Abstract
Objective
Given the number of annual interactions between people who smoke and healthcare providers, even low efficacy interventions would be expected to have a large cumulative effect on smoking prevalence. Efforts to improve uptake of tobacco dependence treatment guidelines have had limited success. It remains unclear whether complex social motivations influence treatment decision-making among providers, despite widespread understanding of the condition’s impact on morbidity.
Methods
Clinicians from across the United States participated in a computer-based survey of potential explicit tobacco treatment biases, relative to care of hypertension. Items corresponded to framework domains of Weiner’s causal attribution theory of social motivation. Single-word, open-response items were used to gain insight into the frequency of spontaneous perceptions regarding treatment of each condition. Implicit Association Testing (IAT) measured strength of association between images of smoking and evaluation of guilt vs. innocence.
Results
Significant differences in agreement scores were identified within the Causal Attribution, Emotional Response, and Help Investment domains. Single-word answers confirmed a significant difference in Emotional Response to tobacco treatment (28.1% vs. 10.5%, p=0.02), and suggested the difference was driven by the frequent perception of frustration (75% vs. 0%, p=0.07). IAT revealed incompatibility between images of smoking and words conveying “innocence” compared to “guilt” (latency 1846 msec vs. 1113 msec, p<0.001).
Conclusions
Complex social motivations may be operational in the context of tobacco dependence treatment, limiting provider willingness to follow treatment guidelines. If confirmed, this represents a critical obstacle to sophisticated guideline implementation, and should be addressed in future implementation strategies.
Suggested Key Words (MeSH): Behavior, Addictive, Bias, Smoking Cessation, Tobacco Use Disorder, Withholding Treatment
INTRODUCTION
Functional obstacles to tobacco dependence treatment, including prohibitive time requirements, disinterest among patients, and insufficient reimbursement, have been reported as important obstacles to physician engagement with patient tobacco use.(Park et al., 2001; Vogt, Hall, & Marteau, 2005) Others have suggested that the institutional responsibility to treat tobacco dependence has not yet been firmly established within the culture of medicine.(M. C. Fiore & Baker, 1995; Leone & Evers-Casey, 2015) In addition, several cognitive biases have recently been proposed as possible barriers to effective tobacco dependence treatment by virtue of their influence on perception of treatment success probability.(Leone, Evers-Casey, Graden, & Schnoll, 2015; Leone, Evers-Casey, Graden, Schnoll, & Mallya, 2015) If true, static patterns of physician behavior in the face of well-organized and widely disseminated clinical guidelines may in fact be a function of complex social motivations rather than simple lack of interest or training. Understanding motivational influences on clinician behavior has enormous potential public health implications given the frequency of contact between tobacco users and the healthcare system.
In contexts such as obesity, lung cancer and substance abuse, it has become clear that beliefs regarding illness causation, and the associated inferences about the capacity for patients to volitionally alter the cause of illness, profoundly influence the willingness to invest effort in help giving (Weiner, 1985, 1993; Weiner, Perry, & Magnusson, 1988), and can constrain acquisition of new knowledge and skills.(Bazerman, 2006) This suggests the possibility that reactions to the perceived causal controllability of illness, and the attribution of culpability onto the patient, may differentially influence provider response to chronic illnesses, regardless of their explicitly stated utility of intervention.(Bass et al., 2018; Miller et al., 2013; Robstad, Siebler, Söderhamn, Westergren, & Fegran, 2018)
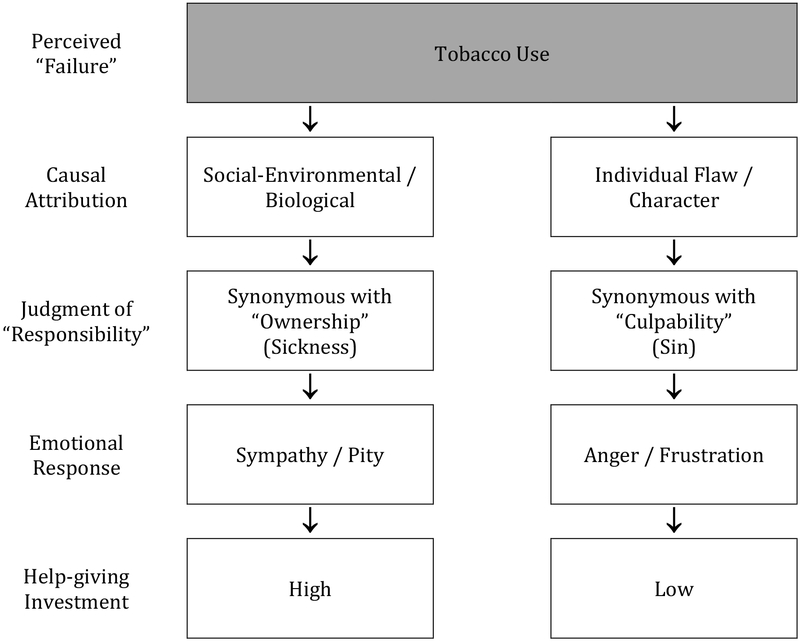
An implicit bias is a subconscious sense of “correctness” that affects our actions or decisions in an unconscious manner, sometimes in unfavorable ways. As opposed to explicit biases which are consciously accessible and can be overcome, clinicians cannot be aware of implicit biases because they are not accessible through introspection.(Blair, Steiner, & Havranek, 2011) When assessing an unexpected or unwelcome behavior in others, people implicitly attribute causality to either personal character deficits or impersonal environmental influences.(Weiner, 1993) The attribution leads to distinct interpretations of “responsibility,” which in turn lead to very different emotional reactions (Figure 1). To explore whether physician tobacco treatment behaviors may be a function of these implicit attributions, we assessed differences in explicit emotional attitudes toward tobacco use treatment compared to hypertension, an alternate chronic illness context requiring evaluation and management. We hypothesized that implicit associations between images of people smoking and evaluations of culpability would be measurably more compatible than similar associations with evaluations of innocence.
Figure 1:
Is tobacco use “Sin or Sickness?” Weiner’s theory of social motivation, relating fundamental attribution error to clinician emotional response and effect on willingness to give help.(Weiner, 1993)
METHODS
Sample
Using a national database of primary care providers, we solicited survey participation via e-mail invitation to a total of 100 candidate clinician respondents, with two randomly generated candidate clinicians from each state. The e-mail invitation included a web link to a study description, a statement of confidentiality and privacy protection, and a link by which participants could affirm their informed consent. Once consent was documented, the participants’ computers were automatically redirected to a web-based survey tool using Inquisit3 software (v3.0.6.0, Millisecond Software, Seattle WA), incorporating several validated methods of assessing both implicit and explicit attitudes.(A G Greenwald, McGhee, & Schwartz, 1998; Pacini & Epstein, 1999) Participants completing the survey received a $100 gift card payment, consistent with published guidance on clinician reimbursement for research participation.(Draper, Wilson, Flanagan, & Ives, 2009)
Explicit Associations
Ten items were designed to evaluate the degree to which clinicians agreed with statements regarding causal attribution, ownership, emotional response, and help-giving. Responses were on a 5-point Likert scale, with values ranging from “1=Strongly Disagree” to “5=Strongly Agree.” One open response item was included asking respondents “Give one adjective to describe treating hypertension/tobacco_ in your practice.” All items were shown twice, for a total of 22 items (Table 1). Items were presented to the respondents randomly to avoid value anchoring.
Table 1:
Items used to estimate clinician agreement with statements reflecting domains within Weiner’s social motivation theory (Fig 1). Mean difference in agreement scores (Δ) expressed as absolute value to account for directionality of items. Confidence intervals (CI) that include zero reflect no difference in attitude between tobacco and hypertension responses. Sig = paired significance level.
| Pair | Item | Domain | |Mean Δ| | 95% CI | Sig |
|---|---|---|---|---|---|
| 1 | My advice about [smoking / hypertension] often falls on deaf ears. | Causal Attribution | 0.579 | (0.258, 0.900) | 0.001 |
| 2 | Treating [smokers / hypertensives] frustrates me. | Emotional Response | 0.702 | (0.337, 1.067) | <0.001 |
| 3 | Adherence issues frequently undermine the effectiveness of [smoking / hypertension] pharmacotherapy. | Ownership | 0.316 | (−0.029, 0.660) | 0.72 |
| 4 | I really don’t have time to provide care for [smoking / hypertension]. | Help Investment | 0.474 | (0.217, 0.730) | <0.001 |
| 5 | Sometimes [smokers / hypertensives] make me angry. | Emotional Response | 0.649 | (0.315, 0.984) | <0.001 |
| 6 | I like the challenge of treating [smoking / hypertension]. | Emotional Response | 0.561 | (−0.953, −0.170) | 0.006 |
| 7 | Patients [who smoke / with hypertension] frequently do not cooperate in their care. | Ownership | 0.018 | (−0.348, 0.313) | 0.916 |
| 8 | I don’t understand how anyone can [smoke / ignore their blood pressure] after a diagnosis of [lung cancer / stroke]. | Causal Attribution | 0.649 | (−1.005, −0.293) | 0.001 |
| 9 | I often feel a twinge of disgust when I notice that my patient [smokes / has hypertension]. | Emotional Response | 0.789 | (0.422, 1.157) | <0.001 |
| 10 | I am responsible for controlling my patient’s [compulsion to smoke / uncontrolled hypertension]. | Help Investment | 1.316 | (−1.711, −0.920) | <0.001 |
| Give 1 adjective to describe treating [tobacco dependence / hypertension] in your practice. |
Implicit Association Testing (IAT)
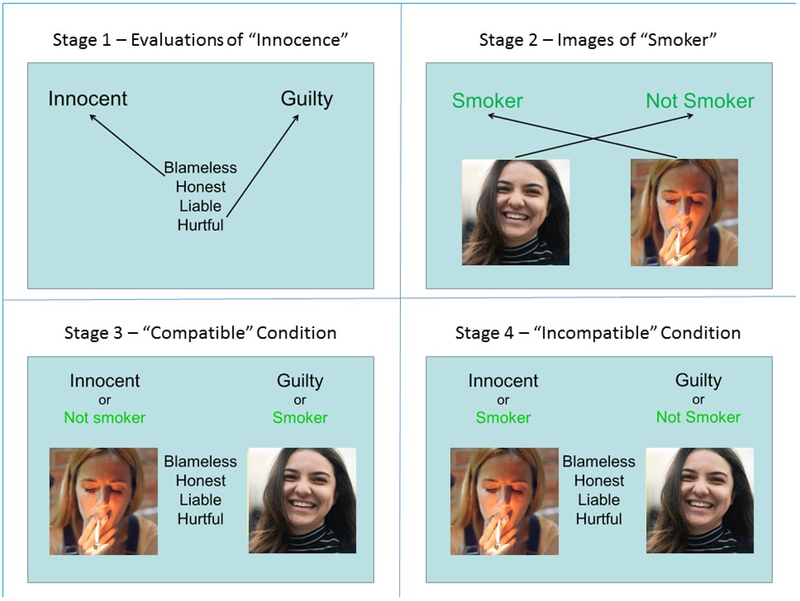
The IAT is a flexible measure of implicit social cognition that requires participants to sort words or images together by category. The method assumes that sorting well-associated evaluations together is easier than grouping evaluations that are poorly associated or incompatible, increasing the response latency time by imperceptible but measurable amounts, a method that has been validated as a measure of social attitudes toward common medical conditions(Sabin & Greenwald, 2012). We assessed compatibility of “smoking” and “culpable” using a 4-stage IAT (Figure 2). Stage 1 asked respondents to sort evaluations of innocence and guilt to opposite sides of the screen. In stage 2, images of people smoking / not-smoking were similarly sorted. In stage 3 (compatible condition), respondents were tasked with sorting smoking images alongside evaluations of culpability, while in stage 4 (incompatible condition) smoking images were sorted alongside evaluations of innocence.
Figure 2:
Four Stage IAT designed to identify implicit associations between smoking status and evaluations of culpability. In Stage 1, the computer randomly presents words consistent with themes of guilt or innocence in the center of the screen. Respondents are asked to sort the words to the left or right side of the screen by depressing the ‘Q’ or ‘P’ keys with their left or right forefingers respectively. In Stage 2, respondents use the same technique to sort images of people, either smoking or not. Stage 3 requires sorting the hypothesized compatible evaluations to the same side of the screen, while Stage 4 requires similarly sorting the hypothesized incompatible evaluations. Latency time, measured from the moment of presentation to the moment of key stroke, are used to calculate the strength of implicit association between concepts. Credit: Getty Images.
Statistics
Paired differences in explicit attitude responses (Δ) were compared to the expected mean difference of zero. Absolute values of Δ were assessed to account for “directionality” of the item, such that higher values represent greater degree of unfavorable explicit tobacco bias. IAT latency times were measured directly, with higher values indicating implicit incompatibility between the two sorted evaluations. A standard scoring algorithm eliminates trials with latencies greater than 10,000 milliseconds or less than 400 milliseconds to minimize the effect of outlier response times. Values were treated as continuous outcomes, and compared using two-sided paired t-test. Single word responses were categorized into five clinically relevant themes, and IAT response rates were compared using Chi-square. Bivariate correlations were assessed using simple linear models. Significance threshold was set at p<0.05, without correction for multiple comparisons.
Institutional Review
All study procedures were approved and overseen by the University of Pennsylvania Institutional Review Board.
RESULTS
Fifty-seven clinicians (57%) completed all survey tasks. Age ranged from 26 to 67-years-old (median 39), 62% male, and between <1 and 38 years in practice (median 8). Mean pair-wise differences in explicit attitude scores are shown in Table 1. Relative to their explicit responses about hypertension, respondents showed significantly more unfavorable explicit tobacco bias within the Causal Attribution, Emotional Response, and Help Investment domains, but no difference was identified among the items related to Ownership. Aggregate Help Investment scores were negatively correlated to aggregate Emotional Response scores (R2 0.14, p=0.002).
The distribution of tobacco-related single word responses differed significantly from the hypertension-related responses (p<0.001). The overall difference was driven by the difference in the Emotional Response category (Table 2). Five recurring emotional responses were offered by clinicians. Patterns of tobacco vs. hypertension responses trended toward statistical significance, with the most striking discrepancy observed in the number of times clinicians expressed frustration.
Table 2:
Single word responses related to care of tobacco dependence and hypertension. Significant differences noted in frequency of emotion-oriented responses, with apparent emphasis on “frustration” within tobacco response set.
| Response Category | Tobacco: n (%) | Hypertension: n (%) | Significance |
|---|---|---|---|
| Utility to patient | 6 (10.5) | 7 (12.3) | 0.77 |
| Technical / Professional | 26 (45.6) | 32 (56.1) | 0.26 |
| Patient Character | 0 (0) | 1 (1.8) | N/A |
| Emotional Response | 16 (28.1) | 6 (10.5) | 0.02 |
| Relentless | |||
| Intervention | 5 (8.8) | 8 (14.0) | 0.38 |
| Uncategorized | 4 (7.0) | 3 (5.3) | 0.70 |
IAT latencies during the compatible condition were significantly lower than latencies observed during the incompatible condition. Latency times for pairing images of smokers with evaluations of culpability averaged 1113 milliseconds (msec), while latencies for pairing smokers with innocence averaged 1846 msec (p<0.001). The IAT-D statistic standardizes the observed mean latency difference to the overall standard deviation (SD), providing an indexed strength of association.(Anthony G Greenwald, Nosek, & Banaji, 2003) We observed a mean latency difference of 733 msec and a latency SD of 610 msec; our observed IAT-D was 1.2, corresponding to a strong effect of association.(Anthony G Greenwald et al., 2003) IAT performance did not vary by age, with average latency difference of 795 msec among clinicians below the median age of 39 and 766 msec among those above the median (p=0.56). Similarly, there was no correlation between IAT latency difference and years of practice (R2 0.00, p=0.50).
DISCUSSION
Given that nearly 85% of adults have contact with their primary care setting each year, healthcare represents an enormous untapped conduit for reach into the tobacco-dependent population.(Centers for Disease Control and Prevention, 2015) Since advice and support given to smokers by healthcare professionals can achieve abstinence rates of 5–10% with even minimal interventions, and 15–30% with more intense interventions (M. Fiore, Jaén, Baker, & et al., 2008), the potential for more fully-implemented tobacco use treatment services to substantially affect prevalence over time should be a primary target for implementation. Unfortunately, outcomes have been limited by a healthcare context that has not been particularly engaging; hypertension is nearly universally addressed in primary care, albeit at time less aggressively than recommended (Hyman & Pavlik, 2000) while fewer than 20% of primary care visits include tobacco counseling, and less than 2% result in pharmacotherapy prescriptions.(Thorndike, Regan, & Rigotti, 2007) Our observations generate an interesting hypothesis as to why this may be the case and can guide efforts to use implementation science strategies to address this practice gap.
While it is possible that practical barriers have made systematic implementation more challenging, it seems improbable that they represent insurmountable and permanent barriers to progress. In fact, when asked for single-word associations, our respondents did not appear to offer adjectives describing technical / professional barriers or complexity of intervention any more frequently for tobacco than they did for hypertension. Instead, it appears that an unfavorable explicit and implicit attribution bias may exist among clinicians, which could in theory limit engagement. Our results suggest that clinicians more strongly agree with negative personal character statements presented relative to tobacco use, compared to hypertension. Implicit association testing suggests that respondents found images of smokers more compatible with “culpable” than “innocent.” In addition, it appears that clinicians experience more strongly negative emotions including frustration and disgust in the context of tobacco use. Single-word open responses appear to further confirm the strong emotional undercurrent that informs attitudes regarding tobacco dependence treatment. We found striking differences in emotionally-laden responses to tobacco dependence treatment, the majority of which referred again to frustration.
This study is limited in its generalizability. First, the sample is small and may not reflect the broader environment of healthcare. Second, there is a potential response bias in that 43% of invited clinicians elected not to respond. Third, because of the visual nature of the IAT employed, it was impossible to directly compare the results of the tobacco IAT to a similar test of associations with hypertension. It is important to note that an IAT index of 1.2 suggests a very strong implicit association between tobacco use and themes of culpability – a strength of association unlikely to be either random or easily replicated in other conditions. Finally, there is no independent measure of clinician behavior to provide criterion validity to IAT results.
If Weiner’s theory of causal controllability holds true, we would predict that a stronger sense of character flaw would align with implicit culpability and lead to more strongly negative emotions of anger and frustration, and expect these to negatively impact the clinician’s willingness to invest in help-giving. Recent anecdotal accounts lend credence to this possibility.(Bhargava, 2019) Our data suggest some signal in this regard, with explicit bias scores in the emotional response domain weakly but significantly correlated with negative bias scores in the help investment domain. These observations did not seem to be related to age or time in practice, which could be construed as potential surrogates for wisdom, idealism, or proximity to training.
This work suggests that strategies to improve implementation of tobacco treatment services within healthcare might be more effective if, along with dissemination of guidelines and evidence, they are also focused on correcting attribution error and the resulting downstream effects. It may be that our methods simply document the fact that treating addiction of any kind is an intrinsically more frustrating endeavor than treating hypertension. Our data do not imply that the frustration experienced by clinicians is misplaced, only that it appears to be founded in an attribution of causality that may not be consistent with current understanding of the complex neurobiology of addiction and that its impact on willingness to help may be underestimated. Further research will be required to confirm the effect we are postulating, and to determine whether clinicians can be sufficiently trained to compensate for an implicit culpability bias in order to capitalize on their unique opportunity to reduce the national rates of tobacco use.
ACKNOWLEDGEMENTS:
The authors thank Dr. Janet Audrain-McGovern for her assistance with study evaluation.
FUNDING: This work was supported by grants from the University of Pennsylvania Research Fund, National Cancer Institute (R01 CA202699; P30 CA016520) and the National Institute on Drug Abuse (K24 DA045244).
Footnotes
DECLARATION OF INTERESTS: Ms. Evers-Casey, Dr. Jenssen, and Dr. Leone have no financial or other relevant interests. Dr. Schnoll receives medication and placebo free from Pfizer and has provided consultation to Pfizer. Dr. Schnoll has provided consultation to GlaxoSmithKline and consults with CuraLeaf.
REFERENCES
- Bass B, Lake E, Elvy C, Fodemesi S, Iacoe M, Mazik E, … Lee A (2018). Smoking-Related Stigma Expressed by Physiotherapists toward Individuals with Lung Disease. Physiotherapy Canada. Physiotherapie Canada, 70(1), 65–71. 10.3138/ptc.2016-98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazerman M (2006). Judgment in Managerial Decision Making (Sixth Edition). New Jersey: John Wiley and Sons. [Google Scholar]
- Bhargava M (2019). What happens when the doctor blames you for your own cancer? - The Washington Post; Retrieved January 19, 2019, from https://www.washingtonpost.com/outlook/what-happens-when-the-doctor-blames-you-for-your-own-cancer/2019/01/11/2791611e-14ff-11e9-90a8-136fa44b80ba_story.html?utm_term=.b0de3ebb611a [Google Scholar]
- Blair IV, Steiner JF, & Havranek EP (2011). Unconscious (Implicit) Bias and Health Disparities: Where Do We Go from Here? The Permanente Journal, 15(2), 71–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2015). FastStats - Ambulatory Care Use and Physician office visits. Retrieved February 7, 2015, from http://www.cdc.gov/nchs/fastats/physician-visits.htm
- Draper H, Wilson S, Flanagan S, & Ives J (2009). Offering Payments, Reimbursement and Incentives to Patients and Family Doctors to Encourage Participation in Research. Family Practice, 26(3), 231–238. 10.1093/fampra/cmp011 [DOI] [PubMed] [Google Scholar]
- Fiore MC, & Baker TB (1995). Smoking cessation treatment and the good doctor club. American Journal of Public Health, 85(2), 161–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore M, Jaén C, Baker T, & et al. (2008). Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service. [Google Scholar]
- Greenwald AG, McGhee DE, & Schwartz JL (1998). Measuring individual differences in implicit cognition: the implicit association test. Journal of Personality and Social Psychology, 74(6), 1464–1480. [DOI] [PubMed] [Google Scholar]
- Greenwald Anthony G, Nosek BA, & Banaji MR (2003). Understanding and using the implicit association test: I. An improved scoring algorithm. Journal of Personality and Social Psychology, 85(2), 197–216. [DOI] [PubMed] [Google Scholar]
- Hyman DJ, & Pavlik VN (2000). Self-reported Hypertension Treatment Practices Among Primary Care Physicians: Blood Pressure Thresholds, Drug Choices, and the Role of Guidelines and Evidence-Based Medicine. Archives of Internal Medicine, 160(15), 2281–2286. 10.1001/archinte.160.15.2281 [DOI] [PubMed] [Google Scholar]
- Leone FT, & Evers-Casey S (2015). Examining the Role of the Health Care Professional in Controlling the Tobacco Epidemic: Individual, Organizational and Institutional Responsibilities In Progress in Respiratory Research Vol. 42 The Tobacco Epidemic, Loddenkemper and Kreuter (eds) (2nd ed., pp. 219–228). Basel, Switzerland: Karger. [Google Scholar]
- Leone FT, Evers-Casey S, Graden S, & Schnoll R (2015). Behavioral economic insights into physician tobacco treatment decision-making. Annals of the American Thoracic Society, 12(3), 364–369. 10.1513/AnnalsATS.201410-467BC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leone FT, Evers-Casey S, Graden S, Schnoll R, & Mallya G (2015). Academic Detailing Interventions Improve Tobacco Use Treatment among Physicians Working in Underserved Communities. Annals of the American Thoracic Society, 12(6), 854–858. 10.1513/AnnalsATS.201410-466BC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller DP, Spangler JG, Vitolins MZ, Davis SW, Ip EH, Marion GS, & Crandall SJ (2013). Are medical students aware of their anti-obesity bias? Academic Medicine: Journal of the Association of American Medical Colleges, 88(7), 978–982. 10.1097/ACM.0b013e318294f817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacini R, & Epstein S (1999). The relation of rational and experiential information processing styles to personality, basic beliefs, and the ratio-bias phenomenon. Journal of Personality and Social Psychology, 76(6), 972–987. [DOI] [PubMed] [Google Scholar]
- Park E, Eaton CA, Goldstein MG, DePue J, Niaura R, Guadagnoli E, … Dube C (2001). The development of a decisional balance measure of physician smoking cessation interventions. Preventive Medicine, 33(4), 261–267. 10.1006/pmed.2001.0879 [DOI] [PubMed] [Google Scholar]
- Robstad N, Siebler F, Söderhamn U, Westergren T, & Fegran L (2018). Design and psychometric testing of instruments to measure qualified intensive care nurses’ attitudes toward obese intensive care patients. Research in Nursing & Health. 10.1002/nur.21914 [DOI] [PubMed]
- Sabin JA, & Greenwald AG (2012). The influence of implicit bias on treatment recommendations for 4 common pediatric conditions: pain, urinary tract infection, attention deficit hyperactivity disorder, and asthma. American Journal of Public Health, 102 (5), 988–995. 10.2105/AJPH.2011.300621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thorndike AN, Regan S, & Rigotti NA (2007). The treatment of smoking by US physicians during ambulatory visits: 1994 2003. American Journal of Public Health, 97(10), 1878–1883. 10.2105/AJPH.2006.092577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vogt F, Hall S, & Marteau TM (2005). General practitioners’ and family physicians’ negative beliefs and attitudes towards discussing smoking cessation with patients: a systematic review. Addiction, 100(10), 1423–1431. 10.1111/j.1360-0443.2005.01221.x [DOI] [PubMed] [Google Scholar]
- Weiner B (1985). An attributional theory of achievement motivation and emotion. Psychological Review, 92(4), 548–573. [PubMed] [Google Scholar]
- Weiner B (1993). On sin versus sickness. A theory of perceived responsibility and social motivation. The American Psychologist, 48(9), 957–965. [DOI] [PubMed] [Google Scholar]
- Weiner B, Perry RP, & Magnusson J (1988). An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology, 55(5), 738–748. [DOI] [PubMed] [Google Scholar]