Abstract
Fortified spread (FS), containing dry food particles embedded in edible fat, offers a convenient means for nutrition rehabilitation. To describe how caregivers feed FS to their undernourished children at home, and how FS use affects other feeding patterns, we conducted a longitudinal observational study in rural Malawi. Sixteen 6‐ to 17‐month‐old underweight children (weight‐for‐age z‐score < −2.0; −3.0 < weight‐for‐height z‐score < 0) received FS for 12 weeks. Twelve‐hour observations were conducted before supplementation and during weeks 1, 4, 8 and 12 of FS use. FS was fed to children about two times per day; each serving was 15–20 g. The spread was first used mainly alone as a between‐meal snack, and then became integrated into the typical complementary feeding pattern by being mixed with porridge. Introduction of FS reduced the number of plain porridge meals, but did not decrease the total number of meals or breastfeeds per day and did not change the daily mean time caregivers spent on feeding. Children accepted the FS well, but more FS was wasted when it was offered mixed with porridge than when given alone (23.6% vs. 1.2%, 95% CI for the difference 13.2% to 31.6%). FS supplementation is feasible for community‐based nutrition interventions in Malawi because it easily becomes part of the feeding routine, does not replace other foods and does not take extra caregiver time. To limit wastage, caregivers should be advised to serve FS plain or to mix it with only a small quantity of porridge.
Keywords: child, underweight, supplementary feeding, fortified spread, feeding patterns, sub‐Saharan Africa
Introduction
Undernutrition affects up to 40% of children aged less than 5 years in low‐income countries (UNICEF 2000). It causes morbidity and adverse long‐term sequelae and contributes to global childhood mortality. Severely undernourished children have the highest risk of morbidity and death from this condition, but mild and moderate undernutrition create a greater health burden at the population level (Pelletier et al. 1995). In Malawi, the problem usually develops in children aged 6–17 months, so that by the age of 18 months, 30–50% of all children in rural Malawi are undernourished (Maleta et al. 2003).
Supplementary feeding is one possible avenue for improving the feeding and growth of children in poor communities. Efficacy trials of a variety of types of food supplements in different settings and with children of different ages have had variable results, with some studies showing that supplements have a positive impact on growth while others show no change (WHO 1998; Allen & Gillespie 2001). Age, initial nutritional status, food availability and feeding practices may all have an effect on the success of supplementation (WHO 1998). Despite these possible constraints, in locations, such as Malawi, where other interventions, like dietary diversification and fortified complementary foods, are too expensive to reach the poor, supplementary feeding may be a feasible and appropriate option.
Fortified spread (FS), containing dry food particles embedded in edible fat, is food supplement that has proven to be effective in research settings and that offers some clear benefits over milk‐ or cereal‐based supplements. FS is five times more energy dense than cereals, needs no cooking before use, is hygienic because it does not support bacterial growth, and contains adequate quantities of micronutrients (Briend et al. 1999; Briend 2001). A therapeutic version of spread, called ready‐to‐use therapeutic food, has been used successfully for rehabilitating severely undernourished children either in hospital or as outpatients (Collins & Sadler 2002; Diop et al. 2003; Manary et al. 2004; Sandige et al. 2004). Increases in weight and length gain have also been reported among moderately undernourished children supplemented with FS at home (Patel et al. 2005; Kuusipalo et al. 2006). These studies suggest that different types of spreads may spread a potential avenue for community‐level management of undernutrition. To date, there is no published information available on the practical aspects of home spread use, which would be needed to plan larger‐scale interventions.
In order to provide data on how FS is used at home, we carried out a longitudinal observational study of feeding patterns among underweight 6‐ to 17‐month‐old children in rural Malawi. The aim of this descriptive study was to look at issues such as the size of a typical FS feed, time spent feeding FS, waste of FS, impact of FS on complementary feeds, and changes in FS use over time.
Methods
Setting, design and overview
The study was conducted around Lungwena and Malindi in a rural area in southern Malawi. Participants were provided with FS for a period of 12 weeks. Ten 12‐h observations were conducted for each child; observations were carried out on two consecutive days. The first pair of observations was completed before the children received FS (week 0). Children and their caregivers were then observed during weeks 1, 4, 8 and 12 of FS use. A background questionnaire to obtain socio‐economic information was completed on the first day of observation. Children’s weight and length were measured at enrolment and at the end of the study. Ethical approval for the study was obtained from the College of Medicine Research and Ethics Committee at the University of Malawi, and from the Ethical Committee of the Pirkanmaa Hospital District in Finland.
Participants
Participants were a sample of 16 6‐ to 17‐month‐old children selected from six villages. Villages were chosen so as to include possible differences in health‐seeking and availability of food (especially fish) based on their distance from health facilities and the lake. Research assistants and village health workers visited the villages to prepare initial lists of children in the age group. The research team then went to each village to measure the children, test for peanut allergy, and verify eligibility [weight‐for‐age z‐score (WAZ) < −2.0; −3.0 < weight‐for‐height z‐score (WHZ) < 0; not participating in another study; looked after by biological mother; no peanut allergy; no chronic illness; and guardian‐signed informed consent]. The weight‐for‐age and weight‐for‐height criteria for this study were selected to obtain children who were underweight but not wasted and not short and fat. At the time the study was conducted, low weight‐for‐height (WHZ < −3.0) was the Malawian Ministry of Health’s criteria for a child to enter inpatient nutrition rehabilitation. Weight was measured using a UNICEF Salter scale (reading increment 0.10 kg), and length was measured using a length board (Shorr Productions, Olney, MD, USA; reading increment 0.10 cm). Weights and heights were converted into z‐scores using the Center for Disease Control and Prevention tables (Kuczmarski et al. 2002).
Procedures
Each trained female research assistant was responsible for carrying out all study activities for four children in one or two villages. Research assistants were assigned to observe and visit the same four participants so that they could develop rapport with the families, thereby minimizing their effect on the observations.
The FS used in this study contained peanut butter, milk powder, sugar, oil and vitamin/mineral mix, and a daily dose provided approximately 250 kcal of energy, 7 g protein, 14 g carbohydrates, 17 g fat, and one recommended daily allowance of 17 micronutrients. It was obtained from a local producer in the capital (Project Peanut Butter, Blantyre, Malawi). Research assistants delivered three plastic jars of FS to participants’ homes every 2 weeks; each jar contained enough FS for 5 days. At the beginning of the FS feeding period, caregivers were informed that they should feed the study child 7 teaspoons (approximately 50 g) of FS per day, and that the FS was specifically for the study child. No advice about how or when to give FS was offered because the aim of the study was to see how families chose to use FS in practice.
Background questionnaire
A background questionnaire was administered to each caregiver on the first day of observation. The questionnaire contained demographic and economic questions, including the age, education and occupation of the parents, number of family members, and food availability.
Observations of feeding
On each day of observation, a research assistant visited the family from approximately 6 am to 6 pm. First, the research assistant asked the caregiver if either she or the child was ill. If so, the research assistant inquired about the kind of illness. Then the research assistant sat near the child and recorded the type of food and duration of all feeding episodes (including breast milk). Research assistants also used a semi‐structured form to collect information about caregiver–child interactions during meals, including who fed the child, what utensil was used, and how many bites were offered and eaten.
The study’s principal investigator conducted 25% of observation visits with research assistants and independently recorded the data. This allowed us to estimate interobserver reliability for individual variables using Pearson’s correlation coefficient and Cohen’s κ statistic. On feeding logs, κ was 0.99 for type of food and r was 0.86 for length of episode. On feeding interaction forms, r ranged from 0.84 to 0.98 for variables counting teaspoons of food offered and eaten, and κ was 0.98 for primary feeders and 0.97 for primary utensils. Because interobserver reliability was high, all analyses presented below use data collected by research assistants.
Method of analysis
Data were entered into a self‐designed Microsoft Access database, extracted to Microsoft Excel tables and analysed with spss (version 11.5) and stata (version 9.2). Linear regression analysis was used to calculate means and to test for differences between some subgroups. The analysis was adjusted for within‐subject correlation by the Huber‐White robust standard error (Binder 1983). Binomial regression was used to analyse proportions (Spiegelman & Hertzmark 2005), with statistical inference based on the robust standard error to allow for correlated data.
In the analysis, foods listed in feeding logs and interaction forms were divided into seven types defined as follows: porridge (made from maize, rice or maize/soy; approximately 10% dry matter); FS alone (spread given straight from the jar); FS mixed (spread mixed with porridge); nsima (dough made from maize; approximately 28% dry matter) and relish (most often green vegetables, fish or beans); other meals (rice or boiled pumpkin); snacks (such as bananas, bread or roasted maize); and breast milk. When breast milk and food were recorded on the same line on feeding logs, only the type of food was used in the analysis. This procedure led to a slight underestimation of the number of breast milk episodes.
Results
A total of 228 children were identified in initial screening; 200 (87.7%) of them were measured by the research team. Of those measured, 177 were not eligible for the following reasons: 119 not underweight, 38 not correct age, 18 in another study, 1 chronically ill, and 1 whose mother was deceased. Out of 23 eligible children, 16 were selected. In four villages, all eligible children (n = 8) were enrolled. In the other two villages, four children were selected randomly (8 children in total). At enrolment, all caregivers were mothers. The background characteristics of the children and their families are shown in Table 1.
Table 1.
Background characteristics of children and their families
| Mean (SD) age of child at enrolment | 13 (3) months |
| Proportion female | 63% |
| Mean (SD) anthropometric measurements | |
| Weight | 7.5 (0.8) kg |
| Length | 69.8 (3.9) cm |
| Weight‐for‐age z‐score | −2.6 (0.3) |
| Height‐for‐age z‐score | −1.8 (0.7) |
| Weight‐for‐height z‐score | −1.2 (0.9) |
| Mean (SD) age of mother | 26 (7) years |
| Mother’s occupation (%) | |
| Housewife/farmer | 75 |
| Small business owner | 19 |
| Other | 6 |
| Mother’s education (%) | |
| None | 6 |
| 1–3 years | 44 |
| 4–6 years | 19 |
| 7–9 years | 12 |
| 10 or more years | 19 |
| Father lives with family (%) | 50 |
| Mean (SD) number of household members | 5 (2) |
| Mean (SD) number of children < 5 years | 2 (1) |
| Mean (SD) birth order of study children | 4 (2) |
Of the planned 160 days of observation, 155 days were completed. The length of most observations was approximately 12 h; however, 11 observation days (7%) were shorter (usually 4–8 h) due to visits away from home (to health centre, traditional healer, fields, funeral or maize mill) by participants.
Table 2 describes the number and duration of different meal types before FS was provided (week 0) and during FS use (weeks 1–12). All children, except one, were breastfed. In the absence of FS, the typical daily feeding pattern was: breast milk 11 times, porridge one to two times, nsima one time, and snacks three times. When FS was introduced, the mean times per day children ate plain porridge decreased (from 1.5 to 0.3, 95% CI for the difference 0.8 to 1.6, P < 0.001), while the mean times they had all other food types, including breast milk, remained the same. The duration of breastfeeding episodes did not change when children received the spread.
Table 2.
Number and duration of feeding episodes before and during FS supplementation
| Porridge | FS mixed | FS alone | Nsima and relish | Other meals | Snacks | Breast milk | |
|---|---|---|---|---|---|---|---|
| Mean (95% CI) times per day | |||||||
| Before FS | 1.5 (1.1, 1.9) | – | – | 1.0 (0.7, 1.4) | 0.3 (0.1, 0.5) | 2.7 (1.2, 2.8) | 11.1 (8.2, 14.1) |
| During FS | 0.3 (0.2, 0.4) | 0.9 (0.5, 1.2) | 0.7 (0.4, 0.9) | 1.0 (0.8, 1.3) | 0.2 (0.1, 0.3) | 2.0 (1.3, 4.1) | 10.1 (6.8, 13.5) |
| Mean (95% CI) minutes per episode | |||||||
| Before FS | 14.5 (11.6, 17.3) | – | – | 17.2 (13.2, 21.3) | 22.0 (14.1, 29.9) | 6.6 (5.6, 7.5) | 6.0 (4.9, 7.2) |
| During FS | 11.8 (7.0, 16.6) | 14.5 (11.7, 17.2) | 5.4 (3.5, 7.2) | 14.3 (12.2, 16.4) | 16.8 (8.5, 24.9) | 4.9 (4.1, 5.7) | 6.6 (5.0, 8.1) |
This table is based on data from feeding logs. Means and confidence intervals were adjusted for within‐subject correlation. Before FS (fortified spread) = week 0. During FS = weeks 1, 4, 8 and 12. Porridge = maize, rice or maize/soy, approximately 10% dry matter; FS mixed = spread mixed with porridge; FS alone = spread given straight from the jar; nsima = dough made from maize, approximately 28% dry matter, and relish = side dish made of green vegetables, fish or beans; other meals = rice or boiled pumpkin; snacks = small quantities of food eaten between meals (such as banana, bread, roasted maize).
FS was generally well accepted by children in this study. It was fed to children two times per day on average, and it comprised or was included in 31% of meals and snacks. There was a large difference in the mean time it took to feed FS alone and FS mixed with porridge (5.4 vs. 14.5 min, 95% CI for the difference 5.6 to 12.5, P < 0.001). Fifteen per cent (19/124) of observation days during weeks 1–12 included no FS feedings; approximately half of these were because the child’s FS supply was already finished. The recommended dose of 7 teaspoons of FS per day was offered to children during 27% of visits (34/124); at least 5 teaspoons of FS were offered during 47% of visits (58/124).
The way in which the feeding patterns changed during the course of the study is shown in detail in Fig. 1a. The number of porridge meals was greatest during week 0 (no FS). Most porridge episodes were replaced by FS episodes (alone and mixed) when the children started receiving FS. Both the total number of FS episodes and the number of FS alone episodes were greatest during week 1 and decreased until the end of the study, while the number of FS mixed episodes remained fairly stable throughout the study. During weeks 8 and 12, the combined number of episodes of FS alone, FS mixed and porridge were approximately equal to the number of porridge episodes during week 0 visits.
Figure 1.
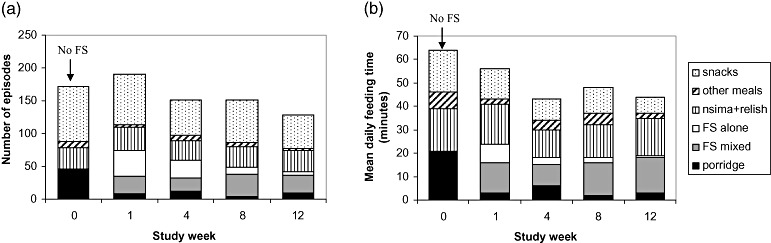
Number of food episodes and mean daily feeding time by study week. Figure 1a,b is based on data from feeding logs. In Fig. 1a, the sum of the number of feeding episodes during each study week is presented. In Fig. 1b, the mean daily feeding time for each type of food during each study week was adjusted for within‐subject correlation. During week 0, no FS (fortified spread) was provided to participants. FS was available to participants during weeks 1, 4, 8 and 12. Porridge = maize, rice or maize/soy, approximately 10% dry matter; FS mixed = spread mixed with porridge; FS alone = spread given straight from the jar; nsima = dough made from maize, approximately 28% dry matter, and relish = side dish made of green vegetables, fish or beans; other meals = rice or boiled pumpkin; snacks = small quantities of food eaten between meals (such as banana, bread, roasted maize).
The daily mean time spent feeding the children decreased when FS was introduced (week 1) and continued to decrease during the rest of the study (Fig. 1b). The mean time spent feeding breast milk, nsima and FS mixed remained fairly constant throughout the study, while the mean time spent feeding porridge and FS alone decreased greatly. Starting from week 4, the combined mean times for feeding porridge, FS alone and FS mixed were less than the mean time spent feeding porridge only during week 0.
Data about the amount of FS offered and eaten, as well as the proportion lost or wasted, are presented in Table 3. One teaspoon equals approximately 7 g of FS; so on average, children ate 15–20 g of FS per episode. More of the FS was wasted when it was offered mixed with porridge than when it was given alone (23.6% vs. 1.2%, 95% CI for the difference 13.2% to 31.6%, P < 0.001).
Table 3.
Teaspoons of FS offered and eaten per episode by study week
| Week 1 | Week 4 | Week 8 | Week 12 | Total | |
|---|---|---|---|---|---|
| Mean (95% CI) teaspoons of FS offered | |||||
| FS alone | 2.7 (1.7, 3.6) | 2.3 (1.4, 3.1) | 3.9 (1.8, 6.0) | 2.6 (− 1.5, 6.7) | 2.7 (2.0, 3.4) |
| FS mixed | 2.8 (2.2, 3.5) | 2.8 (2.3, 3.4) | 3.2 (2.4, 4.0) | 3.0 (2.3, 3.7) | 3.0 (2.6, 3.4) |
| Mean (95% CI) teaspoons of FS eaten | |||||
| FS alone | 2.7 (1.7, 3.6) | 2.2 (1.2, 3.2) | 3.9 (1.8, 6.0) | 2.6 (− 1.5, 6.7) | 2.7 (2.0, 3.4) |
| FS mixed | 2.1 (1.4, 2.8) | 2.2 (1.6, 2.7) | 2.4 (1.6, 3.2) | 2.4 (1.6, 3.3) | 2.3 (1.7, 2.8) |
| Proportion lost (95% CI) during feeding | |||||
| FS alone | 0.0% (–) | 3.9% (−3.1, 9.9) | 0.0% (–) | 0.0% (–) | 1.2% (−1.3, 3.8) |
| FS mixed | 27.0% (11.8, 42.3) | 22.6% (15.1, 30.1) | 24.8% (8.3, 41.2) | 20.0% (8.1, 31.9) | 23.6% (14.0, 33.3) |
This table is based on data from observations of feeding episodes. Means were calculated using linear regression and proportions were calculated using binomial regression. All calculations were adjusted for within‐subject correlation. FS (fortified spread) alone = spread given straight from the jar; FS mixed = spread mixed with porridge. (–) = same value for upper and lower confidence limits.
To describe who fed the children and what type of utensil was used, proportions were calculated using a feeding episode as the unit of analysis. Caregivers were the primary feeders during 95% (57/60) of FS alone, 88% (66/75) of porridge, 78% (85/109) of FS mixed, and 59% (89/151) of nsima episodes. Children fed themselves 92% (22/24) of snacks and 63% (20/32) of other meals. A spoon was used to feed children during 91% (68/75) of porridge, 88% (53/60) of FS alone, and 83% (91/109) of FS mixed episodes. Children’s and caregivers’ hands were used during 88% (21/24) of snacks and 64% (96/151) of nsima meals, respectively. For those types of food that were fed to children throughout the study (i.e. porridge, nsima, other meals and snacks), there was little change in the proportions of feeders and utensils before and during FS use.
During the 12‐week follow‐up, the mean (SD) gain in weight was 1.0 (0.5) kg and in length was 3.8 (1.3) cm. Mean (SD) gains in anthropometric indices were 0.3 (0.6), 0.0 (0.4), and 0.3 (0.5) z‐score units for WAZ, height‐for‐age z‐score and WHZ, respectively. At the end of the study, 81% of the participants still had WAZ < −2.0.
Discussion
This study was conducted to learn about patterns of home FS use for underweight young children and how its use modified other complementary feeding patterns. On average, children in this study had breast milk 11 times, nsima one time, porridge one or two times, and snacks three times per day. When FS was added to the diet, it was fed to the children about two times per day; each serving was 15–20 g (1 teaspoon = 7 g). FS was first used mainly alone as a between‐meal snack, but was then integrated into the usual feeding pattern by being mixed with porridge. The use of FS did not affect the number of times the child was fed per day, the number or duration of breastfeeds, or the amount of caregiver time spent feeding.
Among the Yao people and in other cultures in the region, porridge is a food that caregivers cook specifically for young children until they are old enough to participate in family meals (Cosminsky et al. 1993; Mabilia 1996; Hotz & Gibson 2001). The importance of porridge as a ‘baby food’ may explain why caregivers rarely used FS to replace meals, and why the number of meals and breastfeeds a child had per day did not decrease when FS was introduced. Because caregivers did not see FS as a replacement for porridge, mixing FS with porridge during regular meals, rather than serving FS alone as a snack, minimized the time they spent feeding the child FS. This strategy meant that the use of supplementary FS did not add to the mean time per day caregivers spent feeding the children.
Observations and discussions with caregivers indicated that the difference in the amount of FS wasted when mixed with porridge vs. plain was related to caregivers’ divergent approaches to FS used in these two ways. Caregivers typically offered plain porridge or porridge mixed with FS until the child rejected it or appeared full, and some porridge often remained in the bowl at the end of a feeding session. In contrast, when FS was fed alone, caregivers usually fed it to the children until the supplement they offered was finished. They rarely returned leftover plain FS to the jar or fed it to another family member.
A number of other studies have investigated child feeding with a similar observational methodology to that used here; however, all of these focused only on complementary feeding (Bentley et al. 1991; Brown et al. 1992; Guldan et al. 1993; Izurieta & Larson‐Brown 1995; Engle & Zeitlin 1996; Gittelsohn et al. 1997). Supplementary feeding studies either collect no data on breastfeeding and food intake, or obtain such information through 24‐h recalls. Single or widely spaced recalls are not likely to be as reliable as multiple observations in providing information on what was actually eaten during the entire supplementation period. In addition, such studies have seldom looked at wastage of supplement, or have measured it only when the supplement is supplied at a central location or by a field assistant. We could not identify any published data on time spent feeding supplement.
Our study results agree with findings from Colombia (Mora et al. 1981) that breastfeeding frequency remains the same during supplementation, but contrast with data from India (Bhandari et al. 2001) showing a decrease. Both of these studies, as well as a study in Jamaica (Walker et al. 1991), found that energy intake from regular foods was less during supplementation, whereas data collected from 3‐ to 4‐year‐old Malawian children supplemented with FS showed that energy intake from regular foods was unchanged on average (Maleta et al. 2004). Our study did not attempt to calculate energy intake, but showed that the number of regular food episodes remained the same before and during supplementation.
The differences between existing studies and ours regarding breastfeeding frequency and regular food consumption during supplementation are probably due to the way in which people from different cultures adopt a supplementary food into child feeding patterns and the type of supplementary food that was provided. If the supplement is similar to foods children are typically fed (e.g. cereal‐based food), it is more likely that it will be used in place of regular meals, whereas a supplement like FS may be added to cereals to make an ‘improved’ food or may be given as a snack. This theory is supported by data from our research group and from a study in Gambia that compared supplementation with FS to maize‐soy porridge and high‐fat to high‐carbohydrate supplements, respectively (Krahenbuhl et al. 1998; Maleta et al. 2004).
Because FS easily becomes part of the feeding routine, does not replace other foods and does not take extra caregiver time, we believe it could be integrated into community‐based nutrition interventions in rural Malawi. The amount of FS wasted when it is mixed with porridge might, however, reduce the population impact of any intervention. To limit wastage, caregivers should be advised to offer FS plain or to mix it with a small quantity of porridge that the child can finish. Other issues, such as the means of identifying appropriate children to receive FS, mode of delivery of FS, and cost of the supplement, should be investigated before undertaking large‐scale interventions using this product.
Acknowledgements
We are grateful to the participants, our research assistants, and the staff of Lungwena Health Center and St. Michael’s Hospital for their help and patience in carrying out this study. We also thank Yin Bun Cheung and Heini Huhtala for their advice on statistical analyses, and André Briend and Markus Rimon for comments on earlier drafts. The study was financially supported by grants from the Academy of Finland (grant 200720) and the Foundation for Paediatric Research in Finland. The authors do not have any conflicts of interest associated with this work.
References
- Allen L.H. & Gillespie S.R. (2001) What Works? A Review of the Efficacy and Effectiveness of Nutrition Interventions. United Nations Administrative Committee on Coordination/Sub‐committee on Nutrition in collaboration with the Asian Development Bank: Manila. [Google Scholar]
- Bentley M.E., Stallings R.Y., Fukumoto M. & Elder J.A. (1991) Maternal feeding behavior and child acceptance of food during diarrhea, convalescence, and health in the central Sierra of Peru. American Journal of Public Health 81, 43–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhandari N., Bahl R., Nayyar B., Khokhar P., Rohde J.E. & Bhan M. (2001) Food supplementation with encouragement to feed it to infants from 4 to 12 months of age has a small impact on weight gain. Journal of Nutrition 131, 1946–1951. [DOI] [PubMed] [Google Scholar]
- Binder D.A. (1983) On the variances of asymptotically normal estimators from complex surveys. International Statistical Review 51, 279–292. [Google Scholar]
- Briend A. (2001) Highly nutrient‐dense spreads: a new approach to delivery multiple micronutrients to high‐risk groups. British Journal of Nutrition 85 (Suppl. 2), 175–179. [PubMed] [Google Scholar]
- Briend A., Lacsala R., Prudhon C., Mounier B., Grellety Y. & Golden M.H. (1999) Ready‐to‐use therapeutic food for treatment of marasmus. Lancet 353, 1767–1768. [DOI] [PubMed] [Google Scholar]
- Brown L.V., Zeitlin M.F., Peterson K.E. et al. (1992) Evaluation of the impact of weaning food messages on infant feeding practices and growth in rural Bangladesh. American Journal of Clinical Nutrition 56, 994–1003. [DOI] [PubMed] [Google Scholar]
- Collins S. & Sadler K. (2002) Outpatient care for severely malnourished children in emergency relief programmes: a retrospective cohort study. Lancet 360, 1824–1830. [DOI] [PubMed] [Google Scholar]
- Cosminsky S., Mhloyi M. & Ewbank D. (1993) Child feeding practices in a rural area of Zimbabwe. Social Science and Medicine 36, 937–947. [DOI] [PubMed] [Google Scholar]
- Diop el H.I., Dossou N.I., Ndour M.M., Briend A. & Wade S. (2003) Comparison of the efficacy of a solid ready‐to‐use food and a liquid milk‐based diet for the rehabilitation of severely malnourished children: a randomized trial. American Journal of Clinical Nutrition 78, 302–307. [DOI] [PubMed] [Google Scholar]
- Engle P.L. & Zeitlin M. (1996) Active feeding behavior compensates for low interest in food among young Nicaraguan children. Journal of Nutrition 126, 1808–1816. [DOI] [PubMed] [Google Scholar]
- Gittelsohn J., Thapa M. & Landman L.T. (1997) Cultural factors, caloric intake and micronutrient sufficiency in rural Nepali households. Social Science and Medicine 44, 1739–1749. [DOI] [PubMed] [Google Scholar]
- Guldan G.S., Zeitlin M.F., Beiser A.S., Super C.M., Gershoff S.N. & Datta S. (1993) Maternal education and child feeding practices in rural Bangladesh. Social Science and Medicine 36, 925–935. [DOI] [PubMed] [Google Scholar]
- Hotz C. & Gibson R.S. (2001) Complementary feeding practices and dietary intakes from complementary foods amongst weanlings in rural Malawi. European Journal of Clinical Nutrition 55, 841–849. [DOI] [PubMed] [Google Scholar]
- Izurieta L.M. & Larson‐Brown L.B. (1995) Child feeding practices in Guatemala. Ecology of Food and Nutrition 33, 249–262. [Google Scholar]
- Krahenbuhl J.D., Schutz Y. & Jequier E. (1998) High fat versus high carbohydrate nutritional supplementation: a one year trial in stunted rural Gambian children. European Journal of Clinical Nutrition 52, 213–222. [DOI] [PubMed] [Google Scholar]
- Kuczmarski R.J., Ogden C.L., Guo S.S. et al. (2002) 2000 CDC growth charts for the United States: methods and development. Vital Health Statistics 11, 1–190. [PubMed] [Google Scholar]
- Kuusipalo H., Maleta K., Briend A., Manary M. & Ashorn P. (2006) Growth and change in blood haemoglobin concentration among underweight Malawian infants receiving fortified spreads for 12 weeks. A preliminary trial. Journal of Pediatric Gastroenterology and Nutrition 43, 525–532. [DOI] [PubMed] [Google Scholar]
- Mabilia M. (1996) Beliefs and practices in infant feeding among the Wagogo of Chigongwe (Dodoma rural district) Tanzania, II. Weaning. Ecology of Food and Nutrition 35, 209–217. [DOI] [PubMed] [Google Scholar]
- Maleta K., Virtanen S.M., Espo M., Kulmala T. & Ashorn P. (2003) Childhood malnutrition and its predictors in rural Malawi. Paediatric and Perinatal Epidemiology 17, 384–390. [DOI] [PubMed] [Google Scholar]
- Maleta K., Kuittinen J., Duggan M.B. et al. (2004) Supplementary feeding of underweight, stunted Malawian children with a ready‐to‐use food. Journal of Pediatric Gastroenterology and Nutrition 38, 152–158. [DOI] [PubMed] [Google Scholar]
- Manary M.J., Ndekha M., Ashorn P., Maleta K. & Briend A. (2004) Home‐based therapy for severe malnutrition with ready‐to‐use food. Archives of Disease in Childhood 89, 557–561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mora J.O., Herrera M.G., Suescun J., De Navarro L. & Wagner M. (1981) The effects of nutritional supplementation on physical growth of children at risk of malnutrition. American Journal of Clinical Nutrition 34, 1885–1892. [DOI] [PubMed] [Google Scholar]
- Patel M.P., Sandige H.L., Ndekha M.J., Briend A., Ashorn P. & Manary M. (2005) Supplemental feeding with ready‐to‐use therapeutic food in Malawian children at risk of malnutrition. Journal of Health, Population and Nutrition 23, 351–357. [PubMed] [Google Scholar]
- Pelletier D.L., Frongillo E.A., Schroeder D.G. & Habicht J.P. (1995) The effects of malnutrition on child mortality in developing countries. Bulletin of the World Health Organization 73, 443–448. [PMC free article] [PubMed] [Google Scholar]
- Sandige H., Ndekha M.J., Briend A., Ashorn P. & Manary M.J. (2004) Home‐based treatment of malnourished Malawian children with locally produced or imported ready‐to‐use food. Journal of Pediatric Gastroenterology and Nutrition 39, 141–146. [DOI] [PubMed] [Google Scholar]
- Spiegelman D. & Hertzmark E. (2005) Easy SAS calculations for risk or prevalence ratios and differences. American Journal of Epidemiology 162, 199–200. [DOI] [PubMed] [Google Scholar]
- United Nations Children’s Fund (UNICEF ) (2000) The State of the World’s Children 2001: Early Childhood. Oxford University Press: Oxford. [Google Scholar]
- Walker S.P., Powell C.A., Grantham‐McGregor S.M., Himes J.H. & Chang S.M. (1991) Nutritional supplementation, psychosocial stimulation, and growth of stunted children: the Jamaican study. American Journal of Clinical Nutrition 54, 642–648. [DOI] [PubMed] [Google Scholar]
- World Health Organization (1998) Complementary Feeding of Young Children in Developing Countries: A Review of Current Scientific Knowledge. World Health Organization: Geneva. [Google Scholar]


