Abstract
Background
Pregnant uncorrected congenital heart disease patients, especially those who already developed pulmonary hypertension, have increased risk for maternal mortality. The pulmonary hypertension severity and right ventricle function may be associated with higher maternal mortality. The study aimed to investigate the mortality rate of pregnant uncorrected congenital heart disease and the impact of pulmonary hypertension severity on mortality.
Methods
This is the sub study of COngenital HeARt Disease in adult and Pulmonary Hypertension Registry. The data of pregnant uncorrected congenital heart disease patients were analyzed from registry database. The maternal mortality was recorded. The data of demography, clinics, obstetrics, and transthoracic echocardiography were collected. The factors that influenced maternal mortality were analyzed. A statistical significance was determined when p value < 0.05.
Results
From 2012 until 2017, there were 78 pregnant congenital heart disease patients. Of them, 56 patients were eligible for analyses. The majority of congenital heart disease was atrial septal defect (91.1%). The maternal mortality rate was 10.7% (6 of 56). Pulmonary hypertension occurred in 48 patients, therefore the maternal mortality rate among congenital heart disease-pulmonary hypertension with majority of atrial septal defect was 12.5% (6 of 48). Among nonsurvivors, 100% suffered from severe pulmonary hypertension as compared to survivors (56.0%), p = 0.041. Most nonsurvivors were Eisenmenger syndrome (83.3%), significantly higher compared to survivors (22.0%), p = 0.006. Nonsurvivors had significantly worsened WHO functional class, reduced right ventricle systolic function, and right heart failure. The modes of maternal death were severe oxygen desaturation (66.7%) and respiratory failure and sepsis (33.3%). Most of the maternal deaths occurred within 24 h postpartum period.
Conclusion
Maternal mortality rate among pregnant uncorrected congenital heart disease with majority of atrial septal defect was 10.7% and among congenital heart disease-pulmonary hypertension with majority of atrial septal defect was 12.5%. Factors related with maternal mortality were severe pulmonary hypertension, Eisenmenger syndrome, and reduced right ventricle systolic function.
Keywords: uncorrected CHD, pulmonary hypertension, pregnancy, mortality, oxygen desaturation
Introduction
The maternal mortality rate in pregnant women with pulmonary hypertension (PH) is high, ranging from 25 to 56%.1 In PH associated with congenital heart disease (CHD-PH), the maternal mortality rate varies from 3.8 to 28%.1–3 The wide variation of maternal mortality rate is possibly due to the disparity in patients’ underlying CHDs, treatment modalities, PH-specific medication, pregnancy follow-up, and peripartum care among hospitals/centers.
Women with uncorrected and uncomplicated small patent ductus arteriosus (PDA) and uncomplicated atrial or ventricular septal defect (ASD or VSD) have no risk or slightly increased risk of maternal mortality if pregnancy occurs (modified WHO class risk I and II, respectively).4 Nevertheless, women with CHD-PH are contraindicated for pregnancy and subsequent delivery because it bears a very high-risk maternal mortality rate (WHO class IV risk).4 Pregnant women with CHD-PH have difficulty to endure the alterations in hemodynamics during pregnancy and delivery.
Our hospital registry from 2012 to 2017 indicated that a number of pregnant women did not know that they had CHD, because the CHD was not diagnosed previously. While others with previously diagnosed CHD-PH still choose to become pregnant, although they had been advised to avoid pregnancy. During the period of 2012–2017, in our hospital, the high-risk pregnancy management was conducted through a multidisciplinary approach involving cardiologists, obstetricians, fetomaternal specialists, anesthesiologists, and neonatologists. The important constraints in managing the pregnant women with CHD-PH in our hospital were the lack of PH-specific therapy, along with patients’ and family’s ignorance and delayed presentation in our hospital. This study aimed to investigate the mortality rate of pregnant women with uncorrected CHD and the impact of PH and right ventricle (RV) function on the mortality rate.
Methods
Study population
The COngenital HeARt Disease in adult and Pulmonary Hypertension (COHARD-PH) Registry is a hospital-based clinical registry of adult CHD in the vicinity of Special Province of Jogjakarta and southern parts of Central Java, Indonesia. The COHARD-PH registry was initiated in 2012 and is currently still recruiting patients. The registry has been centered in Dr Sardjito Hospital, Jogjakarta, Indonesia, a national referral hospital in the region. Until the end of 2017, the COHARD-PH registry has comprised more than 800 adult patients with CHD. The initial pilot study of the registry had been published previously.5 For the current study, the pregnant patients were identified from the COHARD-PH registry database and their data were retrieved for analysis.
In the current study, we conducted a retrospective analysis from the COHARD-PH registry database from 2012 to 2017. The inclusion criteria were as follows: (1) pregnant patients, (2) uncorrected septal defects (ASD, VSD, atrioventricular septal defect, and/or PDA), and (3) complete termination of pregnancy was in Dr Sardjito Hospital. The exclusion criteria were as follows: (1) patients with other significant heart diseases, (2) patients with existing pulmonary disease, (3) patients with left heart disease, and (4) patients with uncompleted pregnancy during this study period. Patients with other significant heart diseases were those with pulmonal stenosis, aortic stenosis, mitral stenosis, and/or moderate-to-severe regurgitation detected by transthoracic echocardiography (TTE). Patients with existing pulmonary diseases were those with asthma bronchial, chronic obstructive pulmonary disease, and/or interstitial lung disease from history of patients. Patients with left heart diseases were those with decreased left ventricle ejection fraction (<40%) by TTE, diastolic dysfunction by TTE, and presence of regional wall motion abnormality by TTE. The informed consent from patients was obtained as part of the complete informed consent in the COHARD-PH registry.
Study protocol
The data of demographics, clinics, and obstetrics among patients were collected from the registry database. The TTE results were also accumulated from the registry database. Recorded baseline data included current gestational age, gravid status, parity status, WHO functional class, peripheral oxygen saturation, chief complaints, the presence of PH, Eisenmenger syndrome, mode of delivery, anesthesia used during delivery, and hospital length of stay. The results of TTE performed during current admission were retrieved and reviewed. PH was assessed by TTE criteria, based on current recommendation using tricuspid regurgitation velocity and echocardiography signs suggesting PH.6 Patients with PH were those with high probability of PH defined by TTE.6 We investigated the medical records to assess the outcome of pregnancy from the time of admission until time of postpartum discharge or time of death in our hospital. Based on the outcome of pregnancy, patients were divided as survivors and nonsurvivors. Nonsurvivors were patients who died between time of admission and time of postpartum period in our hospital. Survivors were patients who were safely discharged during postpartum period. The causes of death among nonsurvivors were recorded from the medical records signed by treating clinicians. The study protocol was approved by the Medical and Health Research Ethics Committee of the Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada, Jogjakarta, Indonesia.
Statistical analysis
For statistical analysis, two-group comparison was applied, i.e. survivors versus nonsurvivors. The comparison of continuous data between the two groups was performed with Student’s t-test (for normally distributed data) or Mann–Whitney test (for nonparametric test). The comparison of categorical data between the two groups was performed with Chi-square test or Fisher’s exact test whichever was applicable. A p value < 0.05 was considered statistically significant.
Results
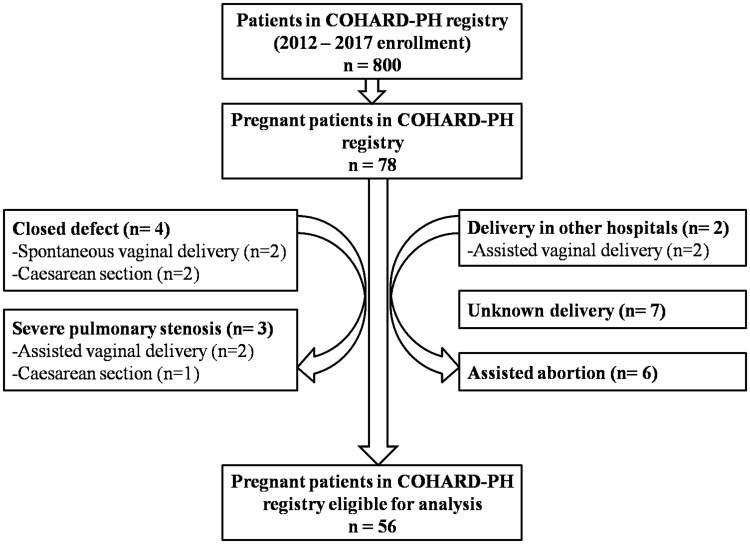
From 2012 until the end of 2017, there were about 800 patients enrolled in the COHARD-PH registry. Among them, 78 patients were pregnant and underwent pregnancy examination in Dr Sardjito Hospital. From 78 patients, four patients had already undergone defect closure (all were ASD patients, with closure time between three and seven years previously), three patients had severe pulmonal stenosis, two patients had undergone assisted vaginal delivery in district hospitals, seven patients had not continued the delivery in our hospital and the delivery data were unknown, and six patients had undergone pregnancy termination by assisted abortion (curettage) in Dr Sardjito Hospital. Four patients with closed defects were delivered safely in our hospital (two spontaneous vaginal delivery (G1P0A0 and G2P1A0), one elective caesarean section (due to history of SC) (G3P2A0), and one emergency caesarean section (due to fetal distress) (G2P1A0)). Three patients with severe pulmonary stenosis were delivered safely (two assisted vaginal delivery (ASD and severe pulmonary stenosis, G2P0A1; and VSD and severe pulmonary stenosis, G2P0A1)) and one elective caesarean section (reason unknown) (ASD and moderate-severe pulmonary stenosis, G2P1A0). Two patients who had delivered in district hospital were referred in our hospital (one died in our hospital due to severe sepsis (P2A0) and one survived a complication of acute heart failure in our hospital (P3A0)). Six patients underwent assisted abortion were all survived (all patients were ASD and severe PH). Therefore, as many as 56 pregnant patients with uncorrected CHD were analyzed in this study. Figure 1 depicted the patients’ selection for current study. The majority of patients were ASD (91.1%).
Fig. 1.
The subjects’ selection for this current study from COHARD-PH registry database.
COHARD-PH: COngenital HeARt Disease in adult and Pulmonary Hypertension.
Among 56 patients, as many as six patients (10.7%) died during postpartum period due to cardiac/obstetric complications. PH was detected in 48 patients; therefore, the maternal mortality rate among patients with CHD-PH in our study, which mostly comprised of ASD, was 6 out of 48 (12.5%). The comparison of characteristics between survivors (n = 50) and nonsurvivors (n = 6) is presented in Table 1. There were no differences in terms of years of age, gestational age, number of gravid, and obstetric status between survivors and nonsurvivors. In nonsurvivors, the majority of patients were primigravida (66.7%). The time of pregnancy termination was significantly longer in nonsurvivors as compared to survivors. All of the nonsurvivors were patients with uncorrected ASD (100%). Among nonsurvivors, five patients (83.3%) were ignorant of CHD and first diagnosed with CHD during current pregnancy, whereas among survivors 31 patients (62.0%) were first diagnosed. The most common chief complaint among survivors and nonsurvivors was dyspnea. As many as 17 survivors (34.0%) had no complaints relating CHD and PH.
Table 1.
The comparison of characteristics between survivors and nonsurvivors.
| Characteristics | All subjects n = 56 | Survivors n = 50 | Nonsurvivors n = 6 | P value* |
|---|---|---|---|---|
| Years of age, mean ± SD | 29.2 ± 5.1 | 29.3 ± 5.2 | 28.0 ± 3.8 | 0.549 |
| Gestational age (weeks), mean ± SD | 30.9 ± 7.6 | 30.9 ± 8.0 | 31.2 ± 2.0 | 0.941 |
| Termination age (weeks), mean ± SD | 34.9 ± 3.2 | 35.3 ± 3.1 | 31.2 ± 2.0 | 0.002 |
| Number of gravid, mean ± SD | 2.2 ± 1.3 | 2.3 ± 1.3 | 1.5 ± 0.8 | 0.162 |
| Oxygen saturation, mean ± SD | 92.2 ± 10.0 | 93.2 ± 9.9 | 86.0 ± 8.4 | 0.101** |
| WHO functional class, n (%) | ||||
| Class I | 7 (12.5) | 7 (14.0) | 0 (0) | 0.012*** |
| Class II | 27 (48.2) | 26 (52.0) | 1 (16.7) | |
| Class III | 7 (12.5) | 4 (8.0) | 3 (50.0) | |
| Class IV | 6 (10.7) | 4 (8.0) | 2 (33.3) | |
| Obstetric status, n (%) | ||||
| Primigravida | 20 (35.7) | 16 (32.0) | 4 (66.7) | 0.246 |
| Secundigravida | 17 (30.4) | 16 (32.0) | 1 (16.7) | |
| Multigravida | 19 (33.9) | 18 (36.0) | 1 (16.7) | |
| Chief complaint, n (%) | 0.242 | |||
| None | 17 (30.4) | 17 (34.0) | 0 (0) | |
| Dyspnea | 28 (50.0) | 22 (44.0) | 6 (100) | |
| Cough | 2 (3.6) | 2 (4.0) | 0 (0) | |
| Fatigue | 7 (12.5) | 7 (14.0) | 0 (0) | |
| Peripheral edema | 1 (1.8) | 1 (2.0) | 0 (0) | |
| Chest pain | 1 (1.8) | 1 (2.0) | 0 (0) | |
| Defect type, n (%) | 0.883 | |||
| ASD | 51 (91.1) | 45 (90.0) | 6 (100) | |
| VSD | 2 (3.6) | 2 (4.0) | 0 | |
| PDA | 2 (3.6) | 2 (4.0) | 0 | |
| AVSD | 1 (1.8) | 1 (2.0) | 0 | |
| First diagnosis, n (%) | 36 (64.3) | 31 (62.0) | 5 (83.3) | 0.292**** |
| Pulmonary hypertension, n (%) | 48 (85.7) | 42 (84.0) | 6 (100.0) | 0.226**** |
| Severe pulmonary hypertension, n (%) | 34 (60.7) | 28 (56.0) | 6 (100.0) | 0.041**** |
| Eisenmenger syndrome, n (%) | 16 (28.6) | 11 (22.0) | 5 (83.3) | 0.006**** |
| PH-specific treatment, n (%) | <0.001 | |||
| Sildenafil | 28 (50.0) | 24 (50.0) | 3 (50.0) | |
| Sildenafil and beraprost | 4 (7.4) | 1 (2.1) | 3 (50.0) | |
| Nonspecific treatment, n (%) | <0.001 | |||
| Furosemid | 3 (5.4) | 0 (0) | 3 (50.0) | |
| Digoxin | 2 (3.6) | 2 (4.7) | 0 (0) | |
| Hospital days of stay, mean ± SD | 5.0 (4.0–6.75) | 6.1 ± 3.8 | 4.6 ± 4.5 | 0.396***** |
ASD: atrial septal defect; AVSD: atrioventricular septal defect; PDA: patent ductus arteriosus; PH: pulmonary hypertension; VSD: ventricle septal defect.
Comparison between survivors and nonsurvivors.
Survivors n = 39, nonsurvivors n = 6.
Survivors n = 41, nonsurvivors n = 6.
Result from Fisher’s exact test.
Survivors n = 47, nonsurvivors n = 6.
The PH-specific drugs available in our hospital, which also in Indonesia, were sildenafil and beraprost. They were given to 32 patients of 48 CHD-PH patients (66.7%). Sildenafil (oral 20 mg t.i.d) was administered mostly to 50% of patients, and combination of sildenafil and beraprost (oral 20 mcg t.i.d) to 7.4% of patients. All nonsurvivors had been administered sildenafil alone or combined sildenafil and beraprost during current pregnancy. The duration of PH-specific drugs in average was started from diagnosis of PH. Other non-specific drugs administered during current pregnancy were furosemid (50% among nonsurvivors) and digoxin (4.7% among survivors).
In all patients, 85.7% had already developed signs of PH. High probability of PH, based on TTE examination, was diagnosed in 42 (84.0%) survivors and 6 (100%) nonsurvivors (p = 0.226). Among nonsurvivors, all patients (100%) had suffered from severe PH based on the TTE result (severe PH was defined as estimated right ventricle systolic pressure ≥ 90 mmHg). Among survivors, 56.0% had severe PH. The difference of severe PH proportion between groups was statistically significant (100% versus 56.0%, p = 0.041). In line with this finding, Eisenmenger syndrome occurred in 83.3% of nonsurvivors, which was significantly higher compared to survivors (22.0%), p = 0.006.
The complete TTE result was retrieved from 48 patients and shown in Table 2. Eight patients had incomplete TTE results performed during current admission, and all of them were among survivors. They had been diagnosed with CHD previously and TTE had been performed. Nonsurvivors had significantly reduced TAPSE value, which indicated decreasing RV systolic function and imminent right heart failure. The LV systolic function was normally comparable between survivors and nonsurvivors.
Table 2.
Transthoracic echocardiography parameters between survivors and nonsurvivors.a
| Parameters | All subjects n = 48 | Survivors n = 42 | Nonsurvivors n = 6 | P value* |
|---|---|---|---|---|
| Tricuspid transvalvular gradient | 71.3 ± 38.2 | 65.4 ± 36.2 | 112.2 ± 26.5 | 0.005 |
| TAPSE | 24.7 ± 6.0 | 25.5 ± 5.9 | 18.7 ± 2.1 | <0.001 |
| RV systolic pressure | 79.2 ± 40.3 | 73.4 ± 38.6 | 120.0 ± 27.9 | 0.007 |
| LV ejection fraction | 67.8 ± 11.4 | 67.9 ± 9.6 | 66.8 ± 21.4 | 0.828 |
LV: left ventricle; RV: right ventricle; TAPSE: tricuspid annular plane systolic excursion.
TTE was performed during current admission.
Comparison between survivors and nonsurvivors.
Table 3 shows the mode of delivery in all patients, which pattern was significantly different. In nonsurvivors, the majority mode of delivery was emergency caesarean section, performed in four (66.7%) nonsurvivors, one patient (16.7%) underwent elective caesarean section, and one patient (16.7%) underwent induced vaginal delivery. All patients underwent emergency caesarean section were referred to our hospital from district hospitals (via emergency room) with poor maternal clinical condition on admission. The decision for performing emergency caesarean section was made based on obstetric indication on admission by obstetrician treating the patients and cardiologist in consultation. The indications for emergency caesarean section were as follows: one patient with severe preeclampsia, one patient with total placenta previa, and two patients due to maternal indication without specific obstetric indication. For survivors, the majority of them had elective caesarean section (38.0%). Other modes of delivery were assisted vaginal delivery (30.0%), induced vaginal delivery (24.0%), and emergency caesarean section (8.0%). The emergency caesarean section in survivors was due to obstetric/fetal indication, i.e. one patient due to failed vacuum extraction and two patients due to fetal distress. The intrathecal/epidural labor anesthesia was the most frequent anesthesia used in the survivors. For nonsurvivors, general anesthesia and spinal anesthesia were the most frequent anesthesia used.
Table 3.
Mode of delivery and type of anesthesia between survivors and nonsurvivors.
| Characteristics | All subjects n = 56 | Survivors n = 50 | Nonsurvivors n = 6 | P value* |
|---|---|---|---|---|
| Mode of delivery, n (%) | 0.001 | |||
| Emergency caesarean section | 8 (14.3) | 4 (8.0) | 4 (66.7) | |
| Elective caesarean section | 20 (35.7) | 19 (38.0) | 1 (16.7) | |
| Assisted vaginal delivery | 15 (26.8) | 15 (30.0) | 0 (0) | |
| Induced vaginal delivery | 13 (23.2) | 12 (24.0) | 1 (16.7) | |
| Anesthesia, n (%) | <0.001 | |||
| ILA/ELA | 29 (51.8) | 28 (58.3) | 0 (0) | |
| Regional/spinal anesthesia | 7 (12.5) | 4 (8.3) | 2 (33.3) | |
| General anesthesia | 6 (10.7) | 2 (4.2) | 4 (66.7) |
ELA: epidural labor anesthesia; ILA: intrathecal labor anesthesia.
Comparison between survivors and nonsurvivors.
Among nonsurvivors, severe oxygen desaturation was the major cause of death (four out of six patients, 66.7%). The severe oxygen desaturation was highly likely due to PH crisis, which was also accompanied by low cardiac output and cardiogenic shock. Sepsis and respiratory failure were the following causes of death, in two out of six nonsurvivors (33.3%). Table 4 shows the individual characteristics of nonsurvivors.
Table 4.
Individual characteristics of nonsurvivors among pregnant patients with CHD-PH.
| No | Congenital defect | Age at pregnancy | Saturation in admission | TTE | WHO class | Pregnancy duration /termination | Mode of delivery | Mode of anesthesia | Obstetric and cardiac events | Mode of death | Time of death |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | ASD II, Eisenmenger Syndrome | 33 | 89 | RVSP: 126 mmHg TAPSE: 18 mm LVEF: 78% | II | 31/31 weeks’ gestation | Emergency caesarean section | ASA IVE, general anesthesia, intubation | Abruptio placentae, IUFD, HELLP syndrome, severe preeclampsia | Respiratory failure, bradycardia–PEA | 24 h post emergency caesarean section |
| 2 | ASD II, Eisenmenger Syndrome | 28 | 70 | RVSP: 106 mmHg TAPSE: 16 mm LVEF: 29% | IV | 30/30 weeks’ gestation | Induced vaginal delivery | Spinal anesthesia | Sepsis, severe desaturation, bradypnea–apnea | Severe desaturation, PH crisis, bradycardia–PEA | 11 days postpartum |
| 3 | ASD II, Eisenmenger syndrome | 32 | 88 | RVSP: 129 mmHg TAPSE: 22 mm LVEF: 93% | III | 28/28 weeks’ gestation | Emergency caesarean section | ASA IIIE, general anesthesia, intubation | Total placenta previa, desaturation | Severe desaturation, cardiogenic shock, PH crisis, bradycardia–PEA | 24 h post emergency caesarean section |
| 4 | ASD II, severe PH | 26 | 94 | RVSP: 163 mmHg TAPSE: 18 mm LVEF: 63% | III | 34/34 weeks’ gestation | Elective caesarean section | Spinal anesthesia | Sepsis, severe pneumonia | Respiratory failure, bradycardia–PEA | 6 days post elective caesarean section |
| 5 | ASD II, Eisenmenger syndrome | 22 | 85 | RVSP: 78 mmHg TAPSE: 20 mm LVEF: 72% | III | 32/32 weeks’ gestation | Emergency caesarean section | ASA IIIE, general anesthesia, intubation | Desaturation, cardiogenic shock | Severe desaturation, cardiogenic shock, PH crisis, bradycardia–PEA | 24 h post emergency caesarean section |
| 6 | ASD II, Eisenmenger syndrome | 28 | 90 | RVSP: 119 mmHg TAPSE: 18 mm LVEF: 66% | IV | 32/32 weeks’ gestation | Emergency caesarean section | ASA IIIE, general anesthesia, intubation | Desaturation, cardiogenic shock | Severe desaturation, cardiogenic shock, PH crisis, bradycardia–PEA | 24 h post emergency caesarean section |
ASA: American Society of Anesthesiologists; ASD: atrial septal defect; CHD-PH: PH associated with congenital heart disease; LVEF: left ventricle ejection fraction; PEA: pulseless electrical activity; RVSP: right ventricle systolic pressure; TAPSE: tricuspid annular plane systolic excursion; TTE: transthoracic echocardiography.
Discussion
In this study we reported that among pregnant patients with uncorrected CHD, the maternal mortality rate was 10.7% and among CHD-PH patients, the maternal mortality rate was 12.5%. Since the majority of patients were ASD, the mortality rate of this study cannot be attributed to generalize for all CHD-PH patients. The factors related with maternal mortality were severe PH, Eisenmenger syndrome, and reduced RV systolic function. The proportion of patients with severe PH and Eisenmenger syndrome was significantly higher in nonsurvivors. Reduced RV systolic function was observed in nonsurvivors. The mode of delivery among nonsurvivors was mostly emergency caesarean section. The causes of maternal death were severe oxygen desaturation, respiratory failure, and sepsis. Most of the maternal deaths were within 24 h of the postpartum period.
The worsened outcome in the pregnancy and delivery of pregnant patients with CHD-PH is mostly due to compromised cardiovascular system and worsening PH.7 In the cases of uncorrected septal defects, especially right-to-left shunt or bidirectional shunt, PH is a threatening condition that increases maternal mortality.2–4,7 Due to improvement in peripartum management involving multidisciplinary teams and availability of PH-specific medication, the maternal mortality in pregnant women with CHD-PH is reduced as low as 3.8%.2 However, in our hospital registry, the maternal mortality rate among pregnant patients with CHD-PH was still high. Other registries reported no or very low maternal mortality rate, mostly related to severe PH.7–9
The most common CHD in our registry is uncorrected ASD.5 All nonsurvivors in our current study were uncorrected ASD and PH. Among other congenital defects, ASD is the most common defect encountered during adult life due to underdiagnosis and late finding. In our registry database, adult ASD is the most common CHD with PH complication.5 They presented to the hospital due to signs and symptoms of PH and/or right heart failure.5 In this study, 64.8% of patients were first diagnosed as CHD during this pregnancy. As many as five of six nonsurvivors were first diagnosed during current pregnancy, therefore no antenatal care for CHD condition was done to the patients. Furthermore, most pregnant patients who came to our hospital were already in their third trimester of pregnancy (mean gestational age: 31.1 ± 7.7 weeks). Among nonsurvivors, the termination of pregnancy was performed straightaway, mostly by emergency caesarean section and needed the general anesthesia. Whereas among survivors there was on average 4.2 weeks waiting time before planned termination of pregnancy, mostly performed by elective/planned caesarean section.
The mode of death among patients with uncorrected CHD-PH during pregnancy and delivery in several previous reports was PH crisis, which was indicated by a sudden rise in pulmonary artery pressure and hampered blood flow to the left heart which subsequently caused a low output state.2 The severe lowered oxygen saturation and reduced systemic blood pressure are hallmarks of PH crisis. The condition is fatal and currently no effective treatment is available.2 In our current study, severe oxygen desaturation and hemodynamic disturbance, in accordance with PH crisis, occurred in four out of six patients. The postpartum period, especially within 72 h of postpartum, is a critical period for maternal mortality. In our current study, the most common duration of maternal death was within 24 h postpartum. The cardiovascular compromise occurs after 20 weeks of gestation, indicated by worsened oxygen desaturation/hypoxemia and heart failure as the most common cardiovascular events.2 Deterioration of WHO functional class may occur with increasing gestational age and associated with maternal cardiovascular complication and mortality.2,10,11 In our study, deteriorated WHO functional class was observed in nonsurvivors (five patients had WHO class III and IV).
In our study, in addition to severe PH, Eisenmenger syndrome was also a predictor for maternal mortality. Almost all nonsurvivors were Eisenmenger syndrome as indicated by right-to-left shunt defects, cyanosis, and reduced oxygen saturation. Eisenmenger syndrome gradually leads to progressive RV failure. Previous study had reported the outcome of Eisenmenger syndrome in pregnancy.12 Similar to our finding, the presence of Eisenmenger syndrome was associated with worst outcome, both for maternal and fetal survival.12 RV dysfunction and failure are also associated with worsened outcome for pregnant women with CHD-PH.13 Reduced TAPSE (mean TAPSE < 19 mm) was observed in nonsurvivors, which indicated the reduced RV systolic function during current pregnancy. The LV function was still normal (mean LVEF 66.8%) in nonsurvivors; however, RV dysfunction might affect LV function, which contributed to reduced cardiac output.14 The unclosed defects and rising mean PAP and PVR during peripartum period also worsened RV dysfunction and subsequently reduced cardiac output.14
In patients with CHD-PH, there is an increasing risk of maternal mortality or severe morbidity. Therefore, pregnancy is contraindicated in patients with CHD-PH. If pregnancy occurs, termination should be discussed by multidisciplinary experts.4 If pregnancy continues, expert counseling is a requisite and intensive cardiac and obstetric monitoring is obligatory throughout pregnancy, delivery, and postpartum period.4 The mode of delivery and anesthetics strategy have to be defined by an expert team.4,15 During the study period (2012–2017), our hospital had already developed a multidisciplinary team for higher risk pregnancy, including pregnancy in CHD-PH patients. However, the uniformed protocol for CHD-PH or CHD with pregnancy had not been developed. In our cases, the decision for pregnancy termination and mode of pregnancy was based on team decision involving cardiologists, obstetricians, and anesthesiologists. Unfortunately, 11% of patients did not survive despite the multidisciplinary effort to manage the patients. Most nonsurvivors underwent emergency caesarean section, were on general anesthesia, were primigravida, were first diagnosed in this current pregnancy, had late findings, and were ASD patients. The high number of emergency caesarean section and general anesthesia was due to maternal indication, who were referred to our emergency unit with deteriorated pregnancy. These patients have never been examined at our hospital, therefore no close monitoring performed during her antenatal care. The availability of PH-specific medication (in our hospital only sildenafil and beraprost were available during the study period) was one factor that also contributed to maternal mortality.
Limitation of this study is the diagnosis of PH, and severity of PH was based on TTE examination. The gold standard for PH diagnosis and severity measurement is by right heart catheterization, which we did not perform. The small number of nonsurvivors made statistical comparison and conclusion challenging. Other limitation was the number of patients who did not continue pregnancy follow-up and delivery in our hospital despite the high-risk pregnancy was already informed. We did not have any information regarding the loss-of-follow up patients.
In conclusion, among pregnant patients with uncorrected CHD, the majority of whom were ASD, the maternal mortality rate was 10.7% and among CHD-PH with ASD as majority, the maternal mortality rate was 12.5%. The factors related to maternal mortality were severe PH, Eisenmenger syndrome, and reduced RV systolic function. The causes of maternal death were severe oxygen desaturation, respiratory failure, and sepsis. Most of the maternal deaths were during the postpartum period.
Authors’ contributions
Concept/design: ABH, LKD; Recruitment and data collection: ABH, DWA, LKD; Drafting and writing of article: ABH, LKD; Data analysis/interpretation, critical revision, and approval of the article: ABH, DWA, DSN, NE, LKD.
Acknowledgement
The authors acknowledge the COHARD-PH registry team members for their assistance during data collection and retrieval and manuscript writing: Arina Prihesti Nugraheni MD, Athanasius Wrin MD, Theresia Dwiamelia MD, Monika Setiawan MD, Aristida Cahyono MD, Zaki Horizon Islami MD, Reza Pandu Aji MD, Vera Christina Dewanto MD, Aditya Doni Pradana MD, Dimas Setiaji MD, Muhammad Reyhan Hadwiono MD, Armalya Pritazahra MD, and Ahmad Musthafa MD. The COHARD-PH registry database enrollment had been initiated in 2012 and is currently still enrolling adult patients with CHD. The authors appreciate the assistance of Klinik Bahasa (Office of Research and Publication, Faculty of Medicine, Public Health and Nursing, Universitas Gadjah Mada) for English language and grammar editing of the manuscript.
Conflict of interest
The author(s) declare that there is no conflict of interest.
Funding
Research Grant Penelitian Kerjasama Luar Negeri (No: 1666/UN1/DITLIT/DIT-LIT/LT/2018) from Direktorat Riset dan Pengabdian Masyarakat, Direktorat Jenderal Penguatan Riset dan Pengembangan, Kementerian Riset, Teknologi dan Pendidikan Tinggi of Indonesia via Universitas Gadjah Mada, Jogjakarta, Indonesia to Principal Investigator ABH. Research Grant Penelitian Dasar 2019 (No: 2798/UN1.DITLIT/DIT-LIT/LT/2019) from Direktorat Riset dan Pengabdian Masyarakat, Direktorat Jenderal Penguatan Riset dan Pengembangan, Kementerian Riset, Teknologi dan Pendidikan Tinggi of Indonesia via Universitas Gadjah Mada, Jogjakarta, Indonesia to Principal Investigator ABH.
ORCID iD
Anggoro B. Hartopo https://orcid.org/0000-0002-6373-1033
References
- 1.Sliwa K, van Hagen IM, Budts W, et al. Pulmonary hypertension and pregnancy outcomes: data from the Registry of Pregnancy and Cardiac Disease (ROPAC) of the European Society of Cardiology. Eur J Heart Fail 2016; 18: 1119–1128. [DOI] [PubMed] [Google Scholar]
- 2.Ladouceur M, Benoit L, Radojevic J, et al. Pregnancy outcomes in patients with pulmonary arterial hypertension associated with congenital heart disease. Heart 2017; 103: 287–292. [DOI] [PubMed] [Google Scholar]
- 3.Bédard E, Dimopoulos K, Gatzoulis MA. Has there been any progress made on pregnancy outcomes among women with pulmonary arterial hypertension? Eur Heart J 2009; 30: 256–265. [DOI] [PubMed] [Google Scholar]
- 4.Regitz-Zagrosek V, Roos-Hesselink JW, Bauersachs J, et al. 2018 ESC guidelines for the management of cardiovascular diseases during pregnancy. Eur Heart J 2018; 39: 3165–3241. [DOI] [PubMed] [Google Scholar]
- 5.Krisdinarti L, Hartopo AB, Anggrahini DW, et al. Clinical characteristics of adult uncorrected secundum atrial septal defect, a pilot study. J Med Sci 2016; 48: 89–97. [Google Scholar]
- 6.Galiè N, Humbert M, Vachiery JL, et al. 2015 ESC/ERS guidelines for the diagnosis and treatment of pulmonary hypertension: the Joint Task Force for the Diagnosis and Treatment of Pulmonary Hypertension of the European Society of Cardiology (ESC) and the European Respiratory Society (ERS): Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC), International Society for Heart and Lung Transplantation (ISHLT). Eur Heart J 2016; 37: 67–119. [DOI] [PubMed] [Google Scholar]
- 7.Ntiloudi D, Zegkos T, Bazmpani MA, et al. Pregnancy outcome in women with congenital heart disease: a single-center experience. Hellenic J Cardiol 2018; 59: 155–159. [DOI] [PubMed] [Google Scholar]
- 8.Song YB, Park SW, Kim JH, et al. Outcomes of pregnancy in women with congenital heart disease: a single center experience in Korea. J Korean Med Sci 2008; 23: 808–813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pillutla P, Nguyen T, Markovic D, et al. Cardiovascular and neonatal outcomes in pregnant women with high-risk congenital heart disease. Am J Cardiol 2016; 117: 1672–1677. [DOI] [PubMed] [Google Scholar]
- 10.Drenthen W, Pieper PG, van der Tuuk K, et al. Cardiac complications relating to pregnancy and recurrence of disease in the offspring of women with atrioventricular septal defects. Eur Heart J 2005; 26: 2581–2587. [DOI] [PubMed] [Google Scholar]
- 11.Yadav V, Sharma JB, Mishra S, et al. Maternal and fetal outcome in operated vs non-operated cases of congenital heart disease cases in pregnancy. Indian Heart J 2018; 70: 82–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duan R, Xu X, Wang X, et al. Pregnancy outcome in women with Eisenmenger’s syndrome: a case series from west China. BMC Pregnancy Childbirth 2016; 16: 356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Siegmund AS, Kampman MAM, Oudijk MA, et al. Maternal right ventricular function, uteroplacental circulation in first trimester, and pregnancy outcome in women with congenital heart disease. Ultrasound Obstet Gynecol 2019; 54: 359–366. [DOI] [PubMed] [Google Scholar]
- 14.Haddad F, Doyle R, Murphy DJ, et al. Right ventricular function in cardiovascular disease, part II: pathophysiology, clinical importance, and management of right ventricular failure. Circulation 2008; 117: 1717–1731. [DOI] [PubMed] [Google Scholar]
- 15.Harris RC, Fries MH, Boyle A, et al. Multidisciplinary management of pregnancy in complex congenital heart disease: a model for coordination of care. Congenit Heart Dis 2014; 9: E204–E211. [DOI] [PubMed] [Google Scholar]