Abstract
Background
Breast cancer is the most common cancer in women worldwide, and reproductive factors and family history of malignancy are considered as high risk factors. The present study aimed to evaluate the synergistic effect of reproductive factors and family history on breast cancer.
Method
A total of 1215 breast cancer patients and 1215 control participants from two medical centers were enrolled, and reproductive factor history and family cancer history information was collected. Multivariate logistic regression analyses were performed to estimate the adjusted odds ratio (OR), and synergy index (SI) was used to assess the combined effect of potential factors.
Results
Compared to the controls, a negative association between full-term pregnancy/breastfeeding and breast cancer was observed regardless of the status of family cancer history (OR: 0.675, 95% CI: 0.560–0.814 and OR: 0.631, 95% CI: 0.503–0.789 respectively) after adjustment of other confounders, while the risk effect of abortion was unproven. The synergistic effect of history of full-term pregnancy and family history of malignancy was indicated in the combined analyses with SI as 9.429 (95% CI:1.248–71.245).
Conclusion
Full-term pregnancy/breastfeeding were protective factors against breast cancer and synergistic additive effect was demonstrated between no full-term pregnancy/breastfeeding and a family history of malignancy on the risk of breast cancer.
Keywords: breast cancer, full-term pregnancy, breastfeeding, family cancer history
Introduction
Worldwide, breast cancer is the most common cancer and the main cause of cancer death in women. In the world, 1.9 million new cases and 601,000 deaths were reported in 2017.1 In China, breast cancer accounts for 15% of all new cancers in women and is the most commonly diagnosed cancer at age 30 to 59.2 It is commonly associated with reproductive, lifestyle, and environmental factors, and the inherited genetic mutation contributes to less than 10% of breast cancer.3 The association between breast cancer risk and family history is significant for women under the age of 60.4
The risk of developing breast cancer is related to the exposure to endogenous and exogenous hormones. Reproductive factors, such as early menstruation and late menopause, can increase the levels and/or duration of exposure to ovarian hormones. Nulliparity or low parity may cause breast tissue to be exposed to high levels of hormones for longer periods of time. Studies have indicated that these factors can increase the risk of breast cancer.5,6 Conversely, pregnancy and breastfeeding can reduce the lifetime number of menstrual cycles, and the cumulative exposure to endogenous hormones.7 These two factors can also introduce the differentiation of breast cells, which are hypothesized to be more resistant to transform into cancer cells.8,9 Some studies have prompted that familial breast cancer susceptibility may be strongly associated with hormonal factors and the breast epithelia may be more prone to abnormal differentiation.10,11
Women with a family history of malignancy (especially first-degree relatives (mothers, sisters, or daughters)) are at increased risk of the disease. In developed nations, the cumulative incidence of breast cancer in women up to age 50 with zero, one or two affected first-degree relatives was 1.7%, 3.7%, and 8.0% respectively.10 However, no systematic research has been done to evaluate the effect of first-degree relatives' family history on the incidence of breast cancer in China.
Here, we conducted a large case-control study and used data from two medical centers to evaluate the effect of reproductive factors on the risk of breast cancer. Also, the synergistic effect of reproductive factors and family history was assessed in the present study.
Materials And Methods
Study Population
This was a clinic-based case-control study. The data were extracted from structured electronic medical record systems for patients. In total, 1215 histologically diagnosed breast cancer cases from January 2012 to January 2016 in two medical centers (the second affiliated hospital of Guangzhou University of Chinese Medicine and the Huadong Hospital affiliated to Fudan University) were enrolled in consecutive sequence. 1215 age matched cases with benign gynecological diseases of the same centers at a 1:1 ratio, were randomly enrolled at the same time. All personal information of enrolled participants was anonymized and de-identified prior to analysis - concealed and replaced as random ID. The participation rate in cases was more than 98 percent while the participation rate in controls was 100 percent. All the patients were of Asian population and the data were extracted from medical records while they had no therapy. The inclusion criteria were: patients pathologically diagnosed as having invasive ductal carcinoma (IDC) or invasive lobular carcinoma (ILC) for cases and benign gynecological diseases (uterine fibroids, ovarian teratoma, cervical polyps) for the controls. Exclusion criteria were as follows: 1) previous or coexisting cancers other than breast cancer; 2) previously diagnosed with breast cancer; 3) not enough data could be extracted.
Clinical Data Collection
Age at diagnosis, the status of breastfeeding, abortion, pregnancy, and history of benign breast surgery, 1st degree family history of all malignancy and breast cancer (i.e., natural mother, father, or siblings) were collected by two independent investigators. History of breastfeeding was defined as more than 1 month of feeding baby with breast milk.13 Abortion was defined as termination of pregnancy during the first 28 weeks of pregnancy.14
Statistical Analysis
Categorical data were described using numbers and percentages, and Chi-squared test was performed to examine the differences between cases and controls. Continuous data were described as mean and standard deviations, and differences between the groups were identified by Student’s t-test. Multivariate logistic regression models were performed to estimate risk of reproductive factors, using the odds ratio (OR) with 95% CI. Also, stratified analyses according to the status of family history of malignancy (positive or negative) were used to elucidate the potential effect of family history for the association between reproductive factors and breast cancer. Further, we examined the joint effect of reproductive factors and family history of malignancy on breast cancer risk, using the synergy index (SI) following the approach proposed by Hosmer and Lemeshow.11 All statistical analyses were performed using SAS, Version 9.1.3 (SAS Institute Inc., Cary, NC, USA) on two-sided probabilities.
Results
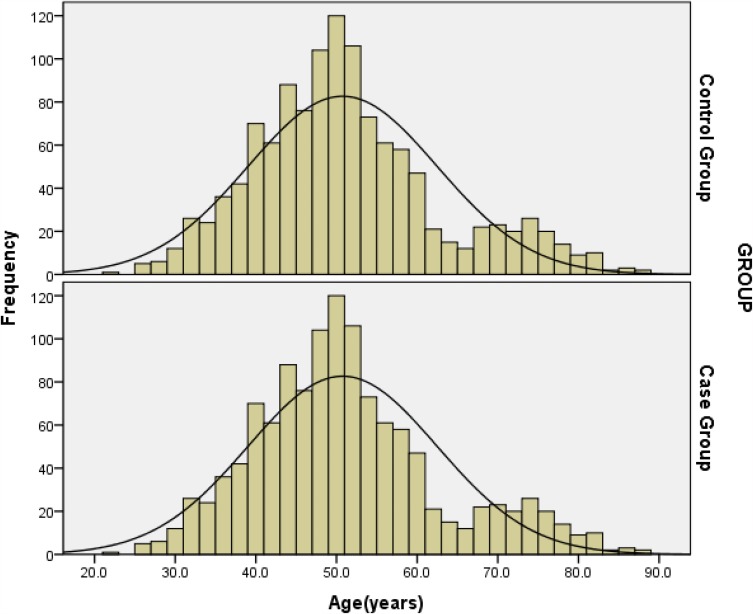
The characteristics of 1215 breast cancer patients and 1215 control participants were described in Table 1. The mean age of both cohorts was 50.76±11.73, and the majority (92.5%) of participants were >40 years old. The age distribution was shown in Figure 1. When considering the reproductive factor, the cases had lower rate of full-term pregnancy, breastfeeding, and abortion (all p<0.05). Furthermore, compared with the controls, more participants with family history of malignancy or breast cancer were observed and had a history of benign breast surgery in cases (all p<0.05).
Table 1.
Characteristic Of Enrolled Patients
| Controls(n=1215) | Cases(n=1215) | P value | |
|---|---|---|---|
| Age (Mean ±SD) | 50.76±11.73 | 50.76±11.73 | 1.00 |
| ≤40 | 222(18.3) | 222(18.3) | 1.00 |
| >40 | 993(81.7) | 993(81.7) | |
| BMI(Mean ±SD) | 22.86±3.26 | 22.69±3.88 | 0.262 |
| Age at first full-term pregnancy(Mean ±SD) | 26.17±3.60 | 26.50±3.75 | 0.053 |
| Breastfeedinga,b | |||
| No | 311(26.1) | 428(35.2) | <0.001 |
| Yes | 884(73.9) | 787(64.8) | |
| Number of pregnancies | |||
| 0 | 147(12.1) | 254(20.9) | |
| 1 | 216(17.8) | 195(16.0) | |
| ≥2 | 852(70.1) | 766(63.0) | |
| Full-term pregnancy | |||
| No | 194(16.0) | 294(24.2) | 0.002 |
| Yes | 1021(84.0) | 921(75.8) | |
| Abortion | |||
| No | 481(39.6) | 538(44.3) | 0.019 |
| Yes | 734(60.4) | 677(55.7) | |
| Family history of malignancy | |||
| Yes | 181(14.9) | 236(19.4) | 0.003 |
| No | 1034(85.1) | 979(80.6) | |
| Family history of breast cancerc | |||
| Yes | 29(2.4) | 57(4.7) | 0.002 |
| No | 1186(97.6) | 1158(95.3) | |
| History of benign breast surgery | |||
| Yes | 181(14.9) | 121(10) | <0.001 |
| No | 1034(85.1) | 1094(90) |
Notes: aThe data of breast-feeding history were missing in 23 patients in the control group; bthe data of breast-feeding time were missing in 24 patients in the control group; cFisher’s exact probability test was used for statistical analysis.
Figure 1.
The age distribution of enrolled participants in case group/control group.
In the multivariate logistic regression models, the history of breastfeeding, full-term pregnancy, history of benign breast surgery, and family history of malignancy were significantly associated with the risk of breast cancer occurrence in the overall cohort (Table 2). The breastfeeding and full-term pregnancy manifested a protective effect (OR: 0.675, 95% CI: 0.560–0.814 and OR: 0.631, 95% CI: 0.503–0.789 respectively), while family history of malignancy was linked with higher risk of breast cancer (OR: 1.251, 95% CI: 1.005–1.557). No effect of abortion was observed in the multivariate logistic analyses.
Table 2.
Estimating The Odds Ratio (OR) And 95% Confidence Interval Of Reproductive Factors In Multivariate Logistic Regression Models
| Breastfeedinga,b,c | P value | Abortion | P value | HBBS | P value | Family History Of Malignancy | P value | |
|---|---|---|---|---|---|---|---|---|
| Overall | 0.68(0.56,0.81) | <0.001 | 0.96(0.80,1.13) | 0.599 | 0.61(0.47,0.76) | <0.001 | 1.25(1.01,1.56) | 0.045 |
| Age | ||||||||
| ≤40 | 1.17(0.78,1.75) | 0.442 | 1.34(0.91,1.99) | 0.144 | 0.79(0.38,1.63) | 0.521 | 2.90(1.38,6.08) | 0.005 |
| >40 | 0.58(0.47,0.72) | <0.001 | 0.90(0.74,1.09) | 0.258 | 0.58(0.45,0.76) | <0.001 | 1.11(0.88,1.40) | 0.396 |
Notes: aThe history of breastfeeding and full-term pregnancy had a linear correlation, either parameter was incorporated in the model independently. bThe breastfeeding history, abortion history, family history of malignant tumor, and history of benign breast surgery with statistical significance in the single factor analysis were included in the multivariate logistic regression model for analysis. cNo history of breast-feeding, no history of abortion, no history of breast disease, and no family history of malignant tumor were used as reference categories in the multivariate logistic regression model for analysis.
Abbreviation: HBBS, history of benign breast surgery.
Stratified analyses were performed to evaluate the effect based on the age subgroup in Table 2. Among participants ≤40 years old, only full-term pregnancy and family history of malignancy were significant parameters associated with the risk of breast cancer (both p<0.05), while the history of benign breast surgery was found to be an important factor for breast cancer occurrence besides full-term pregnancy and family history of malignancy.
In order to eliminate the synergistic effect of full-term pregnancy/breastfeeding and family history of malignancy, the synergistic index was calculated in Table 3. Compared with participants with positive history of full-term pregnancy and negative family history of malignancy, participants with negative history of full-term pregnancy and positive family history of malignancy showed higher risk of breast cancer (OR: 2.993, 95% CI: 2.060–4.348, p<0.05), and the synergistic index was 9.429 (95% CI:1.248–71.245). Similarly, breastfeeding and family history of malignancy also manifested a synergistic effect on the risk of breast cancer. Participants with no breastfeeding and positive family history of malignancy showed the highest risk of breast cancer (OR: 2.630, 95% CI: 1.896,3.648, p< 0.05).
Table 3.
Estimating The Joint Effects Of Full-Term Pregnancy/Breastfeeding And Family History Of Malignancy On The Risk Of Breast Cancer
| Parameter | Family History Of Malignancy | |||
|---|---|---|---|---|
| No | Yes* | |||
| OR (95% CI) | OR (95% CI) | P value | ||
| Full-term pregnancy | Yes | Reference | 0.94(0.72,1.23) | <0.001 |
| No | 1.27(0.99,1.64) | 2.99(2.06,4.35) | ||
| Synergy index | 9.43(1.25,71.25) | 0.030 | ||
| Breastfeeding | Yes | Reference | 0.87(0.65,1.17) | <0.001 |
| No | 1.245(1.02,1.53) | 2.63(1.90,3.65) | ||
| Synergy index | 13.71(0.55,342.19) | <0.001 | ||
Note: *The abortion history and history of benign breast surgery were included as confounders into the model for control.
Discussion
Breast cancer is the most common cancer and the leading cause of cancer death in females worldwide. Even so, the potential causes of breast cancer remain unclear. Previous epidemiological studies have revealed the association of reproductive factors and breast cancer risk, but the mechanism of these factors in breast cancer remains complex.
In the present study, we demonstrated that full-term pregnancy is independently associated with lower risk of breast cancer occurrence. Compared with the controls, participants with history of full-term pregnancy showed 37% decreased risk of breast cancer. Both the malignant family history and the family history of breast cancer in the controls suggested a weaker genetic correlation. Retrospective epidemiological studies have indicated the contributions of parity to long-term protection against breast cancer.12Compared with nulliparous women, women with first full-term pregnancy before 20 years of age showed 50% reduced lifetime risk of developing breast cancer, and earlier first full-term birth is associated with greater protection.13 Full-term pregnancy is hypothesized to reduce the long-term risk of breast carcinogenic transformation.6 During the first trimester of pregnancy, the hormonal changes could induce the proliferation and differentiation of breast tissue in preparation for lactation. Terminal differentiation of the terminal ductal lobular unit occurs in the final trimester. Parity-related gene expression signatures in normal breast tissue have been identified in recent research.14 Experimental animal models have suggested the protective effect of full-term pregnancy.15–17 In rodents, young virgin cycling rats experienced the highest incidence of 7,12-dimethylbenz(a) anthracene (DMBA)-induced mammary cancer, but rats, after a full-term pregnancy, failed to develop induced tumors when exposed to the same carcinogen. For nulliparous women, evaluated exposure of gonadal hormone and the high ratio of undifferentiated epithelial cell might induce transformation and carcinogenesis of the mammary cell.18
Similarly, breastfeeding is hypothesized to be a protective factor for breast cancer. In the present study, we found that breastfeeding was a significant protective factor for breast cancer, with nearly 32% decreased risk. The breast has undergone involution at cessation of lactation, which involves cytokines, growth factors, and matrix metalloprotease.19 Breastfeeding could delay the process of involution, and it has been hypothesized that the more gradual involution associated with lactation may reduce longer-term breast cancer risk. Furthermore, previous analyses indicated that lower estradiol and higher prolactin levels were present in breastfeeding females for up to 12 weeks postpartum, constructing a different postpartum hormonal milieu from non-breastfeeding females. In African American Breast Cancer Epidemiology and Risk (AMBER) Consortium, high risk was observed with higher parity among women who did not breastfeed but not among women reporting ever breastfeeding.20 Meta-analysis has indicated that relative risk of breast cancer decreased by 4.3% for every 12 months of breastfeeding.6
Moreover, the history of nulliparity and no-breastfeeding could have a synergistic effect with family history of malignancy, manifesting the risk of breast cancer occurrence. Compared with participants with negative family malignancy history and positive breastfeeding history, those with positive family history of malignancy and negative breastfeeding experienced 1.6 increased risk of breast cancer, which could not be explained by superimposed effect. And the breast cancer risk increased nearly 3.0 times in the participants with nulliparity and no-breastfeeding/positive family history of malignancy. So far, no previous study has evaluated the combined effect of reproductive factors and family history of malignancy. Family history was considered as essential risk factor of breast cancer and personal feature of germline mutation (such as BRAC1/2 mutation). Theoretically, participants with family history of malignancy might manifest genetic susceptibility of carcinoma and were at high risk of early onset breast cancer.
Although we used large-scale participants for risk evaluation, some limitations existed in the present study. Firstly, this study was performed in Chinese people and the conclusion might be well suited for this patient population only. Further, studies are necessary to evaluate this synergistic effect among participants in other regions and clinical centers. Secondly, the detailed information of pregnancy and breastfeeding (such as duration, quantity of breast milk) was not incorporated in the analyses, which might limit the accurate assessment of pregnancy and breastfeeding. Finally, the controls in this study were patients with benign gynecological diseases recruited at medical centers, which might be a source of selection bias.
In conclusion, the results of our study suggest that full-term pregnancy/breastfeeding and family history of malignancy work synergistically and affect the risk of breast cancer in women. It can be used in the assessment of breast cancer risk in clinical practice.
Ethics Statement
The study protocol was approved by the institutional review board of the second affiliated hospital of Guangzhou University of Chinese Medicine. Clinical data were obtained from each participant prior to surgery. All the personal information of enrolled participants was concealed and replaced as random ID.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017. A systematic analysis for the global burden of disease study. JAMA Oncol. 2019. doi:doi: 10.1001/jamaoncol.2019.2996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F. Cancer statistics in China, 2015. CA Cancer J Clin. 2016. doi: 10.3322/caac.21338 [DOI] [PubMed] [Google Scholar]
- 3.Clavel-Chapelon F, Gerber M. Reproductive factors and breast cancer risk. Do they differ according to age at diagnosis? Breast Cancer Res Treat. 2002;72:107–115. doi: 10.1023/A:1014891216621 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shiyanbola OO, Arao RF, Miglioretti DL, et al. Emerging trends in family history of breast cancer and associated risk. Cancer Epidemiol Prev Biomarkers. 2017;26(12):1753–1760. doi: 10.1158/1055-9965.EPI-17-0531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kobayashi S, Sugiura H, Ando Y, Shiraki N, Yanagi T, Yamashita H. Reproductive history and breast cancer risk. Breast Cancer Tokyo. 2012;19:302–308. doi: 10.1007/s12282-012-0384-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collaborative Group on Hormonal Factors in Breast Cancer. Breast cancer and breastfeeding: collaborative reanalysis of individual data from 47 epidemiological studies in 30 countries, including 50302 women with breast cancer and 96973 women without the disease. Lancet. 2002;360:187–195. doi: 10.1016/S0140-6736(02)09454-0 [DOI] [PubMed] [Google Scholar]
- 7.Colditz GA. Cancer Epidemiology and Prevention. 3rd Ed New York: Oxford University Press; 2006. [Google Scholar]
- 8.Britt K, Ashworth A, Smalley M. Pregnancy and the risk of breast cancer. Endocr Relat Cancer. 2007;14:907–933. doi: 10.1677/ERC-07-0137 [DOI] [PubMed] [Google Scholar]
- 9.Russo J, Moral R, Balogh GA, Mailo D, Russo IH. The protective role of pregnancy in breast cancer. Breast Cancer Res. 2005;7:131–142. doi: 10.1186/bcr1029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Petrakis NL, Ernster VL, King EB, et al. Epithelial dysplasia in nipple aspirates of breast fluid: association with family history and other breast cancer risk factors. J Natl Cancer Inst. 1982;68(1):9–13. [PubMed] [Google Scholar]
- 11.Brinton LA, Hoover R, Fraumeni JF Jr. Interaction of familial and hormonal risk factors for breast cancer. J Natl Cancer Inst. 1982;69(4):817–822. [PubMed] [Google Scholar]
- 12.Collaborative Group on Hormonal Factors in Breast Cancer. Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological studies including 58,209 women with breast cancer and 101,986 women without the disease. Lancet. 2001;358:1389–1399. doi: 10.1016/S0140-6736(01)06524-2 [DOI] [PubMed] [Google Scholar]
- 13.Ilic M, Vlajinac H, Marinkovic J. Breastfeeding and risk of breast cancer: case-control study. Women Health. 2015;55(7):778–794. doi: 10.1080/03630242.2015.1050547 [DOI] [PubMed] [Google Scholar]
- 14.Sánchez-Páez DA, Ortega JA, Amo-Adjei <. Reported patterns of pregnancy termination from demographic and health surveys. PLoS One. 2019;14(8):e0221178. doi: 10.1371/journal.pone.0221178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hosmer DW, Lemeshow S. Confidence interval estimation of interaction. Epidemiology. 1992;3:452–456. doi: 10.1097/00001648-199209000-00012 [DOI] [PubMed] [Google Scholar]
- 16.Ursin G, Bernstein L, Wang Y, Lord SJ, Deapen D, Liff JM. Reproductive factors and risk of breast carcinoma in a study of white and African-American women. Cancer Am Cancer Soc. 2004;101:353–362. [DOI] [PubMed] [Google Scholar]
- 17.MacMahon B, Cole P, Lin TM, Lowe CR, Mirra AP, Ravnihar B. Age at first birth and breast cancer risk. Bull World Health Organ. 1970;43:209–221. [PMC free article] [PubMed] [Google Scholar]
- 18.Rotunno M, Sun X, Figueroa J, Sherman ME, Garcia-Closas M, Meltzer P. Parity-related molecular signatures and breast cancer subtypes by estrogen receptor status. Breast Cancer Res. 2014;16:R74. doi: 10.1186/bcr3689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sinha DK, Pazik JE, Dao TL. Prevention of mammary carcinogenesis in rats by pregnancy: effect of full-term and interrupted pregnancy. Br J Cancer. 1988;57:390–394. doi: 10.1038/bjc.1988.88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang J, Yoshizawa K, Nandi S, Tsubura A. Protective effects of pregnancy and lactation against N-methyl-N-nitrosourea-induced mammary carcinomas in female Lewis rats. Carcinogenesis. 1999;20:623–628. doi: 10.1093/carcin/20.4.623 [DOI] [PubMed] [Google Scholar]
- 21.Rajkumar L, Guzman RC, Yang J, Thordarson G, Talamantes F, Nandi S. Short-term exposure to pregnancy levels of estrogen prevents mammary carcinogenesis. Proc Natl Acad Sci U S A. 2001;98:11755–11759. doi: 10.1073/pnas.201393798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Henderson BE, Feigelson HS. Hormonal carcinogenesis. Carcinogenesis. 2000;21:427–433. doi: 10.1093/carcin/21.3.427 [DOI] [PubMed] [Google Scholar]
- 23.Arwert EN, Hoste E, Watt FM. Epithelial stem cells, wound healing and cancer. Nat Rev Cancer. 2012;12:170–180. doi: 10.1038/nrc3217 [DOI] [PubMed] [Google Scholar]
- 24.Palmer JR, Viscidi E, Troester MA, Hong CC, Schedin P, Bethea TN. Parity, lactation, and breast cancer subtypes in African American women: results from the AMBER consortium. J Natl Cancer Inst. 2014;106:dju237. [DOI] [PMC free article] [PubMed] [Google Scholar]