Abstract
Introduction: We assessed changes in screening mammography cost sharing and utilization before and after the Affordable Care Act (ACA) and the revised U.S. Preventive Services Task Force (USPSTF) recommendations by race and income.
Methods: We used Optum™© Clinformatics™® Data Mart deidentified patient-level analytic files between 2004 and 2014. We first visually inspected trends for screening mammography utilization and cost-sharing elimination over time by race and income. We then specifically calculated the slopes and compared trends before and after 2009 and 2010 to assess the impact of ACA implementation and USPSTF recommendation revisions on screening mammography cost-sharing elimination and utilization. All analyses were conducted in 2018.
Results: A total of 1,763,959 commercially insured women, ages 40–74, were included. Comparing trends for cost-sharing elimination before and after the 2010 ACA implementation, a statistically significant but small upward trend was found among all races and income levels with no racial or income disparities evident. However, screening utilization plateaued or showed a significant decline after the 2009 USPSTF recommendation revision in all income and racial groups except for African Americans in whom screening rates continued to increase after 2009.
Conclusions: Impact of ACA cost-sharing elimination did not differ among various racial and income groups. Among our population of employer-based insured women, the racial gap in screening mammography use appeared to have closed and potentially reversed among African American women. Continued monitoring of screening utilization as health care policies and recommendations evolve is required, as these changes may affect race- and income-based disparities.
Keywords: breast cancer screening, affordable care act, cost sharing, screening utilization
Introduction
Breast cancer is the most commonly diagnosed cancer and the second leading cause of cancer death among U.S. women.1 Screening mammography improves early detection of breast cancer leading to better clinical outcomes and reduced morbidity and mortality.2 Screening mammography utilization, however, varies by sociodemographic characteristics, insurance status, and race/ethnicity,3 and disparities in breast cancer screening persist among vulnerable populations. For example, Hispanic women continue to have lower rates of timely screening mammography than both white and African American women.4 In addition, persistent differences in screening mammography utilization are seen based on poverty level and health insurance status.3,5,6 Type of health insurance is also associated with receipt of preventive health services with screening mammography rates being higher among women with public insurance other than Medicare (such as TRICARE, Indian Health Service, or Tribal Health Service coverage) than those with private insurance or Medicare.5
One barrier to screening mammography utilization, which potentially contributes to these disparities, is the out-of-pocket costs for screening.7 Trivedi et al.8 found that an increase in cost sharing for mammography of $10 or more among Medicare beneficiaries was associated with ∼10% lower rates of biennial screening mammography. In a national sample of predominantly rural women, ages 40–64, the elimination of cost sharing after introduction of the National Rural Electric Cooperative Association plan correlated with increased screening mammography utilization.9 As of October 2010, the Affordable Care Act (ACA) mandated elimination of cost sharing for U.S. Preventive Services Task Force (USPSTF) level A or B preventive services, including screening mammography,10 with the goal to improve breast cancer screening utilization and ameliorate disparities in screening. Despite the ACA's elimination of cost sharing, overall screening mammography utilization declined after 200911 suggesting a greater effect of the USPSTF recommendation revision, with similar trends in utilization over time among 40–49- and 50–65-year-old women. In brief, before 2009, the USPSTF recommended screening mammography, with or without clinical breast examination, every 1–2 years for women ages 40 and older.12 In November, 2009, the USPSTF changed its recommendation to biennial screening for women ages 50–74.13 It further withdrew its previous recommendation for routine screening before age 50, noting that the decision to initiate screening should be an individual one that takes into account specific benefits and harms.
It is unclear whether the impact of the ACA cost-sharing elimination and USPSTF recommendation revisions on screening behaviors varies among women of different races or income levels. The primary objective of this study was to identify disparities in screening mammography utilization before and after cost-sharing elimination under the ACA. Disparities by race/ethnicity and poverty status were assessed to identify unique populations that may be more sensitive to cost-sharing elimination.
Methods
This study was deemed exempt by the University of Michigan Medical School Institutional Review Board.
Data and sample
We used deidentified patient-level analytic files between January 2000 and December 2014 from the Optum™© Clinformatics™® Data Mart (OptumInsight, Eden Prairie, Minnesota, U.S.). The Optum Clinformatics Data Mart includes member enrollment data such as demographic variables and individual-level insurance claims. The advantages of this data source include its large size (75 million unique members as of the time of the study), its inclusion of race, income, and household size, and the ability to follow individuals longitudinally as individuals are reported by employers not health plans. It also contains complete patient payment and charge information, including patient copayment, deductible, and coinsurance amounts, and standardized costs.
Our sample included women ages 40–74 enrolled in employer-based health plans between 2004 and 2014 (1) without a history of breast cancer or prior mastectomy, (2) with at least 12 months of continuous enrollment in a given plan for the plan year, and (3) enrollment in one plan for a given calendar year.
Measures and outcomes
The primary outcomes were screening mammography utilization and cost-sharing elimination over time stratified by the independent variables of race/ethnicity and poverty status. Screening mammography utilization was calculated as the proportion of all women with at least one claim for that service among all women enrolled for each year. For women with more than one screening mammogram claim in a calendar year, only the first service claim was included in the analyses. Patient cost sharing (total out-of-pocket costs) at each calendar year was calculated for each patient who underwent screening mammography as the sum of patient copayments, coinsurance, and deductible payments. Cost-sharing elimination of screening mammography was defined as zero patient cost sharing for the service. The proportion of women without cost sharing for screening mammography each year was calculated as a proportion of those with first dollar coverage divided by all screening mammography users. We characterized poverty status as a dichotomous variable: “income ≤400% of federal poverty level” and “income >400% of federal poverty level” based on 2014 Census Bureau poverty guidelines by household size.14
Analysis
Demographic characteristics, screening mammography utilization, and cost-sharing elimination were summarized by descriptive statistics. Trends for screening mammography utilization and cost-sharing elimination over time were first visually inspected. For cost-sharing elimination, we then specifically calculated the slopes and compared trends before and after 2010 to assess the impact of ACA implementation on cost-sharing elimination. For screening mammography utilization, we specifically calculated the slopes and compared trends before and after 2009 to examine the impact of USPSTF recommendations on screening utilization, as visual inspection of patterns for screening mammography utilization showed change in 2009. All analyses were performed and presented for each year of service stratified by race/ethnicity and poverty status.
All analyses were conducted in 2018 using Stata (StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP) and SAS 9.4 (SAS Institute, Cary, NC).
We conducted a subanalysis of annual screening utilization and cost-sharing elimination by race and income among women 50 and older, the population for whom the 2009 USPSTF recommendations specifically recommend screening.
Results
Sample characteristics
We identified an average of 1,763,959 commercially insured women in a given plan per year meeting our inclusion criteria. Characteristics of members and their health plans have previously been described.15 Screening mammography utilization and cost-sharing elimination for each year of service and by race/ethnicity and poverty status are summarized in Tables 1 and 2, respectively.
Table 1.
Patterns of Screening Utilization and Cost Sharing by Race/Ethnicity Among Women Ages 40–74
| Total eligible women | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1,541,293 | 1,682,880 | 1,717,175 | 1,812,643 | 1,877,042 | 1,899,439 | 1,822,460 | 1,859,587 | 1,834,060 | 1,806,802 | 1,550,172 | ||||||||||||
| Screening utilization | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
| Race/Ethnicity | ||||||||||||||||||||||
| Screening utilization among Asian race | 11,936 | 32.1 | 14,574 | 35.3 | 16,654 | 37.5 | 19,061 | 38.9 | 21,486 | 39.4 | 23,222 | 40.5 | 22,773 | 39.2 | 23,370 | 38.8 | 23,477 | 37.1 | 24,534 | 36.9 | 21,711 | 35.5 |
| Screening utilization among African American race | 38,806 | 32.5 | 46,141 | 34.0 | 53,928 | 36.1 | 69,789 | 37.8 | 76,517 | 37.4 | 83,930 | 38.5 | 77,838 | 38.3 | 78,371 | 38.6 | 75,001 | 38.6 | 74,136 | 39.1 | 51,656 | 35.9 |
| Screening utilization among Hispanic ethnicity | 31,298 | 30.5 | 38,421 | 32.8 | 45,118 | 35.0 | 49,480 | 35.8 | 53,524 | 36.6 | 56,430 | 38.0 | 50,705 | 36.3 | 55,073 | 37.3 | 52,956 | 36.2 | 54,533 | 36.6 | 52,952 | 35.7 |
| Screening utilization among Unknown race | 28,210 | 36.3 | 30,399 | 38.7 | 30,651 | 40.5 | 30,365 | 41.9 | 30,324 | 42.1 | 30,778 | 43.3 | 28,873 | 41.9 | 29,481 | 41.7 | 28,871 | 40.8 | 29,522 | 41.7 | 26,046 | 40.4 |
| Screening utilization among Caucasian race | 423,085 | 37.5 | 493,729 | 39.7 | 530,995 | 41.5 | 570,569 | 42.7 | 588,346 | 43.0 | 603,527 | 43.9 | 565,162 | 42.7 | 569,604 | 42.3 | 552,740 | 41.6 | 549,520 | 42.4 | 461,410 | 41.2 |
| Zero cost share | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Race/Ethnicity | ||||||||||||||||||||||
| Proportion of Asian race with zero cost share | 9,834 | 82.4 | 12,309 | 84.5 | 14,409 | 86.5 | 16,820 | 88.3 | 18,372 | 85.5 | 21,000 | 90.4 | 20,943 | 92.0 | 22,712 | 97.2 | 22,908 | 97.6 | 24,038 | 98.0 | 21,358 | 98.4 |
| Proportion of African American race with zero cost share | 31,557 | 81.3 | 38,035 | 82.4 | 47,619 | 88.3 | 63,307 | 90.7 | 68,784 | 89.9 | 77,933 | 92.9 | 73,912 | 95.0 | 76,783 | 98.0 | 73,464 | 98.8 | 72,940 | 98.4 | 50,728 | 98.2 |
| Proportion of Hispanic ethnicity with zero cost share | 26,706 | 85.3 | 33,487 | 87.2 | 40,204 | 89.1 | 44,491 | 89.9 | 47,975 | 89.6 | 52,131 | 92.4 | 46,971 | 92.6 | 53,798 | 97.7 | 51,632 | 97.5 | 53,199 | 97.6 | 52,075 | 98.3 |
| Proportion of unknown race with zero cost share | 23,183 | 82.2 | 25,440 | 83.7 | 26,933 | 87.9 | 27,046 | 89.1 | 26,812 | 88.4 | 28,167 | 91.5 | 26,683 | 92.4 | 28,432 | 96.4 | 27,984 | 96.9 | 28,741 | 97.4 | 25,574 | 98.2 |
| Proportion of Caucasian race with zero cost share | 344,876 | 81.5 | 410,125 | 83.1 | 466,196 | 87.8 | 508,992 | 89.2 | 522,570 | 88.8 | 555,332 | 92.0 | 525,401 | 93.0 | 550,934 | 96.7 | 536,346 | 97.0 | 536,164 | 97.6 | 453,212 | 98.2 |
Table 2.
Patterns of Screening Utilization and Cost Sharing by Poverty Status Among Women Ages 40–74
| Characteristic | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total eligible women | 1,541,293 | 1,682,880 | 1,717,175 | 1,812,643 | 1,877,042 | 1,899,439 | 1,822,460 | 1,859,587 | 1,834,060 | 1,806,802 | 1,550,172 | |||||||||||
| Screening utilization | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
| Poverty status | ||||||||||||||||||||||
| Screening utilization among ≤400% FPL | 56,374 | 33.9 | 77,401 | 35.7 | 97,288 | 37.0 | 132,845 | 37.8 | 164,661 | 37.0 | 183,251 | 37.8 | 168,307 | 36.8 | 168,388 | 36.0 | 162,801 | 35.6 | 162,099 | 36.3 | 131,170 | 34.8 |
| Screening utilization among >400% FPL | 194,839 | 39.7 | 252,683 | 41.9 | 306,938 | 43.6 | 395,018 | 44.7 | 490,927 | 44.4 | 548,867 | 45.4 | 517,617 | 44.2 | 529,640 | 44.1 | 515,719 | 43.3 | 513,902 | 44.1 | 431,200 | 42.9 |
| Zero cost share | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Poverty status | ||||||||||||||||||||||
| Proportion ≤400% FPL with zero cost share | 45,033 | 79.9 | 63,260 | 81.7 | 83,418 | 85.7 | 117,222 | 88.2 | 146,757 | 89.1 | 168,524 | 92.0 | 156,968 | 93.3 | 164,015 | 97.4 | 158,640 | 97.4 | 158,485 | 97.8 | 128,943 | 98.3 |
| Proportion >400% FPL with zero cost share | 159,302 | 81.8 | 211,458 | 83.7 | 269,267 | 87.7 | 351,900 | 89.1 | 434,371 | 88.5 | 505,466 | 92.1 | 481,725 | 93.1 | 512,453 | 96.8 | 500,742 | 97.1 | 501,789 | 97.6 | 423,582 | 98.2 |
Cost-sharing elimination over time
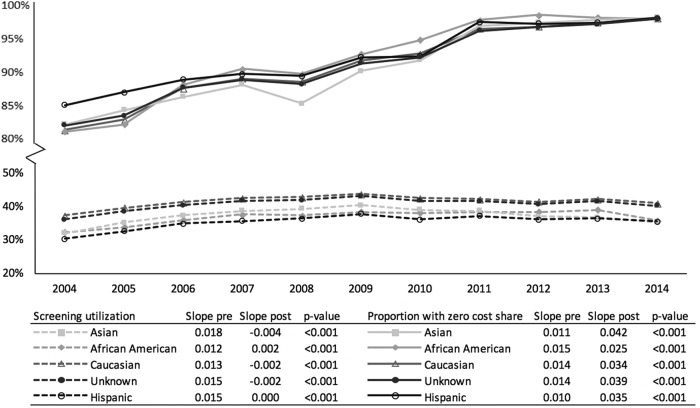
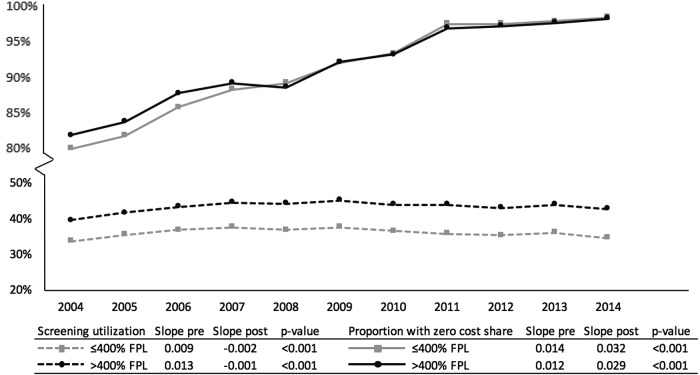
Overall, an upward trend was seen in the proportion of women with zero cost sharing over time among all races/ethnicities (Fig. 1) and income levels (Fig. 2). The trend lines for different races and income levels appeared to have greater slopes from 2004 to 2010 while converging and reaching a plateau in 2010–2011. No racial or income disparities were evident after 2011. Comparing trends for cost-sharing elimination before and after 2010, a statistically significant upward but small trend was found among all races (Fig. 1) and income levels (Fig. 2).
FIG. 1.
Elimination of cost sharing for screening mammography before and after the 2010 ACA implementation and mammography screening utilization before and after the USPSTF breast screening recommendation revision, by race and among women ages 40–74. ACA, Affordable Care Act; USPSTF, U.S. Preventive Services Task Force.
FIG. 2.
Elimination of cost sharing for screening mammography before and after the 2010 ACA implementation and mammography screening utilization before and after the USPSTF breast screening recommendation revision, by income level and among women ages 40–74.
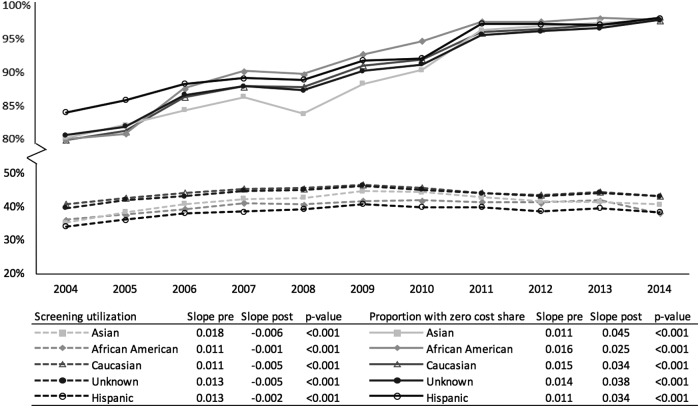
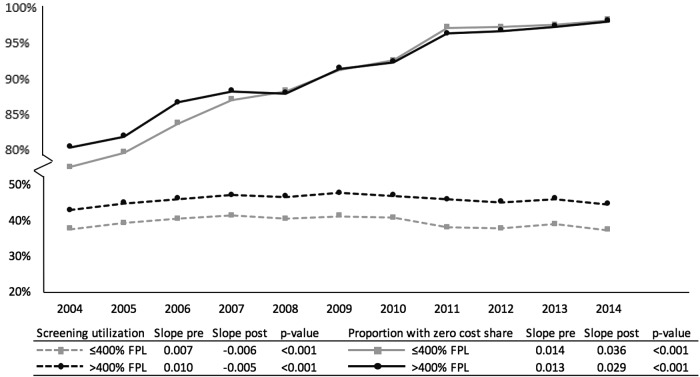
The trends for cost-sharing elimination by race (Fig. 3) and income (Fig. 4) among those 50 and older mirrored the population at large.
FIG. 3.
Elimination of cost sharing for screening mammography before and after the 2010 ACA implementation and mammography screening utilization before and after the USPSTF breast screening recommendation revision, by race and among women ages 50–74.
FIG. 4.
Elimination of cost sharing for screening mammography before and after the 2010 ACA implementation and mammography screening utilization before and after the USPSTF breast screening recommendation revision, by income level and among women ages 50–74.
Screening mammography utilization over time
Screening mammography utilization showed a small upward trend from 2004 to 2009 among all races, while reaching a plateau or trending downward after 2009 in all races except for African Americans (Fig. 1). Comparing slopes for screening mammography utilization before and after 2009 by race/ethnicity, Caucasians and Asians showed a statistically significant decline in screening utilization after 2009, while African Americans were the only racial group who demonstrated a statistically significant increase in screening utilization after 2009 (Fig. 1).
Screening mammography utilization showed a small upward trend from 2004 to 2009 among women with both income levels ≤400% FPL and >400% FPL, while demonstrating a comparable downward trend in both groups after 2009 (Fig. 2). Comparing slopes for screening mammography utilization before and after 2009 by poverty status, both women with income levels ≤400% FPL and >400% FPL showed a significant downward trend after 2009 (Fig. 2).
Regarding the subanalyses of screening utilization by race and income among those 50 and older, we demonstrated that African American women in this age group experienced a plateau in screening utilization after 2009 rather than a decline in other groups (Table 3 and Fig. 3). The trends in screening utilization by income in this older population mirrored the population at large (Table 4 and Fig. 4).
Table 3.
Patterns of Screening Utilization and Cost Sharing by Race/Ethnicity Among Women Ages 50–74
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total eligible women | 792,555 | 901,679 | 940,845 | 1,030,424 | 1,084,522 | 1,106,122 | 1,065,851 | 1,105,982 | 1,098,146 | 1,092,012 | 939,417 | |||||||||||
| Screening utilization | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
| Race/Ethnicity | ||||||||||||||||||||||
| Screening utilization among Asian race | 5,633 | 35.3 | 7,075 | 38.5 | 8,249 | 41.0 | 9,647 | 42.5 | 10,895 | 42.8 | 11,795 | 44.8 | 11,738 | 44.5 | 11,906 | 43.0 | 12,011 | 41.8 | 12,596 | 41.6 | 11,379 | 40.8 |
| Screening utilization among African American race | 22,288 | 36.2 | 27,107 | 37.7 | 31,811 | 39.4 | 44,060 | 41.3 | 48,553 | 40.8 | 53,453 | 41.9 | 49,619 | 42.1 | 49,274 | 41.6 | 47,090 | 41.4 | 46,998 | 42.0 | 31,871 | 38.3 |
| Screening utilization among Hispanic ethnicity | 15,586 | 34.2 | 19,556 | 36.3 | 23,103 | 38.2 | 25,634 | 38.7 | 28,054 | 39.4 | 29,874 | 41.0 | 27,272 | 40.1 | 29,423 | 40.1 | 28,537 | 38.9 | 30,129 | 39.7 | 29,432 | 38.6 |
| Screening utilization among unknown race | 15,317 | 39.8 | 17,030 | 42.2 | 17,169 | 43.2 | 17,564 | 44.9 | 17,960 | 45.2 | 18,423 | 46.4 | 17,636 | 45.3 | 18,018 | 44.1 | 17,849 | 43.2 | 18,646 | 44.4 | 16,565 | 43.2 |
| Screening utilization among Caucasian race | 242,065 | 40.9 | 292,922 | 42.8 | 318,732 | 44.3 | 355,320 | 45.6 | 371,852 | 45.7 | 384,554 | 46.7 | 367,409 | 45.9 | 368,536 | 44.4 | 360,214 | 43.7 | 363,748 | 44.7 | 306,682 | 43.4 |
| Zero cost share | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Race/Ethnicity | ||||||||||||||||||||||
| Proportion of Asian race with zero cost share | 4,528 | 80.4 | 5,824 | 82.3 | 6,971 | 84.5 | 8,347 | 86.5 | 9,149 | 84.0 | 10,439 | 88.5 | 10,628 | 90.5 | 11,494 | 96.5 | 11,676 | 97.2 | 12,294 | 97.6 | 11,161 | 98.1 |
| Proportion of African American race with zero cost share | 17,881 | 80.2 | 21,966 | 81.0 | 27,916 | 87.8 | 39,843 | 90.4 | 43,661 | 89.9 | 49,654 | 92.9 | 47,065 | 94.9 | 48,200 | 97.8 | 46,065 | 97.8 | 46,199 | 98.3 | 31,271 | 98.1 |
| Proportion of Hispanic ethnicity with zero cost share | 13,127 | 84.2 | 16,809 | 86.0 | 20,447 | 88.5 | 22,885 | 89.3 | 25,001 | 89.1 | 27,485 | 92.0 | 25,159 | 92.3 | 28,686 | 97.5 | 27,781 | 97.4 | 29,327 | 97.3 | 28,937 | 98.3 |
| Proportion of unknown race with zero cost share | 12,375 | 80.8 | 13,977 | 82.1 | 14,903 | 86.8 | 15,476 | 88.1 | 15,721 | 87.5 | 16,660 | 90.4 | 16,120 | 91.4 | 17,268 | 95.8 | 17,189 | 96.3 | 18,054 | 96.8 | 16,233 | 98.0 |
| Proportion of Caucasian race with zero cost share | 193,979 | 80.1 | 238,434 | 81.4 | 275,826 | 86.5 | 313,105 | 88.1 | 327,122 | 88.0 | 350,535 | 91.2 | 338,343 | 92.1 | 354,646 | 96.2 | 348,193 | 96.7 | 353,753 | 97.3 | 300,639 | 98.0 |
Table 4.
Patterns of Screening Utilization and Cost Sharing by Poverty Status Among Women Ages 50–74
| Characteristic | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total eligible women | 792,555 | 901,679 | 940,845 | 1,030,424 | 1,084,522 | 1,106,122 | 1,065,851 | 1,105,982 | 1,098,146 | 1,092,012 | 939,417 | |||||||||||
| Screening utilization | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | N |
| Poverty status | ||||||||||||||||||||||
| Screening utilization among ≤400% FPL | 35,792 | 37.8 | 50,029 | 39.5 | 61,152 | 40.6 | 84,481 | 41.5 | 101,605 | 40.7 | 111,240 | 41.4 | 101,423 | 40.9 | 97,694 | 38.3 | 94,234 | 37.9 | 94,550 | 39.1 | 75,295 | 37.5 |
| Screening utilization among >400% FPL | 113,227 | 43.1 | 151,901 | 45.0 | 186,120 | 46.2 | 248,036 | 47.3 | 311,036 | 46.8 | 350,832 | 47.9 | 338,940 | 47.1 | 347,056 | 46.1 | 341,244 | 45.3 | 345,755 | 46.2 | 291,472 | 44.7 |
| Zero cost share | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % | N | % |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Poverty status | ||||||||||||||||||||||
| Proportion ≤400% FPL with zero cost share | 27,789 | 77.6 | 39,806 | 79.6 | 51,191 | 83.7 | 73,494 | 87.0 | 89,664 | 88.2 | 101,429 | 91.2 | 93,823 | 92.5 | 94,844 | 97.1 | 91,609 | 97.2 | 92,182 | 97.5 | 73,947 | 98.2 |
| Proportion >400% FPL with zero cost share | 91,040 | 80.4 | 124,432 | 81.9 | 161,219 | 86.6 | 218,714 | 88.2 | 273,269 | 87.9 | 320,497 | 91.4 | 312,814 | 92.3 | 334,143 | 96.3 | 330,054 | 96.7 | 336,570 | 97.3 | 285,737 | 98.0 |
Discussion
Among our sample of employer-based insured women, we found an upward trend in the proportion of women with zero cost sharing for screening mammography both before and after 2010 among all races/ethnicities and income levels. By 2010, when ACA mandated cost-sharing elimination for screening mammography, >90% of women in our sample already had zero cost share for screening mammography, independent of their race/ethnicity or poverty status. After 2010, a small increase in cost-sharing elimination was seen among all races and income levels with no evident racial or income disparities with respect to the impact of ACA provision on screening mammography cost-sharing elimination.
Despite the universal upward trend in cost-sharing elimination, in our sample of employer-based insured women, screening mammography utilization plateaued or showed a significant decline after 2009 in all income and racial groups except for African Americans.
Extensive efforts to improve breast cancer screening predate the ACA, including the near-complete elimination of financial barriers to breast screening in the employed insured population. In a recent study, Carlos et al.15 suggested that we may be experiencing a ceiling effect in further responses of screening rates to financial incentives that reduce screening cost. Our findings build on prior works to show that this ceiling effect is likely similar among all races/ethnicities and income levels. Screening mammography utilization among our sample of insured women appeared, however, to be more influenced by the 2009 USPSTF revised recommendations. We have previously shown a general decline in screening mammography utilization in the years following the implementation of the 2009 USPSTF recommendations.11 In this study, examining race-specific rates and trends enabled us to show that screening mammography utilization has continued to increase among African American women even after the implementation of the USPSTF recommendations in 2009. In African American women 50 and older, the screening utilization appeared to plateau rather than frankly decline as in the other races and ethnicities. This finding suggests that the increase in utilization among African American women is concentrated in younger women, 40–49-year olds.
Lee et al.16 showed that the release of the revised 2009 USPSTF recommendations for screening mammography was associated with a decline in screening mammography utilization among white, but not African American, women. As breast cancer mortality rate remains higher among African American women, it has been suggested that African American women may better perceive the benefits of screening mammography.17 Similarly, we can speculate that physician recommendations for screening mammography may vary across different racial groups based on prognosis and mortality rates.
Future research is needed to clarify why impact of USPSTF recommendation revisions on screening behaviors varies among women with different races. Nevertheless, these findings suggest that the racial gap in screening mammography has closed and potentially reversed among African American women with employer-based health insurance plans. It is important to continue monitoring screening utilization as health care policies and guidelines change, as these changes may affect disparities in screening between different racial and income groups.
A strength of this study is the use of large patient-level data set, including patient demographics (e.g., race and income) and payment (e.g., copayment and deductible) information, which allowed us to describe and assess patterns of screening mammography utilization and cost-sharing elimination over time by race and income level. However, there are a number of limitations to our study. First, our descriptive cross-sectional design limited our ability to determine causal associations between cost-sharing elimination and screening mammography utilization. In addition, we cannot assess whether individual women experienced reductions in their cost sharing or changed their use of screening mammography in response. Furthermore, our sample of employed insured women has potentially resulted in underestimation of racial and income disparities in screening mammography utilization. Lastly, while using administrative data offers the opportunity to examine changes in large populations, there are inherent weaknesses such as variation in coding and billing.
Acknowledgments
This study was coordinated by the ECOG-ACRIN Cancer Research Group (Peter O'Dwyer, MD, and Mitchell D. Schnall, MD, PhD, Group Co-Chairs) and supported by the National Cancer Institute of the National Institutes of Health under the following award numbers: CA189828, CA180801. SFD is supported by NIH T32 EB005970-09. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, nor does mention of trade names, commercial products, or organizations imply endorsement by the U.S. government.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Siegel RL, Miller KD, Jemal A. Cancer Statistics, 2017. CA Cancer J Clin 2017;67:7–30 [DOI] [PubMed] [Google Scholar]
- 2. Elmore JG, Armstrong K, Lehman CD, Fletcher SW. Screening for breast cancer. JAMA 2005;293:1245–1256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Sabatino SA, White MC, Thompson TD, Klabunde CN, Centers for Disease C, Prevention. Cancer screening test use - United States, 2013. MMWR Morb Mortal Wkly Rep 2015;64:464–468 [PMC free article] [PubMed] [Google Scholar]
- 4.American Cancer Society, Breast Cancer Facts & Figures 2017–2018. Available at: www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/breast-cancer-facts-and-figures/breast-cancer-facts-and-figures-2017-2018.pdf Accessed April1, 2019
- 5. Zhao G, Okoro CA, Li J, Town M. Health Insurance Status and Clinical Cancer Screenings Among U.S. Adults. Am J Prev Med 2018;54:e11–e19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. DeSantis C, Siegel R, Bandi P, Jemal A. Breast cancer statistics, 2011. CA Cancer J Clin 2011;61:409–418 [DOI] [PubMed] [Google Scholar]
- 7. Ayanian JZ, Landon BE, Zaslavsky AM, Newhouse JP. Racial and ethnic differences in use of mammography between Medicare Advantage and traditional Medicare. J Natl Cancer Inst 2013;105:1891–1896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Trivedi AN, Rakowski W, Ayanian JZ. Effect of cost sharing on screening mammography in Medicare health plans. N Engl J Med 2008;358:375–383 [DOI] [PubMed] [Google Scholar]
- 9. Peppercorn J, Horick N, Houck K, et al. Impact of the elimination of cost sharing for mammographic breast cancer screening among rural US women: A natural experiment. Cancer 2017;123:2506–2515 [DOI] [PubMed] [Google Scholar]
- 10. Koh HK, Sebelius KG. Promoting prevention through the Affordable Care Act. N Engl J Med 2010;363:1296–1299 [DOI] [PubMed] [Google Scholar]
- 11. Dehkordy SF, Hall KS, Roach AL, Rothman ED, Dalton VK, Carlos RC. Trends in Breast Cancer Screening: Impact of U.S. Preventive Services Task Force Recommendations. Am J Prev Med 2015;49:419–422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. U.S. Preventive Services Task Force. Screening for Breast Cancer: Recommendations and Rationale. Ann Intern Med 2002;137 (Part 1):344–346 [DOI] [PubMed] [Google Scholar]
- 13. Final Update Summary: Breast Cancer: Screening. U.S. Preventive Services Task Force: 2016. Available at: www.uspreventiveservicestaskforce.org/Page/Document/UpdateSummaryFinal/breast-cancer-screening Accessed April1, 2019
- 14. DeNavas-Walt C, Proctor BD. Income and Poverty in the United States: 2014. Available at: https://census.gov/content/dam/Census/library/publications/2015/demo/p60-252.pdf
- 15. Carlos R, Kolenic G, Fendrick AM, et al. Patterns of Cost-Sharing in Breast Cancer Screening Among Commercially Insured Women: Impact of the Affordable Care Act AcademyHealth Annual Research Meeting. 2017. Available at: https://academyhealth.confex.com/academyhealth/2017arm/meetingapp.cgi/Paper/18972
- 16. Lee JY, Malak SF, Klimberg VS, Henry-Tillman R, Kadlubar S. Change in Mammography Use Following the Revised Guidelines from the U.S. Preventive Services Task Force. Breast J 2017;23:164–168 [DOI] [PubMed] [Google Scholar]
- 17. Haggstrom DA, Schapira MM. Black-white differences in risk perceptions of breast cancer survival and screening mammography benefit. J Gen Intern Med 2006;21:371–377 [DOI] [PMC free article] [PubMed] [Google Scholar]