Abstract
Introduction
Type 2 diabetes mellitus (T2D) confers high atherosclerotic cardiovascular disease (ASCVD) risk. The metabolite trimethylamine N-oxide (TMAO) derived via gut flora has been linked to excess ASCVD.
Research design and methods
We analyzed data, biospecimens, and major adverse cardiovascular events (MACEs) from the prospective multicenter randomized Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial to assess its value in 330 high-risk individuals with T2D without evident atherosclerotic disease at enrollment.
Results
Incident cardiovascular events occurred in 165 cases; 165 controls matched by age, sex, and treatment arm experienced no incident events during follow-up. Cases and controls (mean age 64.5 years) had similar mean glycated hemoglobin (HbA1c) (8.2%) and mean 10-year ASCVD risk (23.5%); groups also had similar use of statins and antihypertensive medications at baseline and follow-up. Baseline plasma TMAO levels did not differ between groups after adjusting for ASCVD risk score, HbA1c, and estimated glomerular filtration rate, nor did TMAO distinguish patients suffering incident MACE from those who remained event-free.
Conclusions
TMAO’s prognostic value for incident ASCVD events may be blunted when applied to individuals with T2D with poor glycemic control and high baseline ASCVD risk. These results behoove further translational investigations of unique mechanisms of ASCVD risk in T2D.
Keywords: atherosclerosis, type 2 diabetes, risk predictors
Significance of this study.
What is already known about this subject?
Patients with type 2 diabetes (T2D) have significant risk of atherosclerotic cardiovascular disease (ASCVD) events like heart attack and stroke. Circulating levels of a metabolite from gut flora called trimethylamine N-oxide (TMAO) has shown association with greater subsequent cardiovascular events in patients with known coronary artery disease (CAD).
What are the new findings?
In a matched case–control cohort of subjects from the ACCORD (Action to Control Cardiovascular Risk in Diabetes) trial with T2D who did not have CAD at baseline, plasma levels of TMAO did not distinguish those with versus those without incident atherosclerotic events over an average of 4.7 years follow-up.
This cohort was unique compared with prior studies of TMAO in studying incident events in high-risk patients with poorly controlled T2D.
Although TMAO levels are known to increase with worsening renal function, it was not able to discriminate among individuals with T2D and normal or near-normal renal function between those with versus those without incident atherosclerotic events.
How might these results change the focus of research or clinical practice?
-
Further research is needed to identify targetable metabolites that better predict incident ASCVD events in patients with T2D. Three potential research questions arising from this research include:
What metabolites can be identified via untargeted assays to distinguish patients with T2D who suffer incident ASCVD events from those who remain ASCVD event-free?
Are there sex differences in ASCVD risk in patients with T2D that could be explained by TMAO?
How do newer antidiabetic and lipid-lowering medications impact TMAO’s predictive value for ASCVD risk in T2D?
Introduction
Diabetes mellitus is a major risk factor for atherosclerotic cardiovascular disease (ASCVD), responsible for most cerebrovascular and ischemic heart disease deaths.1 Strategies to mitigate ASCVD risk in individuals with diabetes include lifestyle modifications,2 statins, and novel antidiabetic drugs.3 4 Yet, the population burden of ASCVD in diabetes remains great, with significant residual risk even in those tolerating high-intensity statins.5–7 While glycemic control is important, the multicenter Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial actually found increased mortality with intensive glycemic control.8 With a global prevalence of type 2 diabetes (T2D) at 8.5% and rising, there is an urgent need to identify novel, targetable mechanisms of excess ASCVD risk in T2D.9
One such mechanism may involve the metabolite trimethylamine N-oxide (TMAO), formed via oxidation of gut flora-derived trimethylamine.10–13 In patients with acute coronary syndrome or highly prevalent coronary artery disease (CAD), higher levels of TMAO were shown to predict major adverse cardiovascular events (MACEs) after adjustment for traditional risk factors.14–16 However, a recent meta-analysis of more than 26 000 subjects noted significant impact of existing CAD as a covariate: as prevalence of CAD increased, so did the reported association between high TMAO levels and mortality.17
Diabetic individuals without evident baseline ASCVD were enrolled in the landmark US National Heart, Lung and Blood Institute (NHLBI)-sponsored ACCORD trial, and followed over a mean of 3.5 years for incident ASCVD.8 We leveraged access to ACCORD trial research data and biospecimens via NHLBI’s Biologic Specimen and Data Repository Information Coordinating Center (BioLINCC),18 to test the association between TMAO level and incident MACE over a long-term follow-up in individuals with T2D and elevated ASCVD risk but no baseline ASCVD.
Research design and methods
Study design
The present study represents a post hoc analysis of the ACCORD trial powered to detect differences in baseline plasma levels of TMAO in a matched case–control cohort of subjects with T2D without baseline ASCVD followed prospectively for occurrence of incident MACE. The NHLBI’s BioLINCC provided access to research data, as well as plasma samples from the ACCORD trial. The ACCORD study group has previously published detailed descriptions of trial design, methods, and study population,19 noting that it involved a randomized double 2×2 factorial design conducted at 77 clinical centers across the USA and Canada (NCT00000620).
Study population
We collected data from subjects (age 55–79 years) with T2D with atherosclerosis risk factors but without baseline clinical ASCVD, defined in ACCORD as: (1) previous myocardial infarction (MI) or stroke, (2) coronary or peripheral revascularization, (3) angina with ischemic ECG or imaging changes. Enrollment required subjects to have evidence of at least one of the following: microalbuminuria, left ventricular hypertrophy, or two additional risk factors among dyslipidemia, hypertension, current smoking, and obesity.19 For the purpose of this study, the 10-year ASCVD risk score at study entry was calculated employing the current prevention guidelines of the American Heart Association and American College of Cardiology.3
Outcome and follow-up
MACE was defined as cardiovascular (CV) death, non-fatal MI, non-fatal stroke, and any revascularization. Per ACCORD trial, CV death was defined as death from MI, heart failure, arrhythmia, invasive CV interventions, CV causes after non-CV surgery, stroke, unexpected death presumed to be from ischemic CV disease occurring within 24 hours after the onset of symptoms, and death from other vascular diseases (eg, pulmonary emboli, abdominal aortic aneurysm rupture).19
From ACCORD trial records, 165 subjects with incident MACE throughout the trial and 165 matched subjects without incident MACE were identified. BioLINCC provided all available cases meeting inclusion criteria with adequate plasma available for assays, and similarly provided controls matched by age, sex, and ACCORD treatment arm (ie, intensive vs standard glycemic/blood pressure/lipid control). MACE outcomes were recorded at 4-month follow-up intervals until ACCORD trial completion.
BioLINCC staff used SAS code to select case/controls through the following process. ACCORD subjects aged 55–79 years at enrollment, without clinical ASCVD and with specimens of sufficient volume were separated into two categories: (1) those with any CV death, non-fatal and fatal stroke, non-fatal MI, non-fatal and fatal congestive heart failure, fatal coronary heart disease, revascularization, or unstable angina event (defined as any of the following variables having a “0” value: censor_po, censor_cm, censor_nst, censor_nmi, censor_chf, censor_tst, censor_maj, censor_ex) and (2) those without the above events (defined as all the above variables having a “1” value). Then subjects in category 1 were randomly matched 1-to-1 with subjects in category 2 as long as they had the same gender, same treatment arm, and same value of the baseline_age variable rounded to the nearest 10 (ie, age groups: 55–<65; 65–<75; and 75–79).
To further explore the independent role of TMAO relative to other risk factors and interventions, we compared baseline and 24 months of follow-up values for the following variables: glycated hemoglobin (HbA1c) levels, total cholesterol, low-density lipoprotein-cholesterol (LDL), high-density lipoprotein-cholesterol (HDL), estimated glomerular filtration rate (eGFR), and CV medications.
We tested the association between levels of TMAO and incident MACE defined as above (primary outcome). A secondary analysis was also conducted to evaluate the relationships among TMAO and hard MACE defined as CV death, non-fatal MI, and non-fatal stroke.
Biomarkers
BioLINCC provided access to the following biomarkers measured during the study: total cholesterol, LDL, HDL, triglycerides, HbA1c, serum creatinine, urine creatinine, urine albumin, eGFR, fasting plasma glucose, alanine aminotransferase, and serum potassium levels. At enrollment, additional fasting blood samples were appropriately collected and processed for storage, including refrigerated transport and storage at around −80°C. Freeze/thaw cycles were minimized prior to transfer to our laboratory. From frozen biospecimens, we additionally measured high-sensitivity C reactive protein, iron, and ferritin levels.
Quantification of TMAO
TMAO was quantified in stored plasma samples with the use of a stable isotope dilution assay and high-performance liquid chromatography (HPLC) with electrospray ionization tandem mass spectrometry (MS), on an UltiMate 3000 HPLC system coupled to a TSQ Quantiva Triple Quadrupole Mass Spectrometer (Thermo Fisher, San Jose, California, USA), using multiple reaction monitoring analysis.20 After thawing, samples underwent methanol protein precipitation, filtration, and dilution in 0.1% formic acid before being passed through an Imtakt Scherzo SM-C18 column (100 mm×1 mm, 3 µm particle size, 38°C) at a flow rate of 50 µL/minute. Separation of TMAO was accomplished using an isocratic flow of 80% solvent A (H2O with 0.1% formic acid) and 20% solvent B (acetonitrile) for 4 min, as published by Petriello et al.21 Sample injection volume was 1 µL. The mass spectrometer was operated in positive electrospray ionization mode set to a capillary voltage of 3.5 kV and a capillary temperature of 300°C. Vaporizer temperature was set to 50°C, sheath gas of 8 arbitrary units, and auxiliary gas set to 3 arbitrary units. Monitored transitions were as followed: 85.1/66.1 for d9-TMAO and 76.1/59.1 for TMAO, with all collision energies at 25 eV. The mean value of triplicate measurements was recorded for each sample. Detailed methodology for sample preparation and liquid chromatography–mass spectrometry quantification for plasma TMAO is provided as online supplementary material. All the analyses were performed blinded to subjects’ clinical information.
bmjdrc-2019-000718supp001.pdf (691.5KB, pdf)
Statistical methods
Sample size and power: The hypothesis that TMAO is significantly elevated in subjects with T2D with versus without incident MACE was based on at least a 30% difference.15 17 22 Using these values, the minimum required sample size is 216 (108 per group) with a type I error rate of 0.05% and 80% power.
Data are presented as mean±SD or as median and IQR for continuous variables and as proportions for categorical variables. Paired t-tests were used to compare the matched cases and controls for continuous variables if the normality assumption was not violated. Otherwise, non-parametric Wilcoxon signed rank tests were conducted. Comparison between matched cases and controls for categorical variables was performed using McNemar’s tests or marginal homogeneity tests. A linear mixed effects regression model was used to test the effect of MACE on plasma levels of TMAO after adjusting for within-pair correlations and multiple covariates. Conditional logistic regression analysis was used to test the predictive power of TMAO on MACE. Statistical significance was set at two-tailed p<0.05. IBM SPSS Statistic 21.0 (Chicago, Illinois, USA) was used for all statistical analyses.
Data and resource availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request. All resources analyzed during the current study are commercially available.
Results
In total, 330 subjects aged 63.5±5.9 years, 44% female, were considered—165 subjects with and 165 subjects without MACE; baseline characteristics are summarized in table 1. Subjects in this cohort were similar to the entire ACCORD population with respect to age, gender, lipid panel, systolic blood pressure, HbA1c levels, creatinine, and fasting plasma glucose levels.19 At study entry, HbA1c and 10-year ASCVD risk score averaged 8.4% (IQR 7.6%–9.0%) and 23.5% (IQR 15.3%–32.1%), respectively, demonstrating elevated CV risk profile of this population at baseline. MACE-positive and MACE-negative groups were similar with regard to total cholesterol, LDL, eGFR, fasting plasma glucose, and rates of major CV medication use including statin, beta-blocker, antiplatelet and antihypertensive drugs (table 1). After an average of 4.7 years, 181 events occurred in the MACE positive group: 25 CV deaths, 46 non-fatal MIs, 17 non-fatal strokes, and 93 coronary revascularizations. Characteristics at 24-month follow-up are summarized in table 2. Notably, clinical trial participation improved lipid profile, glycemic control and CV medication prescription in the entire cohort. Subjects with versus without MACE had similar total cholesterol, LDL, HbA1c, eGFR, and CV medication status after 2 years (table 2).
Table 1.
Cohort characteristics at baseline
| All subjects (N=330) |
Case (n=165) |
Control (n=165) |
P value | |
| Age, years | 62.7 (58.7–67.5) | 62.9 (59.0–67.3) | 62.5 (58.5–67.6) | 0.781† |
| Female, n (%) | 146 (44) | 73 (44) | 73 (44) | 1.000‡ |
| Race | ||||
| Caucasian, n (%) | 219 (66) | 111 (67) | 108 (65) | 0.464 |
| Black, n (%) | 53 (16) | 27 (16) | 26 (16) | |
| Hispanic, n (%) | 22 (7) | 13 (8) | 9 (5) | |
| Other, n (%) | 36 (11) | 14 (8) | 22 (13) | |
| BMI, kg/m2 | 32.2±5.3 | 32.0±5.3 | 32.3±5.4 | 0.551¶ |
| Total cholesterol, mg/dL | 187±47 | 191±50 | 184±45 | 0.214¶ |
| HDL cholesterol, mg/dL | 39 (34–47) | 38 (33–47) | 41 (36–49) | 0.043* |
| LDL cholesterol, mg/dL | 103 (81–127) | 106 (81–131) | 102 (81–125) | 0.356 |
| Triglycerides, mg/dL | 163 (117–242) | 168 (127–261) | 159 (112–235) | 0.078 |
| Systolic blood pressure, mm Hg | 137±17 | 139±18 | 136±17 | 0.050¶ |
| HbA1c, % | 8.2 (7.6–9.0) | 8.3 (7.6–9.2) | 8.1 (7.6–8.9) | 0.144 |
| 10-year ASCVD risk, % | 23.5 (15.3–32.1) | 23.4 (15.4–33.3) | 23.5 (13.5–30.1) | 0.038* |
| eGFR, mL/min | 88.4 (72.3–104.9) | 87.5 (71.8–104.5) | 88.9 (73.1–105.1) | 0.399 |
| Fasting plasma glucose, mg/dL | 165 (135–200) | 162 (132–201) | 169 (138–198) | 0.801 |
| Smoking status | ||||
| Never, n (%) | 157 (48) | 80 (48) | 77 (47) | 0.855§ |
| Former, n (%) | 138 (42) | 69 (42) | 69 (42) | |
| Current, n (%) | 35 (11) | 16 (10) | 19 (12) | |
| ACEI and/or ARB, n (%) | 226 (68) | 114 (69) | 112 (68) | 0.815‡ |
| β-blocker, n (%) | 73 (22) | 38 (23) | 35 (21) | 0.892‡ |
| Statin, n (%) | 187 (57) | 91 (55) | 96 (58) | 0.653‡ |
| Antiplatelet, n (%) | 169 (51) | 83 (50) | 86 (52) | 0.740‡ |
Variables expressed as mean±SD, median (IQR), or n (%).
*P value <0.05 considered significant.
†Wilcoxon signed rank test.
‡McNemar’s test.
§Marginal homogeneity test for paired subjects.
¶Paired t-test.
ACEI, ACE inhibitor; ARB, angiotensin II receptor blocker; ASCVD, atherosclerotic cardiovascular disease; BMI, body mass index; eGFR, estimated glomerular filtration rate; HbA1c, glycated hemoglobin; HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Table 2.
Cohort characteristics at 24-month follow-up
| All subjects at baseline (n=292) | All subjects at follow-up (n=292) | Cases at follow-up (n=146) |
Controls at follow-up (n=146) |
P1 | P2 | |
| Total cholesterol, mg/dL | 182 (154–211) | 164 (138–196) | 166 (138–199) | 162 (137–194) | <0.001*† | 0.619† |
| HDL cholesterol, mg/dL | 39 (34–47) | 40 (34–48) | 39 (33–45) | 42 (35–52) | 0.290† | 0.033*† |
| LDL cholesterol, mg/dL | 103 (81–126) | 87 (70–112) | 92 (71–111) | 86 (70–115) | <0.001*† | 0.981† |
| HbA1c, % | 8.2 (7.6–8.9) | 7.1 (6.4–7.8) | 7.0 (6.3–8.0) | 7.1 (6.4–7.7) | <0.001*† | 0.350† |
| eGFR, mL/min | 89.30 (74.80–105.38) | 79.00 (64.20–91.00) | 79.90 (63.98–90.48) | 75.80 (64.60–94.80) | <0.001*† | 0.527† |
| ACEI and/or ARB, n (%) | 202/292 (69) | 205/258 (79) | 106/133 (80) | 99/124 (80) | 0.009*‡ | 1.000‡ |
| Antiplatelet, n (%) | 148/289 (51) | 165/257 (64) | 86/133 (65) | 79/123 (64) | 0.001*‡ | 0.658‡ |
| Statin, n (%) | 173/290 (60) | 194/258 (75) | 105/133 (79) | 89/124 (72) | <0.001*‡ | 0.043*‡ |
Variables expressed as median (IQR) or n (%).
*P < 0.05 considered significant.
†Wilcoxon signed rank test for paired subjects or repeated measures within each subject.
‡McNemar’s test for paired subjects or repeated measures within each subject.
ACEI, ACE inhibitor; ARB, angiotensin II receptor blocker; eGFR, estimated glomerular filtration rate; HbA1c, glycated hemoglobin; HDL, high-density lipoprotein; LDL, low-density lipoprotein; P1, comparison between baseline and follow-up for all subjects in the entire cohort; P2, comparison between matched cases and controls at follow-up.
Biomarkers
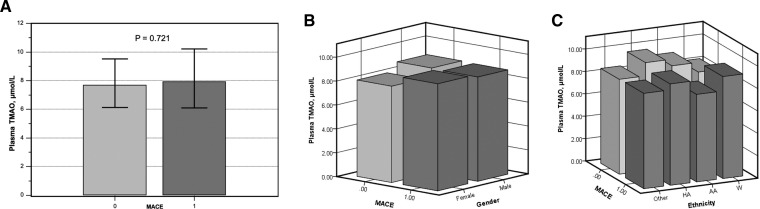
Table 3 summarizes biomarker results showing a trend toward greater albuminuria in cases versus controls but otherwise similar biomarker profiles. Overall, the median plasma TMAO concentration was 7.8 μmol/L (IQR 6.1–9.8). The median plasma TMAO did not differ significantly according to MACE status (p=0.721), levels of 7.9 μmol/L (IQR 6.1–10.2) and 7.7 μmol/L (IQR 6.1–9.6) in MACE-positive and MACE-negative groups, respectively. Based on the linear mixed effects model, MACE status was not significantly associated with plasma levels of TMAO after adjusting for HbA1c, ASCVD risk score, and eGFR (p=0.538). According to the conditional logistic regression model, plasma TMAO was not predictive of MACE outcome (OR 0.991, 95% CI 0.965 to 1.017, p=0.494).
Table 3.
Biomarker profiles
| All subjects (N=330) |
Cases (n=165) |
Controls (n=165) |
P value | |
| hsCRP, mg/L | 6.79±9.27 | 7.04±9.99 | 6.52±8.48 | 0.803 |
| Ferritin, ng/mL | 219.31±211.48 | 218.50±212.40 | 220.15±211.30 | 0.581 |
| Iron, µg/dL | 76.38±27.78 | 75.70±29.19 | 77.05±26.40 | 0.308 |
| ALT, mg/dL | 27.40±12.68 | 25.99±10.33 | 28.82±14.56 | 0.167 |
| Potassium, mmol/L | 4.44±0.42 | 4.48±0.39 | 4.40±0.45 | 0.051 |
| Serum creatinine, mg/dL | 0.89±0.22 | 0.90±0.22 | 0.88±0.22 | 0.349 |
| Urinary creatinine, mg/dL | 124.48±67.12 | 121.01±70.50 | 127.94±63.59 | 0.064 |
| Urinary albumin, mg/dL | 11.68±34.32 | 16.02±44.21 | 7.34±19.23 | 0.017* |
| Plasma TMAO, µmol/L | 7.77 (6.11–9.85) | 7.94 (6.10–10.24) | 7.70 (6.14–9.57) | 0.721 |
Variables expressed as mean±SD or median (IQR). Paired t-tests or Wilcoxon signed rank tests were used for statistical comparisons.
*P value <0.05 considered significant.
ALT, alanine aminotransferase; hsCRP, high-sensitivity C reactive protein; TMAO, trimethylamine N-oxide.
Importantly, we obtained similar results when testing the association between TMAO and hard MACE in a matched case–control subgroup (online supplementary tables S1 and S2). Baseline TMAO also did not distinguish T2D patients with vs without MACE by sex or ethnicity subgroups (figure 1).
Figure 1.
In a cohort of subjects from the ACCORD trial with high risk of major adverse cardiovascular events (MACEs), plasma levels of trimethylamine N-oxide (TMAO) at baseline did not distinguish those who went on to suffer a MACE from those who did not (A). Error bars represent IQR. Similarly, no significant differences were found when evaluating by sex (B) or ethnicity (C). AA, African-American; HA, Hispanic American; W, white.
Discussion
In the present post hoc analysis of 330 subjects with T2D without baseline ASCVD, half of whom suffered incident ASCVD events, we found no significant difference in baseline TMAO between those with incident events versus matched subjects who remained ASCVD event-free over 4.7 years follow-up despite similar ASCVD and cardiometabolic risk profiles. These findings warrant attention as they are novel, differ from previous publications, and help refine our understanding of TMAO as a potential biomarker for ASCVD events.
First, the study population is unique for understanding TMAO’s predictive value in a large, well-matched diabetic case–control cohort followed prospectively for incident ASCVD events. Standard risk predictors and commonly employed biomarkers fail to predict CV events when applied to high-risk diabetic subjects.5 6 In fact, as our study shows, MACE subgroups were tightly matched for all the major biomarkers commonly adopted to predict CV events including age, gender, 10-year ASCVD risk score, serum creatinine, eGFR, HbA1c levels, and CV medication use at baseline and follow-up. With over 23 million individuals with diabetes in the USA alone who carry an enormous healthcare burden, there is an urgent clinical need to identify novel mechanisms of excess atherosclerosis in T2D that can be targeted to reduce risk.1 11 23 Our study cohort was particularly well-suited to explore TMAO’s potential to predict incident ASCVD events in stable, high-risk individuals with T2D when commonly used parameters fail to improve risk stratification.
The second important aspect of our cohort was the elevated CV risk profile at study entry, with poor glycemic control (median HbA1c >8.0%), elevated 10-year ASCVD risk score (median >23%), and suboptimal prescription/adherence to proven cardioprotective medical therapies. Importantly, this population profile deserves the greatest attention as it is very much in line with individuals encountered in daily clinical practice: in a recent pooled analysis of more than 2000 diabetic individuals participating in community-based studies, less than 40% were at target for blood pressure, LDL, and HbA1c levels.6 Thus, as compared with previous studies involving TMA/TMAO, there is a substantial difference in baseline CV risk profile. In a recent study involving subjects with T2D, Tang and colleagues showed that higher plasma levels of TMAO were predictive of MACE (death, non-fatal MI, and non-fatal stroke) even after adjusting for other traditional CV risk factors over a period of 3 years of follow-up.15 However, there are key differences in population profile in the two studies: (1) in our cohort, none of the subjects had CAD at baseline, as compared with almost 50% prevalence in that work where nearly half had a history of prior MI and approximately one-third had previously undergone coronary revascularization; (2) HbA1c levels are substantially different with baseline HbA1c required to be >7.5% for enrollment in ACCORD, compared with HbA1c levels spread over a wide range with a significant proportion of subjects with good glycemic control (HbA1c<6.5%); (3) TMAO levels in our study were significantly higher, averaging 7.8 (6.1–9.8) μmol/L compared with 4.4 (IQR (2.8–7.7) μmol/L) in the prior study. This is not surprising, as TMAO levels tend to track HbA1c levels.22 24
Another important relationship to note is that TMAO levels increase with worsening renal function.25 26 In Tang’s study, renal function was significantly lower in the tertile of higher TMAO levels (eGFR 61 (45–82) mL/min/1.73 m2), which was set as reference to calculate the association with MACE outcome. In our study, we did not have this important confounder effect as the entire cohort demonstrated normal or close to normal eGFR levels and did not differ by MACE status. We further note prior work that indicated a mortality association in patients with eGFR <90 mL/min/1.73 m2 in a cohort without the severity of diabetes as in this study.27
Analyzed together, these two studies help to refine the role of TMAO in T2D. In fact, while TMAO seems to have a powerful predictive value for MACE in T2D populations characterized by high prevalence of CAD and good glycemic control, the discriminatory power of TMAO appears to be lost when measured in subjects with T2D without evident CAD but high ASCVD risk and poor glycemic control.
As TMAO showed no relationship to incident ASCVD events in our study population of high-risk subjects with T2D but without baseline CAD, negative findings have also been recorded in other cohorts. Mueller and colleagues, studying 339 patients undergoing coronary angiography for the evaluation of suspected CAD, found no association between levels of TMAO and incident CV events during 8 years of follow-up.25 Similarly, negative results have been recorded in cohorts with chronic kidney disease and heart failure.25 28 29
The collective evidence to date on TMAO underscores the importance of assessing the entire cardiometabolic profile of diabetic individuals. Their TMAO levels are influenced by renal function, diet, gut microbiome, history of CAD and glycemic control. Our cases and controls were tightly matched for renal function (mostly normal in the two groups) with similar levels of HbA1c and no history of CAD. In this scenario, TMAO did not emerge as a biomarker predictive of ASCVD events.
Limitations
The study was not powered for sensitivity analyses based on sex, underscoring the need to assess TMAO’s prognostic significance in diabetic women versus men in a larger cohort. We also do not know if groups differed in dietary choline and L-carnitine intake, though lack of difference cannot be attributed to variations in standard of care between groups since rates of cardioprotective medication prescriptions at follow-up were similar. Formation of trimethylamine—TMAO’s antecedent—depends on intestinal microbes encountering suitable precursors in the diet.30 Assessment of diet, host genetics, and antibiotic therapy, all of which significantly influence the gut microbiome,31 is warranted in future studies. Focusing on incident events, we did not assay biospecimens at follow-up for TMA/TMAO to inform our understanding of change in these biomarkers over time. TMAO warrants long-term, prospective evaluation in high-risk diabetic individuals receiving newer antidiabetic and lipid-lowering medications compared with the treatment regimens used in ACCORD.
Conclusions
In a cohort of stable high-risk subjects with T2D matched for age, sex, and glycemic control with very similar CV risk profiles, plasma levels of TMAO were not associated with MACE over 4.7 years of follow-up. TMAO’s prognostic value for incident ASCVD events appears to be blunted when applied to diabetic subjects without established CAD but with poor glycemic control and high baseline ASCVD risk.
Acknowledgments
The authors thank the NHLBI’s BioLINCC for its assistance.
Footnotes
Contributors: AC: study design, biospecimen analysis, data interpretation, data analysis and manuscript writing; AO: biospecimen analysis, data interpretation, data analysis and manuscript writing; MCB: biospecimen analysis, data analysis and manuscript writing; AS: biospecimen analysis, data interpretation and manuscript writing; VHW: data interpretation and manuscript writing; SS: study design, data interpretation, manuscript writing; XH: data analysis and statistical analysis; GA: data interpretation and manuscript writing; WAH: data interpretation and manuscript writing; SVR: study design, biospecimen analysis, data interpretation, data analysis and manuscript writing. SVR, principal investigator, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Funding: This work was supported by the US National Center for Advancing Translational Sciences (UL1TR002733).
Competing interests: AC was recipient of a grant-in-aid by Fondazione Umberto Veronesi, Italy.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available on reasonable request.
References
- 1.Benjamin EJ, Virani SS, Callaway CW, et al. . Heart disease and stroke Statistics-2018 update: a report from the American heart association. Circulation 2018;137:e67–492. 10.1161/CIR.0000000000000558 [DOI] [PubMed] [Google Scholar]
- 2.Eckel RH, Jakicic JM, Ard JD, et al. . 2013 AHA/ACC guideline on lifestyle management to reduce cardiovascular risk: a report of the American College of Cardiology/American heart association Task force on practice guidelines. Circulation 2014;129:S76–99. 10.1161/01.cir.0000437740.48606.d1 [DOI] [PubMed] [Google Scholar]
- 3.Goff DC, Lloyd-Jones DM, Bennett G, et al. . 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American heart association Task force on practice guidelines. Circulation 2014;129:S49–73. 10.1161/01.cir.0000437741.48606.98 [DOI] [PubMed] [Google Scholar]
- 4.Newman JD, Vani AK, Aleman JO, et al. . The changing landscape of diabetes therapy for cardiovascular risk reduction: JACC state-of-the-art review. J Am Coll Cardiol 2018;72:1856–69. 10.1016/j.jacc.2018.07.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong ND, Zhao Y, Quek RGW, et al. . Residual atherosclerotic cardiovascular disease risk in statin-treated adults: the multi-ethnic study of atherosclerosis. J Clin Lipidol 2017;11:1223–33. 10.1016/j.jacl.2017.06.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wong ND, Zhao Y, Patel R, et al. . Cardiovascular risk factor targets and cardiovascular disease event risk in diabetes: a pooling project of the Atherosclerosis risk in Communities study, multi-ethnic study of atherosclerosis, and Jackson Heart Study. Diabetes Care 2016;39:668–76. 10.2337/dc15-2439 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Libby P, Ridker PM, Hansson GK. Progress and challenges in translating the biology of atherosclerosis. Nature 2011;473:317–25. 10.1038/nature10146 [DOI] [PubMed] [Google Scholar]
- 8.Gerstein HC, Miller ME, Byington RP, et al. . Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–59. 10.1056/NEJMoa0802743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.International Diabetes Federation IDF diabetes atlas, 2017. Available: http://www.diabetesatlas.org/
- 10.Vinjé S, Stroes E, Nieuwdorp M, et al. . The gut microbiome as novel cardio-metabolic target: the time has come! Eur Heart J 2014;35:883–7. 10.1093/eurheartj/eht467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention National diabetes statistics report: estimates of diabetes and its burden in the United States. Atlanta GUDoHaHS, 2014. [Google Scholar]
- 12.Velasquez MT, Ramezani A, Manal A, et al. . Trimethylamine N-oxide: the good, the bad and the unknown. Toxins 2016;8. doi: 10.3390/toxins8110326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang Z, Klipfell E, Bennett BJ, et al. . Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 2011;472:57–63. 10.1038/nature09922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tang WHW, Wang Z, Levison BS, et al. . Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med 2013;368:1575–84. 10.1056/NEJMoa1109400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tang WHW, Wang Z, Li XS, et al. . Increased trimethylamine N-oxide Portends high mortality risk independent of glycemic control in patients with type 2 diabetes mellitus. Clin Chem 2017;63:297–306. 10.1373/clinchem.2016.263640 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li XS, Obeid S, Klingenberg R, et al. . Gut microbiota-dependent trimethylamine N-oxide in acute coronary syndromes: a prognostic marker for incident cardiovascular events beyond traditional risk factors. Eur Heart J 2017;38:814–24. 10.1093/eurheartj/ehw582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schiattarella GG, Sannino A, Toscano E, et al. . Gut microbe-generated metabolite trimethylamine-N-oxide as cardiovascular risk biomarker: a systematic review and dose-response meta-analysis. Eur Heart J 2017;38:2948–56. 10.1093/eurheartj/ehx342 [DOI] [PubMed] [Google Scholar]
- 18.Giffen CA, Carroll LE, Adams JT, et al. . Providing contemporary access to historical Biospecimen collections: development of the NHLBI Biologic Specimen and Data Repository Information Coordinating Center (BioLINCC). Biopreserv Biobank 2015;13:271–9. 10.1089/bio.2014.0050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Buse JB, et al. Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: design and methods. Am J Cardiol 2007;99:S21–33. 10.1016/j.amjcard.2007.03.003 [DOI] [PubMed] [Google Scholar]
- 20.Bennett BJ, Vallim TQdeA, Wang Z, et al. . Trimethylamine-N-Oxide, a metabolite associated with atherosclerosis, exhibits complex genetic and dietary regulation. Cell Metab 2013;17:49–60. 10.1016/j.cmet.2012.12.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Petriello MC, Hoffman JB, Sunkara M, et al. . Dioxin-Like pollutants increase hepatic flavin containing monooxygenase (FMO3) expression to promote synthesis of the pro-atherogenic nutrient biomarker trimethylamine N-oxide from dietary precursors. J Nutr Biochem 2016;33:145–53. 10.1016/j.jnutbio.2016.03.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Obeid R, Awwad HM, Rabagny Y, et al. . Plasma trimethylamine N-oxide concentration is associated with choline, phospholipids, and methyl metabolism. Am J Clin Nutr 2016;103:703–11. 10.3945/ajcn.115.121269 [DOI] [PubMed] [Google Scholar]
- 23.American Diabetes Association Economic costs of diabetes in the U.S. in 2012. Diabetes Care 2013;36:1033–46. 10.2337/dc12-2625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lever M, George PM, Slow S, et al. . Betaine and trimethylamine-N-oxide as predictors of cardiovascular outcomes show different patterns in diabetes mellitus: an observational study. PLoS One 2014;9:e114969 10.1371/journal.pone.0114969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mueller DM, Allenspach M, Othman A, et al. . Plasma levels of trimethylamine-N-oxide are confounded by impaired kidney function and poor metabolic control. Atherosclerosis 2015;243:638–44. 10.1016/j.atherosclerosis.2015.10.091 [DOI] [PubMed] [Google Scholar]
- 26.Tang WHW, Wang Z, Kennedy DJ, et al. . Gut microbiota-dependent trimethylamine N-oxide (TMAO) pathway contributes to both development of renal insufficiency and mortality risk in chronic kidney disease. Circ Res 2015;116:448–55. 10.1161/CIRCRESAHA.116.305360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gruppen EG, Garcia E, Connelly MA, et al. . Tmao is associated with mortality: impact of modestly impaired renal function. Sci Rep 2017;7:13781 10.1038/s41598-017-13739-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kaysen GA, Johansen KL, Chertow GM, et al. . Associations of trimethylamine N-oxide with nutritional and inflammatory biomarkers and cardiovascular outcomes in patients new to dialysis. J Ren Nutr 2015;25:351–6. 10.1053/j.jrn.2015.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Trøseid M, Ueland T, Hov JR, et al. . Microbiota-Dependent metabolite trimethylamine-N-oxide is associated with disease severity and survival of patients with chronic heart failure. J Intern Med 2015;277:717–26. 10.1111/joim.12328 [DOI] [PubMed] [Google Scholar]
- 30.Romano KA, Vivas EI, Amador-Noguez D, et al. . Intestinal microbiota composition modulates choline bioavailability from diet and accumulation of the proatherogenic metabolite trimethylamine-N-oxide. MBio 2015;6:e02481 10.1128/mBio.02481-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Human Microbiome Project Consortium Structure, function and diversity of the healthy human microbiome. Nature 2012;486:207–14. 10.1038/nature11234 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjdrc-2019-000718supp001.pdf (691.5KB, pdf)