Abstract
The objective was to investigate the effects of novel policing techniques on hospital-observed incidence, healthcare utilization, mortality and costs associated with gun violence, from the perspective of a level-1 trauma center. An eight-year retrospective review evaluating the clinical and financial effects of gunshot wound (GSW) encounters between January 1st, 2010 and December 31st, 2017. Individuals who presented to the emergency department (Level-1 trauma center in Camden, NJ) between January 1, 2010 and December 31, 2017 with GSW (995 encounters) were included; however, patients with incomplete financial or medical record data were excluded (55 encounters). Patients were subdivided into two cohorts: before and after changes in policing tactics (May 1st, 2013). 940 total firearm-related encounters were included in the study. Following the policing changes, the hospital-observed quarterly incidence of GSW encounters decreased by 22% post-policing changes, 44.3 to 34.6 (p = 0.038). Average quarterly days spent in-house for GSW treatment decreased 220.7 to 151.3 (31%) days. Hospital observed mortality increased from 13.5% of presentations to 17.3% of presentations (p = 0.106). Total cost savings associated with the policing change was roughly $254,000 per quarter (p = 0.023). In areas susceptible to high rates of gun violence, similar novel policing tactics could significantly decrease hospital-observed incidence, costs and healthcare utilization demanded by firearm-related injury.
Keywords: Gun violence, Hospital economics, Health policy, Environment, Preventive medicine, Public health
1. Introduction
Firearm injury is a substantial public health concern in the United States, demanding valuable resources from various stakeholders within the US healthcare system. Peaking in 2014 (32,858), violence-related firearm injury was the cause of 282,000 US deaths between 2006 and 2014 (Centers for Disease Control and Prevention, 2005). During the same time period, an estimated 705,000 individuals were hospitalized for firearm injuries in the US, generating $6.6 billion in hospital costs (Gani et al., 2017, Spitzer et al., 2017). While gun violence continues to provoke significant social and financial burden, research endeavors focusing on firearm injury prevention are nearly nonexistent.
Despite New Jersey demonstrating the second strictest gun laws among US states, the city of Camden has perennially suffered exorbitant rates of firearm injury (Giffords Law Center, 2018). In 2011, Camden experienced the highest homicide rate and highest violent crime rate among qualified US cities (population > 50,000); 6.0 and 7.2 times the national average respectively (Federal Bureau of Investigation, 2011). Subsequently, the city of Camden underwent a multitude of changes to mitigate the social and financial effects of violence. In early 2013, the city implemented military grade surveillance technologies and community policing tactics as a last resort. This study seeks to report the hospital-observed effects of the aforementioned policing changes on firearm injury from the perspective of Camden’s only level-1 trauma center, as the vast majority of gunshot victims are brought to this institution. Specifically, the changes in hospital-observed incidence, mortality, healthcare utilization and subsequent healthcare costs associated with firearm injury.
2. Methods
Following Institutional Review Board approval, a retrospective chart review was performed on individuals who presented with a firearm-related injury at our institution. A query of the institutional trauma database was conducted using all gunshot wound (GSW)-related International Classification of Disease (ICD)-9 or ICD-10 codes (assault, self-inflicted, accidental, etc.) to identify the appropriate medical records.
Individuals who presented to Camden’s level-1 trauma center with firearm-related injuries, between January 1, 2010 and December 31, 2017, were included in the review. Patients with incomplete financial or medical record data were excluded. Following initial evaluation of the study population as a whole, patients were subdivided into two cohorts: before and after city changes in policing tactics. The aforementioned changes in Camden’s policing tactics began in early 2013 with the final modification being the turnover of policing authorities. On May 1st, 2013, the Camden County Police Department (CCPD) acquired responsibility of the city’s policing needs. This date served as the cutoff for encounter classification into either cohort. Quarterly reporting is used in statistical evaluation of the cohorts and Q2-2013 is considered a conservative beginning of the policing changes, observing part of the transition period. Quarter yearly rates (ie. annual costs / 4) were analyzed and reported to normalize for the differences in time between the two cohorts. The denominator of quarterly incidence was the city of Camden’s population for the year of the reporting quarter per 100,000. Medical records were reviewed for the following demographic and clinical variables: age, sex, race, date of incident, emergency department (ED) arrival time, ED disposition, length of stay (LOS), Injury Severity Score (ISS), mortality, location of gunshot wound, alcohol screening results and quantity of blood units transfused. Alcohol screenings were classified as positive or negative. Alcohol screenings were omitted if not conducted or if the subject expired upon ED presentation. To capture shootings involving multiple victims, ED arrival times were reviewed and categorized as a cluster if two or more ED presentations occurred within 20 min of each other. In the absence of police reports, clusters are utilized as a potential to identify multiple GSW encounters resulting from a single incident. The institution’s billing database was subsequently queried for encounter cost, charge and insurance information at the time of discharge for each encounter. Insurance was categorized by funding source into public (Medicare, Medicaid, charity care, etc.), private or self-pay.
2.1. Statistical analysis
Significant data outliers were identified using modified z-scores for length of stay and cost variables, where a modified z-score +/− 3.5 was used as cutoff criteria (Iglewicz and Hoaglin, 1993). Two individual encounters were identified as significant outliers for both LOS and cost. These values were winsorized to the next highest length of stay and cost values for each of the extreme outlier encounters. Winsorizing outliers provides a lower-weight of the outliers on the homogenous data set. The winsorized data points were reduced to the nearest value of the respective cohort to limit the outlier’s influence on means analysis. Considering both outliers for cost and LOS were in the before policing changes cohort, this was considered a simple, conservative approach to evaluating the hypothesis without neglecting extraordinary, realistic cost/LOS outcomes for GSW encounters. Reported totals include data outliers; however, mean testing and annual rates, including LOS and total cost, use winsorized data points of the two extreme outlier encounters. Chi-Square analysis was used to compare categorical and dichotomous variables across cohorts. Following normality testing, mean or median based analysis was used to evaluate continuous variables. Independent sample t-tests were used for normally distributed variables and Wilcoxen Mann-Whitney U-tests were used for non-normal variables. Odds ratio testing was conducted using binary linear regression analysis without statistical selection. The binary regression model’s predicted probabilities were tested against the observed values to determine diagnostic ability. Sensitivity, specificity and area under the curve are reported. Statistical analysis of the clinical and billing data was carried out using IBM SPSS Statistics Software Version 16.
3. Results
3.1. Encounter demographics
995 encounters (985 patients) were identified between January 1st, 2010 and December 31st, 2017. 55 encounters were excluded for either incomplete medical charts or incomplete billing data, resulting in 940 hospital encounters included for analysis. Six of the included encounters were a result of suicide, accounting for 3 deaths. Of the 940 analyzed hospital encounters, 68.1% were African-American and 92.0% were males. Average age was 28.67 (range 2–96, median 27). >50% of incidents occurred between 8:00 pm and 2:00AM. Race/ethnicity and funding source were the only significant differences in encounter demographics across cohorts (Table 1).
Table 1.
GSW Patient Demographics and Presentation Characteristics and GSW Clinical Characteristics Before and After Policing Changes.
| Study Population | Before (n = 444) | After (n = 496) | Entire Population (n = 940) | p-value |
|---|---|---|---|---|
| Demographics | ||||
| Gender | N (%) | N (%) | N (%) | |
| Male | 412 (92.8) | 453 (91.3) | 865 (92.0) | 0.409 |
| Female | 32 (7.2) | 43 (8.7) | 55 (8.0) | |
| Ethnicity/Race | ||||
| African-American | 294 (66.2) | 346 (69.8) | 640 (68.1) | <0.001 |
| Caucasian | 14 (3.2) | 29 (5.8) | 43 (4.6) | |
| Hispanic/Latino | 127 (28.6) | 93 (18.8) | 220 (23.4) | |
| Other/Unknown | 9 (2.0) | 28 (5.6) | 37 (3.9) | |
| Age | ||||
| 0–17 | 36 (8.1) | 39 (7.9) | 75 (8.0) | 0.945 |
| 18–30 | 263 (59.2) | 290 (58.5) | 553 (58.8) | |
| 31–40 | 99 (22.3) | 110 (22.1) | 209 (22.2) | |
| 41–50 | 24 (5.4) | 26 (5.2) | 50 (5.3) | |
| >50 | 22 (5.0) | 31 (6.3) | 53 (5.7) | |
| Time of Arrival | ||||
| 2:01 AM − 8:00 AM | 70 (15.8) | 96 (19.4) | 166 (17.7) | 0.334 |
| 8:01 AM − 2:00 PM | 43 (9.7) | 56 (11.3) | 99 (10.5) | |
| 2:01 PM − 8:00 PM | 97 (21.8) | 95 (19.2) | 192 (20.4) | |
| 8:01 PM − 2:00 AM | 234 (52.7) | 249 (50.1) | 483 (51.4) | |
| ED Disposition | ||||
| Not Admitted | 126 (28.4) | 148 (29.8) | 274 (29.1) | 0.006 |
| Admitted | 284 (64.0) | 280 (56.5) | 564 (60.0) | |
| Fatal | 34 (7.7) | 68 (13.7) | 102 (10.9) | |
| Funding Source | ||||
| Public Insurance | 324 (73.0) | 342 (69.0) | 666 (70.9) | <0.001 |
| Private Insurance | 30 (6.7) | 90 (18.1) | 120 (12.8) | |
| Self-Pay | 90 (20.3) | 64 (12.9) | 154 (16.4) | |
| Clinical Characteristics | ||||
| Quarterly Incidence, mean (SD) | 44.3 (12.8) | 34.6 (11.6) | 38.5 (12.8) | 0.038 |
| Cluster Presentations, No. (%) | 85 (19.1) | 47 (9.5) | 132 (14.0) | <0.001 |
| Encounter Length of Stay, median (IQR) | 2 (7) | 2 (7) | 2 (7) | 0.103 |
| Quarterly Length of Stay*, mean (SD) | 220.7 (88.3) | 151.3 (77.4) | 179.5 (87.7) | 0.025 |
| Positive Alcohol Screening, No. (%) | 109 (28.4) | 73 (17.8) | 182 (22.9) | <0.001 |
| Encounters Needing Blood Products, No. (%) | 109 (24.5) | 107 (21.6) | 216 (23.0) | 0.286 |
| Quarterly Units of Blood Transfused, mean (SD) | 184.2 (208.1) | 51.0 (35.8) | 105.1 (148.1) | 0.041 |
| Encounter Injury Severity Score, median (IQR) | 8 (9) | 10 (13) | 9 (15) | <0.001 |
| Mortality Rate, No. (%) | 60 (13.5) | 86 (17.3) | 146 (15.5) | 0.106 |
(*) Denotes windsorized variable used.
3.2. Healthcare utilization
The hospital-observed quarterly incidence of GSW encounters decreased by 22% post-policing changes, 44.3 to 34.6 (p = 0.038). Median encounter LOS remained the same; however, average quarterly days spent in-house for GSW treatment decreased afterwards by 31% (p = 0.025) (Table 1). Similarly, GSW encounter presentations observed a significant decrease in positive alcohol screenings, cluster presentations and quarterly units of blood products transfused. There was a decrease in encounters requiring blood product transfusion, although not significant (p = 0.286). ISS significantly increased (p < 0.001) and hospital-observed mortality rate slightly increased following the policing changes (p = 0.106) (Table 1).
3.3. Hospital mortality
The slight increase in hospital-observed mortality adheres to a significant increase in the rate of fatal ED dispositions (Table 1). Following the policing changes, the rate of fatal ED dispositions increased by nearly 80% from previous years (Table 1). A binary logistic regression model predicting mortality by area of GSW determined chest, head, and abdomen/pelvis as the most significant predictors of mortality (AUC: 0.801, sensitivity 0.747 & specificity 0.738; p < 0.001) (Table 2). Following policing changes, the percentage of ED presentations sustaining GSW of the chest significantly increased, while all other anatomical areas did not experience a significant change (Table 2).
Table 2.
GSW by Anatomical Location Before and After Policing Changes and Mortality Risk.
| Area of GSW | Before (n = 444) |
After (n = 496) |
p-value |
Entire Population |
Unadjusted OR (95% CI) |
|---|---|---|---|---|---|
| No. (%) | No. (%) | No. (%) | |||
| Head | 63 (14.2) | 75 (15.1) | 0.687 | 138 (14.7) | 5.4 (3.2–9.1) |
| Chest | 59 (13.3) | 120 (24.2) | <0.001 | 179 (19.0) | 7.1 (4.5–11.1) |
| Abdomen/Pelvis | 110 (24.8) | 134 (27.0) | 0.434 | 244 (26.0) | 2.6 (1.7–4.1) |
| Upper Back | 44 (9.9) | 68 (13.7) | 0.073 | 112 (11.9) | 1.3 (0.8–2.3) |
| Lower Back/Buttocks | 56 (12.6) | 66 (13.3) | 0.752 | 122 (13.0) | 0.6 (0.3–1.1) |
| Upper Extremity | 119 (26.8) | 140 (28.2) | 0.626 | 259 (27.6) | 1.0 (0.7–1.6) |
| Lower Extremity | 183 (41.2) | 174 (35.1) | 0.053 | 357 (38.0) | 0.7 (0.4–1.2) |
| Neck | 19 (4.3) | 29 (5.8) | 0.276 | 48 (5.1) | 1.2 (0.5–2.8) |
3.4. Healthcare costs
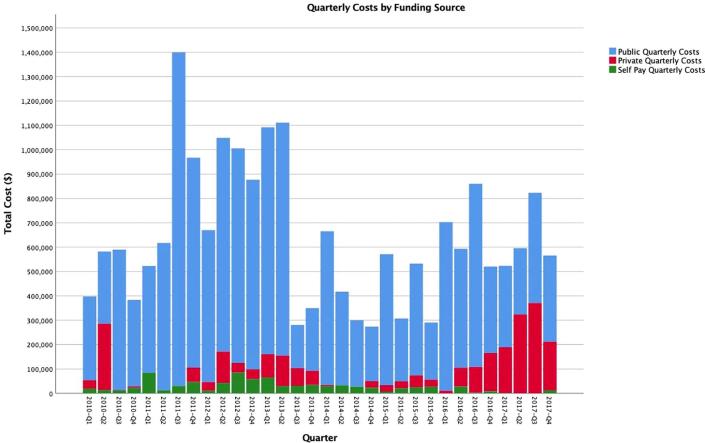
Over the eight-year study, $21.7 million in healthcare costs were generated for treating firearm injuries at Camden’s level-1 trauma center (Table 3). These costs were predominately billed to a form of public funding, with only a small percentage being billed to private insurance or self-pay (Fig. 1). Post-implementation of the new policing tactics, there was a significant decrease in hospital-observed quarterly costs for GSW treatment (Table 3). On average, hospital-observed total cost savings associated with the policing changes estimated $254,000 per quarter year, or $1 million annually (Table 3).
Table 3.
GSW Encounter Hospital Cost Characteristics Before and After Policing Changes.
| Before (n = 13) | After (n = 19) | Entire Population (n = 32) | p-value | |
|---|---|---|---|---|
| Direct Costs | ||||
| Quarterly, mean (SD)* | $ 436,009 ($186,650) | $ 281,676 ($112,341) | $ 344,374 ($163,537) | 0.016 |
| Total | $ 5,899,875 | $ 5,351,838 | $ 11,251,713 | |
| Indirect Costs | ||||
| Quarterly, mean (SD)* | $ 374,196 ($139,650) | $ 274,881 ($110,566) | $ 315,227 ($130,780) | 0.032 |
| Total | $ 5,235,784 | $ 5,222,731 | $ 10,458,515 | |
| Total Costs | ||||
| Quarterly, mean (SD)* | $ 810,205 ($321,984) | $ 556,556 ($219,280) | $ 659,601 ($289,950) | 0.023 |
| Total | $11,135,659 | $10,574,568 | $21,710,227 | |
| Public Costs | ||||
| Quarterly, mean (SD)* | $ 687,494 ($303,307) | $ 425,963 ($208,447) | $ 532,210 ($279,054) | 0.007 |
| Total | $ 9,920,262 | $ 8,093,289 | $ 18,013,551 | |
| Private Costs | ||||
| Quarterly, mean (SD)* | $ 54,881.09 ($76,253) | $ 97,488 ($107,512) | $ 80,179 ($97,027) | 0.228 |
| Total | $ 713,454.17 | $1,852,277.00 | $ 2,565,731 | |
| Uninsured Costs | ||||
| Quarterly, mean (SD)* | $ 38,611.04 ($27,127) | $ 17,864 ($12,831) | $ 26,292 ($22,082) | 0.021 |
| Total | $ 501,943.50 | $339,407.00 | $ 841,351 | |
(*)Denotes windsorized variable used.
Fig. 1.
Total Hospital Costs by Quarter Before and After Policing Changes.
4. Discussion
In efforts to alleviate the social and financial burden of violence experienced in Camden, NJ, the city underwent a series of radical policing modifications. On May 1st, 2013, the Camden City Police Department was disbanded after 141 years of service, leaving the Camden County Police Department (CCPD) as the city’s primary law enforcement body (Why and Camden, 2014). Accompanying this revision in leadership, an emphasis was placed on the joint efforts of community and technology driven policing. As defined by Trojanowicz, “Community policing is a new philosophy of policing, which emphasizes the working partnership between police officers and citizens in creative ways in order to solve community problems relating to crime, fear of crime and neighborhood disorders (Trojanowicz and Community, 1990).” In order to achieve this goal, the following tactics were implemented: increase in police officers (from 160 to over 400), an increase in officer foot patrol, body cameras on all patrol officers, implementation of ShotSpotter® audio technology, license plate detection database of all city-crossing vehicles, installment of 221 rotating cameras, a mobile observation platform spanning a 6-block radius (FLIR Systems Sky Patrol) and an anonymized Interactive Community Alert Network (iCan) (Wiig, 2018, Friedersdorf, 2013, Laday, 2013).
There is a dearth of literature focused on the efficacy of similar policing strategies on reducing gun violence. Popular public health attempts, such as the Cure Violence model, aim to minimize community violence through identifying individuals at risk of violent behavior and enrolling them into programs to change their behavioral tendencies (Butts et al., 2015). However, the efficacy ranges from moderate reductions in gun violence to contradictory increases in gun violence following implementation (Skogan, 2009, Webster et al., 2013, Picard-Fritsche and Cerniglia, 2013, Fox et al., 2015, Wilson et al., 2011). Increasing police patrol at “hot spots” has also shown success, reducing gun violence by 49% in studied Kansas City areas (Sherman and Rogan, 1995). New York City’s (NYC) increase in stop-and-frisk procedures led to a 29% reduction in gun crime and the lowest homicide total since the 1950s (Blumstein and Wallman, 2000, Equal Justice Initiative, 2018). Despite African-American and Latino populations representing only 50% of NYC’s population, these ethnicities accounted for 84% of all searches; 90% of which produced zero basis for summons or arrest (Judge, 2018). Inevitably, racial discrimination stemming from NY’s stop-and-frisk policy predisposed minority groups to mental health issues and was ruled unconstitutional in 2013 (Sewell et al., 2016, Judge, 2018). Seattle introduced similar surveillance technologies as Camden in 2013, although deactivated in 2018 due to constitutional concerns over resident rights (Kiley, 2018). To our knowledge, the efficacy of Seattle’s system on hospital-observed firearm injury was not reported.
Camden’s aggressive, new policing tactics led to multiple changes in GSW presentation characteristics. The hospital observed a significant decrease in the rate of intoxicated GSW encounters, cluster shootings and overall GSW incidence, treated in Camden’s level-1 trauma center. In areas equipped with integrated audio and visual capability, shootings decreased from 704 to 336 between 2013 and 2014 (Bereznak, 2015). ShotSpotter® detection technology – 35-microphones strategically placed across the city – alerts law enforcement of gunshots in real-time and is an integral aspect of the policing efforts in Camden (State of New Jersey, 2014). In 2006, a study by the National Institute of Justice revealed ShotSpotter® technology could detect 233 out of 234 (99.6%) gunshots within 40 feet, across 23 firing locations (Goode, 2012). In the absence of this technology, law enforcement is reliant on citizen reporting of gunfire. ShotSpotter® detection allowed the CCPD to discover that up to 38% of shootings went unreported and, when integrated with the other policing initiatives, decreased police response time from 9 min to 30 s (CBS News, 2015).
Contrary to the observed increase in fatal, firearm-related ED dispositions, the CCPD reported a 50% decrease in firearm-related homicides over a similar time period (2012–2017) (Dougherty, 2019). Due to enhanced gunfire identification and response, we theorize these conflicting reports reflect a shift in mortality declaration: from the scene to the ED. In attempt to reduce the delay in medical intervention, the CCPD implemented a “scoop and go” policy in November 2015. The policy requires police to drive gunshot victims to the ED themselves, bypassing the time otherwise spent waiting for EMT services (Goldstein, 2017). Similar policies implemented in Philadelphia, Pennsylvania, demonstrated that GSW victims transported by the police were more likely to expire due to the greater extent of their injuries than other penetrating wound victims (ie. stab-wound victims) (Band et al., 2014). Despite survival rates of 0–5% for last effort medical interventions (ie. thoracotomy), efficient detection and response allows more poor-prognosis GSW presentations to reach Camden’s, level-1 trauma center within the optimal 30-minute window (Branney et al., 1998, Stratton et al., 1998, Brown et al., 1996, Battistella et al., 1999, Frezza and Mezghebe, 1999). This underlying hypothesis, increase in encounters with patients who have a poor-prognosis, could also apply to the vast increase in hospital-observed ISS and encounters sustaining chest GSW(s) – significant influences on mortality – following the policing changes. Similarly, as more poor-prognosis, GSW encounters present to the ED, and subsequently expire shortly thereafter, there may be less demand for blood product transfusion as demonstrated in our results. Other potential hypotheses to explain the increase in mortality include changes in crime setting (from open to confined areas), increased accuracy of shooters and increased weapon technology. The absence of police reports and firearms used during these encounters is a limitation of this study. Without this information the increase in ED observed GSW mortality remains unknown.
Annually, the United States generates $2.8 billion in healthcare costs for firearm-related injuries (Spitzer et al., 2017). This figure, in addition to our reported costs, only captures the cost of initial hospitalization and services for GSW encounters. Studies have shown GSW readmission rates to be as high as 8% and associated costs for 30-day and 1-year GSW readmissions to be 3.8% and 9.0% of the initial ED encounter, respectfully (Rattan et al., 2018, Spitzer et al., 2017). The cost to implement the current CCPD policing system is estimated to be $4.5 million dollars (Laday, 2013). Through a reduction in firearm-related healthcare utilization, secondary to a decrease in the incidence of GSW encounters, our study found an annual healthcare savings of $1.0 million following the adoption of an encompassing policing system. The annual return on investment could recover the system implementation cost in about four and a half years. In areas susceptible to high rates of gun violence, the preventative cost to adopt a more effective policing infrastructure is far less than the healthcare costs of firearm injury.
Two patients with significantly greater hospital stays, and ensuing encounter costs, were winsorized to allow their inclusion, while limiting the potential effect on our study’s validity. Both extreme outliers belonged to the pre-policing changes cohort. The two hospitalizations were 592 and 201 days, requiring care from multiple surgical specialty services for their unique nature of injuries and subsequent complications. It is important to note, there is a strong possibility of major outliers within a large population. With this in mind, the authors decided to windsorize these values as opposed to completely omitting them or skewing the data if fully included. Our study continues to show the heavy financial burden of treating GSW, and the cost-savings associated with implementing an encompassing policing system, despite adjusting for outlier encounter influences.
One of the major limitations of this study includes the reliability of medical coding and trauma database accuracy. There is a potential for unintentional exclusion of patients who may have met criteria due to the possibility of patient ED presentation in an unidentified state, inaccurate ICD codes in the trauma database and/or misreported coding within the hospital informatics database. However, as our institution is required to have dedicated database manager for all traumas presenting to the trauma bay, we believe the database information is accurate. Our database is limited to hospital-specific information; therefore, variables such as clusters were determined based on hospital accessible information. We cannot accurately depict which encounters stem from the same incident and which did not. Additionally, GSW victims do not always make it into the hospital if they have been confirmed deceased at the scene of the crime. Without access to the police reports for included GSW encounters, the impact of these policing tactics are only from the perspective of the level-1 trauma center. As this institution is the only level-1 trauma center in Camden County, and neighboring counties, GSW encounters brought to the level-1 trauma center are not exclusive to the city of Camden. Similarly, patients could have sought medical care for low severity injuries at other healthcare institutions in the area which we could not capture. Due to the unique situation within the Camden community, our investigation’s data collection was limited to a single institution without a control group. Incidence reporting was adjusted for the city’s population; however, there still remains potential for confounders for incidence and other population-based outcomes. As such our results may represent a biased sample and possess limited generalizability. The inability to conduct alcohol screening for all GSW encounters is another minor limitation of this study.
Additionally, the Affordable Care Act and Medicaid expansion took effect in New Jersey during the study period. Effectively decreasing the number of self-pay individuals and increasing the number of public and privately insured individuals. We believe that using cost data rather than charge data, the influence of funding source was minimized. Lastly, costs are only for the initial encounter and do not capture readmissions, long term care, rehabilitative services, and other post-treatment costs. As we expect these costs to be high, we believe our study is a conservative estimate compared to the overall total cost these patients have on the healthcare system and society.
5. Conclusion
In conclusion, our study has demonstrated that a community and technology focused policing system, as implemented by the CCPD, could alleviate the burden of firearm-related injuries in similar communities and save millions in taxpayer dollars. This money could be reallocated towards programs that can continue to decrease firearm-related injuries. If other cities implement similar policing tactics, future multi-institutional studies are needed to determine the full economic impact these programs have in violence prone communities.
References
- Band R.A., Salhi R.A., Holena D.N., Powell E., Branas C.C., Carr B.G. Severity-adjusted mortality in trauma patients transported by police. Ann. Emerg. Med. 2014;63(5):608–614. doi: 10.1016/j.annemergmed.2013.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battistella F.D., Nugent W., Owings J.T., Anderson J.T. Field triage of the pulseless trauma patient. Arch. Surg. 1999;134(7):742–746. doi: 10.1001/archsurg.134.7.742. [DOI] [PubMed] [Google Scholar]
- Bereznak, A., Published August 19, 2015. High-tech policing: Do cities need Big Brother to lower crime? Yahoo! News. http://news.yahoo.com/the-effects-of-a-high-tech-police-force-in-one-of-america-s-most-dangerous-cities-152325047.html. (Accessed October 25, 2018).
- Blumstein A., Wallman J. Cambridge University Press; 2000. The Crime Drop in America. [Google Scholar]
- Branney S.W., Moore E.E., Feldhaus K.M., Wolfe R.E. Critical analysis of two decades of experience with postinjury emergency department thoracotomy in a regional trauma center. J. Trauma. 1998;45(1) doi: 10.1097/00005373-199807000-00019. [DOI] [PubMed] [Google Scholar]
- Brown S.E., Gomez G.A., Jacobson L.E., Scherer T., McMillan R.A. Penetrating chest trauma: should indications for emergency room thoracotomy be limited? Am. Surg. 1996;62(7):530–533. discussion 533-534. [PubMed] [Google Scholar]
- Butts J.A., Roman C.G., Bostwick L., Porter J.R. Cure violence: a public health model to reduce gun violence. Annu. Rev. Public Health. 2015;36(1):39–53. doi: 10.1146/annurev-publhealth-031914-122509. [DOI] [PubMed] [Google Scholar]
- CBS News, Published January 12, 2015. Crime-sensing microphones hear, locate gunshots. CBS News. https://www.cbsnews.com/news/crime-sensing-microphones-hear-locate-gunshots/. (Accessed October 25, 2018).
- Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS), 2005. https://webappa.cdc.gov/sasweb/ncipc/mortrate.html. (Accessed January 17, 2018).
- Dougherty, M., Published January 1, 2019. Camden police, residents credit building trust among community for 50-year crime low. KYW News Radio. https://kywnewsradio.radio.com/articles/news/camden-crime-50-year-low-police-and-residents-credit-community-relations-renewed-trust. (Accessed January 2, 2019).
- Equal Justice Initiative, Published January 19, 2018. Crime Falls As New York Abandons Stop-and-Frisk. Equal Justice Initiative. https://eji.org/news/new-york-crime-falls-as-police-end-stop-and-frisk. (Accessed October 26, 2018).
- Federal Bureau of Investigation. Uniform Crime Reporting – Offense Data by City Agency. Washington, D.C.: U.S. Department of Justice, 2011. https://ucr.fbi.gov/crime-in-the-u.s/2010/crime-in-the-u.s.-2010/offenses-known-to-law-enforcement/standard-links/city-agency.
- Fox A.M., Katz C.M., Choate D.E., Hedberg E.C. Evaluation of the Phoenix TRUCE project: A replication of Chicago cease fire. Justice Q. 2015;32(1):85–115. [Google Scholar]
- Frezza E.E., Mezghebe H. Is 30 minutes the golden period to perform emergency room thoratomy (ERT) in penetrating chest injuries? J. Cardiovasc. Surg. (Torino) 1999;40(1):147–151. [PubMed] [Google Scholar]
- Friedersdorf, C., Published December 12, 2013. The Surveillance City of Camden, New Jersey. https://www.theatlantic.com/national/archive/2013/12/the-surveillance-city-of-camden-new-jersey/282286/. (Accessed October 6, 2018).
- Gani F., Sakran J.V., Canner J.K. Emergency department visits for firearm-related injuries in the United States, 2006–14. Health Aff. 2017;36(10):1729–1738. doi: 10.1377/hlthaff.2017.0625. [DOI] [PubMed] [Google Scholar]
- Giffords Law Center, 2018. Annual Gun Law Scorecard. https://lawcenter.giffords.org/scorecard/. (Accessed October 1, 2018).
- Goldstein, J., Published April 2, 2017. Changing in Policing Take Hold in One of the Nation’s Most Dangerous Cities. The New York Times. https://www.nytimes.com/2017/04/02/nyregion/camden-nj-police-shootings.html. (Accessed July 13, 2019).
- Goode, E., Published May 28, 2012. Shots Heard, Pinpointed and Argued Over. The New York Times. https://www.nytimes.com/2012/05/29/us/shots-heard-pinpointed-and-argued-over.html. (Accessed October 25, 2018).
- Iglewicz B., Hoaglin D.C. ASQC Quality Press; 1993. How to Detect and Handle Outliers. [Google Scholar]
- Goldstein, J., Published October 19, 2018. Judge Rejects New York’s Stop-and-Frisk Policy. The New York Times. https://www.nytimes.com/2013/08/13/nyregion/stop-and-frisk-practice-violated-rights-judge-rules.html. (Accessed January 15, 2019).
- Kiley, B., Published February 10, 2018. Surveillance system or public-safety tool? Seattle dismantles controversial wireless mesh network | The Seattle Times. Seattle Times. https://www.seattletimes.com/seattle-news/surveillance-system-or-public-safety-tool-seattle-dismantles-controversial-wireless-mesh-network/. (Accessed October 26, 2018).
- Laday J., Published April 29, 2013. County police officially take over public safety in Camden. http://www.nj.com/camden/index.ssf/2013/04/county_police_officially_take.html. (Accessed October 6, 2018).
- Picard-Fritsche, S., Cerniglia, L., Center for Court Innovation (U.S.). Testing a Public Health Approach to Gun Violence: An Evaluation of Crown Heights Save Our Streets, a Replication of the Cure Violence Model. New York, N.Y.: Center for Court Innovation; 2013. http://www.courtinnovation.org/sites/default/files/documents/SOS_Evaluation.pdf. (Accessed October 26, 2018).
- Rattan R., Parreco J., Namias N., Pust G.D., Yeh D.D., Zakrison T.L. Hidden costs of hospitalization after firearm injury: national analysis of different hospital readmission. Ann. Surg. 2018;267(5):810. doi: 10.1097/SLA.0000000000002529. [DOI] [PubMed] [Google Scholar]
- Sewell A.A., Jefferson K.A., Lee H. Living under surveillance: gender, psychological distress, and stop-question-and-frisk policing in New York City. Soc. Sci. Med. 2016;159:1–13. doi: 10.1016/j.socscimed.2016.04.024. [DOI] [PubMed] [Google Scholar]
- Sherman L.W., Rogan D.P. Effects of gun seizures on gun violence: “Hot spots” patrol in Kansas city. Justice Q. 1995;12(4):673–693. [Google Scholar]
- Skogan W.G. Concern about crime and confidence in the police: reassurance or accountability? Police Q. 2009;12(3):301–318. [Google Scholar]
- Spitzer S.A., Staudenmayer K.L., Tennakoon L., Spain D.A., Weiser T.G. Costs and financial burden of initial hospitalizations for firearm injuries in the United States, 2006–2014. Am. J. Public Health. 2017;107(5):770–774. doi: 10.2105/AJPH.2017.303684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- State of New Jersey, Published 2014. Coming together for Camden. http://dspace.njstatelib.org:8080/xmlui/bitstream/handle/10929/44482/GovernorNewsroom20140924b.pdf?sequence=1&isAllowed=y. (Accessed October 25, 2018).
- Stratton S.J., Brickett K., Crammer T. Prehospital pulseless, unconscious penetrating trauma victims: field assessments associated with survival. J. Trauma. 1998;45(1):96–100. doi: 10.1097/00005373-199807000-00021. [DOI] [PubMed] [Google Scholar]
- Trojanowicz, R.C., Bucqueroux, B., Community Policing a Contemporary Perspective. Cincinnati, Ohio Anderson Pub. Co; 1990. https://trove.nla.gov.au/work/18062126. (Accessed October 30, 2018).
- Webster D.W., Whitehill J.M., Vernick J.S., Curriero F.C. Effects of Baltimore’s Safe streets program on gun violence: a replication of Chicago’s CeaseFire program. J. Urban Health. 2013;90(1):27–40. doi: 10.1007/s11524-012-9731-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maciag, M., Why Camden, N.J., the Murder Capital of the Country, Disbanded Its Police Force. http://www.governing.com/topics/public-justice-safety/gov-camden-disbands-police-force-for-new-department.html. Published June, 2014. (Accessed October 6, 2018).
- Wiig A. Secure the city, revitalize the zone: smart urbanization in Camden, New Jersey. Environ. Plann. C: Polit. Space. 2018;36(3):403–422. [Google Scholar]
- Wilson, J.M., Chermak, S., McGarrell, E.F., Community-Based Violence Prevention: An Assessment of Pittsburgh’s One Vision One Life Program. RAND Corporation; 2011:1-11. https://www.rand.org/pubs/monographs/MG947-1.html. (Accessed October 26, 2018).