Abstract
This paper investigates the associations between social relationships, age and the use of preventive health services among German adults. Data stem from the German Ageing Survey (10,324 respondents). The use of preventive health services was assessed by asking for regular use of flu vaccination and cancer screening in the past years. Predictors of interest were structural (having a partner, size of the social network) and functional aspects of social relationships (perceived informational support) and age. Logistic regression models were used to measure the associations between preventive health services use and these predictors. Self-perceived health, gender and education were considered as covariates. Having a partner (OR = 1.20, 95% CI: 1.07–1.34) and perceived informational support (OR = 1.38, 95% CI: 1.13–1.69) were associated with a higher probability of getting flu vaccination regularly over the past years. Informational support (OR = 1.42, 95% CI: 1.17–1.72) and having a partner (OR = 1.57, 95% CI: 1.41–1.75) were positively associated with regular cancer screening over the past years. Associations between the size of the social network and use of preventive health services were not statistically significant. Associations between the use of preventive health services and social relationships varied by age. Structural and functional aspects of social relationships may support preventive health behavior. To increase preventive health behavior and the use of preventive health services, it is necessary to integrate information on social relationships into routine care and to strengthen sources of social support.
Keywords: preventive health services, cancer screening, flu vaccination, social relationships, social networks, informational support, partner, age
1. Introduction
One of the tasks of the statutory health insurance in Germany is to prevent diseases and to promote health and healthy ageing regardless of peoples’ gender and social status [1]. Ageing populations with changing health needs and chronic conditions are associated with a rising demand for health services [2]. Some disorders can be prevented or influenced positively by preventive interventions [3]. Primary prevention aims at reducing the risk of the onset of a disease. Flu vaccinations, for example, are part of primary prevention, since they have the capability to obviate different serious infectious diseases and to prevent unnecessary hospitalizations and premature deaths [3,4]. Secondary prevention aims at detecting and treating diseases as early as possible. In the case of cancer, screening is especially important, since cancer is responsible for a vast number of deaths worldwide [5].
Following the ‘Behavioral Model of Health Services Use’ by Andersen, use of health services, a measure for health care access, is connected to a multitude of predisposing (e.g., age and gender), enabling (e.g., education, income and social status) and need characteristics (e.g., disease, symptoms and pain) [6]. Various studies showed that Andersen’s framework also applies to the use of preventive health services [7,8,9,10]. For cancer screenings, different patterns of usage could be identified depending on sociodemographic features [11,12,13,14,15], health needs [16,17,18] and socioeconomic or psychological factors [11,14,19,20,21,22,23,24,25,26]. The use of flu vaccinations also varies by sociodemographic factors [27,28], health status [4,28] and socioeconomic characteristics [29,30,31]. Since preventive health services are recommended by health authorities and paid for certain ages and risk groups by the statutory health insurance in Germany, age (as a predisposing characteristic) plays an important role regarding the use of cancer screenings and flu vaccinations [6]. From the age of 50, for example, the statutory health insurance pays for mammography screenings every two years [32]. For men, reaching the age of 45, the yearly use of prostate screenings is covered by the statutory health insurance [32]. Statutory health insurance also covers colorectal cancer screening starting with 50 years of age for both sexes [32]. Flu vaccination is a paid service for everybody and recommended for individuals aged 60 and older. Consequently, health institutions are interested in higher rates of preventive health services use reaching certain ages. In Germany, the Federal Joint Committee (G-BA) decides which health and preventive health services (e.g., early detection programs on cancer) are covered by the statutory health insurance [33]. “In its assessments, the G-BA examines patient benefit […]. Patient benefit is defined as recovery, relief from pain or discomfort, improvement in quality of life, extension of life, or reduction of side effects” [33]. The age limits of preventive health services are part of the G-BA assessment.
Within the Behavioral Model of Andersen, enabling resources (e.g., education and family) can play a supportive role in the sense of creating potential access and foster realized access to health services [6]. Enabling resources also include the social environment, such as social relationships, that are known to be connected to health, health promotion and the use of health services [6,34,35,36]. Social relationships are characterized by the individuals’ social support, social influence, social engagement and attachment, and have an impact on how they access resources [37]. In addition, international studies have shown that social relationships have a considerable influence on morbidity and mortality [38,39]. Social relationships comprise structural and functional elements [38]. Structural aspects are assessed by quantitative measures (e.g., living arrangements, social network size and frequency of social participation). Functional aspects include elements of financial, instrumental, informational or emotional support.
To date, few international studies investigated the use of preventive health services in conjunction with dimensions of social relationships [40,41,42,43,44,45]. However, it is not clear how structural and functional aspects of social relationships are linked to preventive health services. Furthermore, it has not been investigated to which extent social relationships do have an impact on the link between age and preventive health services. Therefore, this paper investigates the associations between social relationships, age and the use of preventive health services among German adults aged forty years and older.
2. Materials and Methods
2.1. Data
Data stem from the public release of the fifth wave, in 2014, of the German Ageing Survey (DEAS), provided by the Research Data Centre of the German Centre of Gerontology (DZA) and funded by the Federal Ministry for Family Affairs, Senior Citizens, Women and Youth (BMFSFJ) [46,47]. The population-based survey started in 1996 and included and was representative for individuals 40 years and older in Germany. After the initial survey, other waves followed in 2002, 2008, 2011 and 2014. The interviews covered information on health, occupational status, income, social relationships, life events, psychological well-being and much more [48]. In the fifth wave (2014) 7952 individuals filled out the ‘drop-off’ questionnaire, a questionnaire which was filled by the respondents without an interviewer. Due to panel attrition, each wave introduced new respondents to ‘refresh’ and to stabilize the absolute number of respondents in the sample. As such, 4295 individuals are part of this so-called refreshers sample (54%). The drop-off questionnaire contained items on the use preventive health services (cancer screening and flu vaccination). The response rate of the sample was 61% in 2014. These rates are comparable to other surveys executed in Germany [49]. Our analyses are based on the fifth wave of the German Ageing Survey which included cross-sectional data on perceived informational support, having a partner and social network size for a representative sample of the middle-aged and older population of Germany [49]. A written informed consent was given by every survey participant prior to the interview. The survey respected the Declaration of Helsinki [50].
2.2. Measures
The use of preventive health services was assessed by asking for regular use of flu vaccination and cancer screening in the past years (no, yes). The predictors in focus were structural (having a partner, size of the social network) and functional aspects of social relationships (perceived informational support) and age. Having a partner was dichotomized (0 ‘having no partner’, 1 ‘having a partner’). ‘Having no partner’ includes singles, divorced, widowed and separated individuals. ‘Having a partner’ is defined by married people and registered partnerships living together. Size of the social network was assessed by asking for ‘people who are important to you and who you maintain regular contact with’. ‘These can include co-workers, neighbors, friends, acquaintances, relatives, and members of your household. Which people are important to you?’ (the respondents could name the people; the names were counted and coded as 0 ‘no one’ to 9 ‘nine or more people’). Perceived informational support was measured by asking ‘When you have important personal decisions to make, do you have anyone you can ask for advice?’ (0 ‘no’, 1 ‘yes’). Age was measured in years.
Health indicators and other socio-demographic factors were included as covariates. In the current study, self-perceived health (‘How would you rate your present state of health?’) was measured on a five-point scale (1 ‘very good’, 2 ‘good’, 3 ‘average’, 4 ‘bad’ and 5 ‘very bad’) as one health indicator. Furthermore, we included information on pre-existing diseases by taking into account the number of diseases (‘Which of the following diseases and health problems do you have?’). The list of diseases covered fourteen chronic, somatic illnesses, for example, cardiac and circulatory disorders, respiratory problems/ asthma/ shortness of breath, cancer or diabetes. The respondent’s sex was coded by male (= 0) and female (= 1). Education was based on the International Standard Classification of Education (ISCED 1997) and ranged from 1 to 3 (low to higher education). Low education is defined by ISCED 0–2 (= respondents without formal vocational qualification). Medium education based on ISCED 3–4 (= respondents with vocational training including respondents with higher general school certificate without professional training. Higher education represented ISCED 5–6 (= respondents with completed university studies or with completed professional development training).
2.3. Analyses
Since the two dependent variables “use of preventive health services” (flu vaccination and cancer screening) are binary (no/yes), two logistic regression models were used to measure the associations between each type of preventive health services use and the predictors (flu vaccination = model 1; cancer screening = model 2). To adjust for disproportional stratifications of the baseline sample and selective panel mortality, weights were used [46,51,52]. To analyze a potential moderation of social relationships on the association between age and the two types of preventive health services, two-way interaction terms were introduced [53]. Three interaction terms were calculated for each of the two types of preventive health services: (1) age * informational support (model 1.1 and model 2.1), (2) age * having a partner (model 1.2 and model 2.2) and (3) age * social network size (model 1.3 and 2.3). In terms of cancer screening, age is added as cubic term to the model, since the relationship between the probability of using cancer screening and age was found to be non-linear. We defined p < 0.05 as threshold whether an association was considered statistically significant or not. The analyses were performed with Stata 12 [54] and were replicated with R 3.6.1 [55]. Marginal effects plots were created using the ggeffects-package 0.12.0 [56].
3. Results
Table 1 shows that 42.5% of the respondents used flu vaccinations regularly in the past years, and 63.3% used cancer screenings. Additionally, 69.9% of the respondents had a partner and 93% reported informational support. On average, social networks included 5.2 important persons with regular contact. More than half of the participants were female and the mean age was 64.5 years. Results also show that 51.6% attained a higher education (ISCED-1997 Coding) and 53.7% reported a good or very good health. On average, respondents reported 2.6 physical diseases.
Table 1.
Descriptive statistics of the sample by drop-off questionnaire (n = 7952, (German Ageing Survey), 2014).
| Variables | N (%), Mean (SD) |
|---|---|
| Female: N (%) | 4056 (51.01) |
| Age: Mean (SD) | 64.54 (11.24) |
| Education a (ISCED-1997 Coding): N (%) | |
| ISCED-1: low | 521 (6.55) |
| ISCED-2: medium | 4100 (51.56) |
| ISCED-3: high | 3329 (41.86) |
| Self-perceived health b: N (%) | |
| Very good | 641 (8.06) |
| Good | 3631 (45.66) |
| Average | 2857 (35.93) |
| Bad | 670 (8.43) |
| Very bad | 145 (1.82) |
| Number of physical diseases c : Mean (SD) | 2.6 (1.89) |
| Having a partner (= yes)d: N (%) | 5556 (69.87) |
| Social network size: Mean (SD) | 5.22 (2.70) |
| Perceived informational support (= yes) e: N (%) | 7396 (93.01) |
| Regular flu vaccination in the past years (= yes) f: N (%) | 3383 (42.54) |
| Regular cancer screening in the past years (= yes) g: N (%) | 5034 (63.30) |
| Missing values (out of 7952): a 1, b 8, c 148, d 16, e 22, f 202, g 279 |
a: 1 missing value (mv), b: 8 mv, c: 148 mv, d: 16 mv, e: 22 mv, f: 202 mv, g: 279 mv.
3.1. Associations between Social Relationships, Age and Preventive Health Services Use
Having a partner (OR = 1.20, 95% CI: 1.07–1.34) and perceived informational support (OR = 1.38, 95% CI: 1.13–1.69) were associated with a higher probability of getting flu vaccination regularly over the past years (Table 2). There was no statistically significant association between the size of the social network and flu vaccination. The probability of using flu vaccination increased by age (OR = 1.06, 95% CI: 1.05–1.06). Reporting a very good (OR = 0.50, 95% CI: 0.40–0.62) or good (OR = 0.73, 95% CI: 0.65–0.82) health was associated with a lower probability of getting flu vaccination regularly, whereas a very bad self-perceived health (OR = 1.70, 95% CI: 1.20–2.40) was connected to a higher probability. Furthermore, the probability of using flu vaccination increased by the number of reported physical diseases (OR = 1.08, 95% CI: 1.04–1.11).
Table 2.
Logistic regression models for flu vaccination (Model 1) and cancer screening (Model 2) (German Ageing Survey, 2014).
| Variables | Seasonal Flu Vaccination (Model 1) | Cancer Screening (Model 2) | ||
|---|---|---|---|---|
| Predictors | Odds Ratio | 95% CI | Odds Ratio | 95% CI |
| Partner (Ref. no): yes | 1.20 | 1.07–1.34 | 1.57 | 1.41–1.75 |
| Social network size (number of important persons with regular contact) | 0.99 | 0.97–1.01 | 1.02 | 1.00–1.04 |
| Informational support (Ref. no): yes | 1.38 | 1.13–1.69 | 1.42 | 1.17–1.72 |
| Gender (Ref. male): female | 1.03 | 0.93–1.15 | 2.38 | 2.14–2.64 |
| Age in years | 1.06 | 1.05–1.06 | 1.34 | 1.29–1.40 |
| Age in years (cubic term) | 1.00 | 1.00–1.00 | ||
| Education (ISCED-1997) (Ref. ISCED-2: medium) | ||||
| ISCED-1: low | 0.89 | 0.75–1.06 | 0.87 | 0.73–1.04 |
| ISCED-3: high | 1.03 | 0.93–1.15 | 1.14 | 1.02–1.27 |
| Self-perceived health (Ref. average) | ||||
| Very good | 0.50 | 0.40–0.62 | 0.78 | 0.64–0.95 |
| Good | 0.73 | 0.65–0.82 | 1.07 | 0.95–1.20 |
| Bad | 1.07 | 0.89–1.29 | 0.78 | 0.65–0.94 |
| Very bad | 1.70 | 1.20–2.40 | 0.77 | 0.55–1.08 |
| Number of physical diseases | 1.08 | 1.04–1.11 | 1.05 | 1.01–1.08 |
| Intercept | 0.01 | 0.01–0.02 | 0.00 | 0.00–0.00 |
| Number of observations | 7588 | 7515 | ||
Respondents with perceived informational support (OR = 1.42, 95% CI: 1.17–1.72) and having a partner (OR = 1.57, 95% CI: 1.41–1.75) were more likely to use cancer screening (Table 2). The odds ratios of the size of the social network and of education on using cancer screenings were not statistically significant. Furthermore, we found a statistically significant relationship between age and the use of cancer screening (age: OR = 1.34, 95% CI: 1.29–1.40; age 2: OR = 1.00, 95% CI: 1.00–1.00). Age was positively associated with the use of cancer screening up to around 63 years. However, ageing 63 and older the association is negative. Individuals with a higher education (OR = 1.14, 95% CI: 1.02–1.27) were more likely to utilize cancer screening. Moreover, reporting a very good health (OR = 0.78, 95% CI: 0.64–0.95) or a bad health status (OR = 0.78, 95% CI: 0.65–0.94) was associated with a lower probability of getting cancer screenings regularly. Furthermore, the probability of using cancer screening slightly increased by the number of reported physical diseases (OR = 1.05, 95% CI: 1.01–1.08).
3.2. Moderation of Social Relationships on Age and Preventive Health Services Use
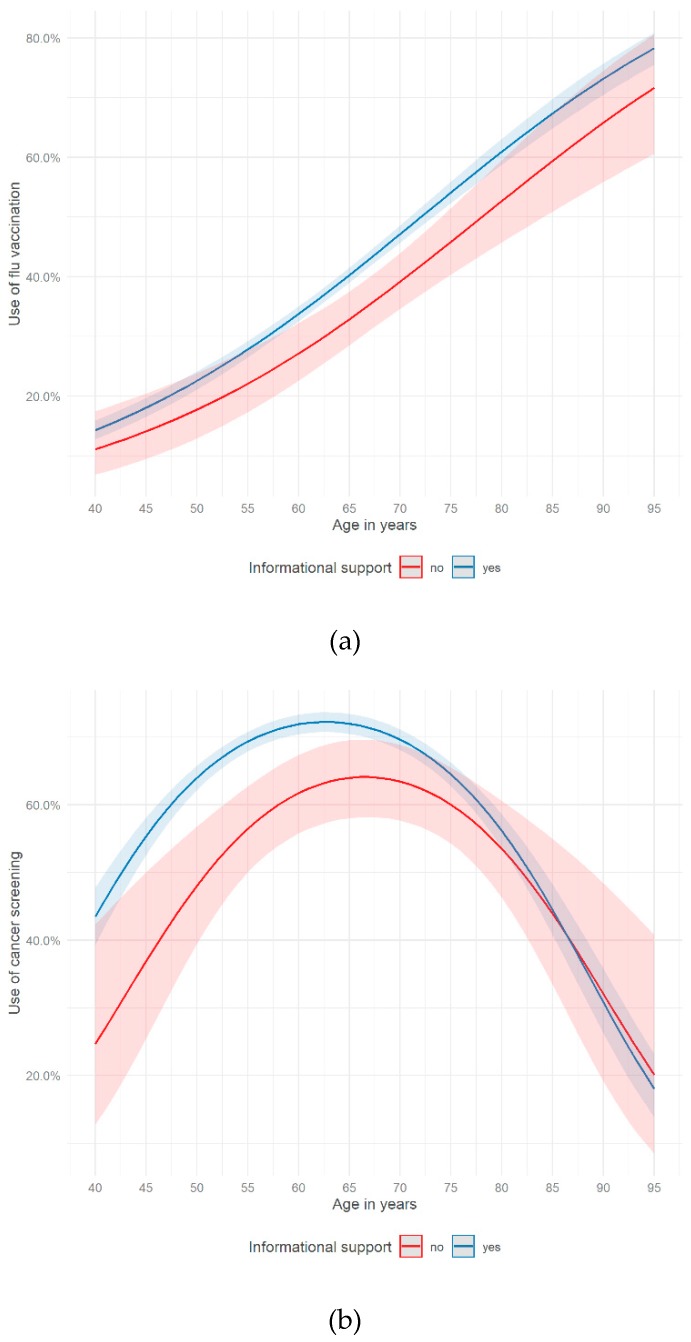
The associations between the use of preventive health services (flu vaccination, cancer screening) and age varied by social relationships (having a partner, perceived informational support). The proportion of respondents using flu vaccination increased by age. We found a difference if someone perceived informational support or not for the age group of 60 to 75 years old (Figure 1a). Within that age group, respondents who perceived informational support showed a significantly higher chance of getting flu shots. The proportion of people using cancer screening increased within the age group of 40 to 65 years, then decreasing constantly until the age of 95 (Figure 1b). The chance of using cancer screenings is significantly higher for people aged 43 to 66 if they perceived informational support.
Figure 1.
Use of (a) flu vaccination (Model 1.1) and (b) cancer screening (Model 2.1) on age and informational support (German Ageing Survey, 2014).
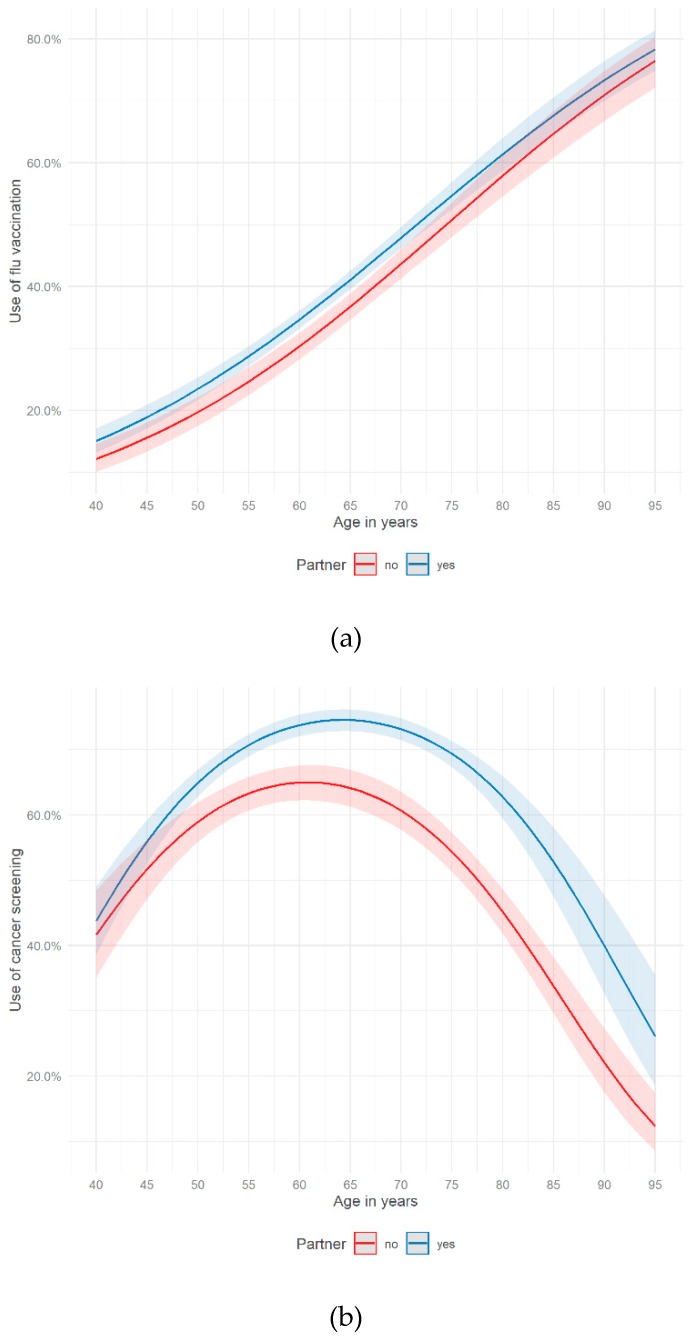
Figure 2a shows the use of flu vaccination by age and having a partner. People having a partner only had a slightly higher chance of using flu shots than people without a partner. In both groups, the proportion of demanding flu vaccination increased by age. For cancer screenings, Figure 2b shows a different picture. From 50 up to 95 years, the ratio of people using cancer screening was higher if respondents reported having a partner. The highest proportion of cancer screening users could be measured at 65 years if a partner was present (75%) and at around 60 years if not having a partner (65%).
Figure 2.
Use of (a) flu vaccination (Model 1.2.) and (b) cancer screening (Model 2.2.) on age and having a partner (German Ageing Survey, 2014).
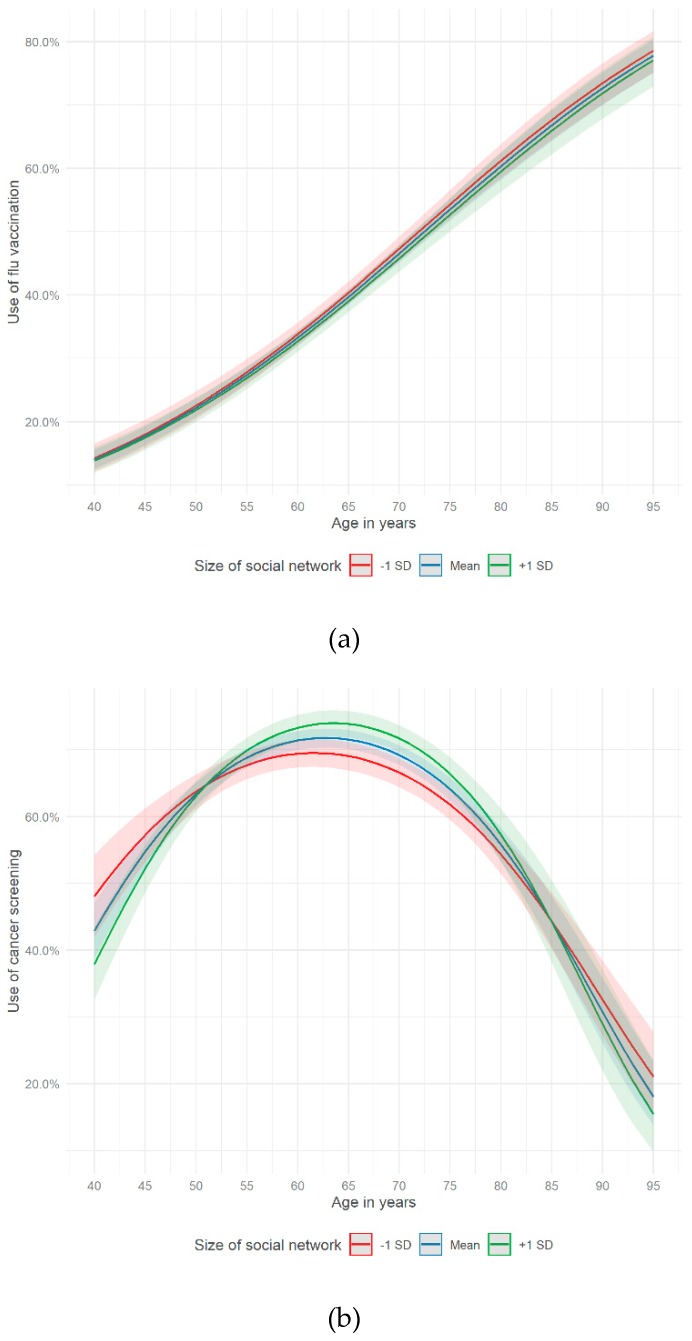
Figure 3a,b do not show any major differences in using preventive health services (flu vaccination and cancer screening) taking age and the size of the social network into account. Merely, the use of cancer screenings demonstrated some small gaps between the subgroups (of social network size) in certain age intervals (Figure 3b). The general curve characteristics in Figure 3a,b were similar to the figures above.
Figure 3.
Use of (a) flu vaccination (Model 1.3) and (b) cancer screening (Model 2.3) on age and social network size (German Ageing Survey, 2014).
The figures, shown above, based on interaction models which are presented in the supplementary material (Table S1).
4. Discussion
4.1. Summary
This study revealed that a functional aspect of social relationships (perceived informational support) was associated with a higher probability of using flu vaccination and cancer screening in a German sample of people aged 40 years and older. The association between one structural factor of social relationships and the use of preventive health services was statistically significant (having a partner), the other one was not (size of the social network). Moreover, the probability of using flu vaccination increased by age. Considering the use of cancer screening, the odds were increasing by age among those aged 40 to 63. After the age of 63 people were less likely to use cancer screening. Potentially, this observation could be partly explained by recommended age limits with regard to certain cancer screening types in Germany (e.g., colon, rectum and mammography screening) [57]. Furthermore, the associations between the use of preventive health services and age varied by different dimensions of social relationships. With regards to the use of flu vaccination, perceiving informal support seems to be a supportive factor especially for the age of 60 to 75. This held also true for people in their early 40s up to 66 with regard to cancer screening. Having a partner seemed to encourage the use of cancer screening, especially for people aged 50 years and older.
Kinney, Bloor, Martin et al. reported that people who were structurally well integrated, had a higher chance of reporting recent use of colorectal cancer screening [41]. Functional and instrumental support, representing functional aspects of social relationships, were not associated with the use of colorectal cancer screening. While the findings on the positive association between social relationships and cancer screening were in line with our results, we also found statistically significant associations between functional aspects of social ties and preventive health services. Allen, Sorensen, Stoddard et al. investigated the relationship between social network characteristics and breast cancer screening among employed women [40]. In their multivariable analyses, social network characteristics did not predict using regular screening. Only the perception that screening is socially desirable led to increased usage. Potentially, our results on social network size could be in line with these findings. Suarez, Ramirez, Villareal et al. formed an index on social integration including structural and functional elements of social relationships (number of close relatives and friends, frequency of contact, church membership) and linked it to various types of cancer screenings among four U. S. Hispanic groups (Mexican, Central-American, Cuban and Puerto Rican) [42]. Their results showed a complex picture of no, weak and strong associations depending on the type of screening and the four Hispanic groups.
Like other studies, we found that age was associated with vaccination uptake [58,59]. Being married or living with others has been associated with vaccination acceptance in some studies [60,61]. Furthermore, several studies on barriers and facilitators of getting influenza immunization indicated that advice from and health discussions with family and friends may trigger the acceptance and use of flu vaccination [43,44,45,62]. Consequently, our results concerning the positive associations between functional aspects of social relationship could support and add to the existing literature on social ties and the use of flu vaccination.
All in all, functional and structural aspects of social relationships were associated with a higher probability of using preventive health services. Living in a partnership and perceiving informational support seem to enable individuals to access preventive health services and to support their preventive health behavior. Furthermore, the results showed that age played a crucial role in using preventive health services. In the age curves of preventive health services, fundamental differences between flu vaccination and cancer screening could be shown. While the age curve of flu vaccination almost showed a linear trend, the age curve of cancer screening was concave. The moderator analyses showed that social relationships moderate the link between age and the use of preventive health services. In the case of flu vaccination, individuals, aged 60–75 and perceiving informational support, had a higher chance of use. With regard to cancer screening, informational support increased the probability of use in the age group 43–66 and living in a partnership promoted the chance of use among those 50 years and older. Consequently, functional and structural aspects of social relationships seem to have the potential to enable the use of preventive health services, especially of cancer screening.
4.2. Limitations
Methodological limitations need to be taken into account, when interpreting the results. Due to changes of the measurement of preventive health services between the waves of the German Ageing Survey, only cross-sectional data were used for the analyses [48]. Therefore, it is not possible to comment on changes over time and causal directions. Secondly, the items on using preventive health services were based on self-reports and on a rather vague time span by asking for regular use of flu vaccination and cancer screening in the past years. The time span covering the preventive health services can be quite long, and considering the older age of some respondents, risk of memory bias could be existent regarding the use of preventive health services [63]. Moreover, the item on using cancer screening did not specify which type of cancer screening was meant. It was formulated in general terms. Consequently, further subgroup analyses were not possible. Moreover, the German Ageing Survey did not provide information on the motives for using preventive health services, their quality and adequacy. Consequently, our preventive health services item represents a proxy for “realized access” [6] only.
Besides methodological limitations, there is an ongoing debate on the effectiveness or harmfulness of preventive health services, especially, concerning cancer screenings and flu vaccination [64,65,66]. It is important to keep that in mind, when discussing the use of preventive health services in general. Simonsen et al. questioned the effectiveness of flu vaccination, for example, concerning mortality benefits of flu vaccination in elderly people, since frailty selection bias, the use of non-specific endpoints could have resulted in exaggerating vaccine benefits in cohort studies [66]. They conclude that “the remaining evidence base is currently insufficient to indicate the magnitude of the mortality benefit, if any, that elderly people derive from the vaccination programme” [66]. Furthermore, flu vaccination may have side-effects for health. Kwok stated that “vaccines do carry risks, ranging from rashes or tenderness at the site of injection to fever-associated seizures […] and dangerous infections in those with compromised immune systems” [67], although severe complications are unusual and it is difficult to show that a vaccine is the cause for them [67]. With regard to the controversy over cancer screenings, radiation risks are one part of it [64]. The controversy also includes arguments on over-treatment and over-diagnosis of cancer. Esserman et al. noted that “screening and patient awareness have increased the chance of identifying a spectrum of cancers, some of which are not life threatening. Policies that prevent or reduce the chance of overdiagnosis and avoid overtreatment are needed, while maintaining those gains by which early detection is a major contributor to decreasing mortality and locally advanced disease” [68].
Concepts of social relationships which were used in our study (having a partner, informational support and social network size) were only indirect measures of structural (having a partner, social network size) and functional aspects (informational support) of social relationships. Especially, the partner variable or the size of social networks were only rough measures for social connectedness and the feeling for belonging and being cared for. Our data did not include information on the qualitative partnership or social network functioning which could be differentiated into costs (e.g., psychological distress, destructive conflicts) and benefits (e.g., belonging, meaning). Since social relationships could have positive and negative aspects, they could lead to different health and health behavior outcomes [69]. Although the indirect approach (referring on socio-demographic proxies) and the direct approach (linking meaningfulness and importance to social relations) are used in the German Ageing Survey, specific information about the quality of social relationships and the level of social support were missing [70].
5. Conclusions
Having a partner and perceived informational support were associated with a higher probability of using preventive health services. The social environment, like structural and functional aspects of social relationships, may support preventive health behavior, especially within certain age groups (flu vaccination: informational support and age of 60–75; cancer screening: informational support and age of 43–66, having a partner and age of 50–95). If health policy and health professionals want to increase preventive health behavior and the use of preventive health services, it is necessary to integrate information on social relationships into routine care and to strengthen sources of social support.
Acknowledgments
Data stem from the public release of the German Ageing Survey (DEAS), provided by the Research Data Centre of the German Centre of Gerontology (DZA) and funded by the Federal Ministry for Family Affairs, Senior Citizens, Women and Youth (BMFSFJ). The analysis refers to the following datasets: SUF DEAS 2014, version 1.0, DOI: 10.5156/DEAS.2014.M.001. Web link: https://www.dza.de/en/fdz/german-ageing-survey/data/data-of-survey-year-2014.html. The DEAS data is available after signing a user contract for research purposes. Publications including DEAS data require reference to the used datasets.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/16/21/4272/s1, Table S1: Interaction models.
Author Contributions
D.B., D.L. and O.v.d.K. developed the research questions. D.B. prepared, analyzed and interpreted the data, and drafted and finalized the manuscript. D.L. made an essential contribution to data analyses and interpretation, drafting the manuscript, and critically revised and approved the final manuscript. O.v.d.K. substantially contributed to interpreting the data, drafting the manuscript, and critically revised and approved the final manuscript.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interest
References
- 1.GKV-Spitzenverband H. Leitfaden Prävention. Handlungsfelder und Kriterien des GKV-Spitzenverbandes zur Umsetzung von. [(accessed on 25 October 2019)];2010 Available online: https://www.zentrale-pruefstelle-praevention.de/admin/download.php?dl=leitfaden.
- 2.Beaglehole R., Irwin A., Prentice T., Organization WH . The World Health Report 2003: Shaping the Future. World Health Organization; Geneva, Switzerland: 2003. [Google Scholar]
- 3.Federal Ministry of Health Prevention 2015. [(accessed on 25 October 2019)]; Available online: https://www.bundesgesundheitsministerium.de/service/begriffe-von-a-z/p/praevention.html.
- 4.Nagata J.M., Hernández-Ramos I., Kurup A.S., Albrecht D., Vivas-Torrealba C., Franco-Paredes C. Social determinants of health and seasonal influenza vaccination in adults ≥ 65 years: A systematic review of qualitative and quantitative data. BMC Public Health. 2013;13:388. doi: 10.1186/1471-2458-13-388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jemal A., Siegel R., Ward E., Hao Y., Xu J., Murray T., Thun M.J. Cancer statistics, 2008. CA Cancer J.Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 6.Andersen R.M. Revisiting the behavioral model and access to medical care: Does it matter? J. Health Soc. Behav. 1995;36:1–10. doi: 10.2307/2137284. [DOI] [PubMed] [Google Scholar]
- 7.Sudano J.J., Jr., Baker D.W. Intermittent lack of health insurance coverage and use of preventive services. Am. J. Public Health. 2003;93:130–137. doi: 10.2105/AJPH.93.1.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Scott T.L., Gazmararian J.A., Williams M.V., Baker D.W. Health literacy and preventive health care use among medicare enrollees in a managed care organization. Med. Care. 2002;40:395–404. doi: 10.1097/00005650-200205000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Newman J.F., Gift H.C. Regular pattern of preventive dental services—A measure of access. Soc. Sci. Med. 1992;35:997–1001. doi: 10.1016/0277-9536(92)90239-M. [DOI] [PubMed] [Google Scholar]
- 10.Stella M.Y., Bellamy H.A., Schwalberg R.H., Drum M.A. Factors associated with use of preventive dental and health services among US adolescents. J. Adolesc. Health. 2001;29:395–405. doi: 10.1016/s1054-139x(01)00252-x. [DOI] [PubMed] [Google Scholar]
- 11.Starker A., Saß A.-C. Inanspruchnahme von Krebsfrüherkennungsuntersuchungen. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz. 2013;56:858–867. doi: 10.1007/s00103-012-1655-4. [DOI] [PubMed] [Google Scholar]
- 12.Spuling S.M., Ziegelmann J.P., Wünsche J. Altern im Wandel. Springer; Wiesbaden, Germany: 2017. Was tun wir für unsere Gesundheit? Gesundheitsverhalten in der zweiten Lebenshälfte; pp. 139–156. [Google Scholar]
- 13.Selvin E., Brett K.M. Breast and cervical cancer screening: Sociodemographic predictors among White, Black, and Hispanic women. Am. J. Public Health. 2003;93:618–623. doi: 10.2105/AJPH.93.4.618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chawla N., Breen N., Liu B., Lee R., Kagawa-Singer M. Asian American women in California: A pooled analysis of predictors for breast and cervical cancer screening. Am. J. Public Health. 2015;105:98–109. doi: 10.2105/AJPH.2014.302250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dickey S.L., Cormier E.M., Whyte I.V.J., Graven L., Ralston P.A. Demographic, social support, and community differences in predictors of African-American and white men Receiving prostate cancer screening in the United States. Public Health Nurs. 2016;33:483–492. doi: 10.1111/phn.12245. [DOI] [PubMed] [Google Scholar]
- 16.Hsia J., Kemper E., Kiefe C., Zapka J., Sofaer S., Pettinger M., Bowen D., Limacher M., Lillington L., Mason E. The importance of health insurance as a determinant of cancer screening: Evidence from the Women’s Health Initiative. Prev. Med. 2000;31:261–270. doi: 10.1006/pmed.2000.0697. [DOI] [PubMed] [Google Scholar]
- 17.Gorin S.S., Heck J.E. Cancer screening among Latino subgroups in the United States. Prev. Med. 2005;40:515–526. doi: 10.1016/j.ypmed.2004.09.031. [DOI] [PubMed] [Google Scholar]
- 18.Richard A., Rohrmann S., Schmid S.M., Tirri B.F., Huang D.J., Güth U., Eichholzer M. Lifestyle and health-related predictors of cervical cancer screening attendance in a Swiss population-based study. Cancer Epidemiol. 2015;39:870–876. doi: 10.1016/j.canep.2015.09.009. [DOI] [PubMed] [Google Scholar]
- 19.Gale C.R., Deary I.J., Wardle J., Zaninotto P., Batty G.D. Cognitive ability and personality as predictors of participation in a national colorectal cancer screening programme: The English longitudinal study of ageing. J. Epidemiol. Community Health. 2015;69:530–535. doi: 10.1136/jech-2014-204888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abuadas M.H., Petro-Nustas W., Albikawi Z.F., Mari M. Predictors of prostate cancer screening intention among older men in Jordan. Int. J. Urol. Nursing. 2017;11:31–41. doi: 10.1111/ijun.12119. [DOI] [Google Scholar]
- 21.Vrinten C., Waller J., Wagner C., Wardle J. Cancer fear: facilitator and deterrent to participation in colorectal cancer screening. Cancer Epidemiol. Prev. Biomark. 2015;24:400–405. doi: 10.1158/1055-9965.EPI-14-0967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wardle J., Robb K., Vernon S., Waller J. Screening for prevention and early diagnosis of cancer. Am. Psychol. 2015;70:119. doi: 10.1037/a0037357. [DOI] [PubMed] [Google Scholar]
- 23.Wardle J., Wagner C., Kralj-Hans I., Halloran S.P., Smith S.G., McGregor L.M., Vart G., Howe R., Snowball J., Handley G., et al. Effects of evidence-based strategies to reduce the socioeconomic gradient of uptake in the English NHS Bowel Cancer Screening Programme (ASCEND): four cluster-randomised controlled trials. Lancet. 2016;387:751–759. doi: 10.1016/S0140-6736(15)01154-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bremer P., Wübker A. Soziale Ungleichheit und Inanspruchnahme Medizinischer und Präventiver Leistungen in Deutschland: eine Empirische Analyse. [(accessed on 25 October 2019)]; Available online: https://www.econstor.eu/bitstream/10419/55524/1/685605523.pdf.
- 25.Jordan S., Lippe E. Teilnahme an verhaltenspräventiven Maßnahmen. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz. 2013;56:878–884. doi: 10.1007/s00103-013-1664-y. [DOI] [PubMed] [Google Scholar]
- 26.Hajek A., Bock J.O., König H.H. The role of general psychosocial factors for the use of cancer screening—Findings of a population-based observational study among older adults in Germany. Cancer Med. 2017;6:3025–3039. doi: 10.1002/cam4.1226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tsutsui Y., Benzion U., Shahrabani S. Economic and behavioral factors in an individual’s decision to take the influenza vaccination in Japan. J. Socio-Econ. 2012;41:594–602. doi: 10.1016/j.socec.2012.05.001. [DOI] [Google Scholar]
- 28.Schmitz H., Wübker A. What determines influenza vaccination take-up of elderly Europeans? Health Econ. 2011;20:1281–1297. doi: 10.1002/hec.1672. [DOI] [PubMed] [Google Scholar]
- 29.Chen J.Y., Fox S.A., Cantrell C.H., Stockdale S.E., Kagawa-Singer M. Health disparities and prevention: racial/ethnic barriers to flu vaccinations. J. Community Health. 2007;32:5–20. doi: 10.1007/s10900-006-9031-7. [DOI] [PubMed] [Google Scholar]
- 30.Carman K.G., Mosca I. Who takes up free flu shots? Examining the effects of an expansion in coverage. De Econ. 2014;162:1–17. doi: 10.1007/s10645-013-9219-z. [DOI] [Google Scholar]
- 31.Tanjani P.T., Babanejad M., Najafi F. Influenza vaccination uptake and its socioeconomic determinants in the older adult Iranian population: A national study. Am. J. Infect. Control. 2015;43:1–5. doi: 10.1016/j.ajic.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 32.German Cancer Society. [(accessed on 25 October 2019)]; Available online: https://www.krebsgesellschaft.de/onko-internetportal/basis-informationen-krebs/vorsorge-und-frueherkennung/krebsfrueherkennungsuntersuchungen-fuer-maenner.html.
- 33.Federal Joint Committee The Federal Joint Committee - Decisions on Healthcare Benefits. [(accessed on 25 October 2019)]; Available online: https://www.g-ba.de/downloads/17-98-3769/2018-12-12_G-BA_Infobrosch%C3%BCre_EN_bf.pdf.
- 34.Berkman L.F. The role of social relations in health promotion. Psychosom. Med. 1995;57:245–254. doi: 10.1097/00006842-199505000-00006. [DOI] [PubMed] [Google Scholar]
- 35.Bremer D., Lüdecke D., Vonneilich N., von dem Knesebeck O. Social relationships and GP use of middle-aged and older adults in Europe: A moderator analysis. BMJ Open. 2018;8:e018854. doi: 10.1136/bmjopen-2017-018854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bremer D., Inhestern L., von dem Knesebeck O. Social relationships and physician utilization among older adults—A systematic review. Plos One. 2017;12:e0185672. doi: 10.1371/journal.pone.0185672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Berkman L.F., Glass T., Brissette I., Seeman T.E. From social integration to health: Durkheim in the new millennium. Soc. Sci. Med. 2000;51:843–857. doi: 10.1016/S0277-9536(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 38.Holt-Lunstad J., Smith T.B., Layton J.B. Social relationships and mortality risk: a meta-analytic review. PLOS Med. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hemingway H., Marmot M. Psychosocial factors in the aetiology and prognosis of coronary heart disease: systematic review of prospective cohort studies. BMJ. 1999;318:1460–1467. doi: 10.1136/bmj.318.7196.1460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Allen J.D., Sorensen G., Stoddard A.M., Peterson K.E., Colditz G. The relationship between social network characteristics and breast cancer screening practices among employed women. Ann. Behav. Med. 1999;21:193–200. doi: 10.1007/BF02884833. [DOI] [PubMed] [Google Scholar]
- 41.Kinney A.Y., Bloor L.E., Martin C., Sandler R.S. Social ties and colorectal cancer screening among Blacks and Whites in North Carolina. Cancer Epidemiol. Prev. Biomark. 2005;14:182–189. [PubMed] [Google Scholar]
- 42.Suarez L., Ramirez A.G., Villarreal R., Marti J., McAlister A., Talavera G.A., Trapido E., Perez-Stable E.J. Social networks and cancer screening in four US Hispanic groups. Am. J. Prev. Med. 2000;19:47–52. doi: 10.1016/S0749-3797(00)00155-0. [DOI] [PubMed] [Google Scholar]
- 43.Kwong E.W., Lam I.O., Chan T.M. What factors affect influenza vaccine uptake among community-dwelling older Chinese people in Hong Kong general outpatient clinics? J. Clin Nurs. 2009;18:960–971. doi: 10.1111/j.1365-2702.2008.02548.x. [DOI] [PubMed] [Google Scholar]
- 44.Lau L., Lau Y., Lau Y.H. Prevalence and correlates of influenza vaccination among non-institutionalized elderly people: an exploratory cross-sectional survey. Int. J. Nurs. Stud. 2009;46:768–777. doi: 10.1016/j.ijnurstu.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nyhan B., Reifler J., Richey S. The role of social networks in influenza vaccine attitudes and intentions among college students in the southeastern United States. J. Adolesc. Health. 2012;51:302–304. doi: 10.1016/j.jadohealth.2012.02.014. [DOI] [PubMed] [Google Scholar]
- 46.Engstler H., Hameister N., Schrader S. German Ageing Survey (DEAS): User Manual SUF DEAS2014, Version 1.0. [(accessed on 25 October 2019)];2017 Available online: https://www.ssoar.info/ssoar/bitstream/handle/document/63346/ssoar-2019-engstler_et_al-German_Ageing_Survey_DEAS_User.pdf?sequence=1&isAllowed=y&lnkname=ssoar-2019-engstler_et_al-German_Ageing_Survey_DEAS_User.pdf.
- 47.FDZ-DZA German Aging Survey. [(accessed on 25 October 2019)]; Available online: https://www.dza.de/en/fdz/german-ageing-survey/data.html.
- 48.Engstler H., Groh A., Klaus D., Mahne K., Spuling S., Wetzel M., Wolff J.K., Tesch-Romer C. German Ageing Survey (DEAS): Instruments of the Fifth Wave 2014. [(accessed on 25 October 2019)]; Available online: https://www.dza.de/fileadmin/dza/pdf/fdz/DEAS2014_Instruments.pdf.
- 49.Klaus D., Engstler H. Altern im Wandel. Springer; Wiesbaden, Germany: 2017. Daten und methoden des deutschen alterssurveys; pp. 29–45. [Google Scholar]
- 50.Association W.M. World medical association declaration of helsinki: Ethical principles for medical research involving human subjects. JAMA. 2013;310:2191. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 51.Tesch-Römer C., Engstler H., Wurm S. Altwerden in Deutschland: Sozialer Wandel und Individuelle Entwicklung in der zweiten Lebenshälfte. Springer; Wiesbaden, Germany: 2009. [Google Scholar]
- 52.Motel-Klingebiel A., Wurm S., Tesch-Römer C. Altern im Wandel: Befunde des Deutschen Alterssurveys (DEAS) Kohlhammer; Stuttgart, Germany: 2010. [Google Scholar]
- 53.Baron R.M., Kenny D.A. The moderator–mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J. Personal. Soc. Psychol. 1986;51:1173. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 54.StataCorp Announcing Stata Release 12: Stata 12. [(accessed on 25 October 2019)]; Available online: https://www.stata.com/news/statanews.26.2.pdf.
- 55.Team, R.C. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; Vienna, Austria: 2013. [(accessed on 25 October 2019)]. Available online: https://www. R-project. org. [Google Scholar]
- 56.Lüdecke D. Ggeffects: Tidy data frames of marginal effects from regression models. J. Open Source Softw. 2018;3:772. doi: 10.21105/joss.00772. [DOI] [Google Scholar]
- 57.Federal Ministry of Health Health Promotion and Prevention for Elderly People. [(accessed on 25 October 2019)]; Available online: https://www.bundesgesundheitsministerium.de/themen/praevention/frueherkennung-vorsorge/aeltere-menschen.html.
- 58.Chiatti C., Di Rosa M., Barbadoro P., Lamura G., Di Stanislao F., Prospero E. Socioeconomic determinants of influenza vaccination among older adults in Italy. Prev. Med. 2010;51:332–333. doi: 10.1016/j.ypmed.2010.06.008. [DOI] [PubMed] [Google Scholar]
- 59.Shemesh A.A., Rasooly I., Horowitz P., Lemberger J., Ben-Moshe Y., Kachal J., Danziger J., Clarfield A.M., Rosenberg E. Health behaviors and their determinants in multiethnic, active Israeli seniors. Arch. Gerontol. Geriatr. 2008;47:63–77. doi: 10.1016/j.archger.2007.07.001. [DOI] [PubMed] [Google Scholar]
- 60.Pena-Rey I., Perez-Farinos N., Sarría-Santamera A. Factors associated with influenza vaccination among elderly Spanish women. Public Health. 2004;118:582–587. doi: 10.1016/j.puhe.2004.04.010. [DOI] [PubMed] [Google Scholar]
- 61.Abramson Z.H., Cohen-Naor V. Factors associated with performance of influenza immunization among the elderly. Isr. Med Assoc. J. 2000;2:902–907. [PubMed] [Google Scholar]
- 62.Evans M.R., Prout H., Prior L., Tapper-Jones L.M., Butler C.C. A qualitative study of lay beliefs about influenza immunisation in older people. Br. J. Gen. Pract. 2007;57:352–355. [PMC free article] [PubMed] [Google Scholar]
- 63.Bhandari A., Wagner T. Self-reported utilization of health care services: Improving measurement and accuracy. Med Care Res. Rev. 2006;63:217–235. doi: 10.1177/1077558705285298. [DOI] [PubMed] [Google Scholar]
- 64.Ali R., England A., McEntee M., Mercer C., Tootell A., Hogg P. Effective lifetime radiation risk for a number of national mammography screening programmes. Radiography. 2018;24:240–246. doi: 10.1016/j.radi.2018.02.001. [DOI] [PubMed] [Google Scholar]
- 65.Kissling E., Rondy M. Early 2016/17 vaccine effectiveness estimates against influenza A (H3N2): I-MOVE multicentre case control studies at primary care and hospital levels in Europe. Eurosurveillance. 2017;22:306040. doi: 10.2807/1560-7917.ES.2017.22.7.30464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Simonsen L., Taylor R.J., Viboud C., Miller M.A., Jackson L.A. Mortality benefits of influenza vaccination in elderly people: an ongoing controversy. Lancet Infect. Dis. 2007;7:658–666. doi: 10.1016/S1473-3099(07)70236-0. [DOI] [PubMed] [Google Scholar]
- 67.Kwok R. Vaccines: The real issues in vaccine safety. Nat. News. 2011;473:436–438. doi: 10.1038/473436a. [DOI] [PubMed] [Google Scholar]
- 68.Esserman L.J., Thompson I.M., Reid B. Overdiagnosis and overtreatment in cancer: An opportunity for improvement. Jama. 2013;310:797–798. doi: 10.1001/jama.2013.108415. [DOI] [PubMed] [Google Scholar]
- 69.Kiecolt-Glaser J.K., Newton T.L. Marriage and health: his and hers. Psychol. Bull. 2001;127:472. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- 70.Pescosolido B. Social connectedness in health, morbidity and mortality, and health care-the contributions, limits and further potential of health and retirement study. Forum Health Econ. Policy. 2011;14:3. doi: 10.2202/1558-9544.1264. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.