Abstract
Background:
There is a continuing gap between the availability of cancer control empirically supported treatments (ESTs) to address psychological needs of cancer patients and their dissemination to and implementation by providers in the community. The Theory of Planned Behavior (TPB), with constructs of attitudes, subjective norms, perceived behavioral control, and intentions, is used to understand the pathways to and prediction of providers’ behavior, i.e., implementation of a cancer control EST and its provision to patients.
Purpose:
To prospectively test the TPB in predicting providers’ usage of a cancer-specific EST, the biobehavioral intervention (BBI).
Methods:
Providers (N=166) were trained. At training’s end, providers completed measures of attitudes, perceived behavioral control, and intentions to use the BBI, and their supervisors completed measures of attitudes operationalized as subjective norms. Providers were followed and 4 months later reported their usage of the BBI with patients in the last 2 months. Regression-based path analyses tested attitudes, perceived behavioral control, subjective norms, and intentions as predictors of BBI usage and for the possible effect of intentions as a mediator.
Results:
Provider’s BBI usage was high, delivered to 65.6% of patients. Providers’ attitudes toward the BBI (β=.006; 95% CI=.002-.010) and subjective norms (supervisors’ attitudes toward providers’ EST usage; β=.021; 95% CI=.007-.034) predicted usage. Intentions predicted usage in univariate analyses but was not a mediator for usage.
Conclusions:
Use of theory in implementation science can test and identify variables key to implementation success. Here, the TPB identified providers’ and supervisors’ attitudes as predictors of EST usage.
Keywords: Theory of Planned Behavior, dissemination, implementation, empirically supported treatments, biobehavioral intervention, cancer control
Introduction
Implementation science is an emerging field with few successful demonstrations of implementations of evidenced-based, health psychology treatments. Many implementation science frameworks and models exist (Moullin, Sabater-Hernández, Fernandez-Llimos, & Benrimoj, 2015; Nilsen, 2015), with the majority identifying the stakeholders to be enlisted (e.g., providers, patients) and describing the processes of implementation and markers for success [e.g., empirically supported treatment (EST) usage]. Alternatively, classical theories define constructs relevant to achieving change in markers and the processes by which their influences arise. The most successful of theories are those which have universally important constructs, articulate processes to achieve change, and have empirical support across contexts. The Theory of Planned Behavior (TPB; Ajzen, 1985, 1991; Fishbein & Ajzen, 1975) is one such example.
The TPB is one of the most influential theories of the prediction of deliberate human behavior. It is widely and successfully used to predict important clinical behaviors, such as medical providers’ actions to change the health behaviors of their patients (Godin, Bélanger-Gravel, Eccles, & Grimshaw, 2008). The TPB is made testable by its specification of measurable constructs and relationships among them. A central tenant is that the direct determinant of behavior is an individual’s intention to perform it (intentions). Further, there are three precursors to an individual’s intentions: attitudes, subjective norms, and perceived behavioral control. Attitudes are the individual’s positive or negative evaluation of the general attributes and consequences of performing the behavior. Subjective norms refer to the approval or disapproval of the behavior by significant others. An element of this normative component is descriptive norms (Fishbein & Ajzen, 2010), the perception of the significant others’ approval of the behavior (Manning, 2009; Rivis & Sheeran, 2003). Perceived behavioral control is the degree of an individual’s beliefs in his/her ability to perform the behavior. An element of perceived behavioral control is self-efficacy, the individual’s perceived ease or confidence to perform the behavior. In sum, the TPB defines constructs and pathways leading to engagement in a specific behavior. The TPB constructs of attitudes, subjective norms, perceived behavioral control, and intentions and its testable processes offer a theoretically rich and empirically based methodology for implementation science studies of psychological and behavioral processes influencing providers’ EST usage.
Importantly, there are several examples of use of TPB constructs to study behavior of health professionals (Eccles et al., 2006; Godin et al., 2008). Regarding attitudes, providers’ positive attitudes toward evidence-based practices have been associated with greater provision of evidence-based care (Aarons, Sommerfeld, & Walrath-Greene, 2009; Beidas et al., 2015; Nelson & Steele, 2007). Studies of perceived behavioral control find that mental health providers with greater self-efficacy to use a treatment also report higher levels of concurrent EST usage (David & Schiff, 2017) and 12 weeks later (Harned, Dimeff, Woodcock, & Contreras, 2013). By contrast, there is less study of providers’ subjective norms as a predictor of EST usage, although examples are available (e.g., Faulkner & Biddle, 2001; Millstein, 1996). Subjective norms could be operationalized, however, with data from the supervisor of a provider, as supervisors can shape the environment to either facilitate or limit EST usage (Aarons et al., 2012). Support for this perspective comes from data showing organizations with a supervisor both supportive and having positive attitudes toward a provider using evidence-based practices actually aids in the provider’s subsequent usage during implementation (Aarons, 2006; Aarons, Wells, Zagursky, Fettes, & Palinkas, 2009; Becker-Haimes et al., 2017; Corrigan, Steiner, McCracken, Blaser, & Barr, 2001).
All the above constructs can be direct predictors of behavior, but the TPB posits their role to occur via intentions—the direct precursor to behavior (Eccles et al., 2006; Godin et al., 2008). For example, fostering greater intentions to implement evidence-based practices through a TPB-guided dissemination education resulted in a 22-32% increase in mental health providers reported usage compared to non-TPB-guided education (Casper, 2007, 2008). Fundamentally, studies of TPB-related components illustrate how theory can be leveraged to guide efforts to achieve implementation success. Yet, test of a single TBP construct provide early confirmatory support but are limited in illuminating the processes (and their reliability) of a complex behavior such as providers’ EST usage. For instance, studies have shown conflicting results with non-significant relationships between EST attitudes and usage when other TPB-related components were not evaluated (e.g., Gray, Elhai, & Schmidt, 2007). As such, study of the collective role of multiple TPB components would yield a more rigorous and informative test for EST usage than studying any one construct alone.
Thus, the present study is a demonstration of a health psychology EST implementation that used the key TPB constructs to test, and thus identify, which of these variables might be most important to implementation success. Specifically, we studied EST implementation of a psychological EST for cancer patients, the Biobehavioral Intervention (BBI). The manualized BBI is theoretically based (Andersen, Kiecolt-Glaser, & Glaser, 1994) and intervenes at multiple levels (e.g., health behaviors, social support, problem solving; see Andersen et al., 2004 for treatment detail). The BBI has robust empirical support demonstrating improvements in psychological, behavioral, and health outcomes in cancer patients (Andersen et al., 2004; Andersen et al., 2010; Andersen et al., 2008). To test the TPB constructs, they were measured prior to any BBI usage, the behavioral outcome of interest.
To do this, the BBI was disseminated to community providers during 3-day training institutes. Early data showed that institutes were effective in fostering positive attitudes towards ESTs in providers (N=62; Brothers et al., 2015). Further, providers’ positive attitudes towards the BBI and high levels of perceived behavioral control predicted greater intention to use the BBI when they returned to their organization. Building on these results, these TPB constructs, with the addition of subjective norm measures from provider’s supervisors, were tested to predict providers’ (N=166) behavior—BBI usage—4 months later. The TPB antecedents were tested as predictors of BBI usage, and intention was tested as a mediator of the effects of attitudes, subjective norms, and perceived behavioral control on BBI usage.
Methods
Participants
Providers.
Oncology mental health providers (N=166) were studied from 117 different settings. The group was predominantly female (n=150; 90.4%), middle-aged (M=42.5 years ± 10.4; range=25-67), and Caucasian (n=136; 82.0%). Providers were employed full time at in the following settings: academic medical centers or Veterans Administration Hospitals (n=68; 41.0%), community hospitals/centers (n=62; 37.3%), community supportive care facilities (n=15; 9.0%), private practice (n=8; 4.8%), and others (n=13; 7.8%). Providers came from 35 US states, Puerto Rico, and five foreign countries (Brazil, Israel, Kenya, Malaysia, and Mexico). The majority were licensed (n=146; 88.0%) and had been so for an average of 12.5 years (SD=9.2; range=0-36). Providers’ disciplines were social work (n=69; 41.6%), clinical psychology (n=65; 39.2%), clinical psychology post-doctoral fellows (n=9; 5.4%), nursing (n=4; 2.4%), or other disciplines (n=19; 11.4%). Providers had been employed an average of 5.8 years (SD=6.2; range=0-30) in their current position, spending most of their time providing clinical services (71.4% ± 24.8; range=0-100%).
Supervisors.
The supervisor of each provider was solicited to participate in the study. In the case of the attendance of multiple providers from the same setting with the same supervisor, participation of the supervisor was only solicited once (for the first provider). Thus, requests were made to 147 different supervisors. Of those, 106 supervisors responded (72.1%) and provided supporting data for 123 providers (74.1%). Their disciplines were mental health (n=51; 48.1%), medicine (n=36; 34.0%), or business/administration (n=19, 17.9%).
Procedures
BBI training institutes have been previously described (Brothers et al., 2015). Briefly, announcements of and instructions to apply to a training institute were placed on relevant listservs (e.g., American Psychosocial Oncology Society) and a website (www.Cancer2Health.osu.edu). Applications were sought from licensed mental health providers employed full-time in clinical service provision to cancer patients. The application process informed individuals of the NIH funding of the institute, the research participation requirement, and the reimbursement of expenses. In addition to an application and resume, a letter of support from the individual’s clinical or administrative supervisor (i.e., the person who could authorize BBI implementation at the institution) and the supervisors’ contact information were required. Applicants were screened for eligibility and fit. Those selected attended one of six 3-day (18 hours) BBI training institutes conducted from 2011-2016 at the Ohio State University led by six clinical psychologist BBI experts. Prior to attending, providers completed an assessment via the website. Paper/pencil assessments in subject coded packets were completed during the institute with only program staff, and not trainers, present. Providers detailed BBI usage online (using Qualtrics) 4 months after completing training. $15 gift card was provided for reporting usage.
Approximately one month after training, the supervisor was informed of the provider’s completion of the training and asked to participate in the research. If multiple trainees from the same setting attended, the supervisor’s participation was solicited once for the first trainee attending. On Qualtrics, supervisors completed the subjective norm measures described below and each received a $5 gift card for participation.
Measures
Attitudes.
Two provider measures were used. 1) The Evidence-Based Practice Attitudes Scale (EBPAS; Aarons, 2004) assessed attitudes, in general, towards evidence-based practices and were operationalized as attitudes towards EST. The EBPAS consists of 15 items (e.g., “I am willing to try new types of therapy/interventions even if I have to follow a treatment manual”) and are scored on a 5-point Likert Scale (0 = “not at all” to 4 = “to a very great extent”). Items were summed for a total score ranging from 0-60 with higher scores indicating more positive attitudes. Internal consistency reliability was α=.757. 2) The classic strategy to assess attitudes (Osgood, 1957) was used to determine BBI-specific attitudes. A 30-item semantic differential scale had 30 pairs of bipolar adjectives descriptive of the BBI intervention and assessed the dimensions of evaluation (e.g., worthless/valuable), potency (e.g., complex/simple), and activity (e.g., dull/stimulating). A 7-point Likert scale (e.g., −3 = “worthless” to +3 = “valuable”) was used. Items were summed for a possible range of −90 to +90 with negative scores corresponding to more negative attitudes and positive scores representing positive attitudes. Internal consistency reliability was α=.885.
Subjective Norms.
Two supervisor measures were used. 1) The EBPAS (Aarons, 2004) as described above assessed general attitudes toward evidence-based practice, adapted to assess supervisor attitudes (e.g., the item, “I like to use new types of therapy/interventions to help my clients” was revised to read, “I like for the trainee to use new types of therapy/interventions to help his/her clients”). An item that did not apply to supervisors was omitted, leaving 14 items scored. Each item was rated on a 5-point Likert scale (0 = “not at all” to 4 = “to a very great extent”) and summed for a total score ranging from 0-56. Internal consistency reliability was α=.834. 2) Supervisors also rated the perceived ratio of costs/benefits of BBI implementation at their institution by his/her provider on a visual analogue scale with anchors of 0 (“The challenges will always outweigh the benefits”) to 100 (“The benefits will always outweigh the challenges”). Scores above the midpoint indicated belief that the benefits outweighed the challenges of BBI implementation.
Perceived Behavioral Control.
Two provider measures were used. 1) The Counselor Activity Self-Efficacy Scale consists of 25 items assessing general self-efficacy of basic (e.g., performing helping skills) and advanced (e.g., handling challenging counseling situations) counseling skills (Lent, Hill, & Hoffman, 2003). Items were scored on a 10-point Likert scale (0 = “not at all confident” to 9 = “totally confident”) and summed for a total score ranging from 0-225 with higher scores indicating greater general counseling self-efficacy. Internal consistency reliability was α=.952. 2) The BBI-specific self-efficacy consists of 8-items used to assess providers’ confidence with delivering general treatment strategies that were included in the BBI (e.g., progressive muscle relaxation, problem solving). Items were rated on a 10-point Likert scale (0 = “not at all confident” to 9 = “totally confident”) and were summed for a total score ranging from 0-72 with higher scores indicating greater self-efficacy to deliver the BBI. Internal consistency reliability was α=.849.
Intentions.
Ten items assessed providers’ intentions to use each of 10 BBI components (e.g., In the next two 2 months, I intend to use assertive communication) using a 5-point Likert scale for each item (0 = “never” to 4 = “always”). Items were summed for a total score ranging from 0-40 with higher scores indicating greater intentions. Internal consistency reliability was α=.869.
Behavior.
Providers reported their delivery of the BBI to patients at 4 months. Using Qualtrics logs, each provider reported 1) the total number of adult cancer patients treated in the past two months, and 2) the total number of adult cancer patients treated with the BBI in the past two months. As noted above, providers spent most of their time in service provision. Thus, we anticipated that they could, in most cases, readily report the number of patients treated, corresponding to billing hours for many. BBI usage was defined as the percentage of each provider’s patients treated with the BBI out of the total number of patients treated in the past two months. Preliminary data were obtained at 2 months to familiarize providers with reporting procedures. The correlation between 2- and 4-month usage was ρ=0.587 (p<01).
Analytical Plan
Preliminary Analyses.
Descriptive statistics were performed on all provider characteristics, TPB constructs (attitudes, subjective norms, perceived behavioral control, and intentions) as operationalized, and BBI usage. Spearman’s correlations were completed to examine the relationship between TPB components and BBI usage at 4 months. For missing usage data, post-hoc one-way analysis of variances (ANOVAs) using 5,000 bootstrap samples tested differences in TPB constructs (attitudes, subjective norms, perceived behavioral control, and intentions) as well as provider (percent of psychologists) and setting characteristics (percent employed at academic medical centers or Veterans Administration Hospitals) between providers reporting and not reporting usage data.
Primary Analyses.
To test the Theory of Planned Behavior, there were three elements. First, attitudes, subjective norms, and perceived behavioral control were tested as predictors of intentions. Linear regression analyses for each predictor (attitudes, subjective norms, and perceived behavioral control) were used. A final model with all TPB constructs included was estimated to predict intentions. Second, the TPB constructs were tested as predictors of BBI usage at 4 months. Structural equation models with a robust maximum likelihood estimation for each predictor were used. Specifically, robust standard errors were computed using the Huber-White method (Huber, 1967; White, 1982) with test statistic correction using Yuan-Bentler scaled test statistic (Yuan & Bentler, 2000) to handle non-normal data. Case-wise maximum likelihood estimation was used during the model fitting for instances of missing data. As providers were nested within institutes, institute attended was entered as a covariate for all models. A final model with all TPB constructs included was estimated to predict usage.
And third, a regression-based path analysis tested intentions as a mediator between attitudes, subjective norms, and perceived behavioral control, and usage (Hayes, 2013). Direct, indirect, and total effects of the predictors were estimated using the robust maximum likelihood estimation. A bootstrap analysis using 5,000 bootstrap samples accounted for the violations of normality assumptions when estimating total and indirect effects (MacKinnon, Lockwood, & Williams, 2004). Institute attended was also entered as a covariate. The final mediation models were estimated using all TPB constructs included. All analyses were conducted using R version 3.4.0.
Results
Preliminary
Of the 166 providers, thirty-nine (23.5%) did not report usage while 13 providers (7.8%) reported not having an opportunity to use the BBI (i.e., left the institution; needed more time to implement; medical leave). Post-hoc one-way ANOVAs found no difference in attitudes, subjective norms, perceived behavioral control, intentions, provider characteristics, and setting characteristics (ps>.263) between providers reporting usage data (n=114) and providers without usage data (n=52).
Provider- and supervisor-reported variables and correlations are provided in Table 1. At the end of the training institute, providers reported high positive attitudes, perceived behavioral control, and intentions when values are compared to the possible range of scores. Providers, on average, reported using the BBI with roughly two-thirds of their patients at 4 months (M=65.6% ± 33.9; median = 71.4%; interquartile range = 38.0-100.0%). Providers’ attitudes [EBT-general attitudes (ρ=.230) and BBI-specific attitudes (ρ=.404)], perceived behavioral control [EST-general self-efficacy (ρ=.196) and BBI-specific self-efficacy (ρ=.282)] were positively correlated with intention to use BBI (ps<05). Moreover, providers’ attitudes [EST-general (ρ=.268) and BBI-specific (ρ=.242)], subjective norms [supervisor EST-general attitudes (ρ=.242)], perceived behavioral control [EBT-general (ρ=.228)], and intentions (ρ=.216) were positively correlated with reported BBI usage (ps<05).
Table 1.
Summary of observed means and ranges of provider (N=166) and supervisor (N=106) measures of the Theory of Planned Behavior constructs and their intercorrelations.
| Measure | Mean ± SD | Observed Range | Range | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Attitudes | 1 EST-general attitudes | 48.2 ± 6.2 | 29-60 | 0-60 | 1 | |||||||
| 2 BBI-specific attitudes | 58.9 ± 15.3 | 4-86 | −90 +90 | .329** | 1 | |||||||
| Subjective Norms | 3 Supervisors’ EST-general attitudes | 42.8 ± 5.7 | 29-54 | 0-56 | .143 | −.067 | 1 | |||||
| 4 Supervisors’ implementation challenges vs. benefits | 71.7 ± 18.9 | 2-100 | 0-100 | .078 | .111 | .408** | 1 | |||||
| PBC | 5 EST-general self-efficacy | 198.2 ± 18.0 | 125-225 | 0-225 | .214* | .293** | <.001 | .099 | 1 | |||
| 6 BBI-specific self-efficacy | 63.3 ± 6.5 | 40-72 | 0-72 | .230** | .150 | −.066 | .146 | .791** | 1 | |||
| Intent | 7 Intentions to use BBI | 31.3 ± 4.9 | 19-40 | 0-40 | .230** | .404** | −.051 | .056 | .196* | .282** | 1 | |
| Usage | 8 Usage at 4 months | 65.6% ± 33.9 | 0-100% | 0-100% | .268* | .242* | .242* | .045 | .228* | .168 | .216* | 1 |
Note: BBI=biobehavioral intervention; EST=empirically supported treatment; PBC=perceived behavioral control;
p<.05;
p<.01.
Primary Analyses
Prediction of Intention.
Linear regressions examined predictors of intentions, controlling for institute attended. Providers’ positive attitudes [EST-general attitudes: β=.217, t(127)=3.174, p=.002; BBI-specific attitudes: β=. 138, t(155)=5.646, p<001] and greater perceived behavioral control [EST-general self-efficacy: β=.063, t(128)=2.179, p=.007; BBI-specific self-efficacy: β=.222, t(128)=3.506, p<.001] predicted greater intention to use BBI. No other measures were significant in predicting intentions alone (ps>.605). All predictors of intentions were entered into a final model that explained 25.3% of the variance of intentions [F(10,75)=2.543, p=.011]. In the final model, only positive attitudes [BBI-specific attitudes: β=.094, t(75)=2.496, p=.015] predicted greater intentions to use the BBI.
Prediction of Usage.
Structural equation models revealed providers’ attitudes [EST-general (β=.017, z=2.842, p=.004); BBI-specific (β=.007, z=3.574, p<.001)] predicted usage. Also, positive subjective norms [supervisor EST-general attitudes (β=.018, z=2.955, p=.003)] and positive intentions (β=.014, z=2.227, p=.026) also predicted BBI usage. No other measures were significant in predicting usage alone (ps>.071). All predictors were entered into a final model, explaining 35.3% of the variance in usage. In the final model, more positive attitudes [BBI-specific attitudes (β=.006, z=2.807, p=.005)] and subjective norms [supervisor EST-general attitudes (β=.021, z=3.301, p=.001)] predicted usage. Intentions did not predict usage (p=.679).
Intentions as a Mediator of Usage.
A structural equation model tested intention as a mediator of usage with attitudes (EBT-general and BBI-specific attitudes), subjective norms (EBT-general attitudes of supervisors), and perceived behavioral control (BBI-specific self-efficacy), controlling for institute attended. The full TPB test explained 25.5% of the variance of intentions and 35.2% of the variance of BBI usage (see Figure 1).
Figure 1.
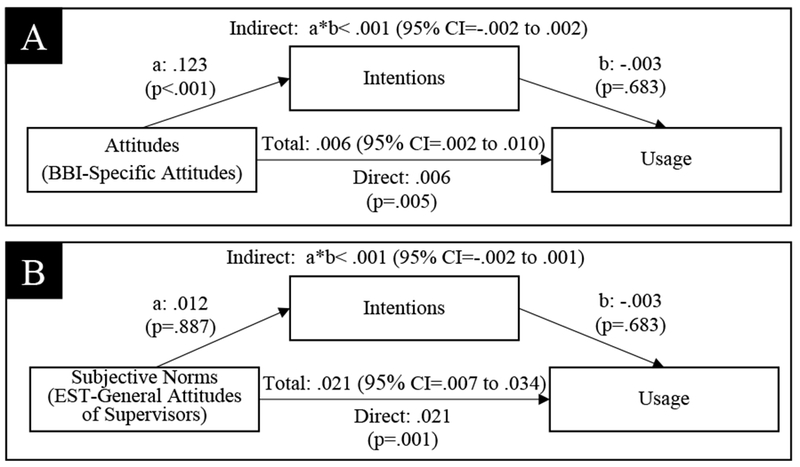
Regression coefficients for the significant relationships between the TPB constructs [(A: attitudes (BBI-specific attitudes) and B: subjective norms (EST-general attitudes of supervisors)] and BBI usage at 4 months as mediated by intentions. The other TPB variables and institute attended were controlled for in the model. Note: TPB=Theory of Planned Behavior; BBI=biobehavioral intervention; EST=empirically supported treatment.
In the full model with all TPB constructs included, attitudes (BBI-specific attitudes; p=.006) and subjective norms (supervisor EST-general attitudes; p=.001) were direct predictors of usage. Contrary to the TPB, intentions neither mediated the effects of the other TPB constructs on usage, nor was it a significant predictor of usage (p=.683). The total effects (i.e., incorporating both direct and indirect effects through intentions on usage) of attitudes [BBI-specific attitudes (β=.006; 95% CI = .002 to .010)] and supervisor [supervisor EST-general attitudes (β=.021; 95% CI = .007 to .034)] were significant in predicting usage.
Discussion
This present study provided a “full” test of the TPB to predict providers’ EST usage with its inclusion of all key TPB constructs and their assessment occurring prior to the measurement of the behavioral outcome. Contributing to implementation science, the high rates of usage provided circumstances for an adequate test of the TPB with a diverse sample of providers, supervisors, and settings from which they came. Data showed that more positive attitudes predicted intentions, the theorized direct antecedent to behavior. Attitudes and subjective norms were significant predictors of EST usage and intentions did not mediate these relationships to usage.
Theories with measurable psychological constructs such as the TPB can guide and evaluate implementation practices by identifying the specific variables that predict EST usage. For this health psychology EST, the TPB identified the predictors of usage, namely positive attitudes of the providers and positive subjective norms assessed through their supervisors. Identifying these predictors has been a difficult task in much of the implementation studies as there are few prospective designs and of them, observed usage rates have been low. Health psychology implementation efforts have not been exempt from this dilemma. For example, a Center for Disease Control and Prevention initiative provided training on 18 HIV/AIDS risk-reduction interventions to over 12,000 providers. During the 6 months since dissemination, each setting offered the intervention to an average of 4 patient groups (Collins et al., 2010; Kelly et al., 2000). Indeed, another national dissemination effort of an EST to reduce risk of cardiovascular disease in women found half of the 85 trained leaders continuing to use the EST one year later (Folta et al., 2015).
In this study, providers’ attitudes towards the BBI was a significant predictor of both intentions and usage—supporting the importance of providers’ attitudes in influencing later EST usage (Aarons & Sawitzky, 2006; Beidas et al., 2015; Nelson & Steele, 2007). Interestingly, perceived behavioral control predicted intentions when examined alone, but did not significantly influence usage in contrast to prior findings (David & Schiff, 2017). Instead, we identified the importance of having an organizational culture supportive of EST usage as reflected through supervisors’ positive attitudes towards ESTs (subjective norms). Although subjective norms did not predict intentions, its positive association with future EST usage highlights the importance of the providers’ social environment that may influence EST usage. Indeed, the lack of organizational and leadership support are limiting factors for implementation (Aarons, 2006). These data underscore the need for supervisors and leadership within the organization to support EST usage by the providers (Corrigan et al., 2001).
Providers’ intentions predicted usage when examined alone, but intentions did not significantly predict usage when covarying other TPB constructs as operationalized. In considering this finding, we note that the reported intentions scores (M=31.3 ± 4.9; range=19.0-40.0) were quite high, which may have limited the variance to detect an effect. Additionally, TPB components, including intentions, are less predictive of behavior performed further into the future (McEachan, Conner, Taylor, & Lawton, 2011). Not surprisingly, intentions may change with time and intervening circumstances relevant to performing the behavior (see Ajzen, 1991; Cooke & Sheeran, 2004; Sniehotta, 2009). Here, intentions were assessed and then EST usage was reported 4-months later. Though attitudes toward the BBI were positive and influential, intentions can waiver as providers returned to their organization and encounter the real-life barriers of implementing an EST (Williams, Brothers, Ryba, & Andersen, 2015). Additionally, intentions’ effect on usage may have been attenuated by the intercorrelation between intentions and other TPB constructs. For instance, intentions was significantly correlated with both usage (ρ=.216) and BBI-specific attitudes (ρ=.404; See Table 1). Thus, a low parameter estimate is not evidence that intentions are of no consequence in predicting usage (Fishbein & Ajzen, 2010). Indeed, data show intentions to be a reliable predictor of behavior in many contexts/studies (Eccles et al., 2006; Godin et al., 2008; Sheeran, 2002).
The analyses tested for the direct effects of attitudes, subjective norms, and perceived behavioral control on usage, as has been done previously in implementation science (e.g., Beidas et al., 2015; David & Schiff, 2017; Faulkner & Biddle, 2001). As specified, the model explained significant variance in usage (35.3%). Regardless of intentions being a mediator here, the practical implications of the findings are consistent with the TPB (Fishbein & Ajzen, 2010), i.e., changes to upstream TPB constructs (e.g., providers’ attitudes) could ultimately lead to greater EST usage.
The construct of subjective norms was operationalized with supervisors’ EST attitudes to assess their approval or disapproval of providers’ choice of using the BBI. Although subjective norms are thought to be injunctive norms (i.e., what providers perceive as acceptable behavior of significant others), descriptive norms (i.e., what the significant others perceive as acceptable behavior; Rivis & Sheeran, 2003) were used. Fishbein and Ajzen (2010) suggest that descriptive norms are relevant to the normative construct of the TPB as they may reflect the organization’s social environment that can influence behavior (Rivis & Sheeran, 2003). As injunctive norms influence behavior in other contexts (Manning, 2009), measuring injunctive and descriptive norms may be optimal for future studies (Rhodes & Courneya, 2003).
According to the TPB, change in TPB constructs could influence behavior such as EST usage. As the BBI training institute was successful in improving providers’ attitudes towards ESTs (Brothers et al., 2015), the assessments of TPB constructs completed after training are used. Other measures were not measured prior to the institute as they would have resulting in random responding and/or measurement error (e.g., prior to the training institute, providers and supervisors had minimal, if any, knowledge of BBI to form attitudes about it). However, it might be inferred that some type of change had occurred based on providers having positive BBI attitudes—not negative or neutral—following training. Thus, it would seem that the TPB hypothesis to consider change in a construct was conceptually met with the measurement model used here.
Limitations of the study are considered. This study was prefaced by a dissemination phase which yielded positive attitudes, high levels of perceived behavioral control, and high intentions to use the BBI, grounded by gains in BBI knowledge and clinical skills (Brothers et al., 2015). These data document the broad success of the dissemination education, yet the restricted variance of these scores may have limited the examination of their effect on usage. It was impressive that the majority of the providers’ supervisors participated (72.1%), but it is unknown if the data from the remainder would have affected the results. Thirty-nine providers (23.5%) did not report usage. The observed number of non-reporting providers highlights the need for procedures to document the circumstances for non-implementation from each individual. This is particularly important when studying implementation which is not “system-wide” (Karlin et al., 2010; Ruzek, Karlin, & Zeiss, 2012). For this study, settings ranged from large, university-affiliated medical centers to individual therapy practices. The reliability of the usage reports from 2 and 4 month was ρ=0.587 (p<01), an estimate that might be considered adequate but also one suggesting some degree of error. Although usage was self-reported and may be subjected to response bias, no differences were found in characteristics between reporting and non-reporting providers. Strengths included a repeated measures design, beginning at dissemination through to implementation. Additionally, this study assessed actual usage, i.e., a head count of patients treated. Usually, implementation outcomes are proxy to actual EST usage (e.g., number of providers/settings using the EST, provider knowledge of the EST, supervisor feedback on implementation) to gauge implementation (see Forsetlund et al., 2009; McHugh & Barlow, 2010). Additional data that could supplement usage are providers’ description of the EST components actually used (i.e., fidelity and adaptation). The measures of the remaining TPB constructs were common to TPB research and implementation of EST usage more generally (Godin et al., 2008). Lastly, the geographic, setting, and professional diversity of the provider and supervisor samples enhanced the generalizability of the findings.
In summary, attitudes (providers’ BBI-specific attitudes) and subjective norms (supervisors’ EST-general attitudes) measured during dissemination predicted providers’ EST usage months later with their effects not mediated by intentions. This is one of the few examples in health psychology of using the TPB in a longitudinal design to identify predictors of EST implementation. The ease of self-report measures of TPB constructs facilitates its application in health psychology and provides a methodology for understanding the processes of EST usage. The findings reveal that dissemination which instills positive attitudes among providers and their supervisors about ESTs appeared to be keys to achieve greater usage of the EST.
Acknowledgements:
We thank the National Institutes of Health for support (R25E CA163197), Cancer to Health (C2H; 2011-2016) Institute educators (Kristen Carpenter, Georita Frierson, Rebecca Shelby, Lisa Thornton), Stress and Immunity Cancer Projects staff and graduate students, and the oncology mental health providers and their supervisors for their expertise and participation.
Funding Source: National Institutes of Health/National Cancer Institute R25E CA163917, K05 CA098133.
Footnotes
Human Rights: This study was approved by the IRB at Ohio State University. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent: Informed consent was obtained from all individual participants included in the study.
Welfare of Animals: This article does not contain any studies with animals performed by any of the authors.
Conflicts of Interest: Stephen B. Lo, Marlena M. Ryba, Brittany M. Brothers, and Barbara L. Andersen declare that they have no conflicts of interest.
References
- Aarons GA (2004). Mental health provider attitudes toward adoption of evidence-based practice: The evidence-based practice attitude scale (EBPAS). Mental Health Services Research, 6(2), 61–74. doi: 10.1023/b:mhsr.0000024351.12294.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA (2006). Transformational and transactional leadership: Association with attitudes toward evidence-based practice. Psychiatric Services, 57(8), 1162–1169. doi: 10.1176/ps.2006.57.8.1162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Glisson C, Green PD, Hoagwood K, Kelleher KJ, & Landsverk JA (2012). The organizational social context of mental health services and clinician attitudes toward evidence-based practice: A united states national study. Implementation Science, 7(1), 56. doi: 10.1186/1748-5908-7-56 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, & Sawitzky AC (2006). Organizational culture and climate and mental health provider attitudes toward evidence-based practice. Psychological Services, 5(1), 61–72. doi: 10.1037/1541-1559.3.1.61 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Sommerfeld DH, & Walrath-Greene CM (2009). Evidence-based practice implementation: The impact of public versus private sector organization type on organizational support, provider attitudes, and adoption of evidence-based practice. Implementation Science, 4, 83. doi: 10.1186/1748-5908-4-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aarons GA, Wells RS, Zagursky K, Fettes DL, & Palinkas LA (2009). Implementing evidence-based practice in community mental health agencies: A multiple stakeholder analysis. American Journal of Public Health, 99(11), 2087–2095. doi: 10.2105/ajph.2009.161711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajzen I (1985). From intentions to actions: A theory of planned behavior In Kuhl J & Beckmann J (Eds.), Action control: From cognition to behavior (pp. 11–39). Berlin, Heidelberg: Springer Berlin Heidelberg. [Google Scholar]
- Ajzen I (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211. doi: 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- Andersen BL, Farrar WB, Golden-Kreutz DM, Glaser R, Emery CF, Crespin TR, … Carson WE 3rd. (2004). Psychological, behavioral, and immune changes after a psychological intervention: A clinical trial. Journal of Clinical Oncology, 22(17), 3570–3580. doi: 10.1200/jco.2004.06.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, Kiecolt-Glaser JK, & Glaser R (1994). A biobehavioral model of cancer stress and disease course. American Psychologist, 49(5), 389–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, Thornton LM, Shapiro CL, Farrar WB, Mundy BL, Yang H-C, & Carson WE (2010). Biobehavioral, immune, and health benefits following recurrence for psychological intervention participants. Clinical Cancer Research, 16(12), 3270–3278. doi: 10.1158/1078-0432.ccr-10-0278 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andersen BL, Yang H-C, Farrar WB, Golden-Kreutz DM, Emery CF, Thornton LM, … Carson WE. (2008). Psychologic intervention improves survival for breast cancer patients. Cancer, 113(12), 3450–3458. doi: 10.1002/cncr.23969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker-Haimes EM, Okamura KH, Wolk CB, Rubin R, Evans AC, & Beidas RS (2017). Predictors of clinician use of exposure therapy in community mental health settings. Journal of Anxiety Disorders, 49(Supplement C), 88–94. doi: 10.1016/j.janxdis.2017.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beidas RS, Marcus S, Aarons GA, Hoagwood KE, Schoenwald S, Evans AC, … Mandell DS. (2015). Predictors of community therapists’ use of therapy techniques in a large public mental health system. JAMA Pediatrics, 169(4), 374–382. doi: 10.1001/jamapediatrics.2014.3736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brothers BM, Carpenter KM, Shelby RA, Thornton LM, Frierson GM, Patterson KL, & Andersen BL (2015). Dissemination of an evidence-based treatment for cancer patients: Training is the necessary first step. Translational Behavioral Medicine, 5(1), 103–112. doi: 10.1007/s13142-014-0273-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casper ES (2007). The theory of planned behavior applied to continuing education for mental health professionals. Psychiatric Services, 58(10), 1324–1329. doi: 10.1176/ps.2007.58.10.1324 [DOI] [PubMed] [Google Scholar]
- Casper ES (2008). Using implementation intentions to teach practitioners: Changing practice behaviors via continuing education. Psychiatric Services, 59(7), 747–752. doi: 10.1176/ps.2008.59.7.747 [DOI] [PubMed] [Google Scholar]
- Collins CB, Hearn KD, Whittier DN, Freeman A, Stallworth JD, & Phields M (2010). Implementing packaged hiv-prevention interventions for hiv-positive individuals: Considerations for clinic-based and community-based interventions. Public Health Reports, 125(Supplement 1), 55–63. doi: 10.1177/00333549101250S108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooke R, & Sheeran P (2004). Moderation of cognition-intention and cognition-behaviour relations: A meta-analysis of properties of variables from the theory of planned behaviour. British Journal of Social Psychology, 43(2), 159–186. doi: 10.1348/0144666041501688 [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Steiner L, McCracken SG, Blaser B, & Barr M (2001). Strategies for disseminating evidence-based practices to staff who treat people with serious mental illness. Psychiatric Services, 52(12), 1598–1606. doi: 10.1176/appi.ps.52.12.1598 [DOI] [PubMed] [Google Scholar]
- David P, & Schiff M. (2017). Self-efficacy as a mediator in bottom-up dissemination of a research-supported intervention for young, traumatized children and their families. Journal of Evidence-Informed Social Work, 14(2), 53–69. doi: 10.1080/23761407.2017.1298072 [DOI] [PubMed] [Google Scholar]
- Eccles MP, Hrisos S, Francis J, Kaner EF, Dickinson HO, Beyer F, & Johnston M (2006). Do self- reported intentions predict clinicians’ behaviour: A systematic review. Implementation Science, 1(1), 28. doi: 10.1186/1748-5908-1-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faulkner G, & Biddle S. (2001). Predicting physical activity promotion in health care settings. American Journal of Health Promotion, 16(2), 98–106. doi: 10.4278/0890-1171-16.2.98 [DOI] [PubMed] [Google Scholar]
- Fishbein M, & Ajzen I (1975). Belief, attitude, intention, and behavior: An introduction to theory and research. Reading, MA: Addison-Wesley. [Google Scholar]
- Fishbein M, & Ajzen I (2010). Predicting and changing behavior: The reasoned action approach. New York, NY: Psychology Press. [Google Scholar]
- Folta SC, Seguin RA, Chui KKH, Clark V, Corbin MA, Goldberg JP, … Nelson ME. (2015). National dissemination of strongwomen-healthy hearts: A community-based program to reduce risk of cardiovascular disease among midlife and older women. American Journal of Public Health, 105(12), 2578–2585. doi: 10.2105/AJPH.2015.302866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forsetlund L, Bjorndal A, Rashidian A, Jamtvedt G, O’Brien MA, Wolf F, … Oxman AD. (2009). Continuing education meetings and workshops: Effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews(2), Cd003030. doi: 10.1002/14651858.CD003030.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godin G, Bélanger-Gravel A, Eccles M, & Grimshaw J (2008). Healthcare professionals’ intentions and behaviours: A systematic review of studies based on social cognitive theories. Implementation Science, 3, 36–36. doi: 10.1186/1748-5908-3-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gray MJ, Elhai JD, & Schmidt LO (2007). Trauma professionals’ attitudes toward and utilization of evidence-based practices. Behavior Modification, 31(6), 732–748. doi: 10.1177/0145445507302877 [DOI] [PubMed] [Google Scholar]
- Harned MS, Dimeff LA, Woodcock EA, & Contreras I (2013). Predicting adoption of exposure therapy in a randomized controlled dissemination trial. Journal of Anxiety Disorders, 27(8), 10.1016/j.janxdis.2013.1002.1006. doi: [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: The Guilford Press. [Google Scholar]
- Huber PJ (1967). The behavior of maximum likelihood estimates under non-standard conditions. Berkeley, CA: University of California Press. [Google Scholar]
- Karlin BE, Ruzek JI, Chard KM, Eftekhari A, Monson CM, Hembree EA, … Foa EB. (2010). Dissemination of evidence-based psychological treatments for posttraumatic stress disorder in the veterans health administration. Journal of Traumatic Stress, 23(6), 663–673. doi: 10.1002/jts.20588 [DOI] [PubMed] [Google Scholar]
- Kelly JA, Somlai AM, DiFranceisco WJ, Otto-Salaj LL, McAuliffe TL, Hackl KL, … Rompa D. (2000). Bridging the gap between the science and service of hiv prevention: Transferring effective research-based hiv prevention interventions to community aids service providers. American Journal of Public Health, 90(7), 1082–1088. doi: 10.2105/AJPH.90.7.1082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lent RW, Hill CE, & Hoffman MA (2003). Development and validation of the counselor activity self-efficacy scales. Journal of Counseling Psychology, 50(1), 97–108. doi: 10.1037/0022-0167.50.1.97 [DOI] [Google Scholar]
- MacKinnon DP, Lockwood CM, & Williams J (2004). Confidence limits for the indirect effect: Distribution of the product and resampling methods. Multivariate Behavioral Research, 39(1), 99–128. doi: 10.1207/s15327906mbr3901_4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manning M (2009). The effects of subjective norms on behaviour in the theory of planned behaviour: A meta-analysis. British Journal of Social Psychology, 48(4), 649–705. doi: 10.1348/014466608X393136 [DOI] [PubMed] [Google Scholar]
- McEachan RRC, Conner M, Taylor NJ, & Lawton RJ (2011). Prospective prediction of health-related behaviours with the theory of planned behaviour: A meta-analysis. Health Psychology Review, 5(2), 97–144. doi: 10.1080/17437199.2010.521684 [DOI] [Google Scholar]
- McHugh RK, & Barlow DH (2010). The dissemination and implementation of evidence-based psychological treatments. A review of current efforts. American Psychologist, 65(2), 73–84. doi: 10.1037/a0018121 [DOI] [PubMed] [Google Scholar]
- Millstein SG (1996). Utility of the theories of reasoned action and planned behavior for predicting physician behavior: A prospective analysis. Health Psychology, 15(5), 398–402. doi: 10.1037/0278-6133.15.5.398 [DOI] [PubMed] [Google Scholar]
- Moullin JC, Sabater-Hernández D, Fernandez-Llimos F, & Benrimoj SI (2015). A systematic review of implementation frameworks of innovations in healthcare and resulting generic implementation framework. Health Research Policy and Systems, 13, 16. doi: 10.1186/sl2961-015-0005-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson TD, & Steele RG (2007). Predictors of practitioner self-reported use of evidence-based practices: Practitioner training, clinical setting, and attitudes toward research. Administration and Policy in Mental Health, 34(4), 319–330. doi: 10.1007/s10488-006-0111-x [DOI] [PubMed] [Google Scholar]
- Nilsen P (2015). Making sense of implementation theories, models and frameworks. Implementation Science, 10, 53. doi: 10.1186/s13012-015-0242-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes RE, & Courneya KS (2003). Investigating multiple components of attitude, subjective norm, and perceived control: An examination of the theory of planned behaviour in the exercise domain. British Journal of Social Psychology, 42(1), 129–146. doi:doi: 10.1348/014466603763276162 [DOI] [PubMed] [Google Scholar]
- Rivis A, & Sheeran P (2003). Descriptive norms as an additional predictor in the theory of planned behaviour: A meta-analysis. Current Psychology, 22(3), 218–233. doi: 10.1007/s12144-003-1018-2 [DOI] [Google Scholar]
- Ruzek JI, Karlin BE, & Zeiss A (2012). Implementation of evidence-based psychological treatments in the veterans health administration In McHugh RK & Barlow DH (Eds.), Dissemination and implementtion of evidence-based psychological interventions. New York: Oxford University Press. [Google Scholar]
- Sheeran P (2002). Intention—behavior relations: A conceptual and empirical review. European Review of Social Psychology, 12(1), 1–36. doi: 10.1080/14792772143000003 [DOI] [Google Scholar]
- Sniehotta FF (2009). Towards a theory of intentional behaviour change: Plans, planning, and self-regulation. British Journal of Health Psychology, 14(2), 261–273. doi: 10.1348/135910708X389042 [DOI] [PubMed] [Google Scholar]
- White H (1982). Maximum likelihood estimation of misspecified models. Econometrica, 50(1), 1–25. doi: 10.2307/1912526 [DOI] [Google Scholar]
- Williams KC, Brothers BM, Ryba MM, & Andersen BL (2015). Implementing evidence-based psychological treatments for cancer patients. Psycho-Oncology, 24(12), 1618–1625. doi: 10.1002/pon.3937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan K-H, & Bentler PM (2000). Three likelihood-based methods for mean and covariance structure analysis with nonnormal missing data. Sociological Methodology, 30(1), 165–200. doi: 10.1111/0081-1750.00078 [DOI] [Google Scholar]


