Abstract
Background: Current evidence demonstrates that, while a widely used tool for childhood obesity prevention, school-based BMI reports do not effectively reduce pediatric obesity. The purpose of this study was to examine the presumed mechanisms by which BMI reporting might impact child weight by assessing parents': (1) recall of BMI reports, (2) accuracy in recalling child overweight status, and (3) reactions to BMI reports.
Methods: Mailed surveys were completed by 2205 racially/ethnically diverse parents of third- to seventh-grade students participating in the Fit Study who had either been exposed to 1 year of child BMI reporting (one report) or 2 years (two reports).
Results: After 1 year of BMI reporting, parents of children with overweight were less likely [odds ratio (OR) = 0.7, 95% confidence interval (CI): 0.5–0.9] to recall receiving a BMI report and less likely (OR = 0.2, 95% CI: 0.1–0.3) to accurately recall their child's weight status from the BMI report, compared with parents of children with healthy weight. Differences in accuracy of child weight status recall persisted after 2 years of BMI reporting exposure. Only 22% of parents of children at risk for overweight and with overweight reported being surprised by the results.
Conclusions: Parents' recall of receiving a school-based BMI report is low, as is the accuracy of recall of child's overweight status. Additionally, parents' surprise at, and concern for, BMI results is limited. Current BMI reports may be ineffective at reducing pediatric obesity due to their lack of salience and ability to compel meaningful behavior change among parents.
Keywords: BMI reports, childhood overweight and obesity, parental recall, school health intervention
Introduction
BMI screening and reporting is widely implemented in public schools to address pediatric obesity,1 which impacts nearly 1 in 5 children in the United States.2 BMI reports are intended to compel parents to make healthy dietary and physical activity changes for their children with overweight or obesity, leading to improvements in child weight status. A recent systematic review suggests that current school-based BMI reports do not reduce childhood obesity,3 warranting a critical analysis of the presumed mechanism by which BMI reporting might impact child weight.
First, for BMI reports to influence parent behavior related to their child's health and weight, reports must be salient to parents, remaining prominent in their minds over an extended period of time. Results from prior studies are inconclusive, however, regarding how likely parents are to remember even receiving a BMI report.4–7 In addition, even though many states require BMI assessments in multiple grades, no prior studies have evaluated the impact of consecutive years of BMI reporting on parent recall of report receipt.8
Second, BMI reports should also help parents correctly identify their child's weight status, so that appropriate behavior modifications can be made, as necessary, to improve student weight. Prior research demonstrates that parents have poor recognition of their child's weight status,6,9,10 particularly parents of children with overweight or obesity.11 While providing parents with a BMI report containing their child's weight status, along with healthy behavior-modification tips, could help parents more accurately recognize their child's weight status4 and compel positive weight-related changes3,12; current evidence in this area is mixed. Prior studies conducted among primarily white populations6,9 suggest that parent accuracy in identifying their child's overweight status does not significantly increase following BMI reporting. Results from an English study (conducted with 66% white parents) showed that the proportion of parents who correctly recognized their child was overweight increased 16% after BMI reporting11; however recognition remained relatively low, with only 38% of parents accurately recalling their child's weight status postreporting. Further evidence is needed to determine if BMI reports actually help improve parental recognition of their child's weight status, particularly among parents from diverse racial/ethnic backgrounds.
Finally, in addition to helping parents accurately recognize their child's weight status, BMI reports must also be understood and viewed as providing relevant, motivating information by parents, if they are to compel positive behavior changes in response to the results.13 BMI reporting shows promise for increasing parental recognition of the health risks associated with child overweight in non-white ethnic groups.11 Few studies to date have examined whether parents find reports helpful14 or whether reports provide concerning or surprising information about child weight status.5
To address these gaps, this article uses parent survey data to examine racially/ethnically diverse elementary and middle school parents': (1) recall of BMI reports; (2) accuracy in recalling child overweight status; and (3) reactions to BMI reports.
Methods
Study Design
This repeated cross-sectional study used parent survey data from the Fit Study, a 3-year, cluster-randomized trial examining the impact of school-based BMI reporting on pediatric obesity.15 Students in the Fit Study (grades 3–7 in California public schools) were recruited in two cohorts during the 2014–2015 and 2015–2016 school years. Participating students in the intervention arm had their BMI assessed in school in the spring of 2015 and 2016; students in grades 5–8 also participated in 5 fitness tests that assessed strength, flexibility, and aerobic capacity.16 BMI reports were sent to parents in October of each year, ∼6 months after the student's BMI had been assessed. BMI reports, described previously,17 classified children as “Overweight” (≥95th percentile), “At-risk-of-overweight” (≥85th percentile and <95th), “At a healthy weight” (≥5th and <85th percentile) or “Underweight” (<5th percentile) based on CDC definitions.18 In BMI report pretests, parents preferred “at-risk for overweight” and “overweight” to the CDC's “overweight” and “obese” when describing students in the ≥85th through the >95th and ≥95th percentiles for BMI, respectively, so these terms were used in all Fit Study BMI reports.17 Students in grades 5–8 were randomly assigned to receive either the standard BMI report or a report that also included fitness results. The reverse side of all reports included colorful pictures with family oriented health information (e.g., “Physical activity is important for children and adults of all ages. Being active as a family is good for everyone”; “Set a rule that no one can spend longer than 2 hours per day playing videogames, watching TV, and using the computer (except for school work)”; and “Make half your plate fruits and vegetables”) and a suggestion that parents talk to their schools about how to make them healthier places for students.17 This study was approved by UC Berkeley's Committee for the Protection of Human Subjects.
Parent Follow-Up Survey Sample
The present study is limited to parents or caregivers (hereafter referred to as parents) who received a BMI report for their child in Fall 2015 or Fall 2016 (surveys mailed to 6010 parents). In Spring 2016, ∼25 parents from 27 intervention schools (n = 698) were randomly selected to receive a survey, roughly 6 months after BMI reports had been mailed. Researchers used stratified sampling to achieve a 2:1 ratio of students at risk for overweight/with overweight to students with underweight/healthy weight. Although the original study protocol only included a single follow-up survey, after results from 2016 revealed low parental recall of BMI reports, researchers sent a second follow-up survey to all intervention-arm parents (n = 5312) in Spring 2017. Parents completing a survey in Spring 2017 had previously received either 1 or 2 BMI reports.
Researchers sent a prenotification postcard to all selected parents before mailing the baseline survey. The postcard indicated that a survey would arrive within 1 week and asked parents to complete it. The following week, parents received a paper survey that included a preaddressed, stamped return envelope and a 1-dollar bill. The survey also included a website URL that parents could use to complete the survey online. Parents who did not return a completed survey within 3 weeks received another mailed survey. Previous research indicates that prenotification postcards, monetary incentives, and duplicate surveys significantly increase response rates.19 Parents received one survey in English and one survey in Spanish or Chinese, based on school district policy.
Survey Content
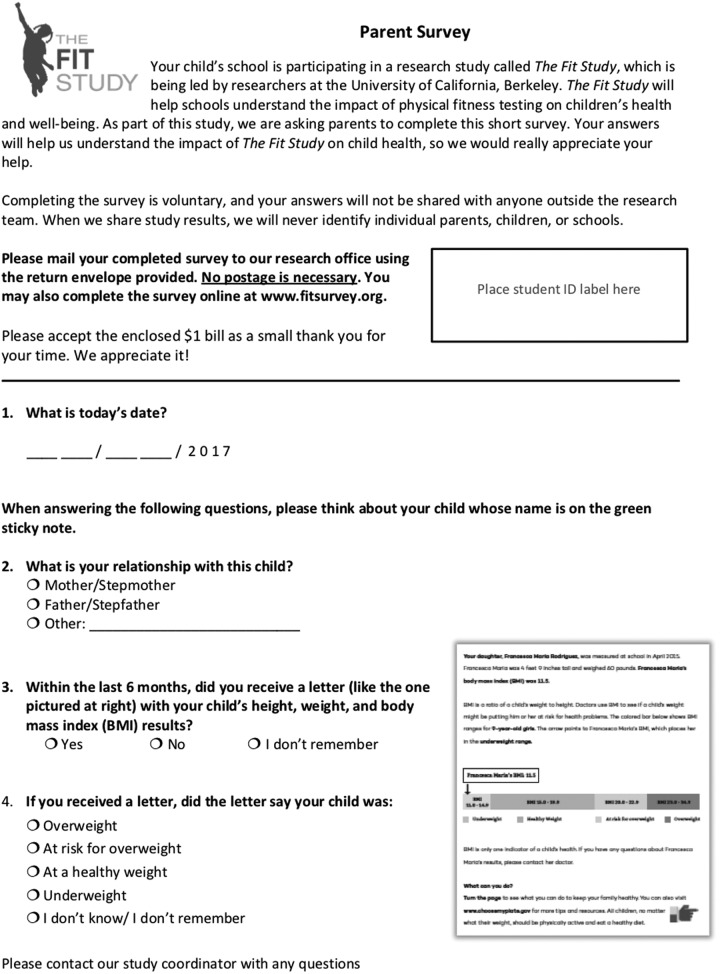
The 2016 and 2017 surveys asked parents if they recalled receiving a report with their child's height and weight results from the previous school year and, if so, how the report had categorized their child's weight status (overweight, at risk for overweight, at a healthy weight, or underweight). To aid in parents' recall of the report, the 2017 survey included an image of an actual report (visual prompt; Fig. 1), measuring 2.5 × 3 inches on the printed page. Both surveys asked parents to report their relationship to their child; the 2016 survey also asked parents to self-report their race/ethnicity, gender, height, and weight.
Figure 1.
Year 2017 parent survey with accompanying recall question (visual prompt).
The 2016 survey assessed parent reactions to the report by asking if parents: (1) understood the information on the report; (2) found the report helpful for themselves; (3) were concerned about their child's results; (4) were surprised about their child's results. Parents responded to each question using a 5-point Likert scale and responses were converted into a binary score of agreement (“strongly disagree/disagree/neither agree nor disagree” or “strongly agree/agree”).
Statistical Analyses
Parents whose child was absent for height and weight measurements (n = 121) were dropped from analyses. A logistic mixed effects regression model, including study year and child grade, sex, weight status, and race was run to assess potential predictors of parental survey response. An indicator variable was set to 1 if a parent accurately recalled their child's reported weight status (accuracy). Mixed effects logistic regression models assessed associations between accuracy and recall of receiving a report (recall). Model 1 was limited to parents who had received only 1 BMI report and assessed whether receiving the survey with the visual (Fig. 1) in 2017 vs. no visual in 2016 increased recall or accuracy. Model 2 was limited to parents surveyed in 2017 (who could have received 1 or 2 reports) to examine whether the number of reports received was associated with recall or accuracy. Model 3, limited to parents of children in grades 5 and above, compared recall and accuracy by report type (BMI only or BMI + fitness). All models included a random effect for school (Model 3 also included a random effect for student) and controlled for: study year (when appropriate); time elapsed between mailing of BMI report and survey completion; school-level proportion of students who qualify for free or reduced-price meals [a proxy for socioeconomic status (SES)]; and child race/ethnicity, grade, sex, and weight status. Statistical analyses were performed using Stata SE v15.1 (StataCorp LLC, College Station, TX).
Results
A total of 2205 parent surveys were returned representing data on unique students (369 were returned in 2016 and 1836 were returned in 2017, with 1249 surveys completed after having received 1 BMI report and 956 after having received 2 BMI reports; 124 parents completed 2 follow-up surveys and we excluded their second survey). Race was the only significant predictor of parent response rates: 28% for African American students, 32% for Hispanic students, 48% for white students, and 52% for Asian students (p = <0.001). Table 1 presents demographic characteristics of students whose parents responded to a survey. Among parents contributing demographic information (parent demographic questions were only asked on the 2016 survey; n = 369), 41% were Hispanic, 26% were non-Hispanic white, 25% were non-Hispanic Asian, and 5% were non-Hispanic Black. Additionally, 30% had a high school degree or less; 24% attended some college; 33% were college graduates; and 14% attended graduate school. Eighty-four percent were female.
Table 1.
Characteristics of Children Whose Parents Responded to the Survey
| Child characteristics | (n = 2205) |
|---|---|
| Sex, n (%) | |
| Male | 1170 (53) |
| Female | 1035 (47) |
| Grade, n (%) | |
| 4th | 656 (30) |
| 5th | 579 (26) |
| 6th | 256 (12) |
| 7th | 390 (18) |
| 8th | 324 (15) |
| Race, n (%) | |
| Hispanic | 987 (45) |
| Non-Hispanic white | 450 (20) |
| Non-Hispanic Asian | 622 (28) |
| Non-Hispanic black | 64 (3) |
| Weight statusa, n (%) | |
| BMI <5th %tile | 91 (4) |
| BMI ≥5th and <85th %tile | 1343 (61) |
| BMI ≥58th and <95th %tile | 408 (19) |
| BMI ≥95th %tile | 363 (16) |
Sample was stratified to ensure that two-thirds of parents who received surveys had a child with a BMI at or above the 85th percentile.
Recall of Report
Recall was 53% among parents who received 1 BMI report and 71% among parents who received 2 reports. Among parents who had only received 1 BMI report (Model 1), parents who saw the visual prompt had greater recall than those without a visual prompt [odds ratio (OR) = 1.9, 95% confidence interval (CI): 1.2–3.2]. Among parents surveyed in 2017 (Model 2), those who had received 2 prior reports had greater recall than those who had received only 1 prior report (OR = 1.5, 95% CI: 1.1–2.1). In Model 2, African American parents had half the odds of recalling the report as Hispanic parents (OR = 0.5, 95% CI: 0.3–0.97). There were no differences in recall rates with white parents as the reference group. Report type (BMI only vs. BMI-plus-fitness; Model 3) was not associated with recall (OR = 1.0, 95% CI: 0.7–1.3).
Table 2 presents recall rates by child weight status following 1 and 2 years of BMI reporting. Compared with parents of children with healthy weight, parents of children with underweight were significantly more likely (OR = 2.2, 95% CI: 1.0–4.8) to recall receiving a BMI report after 1 year of BMI reporting while parents of children with overweight were significantly less likely (OR = 0.7, 95% CI: 0.5–0.9). There were no significant differences by child weight status after 2 years of BMI reporting, however, parents of children with overweight maintained a trend toward lower recall (OR = 0.7, p = 0.053).
Table 2.
Parent Recall of BMI Reports and Child Weight Status by Years of Exposure to BMI Reporting
| 1 Year of exposure to BMI reportinga | 2 Years of exposure to BMI reportingb | |||||||
|---|---|---|---|---|---|---|---|---|
| Recalled receiving BMI report (n = 656) | Accurately recalled child weight status (n = 519) | Recalled receiving BMI report (n = 753) | Accurately recalled child weight status (n = 620) | |||||
| Child baseline weight status | % | OR [95% CI] | % | OR [95% CI] | % | OR [95% CI] | % | OR [95% CI] |
| Healthy weight | 58 | — | 88 | — | 72 | — | 90 | — |
| Underweight | 78 | 2.2* [1.0–4.8] | 72 | 0.3* [0.1–0.7] | 79 | 1.2 [0.6–2.6] | 84 | 0.6 [0.2–1.4] |
| At risk for overweight | 50 | 0.9 [0.7–1.2] | 70 | 0.3* [0.2–0.5] | 65 | 0.8 [0.5–1.1] | 66 | 0.2* [0.1–0.4] |
| Overweight | 42 | 0.7* [0.5–0.9] | 56 | 0.2* [0.1–0.3] | 63 | 0.7 [0.5–1.0] | 63 | 0.2* [0.1–0.3] |
Out of 1249 parents who received 1 BMI report, 656 recalled receiving the report (37 responses were missing). Among the 656 parents who recalled receiving the report, 519 accurately recalled their child's weight status.
Out of 956 parents who received 2 BMI reports, 753 recalled receiving the report (5 responses were missing). Among the 753 parents who recalled receiving the report, 620 accurately recalled their child's weight status.
p < 0.05.
CI, confidence interval; OR, odds ratio.
Accurate Recall of Child's Weight Status
Among parents who remembered receiving a report, 81% accurately recalled how the report had classified their child's weight status. Accuracy did not differ by having received 2 (opposed to 1) reports, report type, child race, or child gender. Accuracy significantly differed by child weight status (Table 2). After 1 year of exposure to BMI reporting, parents of children at risk for overweight (OR = 0.6, 95% CI: 0.4–0.8), and parents of children with overweight (OR = 0.4, 95% CI: 0.3–0.6) were less likely to accurately recall their child's weight status from the BMI report compared with parents of children with healthy weight. Differences persisted after 2 years of exposure to BMI reporting for parents of children at-risk for overweight (OR = 0.4, 95% CI: 0.3–0.6) and parents of children with overweight (OR = 0.4, 95% CI: 0.2–0.5).
Parental Perceptions of BMI Reports
Table 3 summarizes parents' perceptions of the BMI report among the 114 parents completing a survey in 2016 who remembered receiving the report, stratified by child's weight status. Most parents (93%) understood the report, 78% found the report helpful for themselves, and 62% found the report helpful for their child. Parents of children at-risk for overweight and with overweight were more likely to be concerned by results than parents of children with underweight or healthy weight (51% vs. 7%; p < 0.001). Only 22% of parents of children at-risk for overweight and with overweight reported being surprised by the results.
Table 3.
Parent Reactions to BMI Report Information, among Those Who Remember receiving a BMI Report
| Child's weight statusb | ||||
|---|---|---|---|---|
| Overalla (n = 114) | BMI <85th %tile (n = 43) | BMI ≥85th %tile (n = 71) | p-Value for weight statusc | |
| Understood report | 93% | 85% | 97% | 0.05 |
| Found report helpful | 78% | 76% | 80% | 0.64 |
| Found results concerning | 35% | 7% | 51% | <0.001 |
| Found results surprising | 17% | 8% | 22% | 0.06 |
Data are from 2016 survey among parents who had received a BMI report in prior 6 months.
Sample was stratified in 2016 to overrepresent students with a BMI ≥85th percentile.
p-Values from two-sided Fisher's exact tests.
Discussion
This study provides several possible explanations for the results to date from studies showing no impact of school-based BMI reporting on pediatric obesity. We found that parents often did not remember receiving a mailed BMI report, and when they did, they often inaccurately recalled their child's weight status. Although parents of children at risk for overweight and with overweight typically found BMI reports helpful, their surprise and concern at BMI results was limited. Current BMI reports may, therefore, not be sufficiently salient to compel meaningful behavior change among parents and reduce pediatric obesity.
In the present study, 53% of parents remembered receiving their first BMI report, which was mailed 5–7 months before parent surveys. This finding mirrors results from Kubik et al., in which 49% of parents surveyed by mail (n = 790) recalled receiving a BMI report after 2 months.7
Other studies have reported higher recall rates using phone interviews,4–6 but phone interviews likely inflate recall rates due to social desirability bias and the ability of interviewers to provide additional prompts and recall cues. Thus, roughly 1 in 2 parents (∼50%) appear to remember receiving BMI reports without extensive prompting after 1 year of reporting. In the present study, recall increased to 71% among parents who had received two BMI reports, suggesting that repeated BMI reporting could increase parent attention to BMI reports.
We found that parents of children with a BMI ≥95th percentile were significantly less likely to remember receiving a BMI report than parents of children with healthy weight, regardless of prior reporting. This could be related, in part, to parental denial about their child's higher weight status.20 This is particularly concerning given that effectiveness of BMI reporting depends on motivating behavior change among parents of children with overweight, in particular. Findings from the present study contrast with findings by Johnson et al.,5 which suggested that parents of children outside the normal BMI range were more likely to remember BMI reports. Researchers in that study combined parents of children with underweight (n = 63) and parents of children with overweight and obesity (n = 105) into one category, however, masking results for each weight category.5
Parents who saw a picture of the BMI report on their survey had twice the odds of recalling receipt of a BMI report than parents who did not. While this finding suggests that visual aids enhance parent recall, they would not be expected to increase the efficacy of BMI reporting.
Accurate recall of child weight status from BMI reports was significantly lower among parents of children at risk for overweight and with overweight compared with parents of children with healthy weight. These findings are consistent with those from Johnson et al.,5 who reported that 65% of parents of children with overweight accurately recalled their child's weight status compared with 74% of parents of children with normal weight. Based on results from the present study, only 35% of parents of children at risk for overweight and 27% of parents of children with overweight remember receiving a BMI report and accurately recall their child's overweight status after 1 year of exposure to BMI reporting. After 2 years of exposure, the numbers increased to 46% and 42%, respectively, although the increase is driven by an increase in recall of BMI reports, not an increase in accurate recall of child weight status. Thus, while receiving more than 1 report increases parents' recall of the report, and it does not increase accurate recall of their child's reported weight status. In contrast, 94% of parents in a randomized controlled trial accurately recalled their child's reported weights status when the information came from a doctor,21 suggesting that parents may place greater value on results received from a doctor vs. their child's school. Only 2 weeks elapsed between physician notification and assessed recall, however, which may explain greater parent accuracy in that study.
Similar to findings from Johnson et al.,5 almost all parents in the present study agreed that they understood the BMI report. Most parents found the reports helpful for themselves. While parents of children at risk for overweight and with overweight were far more likely to find BMI results concerning and surprising than parents of children with healthy weight, only half found the results concerning and 20% found the results surprising, which may support the lack of positive weight-related behavior change post-BMI report receipt, as prior research has indicated that parents who change their perception of their child's weight status are more likely to subsequently engage in behavior change.22,23 Lack of concern among parents who are told their child has overweight may stem from parent perceptions that school-based BMI reports misclassify children as overweight (due to more muscular body types or “baby fat”) and beliefs that there are many more aspects to health than weight alone.24,25 Regardless, parents who find BMI report information neither concerning nor surprising are unlikely to make changes to their child's dietary or physical activity behaviors,22,23 further reducing the pool of parents who are susceptible to the impact of BMI reports.
This study had several limitations. Despite oversampling and using best recruitment practices,19 our response rate was only 36%, which could limit the generalizability of our findings. Furthermore, white and Asian parents were more likely to respond to the survey than African American and Hispanic parents, which could impact our ability to detect differences by parent race/ethnicity and further limit generalizability. In addition, very few parent respondents received the BMI + fitness report, preventing us from definitively examining differences by report type. While <3% of participating students had missing BMI data each year, students with missing or implausible follow-up BMI data had a higher BMI z-score at baseline and were more likely to be African American than students with complete data, which could also impact generalizability. Moreover, all survey data were self-report, which is prone to recall and social desirability bias. Additionally, while our survey drew from questionnaires used in similar research,26 our questions related to parental understanding, concern, and surprise may not have fully captured all aspects of these complex constructs. Finally, in analyses, we used school-level free or reduced-price meal data as a proxy for SES, but results could have been strengthened with SES information at the individual level.
This study provides several possible explanations for why current BMI reports are not effective at reducing pediatric obesity. Parents often do not remember receiving a mailed BMI report, and when they do, they often inaccurately recall their child's overweight status. Although parents of children with overweight and obesity typically find BMI reports helpful, their surprise at, and concern for, BMI results is limited. Parents of children with overweight and obesity are more likely to make health behavior changes for their child, but fewer than 1 in 3 do so with the consultation of a medical professional. Current BMI reports may be ineffective at reducing pediatric obesity due to their lack of salience and ability to compel meaningful behavior change among parents.
Acknowledgments
The authors extend tremendous gratitude to all of the schools that supported this study and all of the students and families who participated. This work was funded by NIH/NHBLI R01 HL120666. The funder had no role in the design, collection, analysis, and interpretation of data; in the writing of the article; or in the decision to submit the article for publication. Trial registration: ClinicalTrials.gov NCT02088086.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Ruggieri DG, Bass SB. A comprehensive review of school-based body mass index screening programs and their implications for school health: Do the controversies accurately reflect the research? J Sch Health 2015;85:61–72 [DOI] [PubMed] [Google Scholar]
- 2. Hales CM, Fryar CD, Carroll MD, et al. . Trends in obesity and severe obesity prevalence in US youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA 2018;319:1723–1725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thompson HR, Madsen KA. The report card on BMI report cards. Curr Obes Rep 2017;6:163–167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Chomitz VR, Collins J, Kim J, et al. . Promoting healthy weight among elementary school children via a health report card approach. Arch Pediatr Adolesc Med 2003;157:765–772 [DOI] [PubMed] [Google Scholar]
- 5. Johnson SB, Pilkington LL, Lamp C, et al. . Parent reactions to a school-based body mass index screening program. J Sch Health 2009;79:216–223 [DOI] [PubMed] [Google Scholar]
- 6. West DS, Raczynski JM, Phillips MM, et al. . Parental recognition of overweight in school-age children. Obesity (Silver Spring) 2008;16:630–636 [DOI] [PubMed] [Google Scholar]
- 7. Kubik MY, Fulkerson JA, Story M, Rieland G. Parents of elementary school students weigh in on height, weight, and body mass index screening at school. J Sch Health 2006;76:496–501 [DOI] [PubMed] [Google Scholar]
- 8. Linchey J, Madsen KA. State requirements and recommendations for school-based screenings for body mass index or body composition, 2010. Prev Chronic Dis 2011;8:A101. [PMC free article] [PubMed] [Google Scholar]
- 9. Grimmett C, Croker H, Carnell S, Wardle J. Telling parents their child's weight status: Psychological impact of a weight-screening program. Pediatrics 2008;122:e682–e688 [DOI] [PubMed] [Google Scholar]
- 10. Lundahl A, Kidwell KM, Nelson TD. Parental underestimates of child weight: A meta-analysis. Pediatrics 2014;133:e689–e703 [DOI] [PubMed] [Google Scholar]
- 11. Falconer CL, Park MH, Croker H, et al. . The benefits and harms of providing parents with weight feedback as part of the national child measurement programme: A prospective cohort study. BMC Public Health 2014;14:549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Falconer C, Park M, Skow A, et al. . Scoping the impact of the national child measurement programme feedback on the child obesity pathway: Study protocol. BMC Public Health 2012;12:783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Perez A, Ball GD. Beyond oblivobesity: Seven Myths about parental misperception of children's weight. Child Obes 2015;11:735–737 [DOI] [PubMed] [Google Scholar]
- 14. Lee J, Kubik MY. Child's weight status and parent's response to a school-based body mass index screening and parent notification program. J Sch Nurs 2015;31:300–305 [DOI] [PubMed] [Google Scholar]
- 15. Madsen KA, Linchey J, Ritchie L, Thompson HR. The Fit Study: Design and rationale for a cluster randomized trial of school-based BMI screening and reporting. Contemp Clin Trials 2017;58:40–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. National Center for Education Statistics. Educational attainment of high school dropouts 8 years later. 2004. Available at www.nces.ed.gov Last accessed March, 2006
- 17. Thompson HR, Linchey JK, Madsen KA. Critical elements of a school report to parents on body mass index. Prev Chronic Dis 2015;12:E136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kuczmarski R, Ogden C, Guo S. 2000 CDC growth charts for the United States: Methods and development. Vital Health Stat 2002;11:1–190 [PubMed] [Google Scholar]
- 19. Edwards P, Roberts I, Clarke M, et al. . Increasing response rates to postal questionnaires: Systematic review. BMJ 2002;324:1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Katz DL. Oblivobesity: Looking over the overweight that parents keep overlooking. Child Obes 2015;11:225–226 [DOI] [PubMed] [Google Scholar]
- 21. Dawson AM, Taylor RW, Williams SM, et al. . Do parents recall and understand children's weight status information after BMI screening? A randomised controlled trial. BMJ Open 2014;4:e004481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Rhee KE, De Lago CW, Arscott-Mills T, et al. . Factors associated with parental readiness to make changes for overweight children. Pediatrics 2005;116:e94–e101 [DOI] [PubMed] [Google Scholar]
- 23. Park MH, Falconer CL, Croker H, et al. . Predictors of health-related behaviour change in parents of overweight children in England. Prev Med 2014;62:20–24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Moyer LJ, Carbone ET, Anliker JA, Goff SL. The Massachusetts BMI letter: A qualitative study of responses from parents of obese children. Patient Educ Couns 2014;94:210–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Syrad H, Falconer C, Cooke L, et al. . “Health and happiness is more important than weight”: A qualitative investigation of the views of parents receiving written feedback on their child's weight as part of the National Child Measurement Programme. J Hum Nutr Diet 2015;28:47–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Neumark-Sztainer D, Wall M, Story M, van den Berg P. Accurate parental classification of overweight adolescents' weight status: Does it matter? Pediatrics 2008;121:e1495–e1502 [DOI] [PubMed] [Google Scholar]