Abstract
Heavy and problematic drinking is a concern among young adult military veterans. Personalized normative feedback (PNF) interventions that target normative misperceptions regarding drinking have been efficacious among young adults and have recently begun to be implemented among veteran populations in an effort to reduce heavy drinking. However, moderators of PNF intervention efficacy among veterans are largely unexplored. This study is a secondary data analysis that evaluated whether a PNF intervention would work better at reducing perceived norms, drinking, and alcohol-related problems specifically for young adult veterans who drink to cope with negative affect. Veterans of the United States (U.S.) military (86% male; Mean age = 28.9 years, SD = 3.4) were randomly assigned to receive either: 1) PNF comparing their drinking and perceived norms to actual drinking rates for same sex veterans; or 2) feedback about same sex veteran video game play (control condition). Seven hundred eighty-four individuals completed baseline and 622 completed one-month follow-up assessments (79% follow-up), including measures of alcohol use, alcohol-related problems, and drinking motives. Moderated mediation analyses indicated that changes in normative misperceptions as a result of the intervention were more strongly associated with reductions in drinking and problems among veterans scoring higher on drinking to cope. These findings suggest that PNF may be an especially efficacious brief intervention for veterans who drink for coping reasons.
Keywords: personalized normative feedback, intervention, drinking motives, social norms
Young Adult Veteran Drinking
High risk drinking is a problem among military veterans, particularly during the post-deployment period (Jacobson et al., 2008; Scott et al., 2013). Such drinking patterns are highly correlated with Posttraumatic Stress Disorder (PTSD) and other negative health and behavioral outcomes such as aggression, poor quality sleep, suicidal ideation, anxiety disorders, and depression (Fuehrlein et al., 2016; Jakupcak et al., 2010; McDevitt-Murphy et al., 2010; Seal et al., 2011; Swinkels et al., 2013). Heavy drinking and alcohol use disorder (AUD) are particularly common among young adult veterans compared to both young adult civilians (Bray & Hourani, 2007; Kessler, Chiu, Demler, Merikangas, & Walters, 2005) and older veterans (Seal et al., 2011). Studies have found heavy and binge drinking prevalence rates in veteran samples ranging from 19% (Calhoun et al., 2016) to 43% (Stahre et al., 2009) and probable AUD prevalence rates ranging from 9.9% (Seal et al., 2011) to 12% (Kang, Li, Mahan, Eisen, & Engel, 2009). In particular, one study found that male veterans of Operations Enduring Freedom and Iraqi Freedom (OEF/OIF) reported higher rates of alcohol misuse (21%) compared to non-OEF/OIF male veterans (12%; Hawkins, Lapham, Kivlahan, & Bradley, 2010).
In addition to AUDs being the most common substance use disorder among veterans, AUD and alcohol misuse (i.e., alcohol use that crests near AUD levels) largely go untreated, with some estimates indicating that over 80% of veterans who report an AUD do not receive treatment (Golub & Bennett, 2014). Treatment options such as brief, computer-delivered interventions might be especially useful among this population in part because treatment-seeking may be stigmatized (McFarling, D'Angelo, Drain, Gibbs, & Rae Olmsted, 2011). More recently, brief interventions for alcohol misuse which have been found to reduce alcohol consumption in the general population (e.g., Platt et al., 2016) have been adapted with varying success among veterans (Doherty et al., 2017). One approach that has been used with some success is personalized normative feedback (PNF), which presents veterans with accurate normative data regarding the drinking behavior of their peers. Although a recent meta-analysis reporting on nine interventions found that, overall, brief interventions did not significantly reduce the number of average weekly drinks consumed by veterans and military personnel (Doherty et al., 2017), one of these interventions provided PNF of veteran-specific norms and successfully reduced drinking and consequences among veterans (Pedersen, Parast, Marshall, Schell, & Neighbors, 2017).
Personalized Normative Feedback Interventions
PNF appears to be a successful intervention approach with veterans but the target of the normative referent appears to be important. Interventions presenting PNF of same sex college students have demonstrated success in reducing drinking among young adult college samples (e.g., LaBrie et al., 2013; Lewis, Neighbors, Oster-Aaland, Kirkeby, & Larimer, 2007; Martens, Smith, & Murphy, 2013; Neighbors et al., 2016; Neighbors et al., 2010). More recently, such intervention strategies have begun to be adapted for use with populations outside of college. For example, to determine if the essential assumption behind successful PNF interventions (i.e., whether the group is influenced to drink due to perceived norms of the group) was present for veterans, we found that same-sex veteran perceived norms for drinking were associated with veteran drinking behavior (Pedersen, Marshall, Schell, & Neighbors, 2016b). However, in the aforementioned study, civilian-specific norms were not associated with drinking, suggesting that veteran-specific same-sex feedback may be more appropriate for this population. It may also be the reason why normative feedback was not more effective than treatment as usual in one study that used same-gender drinking norms for the general population and not veteran-specific norms (Cucciare, Weingardt, Ghaus, Boden, & Frayne, 2013).
Studies incorporating veteran/military-specific drinking norms into interventions have proven efficacious. The Drinker’s Check-up intervention including PNF was found to significantly reduce drinking at both 1- and 6-month follow-ups among active-duty military personnel (Pemberton et al., 2011). Furthermore, changes in perceived descriptive norms (i.e., perceptions of others’ behaviors) as a result of a Drinker’s Check-up intervention were associated with reductions in drinking at follow-up among active-duty military personnel (Williams, Herman-Stahl, Calvin, Pemberton, & Bradshaw, 2009), which provides further evidence that interventions targeting normative misperceptions of drinking can be efficacious at reducing drinking in this population. PNF, both with and without motivational interviewing, reduced drinking in a sample of veterans seeking care at a Veterans Affairs Medical Center (McDevitt-Murphy, Williams, Murphy, Monahan, & Bracken-Minor, 2015). In our own work, we found that a brief, standalone online PNF intervention was efficacious at reducing drinking among young adult veterans who may not have otherwise sought care (Pedersen et al., 2017b). While other online interventions have been evaluated in veteran populations, they have often been completed at Veterans Affairs centers, have been more intensive and lengthy, have not incorporated veteran specific drinking norms, and have generally not resulted in significant drinking reductions. While the literature continues to demonstrate efficacy for brief interventions using PNF among military personnel, it is important to consider for whom such interventions might be best suited. We recently explored the question of for whom PNF interventions are most effective in a college student sample and found that drinking motives, specifically drinking to cope, moderated intervention efficacy (Young et al., 2016).
Drinking to Cope
Drinking motives have been categorized along two dimensions, namely internal and external/social reward, and positive and negative affect (Cooper, 1994). Of these, drinking to cope with negative affect has most often been associated with problem drinking (Kuntsche, Knibbe, Gmel, & Engels 2005; Lewis et al., 2008; Martens et al., 2008; Merrill & Thomas, 2013; Simpson, Stappenbeck, Luterek, Lehavot, & Kaysen, 2014). Veterans tend to be at higher risk for a number of mental health issues including PTSD, depression, and anxiety (e.g., Ramsey et al., 2017; Wisco et al., 2014), all of which have been associated with drinking to cope (Goldsmith, Tran, Smith, & Howe, 2009; Simpson et al., 2014; Young-Wolff, Kendler, Sintov, & Prescott, 2009). Furthermore, drinking to cope was found to be more strongly associated with both binge drinking and problem drinking among student service members/veterans compared to civilian students, though frequency of drinking for coping reasons did not differ between groups (Whiteman & Barry, 2011). Thus, drinking to cope may be especially problematic for young adult veterans as it is more closely tied to heavy drinking and problems for these individuals.
Drinking to Cope as Moderator of Intervention Efficacy
PNF assumes that drinking is reduced by changing one’s perceptions about what others are doing, which is primarily a social intervention; that is, the individual cares about what their peers are doing and learns that others around them are not drinking as much as they thought. As such, PNF has been efficacious for social drinkers (Lewis & Neighbors, 2006; Neighbors, Larimer, & Lewis, 2004). However, our recent study found that, among college students, higher coping motives were associated with a stronger relationship between reduced perceived norms and reduced drinking, and were directly associated with reduced drinking at three- and six-month follow-ups (Young et al., 2016). In that study, coping motives did not differentiate PNF intervention effects on changes in perceived norms at follow-up. Thus, PNF reduced perceived norms relative to control regardless of coping motives. The stronger effects of PNF for high coping students was thought to be a result of the stronger association between follow-up perceived norms and drinking and the direct effect of PNF on follow-up drinking, which was presumably not driven by a differential effect in reducing perceived norms for higher coping drinkers. Rather, high coping students might have interpreted the feedback as an unexpected indication that their drinking levels were maladaptive. This may have been due to the direct contrast between their own drinking and other students’ drinking, but it appears that it was not due to correcting misperceptions of drinking norms. The present study was intended to replicate these findings in a sample of veterans.
Current Study
PNF interventions have been found to reduce problematic drinking among both active duty and veteran samples (e.g., McDevitt-Murphy et al., 2015; Pedersen et al., 2017b; Pemberton et al., 2011; Williams et al., 2009). Such interventions are thought to work indirectly, as a result of changing perceived norms for drinking (i.e., PNF reduced perceived drinking norms reduced problem drinking). However, PNF may work directly by facilitating reflection on one’s drinking and recognizing it as potentially maladaptive (i.e., PNF reduced problem drinking). Specifically, PNF may have a direct effect on drinking because it serves a diagnostic function for individuals who drink to cope in that the feedback functions as a warning that they are drinking much more than others and that their coping style is unhealthy. This knowledge (rather than changes to their perceived drinking norms) may motivate them to change their drinking behavior or affect regulatory processes. The current study expands the growing literature in this area by examining coping drinking motives as a potential moderator of intervention efficacy in a secondary data analysis. While past research has found that coping drinking motives moderate PNF efficacy in a sample of college students (Young et al., 2016), this is the first study of its kind to examine whether a PNF intervention would be more effective for young adult veterans who drink to cope with negative affect. Given high rates of mental health issues among veterans (Ramsey et al., 2017) and known associations between mental health issues and drinking to cope (Goldsmith et al., 2009; Simpson et al., 2014; Young-Wolff, 2009), a veteran sample is ideal to further examine how PNF can work for coping drinkers. Similar to the study with college students, we expected that veterans who frequently drink for coping reasons would show a greater reduction in perceived norms, alcohol use, and alcohol-related problems at follow-up relative to veterans who drink for coping reasons less frequently.
Method
Participants and Procedure
Participants were 784 young adult veterans (86% male) aged 19–34 (mean age = 28.9, SD = 3.4) who were recruited to participate in a longitudinal trial to evaluate the efficacy of a PNF intervention (Pedersen, Marshall, & Schell, 2016a; Pedersen et al., 2017b). Participants’ racial backgrounds were as follows: 85% White, 4% Black or African American, 1% Asian, 2% American Indian or Alaska Native, 6% More than one race, and 2% Other. Ten percent of participants identified as Hispanic/Latino(a) ethnicity. Eighty-two percent of participants reported experiencing combat. Six hundred twenty-two veterans (79.3%) completed the one-month follow-up. Participants received a $20 Amazon.com gift card for completing the baseline survey and a $25 Amazon.com gift card for completing the follow-up survey.
Young adult veterans were recruited via Facebook advertisements and were screened into the study. Eligibility criteria included: (1) U.S. veteran not on active duty, (2) aged 18 to 34 years old, (3) and a score of at least 3/4 for women/men on the Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, De la Fuente, & Grant, 1993). Individuals who met eligibility criteria were invited to complete the baseline survey wherein they were randomly assigned to receive either a PNF alcohol intervention or receive control feedback about video game usage. Validation checks used successfully in previous research (e.g., Bauermeister et al., 2012; Kramer et al., 2014; Teitcher et al., 2015) were built into this study to limit potential fraudulent or misrepresented data by participants. For example, to limit access to the survey for multiple submissions, individuals could not access the survey more than once from the same Facebook account and we removed participants who spent an insufficient amount of time on the survey. To verify veteran status, we developed an algorithm where participants needed to provide consistent responses to questions about military service (e.g., branch, pay grade, occupation, and rank in the military all needed to match up), and reviewed individual participant data to ensure responses made sense (e.g., matching up age with time spent in the service, ensuring occupation code listed matched codes used by the specific branch of service indicated). Also, the targeted advertisements on Facebook were designed to only be shown to Facebook users that were likely veterans or family members of veterans. Those that did not meet our verification criteria were screened out of the study and could not return. We have written extensively about the recruitment and data verification procedures. For more details regarding the study and recruitment procedures, please see Pedersen, Naranjo, & Marshall, 2017a and Pedersen et al., 2017b, 2016a. Immediately after receiving the feedback, individuals were asked to complete a brief post-intervention survey assessing perceived norms. One month post-baseline, participants were invited to complete the one-month follow-up survey assessing their drinking, perceived norms for drinking, and alcohol-related problems. All procedures were approved by the Human Subjects Protection Committee.
Measures
Demographics and Military Service
Participants were asked to indicate their age, sex, racial background, and ethnicity. Additionally, participants were asked to report which branch of the military they served in, their rank and pay grade when they were discharged, and their particular occupation within the military. These items served to help verify participants were veterans and were not misrepresenting themselves in the online study (Pedersen et al., 2017a,).
Perceived Drinking Norms
The Drinking Norms Rating Form (Baer, Stacy, & Larimer, 1991) assessed perceived descriptive drinking norms of participants with a modified version of the Daily Drinking Questionnaire (DDQ) regarding alcohol consumption behaviors for a same-sex veteran. Specifically, participants were asked how often and how much they thought that a same-sex veteran drinks in a typical week in the past month at baseline, immediately following the intervention procedure, and at one-month follow-up.
Weekly Drinking
The Daily Drinking Questionnaire (Collins, Parks, & Marlatt, 1985; Kivlahan, Marlatt, Fromme, Coppel, & Williams, 1990) evaluated the number of standard drinks participants consumed each day of a typical week (Monday–Sunday) in the previous month.
Alcohol-related Problems
The brief Young Adult Alcohol Consequences Questionnaire (BYAACQ; Kahler, Strong, & Read, 2005) evaluated alcohol-related consequences experienced over the past month. This scale contains 24-items assessing a range of alcohol-related consequences veterans might have experienced. Example items include, “I have passed out from drinking” and “When drinking I have done impulsive things that I regretted later”. Participants could respond ‘yes’ or ‘no’ to whether they had experienced each consequence in the past month.
Drinking Motives
The Drinking Motives Questionnaire-Revised (DMQ-R; Cooper & 1994) was used to evaluate participants’ motivations for drinking. The DMQ-R consists of 20 items assessing how often participants drink for four reasons (i.e., drink to cope with negative affect, drink to enhance positive mood states, drink to conform to the behavior of others, and drink to socialize). The present study focused on coping drinking motives as a moderator of intervention efficacy while the remaining three motives were included in the models as covariates. An example item from the coping motives subscale is, “Because it helps you when you feel depressed or nervous.” Alphas for the subscales were: .90 for coping, .89 for social, .85 for enhancement, and .89 for conformity.
Intervention Procedure
Personalized Normative Feedback
Participants randomly assigned to the PNF condition saw sex-specific feedback for fellow veterans’ drinking behaviors. Specifically, feedback was presented for the average number of drinks consumed per week, average number of drinks consumed per occasion, and the frequency of binge drinking occasions.
Control Video Game Feedback
Participants randomly assigned to the control feedback condition saw feedback for video game play. Feedback for the attention control condition was similar to that presented in the alcohol PNF condition but included how frequently fellow veterans reported playing video games per week, how many hours per day were spent playing video games, and the total number of hours spent playing video games per week.
Data Analytic Plan
Preliminary analyses were conducted to evaluate potential baseline differences between conditions and to examine distributions of outcomes. Baseline differences between conditions on age, gender, weekly drinking, perceived descriptive norms, and drinking motives were evaluated. The only significant difference found was for coping motives, where the control group had higher scores on coping drinking motives at baseline (M = 12.85, 6.06) than the intervention group (M = 11.79, SD = 5.62), t(791) = 2.57, p =.01. Drinks per week and perceived norms for weekly drinking were each capped to have a maximum value of 80 drinks per week. This affected 1.26% and 3.53% of scores for baseline drinking and perceived norms, respectively. Less than 1% of follow-up perceived norms and drinking scores were affected. Examination of skewness and kurtosis values were all lower than thresholds suggested by Kline (2015) as problematic for SEM (i.e., skewness > 3; kurtosis > 10).
MPLUS version 8.0 (Muthen & Muthen, 2017) was used to evaluate moderated mediation models. The specific mediation pathways of interest were the indirect paths from intervention condition to follow-up drinking (or follow-up alcohol-related problems) through follow-up perceived norms. These pathways included direct paths from intervention condition (X) to follow-up perceived norms (M) and a direct path from follow-up perceived norms to follow-up drinking or alcohol-related problems (Y). Both M and Y controlled for sex and non-coping drinking motives (i.e., social, enhancement, and conformity) to test for the unique influence of coping drinking motives relative to other motives for drinking across both sexes. M also controlled for baseline perceived norms whereas Y controlled for baseline drinks per week or baseline alcohol-related problems. Models were estimated using Full Information Maximum Likelihood. Coping motives (W) was tested as a moderator of the path from X to M (a) and from M to Y (b) and from X to Y (c'). Conditional indirect effects at low (−1SD), medium (Mean), and high values (+1SD) of coping motives were evaluated using bias-corrected bootstrapped confidence intervals (1000 samples). Conditional tests of the indirect effect (ab), direct effect (c'), and total effects (ab+c') at low, medium, and high values of coping motives were tested using model constraints. Variables used in interactions were mean centered to facilitate interpretation and to reduce nonessential multicollinearity of uncentered predictors with their product terms (Cohen, Cohen, Aiken, & West, 2013).
Results
Descriptives
At baseline, veterans reported consuming 18.41 drinks per week on average (SD = 17.14). At follow-up, veterans consumed 11.45 drinks per week on average (SD = 13.25). Correlation analyses revealed expected associations between variables, with positive associations between sex and weekly drinking, perceived norms for weekly drinking, and frequency of binge drinking at baseline and follow-up and a positive association between sex and baseline alcohol-related problems. Thus, males reported consuming more drinks per week, had higher perceived drinking norms, reported more binge drinking episodes, and reported more alcohol-related problems compared to females. Drinking, motives for drinking, perceived descriptive drinking norms, and alcohol-related problems were positively correlated with one another (see Table 1). Moderate positive correlations were found between drinking to cope and drinking (rs >= .30) and drinking to cope and alcohol-related problems (rs >= .43) both at baseline and follow-up.
Table 1.
Means, standard deviations, and correlations among variables.
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Sex | -- | |||||||||||
| 2. Coping Motives | −.01 | -- | ||||||||||
| 3. Conformity Motives | −.01 | .35*** | -- | |||||||||
| 4. Enhancement Motives | .09* | .59*** | .43*** | -- | ||||||||
| 5. Social Motives | .04 | .47*** | .42*** | .68*** | -- | |||||||
| 6. T1 Perceived Norms | .36*** | .26*** | .06 | .28*** | .22*** | -- | ||||||
| 7. T2 Perceived Norms | .26*** | .25*** | .07 | .23*** | .15*** | .58*** | -- | |||||
| 8. T3 Perceived Norms | .28*** | .24*** | .05 | .23*** | .15*** | .49*** | .61*** | -- | ||||
| 9. T1 Drinking | .21*** | .46*** | .12** | .42*** | .26*** | .53*** | .48*** | .39*** | -- | |||
| 10. T3 Drinking | .17*** | .30*** | .01 | .26*** | .13** | .41*** | .43*** | .54*** | .64*** | -- | ||
| 11. T1 Problems | .09* | .58*** | .33*** | .46*** | .35*** | .28*** | .25*** | .29*** | .58*** | .34*** | -- | |
| 12. T3 Problems | .05 | .43*** | .18*** | .29*** | .18*** | .21*** | .20*** | .38*** | .42*** | .51*** | .57*** | -- |
| Mean | .83 | 2.45 | 1.56 | 2.55 | 2.91 | 30.59 | 20.14 | 18.27 | 18.41 | 11.45 | 7.49 | 4.52 |
| Standard Deviation | .37 | 1.17 | 0.82 | 1.02 | 1.11 | 19.53 | 15.68 | 14.48 | 17.14 | 13.25 | 6.73 | 6.00 |
| Minimum | 0.00 | 1.00 | 1.00 | 1.00 | 1.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 | 0.00 |
| Maximum | 1.00 | 5.00 | 5.00 | 5.00 | 5.00 | 80.00 | 80.00 | 80.00 | 80.00 | 80.00 | 24.00 | 24.00 |
Note.
p < .001
p < .01
p < .05.
T1 is baseline. T2 is post-intervention. T3 is one-month follow-up.
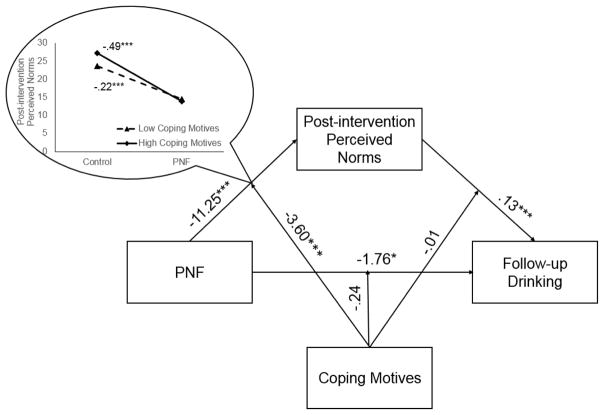
Coping motives as a moderator of intervention efficacy for drinking through post-intervention norms
We evaluated coping motives as a moderator of the indirect effect of PNF on drinking at follow-up through perceived norms post-intervention (see Figure 1). The model showed acceptable fit, RMSEA = .062, CFI = .958, TLI = .894, χ2 = 60.16, p < .001. Controlling for sex, baseline drinking, and all other drinking motives, coping motives significantly moderated the a path and the indirect path between feedback and follow-up drinking through post-intervention norms. Specifically, the indirect path between feedback and changes in drinking was significant for those at means levels of coping motives, b = −1.409, SE = .637, [95% CI: −2.92, −.35], but not for those lower in coping motives, b = −.909, SE = .606, [95% CI: −2.51, .02], or higher in coping motives, b = −1.877, SE = 1.189, [95% CI: −4.44, .28]. Further, neither moderation on the b path nor on the direct path were significant (see Table 2).
Figure 1.
Sex, baseline drinks per week, baseline perceived descriptive drinking norms, enhancement motives, social motives, and conformity motives were included as covariates.
Table 2.
Moderated mediation analyses with coping motives moderating the mediation of PNF on follow-up drinking through post-intervention perceived norms
| Criterion | Predictor | b | se | t | p |
|---|---|---|---|---|---|
| Post- intervention norms | Baseline norms | .419 | .038 | 10.97 | <.0001 |
| Sex | 3.650 | 1.016 | 3.59 | <.0001 | |
| PNF | −11.253 | .841 | −13.37 | <.0001 | |
| Social motives | −.126 | .114 | −1.11 | .269 | |
| Conformity motives | .056 | .141 | .399 | .690 | |
| Enhancement motives | .233 | .136 | 1.71 | .088 | |
| Coping motives | .628 | .492 | 1.28 | .202 | |
| PNF X Coping motives | −3.600 | .744 | −4.84 | <.0001 | |
|
| |||||
| Follow-up drinking | Baseline drinks per week | .444 | .050 | 8.94 | <.0001 |
| Post-intervention norms | .125 | .055 | 2.29 | .022 | |
| Sex | .614 | .797 | .770 | .441 | |
| PNF | −1.759 | .812 | −2.17 | .030 | |
| Social motives | −.064 | .131 | −.49 | .624 | |
| Conformity motives | −.260 | .113 | −2.30 | .021 | |
| Enhancement motives | .025 | .162 | .152 | .879 | |
| Coping motives | .662 | .487 | 1.36 | .174 | |
| Norms X Coping motives | −.003 | .047 | −.07 | .944 | |
| PNF X Coping motives | −.237 | .731 | −.33 | .746 | |
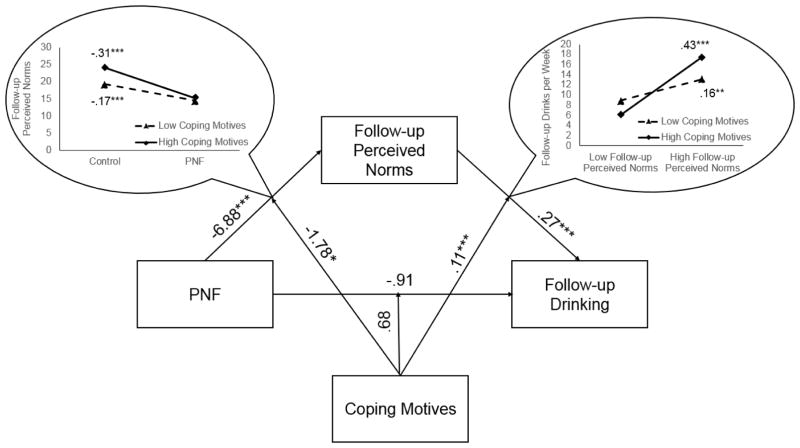
Coping motives as a moderator of intervention efficacy for drinking through follow-up norms
Next, we evaluated coping motives as moderator of the indirect effect of PNF on drinking at follow-up through perceived norms at follow-up (see Figure 2). This model showed good fit, RMSEA = .032, CFI = .985, TLI = .962, χ2 = 27.36, p = .026. Controlling for sex, baseline drinking, and all other drinking motives, coping motives significantly moderated the a path, the b path, and the indirect path between feedback and follow-up drinking through follow-up norms (see Table 3). The indirect path between feedback and follow-up drinking was significant for those at lower levels of coping motives, b = −.697, SE = .350, [95% CI: −1.62, −.22], mean levels of coping motives, b = −1.851, SE = .411, [95% CI: −2.77, −1.17], and at higher levels of coping motives, b = −3.520, SE = .788, [95% CI: −5.32, −2.82]. Consistent with expectations, the moderated mediation effect was stronger the more frequently that participants drank for coping-related reasons. Moderation on the direct path was not significant.
Figure 2.
Sex, baseline drinks per week, baseline perceived descriptive drinking norms, enhancement motives, social motives, and conformity motives were included as covariates.
Table 3.
Moderated mediation analyses with coping motives moderating the mediation of PNF on follow-up drinking through follow-up perceived norms.
| Criterion | Predictor | b | se | t | p |
|---|---|---|---|---|---|
| Follow-up perceived norms | Baseline perceived norms | .293 | .027 | 10.75 | <.0001 |
| Sex | 5.686 | 1.352 | 4.21 | <.0001 | |
| PNF | −6.882 | .960 | −7.17 | <.0001 | |
| Social motives | −.101 | .123 | −.82 | .412 | |
| Conformity motives | −.011 | .136 | −.08 | .938 | |
| Enhancement motives | .172 | .146 | 1.18 | .240 | |
| Coping motives | 1.231 | .525 | 2.35 | .019 | |
| PNF X Coping motives | −1.784 | .837 | −2.13 | .033 | |
|
| |||||
| Follow-up drinking | Baseline drinks per week | .401 | .026 | 15.15 | <.0001 |
| Follow-up perceived norms | .269 | .030 | 8.93 | <.0001 | |
| Sex | −.960 | 1.018 | −.94 | .345 | |
| PNF | −.909 | .759 | −1.20 | .231 | |
| Social motives | −.062 | .094 | −.66 | .508 | |
| Conformity motives | −.216 | .103 | −2.09 | .037 | |
| Enhancement motives | −.003 | .113 | −.03 | .977 | |
| Coping motives | .303 | .412 | .73 | .463 | |
| Perceived norms X Coping motives | .106 | .020 | 5.35 | <.0001 | |
| PNF X Coping motives | .684 | .652 | 1.05 | .294 | |
Coping motives as a moderator of intervention efficacy for problems through post-intervention norms
We then examined coping motives as moderator of the indirect effect of PNF on alcohol-related problems at follow-up through perceived norms post-intervention. The model showed good fit, RMSEA = .030, CFI = .994, TLI = .984, χ2 = 25.55, p = .043. Controlling for sex, baseline alcohol-related problems, and all other drinking motives, coping motives significantly moderated the a path. However, moderation on the b path, the direct path, and the indirect path between feedback and follow-up problems through post-intervention norms were all non-significant (see Table 4).
Table 4.
Moderated mediation analyses with coping motives moderating the mediation of PNF on follow-up problems through post-intervention perceived norms
| Criterion | Predictor | b | se | t | p |
|---|---|---|---|---|---|
| Post- intervention perceived norms | Baseline perceived norms | .418 | .024 | 17.55 | <.0001 |
| Sex | 3.644 | 1.222 | 2.98 | .003 | |
| PNF | −11.255 | .830 | −13.57 | <.0001 | |
| Social motives | −.132 | .104 | −1.26 | .206 | |
| Conformity motives | .063 | .115 | .550 | .583 | |
| Enhancement motives | .236 | .125 | 1.89 | .059 | |
| Coping motives | .604 | .456 | 1.33 | .185 | |
| PNF X Coping motives | −3.634 | .721 | −5.04 | <.0001 | |
|
| |||||
| Follow-up problems | Baseline problems | .443 | .037 | 11.95 | <.0001 |
| Post-intervention perceived norms | .015 | .015 | 1.00 | .319 | |
| Sex | .104 | .539 | .192 | .848 | |
| PNF | −.907 | .420 | −2.16 | .031 | |
| Social motives | −.088 | .050 | −1.75 | .079 | |
| Conformity motives | .008 | .056 | .15 | .882 | |
| Enhancement motives | .014 | .060 | .233 | .816 | |
| Coping motives | .921 | .324 | 2.84 | .005 | |
| Perceived norms X Coping motives | −.004 | .011 | −.33 | .741 | |
| PNF X Coping motives | −.234 | .367 | −.64 | .524 | |
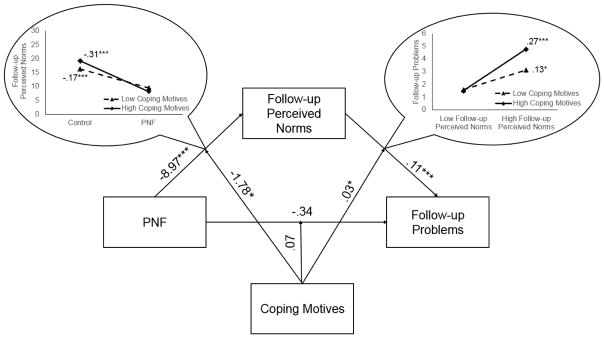
Coping motives as a moderator of intervention efficacy for problems through follow-up norms
Finally, we examined coping motives as moderator of the indirect effect of PNF on problems at follow-up through follow-up perceived norms (see Figure 3). This model showed good fit, RMSEA = .032, CFI = .993, TLI = .982, χ2 = 26.96, p = .029. Controlling for sex, baseline alcohol-related problems, and all other drinking motives, coping motives significantly moderated the a path, the b path, and the indirect path between feedback and follow-up drinking through follow-up norms (see Table 5). The indirect path between feedback and follow-up drinking was significant for those at lower levels of coping motives, b = −.570, SE = .133, [95% CI: −.85, −.35], mean levels of coping motives, b = −1.006, SE = .421, [95% CI: −1.54, −.59], and at higher levels of coping motives, b = −1.564, SE = .456, [95% CI: −2.68, −.83]. Echoing the findings for drinking, the moderated mediation effect was stronger the more frequently that participants reported drinking for coping reasons. Moderation on the direct path was not significant.
Figure 3.
Sex, baseline alcohol-related problems, baseline perceived descriptive drinking norms, enhancement motives, social motives, and conformity motives were included as covariates.
Table 5.
Moderated mediation analyses with coping motives moderating the mediation of PNF on follow-up drinking through follow-up perceived norms.
| Criterion | Predictor | b | se | t | p |
|---|---|---|---|---|---|
| Follow-up perceived norms | Baseline perceived norms | .293 | .027 | 10.75 | <.0001 |
| Sex | 5.687 | 1.352 | 4.21 | <.0001 | |
| PNF | −8.970 | 1.383 | −6.49 | <.0001 | |
| Social motives | −.101 | .123 | −.82 | .412 | |
| Conformity motives | −.011 | .136 | −.08 | .938 | |
| Enhancement motives | .172 | .146 | 1.18 | .240 | |
| Coping motives | 1.230 | .525 | 2.34 | .019 | |
| PNF X Coping motives | −1.783 | .837 | −2.13 | .033 | |
|
| |||||
| Follow-up problems | Baseline problems | .405 | .036 | 11.28 | <.0001 |
| Follow-up perceived norms | .112 | .017 | 6.76 | <.0001 | |
| Sex | −.664 | .521 | −1.27 | .203 | |
| PNF | −.338 | .562 | −.601 | .548 | |
| Social motives | −.085 | .048 | −1.75 | .080 | |
| Conformity motives | .032 | .054 | .60 | .549 | |
| Enhancement motives | −.006 | .058 | −.11 | .916 | |
| Coping motives | .295 | .297 | .99 | .320 | |
| Perceived norms X Coping motives | .025 | .010 | 2.47 | .014 | |
| PNF X Coping motives | .073 | .336 | .22 | .828 | |
Discussion
The present study extends the emerging literature on brief interventions to reduce heavy drinking among veterans by focusing on an important moderator of intervention efficacy: coping drinking motives. Our previous research demonstrated that a PNF intervention was efficacious in reducing normative misperceptions and problematic drinking among veterans (Pedersen et al., 2017b) and another of our studies found that coping motives moderated PNF intervention efficacy among college students (Young et al., 2016). Yet, this study is the first to investigate coping motives as a moderator of PNF intervention efficacy for veterans, a population at higher risk for mental health problems and coping-related drinking (Jakupcak et al., 2010; Lehavot, et al., 2014; McDevitt-Murphy et al., 2010; Miller et al., 2017; Seal et al., 2011). The present study was designed to evaluate whether PNF might similarly be more effective among individuals with higher coping motives in a sample of veterans.
As reported in our previous work (Pedersen et al., 2017b), PNF was associated with significant reductions in drinking and alcohol-related problems. In this case, this effect was fully mediated by changes in norms with the direct path becoming almost zero. Consistent with our original expectations, the indirect effect was moderated by drinking to cope. Thus, among veterans, PNF was more effective in reducing perceived norms among higher coping drinkers. In addition, reductions in perceived norms were more strongly associated with reduced drinking and problems among higher coping drinkers. Furthermore, the indirect effect was stronger among higher coping drinkers. In addition there was no direct effect, regardless of the level of coping drinking motives.
Overall, findings replicated the previous college student study in demonstrating better effects of PNF among individuals higher in coping motives, even when controlling for all other drinking motives. In both studies, individuals who were higher in coping motives had stronger associations between follow-up perceived norms and follow-up drinking. However, among the college student sample, coping motives did not significantly moderate the indirect effect between PNF and alcohol-related problems at follow-up through perceived norms whereas the present study found evidence of a significant moderated mediation for problems. This difference in findings is likely a function of overall study results. PNF was not found to reduce alcohol-related problems overall in the college sample, but did reduce problems in the veteran sample.
The similar findings from both studies suggest that PNF may be particularly effective among high coping drinkers across populations. The primary difference in the two studies seems to be the mechanism of action; that is, coping motives moderated PNF effects on perceived norms among veterans but not among college students. At least part of the explanation may be the level of identification that veterans have with one another relative to college students. Previous research has shown that in military units with high cohesion (e.g., strong social bonds among active duty military) drinking is closely tied to perceived norms (Brown et al., 2008; Wilk et al., 2010). The moderate correlations (e.g., r = .53) between perceived norms and drinking among veterans in these data further support this conclusion. Military personnel who serve in combat situations, as the vast majority (82%) of our sample have, must literally trust their peers with their lives. Lifetime friendships often result from shared extreme experiences unlike any others. Moreover, veterans may much more strongly identify with each other than college students do. As such, seeing that closely connected peers drink less than the participant him/herself did may have been a wake-up call that their own drinking may have crested to an unsafe level, and that others may be managing negative affect with alternate/non-drinking coping mechanisms.
Another significant difference between veterans and college students which may account for much stronger mediation effects for perceived norms among those higher in coping is the relative prevalence of coping motives. Coping motives are considerably stronger relative to social and enhancement motives among veterans. Compared to college student samples where average values for coping motives are 51%–70% lower than for social motives and 41%–62% lower than enhancement motives (Neighbors, Lee, Lewis, Fossos, & Larimer, 2007; Young et al., 2016), in the present study, average values for coping were only 18% lower than social motives and 4% lower than enhancement motives. Averages values for coping motives were 36% higher than conformity motives, which tend to be infrequently endorsed in all samples (e.g., Kuntsche et al., 2005; Lewis et al., 2008; McDevitt-Murphy, Fields, Monahan, & Bracken, 2015; Simpson et al., 2014; Stewart & Devine, 2000). Thus, in comparison to college students, veteran drinking is much more motivated by coping relative to other drinking motives.
Given the relatively higher rates of coping drinking among veterans in our sample and literature documenting that veterans misuse alcohol as a means to cope with underlying behavioral health concerns like PTSD and depression (Brady, Back, & Coffey, 2004; Eisen et al., 2012; Jakupcak et al., 2010; McDevitt-Murphy et al., 2010; Schumm & Chard, 2012), it seems likely that when veterans think about other veterans’ drinking behavior, they assume that others are likely drinking for the same reasons. Thus, when they find out that other veterans are drinking considerably less, they may also infer that they have found other ways to cope. While this is purely speculative, it is consistent with basic research indicating that people often infer others’ motivations to be similar to their own (i.e., false consensus effect; Ross, Greene, & House, 1977). Perhaps these coping drinkers are not drinking in social contexts often, so for them the feedback may not engage social comparison processes related to norms and drinking similarly to others and instead might be more of a reality check suggesting they drink much more than other veterans and that this might be problematic. Thus PNF may serve as a warning sign for veterans who drink to cope, alerting them that their drinking habits and use of alcohol as a means to cope with negative affect are non-normative compared to other veterans and may be maladaptive. This information may serve as a wake-up call which may motivate them to change their drinking habits and/or find other methods to cope with negative affect. Subsequent research assessing perceptions of other veterans’ motives for drinking would provide a means of evaluating this proposition.
An unexpected finding in the present study was the difference between post-intervention perceived norms compared to follow-up perceived norms as moderators of intervention efficacy. We found significant moderation on the a path and the indirect path for post-intervention norms, whereas we found significant moderation on the a path, b path, and indirect paths for follow-up norms. It is difficult to know why this occurred, but one possibility is because participants were asked to report on their perceived norms for drinking immediately after receiving the intervention (i.e., being told the actual norms), they did not have sufficient time to consider the implications of the information with respect to how or why other veterans might be drinking less than they were. If perceived norms really do mediate PNF more strongly for higher copers, they would need time to consider how coping fits with their own versus other veterans’ drinking.
Limitations and Future Directions
The findings from this study should be considered in light of some limitations. The sample was recruited online via Facebook and thus may not be representative of young adult veterans as a whole. For instance, the sample was mostly male and White/Caucasian which, though common for veteran samples, limits its generalizability. However, we have documented that Facebook is a viable mechanism to reach veterans in the community that may not be seeking care for alcohol misuse (Pedersen et al., 2016a; Pedersen et al., 2015). Additionally, the follow-up period of one-month is relatively short. The current study was funded to capture changes in drinking during this brief follow-up time, but future work may explore whether these associations are maintained over a longer period of time.
Conclusions
The current study is a secondary data analysis of a brief norms-based intervention targeting heavy drinking among young adult veterans. Findings generally provided evidence that PNF interventions may be especially efficacious for veterans who drink to cope with negative affect. Specifically, results demonstrated that veterans who more frequently drink to cope with negative affect reduced their perceived norms, drinking, and alcohol-related problems to a greater extent than veterans who reported less frequent drinking to cope. These results are promising, as veterans tend to endorse drinking for coping reasons at high levels, and thus may especially benefit from a brief intervention incorporating PNF.
Acknowledgments
This work was funded by a grant from the National Institute on Alcohol Abuse and Alcoholism (NIAAA R34 AA022400, “Brief Online Intervention to Reduce Heavy Alcohol Use Among Young Adult Veterans”) awarded to Eric R. Pedersen. Preparation of this article was also supported by National Institute on Alcohol Abuse and Alcoholism Grant R01 AA014576.
Footnotes
The ideas and data presented in this manuscript were also presented at the 2017 meeting of the Society for Personality and Social Psychology in San Antonio, TX and the 2017 meeting of the Association for Behavioral and Cognitive Therapies in San Diego, CA.
The original outcomes paper using these data was published in the Journal of Consulting and Clinical Psychology (Pedersen et al., 2017).
References
- Brady KT, Back SE, Coffey SF. Substance abuse and posttraumatic stress disorder. Current Directions in Psychological Science. 2004;13(5):206–209. [Google Scholar]
- Bray RM, Hourani LL. Substance use trends among active duty military personnel: Findings from the United States Department of Defense Health Related Behavior Surveys, 1980–2005. Addiction. 2007;102(7):1092–1101. doi: 10.1111/j.1360-0443.2007.01841.x. [DOI] [PubMed] [Google Scholar]
- Browne T, Iversen A, Hull L, Workman L, Barker C, Horn O, … Hotopf M. How do experiences in Iraq affect alcohol use among male UK armed forces personnel? Occupational and Environmental Medicine. 2008;65(9):628–633. doi: 10.1136/oem.2007.036830. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Schry AR, Wagner HR, Kimbrel NA, Dennis P, McDonald SD, … Straits-Troster K. The prevalence of binge drinking and receipt of provider drinking advice among US veterans with military service in Iraq or Afghanistan. The American Journal of Drug and Alcohol Abuse. 2016;42(3):269–278. doi: 10.3109/00952990.2015.1051185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied multiple regression/correlation analysis for the behavioral sciences. Routledge; 2013. [Google Scholar]
- Cooper ML. Motivations for alcohol use among adolescents: Development and validation of a four-factor model. Psychological Assessment. 1994;6(2):117–128. [Google Scholar]
- Cucciare MA, Weingardt KR, Ghaus S, Boden MT, Frayne SM. A randomized controlled trial of a web-delivered brief alcohol intervention in Veterans Affairs primary care. Journal of Studies on Alcohol and Drugs. 2013;74(3):428–436. doi: 10.15288/jsad.2013.74.428. [DOI] [PubMed] [Google Scholar]
- Doherty AM, Mason C, Fear NT, Rona R, Greenberg N, Goodwin L. Are brief alcohol interventions targeting alcohol use efficacious in military and veteran populations? A meta-analysis. Drug and Alcohol Dependence. 2017;178:571–578. doi: 10.1016/j.drugalcdep.2017.05.029. [DOI] [PubMed] [Google Scholar]
- Eisen SV, Schultz MR, Vogt D, Glickman ME, Elwy AR, Drainoni ML, … Martin J. Mental and physical health status and alcohol and drug use following return from deployment to Iraq or Afghanistan. American Journal of Public Health. 2012;102(S1):S66–S73. doi: 10.2105/AJPH.2011.300609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuehrlein BS, Mota N, Arias AJ, Trevisan LA, Kachadourian LK, Krystal JH, … Pietrzak RH. The burden of alcohol use disorders in US military veterans: Results from the National Health and Resilience in Veterans Study. Addiction. 2016;111(10):1786–1794. doi: 10.1111/add.13423. [DOI] [PubMed] [Google Scholar]
- Goldsmith AA, Tran GQ, Smith JP, Howe SR. Alcohol expectancies and drinking motives in college drinkers: Mediating effects on the relationship between generalized anxiety and heavy drinking in negative-affect situations. Addictive Behaviors. 2009;34(6):505–513. doi: 10.1016/j.addbeh.2009.01.003. [DOI] [PubMed] [Google Scholar]
- Golub A, Bennett AS. Substance use over the military-veteran life course: An analysis of a sample of OEF/OIF veterans returning to low income predominantly minority communities. Addictive Behaviors. 2014;39(2):449–454. doi: 10.1016/j.addbeh.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins EJ, Lapham GT, Kivlahan DR, Bradley KA. Recognition and management of alcohol misuse in OEF/OIF and other veterans in the VA: A cross sectional study. Drug and Alcohol Dependence. 2010;109(1):147–153. doi: 10.1016/j.drugalcdep.2009.12.025. [DOI] [PubMed] [Google Scholar]
- Hayes AF. Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press; 2013. [Google Scholar]
- Jacobson IG, Ryan MA, Hooper TI, Smith TC, Amoroso PJ, Boyko EJ, … Bell NS. Alcohol use and alcohol-related problems before and after military combat deployment. Journal of the American Medical Association. 2008;300(6):663–675. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakupcak M, Tull MT, McDermott MJ, Kaysen D, Hunt S, Simpson T. PTSD symptom clusters in relationship to alcohol misuse among Iraq and Afghanistan war veterans seeking post-deployment VA health care. Addictive Behaviors. 2010;35:840–843. doi: 10.1016/j.addbeh.2010.03.023. [DOI] [PubMed] [Google Scholar]
- Kahler CW, Strong DR, Read JP. Toward efficient and comprehensive measurement of the alcohol problems continuum in college students: The Brief Young Adult Alcohol Consequences Questionnaire. Alcoholism: Clinical and Experimental Research. 2005;29(7):1180–1189. doi: 10.1097/01.alc.0000171940.95813.a5. [DOI] [PubMed] [Google Scholar]
- Kang HK, Li B, Mahan CM, Eisen SA, Engel CC. Health of US veterans of 1991 Gulf War: A follow-up survey in 10 years. Journal of Occupational and Environmental Medicine. 2009;51(4):401–410. doi: 10.1097/JOM.0b013e3181a2feeb. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. Guilford publications; 2015. p. 23. [Google Scholar]
- Kramer J, Rubin A, Coster W, Helmuth E, Hermos J, Rosenbloom D, … Brief D. Strategies to address participant misrepresentation for eligibility in Web-based research. International Journal of Methods in Psychiatric Research. 2014;23(1):120–129. doi: 10.1002/mpr.1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuntsche E, Knibbe R, Gmel G, Engels R. Why do young people drink? A review of drinking motives. Clinical Psychology Review. 2005;25:841–861. doi: 10.1016/j.cpr.2005.06.002. [DOI] [PubMed] [Google Scholar]
- LaBrie JW, Lewis MA, Atkins DC, Neighbors C, Zheng C, Kenney SR, … Larimer ME. RCT of web-based personalized normative feedback for college drinking prevention: Are typical student norms good enough? Journal of Consulting and Clinical Psychology. 2013;81(6):1074–1086. doi: 10.1037/a0034087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehavot K, Stappenbeck CA, Luterek JA, Kaysen D, Simpson TL. Gender differences in relationships among PTSD severity, drinking motives, and alcohol use in a comorbid alcohol dependence and PTSD sample. Psychology of Addictive Behaviors. 2014;28(1):42–52. doi: 10.1037/a0032266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Hove MC, Whiteside U, Lee CM, Kirkeby BS, Oster-Aaland L, … Larimer ME. Fitting in and feeling fine: Conformity and coping motives as mediators of the relationship between social anxiety and problematic drinking. Psychology of Addictive Behaviors. 2008;22(1):58–67. doi: 10.1037/0893-164X.22.1.58. [DOI] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C. Social norms approaches using descriptive drinking norms education: A review of the research on personalized normative feedback. Journal of American College Health. 2006;54(4):213–218. doi: 10.3200/JACH.54.4.213-218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis MA, Neighbors C, Oster-Aaland L, Kirkeby BS, Larimer ME. Indicated prevention for incoming freshmen: Personalized normative feedback and high risk drinking. Addictive Behaviors. 2007;32:2495–2508. doi: 10.1016/j.addbeh.2007.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Cadigan JM, Rogers RE, Osborn ZH. Personalized drinking feedback intervention for veterans of the wars in Iraq and Afghanistan: A randomized controlled trial. Journal of Studies on Alcohol and Drugs. 2015;76(3):355–359. doi: 10.15288/jsad.2015.76.355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Neighbors C, Lewis MA, Lee CM, Oster-Aaland L, Larimer ME. The roles of negative affect and coping motives in the relationship between alcohol use and alcohol-related problems among college students. Journal of Studies on Alcohol and Drugs. 2008;69:412–419. doi: 10.15288/jsad.2008.69.412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martens MP, Smith AE, Murphy JG. The efficacy of single-component brief motivational interventions among at-risk college drinkers. Journal of Consulting and Clinical Psychology. 2013;81(4):691–701. doi: 10.1037/a0032235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Fields JA, Monahan CJ, Bracken KL. Drinking motives among heavy-drinking veterans with and without posttraumatic stress disorder. Addiction Research & Theory. 2015;23(2):148–155. doi: 10.3109/16066359.2014.949696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Murphy JG, Williams JL, Monahan CJ, Bracken-Minor KL, Fields JA. Randomized controlled trial of two brief alcohol interventions for OEF/OIF veterans. Journal of Consulting and Clinical Psychology. 2014;82(4):562–568. doi: 10.1037/a0036714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Williams JL, Bracken KL, Fields JA, Monahan CJ, Murphy JG. PTSD symptoms, hazardous drinking, and health functioning among U.S. OEF/OIF Veterans presenting to primary care. Journal of Traumatic Stress. 2010;23(1):108–111. doi: 10.1002/jts.20482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDevitt-Murphy ME, Williams JL, Murphy JG, Monahan CJ, Bracken-Minor KL. Brief intervention to reduce hazardous drinking and enhance coping among OEF/OIF/OND veterans. Professional Psychology: Research and Practice. 2015;46(2):83–89. doi: 10.1037/a0036771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarling L, D'Angelo M, Drain M, Gibbs DA, Rae Olmsted KL. Stigma as a barrier to substance abuse and mental health treatment. Military Psychology. 2011;23(1):1–5. [Google Scholar]
- Merrill JE, Thomas SE. Interactions between adaptive coping and drinking to cope in predicting naturalistic drinking and drinking following a lab-based psychosocial stressor. Addictive Behaviors. 2013;38:1672–1678. doi: 10.1016/j.addbeh.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller SM, Pedersen ER, Marshall GN. Combat experience and problem drinking in veterans: Exploring the roles of PTSD, coping motives, and perceived stigma. Addictive Behaviors. 2017;66:90–95. doi: 10.1016/j.addbeh.2016.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus (Version 7.4) Los Angeles, CA: 2014. [Google Scholar]
- Neighbors C, Larimer ME, Lewis MA. Targeting misperceptions of descriptive drinking norms: Efficacy of a computer-delivered personalized normative feedback intervention. Journal of Consulting and Clinical Psychology. 2004;72(3):434–447. doi: 10.1037/0022-006X.72.3.434. [DOI] [PubMed] [Google Scholar]
- Neighbors C, Lewis MA, Atkins DC, Jensen MM, Walter T, Fossos N, Larimer ME. Efficacy of Web-based personalized normative feedback: A two-year randomized controlled trial. Journal of Consulting and Clinical Psychology. 2010;78:898–911. doi: 10.1037/a0020766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neighbors C, Lewis MA, LaBrie J, DiBello AM, Young CM, Rinker DV, … Jerabeck JM. A multisite randomized trial of normative feedback for heavy drinking: Social comparison versus social comparison plus correction of normative misperceptions. Journal of Consulting and Clinical Psychology. 2016;84(3):238–247. doi: 10.1037/ccp0000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Helmuth ED, Marshall GN, Schell TL, PunKay M, Kurz J. Using Facebook to recruit young adult veterans: Online mental health research. JMIR Research Protocols. 2015;4(2):e63. doi: 10.2196/resprot.3996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Marshall GN, Schell TL. Study protocol for a web-based personalized normative feedback alcohol intervention for young adult veterans. Addiction Science & Clinical Practice. 2016a;11(1):1–15. doi: 10.1186/s13722-016-0055-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Marshall GN, Schell TL, Neighbors C. Young adult veteran perceptions of peers’ drinking behavior and attitudes. Psychology of Addictive Behaviors. 2016b;30(1):39–51. doi: 10.1037/adb0000120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Naranjo D, Marshall GN. Recruitment and retention of young adult veteran drinkers using Facebook. PLOS One. 2017a;12(3):e0172972. doi: 10.1371/journal.pone.0172972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pedersen ER, Parast L, Marshall GN, Schell TL, Neighbors C. A randomized controlled trial of a web-based, personalized normative feedback alcohol intervention for young-adult veterans. Journal of Consulting and Clinical Psychology. 2017b;85:459–470. doi: 10.1037/ccp0000187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pemberton MR, Williams J, Herman-Stahl M, Calvin SL, Bradshaw MR, Bray RM, … Mitchell GM. Evaluation of two web-based alcohol interventions in the U.S. military. Journal of Studies on Alcohol and Drugs. 2011;72:480–489. doi: 10.15288/jsad.2011.72.480. [DOI] [PubMed] [Google Scholar]
- Platt L, Melendez-Torres GJ, O'Donnell A, Bradley J, Newbury-Birch D, Kaner E, Ashton C. How effective are brief interventions in reducing alcohol consumption: do the setting, practitioner group and content matter? Findings from a systematic review and meta-regression analysis. BMJ Open. 2016;6(8):e011473. doi: 10.1136/bmjopen-2016-011473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramsey C, Dziura J, Justice AC, Altalib HH, Bathulapalli H, Burg M, … Kulas J. Incidence of Mental Health Diagnoses in Veterans of Operations Iraqi Freedom, Enduring Freedom, and New Dawn, 2001–2014. American Journal of Public Health. 2017;107(2):329–335. doi: 10.2105/AJPH.2016.303574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross L, Greene D, House P. The “false consensus effect”: An egocentric bias in social perception and attribution processes. Journal of Experimental Social Psychology. 1977;13(3):279–301. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schumm JA, Chard KM. Alcohol and stress in the military. Alcohol Research: Current Reviews. 2012;34(4):401–407. [PMC free article] [PubMed] [Google Scholar]
- Seal KH, Cohen G, Waldrop A, Cohen BE, Maguen S, Ren L. Substance use disorders in Iraq and Afghanistan veterans in VA healthcare, 2001–2010: Implications for screening, diagnosis and treatment. Drug & Alcohol Dependence. 2011;116:93–101. doi: 10.1016/j.drugalcdep.2010.11.027. [DOI] [PubMed] [Google Scholar]
- Simpson TL, Stappenbeck CA, Luterek JA, Lehavot K, Kaysen DL. Drinking motives moderate daily relationships between PTSD symptoms and alcohol use. Journal of Abnormal Psychology. 2014;123(1):237–247. doi: 10.1037/a0035193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stahre MA, Brewer RD, Fonseca VP, Naimi TS. Binge drinking among US active-duty military personnel. American Journal of Preventive Medicine. 2009;36(3):208–217. doi: 10.1016/j.amepre.2008.10.017. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Devine H. Relations between personality and drinking motives in young adults. Personality and Individual Differences. 2000;29(3):495–511. [Google Scholar]
- Swinkels CM, Ulmer CS, Beckham JC, Buse N, Calhoun PS VA Mid-Atlantic MIRECC Registry Workgroup. The association of sleep duration, mental health, and health risk behaviors among US Afghanistan/Iraq era veterans. Sleep. 2013;36(7):1019–1025. doi: 10.5665/sleep.2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teitcher JE, Bockting WO, Bauermeister JA, Hoefer CJ, Miner MH, Klitzman RL. Detecting, preventing, and responding to “fraudsters” in internet research: ethics and tradeoffs. The Journal of Law, Medicine & Ethics. 2015;43(1):116–133. doi: 10.1111/jlme.12200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whiteman SD, Barry AE. A comparative analysis of student service member/veteran and civilian student drinking motives. Journal of Student Affairs Research and Practice. 2011;48(3):297–313. doi: 10.2202/1949-6605.6322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilk JE, Bliese PD, Kim PY, Thomas JL, McGurk D, Hoge CW. Relationship of combat experiences to alcohol misuse among U.S. soldiers returning from the Iraq war. Drug and Alcohol Dependence. 2010;108:115–121. doi: 10.1016/j.drugalcdep.2009.12.003. [DOI] [PubMed] [Google Scholar]
- Wisco BE, Marx BP, Wolf EJ, Miller MW, Southwick SM, Pietrzak RH. Posttraumatic stress disorder in the US veteran population: results from the National Health and Resilience in Veterans Study. Journal of Clinical Psychiatry. 2014;75(12):1338–1346. doi: 10.4088/JCP.14m09328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young CM, Neighbors C, DiBello AM, Sharp C, Zvolensky MJ, Lewis MA. Coping motives moderate efficacy of personalized normative feedback among heavy drinking US college students. Journal of Studies on Alcohol and Drugs. 2016;77(3):495–499. doi: 10.15288/jsad.2016.77.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young-Wolff KC, Kendler KS, Sintov ND, Prescott CA. Mood-related drinking motives mediate the familial association between major depression and alcohol dependence. Alcoholism: Clinical and Experimental Research. 2009;33(8):1476–1486. doi: 10.1111/j.1530-0277.2009.00978.x. [DOI] [PMC free article] [PubMed] [Google Scholar]