Abstract
Importance
It is critical to develop a better understanding of the strategies provider organizations use to improve the performance of frontline clinicians and whether ACO participation is associated with differential adoption of these tools.
Objectives
Characterize the strategies that physician practices use to improve clinician performance and determine their association with ACOs and other payment reforms.
Data Sources
The National Survey of Healthcare Organizations and the National Survey of ACOs fielded 2017‐2018 (response rates = 47 percent and 48 percent).
Study Design
Descriptive analysis for practices participating and not participating in ACOs among 2190 physician practice respondents. Linear regressions to examine characteristics associated with counts of performance domains for which a practice used data for feedback, quality improvement, or physician compensation as dependent variables. Logistic and fractional regression to examine characteristics associated with use of peer comparison and shares of primary care and specialist compensation accounted for by performance bonuses, respectively.
Principal Findings
ACO‐affiliated practices feed back clinician‐level information and use it for quality improvement and compensation on more performance domains than non‐ACO‐affiliated practices. Performance measures contribute little to physician compensation irrespective of ACO participation.
Conclusion
ACO‐affiliated practices are using more performance improvement strategies than other practices, but base only a small fraction of compensation on quality or cost.
Keywords: Accountable Care Organizations, financial incentives, physician practices, quality improvement
1. INTRODUCTION
Both public and private health insurers in the United States have made significant progress toward introducing value‐based elements into their payment systems.1 We consider payments or nonfinancial mechanisms to be value‐based if they incorporate incentives or information that encourages providers to improve quality, reduce waste (ie, costs that are not justified by benefits), or both. The Accountable Care Organization (ACO) model, which assigns accountability for the cost and quality of care of a population of patients to a provider organization, is the most prominent value‐based payment reform and the centerpiece of Medicare's drive toward more effective and affordable care.2 ACO contracts are also used by Medicaid agencies, Medicaid managed care organizations, and commercial insurers. By design, ACO arrangements delegate responsibility for coordinating and managing care to a high‐level provider organization (the ACO entity), often a health system or physician organization. The ACO pools risk across participating providers and deploys a mix of incentives, information technologies, and care management processes to achieve the cost and quality targets set by payers.
There has been mixed success with ACO models and related value‐based payment approaches (eg, pay for performance) in terms of organizational transformations that lead to improved cost and quality outcomes raising the question of why some provider organizations succeed and others fail.3, 4, 5, 6, 7 The answer to this question may lie in the specific configuration of internal mechanisms (eg, electronic health records) for performance improvement adopted by provider organizations facing new expectations for quality improvement and cost control. While ACO contracts change the incentives between the payer and the provider organization, in organizations that are not owned by frontline clinicians, improvements may also require aligning the incentives further downstream to reach frontline clinicians. Research has shown that financial incentives may influence the behavior of frontline clinicians in ACOs and thus the quality of care for patients, though the optimal design of such incentives remains a subject of debate.8, 9 As ACO participation continues to rise,10, 11 it is critical to develop a better understanding of the strategies provider organizations use to improve the performance of frontline clinicians.
The entities that identify as ACOs (groups of providers that hold ACO contracts) vary widely in size, structure, and adoption of financial and nonfinancial mechanisms to manage the quality and cost of patient care.12, 13 Reporting on 2012‐2013 survey data, Ryan et al14 found that although ACO practices provided comparably higher compensation for quality than non‐ACO practices, they also provide a similar mix of compensation based on productivity and salary. Previous surveys have suggested that physician compensation in ACOs may be evolving and that entities with more experience in risk contracting are using more targeted financial incentives for physicians.13 Little is known, however, about the current use of financial and nonfinancial mechanisms for performance improvement—defined as a combination of cost control and quality improvement—in ACO‐related physician practices compared with other health care organizations. In this paper, we use two recent national surveys to characterize the strategies that physician practices use to improve performance and to determine whether participation in ACOs and other payment reforms is associated with such strategies.
2. METHODS
2.1. Data
The National Survey of Healthcare Organizations and Systems (NSHOS), funded by the Agency for Health Research and Quality and led by the Dartmouth‐Berkeley‐Harvard‐High Value Health Collaborative Center of Excellence, was fielded in 2017 and 2018 and included a physician practice survey that we use here (practice response rate = 47 percent). The physician practice survey sample was extracted from the IQVIA OneKey database that included all primary care or multispecialty medical practice with at least three primary care physicians (general practice, family practice, internal medicine, or geriatrics). Practices are defined as a set of providers delivering care as a group at a single location, and they could be independent or part of a larger medical group (eg, with multiple practice sites) or health care system (eg, integrated delivery system or hospital system). Being part of an ACO, for the purposes of this study, is defined as a practice that participates in any one of four ACO contract models: Medicare ACO upside‐only risk‐bearing contracts, Medicare ACO risk‐bearing contracts, Medicaid ACO contracts, and Commercial ACO contracts. A stratified‐cluster sampling design was used to draw samples of physician practices under different organizational structures, ranging from those within multitiered corporate structures to those that are independent operations.
The NSHOS includes a wide range of questions about practice characteristics, including practice size and ownership, payment models, and the use of specific mechanisms to improve the effectiveness and efficiency of health care delivery. Respondents were typically a practice manager/administrator (69 percent), a currently practicing physician (18 percent), medical director (6 percent), or executive (6 percent). The surveys themselves and the methods for fielding, managing, and analyzing the survey data were approved by the Dartmouth College Institutional Review Board.
Two questions involving the standardization of performance management and the distribution of shared savings compensation practices from the National Survey of ACOs (NSACO) were used to help interpret the findings. This survey was fielded from July 2017 to February 2018. The survey sample, which included ACO entities that participated in any type of ACO contract including those sponsored by public and private payers, was identified through multiple sources, including CMS data, Internet data collection, and information from Leavitt Partners. It included an estimated 862 ACOs with available contact data as of July 2017. Fifty‐five percent returned a survey, and we analyzed 419 complete surveys (adjusted response rate: 48 percent). Respondents typically had leadership roles in the ACO, such as executive director (29 percent), CEO (14 percent), vice president (9 percent), or medical director (7 percent), with a variety of other executive and staff titles making up the remainder.
2.2. Measures
The first set of outcomes from the NSHOS reported in this paper comprises indicators that measure the degree to which physician practices use individual clinician‐level data for feedback, quality improvement, and compensation in seven performance domains including preventive services, patient experience, underuse of high‐value care, overuse of low‐value care, use of acute care services, clinical quality, and total inpatient cost of care. Practices were asked to report whether they shared data in a way that allows individual clinicians to compare their performance with each other (ie, peer comparison). Finally, we examined the reported sources of physician compensation, separately for primary care physicians and specialists. Specifically, we asked practices to report the percentage of compensation in each of the following categories (which sum to 100 percent): guaranteed base salary or hourly compensation, productivity, patient panel size, performance bonuses for clinical quality, performance bonuses for reducing costs or utilization, patient satisfaction or experiences, or for other reasons.
For multivariate analysis, our primary explanatory variable of interest was an indicator of current ACO participation. Our remaining independent variables captured a range of structural and contractual characteristics, along with an indicator for census region. Previous studies have shown that organizational structure and size are associated with differences in financial incentives and capabilities related to quality measurement and improvement.15, 16 To capture these effects, we included a variable for practice size measured as the number of providers (primary care physicians, specialist physicians, nurse practitioners, and physician assistants), ownership (independent, part of a hospital or medical group, and part of a system), whether the practice was multispecialty (vs primary care only), and affiliation with one or more independent physician associations (IPAs). We also included an indicator of Federally Qualified Health Center (FQHC) status, in light of efforts by the federal government to require and support performance improvement in FQHCs.17
Economic theory and previous research have shown that when providers face a mix of payment incentives, they will tend to adopt practices that are consistent with their dominant incentives.18 Thus, we would expect that practices with more of their revenues from ACO and ACO‐like contracts will behave differently from practices with relatively little of such revenues. To capture the intensity of participation in ACO contracts and related incentives, we constructed variables that measure participation in any non‐ACO value‐based payment models or delivery reform (bundled payment, pay for performance, quality improvement initiatives, or capitation) and expectations about the extent of ACO (and ACO‐like models) participation projected in 5 years (none, some, most, or all).
2.3. Statistical analysis
In all analyses, we account for the probability sample and the likelihood of a sampled organization responding to the survey by using weights reflecting both of these and statistical procedures for survey data analysis. More specifically, to account for the complex survey design and survey nonresponse, we used the survey weights in conjunction with the svyset command in Stata19 to inform the analysis of the sample weights and design.
We summarized all outcome and explanatory variables for practices participating in ACOs and those not participating in ACOs (hereafter ACO and non‐ACO practices) according to self‐reported status in the National Survey of Healthcare Organizations and Systems. We used survey design‐adjusted bivariate analysis to assess unadjusted differences between ACO and non‐ACO practices. For multivariable analysis, we constructed simple aggregate counts (ranging from zero to seven) of performance domains for which a practice used data for feedback, quality improvement, or physician compensation, respectively, as the dependent variable in our first three regressions. We analyzed the factors (described above) associated with these count variables using a linear regression for ease of interpretation. These factors were then subject to a sensitivity analysis using ordered logistic regressions. The use of peer comparison was analyzed using logistic regression; marginal effects as a percentage of use of peer comparison were reported. We analyzed the shares of primary care and specialist compensation accounted for by performance bonuses related to either cost or quality (ie, the sum of quality and cost bonuses) using fractional regression; marginal effects as a percentage of compensation were reported. All analyses were conducted using Stata version 15.19
3. RESULTS
Sixty‐five percent of practices (1426 respondents) reported current participation in an ACO arrangement (Table 1). The median practice size (number of employed or affiliated physicians) in the sample was 5, with an interquartile range of 3 to 14 physicians (data not shown). ACO participation varied significantly by region (P < .01) and by size of practice (P = .03). ACO practices were more likely to be owned by systems, medical groups, or hospitals, and less likely to be independent (P < .01). ACO practices were more likely to be affiliated with one or more IPAs (P < .01). ACO practices were significantly more likely to participate in one or more non‐ACO value‐based payment initiatives or delivery reforms and much more likely to expect that all or most of their revenues would come through ACO contracts in 5 years (P < .01).
Table 1.
Practice characteristics
| Variables | All practices | ACO | Non‐ACO | P‐value of differencea |
|---|---|---|---|---|
| Practice characteristics, n | 2002 | 1426 | 576 | |
| Census Region | ||||
| Northeast | 399 | 316 | 83 | <.01 |
| (%) | (21.09) | (24.16) | (15.47) | |
| Midwest | 582 | 412 | 170 | |
| (25.02) | (25.67) | (23.83) | ||
| South | 533 | 355 | 178 | |
| (29.25) | (26.65) | (34.01) | ||
| West | 488 | 343 | 145 | |
| (24.64) | (23.52) | (26.69) | ||
| Multispecialty | 909 | 646 | 263 | .28 |
| (44.32) | (45.67) | (41.85) | ||
| Size of practice (# Clinicians) | 27.11 | 30.85 | 20.28 | .03 |
| (SD) | (139.93) | (166.46) | (68.20) | |
| Ownership | ||||
| System | 771 | 568 | 203 | .01 |
| (34.06) | (36.95) | (28.77) | ||
| Medical group/hospital owned | 639 | 468 | 171 | |
| (32.56) | (34.92) | (28.25) | ||
| Independent practice | 581 | 385 | 196 | |
| (33.38) | (28.13) | (42.98) | ||
| One or more IPAS | 430 | 340 | 90 | <.01 |
| (19.86) | (23.90) | (12.47) | ||
| FQHC | 275 | 205 | 70 | .29 |
| (15.75) | (16.81) | (13.81) | ||
| Participates in non‐ACO VBP | 1733 | 1323 | 410 | <.01 |
| (82.78) | (90.38) | (68.87) | ||
| ACO in 5 y (most or all) | 893 | 761 | 132 | <.01 |
| (39.49) | (55.35) | (19.69) | ||
| Uses of peer comparison | 2002 | 1056 | 327 | <.01 |
| 68.08 | 74.02 | 56.84 | ||
| PCP % Compensation | ||||
| Salary | 47.99 | 48.24 | 47.50 | .82 |
| (SD) | (42.52) | (42.08) | (43.41) | |
| Productivity | 42.08 | 40.97 | 44.26 | .30 |
| (40.03) | (38.88) | (42.15) | ||
| Panel size | 2.02 | 2.12 | 1.79 | .62 |
| (8.02) | (7.90) | (8.26) | ||
| Performance bonuses | 5.22 | 6.20 | 3.42 | <.01 |
| (9.56) | (9.90) | (8.63) | ||
| Specialist % Compensation | ||||
| Salary | 47.23 | 43.87 | 53.21 | .15 |
| (43.73) | (43.47) | (43.71) | ||
| Productivity | 45.70 | 47.70 | 42.14 | .37 |
| (42.91) | (42.83) | (42.96) | ||
| Panel size | 0.86 | 0.95 | 0.76 | .71 |
| (4.71) | (4.81) | (4.56) | ||
| Performance bonuses | 1.30 | 1.52 | 0.90 | .12 |
| (6.24) | (6.52) | (5.67) | ||
P‐values for region and ownership reflect chi‐squared tests for the comparison of the set of mutually exclusive response items in each. Performance bonuses include bonuses for clinical quality, reducing costs or utilizations, and patient satisfaction or experiences. Total number of practices, unweighted, that responded to the NSHOS survey was 2190; this table includes all those with complete data for the relevant questions.
The majority of surveyed practices provided feedback on performance information for individual clinicians in their practice (85.60 percent, data not shown). Bivariate comparisons showed the ACO practices were more likely to use peer comparison (74.02 percent vs 56.84 percent, P < .01) but had similar patterns of primary care and specialist compensation, except that primary care physicians in ACO practices had higher shares of their compensation determined by performance, defined as a combination of patient satisfaction, quality, and cost (6.20 percent vs 3.42 percent, P < .01). On all seven domains of performance, the percentage of ACO practices that feed back clinician‐level information and use it for quality improvement and compensation was higher than non‐ACO practices (Figure 1, all statistically significant differences excepting “overuse of low‐value care” and “total inpatient cost of care” for compensation).
Figure 1.
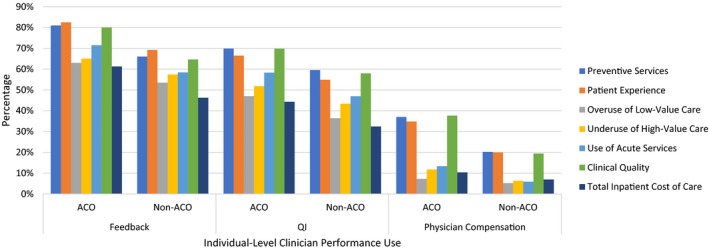
Clinician‐level data collection and use. Note: Bivariate differences between ACO practices and non‐ACO practices were statistically significant with P < .05 for all comparisons except physician compensation for overuse and total inpatient cost of care [Color figure can be viewed at wileyonlinelibrary.com]
In multivariate analysis (Table 2), ACO affiliation was positively associated with feeding performance information back to physicians in more domains (0.55, P = .02), using more performance information for quality improvement (0.53, P = .01) and compensation (0.42, P = .01), and use of peer comparison (marginal effect (percent) = 0.90 percent, P < .01). Participation in non‐ACO value‐based purchasing initiatives was positively associated with the extent of performance feedback (0.87, P < .01), using performance information for compensation (0.42, P = .01), and use of peer comparison (9.03 percent, P = .03). Affiliation with a health system was positively related to the extent performance data were used for compensation (0.31; P = .02) and, conversely, being an independent practice was negatively associated with using performance data for compensation (−0.51, P < .01). Practices that expected most or all revenues within 5 years would be through accountable care models were more likely to provide feedback of clinician‐level performance data (0.49, P = .01), use performance data for quality improvement (0.52, P = .01) and use peer comparison (7.81 percent, P = .03). With the western region as a reference point, location in the northeast region was negatively associated with use of performance data for compensation (−0.39, P = .03) and the use of peer comparison (−21.35 percent, P < .01). Location in the south was also associated with lower odds of using peer comparison (−12.03 percent, P = .01). Practices that were owned by systems (1.67 percent, P = .01), affiliated with IPAs (2.12 percent, P < .01), and expected most or all revenues within 5 years to be through ACO contracts (2.30 percent, P < .01) had a larger share of compensation in the form of performance bonuses for primary care physicians, while independent (−1.68 percent, P = .04) and multispecialty practices (−1.13 percent, P = .03) had smaller performance bonuses. Independent practices also had a lower percentage of using peer comparison (−7.63 percent, P = .04). Only location in the northeast region was associated with size of specialist performance bonuses (−1.35, P = .05). In ordered logistic sensitivity analyses (see Appendix S1), our main results are quantitatively similar with some differences, particularly in the importance of FQHC designation and regional effects.
Table 2.
Association between practice characteristics and use of performance management mechanisms
| Feedback | Quality improvement | Physician compensation | Peer comparison | % Performance bonus—PCPs | % Performance bonus—specialists | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coefficient | P‐value | Coefficient | P‐value | Coefficient | P‐value | Marginal effect (%) | P‐value | Marginal effect (%) | P‐value | Marginal effect (%) | P‐value | |
| Northeast | −0.22 | .42 | −0.53 | .05* | −0.39 | .03* | −21.35 | <.01** | −1.53 | .08 | −1.35 | .05 |
| Midwest | 0.09 | .71 | 0.03 | .92 | −0.17 | .27 | −1.68 | .73 | 0.31 | .68 | −0.01 | .98 |
| South | 0.37 | .15 | 0.11 | .68 | −0.27 | .08 | −12.03 | .01* | 0.46 | .57 | 0.26 | .62 |
| Scaled size of practice | 0.02 | .43 | 0.00 | 1.00 | 0.01 | .86 | 1.33 | .37 | 0.09 | .20 | 0.04 | .14 |
| Independent | 0.22 | .31 | 0.22 | .31 | −0.51 | <.01** | −7.63 | .04* | −1.68 | .04* | −1.16 | .08 |
| System | 0.18 | .35 | 0.08 | .65 | 0.31 | .02* | 1.54 | .66 | 1.67 | .01** | −0.31 | .53 |
| Multispecialty | 0.20 | .25 | 0.11 | .54 | −0.12 | .29 | −1.65 | .60 | −1.13 | .03* | 0.66 | .13 |
| FQHC | 0.09 | .68 | 0.47 | .02* | −0.33 | .03* | 12.87 | <.01** | 0.09 | .92 | 0.50 | .39 |
| IPAs | 0.34 | .09 | 0.15 | .47 | 0.36 | .02* | 0.98 | .79 | 2.12 | <.01** | 0.83 | .16 |
| Part of an ACO | 0.55 | .02* | 0.53 | .01* | 0.42 | .01** | 10.90 | .00** | 1.50 | .06 | 0.36 | .55 |
| Non‐ACO VBP | 0.87 | .00** | 0.48 | .09 | 0.42 | .01** | 9.03 | .03* | 1.67 | .11 | 0.32 | .63 |
| ACO in 5 y | 0.49 | .01* | 0.52 | .01** | 0.19 | .13 | 7.81 | .03* | 2.30 | .00** | 0.36 | .38 |
| Obs. | 2002 | 2002 | 2002 | 2002 | 2002 | 2002 | ||||||
| R‐squared | .06 | .04 | .09 | .09 | .07 | .02 | ||||||
Part of an ACO encompasses practices that participate in a Medicare ACO upside‐only risk‐bearing contract, a Medicare ACO risk‐bearing contract, a Medicaid ACO contract, or a commercial ACO contract. Non‐ACO VBP indicates participation in any non‐ACO value‐based payment models or delivery reform (bundled payment, pay for performance, quality improvement initiatives, or capitation). An ACO in 5 y is defined as a practice that predicts that most or all of its revenue will be covered by ACO contracts with total cost of care accountability within 5 y. Left out categories are west for region and owned by medical group or hospital for ownership.
P < .01.
P < .05.
In the National Survey of ACOs, almost half (47 percent) of ACOs reported that physician compensation processes were at least somewhat standardized across the ACO, while 74 percent reported at least somewhat standardized primary care physician management processes (Figure 2). More than half of ACOs (61 percent) planned to distribute a portion of their potential shared savings rewards directly to physicians (data not shown).
Figure 2.
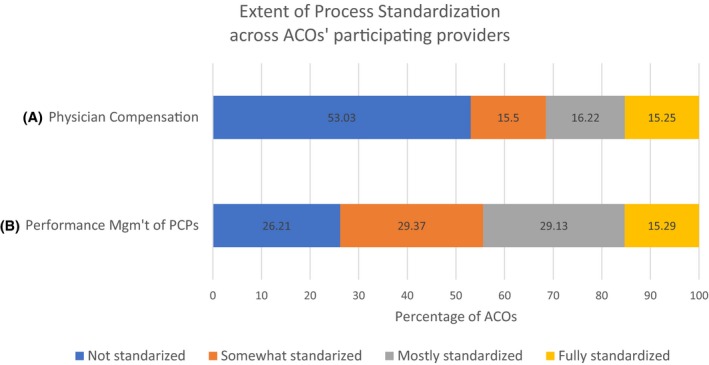
Extent of Process Standardization across ACOs' participating providers. Data source: National Wave 4 of the National Survey of Accountable Care Organizations, fielded 2017‐2018. Shown are responses to the following question: “To what extent are these processes standardized (done in the same way) across the participating organizations in your ACO?: (A) Physician compensation (B) Performance management of primary care physicians.” PCPs refer to primary care physicians [Color figure can be viewed at wileyonlinelibrary.com]
4. DISCUSSION
Across seven domains of measurement, ACO practices were systematically more likely than other practices to use clinician‐level performance data for feedback, quality improvement, and compensation. This pattern included the use of data for peer comparisons. Nonetheless, adoption of these data and physician management tools is far from universal among ACO practices. In contrast, ACO affiliation was not associated with the percent of compensation based on performance bonuses for either primary care or specialists, while ownership by a system, IPA affiliation, and high future expectations of ACO involvement were associated with the size of primary care performance bonuses. Consistent with the hypothesis that external incentives are a factor associated with the adoption of internal performance improvement mechanisms, practices participating in any non‐ACO payment or delivery reforms were also more likely to provide feedback of clinician‐level performance data and use them to compensate physicians. Moreover, our findings underscore that practices with more current and projected activity under value‐based contracts are more engaged in performance management. Thus, if commercial ACO and other value‐based contracts become increasingly prevalent, we may see ACO practices evolve further. For these efforts to be successful, however, it may be necessary to create regional approaches to align value‐based programs across multiple payers. Greater adoption of performance management tools may be a prerequisite and/or a result of participation in practice and delivery system reforms.
Overall, the share of compensation tied to performance remains extremely low for both primary care providers and specialists. Productivity and salary constitute the lion's share of compensation, while panel size represents only a tiny percentage of the average physician's compensation. The fact that even in 2018, ACO practices do not appear to be using financial incentives as an important mechanism for influencing care delivery is an area for further study. It may be that the feedback of performance data and peer comparisons are more effective motivators than increasing the percent of individual compensation based on cost or quality metrics.20 One of the key challenges for implementing financial incentives is that some clinicians may have a small proportion of patients participating in ACOs, and thus, creating financial incentives that are large enough to change behavior may be challenging.
Organizational structure, but not practice size, was independently associated with more extensive use of clinician‐level performance data and larger shares of primary care compensation for performance. Practices integrated with medical groups, hospitals, and health systems may be better able to invest in, build, and deploy performance management mechanisms. Similarly, FQHCs appear to have greater capacity to manage performance, perhaps because FQHC status requires providers to outline and implement processes that are associated with improvements in efficiency, better performance management, and quality of care. Furthermore, obtaining FQHC status comes with some benefits, including higher reimbursement rates, access to lower drug prices, and capacity‐development grants.21
About four‐fifths of ACOs are made up of new partnerships and combinations of previously independent entities.22 An important caveat to these self‐reported results may be that it is true for some parts of the organization participating in an ACO but not all participating entities. Therefore, we included results on standardization of compensation practices within ACOs. We found that three‐quarters of ACOs standardize primary care physician management practices, while only half standardize physician compensation.
Overall, practices participating in ACOs had higher rates of peer comparison of performance, performance reporting, and tying performance data to compensation compared to non‐ACO practices. However, there were high rates of variability in these activities across practices based on geography, organizational characteristics, and participation in other value‐based payment models. This variability may be driven by a lack of evidence related to activities associated with improved ACO success. As the participation of health care organizations in ACO type arrangements increases, it will be important to generate the evidence for practices associated with improved success of ACOs.
Our findings should be considered in light of several limitations. First, all of our information is based on self‐report from respondents (typically the practice manager, the medical director, or a group of practice managers and/or medical directors) who may not have complete information about every survey domain. However, in piloting the survey we found that respondents occupying these positions were able to provide the information. Further, these are objective measures of structure and process that are most likely to be known or easily accessible to practice leaders. Second, we focus only on practices with at least three primary care physicians, so our results may not generalize to very small or specialist‐focused practices. Third, we do not know with any certainty the level of ACO coverage within a practice and rely instead on a qualitative assessment of the future importance of these contracts to measure the strength of incentives. Finally, our study is cross‐sectional in design so that we are unable to examine the direction of impact of ACO contracts or other value‐based purchasing programs on the use of performance management mechanisms.
ACO contracts are intentionally agnostic as to how incentives are transmitted from the entity receiving them to frontline clinicians. To date, it appears that nonfinancial performance management mechanisms are common, while financial incentives are minimally deployed to achieve ACO goals. Future research should examine barriers to adoption of performance incentives for frontline physicians and the relationship between performance management strategies in ACOs and the cost and outcomes of care.
Supporting information
ACKNOWLEDGMENTS
Joint Acknowledgment/Disclosure Statement: This work was supported, in part, by the Agency for Healthcare Research and Quality's (AHRQ's) Comparative Health System Performance Initiative under Grant # 1U19HS024075, which studies how health care delivery systems promote evidence‐based practices and patient‐centered outcome research in delivering care. The findings and conclusions in this article are those of the authors and do not necessarily reflect the views of AHRQ. The statements, findings, conclusions, views, and opinions contained and expressed in this article are based in part on data obtained under license from IQVIA information services: OneKey subscription information services 2010‐2017, IQVIA Incorporated, all rights reserved. The statements, findings, conclusions, views, and opinions contained and expressed herein are not necessarily those of IQVIA Incorporated or any of its affiliated or subsidiary entities. AMA is the source for the raw physician data. Wave 4 of the National Survey of ACOs was supported by the Commonwealth Fund (Grant No 20160616), the National Institute of Mental Health of the National Institutes of Health (Grant No R01MH109531), and the California Health Care Foundation (Grant No 20249). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Rosenthal M, Shortell S, Shah ND, et al. Physician practices in Accountable Care Organizations are more likely to collect and use physician performance information, yet base only a small proportion of compensation on performance data. Health Serv Res. 2019;54:1214–1222. 10.1111/1475-6773.13238
REFERENCES
- 1. McClellan MB, Feinberg DT, Bach PB, et al. Payment reform for better value and medical innovation. NAM Perspect. 2017;7(3):191‐220. [Google Scholar]
- 2. Muhlestein D, Saunder RS, Richards R, McClellan MB. Recent progress in the value journey: growth of ACOs and value‐based payment models in 2018. Health Affairs Blog. 2018.
- 3. Lewis VA, Fisher ES, Colla CH. Explaining sluggish savings under accountable care. N Engl J Med. 2017;377(19):1809‐1811. Add cites 10, 17, 18 from the U19 proposal for Project 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Kaufman BG, Spivack BS, Stearns SC, Song PH, O'Brien EC. Impact of Accountable Care Organizations on Utilization, care, and outcomes: systematic review. Med Care Res Rev. 2019;76(3):255‐290. [DOI] [PubMed] [Google Scholar]
- 5. Colla CH, Wennberg DE, Meara E, et al. Spending differences associated with the Medicare physician group practice demonstration. JAMA. 2012;308:1015‐1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Fisher ES, Staiger DO, Bynum JPW, Gottlieb DJ. Creating Accountable Care Organizations: the extended hospital medical staff. Health Aff. 2007;26:w44‐w57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lewis VA, Colla CH, Schoenherr KE, Shortell SM, Fisher ES. Innovation in the safety net: integrating community health centers through accountable care. J Gen Intern Med. 2014;29(11):1484‐1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Quast T, Sappington DEM, Shenkman E. Does the quality of care in Medicaid MCOs vary with the form of physician compensation? Health Econ. 2008;17(4):545‐550. [DOI] [PubMed] [Google Scholar]
- 9. Helmchen LA, Lo Sasso AT. How sensitive is physician performance to alternative compensation schedules? Evidence from a large network of primary care clinics. Health Econ. 2010;19(11):1300‐1317. [DOI] [PubMed] [Google Scholar]
- 10. Muhlestein D, Saunder RS, Richards R, McClellan MB. Recent progress in the value journey: growth of ACOs and value‐based payment models in 2018. Health Affairs Blog. 2018.
- 11. Shortell SM, Colla CH, Lewis VA, Fisher E, Kessell E, Ramsay P. Accountable care organizations: the national landscape. J Health Polit Policy Law. 2015;40(4):647‐668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Colla CH, Lewis VA, Shortell SM, Fisher ES. First national survey of ACOs finds that physicians are playing strong leadership and ownership roles. Health Aff. 2014;33(6):964‐971. [DOI] [PubMed] [Google Scholar]
- 13. Peiris D, Phipps‐Taylor MC, Stachowski CA, ,et al. ACOs holding commercial contracts are larger and more efficient than noncommercial ACOs. Health Aff. 2016;35(10):1849‐1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ryan AM, Shortell SM, Ramsay PP, Casalino LP. Salary and quality compensation for physician practices participating in accountable care organizations. Ann Family Med. 2015;13(4):321‐324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mehrotra A, Epstein AM, Rosenthal MB. Do integrated medical groups provide higher‐quality medical care than individual practice association? Ann Intern Med. 2006;145(11):826‐833. [DOI] [PubMed] [Google Scholar]
- 16. Damberg CL, Silverman MR, Burgette LF, Vaiana ME, Ridgely MS. Are value‐based incentives driving behavior change to improve value? Am J Manage Care. 2019;25(2):e26‐e32. [PMC free article] [PubMed] [Google Scholar]
- 17. Goldman LE, Chu PW, Tran H, Romano MJ, Stafford RS. Federally qualified health centers and private practice performance on ambulatory care measures. Am J Prev Med. 2012;43(2):142‐149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Glied S, Zivin JG. How do doctors behave when some (but not all) of their patients are in managed care? J Health Econ. 2002;21(2):337‐353. [DOI] [PubMed] [Google Scholar]
- 19. StataCorp . Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC; 2017. [Google Scholar]
- 20. Phipps‐Taylor MC, Shortell SM. More than money: motivating physician behavior change in accountable care organizations. Milbank Q. 2016;94(4):832‐861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Rothkopf J, Brookler K, Wadhwa S, Sajovetz M. Medicaid patients seen at federally qualified health centers use hospital services less than those seen by private providers. Health Aff. 2011;30(7):1335‐1342. [DOI] [PubMed] [Google Scholar]
- 22. Lewis VA, Tierney KI, Colla CH, Shortell SM. The new frontier of strategic alliances in health care: new partnerships under accountable care organizations. Soc Sci Med. 2017;190:1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


