Abstract
Objective
(1) To investigate differences in pain severity and its distribution between patients with and without diabetes mellitus (DM) in a population with advanced osteoarthritis (OA). (2) To explore the role of medication used for diabetes in these associations.
Research design and methods
This is a hospital-based cohort study of patients with advanced OA requiring total joint arthroplasty. Interviews and electronic records included: age, gender, occupation, DM (including medication and duration), analgesics used, anthropometry, joints affected by pain and disease duration. Joint pain was scored by the patients using numerical rating scale. Pain severity score was calculated by adding the number of joints affected by pain and the maximum pain score. All analyses were adjusted and/or stratified by gender, age and body mass index.
Results
In total, 489 patients with painful OA were included. From those, 139 patients had DM (30% males and 28% females, p=0.03). Pain severity, principally the number of joints affected by pain, and analgesic consumption, was higher in males with diabetes compared with males without diabetes (p=0.012 and OR=3.03; 95% CI 1.24 to 7.36, p=0.015, respectively). These associations were not significant in females (p=0.41 and p=0.66). Pain was more severe in males using insulin versus those who did not (p=0.025). Male subjects with diabetes had higher odds of hand pain or knee and hand pain compared with males without diabetes (OR=3.7, 95% CI 1.15 to 12; p=0.028 and OR=5.54; 95% CI 1.43 to 21.5, p=0.013, respectively).
Conclusions
Males with diabetes, especially those who require insulin, have more severe joint pain and consume more analgesics than males without diabetes or those who have DM and use other DM medication.
Keywords: adult diabetes, pain, risk factors, rheumatologic/musculoskeletal disease
Significance of this study.
What is already known about this subject?
Subjects with diabetes are nearly twice as likely to have osteoarthritis (OA) and arthroplasty than subjects without diabetes, independent of age or body mass index.
The association OA-diabetes has been found more frequently in males than in females.
What are the new findings?
Males with diabetes and principally those under insulin treatment present higher pain severity, including more joints affected by pain and higher consumption of analgesics than males without diabetes. We found gender heterogeneity regarding the effect of diabetes on OA-pain.
In females, diabetes mellitus has not a significant role on pain severity, considering the number of joints affected and the maximum pain score. For them, only a wider waist circumference had a significant association with pain severity.
How might these results change the focus of research or clinical practice?
This work will prompt research of the effect of insulin on joint pain in subjects with OA.
The effect of medicines for treating neuropathic pain needs to be measured, especially in males with diabetes and OA, compared with other traditional approaches. Male patients with diabetes and OA might benefit from a more specific analgesic treatment.
Introduction
There is increasing evidence on the association between type 2 diabetes mellitus (DM) and osteoarthritis (OA). Subjects with diabetes are nearly twice as likely to have OA and arthroplasty than subjects without diabetes, independent of age or body mass index (BMI).1–4 It has been suggested that subjects with both DM and OA have more severe symptoms.2 DM and insulin resistance have been considered as prognosticators of joint space narrowing and knee OA only in males.3 4 This difference concerning male gender, DM and OA especially regarding pain symptoms has not been fully investigated.
Patients with OA and diabetes might experience more intense pain than non-diabetic patients and it is unknown whether there are joints that could be more affected than others. Pain in non-weight-bearing joints, such as hand joints, in patients with DM and OA, might especially reflect involvement of neuropathic complications of diabetes in the source of OA pain.5
Enriched insulin receptor (InsR) expression has been demonstrated in the synovium of humans.6 7 In addition, it has been suggested that long-term insulin therapy, often needed to treat diabetes, may overload tissues such as cartilage.8 It is still necessary to know whether the glycemic control done through medications or simply if elevated insulin levels can influence the perception of OA pain in patients with diabetes. We aim to investigate differences in pain severity (level of pain reported, localization and number of joints affected by pain) between patients with and without DM in a population with advanced OA. We want to determine whether these differences exist for both genders. In addition, we would like to explore the role of medication used for diabetes in these associations.
Methods
This is a cohort study of patients with OA and total joint arthroplasty or waiting for the surgery. In total, 700 patients accepted to participate in the research. Electronic records of patients included: demographic information and anamnesis, X-rays of the affected joints (hip and/or knee), laboratory exams, diagnoses, including previous surgeries and dates, between others. Other methodological considerations have been previously described.9 Patients were questioned which joints had pain in the last month for most of the days and pain was rated from 0 to 10 (numerical rating scale, NRS) for each joint. The highest NRS score (most severe pain) was considered for analyses. Pain severity score (PSS) was calculated adding the number of joints affected by pain and the highest NRS score. For this study, only patients with pain at hip and/or knee joint(s) were selected. For diabetes, we used a clinical diagnosis of type 2 diabetes with ongoing antidiabetic treatment or a self-reported diagnosis of diabetes with a fasting glucose result ≥126 mg/dL. Diagnosis date, type of medication and for how long they have taken the medication were taken from the medical records or it was reported by the patients. It was measured waist and hip circumferences, height and weight. BMI was calculated. Family history of OA was defined as at least two first-degree relatives with OA diagnosis. During the interviews, we found 159 cases of patients with other diagnosis than OA (rheumatoid arthritis, lupus, avascular necrosis and fractures). These cases were excluded from the study. Analysis of variance or Mann-Whitney U test (non-normal distribution) was used to compare between two groups. Logistic and linear regression were used to analyze the association between joints affected and DM. χ2 test and Fisher’s exact test were used to compare variables. All analyses were adjusted and/or stratified by gender, age and BMI. The probability of a type I error was set to 0.05 for all analyses. All these analyses were made using SPSS V.15.0.
Results
In total, 489 patients with OA and pain were included in the study. The mean age was 65.8 years (SD: 10.6), 61.6% were females. Most of the population was obese, females were heavier than males and they reported more joint pain than males (table 1, p<0.001 and p=0.04, respectively).
Table 1.
Descriptive statistics of the study population
| Baseline characteristics | All (n=489) | Men (n=188) | Women (n=301) | P value |
| Mean age (SD) | 65.8 (10.6) | 64.5 (9.9) | 66.6 (11.1) | 0.04 |
| Principal joint affected* | <0.001 | |||
| Knee only | 240 (49) | 66 (35) | 174 (58) | |
| Hip only | 111 (23) | 61 (32) | 50 (17) | |
| Both joints affected (%) | 138 (28) | 61 (32) | 77 (26) | |
| Hand pain* | 61 (13) | 15 (8) | 46 (15) | 0.024 |
| Low back pain* | 191 (39) | 58 (31) | 133 (44) | 0.023 |
| Number of joints affected* | 2.11 (0.99) | 2.00 (0.93) | 2.18 (1) | 0.07 |
| Age of OA symptoms onset * | 53 (12.5) | 52.9 (12.6) | 53.7 (12.5) | 0.77 |
| BMI | 30.6 (6) | 29 (5.6) | 31.6 (6.1) | <0.001 |
| Waist circumference* | 99.8 (13) | 101 (14) | 98.9 (13) | <0.001 |
| Hip circumference* | 109.8 (11.8) | 105.7 (10) | 112.4 (12) | <0.001 |
| Waist/hip ratio* | 0.91 (0.09) | 0.96 (0.08) | 0.88 (0.08) | <0.001 |
| High blood pressure* | 339 (69) | 126 (67) | 213 (71) | 0.32 |
| Smoking* | 134 (27) | 8 7 (46) | 47 (16) | <0.001 |
| Alcohol* | 101 (21) | 82 (44) | 19 (6) | <0.001 |
| Cholesterolemia* | 181 (37) | 67 (36) | 114 (38) | 0.69 |
| Diabetes mellitus (%) * | 139 (28) | 56 (30) | 83 (28) | 0.03 |
| Type of DM treatment* | 0.26 | |||
| DM with metformin | 74 (15) | 34 (18) | 40 (13) | |
| DM no treated or other oral medication | 31 (6) | 13 (7) | 18 (6) | |
| Insulin | 34 (7) | 9 (5) | 25 (8) | |
| Age of diabetes diagnoses* | 64 (11) | 63 (10) | 63.8 (12) | 0.22 |
| Maximum pain score (NRS)* | 7 (2.3) | 7.5 (0.17) | 7.9 (0.13) | 0.04 |
| Analgesics/pain killers* | 363 (74) | 141 (75) | 222 (74) | 0.37 |
Values are mean values with SD in parenthesis or number of cases with percentage (%) for categorical variables.
*P values adjusted by age and BMI. Smoking and alcohol use were categorized as past and current versus never used. Maximum pain score was the highest value given by the patients using a numerical rating scale (NRS). In italics, P values <0.05
BMI, body mass index (kg/m2); DM, diabetes mellitus; OA, osteoarthritis.
Overall, 28.4% of the patients had diagnosis of DM. Thirty percent of them were males and 28% females (table 1, p=0.03) and they had a similar age of DM onset, around 64 years (table 1, p=0.22). For most of patients with diabetes (70%), OA symptoms started before diabetes symptoms. Most patients with diabetes were treated only with metformin (53%), with insulin or a combination of insulin and oral medication (25%), or with diet or other oral medication than metformin (22%). Males with DM consumed more analgesics than males without diabetes (84% vs 61%, OR=3.03; 95% CI 1.24 to 7.36, p=0.01, adjusted). There was no difference in analgesic consumption between females with and without diabetes (p=0.66).
There was no significant difference in the level of pain and in the number of joints affected by OA between women with and without diabetes (p=0.46, p=0.70). In our study, diabetes did not influence the severity score of OA symptoms in women (figure 1, p=0.41, respectively). In contrast, males with diabetes had more than two joints simultaneously affected by pain (p=0.002) and slightly higher pain score than those without diabetes. Therefore, males with diabetes had a higher PSS than males without diabetes (figure 1, p=0.01). In males, most severe pain (higher NRS) was found in patients receiving insulin compared with all other patients (p=0.025).
Figure 1.
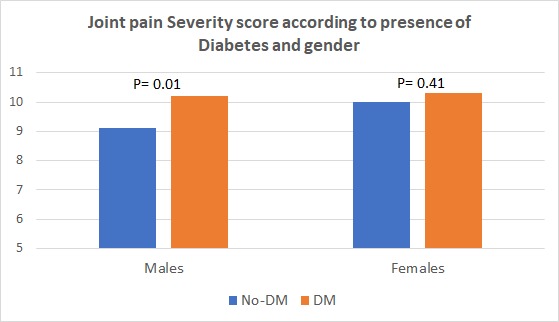
Comparison of pain severity in males and females with and without diabetes mellitus (DM). P adjusted by age and body mass index (BMI).
Regarding the medication to treat diabetes, sensitivity analysis in the group of patients with diabetes confirmed that those using insulin had more severe pain (highest NRS score) and more joints affected by pain than those patients without treatment or with oral treatment (p=0.03 and p=0.025). Therefore, we can affirm that male patients with diabetes taking insulin had a higher PSS than male patients without diabetes or with diabetes and other type of medication (figure 2, p=0.006).
Figure 2.
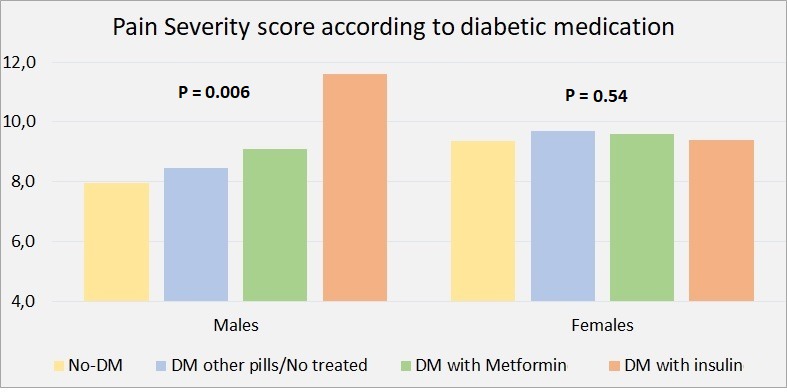
Pain severity was calculated with the maximum pain score in the numerical rating scale (NRS) and number of joints affected by pain. Figure shows a significant P-trend value only for male patients, when comparing the different diabetes mellitus (DM) medications. P adjusted by age and body mass index (BMI).
There was a difference in the duration of the disease among patients with diabetes, according to the treatment received, being greater for the group with insulin (p<0.001). However, duration of diabetes was not associated with pain severity in males, after adjustment for age and BMI (p=0.24).
In addition, male subjects with diabetes had higher odds of having hand or hand and knee, both affected by pain, compared with males without diabetes (OR=3.71, 95% CI 1.15 to 12; p=0.029 and OR=5.54, 95% CI 1.42 to 21.6; p=0.014, respectively). These associations were not significant in females (p=0.85 and p=0.93, respectively).
The most significant factor in females for a higher pain severity was having a wider waist circumference (p=0.002). This factor was not associated with pain in males (p=0.27). All analyses were adjusted for age and BMI.
Discussion
The current study has shown several aspects that were not previously analyzed in the relation of OA with DM. In our study with subjects with clinical OA requiring arthroplasty, pain severity was significantly higher in males with diabetes than in those without diabetes. Regarding symptoms, a previous study found more severe clinical symptoms of OA and higher rates of arthroplasty in subjects with DM compared with those without DM.2 However, in that publication, gender heterogeneity in the effect of diabetes on OA symptoms was not investigated perhaps, by the low number of cases with diabetes (n=69). Other few publications that investigated on this relation found that DM and insulin resistance might predict progression of joint space narrowing and knee OA only in males.3 4
The role of diabetic medication on OA pain was not previously explored. In our study, pain severity was higher in users of insulin than in those with other diabetic treatment or without treatment. Duration of diabetes did not explain differences in pain severity within the different diabetic treatment groups. This might suggest that severity of diabetes (requiring insulin) might influence severity of OA pain in males.
According to these and previous findings, the effect of insulin administration on OA progression (structural and symptomatic) needs further investigation. Insulin Receptors (InsRs) are abundant in normal and OA-affected chondrocytes and are widely distributed in the brain, with highest concentration in areas where nociceptive information is relayed as hypothalamus, cerebral cortex and hippocampus, between others, responding to physiologic insulin concentrations.8 10 11 Therefore, it is logical to propose that insulin dysregulation can contribute to OA, not only through cartilage degradation, but it might also modify pain perception.
Analgesic consumption was three times higher in males with diabetes compared with males without diabetes. Analgesic consumption seems a proxy for pain severity in this population. Higher consumption of analgesics might lead to other health problems that might aggravate diabetes.12
Knee and hand joints were more affected by pain in males with diabetes than without diabetes. The fact of presenting pain in proximal and distal joints, including non-weight-bearing joints, might suggest a direct contribution of one common complication of DM, as diabetic neuropathy, on the severity of OA. Mild to severe neurological alterations are common in patients with diabetes, with a higher prevalence and earlier presentation of distal sensorimotor neuropathy in males.13 14 It has been found a gender bias in diabetes severity also in rodent models of diabetes.15 This might help to explain why more males with diabetes have more pain and are affected with pain at distal joints as hands.
Finally, we found association of pain severity with waist circumference in females, independent of BMI. Larger waist circumference has been previously associated with joint pain in females and it has been proposed there is a link between metabolic syndrome and chronic pain.16
Conclusions
In conclusion, males with DM and principally those under insulin treatment present higher pain severity, including more joints affected by pain and a higher consumption of analgesics than males without diabetes. In females, DM has not a significant role on pain severity. For them, waist circumference and obesity seem to have more important role on pain severity.
The limitations of this study include those inherent to observational studies: exact exposure quantification (in relation to dose and frequency of medication use), unmeasured confounders or residual confounding from variables that might change over time as weight or pain fluctuation, between others. The power to analyze the effect of different diabetic treatments on pain was limited. However, we consider that this manuscript helps in understanding that part of the gender heterogeneity found in OA-DM relation in patients requiring arthroplasty, rely on symptomatic differences and not only on possible structural differences on cartilage tissue produced by DM. Considering the differences in pain between males with and without diabetes and within the diabetic treatment groups, we might hypothesize that the severity of joint pain in males is influenced by the existence and severity of DM, without excluding the possibility of neuropathic complications of diabetes influencing the pain level. We might suggest that this subgroup of patients with diabetes and OA would benefit from specific analgesic treatments for this type of pain, and that the response to medicines for treating neuropathic pain needs to be measured in males with diabetes and OA compared with other traditional approaches.
Acknowledgments
Thanks to all the patients and staff of Orthopedic Department, Hospital de Caridade São Vicente de Paulo, Jundiaí, SP, Brazil.
Footnotes
Contributors: MCCB designed the study, included patients, analyzed and interpreted the data, obtained the funding and wrote the manuscript. CLM, MVNL, MASM, JA and EGM were involved in acquisition of data and revision of the article. EM and MVNL interpreted the data, wrote the manuscript and provided administrative and logistic support. All authors reviewed and approved the manuscript content before submission.
Funding: This study was funded by São Paulo Research Foundation (FAPESP; grant number 2016/21039-0).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The research protocol was approved by the local ethics committee of the Medicine Faculty of Jundiaí (FMJ) and the National Commission for Research Ethics (CONEP-06/10/2015).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data (deidentified participants data) is available upon reasonable request to the corresponding author.
References
- 1.Hart DJ, Doyle DV, Spector TD. Association between metabolic factors and knee osteoarthritis in women: the Chingford study. J Rheumatol 1999;22:1118–23. [PubMed] [Google Scholar]
- 2.Schett G, Kleyer A, Perricone C, et al. Diabetes is an independent predictor for severe osteoarthritis: results from a longitudinal cohort study. Diabetes Care 2013;36:403–9. 10.2337/dc12-0924 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Eymard F, Parsons C, Edwards MH, et al. Diabetes is a risk factor for knee osteoarthritis progression. Osteoarthritis and Cartilage 2015;23:851–9. 10.1016/j.joca.2015.01.013 [DOI] [PubMed] [Google Scholar]
- 4.Karvonen-Gutierrez CA, Sowers MFR, Heeringa SG. Sex dimorphism in the association of cardiometabolic characteristics and osteophytes-defined radiographic knee osteoarthritis among obese and non-obese adults: NHANES III. Osteoarthritis and Cartilage 2012;20:614–21. 10.1016/j.joca.2012.02.644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Piva SR, Susko AM, Khoja SS, et al. Links between osteoarthritis and diabetes: implications for management from a physical activity perspective. Clin Geriatr Med 2015;31:67–87. 10.1016/j.cger.2014.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hamada D, Maynard R, Schott E, et al. Insulin suppresses TNF-dependent early osteoarthritic changes associated with obesity and type 2 diabetes. Arthritis Rheum 2016;68:1392–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ribeiro M, López de Figueroa P, Blanco FJ, et al. Insulin decreases autophagy and leads to cartilage degradation. Osteoarthritis and Cartilage 2016;24:731–9. 10.1016/j.joca.2015.10.017 [DOI] [PubMed] [Google Scholar]
- 8.Rosa SC, Rufino AT, Judas F, et al. Expression and function of the insulin receptor in normal and osteoarthritic human chondrocytes: modulation of anabolic gene expression, glucose transport and GLUT-1 content by insulin. Osteoarthritis and Cartilage 2011;19:719–27. 10.1016/j.joca.2011.02.004 [DOI] [PubMed] [Google Scholar]
- 9.Castano-Betancourt MC, Fruschein Annichino R, de Azevedo e Souza Munhoz M, et al. Identification of high-risk groups for complication after arthroplasty: predictive value of patient’s related risk factors. J Orthop Surg Res 2018;13:328 10.1186/s13018-018-1036-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Plum L, Schubert M, Brüning JC. The role of insulin receptor signaling in the brain. Trends Endocrinol Metab 2005;16:59–65. 10.1016/j.tem.2005.01.008 [DOI] [PubMed] [Google Scholar]
- 11.Tracey I, Mantyh PW. The cerebral signature for pain perception and its modulation. Neuron 2007;55:377–91. 10.1016/j.neuron.2007.07.012 [DOI] [PubMed] [Google Scholar]
- 12.Frishman WH. Effects of nonsteroidal anti-inflammatory drug therapy on blood pressure and peripheral edema. Am J Cardiol 2002;89:18–25. 10.1016/S0002-9149(02)02233-6 [DOI] [PubMed] [Google Scholar]
- 13.Callaghan BC, Cheng HT, Stables CL, et al. Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol 2012;11:521–34. 10.1016/S1474-4422(12)70065-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aaberg ML, Burch DM, Hud ZR, et al. Gender differences in the onset of diabetic neuropathy. J Diabetes Complications 2008;22:83–7. 10.1016/j.jdiacomp.2007.06.009 [DOI] [PubMed] [Google Scholar]
- 15.King KB, Rosenthal AK. The adverse effects of diabetes on osteoarthritis: update on clinical evidence and molecular mechanisms. Osteoarthritis Cartilage 2015;23:841–50. 10.1016/j.joca.2015.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Loevinger BL, Muller D, Alonso C, et al. Metabolic syndrome in women with chronic pain. Metabolism 2007;56:87–93. 10.1016/j.metabol.2006.09.001 [DOI] [PubMed] [Google Scholar]


