Abstract
Clonal evolution of chronic lymphocytic leukemia (CLL) often follows chemotherapy and is associated with adverse outcome, but also occurs in untreated patients, in which case its predictive role is debated. We investigated whether the selection and expansion of CLL clone(s) precede an aggressive disease shift. We found that clonal evolution occurs in all CLL patients, irrespective of the clinical outcome, but is faster during disease progression. In particular, changes in the frequency of nucleotide variants (NVs) in specific CLL-related genes may represent an indicator of poor clinical outcome.
Keywords: Chronic lymphocytic leukemia, Copy number variation, Nucleotide variation, Clonal evolution
To the Editor
In chronic lymphocytic leukemia (CLL), the clonal expansion acquired relevance with the NGS era, which allowed its use for clinical monitoring. Research was mainly performed on large CLL cohorts sampled before and after therapy [1] and only a few studies investigated clonal evolution longitudinally in stable versus progressive untreated patients [2–4]. The key results indicate expansion of specific clones upon therapy and heterogeneity of mutated genes among patients, but the extent to which the genetic dynamics differs between stable and progressive untreated CLLs is still controversial.
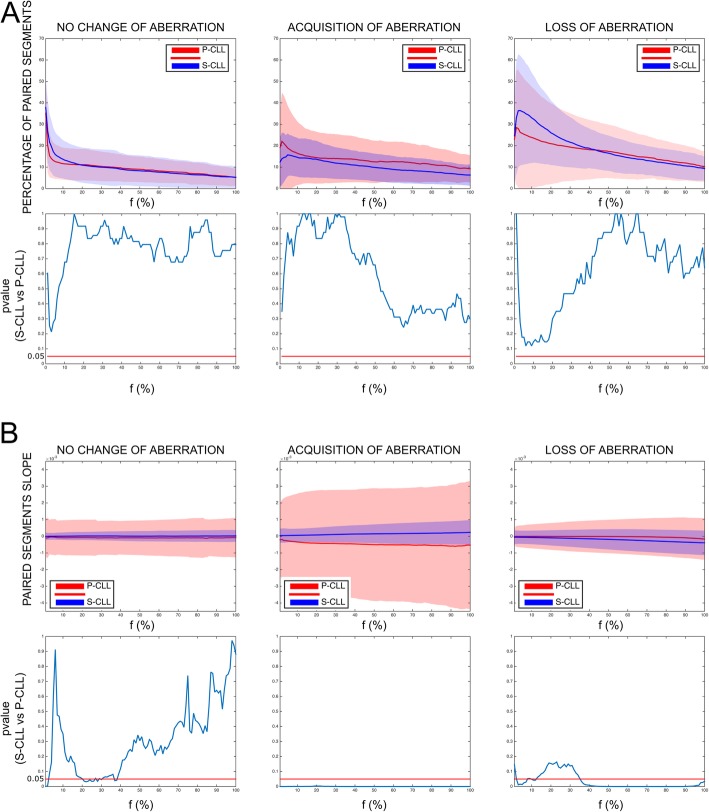
To address this point, we used a CLL cohort including untreated sequential samples from patients with either progressive (P-CLL) or stable (S-CLL) disease. Patients’ features are in Additional file 1: Table S1. At each time point, the diagnosis of stable or progressive CLL was established by the clinicians according to the criteria defined during the International Workshop on Chronic Lymphocytic Leukemia [5]. Using genome-wide copy number variation (CNV) analysis, we investigated copy number fluctuations in 11 stable CLLs (S-CLLs) and 15 progressive CLLs (P-CLLs). Data were processed using the Rawcopy package [6], and paired segments were defined for each patient (Additional file 2: Figure S1). Since the percentage of CLL cells (f) in PBMCs was not always known, analyses were performed varying f from 1 to 100%. To define aberrant loci, we used two sets of thresholds on log ratio (LogR) value, depending on f and on copy number (k) in CLL cells (Additional file 2: Figure S2). We did not find significant differences in percentages of aberrant loci between S-CLLs and P-CLLs (Fig. 1a), but the rate of change (or slope), reflecting the rate of aberrant clones evolving over time, was significantly higher in P-CLLs (p ≤ 0.05, Mann-Whitney U test) (Fig. 1b). Thus, S-CLLs and P-CLLs seemed to have the same probability of acquiring or losing clones, but this phenomenon was faster in P-CLLs. The results were validated on 6 S-CLLs and 5 P-CLLs with known percentage of CLL cells in PBMCs (Additional file 2: Figure S3-S4), suggesting that tracking copy number changes does not mandatorily require knowledge of cancer cell percentage.
Fig. 1.
Longitudinal analysis of copy number aberrations in stable and progressive CLL patients. Genome-Wide Human SNP Arrays 6.0 (Affymetrix) was used to genotype patient DNAs at the two sequential sampling points, first time point (FTP), and last time point (LTP). Data were processed using the Rawcopy package, and paired segments (PSs) were identified between FTP and LTP of each patient (see Methods in Additional file 2). Aberrant loci were identified by varying the percentage of cancer cells (f) using two sets of threshold on log ratio (LogR), one for DNA amplification (LogRA) and one for DNA deletion (LogRD). a The percentage of PSs and b their slopes (∆LogRLTP, FTP/∆tLTP, FTP) are shown as mean (solid line) and standard deviation (shades) based on no change, acquisition, or loss of aberration as a function of f. No change of aberration: the considered locus was aberrant both in FTP and in LTP; acquisition of aberrations: the considered locus was aberrant only in LTP; loss of aberrations: the considered locus was aberrant only in FTP. Red colors indicate the P-CLLs; blue the S-CLLs. p values’ graphs (lower panel) report the Mann-Whitney U test for each f, significance was defined as p < 0.050
To identify genetic events associated with faster clonal expansion, we characterized the CLL-specific genetic features of our cohort. Analyses by qPCR of three chromosomal abnormalities of prognostic value, del (11q), tri (12), and del (17p) [7], did not reveal significant differences between S-CLLs and P-CLLs (Additional file 2: Figure S5). Subsequently, we characterized 11 S-CLLs and 17 P-CLLs for point mutations or indels in regions of 27 genes reported as mutated in CLL (Additional file 3: Table S2). We did not register any significant difference between S-CLLs and P-CLLs with regard to frequency and number of nucleotide variants (NVs) (data not shown). Next, we focused only on NVs with variant allele frequencies (VAF) changing more than 20% between longitudinal samples (dynamic NV: dNVs, synonymous or non-synonymous). We detected on average 1.18 and 3.35 dNVs per sample in S-CLLs and P-CLLs, respectively (Additional file 4: Table S3). P-CLLs showed higher gains/increases of dNVs (p = 0.0008, Fisher’s test) (Fig. 2a). Patients with dNV > 1 had shorter treatment-free survival (TFS), considering as starting point the date at first sampling (p = 0.0029) or at diagnosis (p = 0.0004, log rank test) (Fig. 2b and Additional file 2: Figure S6). A dNV > 1 was also associated with poor prognostic factors, including unmutated IGVH and trisomy 12 (p = 0.0461 and p = 0.0407, respectively, Fisher’s test) (Additional file 5: Table S4). Patients with unmutated IGVH showed shorter TFS, supporting the reliability of our cohort (Fig. 2b). Finally, we found that in P-CLLs the average of dNV frequencies was higher in the first sample (p = 0.0074, Mann-Whitney U test), where it was not associated with IGVH mutational status (Fig. 2c). These findings suggest that dNVs could have an exploitable clinical relevance. However, since dNVs include synonymous/non-synonymous mutations and NVs in non-coding regions, we cannot speculate on the molecular role of the targeted genes most frequently mutated, such as ITPKB and NOTCH1 (Fig. 2a). Indeed, these dNVs were only used here to track genetic evolution.
Fig. 2.
Mutational status of CLL samples. a Next-generation sequencing of 27 CLL-associated genes in 11 and 17 patients with stable and progressive disease, respectively. Sequence variants were identified using Torrent Suite 3.4 and Variant Caller plugin 3.4.4. NVs with a coverage < 100 were not considered; NVs with a mutation frequency < 5% were not considered; NVs residing in homopolymer DNA sequences (≥ 4 nucleotides) were also not considered. Each square report either gain or loss of mutation or change in mutation frequency (> 20%) between FTP (left side) and LTP (right side); the mutation frequency of dynamic nucleotide variants (dNVs) was reported in Additional file 4: Table S3. Fisher’s exact tests were used to compare groups. Statistical tests were two-sided, and significance was defined as p < 0.050. b Kaplan-Meier curve of treatment-free survival in CLL patients dichotomized based on the number of NVs that change more than 20% between FTP and LTP (dNVs) (upper panel) and on the mutational status of the poor prognostic factor IGVH (lower panel). The median of dNVs changed across all the samples was used as cut-off. Time to treatment was calculated from the first sampling; the last follow-up was considered for patients, which did not undergo treatment. The Log-rank test was used to test for significance. c Mutation frequency of dNVs in stable and progressive CLL groups, and in mutated or unmutated IGVH CLL groups; data are reported as median and interquartile range (box); whiskers range from min to max. Mann-Whitney test was used to compare groups; **denotes a p value ≤ 0.01
In conclusion, differently from previous studies, we calculated VAFs on PBMCs, demonstrating that this is reliable to track CLL evolution. In fact, an increase of a single VAF over time indicates expansion of the clone carrying that NV, regardless of variation in cancer cell fraction. Overall, our study points to a higher genetic dynamics in P-CLLs and suggests that monitoring VAFs of a specific gene panel in PBMCs from sequential samples of a CLL patient may predict disease progression.
Supplementary information
Additional file 1: Table S1 Molecular and clinical features of all patients included in the study.
Additional file 2. Supplemental Data (Additional files 6 and 7).
Additional file 3: Table S2 HaloPlex SureDesign Report.
Additional file 4: Table S3 Genetic variants represented in Fig. 2.
Additional file 5: Table S4. Characteristics of patients having few (dNV≤1) versus many (dNV>1) nucleotide variants.
Additional file 6: Table S6. SNPs and mutations described by dbSNP and COSMIC databases, respectively, and localized in the regions analyzed by Haloplex SureDesign.
Additional file 7: Table S7. SNPs and mutations detected by Haloplex SureDesign Panel.
Acknowledgements
We thank Ms. Lia De Amicis for the administrative work. We thank Valerie Matarese for the manuscript editing and Prof. Carlo Maria Croce for providing DNA samples.
Abbreviations
- CLL
Chronic lymphocytic leukemia
- CN
Copy number
- CNV
Copy number variation
- dNV
Dynamic nucleotide variant
- FTP
First time point
- LogR
Log ratio
- LTP
Last time point
- NV
Nucleotide variant
- PBMC
Peripheral blood mononuclear cell
- P-CLL
Progressive chronic lymphocytic leukemia
- PS
Paired segment
- S-CLL
Stable chronic lymphocytic leukemia
- VAF
Variant allele frequency
Authors’ contributions
RV and AV designed the study. ADA and AR performed the experiments with contributions of CB, LL, ES, VB, FP, SS, SP, and MF. RV, AV, AR, AB, and ADA analyzed the experiments with contribution of CB, MF, SV, and LM. LZR, TJK, FA, II, and LL provided CLL samples and/or clinical data. RV, AV, AR, ADA, RMC, and MN discussed the data analysis. AR, ADA, AV, and RV wrote the manuscript. All the authors critically reviewed and edited the paper. All authors read and approved the final manuscript.
Funding
This study is supported by the Italian Association for Cancer Research (AIRC) with Start Up grant 2010 (10054) to RV and partially by the Italian Association for Cancer Research (AIRC IG-17063) to SV. RV was supported by her own Marie Curie Career Integration Grant (GA-2011-303735).
Availability of data and materials
DNA CNVs and mutational data are freely available to ArrayExpress database (accession number E-MTAB-8020) and European Nucleotide Archive database (accession number ERP115524). All the other raw data are freely available at the code-hosting platform GitHub (https://github.com/VeroneseVisoneLabs/Genetic-dynamics-in-untreated-CLL-patients-with-either-stable-or-progressive-disease-a-longitudinal).
Ethics approval and consent to participate
The institutional review board of the University of California, San Diego (171884CX), and of the Fondazione Policlinico Agostino Gemelli (P/948/CE/2011) approved the research protocol. Samples were provided upon written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Alice Ramassone, Andrea D’Argenio and Angelo Veronese contributed equally to this work.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s13045-019-0802-x.
References
- 1.Sutton LA, Rosenquist R. Deciphering the molecular landscape in chronic lymphocytic leukemia: time frame of disease evolution. Haematologica. 2015;100(1):7–16. doi: 10.3324/haematol.2014.115923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hernandez-Sanchez M, Kotaskova J, Rodriguez AE, Radova L, Tamborero D, Abaigar M, et al. CLL cells cumulate genetic aberrations prior to the first therapy even in outwardly inactive disease phase. Leukemia. 2019;33(2):518–558. doi: 10.1038/s41375-018-0255-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Leeksma AC, Taylor J, Wu B, Gardner JR, He J, Nahas M, et al. Clonal diversity predicts adverse outcome in chronic lymphocytic leukemia. Leukemia. 2019;33(2):390–402. doi: 10.1038/s41375-018-0215-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rose-Zerilli MJ, Gibson J, Wang J, Tapper W, Davis Z, Parker H, et al. Longitudinal copy number, whole exome and targeted deep sequencing of 'good risk' IGHV-mutated CLL patients with progressive disease. Leukemia. 2016;30(6):1301–1310. doi: 10.1038/leu.2016.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Dohner H, et al. Guidelines for the diagnosis and treatment of chronic lymphocytic leukemia: a report from the International Workshop on Chronic Lymphocytic Leukemia updating the National Cancer Institute-Working Group 1996 guidelines. Blood. 2008;111(12):5446–5456. doi: 10.1182/blood-2007-06-093906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mayrhofer M, Viklund B, Isaksson A. Rawcopy: improved copy number analysis with Affymetrix arrays. Sci Rep. 2016;6:36158. doi: 10.1038/srep36158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Dohner H, Stilgenbauer S, Benner A, Leupolt E, Krober A, Bullinger L, et al. Genomic aberrations and survival in chronic lymphocytic leukemia. N Engl J Med. 2000;343(26):1910–1916. doi: 10.1056/NEJM200012283432602. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1 Molecular and clinical features of all patients included in the study.
Additional file 2. Supplemental Data (Additional files 6 and 7).
Additional file 3: Table S2 HaloPlex SureDesign Report.
Additional file 4: Table S3 Genetic variants represented in Fig. 2.
Additional file 5: Table S4. Characteristics of patients having few (dNV≤1) versus many (dNV>1) nucleotide variants.
Additional file 6: Table S6. SNPs and mutations described by dbSNP and COSMIC databases, respectively, and localized in the regions analyzed by Haloplex SureDesign.
Additional file 7: Table S7. SNPs and mutations detected by Haloplex SureDesign Panel.
Data Availability Statement
DNA CNVs and mutational data are freely available to ArrayExpress database (accession number E-MTAB-8020) and European Nucleotide Archive database (accession number ERP115524). All the other raw data are freely available at the code-hosting platform GitHub (https://github.com/VeroneseVisoneLabs/Genetic-dynamics-in-untreated-CLL-patients-with-either-stable-or-progressive-disease-a-longitudinal).