Abstract
The most common reasons cited by women for giving up breastfeeding early can be attributed to ineffective positioning and attachment and are therefore preventable. This study aimed to determine whether a 4‐h training programme in ‘hands off’ positioning and attachment support increases midwives’ knowledge and problem‐solving skills. Using an unrelated comparison group and a pre‐ and post‐intervention design, 108 midwives (experimental group) completed a 4‐h standard breastfeeding training workshop focusing on effective positioning and attachment and the use of hands‐off teaching methods. Knowledge and problem‐solving skills were assessed using a modified form of the previously validated Breastfeeding Support Skills Tool. Pre‐ and post‐training scores were compared with those of 27 student midwives (control group) who undertook the same assessments but without the breastfeeding training. Baseline knowledge scores of the midwives and the student midwives did not differ significantly (average difference 0.7 points to qualified midwives’ advantage, 95% CI = −3.4 to 1.9). Following training, the qualified midwives’ total scores increased significantly (7.2 points, 95% CI = 6.2–8.2). Minimal changes (1.4 points, 95% CI = −0.15 to 2.9) in students’ scores were found. The additional increase owing to training above that which might be expected due to practice (i.e. the average difference in change scores between the two groups) was 5.8 points (95% CI = 3.75–7.96), representing a large effect size for the training (d = 0.95). There is a large variation in the breastfeeding knowledge of midwives working in post‐natal care and, on average, they are no more skilled than senior student midwives. The study has shown that a 4‐h workshop in a positioning and attachment intervention, using a ‘hands‐off’ approach, can increase midwives’ knowledge of breastfeeding support relevant to the immediate post‐natal period. It is applicable to all midwives, and could be a cost‐effective way of improving the ability of mothers to begin and continue to breastfeed successfully.
Keywords: breastfeeding, knowledge assessment, training, positioning and attachment, infant feeding
Introduction
The long‐term benefits of breastfeeding for babies and their mothers have become well established in the past 20 years (Heinig & Dewey 1996, 1997). They include significant protection against childhood infections, including gastro‐enteritis (Howie et al. 1990), otitis media (Duncan et al. 1993) and urinary tract infections (Marild et al. 2004), and childhood diseases, including juvenile‐onset insulin‐dependent diabetes mellitus (Sadauskaite‐Kuehne et al. 2004), respiratory disease (Wilson et al. 1998) and obesity (Fewtrell 2004). A mother who breastfeeds is significantly less likely to develop premenopausal breast cancer (United Kingdom Case Control Study Group 1993; Beral 2002), ovarian cancer (Rosenblatt & Thomas 1993) and hip fracture (Cumming & Kleineberg 1993). The hazards of bottle feeding with formula are also increasingly being acknowledged, not only because of the increased incidence of diseases that could be prevented by breastfeeding, but also with errors and omissions in formulation (Renfrew et al. 2003) and contamination with pathogenic micro‐organisms (Weir 2002).
In England, midwifery policies in hospitals have been found to be confusing, not evidence based, and poorly implemented (Garforth & Garcia 1989; West & Topping 2000). Indeed, a small telephone survey in Scotland of community midwives and health visitors (Chalmers 1991) showed significant inter‐professional differences in advice given to breastfeeding mothers. It is to be expected that breastfeeding advice in National Health Service (NHS) hospitals in England will vary greatly, because practice is seldom supported by evidence‐based guidelines, although new guidance from the National Institute for Health and Clinical Excellence may help improve this in future (Dyson et al. 2006). A recent survey of healthcare practitioners, which included 212 midwives and 189 health visitors, found that only half had access to breastfeeding guidance at work, and many cited the different practices of others, leading to conflicting advice to mothers (Wallace & Kosmala‐Anderson 2007).
It is plausible that lack of guidance and divergent practices is a product of inadequate knowledge of evidence‐based practice. Poor knowledge of breastfeeding support has been demonstrated in a large survey of a range of community health professionals in Derbyshire, including midwives, health visitors, clinical medical officers and general practitioners (Hyde 1994). Knowledge levels among those routinely providing post‐natal care have been found to be hugely varied and often quite inadequate, in a study with maternal–neonatal nurses in the USA (Anderson & Geden 1990) and with a large survey of midwives in six maternity units in Scotland (Scott et al. 2004). A further survey in England and Wales of 549 non‐medical healthcare practitioners (Wallace & Kosmala‐Anderson 2007) showed that practitioners, irrespective of professional background and intensity of breastfeeding support in their current jobs, had self‐assessed themselves as having considerable knowledge deficits. There was somewhat more confidence in dealing with specific clinical problems, socio‐cultural aspects of breastfeeding, than the educative and practice skills. Of note, some 46% believed that they were less than competent at advising on positioning and attachment (Wallace & Kosmala‐Anderson 2007).
From April 2004, health targets for English and Welsh Primary Care Trusts were required to meet targets to increase the initiation of breastfeeding by two percentage points per annum, especially in those groups least likely to breastfeed (Department of Health 2002). The Department of Health (2003) has adopted the World Health Organization (WHO 2001) standard of exclusive breastfeeding to 6 months. It is now more important than ever that midwives deliver evidence‐based support, to enable mothers who choose to breastfeed, to do so for as long as they wish. At the time of the study, the most recent national infant feeding survey in 2000 showed that 71% initiated breastfeeding in England and Wales, although when the sample was standardized to reflect the age and education of participants in the 1985 survey (Martin & White 1988), it was reduced to 62%, suggesting that any improvement had been due to changes in the sample, rather than a true increase in breastfeeding uptake (Hamlyn et al. 2002). The prevalence of any breastfeeding declined to 54% at 2 weeks, 44% at 6 weeks and 28% at 4 months, with large differences according to socio‐economic classification and educational background. Most women reported that they gave up breastfeeding earlier than they had planned, and 90% of those who gave up by 6 weeks said that they had wanted to breastfeed for longer (Hamlyn et al. 2002).
It is now evident that mothers need skilled support if they are to breastfeed their babies successfully. A systematic review of 20 trials from 10 countries involving 23 712 mother–infant pairs found that all forms of extra professional support were associated with increased duration of any breastfeeding and the effect was even greater on the duration of exclusive breastfeeding (Sikorski et al. 2004). These studies do not specify the skill and knowledge needed to deliver these interventions. A systematic review of interventions to support the duration of breastfeeding (Renfrew et al. 2005) showed that none of the nine trials of educational interventions with professionals which included breastfeeding outcomes were effective on this key outcome variable.
Measures of midwifery skill and knowledge are generally inadequate, most studies using unstandardized questionnaires without reported psychometric properties of reliability and validity, making interpretation of differences between groups and between studies difficult. To address this, the Breastfeeding Support Skills Tool (BeSST), consisting of video footage and a pen‐and‐paper questionnaire, was developed with specific attention to validity and reliability (Hall Moran et al. 1999). It was subsequently used to evaluate skills gained during the 20‐h WHO/UNICEF Breastfeeding Management Course, where significant improvements in breastfeeding knowledge were demonstrated in separate groups tested before and after training (Hall Moran et al. 2000).
Studies of the impact of training on staff knowledge have shown mixed effects, with many hampered by poor design (Fairbank et al. 2000). Some studies use pre‐ and post‐test design comparing one cohort of practitioners before and after training using the same assessment (e.g. McIntyre & Lawlor‐Smith 1996). However, in the absence of a comparison group, it is not clear whether any gains seen are merely due to practice at completing the assessment, rather than increased knowledge or other unrelated factors which may change between the assessment points. Other studies have adopted a cross‐sectional design comparing two partially or completely different groups of practitioners, one before training and one after training (e.g. Bleakney & McErlain 1996; Hall Moran et al. 2000). While potentially avoiding the practice effect confound, if groups are not randomly allocated, then it cannot be ascertained with any confidence that any knowledge differences are not due to pre‐existing group differences.
This current paper reports the results of the midwifery training element of the Breastfeeding Best Start Randomised Controlled Trial (RCT), commissioned by the English Department of Health, to determine whether midwives can be trained to deliver a hands‐off midwifery intervention to primiparous mothers who wish to breastfeed, at the first feed on the post‐natal ward. The impact on mother outcomes is reported elsewhere (Wallace et al. 2006). The aim of the midwife training part of the study is: (1) to test the difference in breastfeeding knowledge of midwives before and after a training workshop; and (2) to determine whether any differences are attributable to test and retest practice effects, or to acquired learning. Secondary aims are to establish whether any job‐related variables predict which midwives make most gains, because these may be useful indicators in future of those most likely to require different or additional training.
Materials and methods
Study setting
The trial was conducted in four hospitals in the Midlands of England. Two of these were large teaching hospitals, each with three maternity wards with separate post‐natal bed areas, including tertiary referrals and serving largely urban and therefore socially diverse populations, compared with the two local general hospitals, each having one maternity ward with separate post‐natal bed areas and more rural catchment populations with less social diversity.
Sample eligibility and recruitment
Registered midwives working on post‐natal wards in the four hospitals were eligible for the study. Post‐natal ward midwives were invited to take part verbally and in writing by managers and researchers. All were volunteers to the Best Start Breastfeeding (BSB) trial. Those who consented were randomly allocated to either control or experimental groups of the BSB trial (Wallace et al. 2006). Although the control arm in the BSB trial had no additional training, the experimental arm did have additional training, as reported in this paper. A total of 108 midwives were allocated to undertake the experimental group training and provided complete data before and after training. The total number of qualified midwives available was determined by the larger RCT of which this study was part. A further 27 final‐stage student midwives at Coventry University formed a comparison control group, who were volunteers to undertake the assessments of breastfeeding knowledge used in this study. They were invited to participate by their tutor and all consented.
Ethical approval for the study was gained from three Local Research Ethics Committees and the Coventry University ethics committee.
Design
The design was a pre‐ and post‐training comparison using repeated‐measures analyses for the trained group of midwives, and comparison with final‐year student midwives to allow a check for a possible confound of repeated testing. The control midwives in the BSB trial were not available for testing, as discussed below. Knowledge gains due to training were anticipated to be large, based on an earlier study using the full version of the BeSST (Hall Moran et al. 2000). The effect size (d) in that study was calculated from the mean difference between the two groups pre‐ and post‐training (10.10) divided by the calculated pooled standard deviation for the two groups (9.39), giving an effect size of d = 1.076. Given an effect size of 1.076, and a within‐subjects comparison using a significance level of P = 0.05, a minimum group size of 9 would be required for an 80% power to detect an improvement of this magnitude. The 108 participants available and requiring training for the main trial far exceeded this. A control comparison group was included to evaluate the hypothesis that improvements might be attributable to the effects of practice on the same assessment. The size of the control group was planned so that improvements due to practice of half this size (d = 0.538) might be detected: this would require 30 participants.
Measures
Knowledge of breastfeeding practice was assessed using a modified version of the BeSST (1999, 2000), with permission of the authors. The BeSST involves a time‐limited questionnaire, with open‐ and closed‐ended questions, which are scored against a marking grid. As there is room for interpretation of free‐form responses, it is designed to be scored by experts in breastfeeding. The topics are grouped by phases of breastfeeding and, in the full version, there are four video clips which provide tests of observation and problem solving of breastfeeding difficulties. The study version retained those items relevant to the immediate post‐natal ward period of care (observation of a mother putting the baby to the breast, and questions relevant to attachment and positioning). Modification included the removal of five questions and one video clip related to breastfeeding at a later phase. Two new questions were inserted, relating to maternal perception of attachment and the recommended frequency and duration of feeds. The version used in this study therefore consisted of 16 items, with a potential range of scores from 0 to 51 and including responses to three video clips.
Biographic data were obtained by questionnaire for all participants, and included details of professional qualifications and training, clinical grade, working status (full‐time/part‐time), years practicing as a midwife (up to 2 years, 2–5 years, 6–10 years, 11–15 years, 16–20 years, and over 20 years), and duration of post‐natal experience in past 2 years (0–3 months, 4–6 months, 7–9 months, 10–12 months, and more than 12 months).
Procedure for assessment and training
Experimental group midwives attended a 4‐h training workshop in groups of about 6–8 staff on the hospital site where they normally worked, completing the biographic questionnaire and modified BeSST measure at the start of the workshop, and the same modified BeSST was repeated at the end. Each administration of the BeSST took approximately 30 min. To ensure anonymity but also enable tracking of data, midwives allocated personal codes to their questionnaires. The completed questionnaires were kept in envelopes and concealed from all but the first author, who was blind to individual midwives’ identities.
Training intervention
The training package was delivered by midwifery breastfeeding advisers attached to each site and is described in detail elsewhere (2003a, 2003b). It included factual knowledge about the anatomy and physiology of lactation, presentations on correct positioning and attachment, and interactive role‐play exercises to teach a ‘coaching style’ of communication necessary to achieve a ‘hands‐off’ approach to breastfeeding support at the first post‐natal ward feed. Student midwives in the comparison group had training on an unrelated topic, which lasted for a comparable length of time. Delivery of all assessments was as for the experimental group.
Analysis
BeSST answers were scored by an experienced midwifery lecturer (S.M.L.), who was independent of the delivery of the training. A random sample of 20% of papers was second marked by another experienced midwifery lecturer unconnected with the research project. This showed only one disagreement in 704 mark comparisons, representing 0.15% disagreement, and suggesting an excellent level of inter‐rater reliability. Examination of the variance of responses of the new items added to the BeSST confirmed that they were of a similar level to the original items and thus measured a similar range of ability. Internal reliability was assessed using Cronbach’s alpha. Ideally, a consistent scale where all items are measuring the same domain would have an alpha of 0.70 or over (Nunnally 1978). Examination of internal reliability using pre‐test scores gave a modest Cronbach’s alpha coefficient of 0.63. Scrutiny of item–total correlations demonstrated that the least consistent items were not the new ones created for the current trial. A maximum alpha of 0.67 was reached with removal of five items (4 original and 1 new). This alpha level was still not ideal, and concerns that validity of the scope of the scale might be sacrificed for a modest increase in consistency led to the decision to retain all items in subsequent analyses. Concurrent validity of the modified scale was investigated by the examination of baseline differences between groups expected to differ (i.e. those with differing levels of post‐natal experience). Baseline differences were analysed using t‐tests, one‐way analysis of variance (anova) or Spearman’s rank order correlations as appropriate to the data under consideration.
A two‐way anova (time: pre‐ and post‐training) (group: experimental group and control group) was used to examine the effects of training on the two groups of participants. Analyses of covariance (ancovas) were used to examine whether the effect of time (pre‐ and post‐training), i.e. the training effect seen within the trained midwives, was moderated when biographic factors were taken into account (e.g. previous breastfeeding training). All analyses were conducted using spss version 12 and using two‐tailed tests with alpha at 5%.
Results
The characteristics of two groups
All but one of the participants in the qualified midwives group was female. All participants in the student group were female. Data were not collected on age, as discussions at the design stage suggested that participants may have felt that this could compromise their anonymity within the smaller training groups. Of the qualified midwives, a total of 69 were based in the two larger hospitals, with the remaining 39 employed in the two smaller hospitals.
All the 108 experimental group participants who undertook the assessments and training were registered practicing midwives. Seventy‐five (69%) held a general registered or enrolled nurse qualification, six (6%) held a neonatal nurse qualification, and one (1%) was a qualified sick children’s nurse. Midwifery experience ranged from less than 2 years to more than 20 years (median category 6–10 years). More midwives were employed part‐time than full‐time (56% compared with 44%), a standard full‐time contract being 37.5 h per week. The majority of participants were employed on the minimum clinical grade E. None was employed at grade H and only two at grade I or above.
All but one participant had gained some post‐natal ward experience during the previous 2‐year period. Most (66%) had been working with post‐natal mothers and their babies for at least 6 months. Sixty‐four per cent had undertaken some form of formal post‐registration study. Table 1 illustrates the range of studies undertaken, showing that English National Board‐accredited breastfeeding support courses were the most popular, having been undertaken by almost half, followed by diploma courses, studied by almost a quarter.
Table 1.
Formal post‐registration and breastfeeding courses undertaken by participants
| No. (%) | |
|---|---|
| Post‐registration course | |
| Diploma | 25 (23) |
| Degree | 16 (15) |
| Master’s degree | 2 (2) |
| ENB course (any type) | 50 (46) |
| Other | 4 (4) |
| No study | 39 (36) |
| Breastfeeding training | |
| In‐Trust training | 64 (59) |
| Baby‐Friendly training | 25 (23) |
| ENB N64* | 3 (3) |
| ENB N75* | 1 (1) |
| NCT/La Leche | 3 (3) |
| Lactation consultant | 1 (1) |
| None | 31 (29) |
Percentages do not add up to 100 as some midwives had undertaken more than one course. *The ENB‐accredited breastfeeding support courses were N64 – Lactation and Breastfeeding for Nurses, Midwives and Health Visitors and N75 – Breastfeeding Theory and Practice for Nurses, Midwives and Health Visitors. ENB, English National Board.
The majority (71.2%) of participants had undertaken at least one breastfeeding support course. Table 1 shows the types of courses undertaken, with the most popular type being in‐Trust training as part of the midwife’s employment. Almost a quarter had undertaken training designed and accredited by the UNICEF Baby Friendly Initiative. However, more than a quarter (28.7%) had not undertaken a breastfeeding course of any type.
The 27 full‐time student midwives were all in the final stages of training leading to registration with the Nursing and Midwifery Council. All had completed the taught breastfeeding component of their studies, and all had undertaken post‐natal care involving clinical breastfeeding support. However, the majority (67%) had less than 6 months’ experience working in a post‐natal ward setting. No student midwife had attended any specific breastfeeding training courses outside of their programme of study.
Baseline levels of knowledge
The range of baseline scores for the qualified midwives was from 3 to 35, with a mean of 18.8 (SD = 6.47) (out of a maximum score of 51). Student midwives were very similar, with a mean baseline score of 18.1 (SD = 5.33). There were no significant differences between the scores of the two groups at baseline (95% CI = −3.4 to 1.9).
Supporting the concurrent validity of the modified BeSST, there was a modest trend for qualified midwives with a longer duration of post‐natal experience in the past 2 years to have higher baseline scores (r s = 0.18, n = 108, P = 0.057). Midwives with longer practice (although not necessarily in the post‐natal field) had significantly lower scores than those who had practiced for a shorter period of time (r s = −0.25, n = 108, P < 0.01) (see Fig. 1). Midwives who had undertaken some form of post‐registration study (details in Table 1) (n = 69, mean score = 18.9, SD = 7.00) did not differ on baseline scores from those who had no post‐registration study (n = 39, mean score = 18.7, SD = 5.48) (t 106 = 0.13, P = 0.90). However, there was a trend (t 106 = 1.89, P = 0.062) for those who had taken some form of specific breastfeeding training to have higher baseline scores (n = 77, mean score = 19.5, SD = 6.74) than those who had not undertaken any breastfeeding training (n = 31, mean score = 17.0, SD = 5.44).
Figure 1.
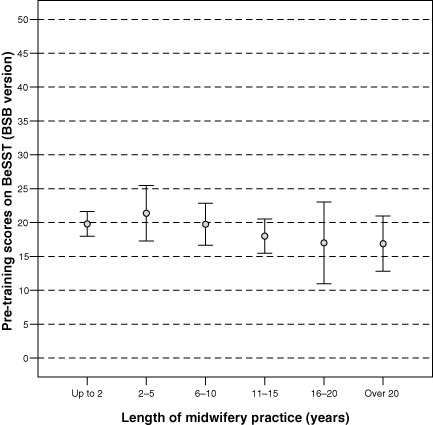
Pre‐training scores by midwifery experience, average and bars showing 95% confidence intervals for each group. Lower levels of pre‐training knowledge were found among those with longer midwifery experience. BeSST, Breastfeeding Support Skills Tool; BSB, Best Start Breastfeeding.
Pre‐training scores differed by hospital site (F 3,104 = 6.90, P < 0.01), with one site having significantly lower scores than the other three sites. This effect was partially accounted for by the higher numbers of midwives at this site with fewer months of recent post‐natal experience, although it remained significant even when this variable was taken into account.
Training results
Following exposure to the training package, the qualified midwives’ total scores increased on average by 7.2 points (95% CI = 6.2–8.2) to a mean of 26.0 (SD = 6.05) (Fig. 2). Scores of the student midwives who received training unrelated to breastfeeding were relatively unchanged at the second assessment, with a mean increase of 1.4 points (95% CI = −0.15 to 2.9) to a mean of 19.4 (SD = 4.87). A significant interaction between time and group within the anova confirmed that the effects of training differed significantly between the two groups (F 1,133 = 30.45, P < 0.01). The additional increase owing to training above that which might be expected due to practice (i.e. the average difference in change scores between the two groups) was 5.8 points (95% CI = 3.75–7.96). Comparison of this value against the SD of the experimental group post‐training (6.1) demonstrates a large effect size for the training (d = 0.95).
Figure 2.
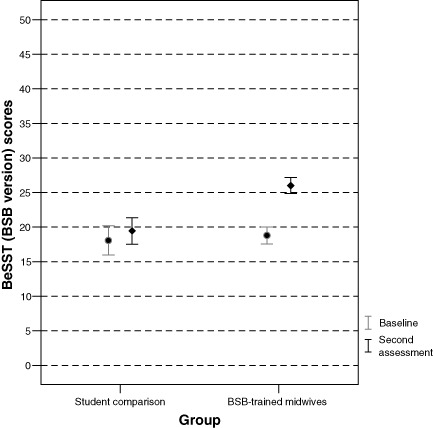
Mean pre‐test (baseline) and post‐test (second assessment) scores for BSB midwives exposed to the training and for student midwives who were not. BeSST, Breastfeeding Support Skills Tool; BSB, Best Start Breastfeeding.
To investigate the impact of potentially relevant biographic variables on the training increases observed in the qualified midwives, within‐subjects ancovas were performed. A significant covariate would demonstrate that training effects vary by levels of the biographic factor under consideration. None of the covariates made a significant contribution to the model (clinical grade F 1,106 = 0.03, P = 0.87; total experience F 1,106 < 0.01, P = 0.96; recent post‐natal experience F 1,106 = 1.21, P = 0.28; post‐registration qualifications F 1,106 = 0.24, P = 0.62; and previous breastfeeding training F 1,106 = 0.18, P = 0.67). This demonstrates that the training was equally effective for midwives in each of these biographic groupings. Training effects were comparable across the four hospital sites (F 3,104 = 0.89, P = 0.44), and remained so even when biographic differences were taken into account.
Discussion
This study demonstrates that a 4‐h training programme based on a ‘hands off’ midwifery intervention for post‐natal clinical practice is associated with significant increases in midwives’ knowledge and problem‐solving skill levels. The study design is an advance over others, in that the training intervention was standardized (2003a, 2003b) and the assessment of knowledge uses a modified existing measure with good reliability and face validity (Hall Moran et al. 1999). The study supports the effectiveness of a shorter 4‐h training programme as producing similar levels of knowledge gain on specific post‐natal breastfeeding support skills as the 20‐h UNICEF/WHO training programme (Hall Moran et al. 2000), with similar effect sizes, although it must be acknowledged that the UNICEF course provides training on a wider range of topics. For comparison, using their 28‐item scale, Hall Moran et al. (2000) found a group of midwives pre‐training had scores of 19.8 (SD = 6.7), whereas a different group post‐training had scores of 29.9 (SD = 11.2). In the current study, using the 16‐item scale, pre‐training scores for the qualified midwives were 18.7 (SD = 6.5), and the same midwives post‐training scored 26.6 (SD = 6.1).
This study also provides further evidence for the reliability and validity of the BeSST, although the instrument was modified in the current study to take account of the content areas required by post‐natal ward‐based midwives. The high levels of inter‐rater reliability in assessment of answers concur with previous published findings (Hall Moran et al. 1999). However, Cronbach’s alpha was much lower than found by Hall Moran et al. Even when the least consistent items were omitted, alpha levels did not reach those previously published. In part this may have been as the number of items in the modified BeSST was less than the number of items in the original BeSST – given the same level of inter‐item correlation, Cronbach’s alpha increases as a function of scale length. Alternatively, the low alpha may indicate that the BeSST is not a unidimensional scale. The least consistent items were not the new items created for this study, suggesting that this was not due to modifications to the BeSST within the current trial. For the purposes of assessment of knowledge increases, unidimensionality is not necessary, and a lack of this may correctly reflect the multifaceted nature of knowledge regarding breastfeeding which may fall into potentially unrelated domains. However, whether the BeSST is a unidimensional scale and, by extension, whether breastfeeding knowledge is a unitary construct are interesting questions worthy of further empirical investigation.
Further analyses carried out on the data suggest that many midwives are still confused after training between the use of the terms attachment and positioning, for example, by using the terms interchangeably (Law 2002; Inch et al. 2003c; Law et al. 2004). There may be historical reasons for this, as it has only been in the last 10 years or so, specifically since the inception of the Baby Friendly Hospital Initiative in 1989/90, that UNICEF and WHO agreed to use consistent terms that were non‐idiomatic and easy to translate, in order to make (global) teaching easier. Until then many people were using the term positioning to cover everything, and some were using words like ‘latch‐on’ or ‘fixing’. Although these had the merit of being precise, they could only refer to the relationship between the baby’s mouth and the breast, and were impossible to translate.
The current study represents a methodological advance over previous papers investigating breastfeeding knowledge gains in midwives due to training. In the current study, the BeSST is shown to be responsive to changes seen due to training and not suffering from ceiling effects (inability to detect improvements as participants already score at the highest level). Crucially, the analysis in the current study includes a comparison group, also given two applications of the BeSST, results of which demonstrate that repeated testing with no breastfeeding intervention training had no significant effect on scores due simply to practice on the assessment questions. It is possible, although somewhat implausible, that there may have been a level of practice effect present in the qualified midwives group that was not evident in the student group. Arguably, there may have been a ceiling effect with the students, in that they had reached their full potential for theoretical learning and thus no practice effect would be apparent. However, the baseline scores suggest that both groups had similar initial knowledge levels. In addition, we found no change in ability to learn within the qualified staff as they become more experienced, suggesting that there is no trend in ability to learn by level of experience and, therefore, ability to learn should be similar between the final‐stage student midwives and qualified midwives.
Ideally, our study would have used a comparison group that was composed of midwives within the larger RCT who had been randomly allocated not to receive the training. Each midwife and student midwife was given full information about the study prior to being invited to participate, and efforts were made to ensure that no one was made to feel compelled to take part. Full ethical committee approval was granted. However, it was not possible to obtain parallel biographic and modified BeSST knowledge scores of controls. The trial was conducted under time constraints, and it was believed by midwifery managers that participation by midwives as volunteers to the trial would be reduced if midwives in the control group were asked to undertake the same assessments as the experimental group, yet be expected to continue working alongside these midwives with the perceived advantage of additional training. Furthermore, the local NHS ethical committees objected to this aspect of the original protocol. Therefore, a non‐random comparison group was used. However, due to the similarity between baseline scores in the two groups and the clarity of the results, this is not likely to have had a major confounding effect.
This paper adds to our knowledge of the external validity of the BeSST by detecting plausible differences in baseline scores between midwives of different total lengths of practice experience and differing lengths of recent post‐natal experience over the past 2 years. Within the qualified midwives, the pre‐test baseline scores showed a surprisingly large variation in knowledge and no advantage over student midwives. In fact, the results suggest that qualified midwives who have been in practice longer had significantly lower scores than qualified midwives with fewer years of experience. This may in part be a function of the continually changing terminology used in breastfeeding training and the more recent shift to a hands‐off approach (2003a, 2003b). The pre‐test scores were not significantly moderated by grade, qualifications, full‐ or part‐time employment contract, or formal qualifications. This strongly suggests that all midwives need training in breastfeeding practice on a regular basis, perhaps with practical assessment and feedback on the application of this knowledge in situ. Further, as job‐related subgroup analyses did not moderate the training effect, it is recommended that all post‐natal ward staff can benefit from training. However, the wide range of scores at baseline also suggests that some form of training needs analyses would be useful to ensure that those with greatest deficits are given more intensive training to reach an acceptable level.
This pattern of varied knowledge may be typical of the UK context. Following qualification, a midwife is required to provide evidence of practice and continuing professional development (CPD) in order to remain registered (Nursing and Midwifery Council 2005). As long as the individual completes a minimum of 35 hours’ learning activity in the 3‐year period prior to re‐registration, the CPD requirement can be met through study of any subject of the midwife’s choice, as long as it is relevant for practice. There is no obligation for any midwife to study breastfeeding ever again. Indeed, a large survey of how midwives identify and meet their learning needs showed that the least popular topics were post‐natal issues (Mitchell 1997). Most (92%) identified their needs through discussion with colleagues, and few involved educationalists or used their appraisals. Given that the recent survey described above (Wallace & Kosmala‐Anderson 2007) showed that those with lower self‐assessed competence were least likely to seek update of their skills, it is all the more essential that actual, as opposed to self‐assessed, competence is part of a training needs analysis. Only then can training resources be targeted on those who need training, and that training can be targeted to job‐specific requirements. It is unsurprising therefore that midwives in current practice show huge variation in skill and confidence in supporting breastfeeding mothers.
Indeed, breastfeeding has had a low profile in midwifery education for many years. Programmes of education leading to registration as a midwife in the UK are governed by statute, and students must meet proficiency standards set by the Nursing and Midwifery Council (2004). At one time, breastfeeding was specifically included among the list of subjects to be taught to student midwives (UKCC 1983). However, it disappeared as compulsory course content, and was eventually replaced by 11 broad learning outcomes (UKCC 1993) and 29 competencies (English National Board 2000) that did not mention infant feeding at all. However, the most recently published standards of proficiency for pre‐registration midwifery education now specify that the education required to meet those standards must include providing advice and support to mothers for feeding babies (Nursing & Midwifery Council 2004). Individual educational institutions meet these requirements differently, and the amount and quality of breastfeeding education in curricula can vary. Indeed, the UNICEF UK Baby Friendly Initiative (2002) has proposed three specific standards for pre‐registration midwifery and health visiting education, with specific learning outcomes for breastfeeding, which has been met with an enthusiastic response. A Scottish university was recently awarded the first certificate of commitment to the Baby Friendly Education Award and could receive full accreditation within 2 years (UNICEF UK Baby Friendly Initiative 2005).
The equivalence at baseline of midwifery students who are about to qualify and those qualified midwives actively working on post‐natal wards is of concern in so far as it is to be expected that qualified midwives will be more skilled, and may be supervising students. A similar test of students from university courses providing less education on breastfeeding than Coventry University might create more divergent results.
The impact of training was a robust effect because improvement was consistent across almost all midwives, irrespective of grade and prior experience. Future research should examine whether the training can be delivered effectively to staff other than qualified midwives. In two of the larger hospital maternity sites, midwifery assistants routinely give breastfeeding care, but research has not addressed whether a 4‐h course would be sufficient, and whether their practice is more or less effective in sustaining breastfeeding.
The current study has shown that a 4‐h workshop in a positioning and attachment intervention, using a coaching, ‘hands‐off’ approach, can increase midwives’ knowledge of breastfeeding support relevant to the immediate post‐natal period. The programme could be rolled out to the large numbers of staff who need to address correct positioning and attachment care with early post‐natal mothers with only the cost of a 4‐h workshop. It is applicable to all midwives, and could be a cost‐effective way of improving the ability of mothers to begin and continue to breastfeed successfully.
Acknowledgements
The authors would like to thank the midwives, student midwives and the midwifery breastfeeding advisers who participated in this study, and Victoria Hall Moran and colleagues at the University of Central Lancashire for allowing the BeSST to be used. This work was funded by the Infant Feeding Initiative, Department of Health, England. The authors would also like to thank the two anonymous reviewers for their comments on an earlier draft of this paper.
References
- Anderson E. & Geden E. (1990) Nurses’ knowledge of breastfeeding. Journal of Obstetric Gynecological and Neonatal Nursing 20, 58–64. [DOI] [PubMed] [Google Scholar]
- Beral V. (2002) Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries including 50 302 women with breast cancer and 96 973 women without diseases. Lancet 360, 187–195. [DOI] [PubMed] [Google Scholar]
- Bleakney G. & Mcerlain S. (1996) Infant feeding guidelines: an evaluation of their effect on health professionals’ knowledge and attitudes. Journal of Human Nutrition and Dietetics 9, 437–450. [Google Scholar]
- Chalmers J.W.T. (1991) Variations in breastfeeding advice, a telephone survey of community midwives and health visitors. Midwifery 7, 162–166. [DOI] [PubMed] [Google Scholar]
- Cumming R.G. & Kleineberg R.J. (1993) Breastfeeding and other reproductive factors and the risk of hip fractures in elderly women. International Journal of Epidemiology 22, 684–691. [DOI] [PubMed] [Google Scholar]
- Department of Health (2002) Improvement, Expansion and Reform – The Next 3 Years: Priorities and Planning Framework 2003–2006. Department of Health: London. [Google Scholar]
- Department of Health (2003) New Recommendation Offers Mothers Support to Mark National Breastfeeding Awareness Week. Department of Health: London. [Google Scholar]
- Duncan B., Ey J., Holberg C.J., Wright A.L., Martinez F.D. & Taussig L.M. (1993) Exclusive breastfeeding for at least four months protects against otitis media. Pediatrics 5, 867–872. [PubMed] [Google Scholar]
- Dyson L., Renfrew M., Mcfadden A., Mccormick F., Herbert G. & Thomas J. (2006) Effective Action Briefing on the Initiation and Duration of Breastfeeding: Effective Action Recommendations. National Institute for Health and Clinical Excellence: York. [Google Scholar]
- English National Board for Nursing Midwifery and Health Visiting (2000) Education in Focus: Strengthening Pre‐registration Nursing and Midwifery Education. English National Board: London. [Google Scholar]
- Fairbank L., O’meara S., Renfrew M.J., Woolridge M., Sowden A.J. & Lister‐Sharp D. (2000) A systematic review to evaluate the effectiveness of interventions to promote the initiation of breastfeeding: Health Technology Assessment Programme 4. [PubMed]
- Fewtrell M.S. (2004) The long‐term benefits of having been breast‐fed. Current Paediatrics 14, 97–103. [Google Scholar]
- Garforth S. & Garcia J. (1989) Breastfeeding policies in practice – no wonder they get confused. Midwifery 5, 75–83. [DOI] [PubMed] [Google Scholar]
- Hall Moran V., Dinwoodie K., Bramwell R., Dykes F. & Foley P. (1999) The development and validation of the Breastfeeding Support Skills Tool (BeSST). Clinical Effectiveness in Nursing 3, 151–155. [Google Scholar]
- Hall Moran V., Bramwell R., Dykes F. & Dinwoodie K. (2000) An evaluation of skills acquisition on the WHO/UNICEF Breastfeeding Management Course using the pre‐validated Breastfeeding Support Skills Tool (BeSST). Midwifery 16, 197–203. [DOI] [PubMed] [Google Scholar]
- Hamlyn B., Brooker S., Oleinikova K. & Wands S. (2002) Infant Feeding 2000: A Survey Conducted on Behalf of the Department of Health, the Scottish Executive, The National Assembly for Wales and the Department of Health, Social Services and Public Safety in Northern Ireland. The Stationery Office: London. [Google Scholar]
- Heinig M.J. & Dewey K.G. (1996) Health advantages of breastfeeding for infants: a critical review. Nutrition Research Reviews 9, 89–110. [DOI] [PubMed] [Google Scholar]
- Heinig M.J. & Dewey K.G. (1997) Health effects of breastfeeding for mothers: a critical review. Nutrition Research Reviews 10, 35–56. [DOI] [PubMed] [Google Scholar]
- Howie P.W., Forsyth J.S., Ogston S.A., Clark A. & Florey C.V. (1990) Protective effect of breastfeeding against infection. British Medical Journal 300, 11–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde L. (1994) Knowledge of basic infant nutrition amongst community health professionals. Maternal and Child Health 19, 27–32. [Google Scholar]
- Inch S., Law S. & Wallace L. (2003a) Hands off! The Breastfeeding Best Start Project (1). Practising Midwife 6, 17–19. [PubMed] [Google Scholar]
- Inch S., Law S. & Wallace L. (2003b) Hands off! The Breastfeeding Best Start Project (2). Practising Midwife 6, 23–25. [PubMed] [Google Scholar]
- Inch S., Law S., Wallace L. & Hills R.K. (2003c) Confusion surrounding the breastfeeding terms ‘positioning’ and ‘attachment’. British Journal of Midwifery 11, 148. [Google Scholar]
- Law S.M. (2002) A Study of the Effect of a Training Package on Midwives’ Knowledge of Breastfeeding Support . Masters of Science. School of Health Sciences, University of Birmingham.
- Law S.M., Dunn O.M., Wallace L.M., Inch S.A. & Brown V. (2004) Is midwives’ knowledge of attachment and positioning really improved after training? In: Mapping New Horizons: Politics and Change – RCM Annual Conference Handbook, pp 67–68. Profile Productions Ltd: London. [Google Scholar]
- McIntyre E. & Lawlor‐Smith C. (1996) Improving the breastfeeding knowledge of health professionals. Australian Family Physician 25, S68–S70. [PubMed] [Google Scholar]
- Marild S., Hansson S., Jodal U., Oden A. & Svedberg K. (2004) Protective effect of breastfeeding against urinary tract infection. Acta Paediatica. 93, 164–168. [DOI] [PubMed] [Google Scholar]
- Martin J. & White A. (1988) Infant Feeding 1985 Office of Populations. Censuses and Surveys: London. [Google Scholar]
- Mitchell M. (1997) The continuing professional education needs of midwives. Nurse Education Today 17, 394–402. [DOI] [PubMed] [Google Scholar]
- Nunnally J.C. (1978) Psychometric Theory. McGraw‐Hill, New York. [Google Scholar]
- Nursing and Midwifery Council (2004) Standards of Proficiency for Pre‐registration Midwifery Education. Nursing and Midwifery Council: London. [Google Scholar]
- Nursing and Midwifery Council (2005) The PREP Handbook. Nursing and Midwifery Council: London. [Google Scholar]
- Renfrew M., Dyson L., Wallace L.M., D’Souza L., McCormick F. & Spiby H. (2005) Breastfeeding for Longer – What Works? National Institute for Clinical Excellence: London. [DOI] [PubMed] [Google Scholar]
- Renfrew M.J., Ansell P. & Macleod K.L. (2003) Formula feed preparation: helping to reduce the risks; a systematic review. Archives of Disease in Childhood 88, 855–858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblatt K.A. & Thomas D.B. (1993) Lactation and the risk of epithelial ovarian cancer. International Journal of Epidemiology 22, 192–197. [DOI] [PubMed] [Google Scholar]
- Sadauskaite‐Kuehne V., Ludvigsson J., Padaiga Z., Jasinskiene E. & Samuelsson U. (2004) Longer breastfeeding is an independent protective factor against development of type 1 diabetes mellitus in childhood. Diabetes/Metabolism Research Reviews 20, 150–157. [DOI] [PubMed] [Google Scholar]
- Scott J., McInnes R., Tappin D. & Guthrie E. (2004) Breastfeeding Opinions, Knowledge, Management Practices and Training of Scottish Midwives. Report (CZG/4/2/66) for the Scottish Executive Health Department Chief Scientist’s Office: Edinburgh. Executive summary available at: http://www.sehd.scot.nhs.uk/cso/Publications/ExecSumms/OctNov03/Scott.pdf [Google Scholar]
- Sikorski J., Renfrew M.J., Pindoria S. & Wade A. (2004) Support for Breastfeeding Mothers (Cochrane Review). Update Software: Oxford. [DOI] [PubMed] [Google Scholar]
- UKCC (1983) Handbook of Midwives Rules. United Kingdom Central Council: London. [Google Scholar]
- UKCC (1993) Midwives Rules. United Kingdom Central Council: London. [Google Scholar]
- UNICEF UK Baby Friendly Initiative (2002) Preliminary Consultation Report – Proposal to Introduce Best Practice Standards for Breastfeeding Education Provided to Midwifery and Health Visiting Students. UNICEF: London. [Google Scholar]
- UNICEF UK Baby Friendly Initiative (2005) Paisley celebrates first Baby Friendly University certificate at UNICEF annual conference. Baby Friendly News 19, 1. [Google Scholar]
- United Kingdom Case Control Study Group (1993) Breastfeeding and the risk of breast cancer in young women. British Medical Journal 307, 11–15. [Google Scholar]
- Wallace L.M. & Kosmala‐Anderson J. (2007) Training needs survey of midwives, health visitors and voluntary‐sector breastfeeding support staff in England. Maternal and Child Nutrition 3, 25–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace L.M., Dunn O.M., Alder E.M., Inch S., Hills R.K. & Law S.M. (2006) A randomised‐controlled trial in England of a postnatal midwifery intervention on breast‐feeding duration. Midwifery 22, 262–273. [DOI] [PubMed] [Google Scholar]
- Weir E. (2002) Powdered infant formula and fatal infection with Enterobacter sakazakii. Canadian Medical Association Journal 166, 1570. [PMC free article] [PubMed] [Google Scholar]
- West J. & Topping A. (2000) Breast‐feeding policies: are they used in practice? British Journal of Midwifery 8, 36–41. [Google Scholar]
- Wilson A.C., Forsyth J.S., Greene S.S., Irvine I., Hau C. & Howie P.W. (1998) Relation of infant diet to childhood health: seven year follow up of cohort of children in Dundee infant feeding study. British Medical Journal 316, 21–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2001) The Optimal Duration of Exclusive Breastfeeding: Results of a WHO Systematic Review. World Health Organization: Geneva. Available at: http://www.who.int/inf-pr-2-1/en/note2001-07.html [Google Scholar]


