
dDifference by Hispanic vs. white (
= 11.89, P < 0.001).
dDifference by Hispanic vs. white ( = 8.49, P = 0.003).
eDifference by Hispanic vs. African American (
= 8.49, P = 0.003).
eDifference by Hispanic vs. African American ( = 9.46, P = 0.003).
fDifference by Hispanic vs. white (
= 9.46, P = 0.003).
fDifference by Hispanic vs. white ( = 14.90, P < 0.001).
gDifference by Hispanic vs. African American (
= 14.90, P < 0.001).
gDifference by Hispanic vs. African American ( = 2.99, P = 0.09).
hDifference by African American vs. white (
= 2.99, P = 0.09).
hDifference by African American vs. white ( = 5.93, P = 0.02).
= 5.93, P = 0.02).
Discussion
The current study reveals three major findings related to breastfeeding initiation and duration among low‐income mothers in the USA. First, rates of breastfeeding initiation among this low‐income sample of WIC participants are approaching the national goal of 75%. These data are consistent with other reports that rates of breastfeeding initiation among mothers in the WIC programme are increasing (Li et al. 2005). However, the rates of breastfeeding at 6 and 12 months (21.1% and 0.04%, respectively) are still far below the national goals. Second, a strong racial/ethnic difference in the decision to breastfeed was found, favouring Spanish‐speaking Hispanic mothers, even after controlling for socio‐economic background and birth characteristics. This finding concurs with past research (Lee et al. 2005) and suggests that ethnotheories about breastfeeding inherent in Hispanic cultures may influence breastfeeding decisions. Spanish‐speaking Hispanic mothers may live in communities with strong ties to their native cultural values and beliefs where breastfeeding is the norm. These mothers may therefore have strong, informal community role models for breastfeeding, including relatives, friends and neighbours, who breastfed their own children (Guendelman & Siega‐Riz 2002; Chatterji & Brooks‐Gunn 2004; Celi et al. 2005; Gibson et al. 2005).
Unlike previous research (Lee et al. 2005), no discrepancy between breastfeeding rates for white and African American mothers was found. One possible explanation for the lack of difference in breastfeeding rates between white and African American mothers is that by studying a sample that was exclusively low‐income, economic confounders were minimized. An alternative explanation is that many of the mothers, regardless of race/ethnicity, may have been exposed to breastfeeding education through WIC.
Third, breastfeeding perceptions and experiences were related to maternal breastfeeding initiation and cessation, but varied by race/ethnicity. Among African American and white mothers, fears of breastfeeding difficulty or pain were the most common reasons reported for deciding not to breastfeed. Similarly, breast discomfort and pain were related to the mothers' decision to terminate breastfeeding. In contrast, Spanish‐speaking Hispanic mothers expressed more concern regarding their milk supply and their infant rejecting the breast than white or African American mothers. Finally, African American mothers were more likely to report breastfeeding cessation because of the need to return to work than white mothers.
These perceptions and experiences may be influenced by the beliefs and ethnotheories that constitute appropriate infant care and feeding behaviours within a particular culture or subculture (Harkness & Super 1994, 1996). Despite the recent increase in breastfeeding initiation across racial/ethnic groups, the rates of breastfeeding duration are still low (across all race/ethnicity groups) and may indicate limited successful breastfeeding experiences among older women in the community. Without ongoing support from their own mothers or other female role models, African American and white mothers may have few resources to overcome the temporary pain or discomfort that can accompany breastfeeding. In contrast, breastfeeding is an established tradition in the Hispanic community, in which older women are able to provide support for newly breastfeeding mothers (Guendelman & Siega‐Riz 2002; Chatterji & Brooks‐Gunn 2004; Celi et al. 2005; Gibson et al. 2005). Apprehensions related to milk insufficiency and infant rejection may reflect the Spanish‐speaking Hispanic mothers' beliefs that although they are technically able to breastfeed, they may not be able to meet their infants' nutritional demands. Finally, the African American mothers' concerns regarding the need to terminate breastfeeding to return to work may be a result of their demographic position, with relatively high rates of being single and employed.
Some methodological limitations should be considered when interpreting these findings. First, we were unable to contact 52% of the potentially eligible participants, thereby possibly limiting the generalizabilty of our findings. While the use of telephone interviews enabled participants to be interviewed in their homes, it might have prevented less stable, lower‐income households without telephones from participating in the study. Similarly, voluntary participation may have introduced a bias, with those who were more negative about breastfeeding declining to participate.
The sample of Spanish‐speaking Hispanic women is small due to examiner availability. Further, most Spanish‐speaking Hispanic mothers initiated breastfeeding (91%), leaving a small sample size for looking at race/ethnic differences in reasons for not breastfeeding.
Finally, the exclusive focus on low‐income participants limits the generalizabilty of the study findings. However, the diverse statewide sample of WIC participants may enable the findings to be generalized to WIC participants in other states and to low‐income populations that have a similar racial/ethnic make‐up. Because few studies have examined racial/ethnic differences associated with maternal‐reported determinants of breastfeeding, qualitative methods may be helpful to confirm and expand on the current findings.
Conclusions and recommendations
Given the recent increase in breastfeeding initiation among low‐income women and the effectiveness of some breastfeeding promotion programmes (Hartley & O'Connor 1996; Shaw & Kaczorowski 1999;Zimmerman 1999; Merewood & Philipp 2001; Wright 2001), our findings may be useful in further achieving the national breastfeeding goals by the year 2010. While breastfeeding benefits and techniques are commonly discussed with expecting mothers, it may also be beneficial to probe for maternal breastfeeding perceptions and to develop strategies to decrease maternal breastfeeding fears and concerns. Focusing on maternal breastfeeding experiences post delivery is also important for breastfeeding success and continuation. The decreasing trend in breastfeeding from birth to 3 months postpartum, along with the frequency of breast discomfort, milk insufficiency and the need to return to work, as reasons for cessation, suggests that breastfeeding mothers may benefit from special attention to breastfeeding experiences, perhaps through physician interventions and breastfeeding peer‐support groups. Recent evidence suggests that physician breastfeeding support is positively associated with increased breastfeeding duration (Taveras et al. 2003) and peer‐group breastfeeding interventions (i.e. peer counselling) may increase breastfeeding support, confidence and duration (Bronner et al. 2001). Although the AAP recommends that physicians provide breastfeeding counselling and support, medical education in the USA often lacks formal training in breastfeeding care (Ogburn et al. 2005). Thus, physician trainees may benefit from increased attention to breastfeeding practices.
Our findings also suggest a need for culturally appropriate breastfeeding interventions. Among white and African American mothers, intervention efforts might focus on providing peer support (thereby increasing the normalcy of breastfeeding), managing problems of lactation, and enhancing the mother's confidence regarding breastfeeding. For Spanish‐speaking Hispanic mothers, the focus might be placed on the importance of exclusive breastfeeding for the maintenance of milk supply. Interventions that target exclusivity should begin in the prenatal period and might include strategies to address cultural values that may exist within Hispanic cultures that hinder exclusive breastfeeding (e.g. early introduction of solids) (Mennella et al. 2006).
Finally, African American mothers expressed concern about returning to work, suggesting that the provision of flexible work hours, paid maternity leave, on‐site child care, and a supportive work environment (e.g. lactation breaks and facilities) are likely to have positive effects on rates of breastfeeding duration among all breastfeeding mothers, thus bringing low‐income families closer to the goals proposed by Healthy People 2010 (United States Department of Health & Human Services 2000).
Acknowledgements
This research was supported by the Maryland Special Supplemental Nutrition Program for Women, Infants, and Children (WIC). The authors extend their appreciation to Kathleen Knolhoff, MPH (Maryland WIC Director) and Mary Dallavalle, MS, RD, LD (Maryland WIC Nutrition Education Specialist), and to the families who participated in the project.
Conflict of Interest: There are no financial or other relationships that might lead to conflict of interest by any author(s) of this paper.
References
- American Academy of Pediatrics Work Group on Breastfeeding, Gartner, L.M. , Morton J., Lawrence R.A., Naylor A.J., O'Hare D. et al. (2005) Breastfeeding and the use of human milk. Pediatrics 115, 496–506. [DOI] [PubMed] [Google Scholar]
- American Dietetic Association, James D. & Dobson B. (2005) Position of the American Dietetic Association: promoting and supporting breastfeeding. Journal of the American Dietetic Association 105, 810–818. [DOI] [PubMed] [Google Scholar]
- Bronner Y., Barber T. & Miele L. (2001) Breastfeeding peer counseling: rationale for the National WIC Survey. Journal of Human Lactation 17, 135–139. [DOI] [PubMed] [Google Scholar]
- Celi A., Rich‐Edwards J., Richardson M., Kleinman K. & Gillman M. (2005) Immigration, race/ethnicity, and social and economic factors as predictors of breastfeeding initiation. Archives of Pediatrics and Adolescent Medicine 159, 255–260. [DOI] [PubMed] [Google Scholar]
- Chatterji P. & Brooks‐Gunn J. (2004) WIC participation, breastfeeding practices, and well‐child care among unmarried, low‐income mothers. American Journal of Public Health 94, 1324–1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Scientific Evaluation of WIC Nutrition Risk Criteria Food and Nutrition Board (1996) Summary of WIC nutrition risk criteria: a scientific assessment. Committee on Scientific Evaluation of WIC Nutrition Risk Criteria Food and Nutrition Board, Institute of Medicine, National Academy of Sciences. Journal of the American Dietetic Association 96, 925–930. [PubMed] [Google Scholar]
- Forste R., Weiss J. & Lippincott E. (2001) The decision to breastfeed in the United States: does race matter? Pediatrics 108, 291–296. [DOI] [PubMed] [Google Scholar]
- Gibson M., Diaz V., Mainous A. & Geesey M. (2005) Prevalence of breastfeeding and acculturation in Hispanics: results from the NHANES 1999–2000 Study. Birth 32, 93–98. [DOI] [PubMed] [Google Scholar]
- Grimm L. & Yarnold P. (2000) Reading and Understanding More Multivariate Statistics. American Psychological Association: Washington, DC. [Google Scholar]
- Guendelman S. & Siega‐Riz A. (2002) Infant feeding practices and maternal dietary intake among Latino immigrants in California. Journal of Immigrant Health 4, 137–146. [DOI] [PubMed] [Google Scholar]
- Harkness S. & Super C. (1994) The developmental niche: a theoretical framework for analyzing the household production of health. Social Science and Medicine 38, 217–226. [DOI] [PubMed] [Google Scholar]
- Harkness S. & Super C. (1996) Parents' Cultural Belief Systems: Their Origins, Expressions, and Consequences. The Guilford Press: New York. [Google Scholar]
- Hartley B. & O'Connor M. (1996) Evaluation of the ‘Best Start’ breast‐feeding education program. Archive of Pediatrics and Adolescent Medicine 150, 868–871. [DOI] [PubMed] [Google Scholar]
- Kurinij N., Shiono P. & Rhoads G. (1988) Breast‐feeding incidence and duration in black and white women. Pediatrics 81, 365–371. [PubMed] [Google Scholar]
- Lee H., Rubio M., Elo I., Mccollum K., Chung E. & Culhane J. (2005) Factors associated with intention to breastfeed among low‐income, inner‐city pregnant women. Maternal and Child Health Journal 9, 253–261. [DOI] [PubMed] [Google Scholar]
- Li R., Darling N., Maurice E., Barker L. & Grummer‐Strawn L. (2005) Breastfeeding rates in the United States by characteristics of the child, mother, or family: the 2002 National Immunization Survey. Pediatrics 115, e31–e37. [DOI] [PubMed] [Google Scholar]
- Mennella J., Ziegler P., Briefel R. & Novak T. (2006) Feeding infant and toddlers study: the types of foods fed to Hispanic infants and toddlers. Journal of the American Dietetic Association 106, S96–S106. [DOI] [PubMed] [Google Scholar]
- Merewood A. & Philipp B. (2001) Implementing change: becoming baby‐friendly in an inner city hospital. Birth 28, 36–40. [DOI] [PubMed] [Google Scholar]
- Ogburn T., Espey E., Leeman L. & Alvarez K. (2005) A breastfeeding curriculum for residents and medical students: a multidisciplinary approach. Journal of Human Lactation 21, 458–464. [DOI] [PubMed] [Google Scholar]
- Ryan A.S. & Zhou W. (2006) Lower breastfeeding rates persist among the Special Supplemental Nutrition Program for Women, Infants, and Children participants, 1978–2003. Pediatrics 117, 1136–1146. [DOI] [PubMed] [Google Scholar]
- Ryan A.S., Zhou W. & Acosta A. (2002) Breastfeeding continues to increase into the new millennium. Pediatrics 110, 1103–1109. [DOI] [PubMed] [Google Scholar]
- Shaw E. & Kaczorowski J. (1999) The effect of a peer counseling program on breastfeeding initiation and longevity in a low‐income rural population. Journal of Human Lactation 15, 19–25. [DOI] [PubMed] [Google Scholar]
- SPSS (2001) Statistical Package for the Social Sciences (SPSS) for Windows, Release 11.0.1. [Software program.] SPSS Inc.: Chicago, IL. [Google Scholar]
- Taveras E., Capra A., Braveman P., Jensvold N., Escobar G. & Lieu T. (2003) Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics 112, 108–115. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services (2000) Healthy People 2010, 2nd edn . With Understanding and Improving Health and Objectives for Improving Health. U.S. Government Printing Office: Washington, DC. [Google Scholar]
- United States Department of Agriculture (2006) WIC: The Special Supplemental Nutrition Program for Women, Infants and Children; Nutrition Program Facts Food and Nutrition Service. Available at: http://www.fns.usda.gov/wic/WIC-FACT-Sheet.pdf (accessed 10 August 2006).
- Wiemann C., Dubois J. & Berenson A. (1998) Racial/ethnic differences in the decision to breastfeed among adolescent mothers. Pediatrics 101, E11. [DOI] [PubMed] [Google Scholar]
- Wright A. (2001) The rise of breastfeeding in the United States. Pediatric Clinics of North American 48, 1–12. [DOI] [PubMed] [Google Scholar]
- Zimmerman D. (1999) You can make a difference: increasing breastfeeding rates in an inner‐city clinic. Journal of Human Lactation 15, 217–220. [DOI] [PubMed] [Google Scholar]


