Abstract
Responsive complementary feeding, whereby the mother feeds her child in response to child cues of hunger state and psychomotor abilities, is a problem in some countries, and likely contributes to malnutrition. Interventions are needed to evaluate whether promoting responsive feeding would add any benefit. Using a cluster randomized field trial, we evaluated a six‐session educational programme that emphasized practice of two key behaviours, namely child self‐feeding and maternal responsiveness. One hundred mothers and their 12‐ to 24‐month‐olds attended the sessions as part of village clusters randomly assigned to the intervention group. A similar number of controls received sessions on foods to feed and nutritional disorders. Outcomes assessed at pre‐test, 2‐week post‐intervention and again 5‐months post‐intervention included weight, mouthfuls of food taken, self‐feeding and maternal responsiveness. Research assistants, blind to group assignment, observed and coded mother and child behaviours during the midday meal. Secondary measures included foods fed and feeding messages recalled. Analysis was based on intention to treat and accounted for clustering. Only 10% of each group was lost to follow‐up. Weight (d = 0.28), weight gain (d = 0.48) and child self‐feeding (d = 0.30) were significantly higher in the responsive feeding group. Mouthfuls of food eaten and maternal responsiveness were not significantly increased by the intervention. Mothers in the intervention gave their children more vegetables, and spontaneously recalled more feeding messages at the 5‐month follow‐up. These results provide evidence that self‐feeding and weight gain can improve by targeting specific behaviours, while maternal responsiveness may require more intensive strategies.
Keywords: responsive feeding, complementary feeding, cluster randomized field trial, nutrition education, behaviour change, Bangladesh
Introduction
Nutrition education, with or without the provision of food, is the common way of intervening to enhance children's nutritional status. Outcomes have been mixed, with only a few showing significantly better weight gains in comparison with controls (e.g. Dewey & Adu‐Afarwuah 2008). Nutrition education programmes tend to provide mothers with information on foods to feed, quantities and frequencies for differently aged children, particularly those from 6 to 36 months of age (e.g. Roy et al. 2005). Although supplementary feeding may sometimes benefit children's length and weight gain (Sguassero et al. 2007), it is not feasible on a continuing basis in most developing countries. Consequently, alternative strategies for improving the nutritional status of young children are needed.
One important, yet relatively under‐utilized, behavioural strategy involves responsive feeding. Although the concept, measurement and benefits of responsiveness in parent‐child interaction are not new (see Isabella et al. 1989; Isabella 1993; Tamis‐LeMonda et al. 2001; Eshel et al. 2006), its application to feeding is more recent (Engle & Zeitlin 1996). Responsive caregiver's behaviour refers to the caregiver responding to a child's cues in a contingent and appropriate manner, or synchronous coordinated interaction between the caregiver and child who respond to each other. Responsiveness requires a three‐step process, whereby a mother observes the child, interprets the cue or state of the child, and then acts in accordance with the intended meaning of the cue (Eshel et al. 2006). Some feeding examples are: The child eats a mouthful and then the mother offers more; the child refuses food and then the mother asks if the child wants water; the child touches food and then the mother offers the plate for the child to self‐feed.
Behavioural observations of mealtime with children aged 6–24 months in some countries have revealed low levels of responsive feeding, high levels of forceful or controlled feeding and either too much or too little self‐feeding given the child's age (e.g. Bentley et al. unpublished observations; Engle & Zeitlin 1996; Ha et al. 2002; Moore et al. 2006). These behaviours are associated with fewer mouthfuls of food taken by the child and more refusals, despite the child's malnourished state. Consequently, mothers' feeding style is likely contributing to the poor appetite and nutritional status of young children in these countries.
Two behaviours, in particular, may be central to the problem: child self‐feeding and maternal responsiveness. In a recent Bangladesh study, as in others, self‐feeding was delayed beyond 24 months (Moore et al. 2006), despite children's acquired psychomotor abilities to feed themselves partly by 9 months (see Engle et al. 2000, Table 1). Furthermore, mothers rarely responded to refusals by asking if the child wanted water, another food or a slower pace of feeding. Rather, they resorted to temporary diversions of the child's attention, promises, threats, following the child around the room, and sometimes forceful feeding. Although these strategies might lead to short‐term compliance, they are unlikely to help the child develop a healthy appetite, recognition of hunger and satiety cues and properly paced self‐feeding.
Table 1.
Means (standard deviation) or frequency (%) and statistics comparing pre‐test variables
| Variable | Control | Intervention | F (1,183) | P |
|---|---|---|---|---|
| (n = 100) | (n = 102) | |||
| Child age in months | 17.24 (3.2) | 17.46 (3.1) | 0.17 | 0.68 |
| Mother's age in years | 24.99 (5.2) | 24.43 (5.6) | 0.54 | 0.46 |
| Mother's education | 5.37 (3.8) | 6.40 (3.7) | 3.85 | 0.06 |
| Family assets out of 11 | 7.12 (2.5) | 8.16 (2.0) | 10.78 | 0.001 |
| Household size | 5.09 (1.6) | 5.21 (1.8) | 0.23 | 0.63 |
| Weight (kg) | 8.78 (1.4) | 8.96 (1.1) | 0.96 | 0.33 |
| Mouthfuls | 13.08 (8.6) | 13.38 (8.3) | 0.03 | 0.86 |
| % self‐fed mouthfuls | 19.64 (34.9) | 27.30 (39.8) | 1.45 | 0.15 |
| Mother's responsive acts | 11.08 (7.5) | 10.69 (7.6) | 0.16 | 0.69 |
| Girls | 45 (45%) | 63 (61.8%) | 5.59 | 0.02 |
| Diarrhoea past week | 11 (11%) | 10 (9.8%) | 1.20 | 0.27 |
| Mother housewife | 93 (93%) | 98 (96%) | 5.78 | 0.33 |
Mouthfuls = total number of mother‐ and self‐fed mouthfuls of food taken; % Self‐fed Mouthfuls = percentage of total mouthfuls that were self‐fed (child put food in own mouth); Mother's responsive act = number of acts by mother that corresponded to the meaning or intent of the child's preceding act, i.e. contingent and appropriate to child's prior behaviour.
Although responsive feeding messages have been included in programmes with broader aims, such as to actively encourage greater intakes of food (Bhandari et al. 2004), to feed with love, patience and good humour (Penny et al. 2005), and to provide positive deviance foods and caretaking (Schroeder et al. 2002), no published research has evaluated an intervention focused on self‐feeding and responsive feeding. To assess the benefits of a responsive feeding behaviour‐change programme, we helped an organization implement a six‐session module to groups of rural mothers in Bangladesh, and compared them with mothers and children who received only the regular nutrition education, mainly on foods to feed. A cluster randomized field trial was used in which randomization occurred and interventions were delivered at the cluster level and outcomes measured at the individual level.
Although randomly assigning clusters rather than individuals to groups run the risk of introducing bias, there was a strong rationale for using clusters in this trial. Development activities in rural Bangladesh are normally offered to groups of women living near each other in villages. Group educational sessions for health, nutrition and child development were an ongoing feature of the implementing organization. Implementation at the group level reduces the cost, and mothers who are generally confined to home enjoy the sociability and peer support. Village groups that had been formed at the beginning of the year were designated as clusters.
The hypotheses for children were that, compared with the control children, those in the responsive feeding intervention would show more self‐feeding, more mouthfuls of food taken, and greater weight gain. The hypothesis for mothers was that, compared with control mothers, those in the responsive feeding programme would show more responsive behaviours.
Methods
The design was a cluster randomized field trial where the fixed variable was assignment to the responsive feeding or a control group. Clusters were the villages where mothers lived and met in a group to receive either the Responsive Feeding or Regular nutrition education. Ethical approval was granted by the International Centre for Diarrhoeal Diseases Research (ICDDR,B) and McGill University. Mothers were informed that they would receive nutrition education, and signed their consent to participate in data collection. The study took place between March and November 2006, and was registered with ISRCTN.
Participants
The mothers and children resided in the rural sub‐district of Sripur, in the district of Gazipur, Bangladesh, 60 km north of the capital Dhaka. In Sripur, a local non‐governmental organization regularly delivered parenting programmes to mothers of children under 3 years, with funds and training from an international non‐governmental organization (hereafter called ‘the organization’). The population served by the organization is mostly Muslim, involved in farming or wage labour, and classified as poor and very poor (Aboud 2007). A recent survey of children 30–48 months found that 37% were moderately to severely underweight (Aboud 2007), a figure comparable with the overall current prevalence in Bangladesh (UNICEF 2007).
Eligible clusters consisted of 140 village groups where mothers of children under 3 years had met weekly since the start of 2006 to hear about parenting. From these clusters, children were eligible to participate in the study if they were between the ages of 12 and 24 months at pre‐test (exclusion criteria, namely that the child be physically or mentally handicapped, or not yet started on complementary foods, did not apply to anyone).
Sample size estimation
The sample size was based on the number of mouthfuls eaten by a child – an indicator for which the definition is commonly agreed (Ha et al. 2002; Moore et al. 2006). Based on a prior pilot study which yielded a mean of 20 mouthfuls consumed at the midday meal and a standard deviation (SD) of 10, we predicted a mean difference of 5 (or 0.5 SD). With an alpha of 0.05, power of 0.80 and a SD of 10, the required sample size was calculated to be 85 per group. Intracluster correlation (ICC) was set low at 0.03 because not all mothers and children would be able or willing to comply fully with the feeding messages. Cluster sizes were expected to be eight. Based on the formula 1 + ICC (cluster size −1), the sample size was multiplied by 1.25 to accommodate clustering, thus requiring a sample of 105 per group.
Randomization and recruitment
Randomization of village clusters took place before mothers were enrolled. Using a random numbers table and a numbered list of the villages with parenting groups, we first selected 16 intervention villages and then 16 control villages. To avoid contamination, three intervention villages situated close to controls were excluded and replaced with three randomly selected that were not potentially contaminated. Likewise two control villages were replaced. Two more randomly selected villages were added to each during enrolment to reach the required sample size. Although control villages tended to be situated in the northern part of the sub‐district, there was no evidence that they differed on social or economic indicators (Aboud 2007). Of the organization's four local staff, only one supervised peer educators in both control and intervention sites.
Eight research assistants, blind to the group assignment, recruited mothers to the study during April. They recruited all mothers of children 12–24 months of age who participated in the organization's ongoing parenting programme. Mothers were visited at home and asked if they would permit data collection before, during and after the upcoming nutrition education sessions. If willing, mothers signed the consent form. Mothers were told they could participate in the group sessions even if they did not want to be involved in the research. Thus, allocation to the intervention group was concealed during recruitment.
The research team's independence from the implementation of sessions was maintained; research assistants were not present in the area when the intervention was being implemented. To assess the continued blindness of research assistants, after follow‐up we asked them what parenting programmes the mothers had received. They assumed all had received messages about responsive feeding, and were unaware that there were two programmes. No one noticed special feeding messages or materials in the homes they visited. Peer educators implementing the responsive feeding intervention received extra training and knew that they were participating in a non‐regular programme. Mothers' awareness of different programmes was not assessed; however, contamination was reduced by selecting non‐neighbouring villages.
Intervention
Interventions were delivered to clusters. The Intervention group received six sessions added on to the regular programme. Both control and intervention groups had earlier (January–April) received 12 sessions on child development, dealing with how parents can help children learn, provide stimulation through toys and talk, and use gentle discipline (Plan Bangladesh 2004). During the month of May, while the control group received regular weekly sessions on nutrition, the intervention group received weekly sessions on responsive feeding. Immediately after the post‐test, the intervention group received the regular nutrition sessions. Peer educators for these sessions were young mothers who lived in the village; they normally had grade 8–10 education and received special training along with a manual from the organization. More details of the control and responsive feeding messages follow.
The control group received five health‐nutrition sessions relevant to complementary feeding (Plan Bangladesh 2005). Mothers were told about food requirements, nutrients and their functions, along with growth monitoring and breastfeeding. Foods such as rice, chapatti, potato, fish, meat, eggs, milk products, pulses, vegetables and fruits were identified. Child growth, meal frequency and foods were discussed for children 6–12 months and 12–24 months when family foods were introduced. Causes of weight reduction were said to be not enough food, low appetite and diseases; signs of malnutrition were dry skin, bones sticking out and no bone growth. Several sessions focused on foods for vitamin A, vitamin C, iron and iodine and the consequences of deficiencies. The information was imparted by peer educators verbally and with the help of a picture book and stories. Although a few mothers brought children, the latter were not actively involved. Mothers answered questions asked by the educators but rarely raised problems. Training of village peer educators was done by the organization.
The intervention group received five sessions on responsive feeding during the month of May and a booster session in early October. The behaviour‐change strategy, based on components of social‐cognitive learning theory, including practice, problem‐solving and peer support (Baranowski et al. 2002). The 20‐page manual for peer educators, in English and Bangla, imparted the following messages about self‐feeding and responsive feeding that mothers discussed and practiced with children during the sessions: (1) Wash your child's hands, and then let the child pick up food and eat; (2) Read your child's signals by watching, listening and interpreting what they mean, and then Respond positively; (3) When your child refuses, pause and question why; don't force feed or threaten; and (4) Offer a variety of foods. To allow participants to practice self‐feeding and responsive feeding, peer educators provided five or six small, soft pieces of fruit, vegetable and/or egg on a plate. The village peer educators received group training over a 5‐day period from staff of the organization and two researchers, at which time the manual was jointly read and role plays conducted so peer educators could practice demonstrating the behaviours to mothers.
Details of the messages, the training of peer educators and the implementation were revised after a pilot intervention delivered a year prior, with two groups of 10 mother–child pairs each. Focus group discussions with mothers and peer educators of the pilot study, along with structured questions and observations, informed the current programme. For example, we learned that mothers recalled the importance of washing their child's hands before eating, so we introduced a hand‐washing ritual in each session, and linked it to self‐feeding with the phrase, ‘First you wash your hands; then you touch the food’. Mothers needed cues to help recall the messages, so at the end they received laminated coloured drawings of a happy child self‐feeding, while the mother watched in an alert and interested manner.
Observations of eight responsive feeding sessions, selected unsystematically from among those delivered in the second and third weeks, indicated that certain activities were done better than others. Relatively well done was the self‐feeding activity. Relatively poorly done was teaching responsive behaviours to the mothers. Often educators forgot to tell mothers to sit the child facing them so they could read facial signals; educators often demonstrated the behaviour with a mother playing the role of a child rather than with a child; many mothers did not talk to their child or praise good behaviour. A refresher course was given to the peer educators before the fifth and booster sessions.
Measurement of outcomes
Primary outcomes were attained and gained weight, mouthfuls eaten, self‐fed mouthfuls and mother's responsive acts. The rationale for selecting these was that mouthfuls and weight were indicators of nutrition, while self‐feeding and maternal responsiveness were behaviours targeted by the programme. Secondary outcomes were other potentially relevant feeding behaviours, such as child refusals and maternal non‐responsive encouragement, forceful feeding, foods fed to the child and messages recalled by the mother. All but the last outcome were measured at three points: recruitment (pre‐test), 2 weeks after the sessions ended (post‐test) and at a 5‐month follow‐up. All research assistants collected data from intervention and control clusters.
Child and mother behaviours were observed during a midday meal when mothers were most likely to feed the child individually. The time was arranged during an interview in the morning, when the mother provided information on the child's birth date, mother's and father's age and education, 11 family assets (e.g. bed, table, radio, bicycle, electricity), breastfeeding, sickness in the past week and types of food fed yesterday. After the interview, the child was weighed two times on a Seca uniscale (Seca GmbH, Hamburg, Germany) and recorded to the nearest 100 gm; the average was analysed. Weight rather than weight‐for‐age was analysed because we could not be sure of children's exact ages.
The behavioural outcomes were measured through observation of a midday meal, as follows. The research assistant returned at the arranged time and sat unobtrusively in a position to observe feeding behaviours of the mother and child. The assistant wrote down all behaviours of mother and child (and other interactants), along with foods fed, and the time when the meal began and finished. Subsequent coding of each behavioural act followed the Moore et al. (2006) framework, to be described shortly. To assess its representativeness, when the meal was over, the mother was asked if the child was hungry before the meal, if this was the usual time for the child's meal, and if it was a typical intake (‘yes’ or ‘no’ for each).
Messages recalled by the mothers were assessed at the 5‐month follow‐up by asking if they remembered any messages given by the organization. After each, the assistant asked ‘What else did they tell you?’ Answers were organized according to the eight categories of information provided, namely ages to feed, what to feed, hygiene, growth monitoring, nutritional disorders, responsive feeding, encouraging self‐feeding and talking to child. Each answer was scored a point for a total of three per category, but later dichotomized as 0 and 1 or more.
Behaviour assessment training and reliability
Training ensured that research assistants wrote reliably full records of observed feeding behaviours, and subsequently coded each behaviour reliably. Research assistants were trained in a 1‐week period before conducting the pre‐test. This included observation of videos of mother–child interaction with which written records could be compared. They also practiced coding behaviours in order to become familiar with the key behaviours. Ten videos were subsequently taken of children while a record was being written; codings of the two allowed for an assessment of the completeness of written records. The observed means ranged from 84% to 95% of the video scored means for seven key codes including the ones reported here; only for mothers' non‐responsive encouragement was the observed mean 77% of the video scored mean. Correlations ranged from r = 0.85 to 0.99.
Observed feeding behaviours were coded using a responsive feeding framework (Moore et al. 2006), particularly for mouthfuls taken (swallowing a mouthful of food or milk which was often mixed with rice flakes and sugar), child self‐feeding (act aimed at putting food in his/her own mouth) and mother responding to a preceding child signal in accordance with the intent of the child's behaviour (e.g. child takes the previous mouthful and the mother offers food again; child refuses and the mother pauses or asks, ‘Do you want more?’; child asks for water and the mother offers water). Coded but not primary outcomes were child refusals (actively rejecting the mother's offer of food by closing mouth, turning head, saying ‘No’, or leaving), mother's encouraging but non‐responsive behaviour (e.g. after refusal, the mother offers again and says, ‘Eat, eat’) and mother's forceful or threatening feeding (e.g. threatens to take food away, tells the child to hurry up, forces food into the child's mouth).
Each meaningful unit of behaviour in the transcripts received a code. For example, if the written record stated: ‘Child picks up egg and puts in mouth’ a code of self‐feeding was given; if the mother subsequently said, ‘you eat nicely’ a code of mother responsive was given. If the written record stated: ‘Mother puts rice into child's mouth’ without any prior signal of child interest, or even after a refusal, a code of mother non‐responsive encouragement was given. If the child pointed at food or said ‘banana’ and the mother gave it, a code of mother responsive was given. Consequently, a frequency count of each behaviour code was available for each mother–child pair, reflecting the number of times that behaviour occurred, for example, the number of responsive mother behaviours and the number of non‐responsive encouraging behaviours. Frequencies are found to be more pertinent than rates or proportions in mother–child research (Hubbs‐Tait et al. 2002), because peoples' memory for an event and their consequent reaction is influenced by the frequency of occurrence. Mouthfuls ingested by the child were identified independent of the behaviour codes surrounding it and were summed; the number of mouthfuls that resulted from self‐feeding was calculated as a percent of the total. Inter‐rater reliability on 10 transcripts coded by the principal investigator (PI) and four coders ranged from r = 0.88 to 1.00, reflecting over 90% agreement.
Method of analysis
The unit of analysis was the individual child. All analyses used the MIXED procedure in SAS for continuous scores, except for foods observed and messages recalled which required the GLIMMIX procedure for dichotomized scores (version 8.2, Cary, NC, USA). The between‐subjects fixed variable was group assignment; the random variables were clusters and mothers within clusters. Group differences at the post‐test and 5‐month follow‐up were analysed using as covariates the pre‐test value of the outcome, child's age and sex, mother's education and family assets. Effect sizes for d, or the number of SDs separating the two means, were calculated from adjusted means at follow‐up. Although we expected child's age to affect weight and behaviours, we did not expect age to interact with the intervention. Pre‐test child and family variables of the two groups were compared using the same analysis without covariates to assess the success of random assignment. Those who were lost to follow‐up were compared with those who were analysed. Outcomes were statistically analysed based on intention to treat.
Results
Figure 1 outlines the flow of participants through each stage. One hundred control mothers and 102 intervention mothers were recruited; none refused consent at this point. Approximately, 10% of each group was lost to follow‐up.
Figure 1.
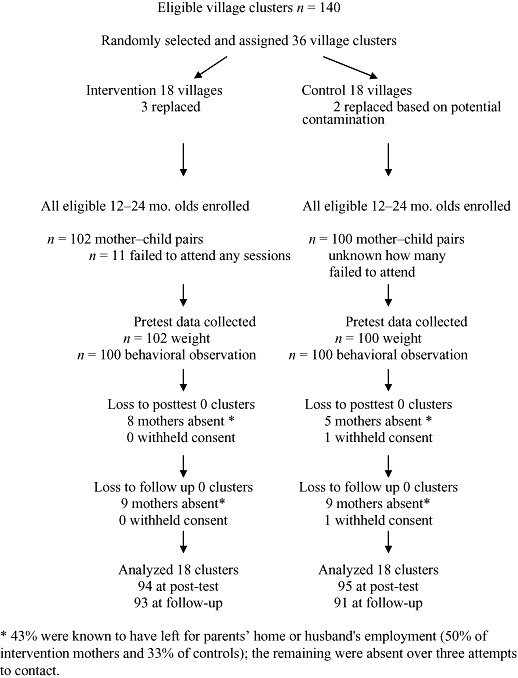
Flowchart of clusters and participants.
Randomization appeared to be largely successful according to an analysis of the pre‐test variables (see Table 1). Socio‐demographic indicators were not significantly different except for family assets and child's sex – the intervention group had more assets and more girls. These were included as covariates in subsequent analyses. The groups did not initially differ on weight, sickness or feeding behaviours.
Only 5.4% or 33 out of 606 midday observations were missing, and 5.3% or 32 children were missing a weight for one of the last two occasions. Those missing a 5‐month follow‐up did not differ from those retained on any of the pre‐test variables in either the control or intervention group.
Preliminary descriptive analyses indicated that intra‐class correlations for the four major outcomes were lower than expected, varying between −0.07 and +0.04. Cluster sizes ranged from four to eight. The variables weight, percent of mouthfuls that were self‐fed, and mother's responsive behaviours were not skewed; the number of mouthfuls was positively skewed (skew = 1.12) but could be normalized with a square root transformation. Consequently, weight, self‐fed mouthfuls and mother's responsive behaviours were analysed raw, and number of mouthfuls was analysed in its transformed state. Other behaviour variables such as child refusals, non‐responsive encouragement and forceful feeding were also transformed.
Table 2 presents the raw means and SD for all variables, along with the F and P values, and the d effect sizes at follow‐up. Weight attained and weight gain were significant, indicating that intervention children gained more weight than controls. Based on the adjusted means, the effect size for follow‐up weight attained was d = 0.28 and for follow‐up weight gain was d = 0.48. Child self‐feeding was also significant; the percentage of self‐fed mouthfuls was greater for the intervention than control group with an effect size d = 0.30 at follow‐up. However, the total number of mouthfuls eaten by the children and mothers' responsiveness were not higher in the intervention group. Secondary analyses on other behaviours indicated that non‐responsive encouragement dropped significantly more among intervention mothers, but forceful feeding did not.
Table 2.
Cluster ANCOVA tests of group effects at post‐test and follow‐up co‐varying the effects of pre‐test levels, child's age and sex, mother's education and family assets
| Outcome variable | Pre‐test | Post‐test | Follow‐up | ||
|---|---|---|---|---|---|
| M (SD) | M (SD) | F (1,164) | M (SD) | F (1,158) | |
| P | P, d | ||||
| Attained weight (kg) | |||||
| Control | 8.84 (1.4) | 9.06 (1.4) | 6.45 | 9.88 (1.4) | 9.74 |
| Intervention | 8.96 (1.1) | 9.31 (1.1) | P = 0.01 | 10.34 (1.3) | P = 0.0021, d = 0.28 |
| Weight gain (kg) | |||||
| Control | 0.22 (0.49) | 6.45 | 1.04 (0.75) | 9.74 | |
| Intervention | 0.35 (0.46) | P = 0.01 | 1.38 (0.75) | P = 0.002, d = 0.48 | |
| Child mouthfuls | |||||
| Control | 13.08 (8.6) | 14.06 (7.6) | 0.02 | 14.85 (6.7) | 0.98 |
| Intervention | 13.30 (8.3) | 14.98 (7.7) | P = 0.90 | 16.30 (8.4) | P = 0.32 |
| % self‐fed mouthfuls | |||||
| Control | 19.64 (34.9) | 26.65 (38.0) | 14.85 | 32.89 (43.4) | 4.52 |
| Intervention | 27.30 (39.8) | 48.53 (45.2) | P = 0.0002 | 49.31 (47.2) | P = 0.03, d = 0.30 |
| Mother responsive | |||||
| Control | 11.08 (7.5) | 9.89 (6.3) | 0.04 | 9.95 (5.7) | 1.75 |
| Intervention | 10.69 (7.6) | 10.29 (8.3) | P = 0.83 | 8.81 (6.3) | P = 0.19 |
| Child refusals | |||||
| Control | 3.94 (3.2) | 3.00 (3.0) | 0.90 | 2.92 (2.6) | 2.86 |
| Intervention | 4.48 (4.1) | 2.82 (2.9) | P = 0.34 | 2.40 (2.5) | P = 0.09 |
| Non‐responsive encouragement | |||||
| Control | 6.75 (4.3) | 5.60 (4.0) | 4.71 | 4.59 (2.7) | 8.62 |
| Intervention | 6.91 (5.0) | 4.82 (3.2) | P = 0.03 | 3.56 (2.8) | P = 0.004 |
| Forceful, threatening | |||||
| Control | 2.22 (4.6) | 1.91 (2.3) | 0.59 | 2.58 (3.4) | 0.36 |
| Intervention | 2.32 (3.1) | 1.63 (1.7) | P = 0.44 | 1.74 (2.4) | P = 0.55 |
Weight n were 100, 95, 91 for control; 102, 95, 92 for intervention; Behavioural n were 100, 95, 91 for control; 100, 94, 93 for intervention. Behaviour scores are the number of such behaviours occurring during the meal. M, mean; SD, standard deviation; Mouthfuls = total number of mother‐ and self‐fed mouthfuls of food taken; % self‐fed Mouthfuls = percent of total mouthfuls that were self‐fed (child put food in own mouth); Mother responsive = number of acts by mother that corresponded to the meaning or intent of the child's preceding act, i.e. contingent and appropriate to child's prior behaviour; Child refusal = number of offered mouthfuls of food that were rejected by child; Non‐responsive encouragement = number of acts by mother that encouraged the child to eat but did not respond to the child's preceding act; Forceful, threatening = number of acts by mother that were intrusive, aversive, or warned of such consequences to the child.
Mothers believed that their child was hungry (99–100% reported so), that this was the usual time for their child to eat (98–100%), and that it was a typical intake (81–95%) for the two groups who did not differ over the three time periods. So the meals were similarly representative of children's lunch.
To understand why weight increased even though mouthfuls did not, we analysed the kinds of food eaten yesterday, as reported by the mother, and during the midday meal as observed by the research assistants. The number of ‘meals’ at which a child ate each type of food yesterday during follow‐up was analysed. Table 3 (left panel) shows that eggs, fruit, vegetables and carbohydrates were more often reportedly given to intervention children, and biscuits/sugar more often given to controls. This was confirmed by assistants' observation that more intervention children were given vegetables at the midday meal (Table 3 right panel). More control children were given cow's milk mixed with rice flakes and sugar, normally spooned into the child's mouth. No such differences were observed at the pre‐test, and only two differences in yesterday's food were reported by mothers at pre‐test, namely control mothers reported giving more rice and fish. Consequently, although assets might be associated with food security, they had little impact on results and were, in any case, co‐varied in all analyses.
Table 3.
Mean (standard deviation) number of times foods were eaten yesterday as reported by mother (left panel) and number of children observed to be offered foods at the midday meal (right panel) at 5‐month follow‐up, along with cluster ANCOVA F‐and P‐values when pre‐test foods, child age, sex, mother's education and assets were co‐varied
| Food type | Foods reported by mother | Foods observed at midday meal | ||||||
|---|---|---|---|---|---|---|---|---|
| Control | Intervention | F (1,159) | P | Control | Intervention | F (1,159) | P | |
| (n = 91) | (n = 92) | (n = 91) | (n = 92) | |||||
| Rice | 2.64 (0.72) | 2.71 (0.62) | 0.90 | 0.34 | 90 | 91 | no convergence | |
| Dal | 0.41 (0.70) | 0.29 (0.64) | 1.52 | 0.22 | 11 | 13 | 0.02 | 0.88 |
| Animal (fish) | 1.01 (0.99) | 0.86 (0.91) | 0.16 | 0.69 | 20 | 21 | 0.13 | 0.72 |
| Egg | 0.09 (0.28) | 0.28 (0.52) | 5.43 | 0.02 | 5 | 7 | no convergence | |
| Fruit | 0.32 (0.68) | 0.60 (0.84) | 4.27 | 0.04 | 5 | 5 | no convergence | |
| Vegetable | 0.80 (0.99) | 1.37 (1.13) | 8.32 | 0.004 | 23 | 53 | 17.36 | <0.0001 |
| Cow's milk | 0.73 (1.07) | 0.85 (1.09) | 0.26 | 0.61 | 12 | 2 | 25.13 | <0.0001 |
| Carbohydrate | 0.31 ((0.69) | 0.63 (0.95) | 4.25 | 0.04 | 7 | 10 | 0.23 | 0.63 |
| Biscuit | 1.52 (1.12) | 1.22 (0.97) | 5.44 | 0.02 | 14 | 10 | 0.43 | 0.51 |
Cow's milk is offered mixed with rice flakes and sugar. Carbohydrate foods were mainly potato and bread; Biscuit includes store‐bought foods and sugar. Glimmix analysis yielded no convergence on a solution after 20 iterations for three foods that were either too frequent or infrequent among both groups.
More intervention mothers recalled messages (five out of eight message categories P < 0.0001), especially hygiene (washing hands before eating), responsive feeding and talking to the child during the meal (see Table 4). These were important messages in the responsive feeding programme, but emphasized much less in the regular nutrition sessions. These data confirm the salience of certain messages months after they were delivered. Intervention mothers also recalled more foods to feed their child at the ages when they could eat these foods, in particular the fruit, vegetables and eggs given to children during the practice sessions.
Table 4.
Number of mothers recalling any message given by any organization, categorized
| Message | Control | Intervention | F (1,160) | P |
|---|---|---|---|---|
| (n = 91) | (n = 92) | |||
| Ages to feed | 1 | 19 | 7.66 | 0.006 |
| What to feed | 23 | 62 | 30.66 | <0.0001 |
| Hygiene | 5 | 34 | 34.35 | <0.0001 |
| Growth monitoring | 0 | 2 | no convergence | |
| Nutritional disorders | 1 | 7 | 16.31 | <0.0001 |
| Responsive feeding | 5 | 31 | 17.33 | <0.0001 |
| Encourage self‐feeding | 1 | 7 | 2.13 | 0.15 |
| Talk to child | 1 | 10 | 18.53 | <0.0001 |
The analysis on dichotomized scores included clusters and controlled for child's age and sex, mother's education and assets.
Discussion
The findings demonstrate partial success of the responsive feeding intervention. Children showed more self‐feeding behaviours and gained more weight after the programme compared with control children whose mothers took the regular programme only. The effect sizes of 0.28 for weight and 0.48 for weight gain were respectable in comparison with past research. Reviews of nutrition educational interventions found a mean effect size of 0.28, usually in comparison with a no‐education control, and 0.42 when food supplements were combined with education (Dewey & Adu‐Afarwuah 2008). However, there were no benefits with regard to mouthfuls of food taken by the child and responsive behaviours of the mother. The findings are important in that they constitute the first evaluation of a behaviour‐change programme explicitly designed to practice self‐feeding and responsive feeding, and the intervention was delivered within an existing programme. Nonetheless, replications are required before it is determined exactly what behaviours should be targeted and how.
Questions may be raised as to how children gained weight if they did not eat more mouthfuls. The intake was reported to be representative and equivalent in both groups, as was morbidity. Two findings are relevant to the explanation: the variety of high quality foods and self‐feeding. Intervention mothers were observed to give more vegetables and less milk‐rice at the midday meal, and reported giving more eggs, fruit, vegetables and carbohydrates (bread, potatoes), which could have been given as snacks at follow‐up. Snacks typically do not include rice and so might be self‐fed, particularly by intervention children. Self‐feeding actions were positively correlated with mouthfuls taken here (r = 0.70, data not shown) and elsewhere (Moore et al. 2006), controlling for age. So although the intervention children did not consume more mouthfuls at the midday meal, they might have done so cumulatively throughout the day. The combination of more variety, higher quality, self‐fed foods throughout the day could explain the greater weight gain among intervention children.
Mothers in the responsive feeding intervention were not more responsive than controls. All mothers showed declines over time in responsive acts. This might have been because mothers saw less need to respond to children who were self‐feeding, although few fed themselves the entire meal. Because responsive praise and talk benefit children's development throughout the preschool years (e.g. Tamis‐LeMonda et al. 2001; Eshel et al. 2006), we tried to promote verbal responsiveness especially during self‐feeding and after refusals. However, refusals were more likely to elicit non‐responsive encouragement, such as attempting to push another mouthful of food, or forceful and threatening feeding, such as pressing the child to eat quickly (‘hurry, hurry’ was common) or warning the food would be given away. Mothers may also have been less responsive to children's signals to feed themselves because self‐feeding took place at a slower pace and so took longer.
Criticisms of efforts to promote responsive feeding often rely on the notion that cultural practices not only are difficult to change but also should not be changed. The implication is that the practice is homogeneous and stable because it is functional in a specific context. Some suggest that children should not be pushed to self‐feeding if they will eventually adopt such behaviours at 36 months. In defence of the need to promote responsive and self‐feeding is our evidence that it encourages better nutritional status; it may also improve appetite and child development. Although there are culturally common ways of feeding children, the ways are not homogeneous or static. The pre‐test variances of self‐feeding and responsive behaviours were large, indicating that some children did feed themselves and some mothers did respond to child cues. It was clear from our sessions that children did not need to be pushed to feed themselves; they did it willingly and with great enthusiasm. It will be necessary to demonstrate that 24–30 extra months of responsive and self‐feeding make a difference to the child's weight gain and appetite in these crucial years.
Limitations of the study include potential bias in the selection of groups, the delivery of the programmes and measurement. The need to exclude certain villages to avoid contamination may have introduced selection bias, although randomization appeared to be largely successful. Village clusters receiving the two programmes differed in size: the responsive feeding sessions were attended by four to eight mothers and their children, whereas the control sessions were attended by 10–20 women only some with children; this was due to our age restriction for responsive feeding. We had little control over the fidelity of programme implementation, as befits an effectiveness study. Peer educators were village mothers and the programme was new to them so they were not always thorough. Our behavioural outcomes were measured through observation and records written by trained and reliable assistants. Video recordings are expected to provide more reliable data but in this context aroused too much self‐consciousness. Also, we observed only one midday meal, although it appeared to be representative and the best time for maternal responsiveness. Snacks may have been the occasion for greater self‐feeding. A final limitation concerns the lack of group equivalence at baseline: intervention mothers had 1 year more schooling and more family assets than control mothers. Although both variables were statistically co‐varied, their combined effect could have led educated mothers to understand the feeding messages better and thereby use family resources to provide more high quality foods. This interpretation is consistent with the view expressed by others (e.g. Dewey & Adu‐Afarwuah 2008) that nutrition education may have sufficient impact without food supplementation only in contexts of food security. Food security, family assets and schooling are resources that allow parents to provide the food that must accompany newly learned feeding practices.
In conclusion, the responsive feeding intervention tested here provided significant improvements in children's weight and self‐feeding. Further refinements to the programme and replication with children of different ages and contexts are needed. However, the demonstrated gains indicate that a behaviour‐change nutrition programme focused on self‐feeding and responsive feeding behaviours adds value to existing education programmes for malnourished children.
Conflicts of interest
None declared.
Key messages
-
•
Targeting responsive feeding alone improves self‐feeding and weight gain.
-
•
Behaviour‐change interventions should include practice, not merely knowledge transfer.
Acknowledgements
Scientific and ethical approval was granted by ICDDR, B in Dhaka, Bangladesh and McGill University. The study has been registered as ISRCTN 24161700. Funding was provided by the UK Department for International Development, Bangladesh, with additional amounts from Plan International, Bangladesh and BRAC University's Institute of Educational Development. The pilot study was funded by Concordia University's Human Development Research Center grant from FQRSC. We especially thank Plan and Grameen Shikkha for permitting us to use their parenting groups as implementing sites, and also the peer educators, mothers and children for participating.
References
- Aboud F.E. (2007) Evaluation of an early childhood parenting program in rural Bangladesh. Journal of Health, Population and Nutrition 25, 3–13. [PMC free article] [PubMed] [Google Scholar]
- Baranowski T., Perry C.L. & Parcel G.S. (2002) How individuals, environments and health behaviors interact: social cognitive theory In: Health Behavior and Health Education (eds Glanz K., Rimer B.K. & Lewis F.M.), pp 165–184. Jossey‐Bass: San Francisco, CA. [Google Scholar]
- Bhandari N., Mazumder S., Bahl R., Martines J., Black R.E. & Bhan M.K. (2004) An educational intervention to promote appropriate complementary feeding improves child feeding practices and linear growth in rural Haryana, India. Journal of Nutrition 134, 2342–2348. [DOI] [PubMed] [Google Scholar]
- Dewey K.G. & Adu‐Afarwuah S. (2008) Systematic review of the efficacy and effectiveness of complementary feeding interventions in developing countries. Maternal and Child Nutrition 4, 24–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engle P.L. & Zeitlin M. (1996) Active feeding behavior compensates for low interest in food among young Nicaraguan children. Journal of Nutrition 126, 1808–1816. [DOI] [PubMed] [Google Scholar]
- Engle P.L., Bentley M. & Pelto G. (2000) The role of care in nutrition programmes: current research and a research agenda. Proceedings of the Nutrition Society 59, 25–35. [DOI] [PubMed] [Google Scholar]
- Eshel N., Daelmans B., Cabral de Mello M. & Martines J. (2006) Responsive parenting: interventions and outcomes. Bulletin of the World Health Organization 84, 992–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ha P.B., Bentley M.E., Pachon H., Sripaipan T., Caulfield L.E., Marsh D.R. et al. (2002) Caregiver styles of feeding and child acceptance of food in rural Vietnam. Food and Nutrition Bulletin 23 (Suppl. 4), 95–100. [PubMed] [Google Scholar]
- Hubbs‐Tait L., McDonald Culp A., Culp R.E. & Miller C.E. (2002) Relation of maternal cognitive stimulation, emotional support, and intrusive behavior during head start to children's kindergarten cognitive abilities. Child Development 73, 110–131. [DOI] [PubMed] [Google Scholar]
- Isabella R.A. (1993) Origins of attachment: maternal interactive behavior across the first year. Child Development 62, 605–621. [DOI] [PubMed] [Google Scholar]
- Isabella R.A., Belsky J. & Von Eye A. (1989) Origins of infant–mother attachment: an examination of interactional synchrony during the infant's first year. Developmental Psychology 25, 12–21. [Google Scholar]
- Moore A.C., Akhter S. & Aboud F.E. (2006) Responsive complementary feeding in rural Bangladesh. Social Science and Medicine 62, 1917–1930. [DOI] [PubMed] [Google Scholar]
- Penny M.E., Creed‐Kanashiro H.M., Robert R.C., Narro M.R., Caulfield L.E. & Black R.E. (2005) Effectiveness of an educational intervention delivered through the health services to improve nutrition in young children: a cluster‐randomised controlled trial. Lancet 365, 1863–1872. [DOI] [PubMed] [Google Scholar]
- Plan Bangladesh (2004) Parenting Manual and Picture Book. Author: Dhaka, Bangladesh. [Google Scholar]
- Plan Bangladesh (2005) Health of Mother and Child. Author: Dhaka, Bangladesh. [Google Scholar]
- Roy S.K., Fuchs G.J., Mahmud Z., Ara G., Islam S., Shafique S. et al. (2005) Intensive nutrition education with or without supplementary feeding improves the nutritional status of moderately‐malnourished children in Bangladesh. Journal of Health Population & Nutrition 23, 320–330. [PubMed] [Google Scholar]
- Schroeder D.G., Pachon H., Dearden K.A., Ha T.T., Lang T.T. & Marsh D.R. (2002) An integrated child nutrition intervention improved growth of younger, more malnourished children in northern Vietnam. Food and Nutrition Bulletin 23 (Suppl. 4), 50–58. [PubMed] [Google Scholar]
- Sguassero Y., De Onis M. & Carroli G. (2007) Community‐based supplementary feeding for promoting the growth of young children in developing countries (Review). The Cochrane Library 2, 1–17. [DOI] [PubMed] [Google Scholar]
- Tamis‐LeMonda C.S., Bornstein M.H. & Baumwell L. (2001) Maternal responsiveness and children's achievement of language milestones. Child Development 72, 748–767. [DOI] [PubMed] [Google Scholar]
- UNICEF (2007) Child and Mother Nutrition Survey in Bangladesh 2005. Author: Dhaka, Bangladesh. [Google Scholar]


