Abstract
Introduction:The objective of the current retrospective study is to present the results of a personal research on the prevalence and treatment of alithiasic cholangitis in hospitalized patients.
Material and methods:The research was based on the following criteria: case selection according to gender, age and diagnosis, anamnesis information, clinical, paraclinical, imagery and laboratory investigation methods, therapeutic approach.
Results:Between 2016-2018, 109 cases had a discharge diagnosis of postcholecystectomy cholangitis following clinical and paraclinical examinations. In a large percentage, cholangitis was alithiasic, imagery assessments showing only a dilation of the intra- and/or extra-hepatic biliary ducts (81 cases, 91.01%).
Conclusions:Alithiasic cholangitis has been the main biliary cause in the postcholecystectomy pathology in this reference study (91.01%). In hospitalized people with alithiasic cholangitis as main diagnosis, highlighted endoscopic retrograde cholangiopancreatography (ERCP) represented a modern therapeutic approach; this allows the improvement of sphincter Oddi functional disorders through sphincterotomy/sphincteroplasty (6.75%).
Keywords:cholangitis, alithiasic, non-invasive treatment.
INTRODUCTION
Postcholecystectomy cholangitis can be caused by the persistence of certain factors which existed before the surgical intervention, by certain causes associated with surgery performance, or it can be due to certain causes which developed during the postoperative period. The clinical evidence for postcholecystectomy cholangitis is represented by pain syndrome with different degrees, localized in the upper level of the abdomen, dyspepsia, and fever. Jaundice syndrome can be present.
The present-time trend in the biliary pathology is to choose the most adequate surgical treatment based on the degree and severity of the inflammatory process and associated disorders; through this conduct, the trend is to reduce the period of hospitalization and post-surgery complications, thus increasing patients’ quality of life.
Postcholecystectomy cholangitis is represented by the intra-hepatic and/or extra-hepatic biliary tract modifications, which are imagistically translated by their enlargement, with or without parietal modifications, with or without obstructive injuries on the level of the terminal common bile duct. The clinical diagnosis can occur when performing biliary surgery in the absence of a rigorous indication (dyspeptic symptoms in the absence of lithiasis). To avoid the occurrence of postcholecystectomy cholangitis, a rigorous preoperative assessment is required. In the absence of typical clinical manifestations specific for gallstones and abdominal ultrasound argumentation of lithiasis, cholecystectomy will not be performed.
For most patients, the polymorphic etiology of postcholecystectomy cholangitis is established after clinical and imagistic and laboratory investigations. The objective of this study is to present the results of a personal research on the prevalence, etiology and treatment of cases with postcholecystectomy alithiasic cholangitis admitted at the Gastroenterology Department of the Emergency County Clinical Hospital of Oradea, Romania.
MATERIAL AND METHOD
Clinical observation sheets of patients hospitalized at the Clinical Gastroenterology Department with upper abdominal symptoms after cholecystectomy were used as materials.
The research was based on the following criteria: case selection according to gender, age and diagnosis, anamnesis information, clinical, paraclinical, imagery and laboratory investigation methods, and therapeutic approach. ERCP was also a modern diagnostic and therapeutic method (Figure 1). Anamnestic data revealed a previous history of cholecystectomy, upper abdominal pain syndrome, dyspepsia, fever, and jaundice syndrome.
In the present study, we analysed and referenced the biological parameters as an expression of the non-specific inflammatory syndrome (white blood cell and neutrophil count); biliaryexcretory (serum bilirubin level, urinary bile pigment); cholestatic and hepatocytolytic syndrome: and transaminases-aspartate aminotransferase (ASAT/GOT), alanine aminotransferase (ALAT/ALT), gamma-glutamil-transferase (GGT), alkaline phosphatase.
Clotting factors, lipase, blood culture, serum iron, blood urea, serum glucose, lactic dehydrogenase, immunoassay tests, albumin hypofunction tests, and erythrocyte sedimentation rate were also important parameters analysed in this study. Erythrocyte sedimentation rate is increased in the postcholecystectomy cholangitis jandice and in malignant etiology. Hypoleukocytosis suggests malignant etiology or hemolytic in antehepatic jaundice and liver cirrhosis. Hyperleukocytosis with neutrophilia was presented like a biological marker in the inflammatory syndrome in postcholecystectomy alithiasic cholangitis.
Abdominal ultrasound and computed tomography, magnetic resonance cholangiography (MRCP), upper gastrointestinal endoscopy, and barium swallow test were used for imagistic examinations. Therapeutic options for postcholecystectomy alithiasic cholangitis consisted of non-invasive pharmacological methods and endoscopic methods (endoscopic retrograde cholangiopancreatography – ERCP).
The pharmacological methods were complex, different classes of medication being associated. In gastric and duodenum conditions with bile reflux, proton-pump inhibitors are mainly used. Magnesium and aluminum salts had been associated to the treatment, having a protective effect on the esophagus-gastric-duodenum mucous, and improving dyspeptic functional disturbances. Antibiotics were used either as monotherapy or in therapeutic schemes in order to eradicate Helicobacter pylori infection. Analgesics, synthetic anticholinergics, dopamine antagonists, pain killers were administered for the symptomatic treatment of pain or abdominal discomfort caused by postcholecystectomy alithiasic cholangitis. For rebuilding the bacterial flora, in the treatment of infection with Helicobacter pylori and/or for rebuilding intestinal transit, probiotics were also associated, consecutive with the remission of symptomatology. Administration of probiotics increased the extent of H. pylori eradication and prevented the development of relapses.
Prokinetics were given as symptomatic drugs in the treatment of digestive motility disturbances. Biliary acids were also administered (ursodeoxycholic acid) due to their role in the treatment of bile reflux. Being a modern therapeutic approach, endoscopic sphincterotomy/sphincteroplasty allowed the improvement of sphincter Oddi dyskinesia. A dietary treatment was associated to the therapy of postcholecystectomy alithiasic cholangitis.
RESULTS
For the aforesaid period, 109 patients were admitted at the Gastroenterology Department with postcholecystectomy cholangitis, and 85 of them were females, accounting for 77.98% of the total number of hospitalized cases (Table 1). The most representative age decade was between 55 and 64, with 41 (37.11%) patients out of 109.
Imaging assessments showed that, out of the 109 cases of cholangitis, six had cholelithiasis; two, lithiasis of the intra-hepatic biliary ducts; and four, sclerosis odditis. In three cases, cholangitis was observed after retrograde endoscopic colangiopancreatography (ERCP), in five other cases, cholangitis developed after biliary-digestive anastomosis, and in one case, tumor of Vater papilla (Table 2)
In a large percentage, cholangitis was alithiasic (Table 3), imaging examinations presenting only a dilation of the intrahepatic and/or common bile ducts.
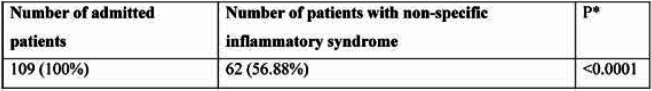
Non-specific inflammatory syndrome was prevalent among patients admitted at the gastroenterology ward, with 62 (56.88%) subjects out of 109 (Table 4). Laboratory investigations have identified leukocytosis with neutrophilia. As a secondary discharge diagnosis in cases of hospitalized postcholecystectomy cholangitis, as a consequence of the gastric-duodenum-esoDiagnosis phagus biliary reflux, the reference study revealed a wide pathological diversity (Table 5).
Multiple organic damages can coexist in case of the same patient due to the biliary reflux after cholecystectomy. In the reference study, 12 cases of pancreas damage with symptoms of acute or cephalic chronic pancreatitis were observed. In 37 cases, imagery and laboratory investigations revealed pathological liver modifications, represented by cholestasis and/or hepatic steatosis, satellite hepatitis as a secondary discharge diagnosis. As shown in table 6, medication was the basic therapy, which enabled a favorable evolution of patients.
DISCUSSION
Information provided by the research made for this study significantly show that patients with postcholecystectomy symptoms admitted at the Clinical Gastroenterology Department have cholangitis as a discharge diagnosis. Postcholecystectomy cholangitis lead to intrahepatic ducts and common bile duct modifications, which are imagistically translated by their enlargement, with the absence or presence of biliary duct wall modifications. Imaging argumentation of the inferior common bile duct obstructive lesions can also exist (1-3). In 89 of the admitted cases, following clinical and paraclinical examinations, the primary discharge diagnosis was cholangitis with or without lithiasis of the main biliary ducts. The literature describes the frequency of postcholecystectomy cholan- gitis (4-6).
In this context, cholangitis was clinically objectified by mild pain syndrome from the right hypochondrium area, by the biological markers of the presence of inflammatory syndrome. Laboratory investigations revealed hyperleukocytosis and neutrophilia and/or of bile excretory syndrome and/or of cholestasis and hepatic cytolysis syndrome (7, 8). Non-specific inflammatory syndrome with hyperleukocytosis and neutrophilia was more prevalent among patients admitted at the gastroenterology department.
In most of the cases, hepatic, pancreas, gastric and duodenum conditions were highlighted, which created complexity and a wide diversity for the pharmacological treatment. Also, such patients often have associated cardiovascular conditions. Most of the cases hospitalized at the Gastroenterology Department received pharmacological treatment in association with a gastric or hepatic cleansing diet.
Several gastric conditions were diagnosed, including axial hiatal hernia, gastric-esophagus reflux diseases, reflux antro-pyloric or antral gastritis, pseudopolypoid gastritis, atrophic chronic gastritis, erythematous or erosive pangastritis, antral gastric ulcer, reflux gastritis with Helicobacter pylori, erosive bulbitis, hypertrophic chronic gastritis, prepyloric ulcer, etc. In other 20 cases of postcholecystectomy syndrome, duodenum gastric biliary reflux was the predominant etiology, with upper digestive endoscopy also showing different degrees of damage of the esophagus, stomach and duodenum. In the current study, among cases of hospitalized postcholecystectomy cholangitis, a wide pathological diversity was noticed as a secondary discharge diagnosis, due to this gastric-duodenum- esophagus biliary reflux, which could be responsible for multiple organic damages in one and the same patient (9, 10).
There was a complex etiology of the disorders after cholecystectomy in patients admitted at our Gastroenterology Department, including gastritis, hiatal hernia, reflux esophagitis, duodenum- gastric biliary reflux, chronic duodenal bulbitis, chronic or acute pancreatitis, fatty liver (hepatic steatosis), reactive satellite hepatitis, intrahepatic lithiasis, common bile duct lithiasis, odditis, oddian dyskinesia, relapsing acute or chronic cholangitis based on certain biliary-digestive anastomosis, and irritable bowel. Gastric-duodenum-esophagus biliary reflux lead to the development of pathological esophagus, gastric and duodenal modifications (11, 12). On the level of the esophagus, endoscopy can reveal esophagitis or stenosis or hiatal hernia type of injuries. Rarely, Barret epithelium injuries can be seen (13). Gastric-duodenum type of injuries often coexist. Reflux esophagitis is a frequent consequence of this biliary alkaline reflux. For assessing the severity of these esophagus mucous denudation injuries, the Los Angeles reflux esophagitis classification has been adopted. In the reference study, upper digestive endoscopy has more frequently shown lighter types, Los Angeles A reflux esophagitis.
Another pathology revealed by endoscopy investigations from the reference study was biliary reflux caused digestive cancers. According to the literature, the incidence of this malignant pathology is consecutive to cholecystectomy (13, 14). Bile acids act aggressively on the lipids from the gastric mucous through a detergent mechanism. There were several endoscopy types of biliary reflux gastritis seen in this study such as exudative erythematous, antral erosive or antro-corporeal, type B antral–infection with Helicobacter pylori, hypertrophic, atrophic and gastritis (pangastritis). The risk on Helicobacter pylori infection increases after cholecystectomy (15, 16).
An exact etiological differentiation cannot be performed in case of the postcholecystectomy cholangitis because there a hepatic and/or pancreas damage can also coexist. In the reference study, 12 cases of pancreas damage with symptoms of acute pancreatitis or cephalic chronic pancreatitis were seen. In 37 cases, imagery and laboratory investigations revealed liver pathological modifications, with cholestatic and/or hepatic steatosis satellite hepatitis as a diagnosis expression. In 27 of the 37 cases, satellite hepatitis was observed as a secondary discharge diagnosis. All information comes to confirm the findings reported in the published studies, namely that these hepatic-cellular and pancreatic conditions are frequently occurring in postcholecystectomy cholangitis (17).
Many times, these patients also present conditions from the area of cardiovascular or metabolic diseases such as dyslipidemia, type II diabetes mellitus, which require insulin. The medical treatment of patients hospitalized at the Gastroenterology Department with postcholecystectomy cholangitis was mainly pharmacological. In six (6.75%) cases, endoscopic treatment was performed. Endoscopic retrograde cholangiopancreatography is a modern therapeutic method, which helps to improve sphincter Oddi dyskinesia through sphincterotomy/ sphincteroplasty (18-22). In Oddi sphincter dyskinesia, the initial medical option will be represented by drugs like nitroglycerin, nifedipine, anticholinergics agents, amyl nitrite (23-25). In 94.5% of our cases, medication was administered (Table 6), which is consistent with the literature (26-28).
The pharmacological treatment is complex, with different classes of medication being associated. It is based on antibiotics, antispastics, pain killers, proton-pump inhibitors, prokinetic agents, liver protectors, bile acid substitutes (ursodeoxycholic acid) (29) pancreatic enzymes; in case of oddian dyskinesis – nifedipines, nitroglicerina, amyl nitrite (23).
The antimicrobial treatment is initiated according to the blood culture results. In cases of severe acute cholangitis, empirical therapy with fluoroquinolones is applied. Subsequently, treatment will be readjusted according to the results of the antibiogram of the blood culture test. These therapeutic aspects are underlined in the updated Tokyo Guidelines (30-32). Thus, after the microbial etiology of cholangitis is identified and antibiogram is performed, the anti-infective therapy will be adjusted according to specific pathogens. If there is no noticeable improvement in patients’ general condition, it is associated with antimicrobial treatment, beta-lactamase inhibitors, carbapenems, cephalosporins, metronidazole. There is a possibility of an ineffective antimicrobial response due to a low penetration of antibiotics into the biliary secretion from the obstructed bile ducts (excluding fluoroquinolones). Ureidopenicillin-based therapy consists in administration of Piperacillin/Tazobactam. The effectiveness of penicillin increases by pairing with Metronidazole and aminoglycosides. Monobactam or carbapenem antibiotics may also be administered, according to the Tokyo 2018 Guide (TG18), in cases with severe acute cholangitis grade III. Monobactams and carbapenems are antibiotics with a very large spectrum of action covering both Gram-negative and positive germs and anaerobic germs. Ampicillin/ Sulbactam has a reduced antimicrobial activity against Escherichia coli; it was removed from the North American guide of antimicrobial treatment for ascending cholangitis (33).
Also, in patients with repeated relapsing cholangitis, parasitic infections, or previous surgical or endoscopic interventions, the response to antimicrobial treatment may be absent. Antimicrobial therapy and biliary decompression are the main pillars in the current therapeutic management of acute cholangitis. Associated to the treatment of postcholecystectomy cholangitis etiology, the adequate medication for cardiovascular disturbances and lipid, triglyceride and cholesterol metabolism disturbances will also be administered. It is not infrequent for these patients to have type II insulin addicted diabetes mellitus in their medical history. Pharmacological treatment, once initiated in hospital, was continued in ambulatory, leading to symptom remission. Medication was accompanied by a gastric, hepatic and pancreas cleansing diet (34, 35).
Treatment of pathology after cholecystectomy is complex, considering the diversity of pathogeny and the symptomatology which creates discomfort, affecting patients’ social and family life. Dietary treatment not only contributes to the activation of the gastric-intestinal system, but also to that of metabolic processes, including the cellular level. Prolonged sparing of certain organs results in progression of the pathological process, inadaptation of many compensatory mechanisms. Diet therapy has to offer a balanced nutrition, in accordance with the energetic needs of the body and also with other factors such as age, gender, profession, etc. The gastric, hepatic sparing diet improves symptoms of postcholecystectomy cholangitis. The quality of life depends on both the clinical status of the patient and the accuracy of pre-surgery diagnosis.
CONCLUSION
Non-specific inflammatory syndrome is more prevalent in patients with postcholecystectomy alithiasic cholangitis admitted at the gastroenterology department; in a large percentage, imagery assessments showed only enlarged intrahepatic ducts and/or common bile duct.
As a secondary discharge diagnosis, multiple organic damages can coexist in one and the same patient admitted with alithiasic postcholecystectomy cholangitis due to the gastric-duodenum- esophagus biliary reflux. The management of postcholecystectomy alithiasic cholangitis is non-invasive, being mainly based on medication.
The current study on patients hospitalized in the Clinical Gastroenterology Department with postcholecystectomy alithiasic cholangitis as main diagnosis highlighted ERCP as being a modern therapeutic method; this, through the sphincterotomy/sphincteroplasty procedure, allows an improvement of sphincter Oddi functional disorders.
Conflict of interests: none declared
Financial support none declared.
Authors’ contribution: Mariana Ungur developed the idea and theory of this research, analysed the data, carried out the implementation, interpretation and discussion of results.
She also performed the analytic calculations, wrote the manuscript and translated it into English. Petru Aurel Babes helped to interpret the results and worked on the manuscript. Also, he supervised the entire work, provided critical feedback and contributed in the final version of the manuscript.
All authors discussed the final results and conclusions of the manuscript.
Acknowledgments: The authors would like to thank Dr. Carp, Manager of the Emergency County Clinical Hospital of Oradea, who provided technical support.
FIGURE 1.
Endoscopic retrograde cholangiopancreatography. Terminal common duct tumoral stenosis
TABLE 1.
Distribution of hospitalized postcholecystectomy cholangitis patients based on gender
FIGURE 2.
Percentage representation of admitted patients with postcholecystectomy cholangitis based on their living environments
TABLE 2.
Detailed presentation of cases with postcholecytectomy cholangitis
TABLE 3.
Increased prevalence of cases with alithiasic cholangitis
TABLE 4.
Prevalence of non-specific inflammatory syndrome in postcholangitis syndrome
TABLE 5.
Secondary discharge diagnosis in postcholecystectomy cholangitis
FIGURE 3.
Prevalence of the secondary discharge diagnosis in postcholecystectomy cholangitis
TABLE 6.
Comparison between types of treatment for patients admitted at the Gastroenterology Department
Contributor Information
Mariana UNGUR, Faculty of Medicine and Pharmacy, University of Oradea, Romania.
Petru Aurel BABES, Faculty of Medicine and Pharmacy, University of Oradea, Romania; “Maria” Health and Imagery Medical Center, Romania.
Adrian MAGHIAR, Faculty of Medicine and Pharmacy, University of Oradea, Romania; Pelican Hospital, Oradea, Romania.
Gheorghe Mircea POP, Faculty of Medicine and Pharmacy, University of Oradea, Romania; Emergency County Clinic Hospital of Oradea, Romania.
Bogdan FEDER, Faculty of Medicine and Pharmacy, University of Oradea, Romania; Emergency County Clinic Hospital of Oradea, Romania.
References
- 1.Wilkins T, Agabin E, Varghese J, Talukder A. Gallbladder dysfunction: cholecystitis, choledocholithiasis, cholangitis, and biliary dyskinesia. Prim Care. 2017;4:575–597. doi: 10.1016/j.pop.2017.07.002. [DOI] [PubMed] [Google Scholar]
- 2.Butte JM, Hameed M, Ball CG. Hepato-pancreato-biliary emergencies for the acute care surgeon: etiology, diagnosis and treatment. World J Emerg Surg. 2015;10:13. doi: 10.1186/s13017-015-0004-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ramchandani M, Pal P, Reddy DN. Endoscopic management of acute cholangitis as a result of common bile duct stones. Dig Endosc. 2017;29(Suppl 2):78–87. doi: 10.1111/den.12848. [DOI] [PubMed] [Google Scholar]
- 4.Ely R, Long B, Koyfman A. The Emergency Medicine-Focused Review of Cholangitis. J Emerg Med. 2018;1:64–72. doi: 10.1016/j.jemermed.2017.06.039. [DOI] [PubMed] [Google Scholar]
- 5.Riley J, Chew K, Jang T. How Do I Diagnose and Manage Acute Cholangitis? In: Gastrointestinal Emergencies. Springer, Cham. 2019. pp. 223–225.
- 6.Cai JS, Qiang S, Bao-Bing Y. Advances of recurrent risk factors and management of choledocholithiasis. Scand J Gastroenterol. 2017;1:34–43. doi: 10.1080/00365521.2016.1224382. [DOI] [PubMed] [Google Scholar]
- 7.Lan Cheong Wah D, Christophi C, Muralidharan V. Acute cholangitis: current concepts. ANZ J Surg. 2017;7-8:554–559. doi: 10.1111/ans.13981. [DOI] [PubMed] [Google Scholar]
- 8.Sulzer JK, Ocuin LM. Cholangitis: Causes, Diagnosis, and Management. Surg Clin North Am. 2019;2:175–184. doi: 10.1016/j.suc.2018.11.002. [DOI] [PubMed] [Google Scholar]
- 9.Tsai MC, Huang CC, Kao LT, Lin HC, Lee CZ. Increased Risk of Peptic Ulcers Following a Cholecystectomy for Gallstones. Sci Rep. 2016;6:30702. doi: 10.1038/srep30702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schmidt M, Søndenaa K, Dumot JA, et al. Post-cholecystectomy symptoms were caused by persistence of a functional gastrointestinal disorder. World J Gastroenterol. 2012;12:1365–1372. doi: 10.3748/wjg.v18.i12.1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mercan E, Duman U, Tihan D, et al. Cholecystectomy and duodenogastric reflux: interacting effects over the gastric mucosa. Springerplus. 2016;1:1970. doi: 10.1186/s40064-016-3641-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Latenstein CSS, Wennmacker SZ, de Jong JJ, et al. Etiologies of Long-Term Postcholecystectomy Symptoms: A Systematic Review. Gastroenterol Res Pract. 2019;2019:4278373. doi: 10.1155/2019/4278373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Atak I, Ozdil K, Yücel M, et al. The effect of laparoscopic cholecystectomy on the development of alkaline reflux gastritis and intestinal metaplasia. Hepatogastroenterology. 2012;113:59–61. doi: 10.5754/hge11244. [DOI] [PubMed] [Google Scholar]
- 14.Coats M, Shimi SM. Cholecystectomy and the risk of alimentary tract cancers: a systematic review. World J Gastroenterol. 2015;12:3679–3693. doi: 10.3748/wjg.v21.i12.3679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sifrim D. Management of bile reflux. Gastroenterol Hepatol (NY) 2013;3:179–180. [PMC free article] [PubMed] [Google Scholar]
- 16.Patnayak R, Reddy V, Jena A, et al. Helicobacter pylori in Cholecystectomy Specimens-Morphological and Immunohistochemical Assessment. J Clin Diagn Res. 2016;5:EC01–EC03. doi: 10.7860/JCDR/2016/14802.7716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ahmed M. Acute cholangitis-an update. World J Gastrointest Pathophysiol. 2018;91:1–7. doi: 10.4291/wjgp.v9.i1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mohammad Alizadeh AH. Cholangitis: diagnosis, treatment and prognosis. J Clin Transl Hepatol. 2017;4:404–413. doi: 10.14218/JCTH.2017.00028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lim CH, Jahansouz C, Freeman ML, et al. Outcomes of endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy for suspected sphincter of Oddi dysfunction (SOD) post Roux-en-Y gastric bypass. Obes Surg. 2017;10:2656–2662. doi: 10.1007/s11695-017-2696-4. [DOI] [PubMed] [Google Scholar]
- 20.Sugawa C, Brown KL, Matsubara T, et al. The role of endoscopic biliary sphincterotomy for the treatment of type 1 biliary dysfunction (papillary stenosis) with or without biliary stones. Am J Surg. 2014;1:65–69. doi: 10.1016/j.amjsurg.2013.04.007. [DOI] [PubMed] [Google Scholar]
- 21.ASGE Standards of Practice Committee, Chathadi KV, Chandrasekhara V, Acosta RD, et al.Sugawa C, Brown KL, Matsubara T, et al. The role of ERCP in benign diseases of the biliary tract. Gastrointest Endosc Clin N Am. 2015;4:795–803. doi: 10.1016/j.gie.2014.11.019. [DOI] [PubMed] [Google Scholar]
- 22.Small AJ, Kozarek RA. Sphincter of Oddi dysfunction. Gastrointest Endosc Clin N Am. 2015;4:749–763. doi: 10.1016/j.giec.2015.06.009. [DOI] [PubMed] [Google Scholar]
- 23.Craig AG, Toouli J. Slow release nifedipine for patients with sphincter of Oddi dyskinesia: results of a pilot study. Intern Med J. 2002;3:119–120. [PubMed] [Google Scholar]
- 24.Kyanam Kabir Baig KR, Wilcox CM. Translational and clinical perspectives on sphincter of Oddi dysfunction. Clin Exp Gastroenterol. 2016;9:191–195. doi: 10.2147/CEG.S84018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nakeeb A. Sphincter of Oddi dysfunction: how is it diagnosed? How is it classified? How do we treat it medically, endoscopically and surgically? J Gastrointest Surg. 2013;9:1557–1558. doi: 10.1007/s11605-013-2280-8. [DOI] [PubMed] [Google Scholar]
- 26.Freeman ML, Gill M, Overby C, Cen YY. Predictors of outcomes after biliary and pancreatic sphincterotomy for sphincter of oddi dysfunction. J Clin Gastroenterol. 2007;1:94–102. doi: 10.1097/01.mcg.0000225584.40212.fb. [DOI] [PubMed] [Google Scholar]
- 27.Afghani E, Lo SK, Covington PS, Cash BD, Pandol SJ. Sphincter of Oddi function and risk factors for dysfunction. Front Nutr. 2017;4:1. doi: 10.3389/fnut.2017.00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wilcox CM. Sphincter of Oddi dysfunction Type III: New studies suggest new approaches are needed. World J Gastroenterol. 2015;19:5755–5761. doi: 10.3748/wjg.v21.i19.5755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chang HY, Wang CJ, Liu B, et al. Ursodeoxycholic acid combined with percutaneous transhepatic balloon dilation for managementof gallstones after elimination of common bile duct stones. World J Gastroenterol. 2018;39:4489–4498. doi: 10.3748/wjg.v24.i39.4489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kimura Y1, Takada T, Kawarada Y, et al. Definitions, pathophysiology, and epidemiology of acute cholangitis and cholecystitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg. 2007;1:15–26. doi: 10.1007/s00534-006-1152-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lehmann S, Ferrie S, Carey S. Nutrition Management in Patients with Chronic Gastrointestinal Motility Disorders: A Systematic Literature Review. Nutr Clin Pract. 2019. [DOI] [PubMed]
- 32.Miura F, Okamoto K, Takada T, et al. Tokyo Guidelines 2018: initial management of acute biliary infection and flowchart for acute cholangitis. J Hepatobiliary Pancreat Sci. 2018;1:31–40. doi: 10.1002/jhbp.509. [DOI] [PubMed] [Google Scholar]
- 33.Mazuski JE, Tessier JM, May AK, et al. The Surgical Infection Society Revised Guidelines on the Management of Intra-Abdominal Infection. Surg Infect. 2017;1:1–76. doi: 10.1089/sur.2016.261. [DOI] [PubMed] [Google Scholar]
- 34.Reshetnyak VI. Concept of the pathogenesis and treatment of cholelithiasis. World J Hepatol. 2012;2:18–34. doi: 10.4254/wjh.v4.i2.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lehmann S, Ferrie S, Carey S. Nutrition Management in Patients with Chronic Gastrointestinal Motility Disorders: A Systematic Literature Review. Nutr Clin Pract. 2019. [DOI] [PubMed]