Abstract
The national EHDI 1-3-6 goals state that all infants should be screened for hearing loss before 1 month of age; with diagnostic testing before 3 months of age for those who do not pass screening; and early intervention (EI) services before 6 months of age for those with permanent hearing loss. This report updates previous summaries of progress on these goals by U.S. states and territories. Data are based on the Hearing Screening and Follow-up Survey (HSFS) conducted annually by the Centers for Disease Control and Prevention for the years 2006–2016. Trends were assessed using 3-year moving averages, with rates of newborns lost to follow-up or lost to documentation (LTF/D) also examined. During this period, the percentage of infants screened before one month increased from 85.1% to 95.3%, while the percentage receiving diagnostic testing before three months increased from 19.8% to 36.6%, and the percentage of infants identified with permanent hearing loss enrolled in early intervention (EI) before six months increased from 25.1% to 47.2%. Percentages of infants who ultimately received screening, diagnostic testing, and early intervention services – regardless of timing – were higher. During this period, LTF/D declined from 42.1% to 31.3% for diagnostic testing, and 39.4% to 20.3% for EI services. Diagnoses of hearing loss recorded increased from 0.9 to 1.7 per 1,000 infants screened, likely reflecting improved data.
Introduction
Congenital hearing loss (HL) affects 1.5 to 3 per 1,000 infants in the United States (Grosse et al., 2017). Children who are born deaf or hard of hearing (DHH) are at increased risk for delays in nonverbal communication skills and speech and language development (Caskey & Vohr, 2013). In particular, in the absence of universal newborn hearing screening (UNHS), many children are not diagnosed as DHH until 2 years of age or later (Elssmann, Matkin, & Sabo, 1987), at which point delays in language development are more difficult to remediate (Yoshinaga-Itano & Apuzzo, 1998; Yoshinaga-ltano, Sedey, Coulter, & Mehl, 1998). Early identification facilitated by UNHS accompanied by prompt initiation of early intervention (EI) services has been shown to directly benefit infants who are DHH by reducing deficits in their language and vocabulary (Kennedy et al., 2006; Nelson, Bougatsos, & Nygren, 2008; Vohr et al., 2011; Yoshinaga-Itano, Sedey, Wiggin, & Chung, 2017).
We used data collected through the Centers for Disease Control and Prevention (CDC) Early Hearing Detection and Intervention (EHDI) Hearing Screening and Follow-up Survey (HSFS) for the years 2006–2016 to assess progress towards meeting the national “1-3-6” EHDI goals or benchmarks. The goals, which together constitute the 1-3-6 EHDI plan, have been agreed upon by EHDI partners since the early 2000s: (a) all infants be screened for HL before 1 month of age; (b) those not passing the screening receive diagnostic testing before 3 months of age; and (c) those confirmed as DHH begin receiving appropriate early intervention services before 6 months of age (CDC, 2003; White, 2003; White, Forsman, Eichwald, & Munoz, 2010). This report updates previous summaries of HSFS data by including additional survey years and using a different analytical approach (Gaffney, Eichwald, Gaffney, Alam, & CDC, 2014; Gaffney, Green, & Gaffney, 2010; Williams, Alam, & Gaffney, 2015).
Previous studies have demonstrated that the vast majority of U.S. infants are screened for HL soon after birth. From 1996 to 2000, the estimated percentage of U.S. infants screened for hearing loss prior to hospital discharge increased from roughly 10% to roughly 50% (White, 2003). Using annual state screening estimates collected by the Directors of Speech and Hearing Programs in State Health and Welfare Agencies (DSHPSHWA), screening rates in participating states increased from 53% in 2000 to 92% in 2003 (Green, Gaffney, Devine, & Grosse, 2007). However, although almost all (> 97%) U.S. infants now undergo hearing screening soon after birth, those who fail to pass screening do not necessarily receive timely diagnostic evaluations or timely intervention services once diagnosed with permanent HL (Grosse et al., 2017). The key challenges facing EHDI programs are to increase the percentage of infants who meet the 3-month diagnostic evaluation and 6-month early intervention goals and to document that those goals are met.
This can be challenging because there are multiple, diverse reasons why the 1-3-6 goals are not met. Parents face competing demands on their time and resources as well as possess different levels of confidence in the healthcare system. Those who have low resources and/or trust levels may be less likely to keep appointments or respond as expected by providers. They may be classified as refusing services or lost to follow-up (LTF) or they may go on to simply receive services at a later age. However, greater efforts by providers or program staff may increase the likelihood of the infants in those families receiving timely services. In other cases, families may be engaged and supportive of follow-up, yet be stymied by external factors, such as reduced access to services—either due to limited availability of diagnostic or EI providers, or lack of insurance coverage. In addition, infants may meet the goals but that information is not reported by service providers to the EHDI program, resulting in loss to documentation (LTD; Mason, Gaffney, Green, & Grosse, 2008). In practice, it can be difficult or impossible to distinguish cases of LTD from LTF, and so the two are often examined together (LTF/D).
Method
In 2007, CDC began using the HSFS to collect annual, aggregate EHDI data from states based on births from the calendar year two years prior (i.e., all infants born during 2005) to ensure that they had sufficient time to complete the EHDI process. This report uses HSFS data submitted for 2006–2016 to describe the progress of EHDI programs in the 50 states and District of Columbia toward the early identification and treatment of DHH infants, including meeting the 1-3-6 goals. The number of jurisdictions submitting data varied each year due to the inability of some jurisdictions to provide empirical estimates for one or more reporting years.
To better assess progress, jurisdictions were assigned a population weight based on the total number of occurrent live births each year. Trends in meeting the three goals of EHDI were assessed by determining the percentage of infants reported as (a) screened among the total reported occurrent births; (b) having received diagnostic testing among the total reported as not passing the hearing screening; and (c) enrolled in EI among the total reported as diagnosed with permanent HL. Percentages were calculated for screening, diagnostic, and EI services, both overall, regardless of timing, and in accordance with the 1-3-6 goals.
Finally, progress in identification was determined by comparing the percentage of infants classified as LTF/D for diagnosis and EI to the prevalence of HL in each year. CDC defines LTF/D as not having received or not documented as having received follow-up diagnostic and intervention services. Infants are classified as LTF/D if the EHDI program was unable to contact their family, or if the child’s status was otherwise unknown. Cases were also classified as LTF/D if the parents/family were contacted by the EHDI program but unresponsive—choosing not to engage in the diagnostic or early intervention systems—for reasons (possibly those described previously) not conveyed to the EHDI program. To account for year-to-year fluctuations, a 3-year moving average of these weighted percentages was calculated.
Results
The percentage of infants screened by one month of age increased from an average of 85.1% during 2006–2008 to 95.3% during 2014–2016 (see Table 1). This change reflects a two-thirds reduction in the number of children not screened in the first month of life (from 14.9% to 4.7%). When the time frame is expanded to include infants not screened before one month of age, the overall percentage of infants screened remained consistently high, increasing slightly from 97.0% to 98.4%.
Table 1.
Weighted Percentages of Documented Infants Receiving Screening and Diagnostic Testing and Enrolled in Early Intervention Services, (CDC EHDIHSFS*, United States, 20062016†§
| Data Point§ | EHDI Stage & 1-3-6 Goal | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Screening¶ | Diagnostic Testing†† | Screening¶¶ | |||||||
| Total Births | Total % Screen | By 1 month ** | Not Pass Screen N | Total % Diag | By 3 months§§ | Permanent Hearing Loss N | Total % in EI | By 6 months | |
| 2007§ | 3,389,056 | 97.0% | 85.1% | 68,212 | 30.2% | 19.8% | 3,544 | 54.1% | 25.1% |
| 2008 | 3,648,433 | 97.6% | 87.4% | 65,588 | 37.3% | 24.9% | 4,185 | 63.8% | 37.8% |
| 2009 | 3,819,981 | 98.0% | 92.1% | 65,374 | 39.7% | 25.5% | 4,722 | 67.8% | 43.5% |
| 2010 | 3,919,705 | 98.2% | 94.4% | 63,841 | 44.8% | 29.3% | 5,099 | 69.1% | 48.2% |
| 2011 | 3,728,962 | 97.6% | 95.1% | 62,346 | 44.4% | 30.1% | 5,301 | 66.9% | 46.5% |
| 2012 | 3,547,267 | 97.0% | 94.6% | 60,404 | 44.8% | 30.9% | 5,435 | 65.8% | 46.7% |
| 2013 | 3,603,806 | 97.0% | 94.4% | 59,872 | 45.4% | 31.0% | 5,761 | 65.6% | 46.5% |
| 2014 | 3,732,653 | 97.8% | 95.3% | 61,931 | 52.7% | 33.0% | 5,992 | 67.4% | 47.5% |
| 2015§ | 3,859,270 | 98.4% | 95.3% | 63,718 | 58.6% | 36.6% | 6,728 | 67.9% | 47.2% |
Note. Annual data for individual jurisdictions is available at www.cdc.gov/ncbddd/hearingloss/ehdi-data.html; CDC = Center for Disease Control and Prevention; EHDI = Early Hearing Detection and Intervention; EI = Early Intervention; HSFS = Hearing Screening and Follow-up Survey
Hearing Screening and Follow-up Survey (HSFS) is an annual, voluntary, Office of Management and Budget approved data survey (OMB No. 0920–05AA) administered by CDC.
Number of HSFS state respondents by year: 45 in 2006, 45 in 2007, 48 in 2008, 47 in 2009, 49 in 2010, 49 in 2011, 51 in 2012, 51 in 2013, 51 in 2014, 49 in 2015, and 49 in 2016
This analysis does not include U.S. territories that may have responded to the survey. Data are analyzed as population weighted, three-year moving averages, with 2007 as the first data point (the average of 2006–2008 data) and 2015 as the final data point (the average of 2014–2016 data).
Percent screened and screened by 1 month of age, among total occurent live births as reported in HSFS.
For 2012 and 2013 annual data, one jurisdiction was excluded for the inability to report complete data for the number of infants screened by 1 month of age, due to temporary reporting issues with their data system. This jurisdiction was able to report all other measures.
Percent diagnostically tested and diagnostically tested by 3 months of age, among total not passing hearing screening.
For 2015 annual data, one jurisdiction was excluded for the inability to report complete data for the number of infants diagnosed by 3 months of age, due to temporary reporting issues with their data system. This jurisdiction was able to report all other measures.
Percent enrolled in EI and enrolled by 6 months of age, among total diagnosed with permanent HL.
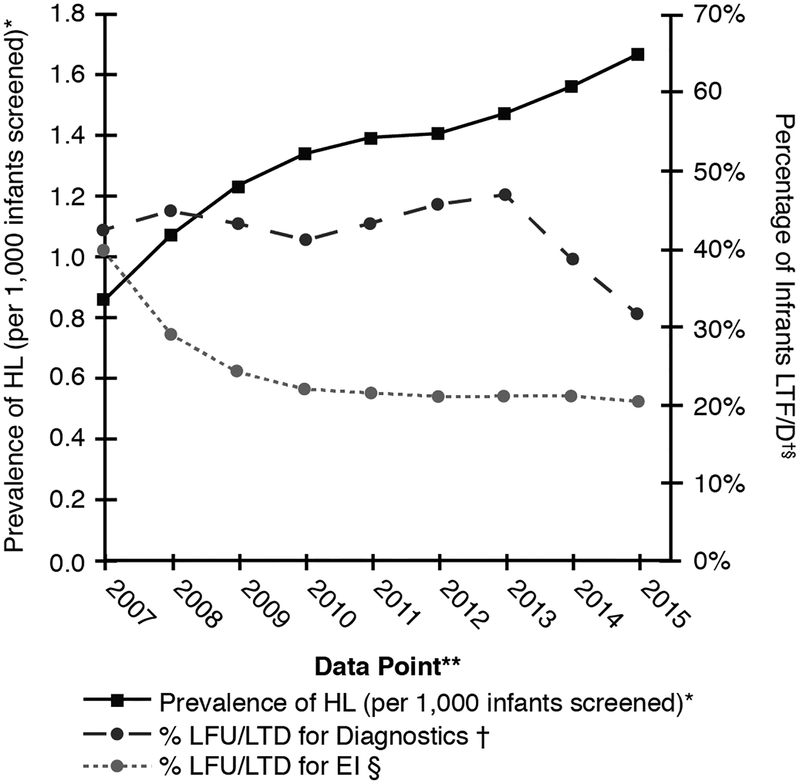
The percentage of infants who did not pass screening and who received diagnostic testing by three months of age increased from 19.8% during 2006–2008 to 36.6% during 2014–2016 (see Table 1). Including those diagnosed after the 3-month target date, the overall percentage of infants who did not pass screening but who received diagnostic testing nearly doubled—increasing from 30.2% to 58.6%. These increased numbers were also associated with reductions in the percentage of infants who were LTF/D, another indicator of progress. An average of 42.1% of infants who did not pass screening in the 2006–2008 period were classified as LTF/D for diagnostic testing, which declined to 31.3% in the 2014–2016 period (see Figure 1).
Figure 1. Prevalence of HL* and LTF/D for Diagnostic Testing† and Enrollment in Early Intervention Services§ (CDC EHDI HSFS¶, United States, 2006–2016**).
HL = Hearing loss; LTF/D = Loss to folow-up/loss to documentation; EHDI = Early Hearing Detection and Intervention; EI = Early Intervention; HSFS = Hearing Screening and Follow-up Survey.
* Prevalence of HL is calculated using the following formula: (# Diagnosed with HL/#Total Screened)* 1000.
† Percent LTF/D for Diagnostic Testing is calculated using the following formula: ((# No Diagnostic Data due to Unable to Contact + # No Diagnostic Data due to Parents/Family Contacted but Unresponsive + # No Diagnostic Data Due to Unknown Reason)/# Total Not Passing Screening) * 100.
§ Percent LTF/D for Enrollment in EI is calculated using the following formula: ((# No EI Data due to Unable to Contact + # No EI Data due to Parents/Family Contacted but Unresponsive + # No EI Data due to Unknown Reason)/# Total Diagnosed with HL) * 100.
¶ Hearing Screening and Follow-up Survey (HSFS) is an annual, voluntary, Office of Management and Budget approved data survey (OMB No. 0920–05AA) administered by CDC.
** This analysis does not include U.S. territories that may have responded to the survey. Data are analyzed as population weighted, three-year moving averages, with 2007 as the first data point (the average of 2006–2008 data) and 2015 as the final data point (the average of 2014–2016 data).
Finally, during the same timeframe, the percentage of DHH infants enrolled in EI before six months of age increased from 25.1% to 47.2%. When the time frame was expanded to include those who were enrolled in EI but did not meet the six-month goal, the percentages of DHH infants reported as enrolled in EI increased from 54.1% to 67.9% (see Table 1). The corresponding decrease in LTF/D for enrollment in EI was greater, dropping from 39.4% to 20.3% — a nearly fifty percent reduction in LTF/D (Figure 1).
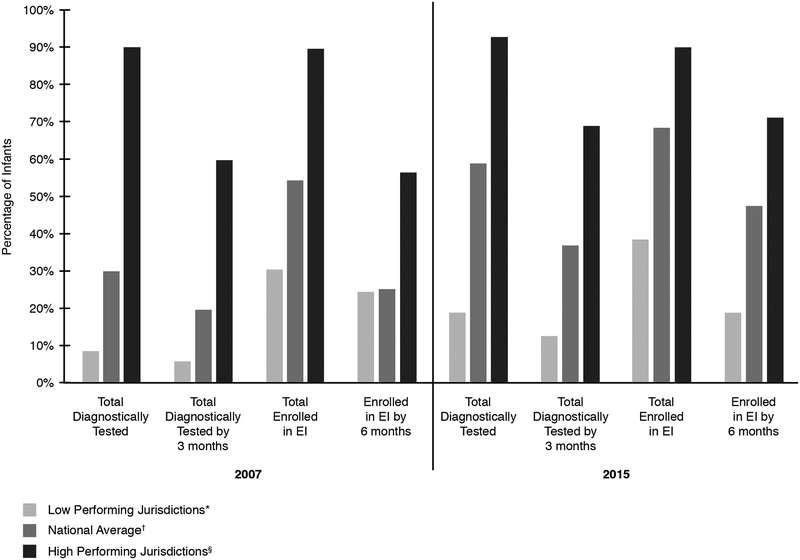
Given these changes, it was not surprising that diagnoses of infants as DHH increased from 0.9 to 1.7 per 1,000 infants screened between these data points (see Figure 1). This increase likely reflects the improvement in early identification along with decreased LTF/D for diagnosis and EI. Although there continues to be jurisdictional-level variation in early identification and enrollment in EI (see Figure 2), these overall trends reflect progress in the reporting and documentation of recommended services among EHDI programs.
Figure 2. Weighted Percentages of Infants Receiving Diagnostic Testing and Enrolled in Early Intervention Services Among the 5 Lowest Performing Jurisdictions*, the National Average†, and 5 Highest Performing Jurisdictions§, for the 2007 versus 2015 data point (CDC EHDI HSFS¶, United States, 2006–2016**).
* The average of the 5 jurisdictions with the lowest weighted three-year moving averages, for each category for the corresponding year.
† The weighted three-year moving average, for each category for the corresponding year (Table 1).
§ The average of the 5 jurisdictions with the highest weighted three-year moving averages, for each category for the corresponding year.
¶ Hearing Screening and Follow-up Survey (HSFS) is an annual, voluntary, Office of Management and Budget approved data survey (OMB No. 0920–05AA) administered by CDC.
** This analysis does not include U.S. territories that may have responded to the survey. Data are analyzed as population weighted, three-year moving averages, with 2007 as the first data point (the average of 2006–2008 data) and 2015 as the final data point (the average of 2014–2016 data).
Discussion
Substantial progress has been made since 2007, especially in the delivery and reporting by providers to EHDI programs of diagnostic testing before age 3 months and of enrollment of DHH infants in EI before age 6 months. However, the rate of overall progress has slowed since 2011 and there is variation in progress between jurisdictions. In particular, the fluctuating trend of LTF/D rates for early diagnoses and the recent plateau of LTF/D rates for EI indicate that challenges remain. For the most recent data points, 2011–2015, the percentages of infants reported as completing the three EHDI stages and meeting the 1-3-6 goals show smaller yearly improvements compared to 2007–2010 (see Table 1). There are also wide discrepancies at the jurisdictional level in early identification and enrollment in EI services, with some programs performing well above the national average, whereas others have not been as successful (see Figure 2). Reasons for some states having less success in meeting the 1-3-6 goals could potentially include lack of comprehensive follow-up strategies to ensure receipt of diagnostic and EI services; reductions in resources available to some programs; and differences in state laws, regulations, or policies. Differences in patterns over time across states could also reflect changes in reporting, data systems, reporting capacity, and best practice policies for audiologists and EI providers.
The relatively low absolute percentages of children documented as receiving timely diagnosis and initiation of EI highlight the need for continued efforts to ensure all DHH infants are identified early and able to reach their full potential. The observed variability in progress by goal and across states can be used to focus additional efforts to improve the delivery and documentation of essential EHDI follow-up diagnostic and EI services and to reduce variability in access to needed services (Liu, Farrell, MacNeil, Stone, & Barfield, 2008).
Calculations using population-weighted, 3-year moving averages allow for a more standardized comparison of data that has varying respondents between years. Nonetheless, the findings in this report are subject to at least four limitations. First, the use of moving averages minimizes fluctuations associated with random variation, which can indicate no overall trend despite large differences between adjacent years. Second, some jurisdictions did not report data for one or more years. Third, the HSFS is a voluntary survey and although there are standardized data definitions, the data reported are subject to different interpretations. For example, the question of what constitutes an “in process” diagnostic evaluation was clarified and refined to improve consistency. Fourth, incomplete reporting of services could understate the receipt of services and overstate rates of LTF/D.
Despite smaller improvements at the national level in recent years, some high performing state EHDI programs have shown continued progress through implementation of innovative strategies. For example, the Kentucky and Louisiana EHDI programs have reported that scheduling follow-up appointments at the time a hearing screening is not passed prior to hospital discharge is associated with increased receipt of follow-up services, and the programs encourage and track this practice (Lester, 2017; Ye et al., 2014). Louisiana has also created a system for the routine linkage of Medicaid data, which is used by the EHDI program to verify initiation of follow-up and improve communication between EHDI coordinators and clinical providers (Tran et al., 2016). However, relatively few children can be tracked through that linkage. During 2012–2013, of 682 infants classified as LTF/D in Louisiana, 57 had Medicaid records, and 38 of those had records that could be retrieved and matched. Of those 38 infants, 25 were reclassified as having received follow-up services (Tran et al., 2016).
The EHDI program in Georgia has shown that texting parents after an unsuccessful attempt to contact them by telephone can improve families’ response to a reminder of audiological follow-up (Hermanns, Currie, LaVell, & Lo, 2016). The program recommends incorporating texting into the follow-up protocol for all EHDI programs. Other states have focused efforts on encouraging pediatric audiologists to report diagnostic results and provide technical assistance with electronic reporting of diagnostic results.
In 2011, Wisconsin started providing varying levels of assistance to families, hospitals, and providers to reduce LTF/D rates (Wisconsin Sound Beginnings, 2016). These changes included in-home and in-community, infant-specific outreach to families reluctant to or unable to access follow-up services, and training and technical support to health care systems. These state-implemented strategies involved a team approach including families, state EHDI staff, and providers. The various initiatives helped further improve the receipt of follow-up services. Among 1,819 infants who did not pass initial screening in Wisconsin in 2015, 138 never received further services, mostly because parents refused (n = 38) or were unresponsive (n = 49); just 9 infants were LTF/D. The primary remaining challenge in Wisconsin is assuring timely intervention. Of 133 infants diagnosed with permanent hearing loss, 122 were referred to EI, but just 44 were enrolled by 6 months of age.
One strategy that might help reduce LTF/D is to more closely integrate EHDI activities into other newborn health and development services. For example, in 2012 to 2014, Ohio tested an intervention that involved a partnership between EHDI and WIC, in which WIC infants who did not pass initial newborn hearing screening received an outpatient rescreen at their WIC office (Hunter et al., 2016). Combining co-location of services with timely scheduling and contact with families reduced LTF/D rates from 33.3% to 9.6%, while the mean age of diagnosis dropped from 68 days to 34.8 days for children in the study.
In addition to LTF that reflects children not receiving a diagnostic evaluation or services, LTD can occur if providers fail to report information to their state EHDI program. For example, 13.6% of a national sample of 1,024 pediatric audiology facilities indicated that they reported less than two-thirds of their results to their state EHDI program—with 8.6% reporting none of their results (Chung, Beauchaine, Grimes, et al., 2017). Furthermore, among facilities that do report data, 14.5% indicated that they did not report normal hearing results. This gap in reporting and documentation will inevitably impact overall LTF/D rates and lead to underestimating true EHDI program coverage and impact.
Beyond state-level strategies designed to reduce LTF/D, at the national level CDC, the National Center for Hearing Assessment and Management (NCHAM), the American Speech-Language-Hearing Association (ASHA), the American Academy of Audiology (AAA), and other partners collaborated on the creation of EHDI Pediatric Audiology Links to Services (EHDI-PALS). EHDI-PALS is a web-based, geocoded national directory of facilities that offer pediatric audiology services to children who are younger than five years of age (Chung, Beauchaine, Hoffman, et al., 2017). EHDI-PALS is designed to help parents find pediatric audiologists with the training and tools necessary to provide evaluation services for young children, and who also report data to state EHDI programs. Parents can enter the age and other relevant information about their child and, based on their zip code, be given a highly detailed list of facilities in their area or region.
Also at the national level, the National Institute for Children’s Health Quality (NICHQ), with support from the Health Resources and Services Administration (HRSA), conducted a Learning Collaborative from 2010 to 2013 to seek out ways to reduce LTF/D. In 2016 it published an Action Kit for audiologists that summarized lessons from the Collaborative (NICHQ, 2016). For example, NICHQ emphasizes the importance of communication with families prior to the first diagnostic appointment regarding what to expect and how to prepare their infant as well as the logistics of getting to the appointment to reduce the frequency of “no-show” appointments. EHDI programs can partner with peer support organizations such as Hands & Voices to facilitate the communication process and hopefully reduce LTF/D at the diagnostic evaluation stage, although we are not aware of formal evaluations.
Conclusion
Meeting the 1-3-6 EHDI goals helps DHH infants improve vocabulary outcomes and minimizes developmental delays that can last a lifetime. Although screening by 1 month of age is necessary and is routinely occurring, it is not sufficient to improve outcomes without timely diagnosis and enrollment in EI services. Although progress in the receipt of diagnostic testing and EI has been made, as illustrated in this report, further progress will require strengthening current practices. Continued efforts in these areas will help ensure all infants who are DHH are identified early while supporting improved developmental outcomes.
Acknowledgements:
This report is based on data reported by jurisdictional EHDI programs in U.S. states and the District of Columbia.
Acronyms:
- AA
American Academy of Audiology
- ASHA
American Speech-Language-Hearing Association
- CDC
Centers for Disease Control and Prevention
- DHH
deaf or hard of hearing
- EI
early intervention
- DSHPSHWA
Directors of Speech and Hearing Programs in State Health and Welfare Agencies
- EHDI
Early Hearing Detection and Intervention
- EHDI-PALS
EHDI Pediatric Audiology Links to Services
- HL
hearing loss
- HRSA
Health Resources and Services Administration
- HSFS
Hearing Screening and Follow-up Survey
- LTF/D
lost to follow-up or lost to documentation
- NCHAM
National Center for Hearing Assessment and Management
- NICHQ
National Institute for Children’s Health Quality
- UNHS
universal newborn hearing screening
References
- Caskey M, & Vohr B (2013). Assessing language and language environment of high-risk infants and children: A new approach. Acta Paediatrics, 102(5), 451–461. doi: 10.1111/apa.12195 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2003). Infants tested for hearing loss-United States, 1999–2001. MMWR. Morbidity and Mortality Weekly Report, 52(41), 981–984. [PubMed] [Google Scholar]
- Chung W, Beauchaine KL, Grimes A, O’Hollearn T, Mason C, & Ringwalt S (2017). Reporting newborn audiologic results to state EHDI programs. Ear and Hearing, 38(5), 638–642. doi: 10.1097/AUD.0000000000000443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chung W, Beauchaine KL, Hoffman J, Coverstone KR, Oyler A, & Mason C (2017). Early hearing detection and intervention-Pediatric audiology links to services EHDI-PALS: Building a national facility database. Ear and Hearing, 38(4), e227–e231. doi: 10.1097/AUD.0000000000000426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elssmann S, Matkin N, & Sabo M (1987). Early identification of congenital sensorineural hearing impairment. The Hearing Journal, 40(9), 13–17. [Google Scholar]
- Gaffney M, Eichwald J, Gaffney C, Alam S, & Centers for Disease Control and Prevention. (2014). Early hearing detection and intervention among infants: Hearing screening and follow-up survey, United States, 2005–2006 and 2009–2010.Morbidity and Mortality Weekly Report, Supplement, 63(2), 20–26. [PubMed] [Google Scholar]
- Gaffney M, Green DR, & Gaffney C (2010). Newborn hearing screening and follow-up: Are children receiving recommended services? Public Health Report, 125(2), 199–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green DR, Gaffney M, Devine O, & Grosse SD (2007). Determining the effect of newborn hearing screening legislation: An analysis of state hearing screening rates. Public Health Reports, 122(2), 198–205. doi: 10.1177/003335490712200209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grosse SD, Riehle-Colarusso T, Gaffney M, Mason CA, Shapira SK, Sontag MK, … Iskander J (2017). CDC grand rounds: Newborn screening for hearing loss and critical congenital heart disease. MMWR. Morbidity and Mortality Weekly Report, 66(33), 888–890. doi: 10.15585/mmwr.mm6633a4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermanns K, Currie M, LaVell C, & Lo M (2016). Implementing texting into your follow up protocol: Georgia’s experience. Paper presented at the 15th Annual Early Hearing Detection & Intervention Meeting, San Diego, CA https://ehdimeeting.org/archive/2016/Schedule/griddetails.cfm?aid=1912&day=TUESDAY [Google Scholar]
- Hunter LL, Meinzen-Derr J, Wiley S, Horvath CL, Kothari R, & Wexelblatt S (2016). Influence of the WIC program on loss to follow-up for newborn hearing screening. Pediatrics, 738(1). doi: 10.1542/peds.2015-4301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kennedy CR, McCann DC, Campbell MJ, Law CM, Mullee M, Petrou S, … Stevenson J (2006). Language ability after early detection of permanent childhood hearing impairment. New England Journal of Medicine, 354(20), 2131–2141. doi: 10.1056/NEJMoa054915 [DOI] [PubMed] [Google Scholar]
- Lester C (2017). Impact of Hospital Scheduling on Follow-up Appointments After Failed Newborn Hearing Screening. Paper presented at the 16th Annual Early Hearing Detection & Intervention Meeting, Atlanta, GA https://ehdimeeting.org/archive/2017/Schedule/griddetails.cfm?aid=5623&day=MONDAY [Google Scholar]
- Liu CL, Farrell J, MacNeil JR, Stone S, & Barfield W (2008). Evaluating loss to follow-up in newborn hearing screening in Massachusetts. Pediatrics, 121(2), e335–343. doi: 10.1542/peds.2006-3540 [DOI] [PubMed] [Google Scholar]
- Mason CA, Gaffney M, Green DR, & Grosse SD (2008). Measures of follow-up in early hearing detection and intervention programs: A need for standardization. American Journal of Audiology, 77(1), 60–67. doi: 10.1044/1059-0889(2008/007) [DOI] [PubMed] [Google Scholar]
- Nelson HD, Bougatsos C, & Nygren P (2008). Universal newborn hearing screening: Systematic review to update the 2001 US Preventive Services Task Force Recommendation. Pediatrics, 722(1), e266–276. doi: 10.1542/peds.2007-1422 [DOI] [PubMed] [Google Scholar]
- NICHQ. (2016). Improving follow-up after newborn hearing screening: An action kit on improving follow-up care for newborns. Retrieved from https://www.nichq.org/resource/improving-follow-afternewborn-hearing-screening
- Tran T, Wang H-Y, Webb J, Smith MJ, Soto P, Ibieta T, … Berry S (2016). Using Medicaid data to improve newborn hearing screening follow-up reporting: Results from a pilot study. Journal of Healthcare Communications, 1(2), 13. [Google Scholar]
- Vohr B, Jodoin-Krauzyk J, Tucker R, Topol D, Johnson MJ, Ahlgren M, & Pierre LS (2011). Expressive vocabulary of children with hearing loss in the first 2 years of life: Impact of early intervention. Journal of Perinatology, 31(4), 274–280. doi: 10.1038/jp.2010.110 [DOI] [PubMed] [Google Scholar]
- White KR (2003). The current status of EHDI programs in the United States. Mental Retardation and Developmental Disabilities Research Reviews, 9(2), 79–88. doi: 10.1002/mrdd.10063 [DOI] [PubMed] [Google Scholar]
- White KR, Forsman I, Eichwald J, & Munoz K (2010). The evolution of early hearing detection and intervention programs in the United States. Seminars in Perinatology, 34(2), 170–179. doi: 10.1053/j.semperi.2009.12.009 [DOI] [PubMed] [Google Scholar]
- Williams TR, Alam S, & Gaffney M (2015). Progress in identifying infants with hearing loss: United States, 2006–2012. MMWR Morbidity and Mortality Weekly Report, 64(13), 351–356. [PMC free article] [PubMed] [Google Scholar]
- Wisconsin Sound Beginnings Early Hearing Detection and Intervention. (2016). Annual Report 2015. Retrieved from http://www.dhs.wisconsin.gov/publications/p00606-15.pdf
- Ye X, Tran T, Smith MJ, Webb J, Mohren T, & Peat M (2014). Improvement in loss to follow-up of newborn hearing screening: A lesson from Louisiana Early Hearing Detection and Intervention Program. Online journal of public health informatics, 6(1). [Google Scholar]
- Yoshinaga-Itano C, & Apuzzo ML (1998). Identification of hearing loss after age 18 months is not early enough. American Annals of the Deaf, 143(5), 380–387. [DOI] [PubMed] [Google Scholar]
- Yoshinaga-Itano C, Sedey AL, Coulter DK, & Mehl AL (1998). Language of early- and later-identified children with hearing loss. Pediatrics, 102(5), 1161–1171. [DOI] [PubMed] [Google Scholar]
- Yoshinaga-Itano C, Sedey AL, Wiggin M, & Chung W (2017). Early hearing detection and vocabulary of children with hearing loss. Pediatrics, 140(2). doi: 10.1542/peds.2016-2964 [DOI] [PMC free article] [PubMed] [Google Scholar]