Abstract
Improving infant and young child feeding practices will help South Asian countries achieve the Millennium Development Goal of reducing child mortality. This paper aims to compare key indicators of complementary feeding and their determinants in children aged 6–23 months across five South Asian countries – Bangladesh, India, Nepal, Pakistan and Sri Lanka. The latest Demographic and Health Survey and National Family Health Survey India data were used. The analyses were confined to last‐born children aged 6–23 months – 1728 in Bangladesh, 15 028 in India, 1428 in Nepal, 2106 in Sri Lanka and 443 infants aged 6–8 months in Pakistan. Introduction of solid, semi‐solid or soft foods, minimum dietary diversity, minimum meal frequency and minimum acceptable diet, and their significant determinants were compared across the countries. Minimum dietary diversity among children aged 6–23 months ranged from 15% in India to 71% in Sri Lanka, with Nepal (34%) and Bangladesh (42%) in between. Minimum acceptable diet among breastfed children was 9% in India, 32% in Nepal, 40% in Bangladesh and 68% in Sri Lanka. The most consistent determinants of inappropriate complementary feeding practices across all countries were the lack of maternal education and lower household wealth. Limited exposure to media, inadequate antenatal care and lack of post‐natal contacts by health workers were among predictors of inappropriate feeding. Overall, complementary feeding practices among children aged 6–23 months need improvement in all South Asian countries. More intensive interventions are necessary targeting the groups with sup‐optimal practices, while programmes that cover entire populations are being continued.
Keywords: infant feeding, child feeding, infant feeding behaviour, complementary feeding, complementary foods, dietary patterns, South Asia
Introduction
Globally, child undernutrition is the underlying cause of 3.5 million deaths, 35% of the disease burden in children under 5 years of age and 11% of total global disability‐adjusted life years (Black et al. 2008). South Asia has the highest burden of infant and child malnutrition and mortality in the world (Black et al. 2008). Sub‐optimum complementary feeding practices including inadequate feeding frequency, low energy density and insufficient micronutrients are associated with undernutrition in young children (Brown et al. 1998). Therefore, improving infant and young child feeding (IYCF) practices will be of great importance in helping countries in South Asia achieve their Millennium Development Goal of reducing child mortality by two‐thirds between 1990 and 2015 (United Nations 2005).
From 6 months onwards, when breast milk or formula milk alone is no longer sufficient to meet all nutritional requirements, infants need complementary feeding during which they make a gradual transition from breastfeeding/milk feeding to eating family foods. The incidence of malnutrition rises sharply during the period from 6 to 23 months of age in most countries, and the deficits acquired at this age are difficult to compensate for later in childhood. Despite the numerous benefits of appropriate complementary feeding practices during early childhood, it has been previously shown that timely complementary feeding rates in South Asian countries were grossly inadequate (Dibley et al. 2010).
During the past decade, there has been considerable improvement in breastfeeding practices in many countries; however, similar progress has not been made in the area of complementary feeding. While research and development have contributed to an expanding evidence base for recommendations on appropriate feeding and effective interventions for children after 6 months of age, the translation of this new knowledge into action has lagged behind (WHO 2002).
It is important to recognise the factors that are common to South Asia, as the member countries share many common socio‐economic and cultural attributes. Identification of the modifiable factors, which are consistent across several countries, would be essential for building effective nutritional interventions by targeting individuals, families and communities at risk for suboptimal feeding behaviours. Despite these commonalities, some countries lag behind in their ability to improve infant feeding practices, and consequently reduce child undernutrition, and those countries could potentially learn from others that have lower rates of undernutrition (International Institute for Population Sciences 2007). Across‐country comparisons may thus be useful to understand these unique characteristics of each country and develop locally acceptable interventions to improve their infant feeding practices. These comparisons may also be beneficial to regional development assistance partner organisations for the purpose of resource allocation and programme evaluation (Dibley et al. 2010).
Previously, a comparison of key IYCF indicators has been compiled in the Infant and Young Child Feeding Update using the Demographic and Health Survey (DHS) results by Mukuria et al. (2006); however, the new complementary indicators were not available when this report was prepared. Recently, the World Health Organization (WHO) has compiled country profiles using the new IYCF indicators, but there was no comparison according to socio‐demographic or other characteristics (WHO et al. 2010a). The present paper aims to compare the key indicators of complementary feeding in children aged 6–23 months among five South Asian countries – Bangladesh, India, Nepal, Pakistan and Sri Lanka – using the latest available DHS data. It also aims to identify and discuss the socio‐demographic and other factors associated with inappropriate complementary feeding practices across these countries.
Key messages
-
•
Complementary feeding practices among children aged 6–23 months were not satisfactory across the South Asian countries, with the lowest rate in India and the highest in Sri Lanka.
-
•
The most consistent determinants of inappropriate complementary feeding practices across all countries were the low level of maternal education and household poverty.
-
•
Limited exposure to media was also found to be a predictor for poor practices.
-
•
Inadequate antenatal care, untrained assistance at delivery and lack of post‐natal contacts by health workers were among the health service factors that were associated with inappropriate feeding.
Methods
Data sources
The present analysis included the most recent DHS data of Bangladesh 2007 (National Institute of Population Research and Training et al. 2009), Nepal 2006 (Ministry of Health and Population 2006), Sri Lanka 2006–2007 (Department of Census and Statistics & Ministry of Healthcare and Nutrition 2009), Pakistan 2006–2007 (National Institute of Population Studies & Macro International Inc. 2008) and the third National Family Health Survey (NFHS) of India 2005–2006 (International Institute for Population Sciences 2007). Data on types of food and feeding frequency were not available in the Pakistan DHS data set; thus, the analysis was restricted to the introduction of complementary foods.
Survey designs
The details of survey methodology, sampling procedures and the questionnaires are available in the respective DHS and NFHS reports and are also described in the individual country papers in this supplement. All surveys have used a multi‐stage cluster sampling design and interviewed ever‐married women in the reproductive age group from the selected households. The response rate of ever‐married women in the age group 15–49 years was 98.4% in Bangladesh, 94.5% in India, 98.4% in Nepal and 97.5% in Sri Lanka. The corresponding rate in women aged 12–49 years in Pakistan was 94.5%. The present analysis was confined to last‐born children aged 6–23 months living with the respondent and included 1728 children in Bangladesh, 15 028 in India, 1428 in Nepal and 2106 in Sri Lanka. The number of infants aged 6–8 months in Pakistan was 443. All surveys have followed similar data collection methods using standard questionnaire; however, the number of individual food items listed in the questionnaires varied from country to country because of the different country‐specific foods available for young children.
Data sets for Bangladesh, Nepal, India and Pakistan were available in the public domain, while special permission was obtained from the relevant authority for the data from Sri Lanka. The data used in these analyses were de‐identified; thus, no ethical clearance for these secondary data analyses was required.
Complementary feeding indicators and explanatory factors
Analyses for all the countries, except Pakistan, used the new and updated IYCF indicators recommended by the WHO (Daelmans et al. 2009; WHO et al. 2010a), which were based on mother's recall of foods given to her child in the 24 h before the survey. These indicators were: the introduction of solid, semi‐solid or soft foods (the proportion of infants 6–8 months of age who receive solid, semi‐solid or soft foods); the minimum dietary diversity [the proportion of children 6–23 months of age who receive foods from four or more food groups of the seven food groups – (1) grains, roots and tubers; (2) legumes and nuts; (3) dairy products; (4) flesh foods; (5) eggs; (6) vitamin‐A‐rich fruits and vegetables; and (7) other fruits and vegetables]; the minimum meal frequency (the proportion of children 6–23 months of age who receive solid, semi‐solid or soft foods the minimum number of times or more) and the minimum acceptable diet for the breastfed child (the proportion of breastfed children 6–23 months of age who had at least the minimum dietary diversity and the minimum meal frequency during the previous day). The calculation of minimal acceptable diet was not possible for non‐breastfed children, thus confined to breastfed children only, because the minimum number of non‐breast milk feeds as in the definition was not available in the DHS data. The consumption of iron‐rich or iron‐fortified foods was also not estimated because the required information especially about consumption of iron‐fortified foods was not collected in these surveys.
For the purpose of better interpretation of results, the independent variables were grouped as characteristics of the child, parents, household, health care services and the community. The child characteristics included sex, age, birth order and having common childhood illnesses. Education of mother and father, age of mother and her working status were among the variables related to parents. The household wealth index and exposure to media were considered as key household characteristics, whereas the nature of residence and geopolitical regions were considered as community level variables. Some standard composite indices, such as the household wealth index, were used across all countries. Wealth index was constructed using principal components analysis to determine the weights for the index based on information collected about household's ownership of consumer goods, dwelling characteristics, source of drinking water, toilet facilities and other characteristics (Filmer & Pritchett 1998). This index was divided into five categories (quintiles), and each household was assigned to one of these categories. While for some attributes, new composite indices were developed in selected countries. For example, the exposure to media was used as a composite index in Sri Lanka, and a mother with adequate exposure was defined as a respondent who reads newspapers at least once a week, or watches television daily or listens to radio daily. But for other countries, the individual elements regarding exposure to media were analysed separately. Consistency of explanatory variables and their categorisation were maintained as far as possible in order to facilitate comparisons across countries.
Statistical analysis
A uniform analytical method was applied across all data sets by a specially trained data analyst from each country. Four complementary feeding indicator variables, namely, introduction of solid, semi‐solid or soft foods, minimum dietary diversity, minimum meal frequency and minimum acceptable diet were examined against a set of independent variables to determine the prevalence and factors associated with inappropriate practices. Statistical analyses were performed using Stata version 10.0 (Stata Corp., College Station, TX, USA) with ‘svy’ commands to estimate prevalence and confidence intervals accounting for cluster sampling design. Multiple logistic regression analyses were used in stepwise backward models in order to determine the factors significantly associated with inappropriate feeding practices. We used a framework of variables to guide our analyses and individually examined each model as we eliminated non‐significant variables, and in some cases tested alternative variables that on theoretical grounds were similar and reported these findings. The odds ratios (OR) with 95% confidence intervals were calculated to assess the adjusted risk of independent variables, and those with P < 0.05 were retained in the final model.
The number of missing values were 210 in Bangladesh, 3492 in India, 105 in Nepal, one in Pakistan and 75 in Sri Lanka. Because the proportions with missing values were relatively small, this may not have a substantial impact on the final results. Details of the statistical analyses have been reported in each of the country‐specific articles in this supplement.
Results
Complementary feeding indicators
The four complementary feeding indicators are tabulated by country in Table 1, and also illustrated in 1, 2, 3, 4. The rates of minimum dietary diversity, meal frequency and acceptable diet were not available for Pakistan. Introduction of solid, semi‐solid or soft foods among 6–8 months aged infants was low in Pakistan (39%), average in India (55%) and higher in Nepal (70%), Bangladesh (71%) and Sri Lanka (84%). The minimum dietary diversity among children aged 6–23 months ranged from a very low rate of 15% in India to 71% in Sri Lanka, while the rates in Nepal (34%) and Bangladesh (42%) fell in between. The minimum meal frequency rate was above 80% in all countries except in India (42%). The rate of minimum acceptable diet among breastfed children was 9% in India, 32% in Nepal, 40% in Bangladesh and 68% in Sri Lanka. The pattern of minimum acceptable diet across countries was almost similar to that of dietary diversity.
Table 1.
Across‐country comparison of complementary feeding indicators in five South Asian countries, 2005–2007
| Country | Year | Introduction of solid, semi‐solid or soft food (6–8 months) | Minimum dietary diversity (6–23 months) | Minimum meal frequency (6–23 months) | Minimum acceptable diet (6–23 months breastfed) | Total children 6–23 months (weighted) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| % | 95% CI | % | 95% CI | % | 95% CI | % | 95% CI | |||
| Bangladesh | 2007 | 71.1 | (64.5, 76.9) | 41.9 | (39.1, 44.8) | 81.1 | (78.6, 83.3) | 39.6 | (36.8, 42.4) | 1 728 |
| India | 2005–2006 | 54.6 | (52.0, 57.1) | 15.2 | (14.4, 16.1) | 41.5 | (40.2, 42.8) | 9.2 | (8.5, 9.9) | 15 028 |
| Nepal | 2006 | 69.7 | (62.4, 76.2) | 34.2 | (30.7, 37.8) | 82.0 | (78.9, 84.7) | 31.8 | (28.5, 35.4) | 1 428 |
| Sri Lanka | 2006–2007 | 83.9 | (78.8, 87.9) | 71.1 | (68.4, 73.7) | 88.3 | (86.5, 90.0) | 67.9 | (65.1, 70.5) | 2 106 |
| Pakistan | 2006–2007 | 39.2 | (33.8, 44.9) | 443* | ||||||
CI, confidence interval. *Number of children aged 6–8 months is given for Pakistan.
Figure 1.
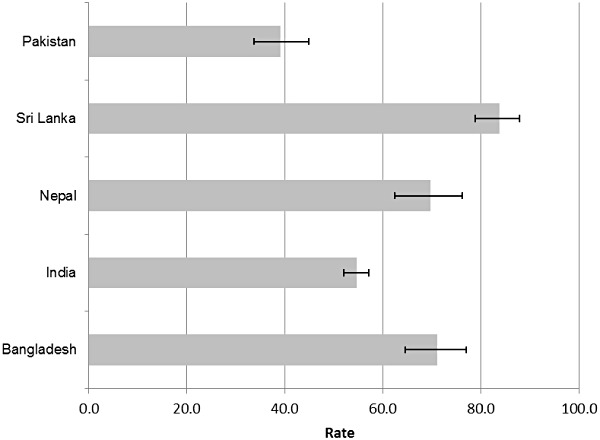
Across‐country comparison of prevalence of introduction of solid, semi‐solid or soft food in infants aged 6–8 months in five South Asian countries, 2005–2007. Error bars in the columns represent 95% confidence intervals.
Figure 2.
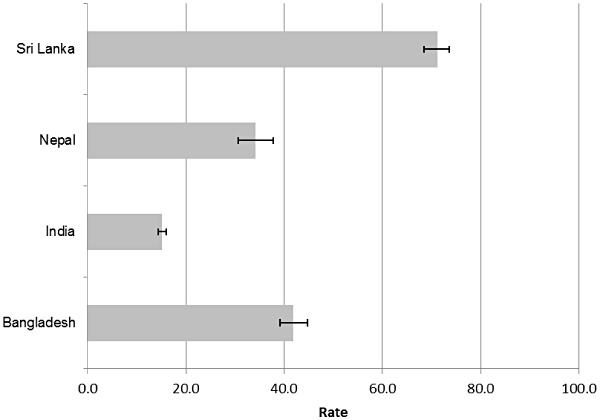
Across‐country comparison of prevalence of minimum dietary diversity in children aged 6–23 months in four South Asian countries, 2005–2007. Error bars in the columns represent 95% confidence intervals.
Figure 3.
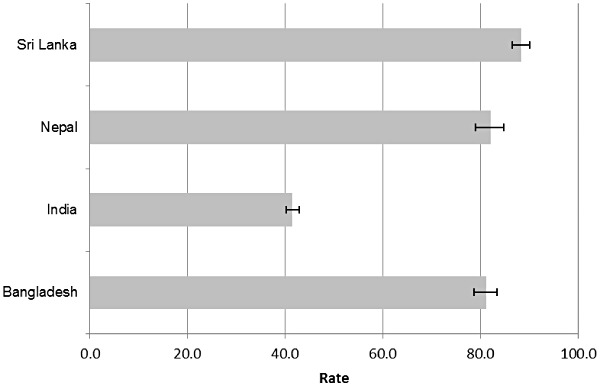
Across‐country comparison of prevalence of minimum meal frequency in children aged 6–23 months in four South Asian countries, 2005–2007. Error bars in the columns represent 95% confidence intervals.
Figure 4.
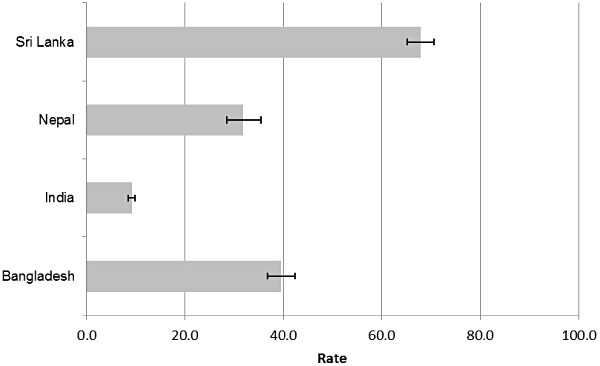
Across‐country comparison of prevalence of minimum acceptable diet for breastfed children aged 6–23 months in four South Asian countries, 2005–2007. Error bars in the columns represent 95% confidence intervals.
Determinants of inappropriate feeding practices
As shown in Table 2, within the 6–8 months age window, rate of introducing solid, semi‐solid or soft foods significantly improved with increasing age in Bangladesh, India and Nepal. Lower maternal education was significantly associated with delayed introduction of complementary foods both in Bangladesh and Nepal. Introduction of complementary food within 6–8 months was significantly delayed in the middle, poorer and poorest families compared with the richest in India and Pakistan. Both in India and Sri Lanka, fewer antenatal clinic visits were associated with delay in the introduction of complementary food. The regional differences in the introduction rates were seen across all countries but were more pronounced in India and Sri Lanka.
Table 2.
Determinants of not introducing solid, semi‐solid or soft food in infants 6–8 months in five South Asian countries (adjusted odds ratios)
| Characteristic | Bangladesh | India | Nepal | Sri Lanka | Pakistan | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 339 | n = 2251 | n = 254 | n = 772 | n = 443 | |||||||||||
| OR | [95% CI] | P | OR | [95% CI] | P | OR | [95% CI] | P | OR | [95% CI] | P | OR | [95% CI] | P | |
| Child characteristics | |||||||||||||||
| Age of child (in months) | 0.62 | (0.41, 0.92) | 0.018 | 0.54 | (0.46, 0.62) | <0.001 | 0.46 | (0.3, 0.7) | 0.001 | ||||||
| Birth order | |||||||||||||||
| First‐born | 1.00 | ||||||||||||||
| 2nd–4th | 1.80 | (0.99, 3.26) | 0.051 | ||||||||||||
| 5 or more | 2.04 | (1.00, 4.14) | 0.049 | ||||||||||||
| Diarrhoea | |||||||||||||||
| No | 1.00 | ||||||||||||||
| Yes | 0.70 | (0.51, 0.96) | 0.026 | ||||||||||||
| Parental characteristics | |||||||||||||||
| Maternal education | |||||||||||||||
| Secondary and above | 1.00 | 1.00 | |||||||||||||
| Primary | 2.31 | (1.07, 4.96) | 0.033 | 9.14 | (2.5, 33.4) | 0.001 | |||||||||
| No education | 2.14 | (1.08, 4.23) | 0.029 | 13.83 | (4.2, 45.3) | <0.001 | |||||||||
| Mother's age | |||||||||||||||
| 35–49 years | 1.00 | ||||||||||||||
| 25–34 years | 3.41 | (0.6, 18.6) | 0.155 | ||||||||||||
| 15–24 years | 5.66 | (1.2, 27.7) | 0.032 | ||||||||||||
| Mother working | |||||||||||||||
| Non‐working | 1.00 | ||||||||||||||
| Working | 2.47 | (1.2, 5.0) | 0.013 | ||||||||||||
| Mother's BMI (kg/m2) | |||||||||||||||
| 18.5–24.9 | 1.00 | ||||||||||||||
| <18.5 | 1.08 | (0.75, 1.54) | 0.679 | ||||||||||||
| ≥25 | 0.63 | (0.44, 0.90) | 0.012 | ||||||||||||
| Father's occupation | |||||||||||||||
| Agricultural | 1.00 | ||||||||||||||
| Non‐agricultural/other/do not know | 3.05 | (1.33, 7.00) | 0.009 | ||||||||||||
| Household characteristics | |||||||||||||||
| Reads newspaper | |||||||||||||||
| Almost everyday | 1.00 | ||||||||||||||
| Not at all/at least once a week | 2.99 | (1.43, 6.26) | 0.004 | ||||||||||||
| Household wealth index | |||||||||||||||
| Richest | 1.00 | 1.00 | |||||||||||||
| Richer | 1.64 | (1.01, 2.68) | 0.046 | 2.22 | (0.99, 4.94) | 0.051 | |||||||||
| Middle | 2.42 | (1.42, 4.13) | 0.001 | 7.82 | (3.49, 17.55) | <0.001 | |||||||||
| Poorer | 2.43 | (1.39, 4.24) | 0.002 | 4.84 | (2.34, 10.45) | <0.001 | |||||||||
| Poorest | 1.58 | (0.91, 2.75) | 0.106 | 5.72 | (2.60, 12.57) | <0.001 | |||||||||
| Religion | |||||||||||||||
| Christian | 1.00 | ||||||||||||||
| Hindu | 2.77 | (1.24, 6.19) | 0.013 | ||||||||||||
| Muslim | 2.15 | (0.93, 4.98) | 0.074 | ||||||||||||
| Others | 4.24 | (1.63, 10.99) | 0.003 | ||||||||||||
| Health care characteristics | |||||||||||||||
| Antenatal clinic visits | |||||||||||||||
| 7+ | 1.00 | 1.00 | |||||||||||||
| 3–6 | 1.55 | (1.01, 2.38) | 0.043 | 1.13 | (0.79, 1.61) | 0.50 | |||||||||
| 1–2 | 1.82 | (1.13, 2.91) | 0.013 | 0.64 | (0.41, 1.00) | 0.05 | |||||||||
| None | 2.05 | (1.23, 3.42) | 0.006 | 2.63 | (0.58, 11.96) | 0.21 | |||||||||
| Community level characteristics | |||||||||||||||
| Geographical region* | |||||||||||||||
| Region 1 | 1.00 | 1.00 | |||||||||||||
| Region 2 | 3.60 | (2.15, 6.00) | <0.001 | 1.33 | (0.88, 2.03) | 0.173 | |||||||||
| Region 3 | 2.77 | (1.71, 4.50) | <0.001 | 0.69 | (0.48, 1.00) | 0.049 | |||||||||
| Region 4 | 1.92 | (1.16, 3.17) | 0.011 | 1.18 | (0.79, 1.77) | 0.420 | |||||||||
| Region 5 | 1.64 | (0.83, 3.21) | 0.151 | 0.95 | (0.60, 1.52) | 0.842 | |||||||||
| Region 6 | 3.05 | (1.75, 5.31) | <0.001 | 1.45 | (0.71, 2.95) | 0.306 | |||||||||
| Region 7 | 1.10 | (0.77, 1.56) | 0.613 | ||||||||||||
| Region 8 | 0.90 | (0.50, 1.63) | 0.735 | ||||||||||||
OR, odds ratio; CI, confidence interval; BMI, body mass index. *Geographical region: Regions 1–6 in India: South; North; Central; East; Northeast; West. Regions 1–8 in Sri Lanka: Western Province; Central Province; Southern Province; Eastern Province; North Western Province; North Central Province; Uva Province; Sabaragamuwa Province.
Table 3 reveals that the dietary diversity was poor in lower age categories especially in the 6–11 months group in most countries. Mothers with little or no education were a significant predictor of poor dietary diversity across all countries. Children of working mothers were at a higher risk for inadequate dietary diversity in Nepal, while in contrast they were at a lower risk in Sri Lanka. Children from the lower household wealth categories, especially the poorer and poorest did not have adequate dietary diversity compared with the richest in all four countries. Both in India and Nepal, inadequate maternal exposure to media, such as newspaper, radio or television, was found to be a predictor of inadequate dietary diversity. Among the health service factors, fewer antenatal clinic visits or lack of post‐natal check‐ups were found as significant determinants of poor dietary diversity. As in other indicators, the regional differences within country were observed in relation to dietary diversity.
Table 3.
Determinants of inappropriate dietary diversity in children 6–23 months in four South Asian countries (adjusted odds ratios)
| Characteristic | Bangladesh | India | Nepal | Sri Lanka | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 1518 | n = 11 536 | n = 1428 | n = 2106 | |||||||||
| OR | [95% CI] | P | OR | [95% CI] | P | OR | [95% CI] | P | OR | [95% CI] | P | |
| Child characteristics | ||||||||||||
| Child age | ||||||||||||
| 18–23 | 1.00 | 1.00 | 1.00 | |||||||||
| 12–17 | 1.72 | (1.27, 2.32) | <0.001 | 1.35 | (1.14, 1.60) | <0.001 | 1.37 | (1.05, 1.80) | 0.023 | |||
| 6–11 | 7.78 | (5.53, 10.94) | <0.001 | 6.34 | (5.05, 7.95) | <0.001 | 4.71 | (3.53, 6.29) | <0.001 | |||
| Acute respiratory infection | ||||||||||||
| No | 1.00 | |||||||||||
| Yes | 2.08 | (1.22, 3.54) | 0.007 | |||||||||
| Parental characteristics | ||||||||||||
| Maternal education* | ||||||||||||
| Secondary and above | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Primary | 1.41 | (1.03, 1.94) | 0.034 | 1.11 | (0.89, 1.39) | 0.362 | 1.48 | (0.95, 2.30) | 0.085 | 1.97 | (1.38, 2.82) | <0.001 |
| No education | 1.70 | (1.14, 2.54) | 0.01 | 1.70 | (1.40, 2.08) | <0.001 | 1.94 | (1.31, 2.88) | 0.001 | 1.48 | (1.11, 1.98) | 0.009 |
| Mother working | ||||||||||||
| Non‐working | 1.00 | 1.00 | ||||||||||
| Working | 1.48 | (1.08, 2.01) | 0.014 | 0.71 | (0.52, 0.98) | 0.040 | ||||||
| Mother's height (cm) | ||||||||||||
| More than 155 | 1.00 | |||||||||||
| 150–155 | 1.45 | (1.11, 1.89) | 0.006 | |||||||||
| Less than 150 | 1.06 | (0.84, 1.34) | 0.637 | |||||||||
| Mother's BMI (kg/m2) | ||||||||||||
| ≥18 | 1.00 | |||||||||||
| <18.5 | 1.18 | (1.00, 1.39) | 0.045 | |||||||||
| Household characteristics | ||||||||||||
| Decision making at household | 1.00 | |||||||||||
| Mother involved | 1.33 | (1.03, 1.71) | 0.028 | |||||||||
| Mother not involved | ||||||||||||
| Household wealth index | ||||||||||||
| Richest | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Richer | 1.18 | (0.74, 1.89) | 0.49 | 1.00 | (0.80, 1.24) | 0.994 | 2.19 | (1.28, 3.75) | 0.005 | 1.12 | (0.75, 1.68) | 0.579 |
| Middle | 1.35 | (0.83, 2.19) | 0.23 | 1.28 | (0.99, 1.65) | 0.057 | 2.63 | (1.46, 4.72) | 0.001 | 1.79 | (1.19, 2.68) | 0.005 |
| Poorer | 2.16 | (1.23, 3.77) | 0.007 | 1.19 | (0.90, 1.59) | 0.226 | 2.94 | (1.60, 5.43) | 0.001 | 1.85 | (1.16, 2.97) | 0.010 |
| Poorest | 2.63 | (1.39, 4.94) | 0.003 | 1.84 | (1.31, 2.60) | <0.001 | 2.91 | (1.54, 5.47) | 0.001 | 2.05 | (1.32, 3.19) | 0.001 |
| Reads newspaper | ||||||||||||
| Almost everyday | 1.00 | |||||||||||
| Not at all/at least once a week | 1.75 | (1.37, 2.25) | <0.001 | |||||||||
| Watches television | ||||||||||||
| Almost everyday | 1.00 | |||||||||||
| Not at all/at least once a week | 1.27 | (1.07, 1.51) | 0.006 | |||||||||
| Listens to radio | ||||||||||||
| Almost everyday | 1.00 | |||||||||||
| Not at all/at least once a week | 1.41 | (1.02, 1.94) | 0.036 | |||||||||
| Health care characteristics | ||||||||||||
| Antenatal clinic visits | ||||||||||||
| ≥7 | 1.00 | 1.00 | ||||||||||
| 4–6 | 1.52 | (1.24, 1.85) | <0.001 | 1.00 | 1.30 | (1.01, 1.66) | 0.04 | |||||
| 1–3 | 1.76 | (1.36, 2.26) | <0.001 | 1.37 | (1.01, 1.86) | 1.20 | (0.84, 1.73) | 0.31 | ||||
| Unknown/none | 1.92 | (1.40, 2.63) | <0.001 | 1.66 | (1.12, 2.46) | 0.67 | (0.26, 1.76) | 0.42 | ||||
| No. of post‐natal home visits by PHM | ||||||||||||
| ≥3 | 1.00 | |||||||||||
| 2 | 0.89 | (0.65, 1.22) | 0.457 | |||||||||
| 1 | 1.44 | (1.08, 1.92) | 0.013 | |||||||||
| None | 1.57 | (1.13, 2.17) | 0.007 | |||||||||
| Timing of post‐natal check‐up | ||||||||||||
| 7+ days | 1.00 | |||||||||||
| 0–2 days | 0.97 | (0.73, 1.30) | 0.842 | |||||||||
| 3–6 days | 0.58 | (0.39, 0.84) | 0.004 | |||||||||
| No check‐ups | 1.25 | (1.02, 1.52) | 0.029 | |||||||||
| Community level characteristics | ||||||||||||
| Type of residence | ||||||||||||
| Urban | 1.00 | |||||||||||
| Rural | 0.99 | (0.70, 1.39) | 0.947 | |||||||||
| Estate | 2.38 | (1.49, 3.80) | <0.001 | |||||||||
| Geographical region † | ||||||||||||
| Region 1 | 1.00 | 1.00 | 1.00 | |||||||||
| Region 2 | 4.007 | (2.01, 8.00) | <0.001 | 1.34 | (1.04, 1.72) | 0.022 | 0.85 | (0.57, 1.26) | 0.412 | |||
| Region 3 | 1.69 | (1.15, 2.48) | 0.008 | 1.12 | (0.86, 1.46) | 0.382 | 0.93 | (0.64, 1.37) | 0.727 | |||
| Region 4 | 1.39 | (0.894, 2.149) | 0.144 | 0.59 | (0.46, 0.76) | <0.001 | 1.75 | (1.13, 2.72) | 0.012 | |||
| Region 5 | 2.25 | (1.48, 3.43) | <0.001 | 0.81 | (0.60, 1.11) | 0.188 | 1.31 | (0.91, 1.87) | 0.146 | |||
| Region 6 | 1.98 | (1.20, 3.26) | 0.008 | 2.17 | (1.55, 3.02) | <0.001 | 1.60 | (0.93, 2.76) | 0.089 | |||
| Region 7 | 1.46 | (0.80, 2.67) | 0.217 | |||||||||
| Region 8 | 0.84 | (0.55, 1.27) | 0.404 | |||||||||
OR, odds ratio; CI, confidence interval; BMI, body mass index; PHM, Public Health Midwife. Minimum dietary diversity was defined as the proportion of children 6–23 months of age who receive foods from four or more food groups of the seven food groups – grains, roots and tubers; legumes and nuts; dairy products; flesh foods; eggs; vitamin‐A‐rich fruits and vegetables; and other fruits and vegetables. *Maternal education categories for Sri Lanka were: Higher; Secondary; No schooling or primary. †Geographical region: Regions 1–6 in Bangladesh: Rajshahi; Sylhet; Dhaka; Khulna; Chittagong; Barisal. Regions 1–6 in India: South; North; Central; East; Northeast; West. Regions 1–8 In Sri Lanka: Western Province; Central Province; Southern Province; Eastern Province; North Western Province; North Central Province; Uva Province; Sabaragamuwa Province.
Table 4 describes the adjusted OR for the association between risk factors and inadequate meal frequency among children aged 6–23 months across the four countries. The child's age was significantly associated with complementary feeding practices, and children of lower age showed alarmingly inadequate meal frequency in all four countries. Poor maternal education was another common predictor for inadequate meal frequency. A contradictory association was observed with respect to mother's working status between India and Nepal: ‘working mother’ was a protective factor against inadequate meal frequency in India, whereas it was a risk factor in Nepal. Unlike other indicators, the household wealth index was not strongly associated with inadequate meal frequency, except for India. Inadequate exposure to media, fewer antenatal clinic visits and geographical region were the other common risk factors for not meeting the required meal frequency.
Table 4.
Determinants of inadequate meal frequency in children 6–23 months in four South Asian countries (adjusted odds ratios)
| Characteristic | Bangladesh | India | Nepal | Sri Lanka | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 1518 | n = 11 536 | n = 1428 | n = 2106 | |||||||||
| OR | [95% CI] | P | OR | [95% CI] | P | OR | [95% CI] | P | OR | [95% CI] | P | |
| Child characteristics | ||||||||||||
| Child age | ||||||||||||
| 18–23 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 12–17 | 2.43 | (1.45, 4.08) | 0.00 | 1.37 | (1.21, 1.55) | <0.001 | 1.74 | (1.02, 2.98) | 0.04 | 1.30 | (0.85, 1.99) | 0.231 |
| 6–11 | 8.89 | (5.56, 14.21) | <0.001 | 2.15 | (1.87, 2.46) | <0.001 | 4.46 | (2.67, 7.46) | <0.001 | 3.09 | (1.99, 4.81) | <0.001 |
| Parental characteristics | ||||||||||||
| Maternal education | ||||||||||||
| Secondary and above | 1.00 | 1.00 | 1.00 | |||||||||
| Primary | 1.26 | (0.88, 1.82) | 0.21 | 1.28 | (1.08, 1.53) | 0.005 | 2.23 | (1.13, 4.41) | 0.02 | |||
| No education | 1.70 | (1.09, 2.67) | 0.02 | 1.26 | (1.08, 1.46) | 0.002 | 3.06 | (1.67, 5.63) | <0.001 | |||
| Mother working | ||||||||||||
| Non‐working | 1.00 | 1.00 | ||||||||||
| Working | 0.85 | (0.74, 0.96) | 0.012 | 1.91 | (1.35, 2.69) | <0.001 | ||||||
| Mother's BMI (kg/m2) | ||||||||||||
| 18.5–24.9 | 1.00 | |||||||||||
| <18.5 | 1.60 | (1.15, 2.22) | 0.005 | |||||||||
| ≥25 | 1.05 | (0.66, 1.67) | 0.846 | |||||||||
| Household characteristics | ||||||||||||
| Decision making at household | ||||||||||||
| Mother involved | 1.00 | |||||||||||
| Mother not involved | 1.20 | (1.04, 1.38) | 0.015 | |||||||||
| Household wealth index | ||||||||||||
| Richest | 1.00 | |||||||||||
| Richer | 1.35 | (1.11, 1.63) | 0.002 | |||||||||
| Middle | 1.44 | (1.16, 1.79) | 0.001 | |||||||||
| Poorer | 1.44 | (1.14, 1.82) | 0.002 | |||||||||
| Poorest | 1.39 | (1.09, 1.78) | 0.008 | |||||||||
| Reads newspaper | ||||||||||||
| Almost everyday | 1.00 | |||||||||||
| Not at all/at least once a week | 1.33 | (1.05, 1.69) | 0.017 | |||||||||
| Listens to radio | ||||||||||||
| Almost everyday | 1.00 | |||||||||||
| Not at all/At least once a week | 1.25 | (1.08, 1.45) | 0.002 | |||||||||
| Watches television | ||||||||||||
| Almost everyday | 1.00 | |||||||||||
| Not at all/At least once a week | 1.82 | (1.14, 2.89) | <0.001 | |||||||||
| Exposure to media | ||||||||||||
| Satisfactory | 1.00 | |||||||||||
| Limited | 1.55 | (1.08, 2.21) | 0.015 | |||||||||
| Health care characteristics | ||||||||||||
| Antenatal clinic visits | ||||||||||||
| ≥7 | 1.00 | 1.00 | ||||||||||
| 4–6 | 1.32 | (1.11, 1.58) | 0.002 | 1.56 | (1.10, 2.21) | 0.014 | ||||||
| 1–3 | 1.43 | (1.17, 1.76) | 0.001 | 1.54 | (1.00, 2.36) | 0.048 | ||||||
| Unknown/none | 1.18 | (0.94, 1.48) | 0.164 | 1.65 | (0.50, 5.48) | 0.411 | ||||||
| Antenatal home visits by PHM | ||||||||||||
| Yes | 1.00 | |||||||||||
| No | 1.85 | (1.26, 2.73) | 0.002 | |||||||||
| Community level characteristics | ||||||||||||
| Type of residence | ||||||||||||
| Rural | 1.00 | |||||||||||
| Urban | 2.00 | (1.23, 3.25) | 0.005 | |||||||||
| Geographical region* | ||||||||||||
| Region 1 | 1.00 | 1.00 | 1.00 | |||||||||
| Region 2 | 3.40 | (1.67, 6.94) | <0.001 | 1.24 | (1.01, 1.51) | 0.040 | 3.16 | (1.87, 5.34) | <0.001 | |||
| Region 3 | 1.63 | (0.96, 2.76) | 0.07 | 1.12 | (0.92, 1.36) | 0.269 | 1.51 | (0.89, 2.55) | 0.124 | |||
| Region 4 | 1.02 | (0.50, 2.07) | 0.96 | 0.74 | (0.60, 0.90) | 0.003 | 1.24 | (0.68, 2.27) | 0.477 | |||
| Region 5 | 4.52 | (2.57, 7.94) | <0.001 | 0.99 | (0.78, 1.26) | 0.938 | 1.40 | (0.62, 3.18) | 0.417 | |||
| Region 6 | 3.40 | (1.82, 6.35) | <0.001 | 1.55 | (1.21, 1.99) | 0.001 | 3.97 | (2.31, 6.82) | <0.001 | |||
| Region 7 | 2.65 | (1.52, 4.62) | 0.001 | |||||||||
| Region 8 | 1.13 | (0.51, 2.50) | 0.770 | |||||||||
OR, odds ratio; CI, confidence interval; BMI, body mass index; PHM, Public Health Midwife. Minimum meal frequency was defined as the proportion of children 6–23 months of age who receive solid, semi‐solid, or soft foods the minimum number of times or more. *Geographical region: Regions 1–6 in Bangladesh: Rajshahi; Sylhet; Dhaka; Khulna; Chittagong; Barisal. Regions 1–6 in India: South; North; Central; East; Northeast; West. Regions 1–8 In Sri Lanka: Western Province; Central Province; Southern Province; Eastern Province; North Western Province; North Central Province; Uva Province; Sabaragamuwa Province.
The factors that were associated with failure to receive the minimum acceptable diet in breastfed children are summarised in Table 5. A higher percentage of children from younger age groups failed to receive the minimum acceptable diet than older children across all the countries. Poor maternal education was a significant determinant that was consistently found across all four countries. Children from the families of middle, poorer or poorest wealth quintiles had a greater risk in India, Nepal and Sri Lanka. Limited exposure to media was found to be a risk in India and Sri Lanka. Among the health service factors, delivery at health facility and delivery assistance by non‐professionals in Bangladesh, fewer antenatal checks in India and less post‐natal home visits by a public health midwife in Sri Lanka were associated with poor acceptable diet. Significant regional differences in this indicator were observed in each country. Mothers living in the tea estate sector in Sri Lanka reported significantly lower minimum acceptable diet.
Table 5.
Determinants of not meeting the minimum acceptable diet for breasted children 6–23 months in four South Asian countries (adjusted odds ratios)
| Characteristic | Bangladesh | India | Nepal | Sri Lanka | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n = 1518 | n = 10 164 | n = 1393 | n = 1920 | |||||||||
| OR | [95% CI] | P | OR | [95% CI] | P | OR | [95% CI] | P | OR | [95% CI] | P | |
| Child characteristics | ||||||||||||
| Child age | ||||||||||||
| 18–23 | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| 12–17 | 1.54 | (1.15, 2.06) | 0.004 | 1.46 | (1.17, 1.82) | 0.001 | 1.12 | (0.82, 1.54) | 0.474 | 1.24 | (0.96, 1.59) | 0.096 |
| 6–11 | 6.22 | (4.39, 8.81) | <0.001 | 5.14 | (3.94, 6.71) | <0.001 | 3.13 | (2.16, 4.53) | <0.001 | 3.61 | (2.71, 4.79) | <0.001 |
| Acute respiratory infections | ||||||||||||
| No | 1.00 | |||||||||||
| Yes | 2.13 | (1.37, 3.31) | 0.001 | |||||||||
| Parental characteristics | ||||||||||||
| Maternal education* | ||||||||||||
| Secondary and above | 1.00 | 1.00 | 1.00 | 1.00 | ||||||||
| Primary | 1.36 | (1.01, 1.84) | 0.046 | 0.98 | (0.74, 1.29) | 0.889 | 1.68 | (1.08, 2.62) | 0.021 | 1.84 | (1.24, 2.76) | 0.003 |
| No education | 1.73 | (1.20, 2.49) | 0.003 | 1.47 | (1.12, 1.93) | 0.005 | 2.67 | (1.84, 3.89) | <0.001 | 1.48 | (1.21, 1.96) | 0.006 |
| Mother working | ||||||||||||
| Non‐working | 1.00 | |||||||||||
| Working | 1.54 | (1.11, 2.14) | 0.01 | |||||||||
| Mother's height (cm) | ||||||||||||
| More than 155 | 1.00 | |||||||||||
| 150–155 | 1.34 | (1.05, 1.72) | 0.021 | |||||||||
| Less than 150 | 1.03 | (0.83, 1.27) | 0.800 | |||||||||
| Mother's BMI (kg/m2) | ||||||||||||
| ≥18 | 1.00 | |||||||||||
| <18.5 | 1.29 | (1.05, 1.60) | 0.016 | |||||||||
| Household characteristics | ||||||||||||
| Decision making at household | ||||||||||||
| Mother involved | ||||||||||||
| Mother not involved | ||||||||||||
| Household wealth index | ||||||||||||
| Richest | 1.00 | 1.00 | 1.00 | |||||||||
| Richer | 1.26 | (0.96, 1.64) | 0.092 | 1.75 | (1.04, 2.94) | 0.037 | 1.10 | (0.75, 1.61) | 0.618 | |||
| Middle | 1.86 | (1.37, 2.53) | <0.001 | 2.17 | (1.17, 4.04) | 0.014 | 1.45 | (1.00, 2.10) | 0.049 | |||
| Poorer | 1.56 | (1.12, 2.16) | 0.008 | 2.42 | (1.26, 4.67) | 0.008 | 1.52 | (1.00, 2.31) | 0.050 | |||
| Poorest | 3.07 | (1.98, 4.77) | <0.001 | 2.32 | (1.23, 4.36) | 0.009 | 1.45 | (0.94, 2.24) | 0.089 | |||
| Reads newspaper | ||||||||||||
| Almost everyday | 1.00 | |||||||||||
| Not at all/at least once a week | 1.55 | (1.15, 2.08) | 0.004 | |||||||||
| Listens to radio | ||||||||||||
| Almost everyday | 1.00 | |||||||||||
| Not at all/At least once a week | 1.34 | (1.06, 1.70) | 0.014 | |||||||||
| Exposure to media | ||||||||||||
| Satisfactory | 1.00 | |||||||||||
| Limited | 1.36 | (1.01, 1.85) | 0.044 | |||||||||
| Health care characteristics | ||||||||||||
| Delivery assistance | ||||||||||||
| Health professional | 1.00 | |||||||||||
| Traditional birth attendance | 3.41 | (1.17, 9.93) | 0.025 | |||||||||
| Other untrained | 2.41 | (1.26, 4.63) | 0.008 | |||||||||
| Antenatal clinic visits | ||||||||||||
| ≥7 | 1.00 | |||||||||||
| 4–6 | 1.95 | (1.53, 2.49) | <0.001 | |||||||||
| 1–3 | 2.64 | (1.94, 3.60) | <0.001 | |||||||||
| Unknown/none | 2.58 | (1.77, 3.76) | <0.001 | |||||||||
| Post‐natal home visits by PHM | ||||||||||||
| ≥3 | 1.00 | |||||||||||
| 2 | 0.90 | (0.67, 1.21) | 0.482 | |||||||||
| 1 | 1.34 | (1.02, 1.76) | 0.033 | |||||||||
| None | 1.71 | (1.22, 2.38) | 0.002 | |||||||||
| Community level characteristics | ||||||||||||
| Type of residence | ||||||||||||
| Urban | 1.00 | |||||||||||
| Rural | 0.82 | (0.58, 1.17) | 0.266 | |||||||||
| Estate | 2.04 | (1.23, 3.38) | 0.006 | |||||||||
| Geographical region † | ||||||||||||
| Region 1 | 1.00 | 1.00 | 1.00 | |||||||||
| Region 2 | 3.44 | (1.82, 6.47) | <0.001 | 1.48 | (1.10, 1.98) | 0.009 | 1.15 | (0.70, 1.91) | 0.579 | |||
| Region 3 | 1.74 | (1.19, 2.55) | 0.004 | 1.15 | (0.85, 1.56) | 0.363 | 0.98 | (0.70, 1.38) | 0.924 | |||
| Region 4 | 1.30 | (0.86, 1.97) | 0.213 | 0.65 | (0.48, 0.87) | 0.003 | 1.77 | (1.16, 2.70) | 0.008 | |||
| Region 5 | 2.19 | (1.50, 3.19) | 0.000 | 1.08 | (0.77, 1.53) | 0.657 | 1.23 | (0.85, 1.78) | 0.262 | |||
| Region 6 | 2.14 | (1.24, 3.68) | 0.003 | 2.19 | (1.43, 3.37) | <0.001 | 1.80 | (1.11, 2.88) | 0.016 | |||
| Region 7 | 1.58 | (0.94, 2.66) | 0.082 | |||||||||
| Region 8 | 0.90 | (0.59, 1.36) | 0.614 | |||||||||
OR, odds ratio; CI, confidence interval; BMI, body mass index; PHM, Public Health Midwife. Minimum acceptable diet was defined as the proportion of breastfed children 6–23 months of age who had at least the minimum dietary diversity and the minimum meal frequency. *Maternal education categories for Sri Lanka were: Higher; Secondary; No schooling or primary. †Geographical Region: Regions 1–6 in Bangladesh: Rajshahi; Sylhet; Dhaka; Khulna; Chittagong; Barisal. Regions 1–6 in India: South; North; Central; East; Northeast; West. Regions 1–8 In Sri Lanka: Western Province; Central Province; Southern Province; Eastern Province; North Western Province; North Central Province; Uva Province; Sabaragamuwa Province.
The analyses did not reveal any association between sex of the child and feeding practices in any of the five South Asian countries.
Discussion
The present series of articles used complementary feeding indicators as the main outcome variable because this has not been investigated in detail before, and also with the strong belief that countries can enhance complementary feeding by effectively addressing the determinants of sub‐standard practices. The comparisons of the complementary feeding indicators between the four countries in South Asia showed a consistent pattern ranging from the lowest in India to the highest in Sri Lanka, while the rates in Nepal and Bangladesh were falling in between, with marginally higher rates in Bangladesh than Nepal. The minimum meal frequency was satisfactory (above 80%) in Bangladesh, Nepal and Sri Lanka. However, the minimum dietary diversity and minimum acceptable diet were less than 50% in all except Sri Lanka. The minimum dietary diversity in children 6–23 months varied from 15% in India to 71% in Sri Lanka, whereas the minimum acceptable diet in breastfed children varied from 9% in India to 68% in Sri Lanka.
The pattern of minimum acceptable diet among breastfed children was almost similar to that of dietary diversity; however, the corresponding rates were 2–6% lower than the diversity. The lowest rate was in India indicating an alarming situation because the large population and the extent of the problem indicated that a very large child population did not have a minimal acceptable diet. This analysis cannot make comments about Pakistan except for the only available indicator, the introduction of complementary food, which was low compared with all the other four countries.
The high level of stunting in many countries in South Asia indicates the extent to which complementary feeding practices are inadequate. For example, in India, the rate of stunting (proportion of children under 5 years of age with height‐for‐age less than −2Z) was 48% and the complementary feeding practices were very poor, compared with Sri Lanka which had relatively low rate of stunting (17%) and better complementary feeding practices (International Institute for Population Sciences 2007; Department of Census and Statistics & Ministry of Healthcare and Nutrition 2009).
One of the reasons for Sri Lanka to have better complementary feeding indicators is the higher level of women's education and literacy in the country, despite inequalities in income or wealth. In Sri Lanka, the female literacy rate was 90%, and almost 94% had some form of school education (Department of Census and Statistics & Ministry of Healthcare and Nutrition 2009, Department of Census and Statistics 2010). The well‐organised state health services have also contributed to this success. The health staff is regularly trained on IYCF counselling, and the messages are delivered during antenatal home and clinic visits, child welfare clinics and post‐natal home visits by the public health midwives and other health staff throughout the country.
According to the present analysis, the most consistent determinant of inappropriate complementary feeding practices across all countries was the lack of maternal education. Children in households from the lower quintiles of household wealth were found to have a low dietary diversity and acceptable diet in almost all countries. This study also revealed that the limited exposure to media was an important determinant for most indicators. Inadequate antenatal care, untrained assistance at delivery and lack of post‐natal contacts by health workers were among the health service factors that predict inappropriate feeding, indicating the importance of continuum of care from the antenatal period in promoting appropriate IYCF practices.
There were only a few previous studies that examined factors associated with complementary feeding practices in children. According to some studies, dietary diversity has been influenced by socio‐economic factors (Bernal Rivas & Lorenzana Albert 2003; Ministry of Healthcare and Nutrition & UNICEF 2008; Jayatissa & Hossain 2010). The present study provides the strongest evidence for this association and reveals that poor maternal education and lower household wealth were significant factors associated with inadequate dietary diversity, meal frequency and acceptable diet across South Asia.
This comparison identified a set of consistent determinants across the region despite different levels of these indicators in each country. All the surveys have been conducted within a limited time span; thus, the influence of timing in for differences would be minimal. The DHSs used a common survey methodology, standard procedures and a common questionnaire with only minor adaptations to country settings. Further, the present analyses have used the standard definitions with clear operational guidelines released by the WHO (WHO et al. 2010b). There was high degree of similarity in the survey procedures and methods used across the country studies. In addition to the policy makers and programme managers within each country, this information would be useful for regional level health and development assistance partners and researchers to make regional level policies and strategies within their programmes to improve IYCF.
The main limitation was the cross‐sectional nature of the surveys and the 24‐h recall data regarding IYCF. The 24‐h recall based on maternal recall has the potential for respondent bias such as the tendency to give socially desirable answers. Nutritional adequacy of diet could not be assessed because of absence of quantitative information on the amount of food fed. However, the appropriate statistical adjustments for survey design and modelling for confounding effects add strength to the validity of the findings. Despite few limitations, we found some common determinants across the countries that could be epidemiologically plausible. For example, maternal illiteracy and household poverty were common factors that can be explainable and useful for policies and programmes.
Another important observation made through this comparison was the close relationship between minimum dietary diversity and minimum acceptable diet. The rate of minimum acceptable diet was close to that of dietary diversity in countries where the minimum meal frequency was high, for example above 80%. This relationship can be observed in the country profiles in the WHO indicators for IYCF Part III (WHO et al. 2010a). There is sufficient evidence that dietary diversity is an important predictor of nutritional adequacy, especially micronutrient intake. So, dietary diversity can be regarded as a simple and useful indicator (Steyn et al. 2006; Kennedy et al. 2007; Moursi et al. 2008). However, it has been found that food group diversity indicators derived from qualitative list‐based questionnaire misreported some foods compared with same indicators derived from quantitative 24‐h recall in the assessment of micronutrient adequacy womens' diets (Martin‐Prevel et al. 2010). Thus, it would be useful to further explore how each individual food group contributes to nutritional adequacy of a diet among young children.
Age of child was a significant determinant of complementary feeding practices. Indicators of complementary feeding were consistently inappropriate in relation to those recommended for their age in younger children compared with older children. Therefore, health programmes should take measures to support younger age groups probably through antenatal and early post‐natal contacts. There was no single factor that predicts delay in introducing solid, semi‐solid or soft foods common to all countries. However, the factors that were consistent in more than one country were lower maternal education, poor household wealth categories and inadequate antenatal clinic visits.
What are the implications of this comparison for policy, practice and research? The alarmingly low level of adherence to the WHO recommended complementary feeding indicators across the region itself demands attention at national and regional level organisations to make a collective effort to combat the problem of poor IYCF. This analysis should be a baseline assessment to set goals, objectives and targets in health programmes. Further, this would be an eye‐opener for one country to explore policies, programmes and strategies of another which had better indicators. More consistent determinants should be used to target interventions – for example children of uneducated women, average‐to‐poorest income families may be targeted because such groups are at a greater risk irrespective of their country. These findings are relevant to researchers and should help them to design and evaluate interventions and assess their cost‐effectiveness for improving IYCF practices and reducing child undernutrition. For example, multi‐country trials that involve interventions such as extended peer counselling and use of community facilitators need to be tested on target groups or populations with inappropriate practices. Because Pakistan DHS did not have details of foods given to infants, we suggest that the subsequent household surveys in Pakistan should include such data.
In conclusion, the complementary feeding practices among children aged 6–23 months were not satisfactory across the South Asian countries included in this study. There were wide variations in the rates of minimum dietary diversity and acceptable diet across countries with the lowest rates in India and the highest in Sri Lanka. The most consistent determinants of inappropriate complementary feeding practices across all countries were the lack of maternal education and the lower household wealth quintiles. Limited exposure to media was also found as a predictor for most indicators. Inadequate antenatal care, untrained assistance at delivery and lack of post‐natal contacts by health workers were among the health service factors that predict inappropriate feeding. More intensive counselling of mothers through peers, community facilitators and health care providers would be necessary targeting the groups with sup‐optimal practices, while continuing with programmes that cover the entire population.
Contributions
US had the main responsibility to compile the manuscript, KEA was responsible for statistical analyses, and all others (DSA, SSPG, TH, HJ, NJ, IK, MK, AP, YP, SKR, IS, KT and MJD) contributed equally to concept, design, analyses and manuscript writing.
References
- Bernal Rivas J. & Lorenzana Albert P. (2003) Dietary diversity and associated factors among beneficiaries of 77 child care centers, Central Regional, Venezuela. Archivoslatinoamericanos de nutricion 53, 52–58. [PubMed] [Google Scholar]
- Black R.E., Allen L.H., Bhutta Z.A., Caulfield L.E., de Onis M., Ezzati M. & Rivera J. (2008) Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371, 243–260. doi: 10.1016/S0140‐6736(07)61690‐0. [DOI] [PubMed] [Google Scholar]
- Brown K., Dewey K. & Allen L. (1998) Complementary Feeding of Young Children in Developing Countries: A Review of Current Scientific Knowledge. World Health Organization: Geneva. [Google Scholar]
- Daelmans B., Dewey K. & Arimond M. (2009) New and updated indicators for assessing infant and young child feeding. Food and Nutrition Bulletin 30, S256–S262. [DOI] [PubMed] [Google Scholar]
- Department of Census and Statistics (2010) Statistical Abstract 2010 . Available at: http://www.statistics.gov.lk/home.asp (Accessed 01 June 2010).
- Department of Census and Statistics (DCS) & Ministry of Healthcare and Nutrition (MOH) (2009) Sri Lanka Demographic and Health Survey 2006–07. DCS and MOH: Colombo, Sri Lanka. [Google Scholar]
- Dibley M.J., Roy S.K., Senarath U., Patel A., Tiwari K., Agho K.E. & Mihrshahi S. (2010) Across‐country comparisons of selected infant and young child feeding indicators and associated factors in four South Asian countries. Food and Nutrition Bulletin 31, 366–375. [DOI] [PubMed] [Google Scholar]
- Filmer D. & Pritchett L. (1998) Estimating Wealth Effects without Expenditure Data or Tears: An Application to Educational Enrolments in States of India. World Bank Policy Research: Washington, DC. [DOI] [PubMed] [Google Scholar]
- International Institute for Population Sciences (2007) National Family Health Survey (NFHS‐3) 2005–06. Vol 1. Mumbai, India.
- Jayatissa R. & Hossain S.M.M. (2010) Nutrition and Food Security Assessment in Sri Lanka: Nutrition and Food Security Survey. Medical Research Institute and UNICEF: Colombo. [Google Scholar]
- Kennedy G.L., Pedro M.R., Seghieri C., Nantel G. & Brouwer I. (2007) Dietary diversity score is a useful indicator of micronutrient intake in non‐breast‐feeding Filipino children. The Journal of Nutrition 137, 472–477. [DOI] [PubMed] [Google Scholar]
- Martin‐Prevel Y., Becquey E. & Arimond M. (2010) Food group diversity indicators derived from qualitative list‐based questionnaire misreported some foods compared to same indicators derived from quantitative 24‐h recall in urban Burkina Faso. The Journal of Nutrition 140, 2086S–2093S. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Population (2006) Nepal Demographic and Health Survey 2006. Ministry of Health and Population, New ERA and USAID.
- Ministry of Healthcare and Nutrition & UNICEF (2008) Sri Lanka Complementary Feeding Study – Factors Associated with Complementary Feeding in Sri Lanka. Ministry of Healthcare and Nutrition and UNICEF: Colombo. [Google Scholar]
- Moursi M.M., Arimond M., Dewey K.G., Treche S., Ruel M.T. & Delpeuch F. (2008) Dietary diversity is a good predictor of the micronutrient density of the diet of 6‐ to 23‐month‐old children in Madagascar. The Journal of Nutrition 138, 2448–2453. [DOI] [PubMed] [Google Scholar]
- Mukuria A.G., Kothari M.T. & Abderrahim N. (2006) Infant and young child feeding updates. Calverton, MD: ORC Macro.
- National Institute of Population Research and Training (NIPORT) , Mitra and Associates & Macro International (2009) Bangladesh Demographic and Health Survey 2007. National Institute of Population Research and Training, Mitra and Associates, and Macro International: Dhaka, Bangladesh and Calverton, MD. [Google Scholar]
- National Institute of Population & Studies (NIPS) & Macro International Inc. (2008) Pakistan Demographic and Health Survey 2006–07. NIPS and Macro International Inc.: Islamabad, Pakistan. [Google Scholar]
- Steyn N.P., Nel J.H., Nantel G., Kennedy G. & Labadarios D. (2006) Food variety and dietary diversity scores in children: are they good indicators of dietary adequacy? Public Health Nutrition 9, 644–650. [DOI] [PubMed] [Google Scholar]
- United Nations (2005) The Millennium Development Goals Report 2005 . United Nations: New York. Available at: http://unstats.un.org/unsd/mi/pdf/MDG%20Book.pdf
- WHO (2002) Complementary Feeding: Report of the Global Consultation, and Summary of Guiding Principles for Complementary Feeding of the Breastfed Child. World Health Organization: Geneva. [Google Scholar]
- WHO , UNICEF , IFPRI , UC Davis , FANTA , AED et al (2010a) Indicators for Assessing Infant and Young Child Feeding Practices Part III: Country Profiles. World Health Organization: Geneva. [Google Scholar]
- WHO , UNICEF , IFPRI , UC Davis , FANTA , AED et al (2010b) Indicators for Assessing Infant and Young Child Feeding Practices Part II: Definition. World Health Organization: Geneva. [Google Scholar]


