Abstract
Background
Syphilis is a common disease that has been researched and focused on for many years, however, syphilitic hepatitis has not been well-recognized. We report this case of syphilitic hepatitis with intrahepatic cholestasis and liver granulomas to make a deeper impression.
Case presentation
A 47-year-old male was admitted with jaundice and rashes. The laboratory examination showed abnormal liver enzymes with significant increases in ALP and GGT but mild increases in ALT and AST. His HBV surface antigen was weakly positive, with negative HIV antibody, HCV antibody, and undetectable HBV DNA. The rapid plasma reagin test and the Treponema pallidum particle assay tests for Syphilis were both positive. Abdominal ultrasonography and magnetic resonance cholangiopancreatography revealed the normal biliary tract, liver, and spleen. The liver pathological examination showed cholangiocyte inflammation and micro-granulomas with coagulation necrosis. After 2 months of benzathine penicillin treatment, his liver enzyme decreased rapidly and remained normal after 1-year of follow-up.
Conclusions
Increased liver enzymes, intrahepatic cholestasis and liver granulomas with well-response to antibiotics may provide clues for the diagnosis of syphilitic hepatitis.
Keywords: Syphilis, Hepatitis, Rashes, Enzymes, Infection
Background
Syphilis is a multi-systemic disease caused by spirochete Treponema pallidum. Liver is one of the organs that can be affected [1]. Congenital syphilitic hepatitis is more common and easily recognized for its typical clinical features, while acquired syphilitic hepatitis in adults were rarely reported. Here we present a clinical case of syphilitic hepatitis whose diagnosis has been confirmed by the pathology of liver biopsy.
Case presentation
A 47-year-old man was hospitalized because of jaundice and rashes. He developed jaundice 2 weeks prior to admission. He had no fever, fatigue, anorexia, abdominal pain, or waist pain. The laboratory examinations in local hospital revealed an alanine aminotransferase (ALT) of 359 U/L, an aspartate aminotransferase (AST) of 161 U/L, an alkaline phosphatase (ALP) of 580 U/L, a gamma-glutamyl transpeptidase (GGT) of 883 U/L and a total bilirubin (TBIL) of 75.1 umol/L. He received a liver protective medication (diammonium glycyrrhizinate), but jaundice did not improve. On the third day of diammonium glycyrrhizinate treatment, multiple non-itchy rashes appeared all over his body, which remained after the withdrawal of diammonium glycyrrhizinate and the application of anti-allergic agents. In addition, his ALP and GGT increased to 853 and 1012 U/L in the fifth day. He was then transferred to our hospital. He denied any chronic diseases, drug administration, alcohol consumption or venereal exposure. Physical examination showed the temperature of 36.0 °C, the blood pressure of 108/75 mmHg, the heart rate of 77 times/min and the breath rate of 18 times/min. His skin and sclera were mildly yellowish. No hepatomegaly, splenomegaly or ascites was found. Non-itchy macular rashes measuring 0.5 to 2 cm were observed all over his body, including some on the soles and palms (Fig. 1a and b). No genital or buccal lesions were found. Biochemical examinations in our hospital revealed a weakly positive in hepatitis B surface antigen (HBsAg). His hepatitis B surface antibody, hepatitis B extracellular antigen (HBeAg) were both negative and his hepatitis B virus DNA was undetectable (< 500 IU/ml). The other laboratory tests including Hepatitis A virus, Hepatitis C virus, Hepatitis E virus, human immunodeficiency virus, Epstein-Barr virus, cytomegalovirus, and other autoantibodies were all negative. Abdominal ultrasonography and magnetic resonance cholangiopancreatography revealed the normal biliary tract, liver, and spleen. He underwent liver biopsy and the results revealed granulomatous hepatitis with stage 2 inflammation and stage 1 fibrosis (Fig. 1c, d, e, and f). Mild hepatic lobule inflammation and plasma cells infiltrating were found in the portal area. In addition, micro-granulomas with coagulation necrosis were noticed in the portal area. Immunohistochemistry examination showed a weakly staining of HBsAg and HBcAg. He received a following test of syphilis. The rapid plasma reagin test (RPR) was positive (1,32 titer), and the Treponema pallidum particle assay (TPPA) test was 1:38, which confirmed the diagnosis of syphilis. The patient was then given intramuscular benzathine penicillin treatment at a dose of 2.4 million units per week for successive 2 months. No anti-HBV drug was given. The liver enzymes decreased rapidly after penicillin treatment and finally returned to normal level after 2 months of treatment. The follow-up showed that the liver function kept normal and HBV DNA was still undetected after 1-year.
Fig. 1.
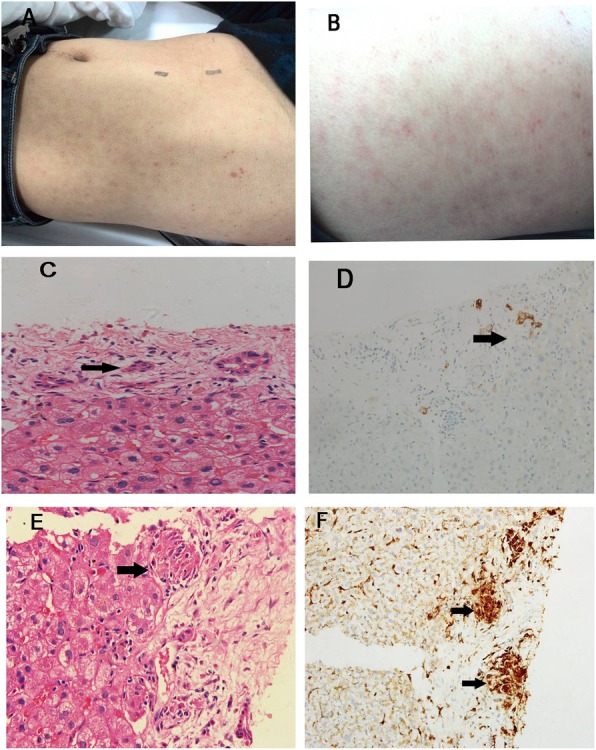
Patient’s body appearance and histological findings. a multiple erythematous macules and hyperpigmentation on the back; b, multiple erythematous macules and hyperpigmentation over the belly; c, HE staining shows bile duct epithelial cell injury, atrophy cholangiocyte, and portal tract inflammation (× 400); d, CK7 staining of cholangiocyte reveals atrophy cholangiocyte and bile duct lesion (× 100); e, HE staining shows granulomas (× 400); f, CD68 staining of macrophagocyte shows granulomas (× 100). Black arrows indicate lesions
Discussion and conclusions
Liver injury is often caused by hepatic pathogens infection, while, non-hepatotropic pathogens, such as Toxoplasma gondii, Salmonella, Leishmaniasis and Tuberculosis are able to cause the liver injury [2, 3]. Syphilis is one of the non-hepatotropic pathogens that cause unidentified hepatitis. Syphilitic hepatitis was first described by Harn in 1943 [4]. In 2004, Mullick [5] proposed the diagnostic criteria of syphilitic hepatitis, which includes:(1) abnormal liver enzyme levels; (2) serological evidence for syphilis; (3) exclusion of other causes of liver diseases; (4) liver enzyme levels returning to normal after appropriate antimicrobial therapy. In this case, the patient met all of the above diagnostic criteria.
The clinical manifestations of syphilitic hepatitis in adults tend to be nonspecific and protean [1]. Though rashes and icterus are observed in the majority of patients. The rashes of syphilis often present as non-pruritis multiple erythematous and nonconfluent maculopapular lesions, concentrating in trunk, palms, and soles [6, 7]. Other common symptoms include low-grade fever, abdominal pain, phallodynia, sore throat, headache, weight loss, arthralgia or myodynia, splenomegaly, lymphadenopathy, and uveitis [1, 8, 9].
The histological features of syphilitic hepatitis can include bile duct inflammatory infiltration, which may contribute to the elevated ALP and GGT levels in biochemistry tests [1, 7]. Hepatic granulomas are another characteristic of syphilitic hepatitis [3]. Our case presented the typical intrahepatic bile duct inflammation and granuloma, which is consistent with the previously reported cases [9]. In theory, the spirochetes could be identified in liver tissue by immunohistochemical staining or a Warthin–Starry stain [10], however, it was rarely reported in cases published.
Penicillin is the first-line treatment of syphilis and the response to antimicrobial therapy is regarded as one of the diagnostic criteria of syphilitic hepatitis [5]. In this case, standard therapy was given where significant improvement was afterward achieved. These further confirmed the diagnosis of syphilitic hepatitis. The Jarisch-Herxheimer reaction (JHR) is a severe immunological phenomenon easily seen in patients during penicillin therapy, and it mainly manifests as short-term symptoms such as fever, headache, myalgias, chills, even a sudden drop of body temperature [11]. Fortunately, JHR did not occur in our patient. According to previous reports, patients who had JHR can also achieve therapeutic effects through dose adjustment or the replacement of antibiotics [12].
In conclusion, there are no specific symptoms for syphilitic hepatitis. Elevated liver enzymes, especially for ALP and GGT, are common in patients. Bile duct inflammation or granuloma formation in hepatic pathology, as well as the response to antibiotic therapy, can also provide some clues for the diagnosis of syphilitic hepatitis.
Acknowledgments
Not Applicable.
Abbreviations
- ALP
Alkaline phosphatase
- ALT
Alanine transaminase
- AST
Aspartate aminotransferase
- GGT
Gamma-glutamyl transpeptidase
- HBV
Hepatitis B virus
- HCV
Hepatitis C virus
- HIV
Human immunodeficiency virus
- JHR
Jarisch-Herxheimer reaction
- RPR
Apid plasma reagin test
- TPPA
Treponema pallidum particle assay
Authors’ contributions
HJF did the data collection and wrote the primary draft. LS did the study design. WMF and WB were involved in manuscript preparation. LS and ZYY contributed to reporting edits and the idea for the Clinical Picture. All authors have read and approved the manuscript in its current state.
Funding
This work was supported by the Medical Project of Fujian Province (2016-CX-33), Fujian Province Health Youth Research Project (2019-1-37) and Fujian Medical University Sailing Fund Project (2018QH1047). The funders had no role in study design, d conduct and outcome of the manuscript. No additional external funding was received for this study.
Availability of data and materials
The datasets supporting the conclusions of this article are included in the article.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for publication of their clinical details and/or clinical images was obtained from the patient.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Jiaofeng Huang, Email: huangjiaofeng@fjmu.edu.cn.
Su Lin, Email: sumer5129@fjmu.edu.cn.
Mingfang Wang, Email: wangmingfang@fjmu.edu.cn.
Bo Wan, Email: wblu@163.com.
Yueyong Zhu, Phone: +86-591-87981660, Email: zhuyueyong@fjmu.edu.cn.
References
- 1.Huang J, Lin S, Wan B, Zhu Y. A systematic literature review of syphilitic hepatitis in adults. J Clin Transl Hepatol. 2018;6(3):306–309. doi: 10.14218/JCTH.2018.00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang J, Zhang H, Liu S, Wang M, Wan B, Velani B, et al. Is toxoplasma gondii infection correlated with nonalcoholic fatty liver disease?- a population-based study. BMC Infect Dis. 2018;18(1):629. doi: 10.1186/s12879-018-3547-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lamps LW. Hepatic granulomas: a review with emphasis on infectious causes. Arch Pathol Lab Med. 2015;139(7):867–875. doi: 10.5858/arpa.2014-0123-RA. [DOI] [PubMed] [Google Scholar]
- 4.Harn RD. Syphilis of the liver. Am J Syph. 1943;27:529–562. [Google Scholar]
- 5.Mullick CJ, Liappis AP, Benator DA, Roberts AD, Parenti DM, Simon GL. Syphilitic hepatitis in HIV-infected patients: a report of 7 cases and review of the literature. Clin Infect Dis. 2004;39(10):e100–e105. doi: 10.1086/425501. [DOI] [PubMed] [Google Scholar]
- 6.Rubio-Tapia Alberto, Hujoel Isabel A., Smyrk Thomas C., Poterucha John J. Emerging secondary syphilis presenting as syphilitic hepatitis. Hepatology. 2017;65(6):2113–2115. doi: 10.1002/hep.28974. [DOI] [PubMed] [Google Scholar]
- 7.Aggarwal SK, Radhakrishnan S. Syphilitic hepatitis: look for raised alkaline phosphatase level. Med J Armed Forces India. 2016;72(2):192–193. doi: 10.1016/j.mjafi.2015.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khambaty M, Singal AG, Gopal P. Spirochetes as an almost forgotten cause of hepatitis. Clin Gastroenterol Hepatol. 2015;13(2):A21–A22. doi: 10.1016/j.cgh.2014.09.043. [DOI] [PubMed] [Google Scholar]
- 9.Solari PR, Jones C, Wallace MR. Hepatic lesions with secondary syphilis in an HIV-infected patient. Case Rep Med. 2014;2014:604794. doi: 10.1155/2014/604794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim GH, Kim BU, Lee JH, Choi YH, Chae HB, Park SM, et al. Cholestatic hepatitis and thrombocytosis in a secondary syphilis patient. J Korean Med Sci. 2010;25(11):1661–1664. doi: 10.3346/jkms.2010.25.11.1661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Butler T. The Jarisch-Herxheimer reaction after antibiotic treatment of Spirochetal infections: a review of recent cases and our understanding of pathogenesis. Am J Trop Med Hyg. 2017;96(1):46–52. doi: 10.4269/ajtmh.16-0434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adachi E, Koibuchi T, Okame M, Sato H, Imai K, Shimizu S, et al. Case of secondary syphilis presenting with unusual complications: syphilitic proctitis, gastritis, and hepatitis. J Clin Microbiol. 2011;49(12):4394–4396. doi: 10.1128/JCM.01240-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets supporting the conclusions of this article are included in the article.


