Abstract
Filipino Americans have high rates of cardiovascular diseases (CVD). This study explored the dietary behaviors, a modifiable risk factor, of Filipinos with CVD. Filipinos with CVD were recruited and trained to do Photovoice. Participants took photos to depict their “food experience,” defined as their daily dietary activities. Participants then shared their photos during focus groups. Focus group transcripts were analyzed using an iterative, grounded theory approach. Among 38 Filipino participants, the mean age was 70 years old and all were foreign-born. Major themes included efforts to retain connection to Filipino culture through food, and dietary habits shaped by cultural health beliefs. Many believed that traditional dietary practices increased CVD risk. Receiving a CVD diagnosis and clinician advice changed their dietary behaviors. Household members, the physical environment, and economic constraints also influenced dietary behaviors. Photovoice is feasible among older Filipinos and may enhance understanding of drivers of dietary behaviors.
Keywords: Filipino Americans, Photovoice, Dietary behaviors, Cardiovascular disease, Community-based participatory research
INTRODUCTION
From 2000-2010, Asian Americans were the fastest growing U.S. racial group, and Filipino Americans were the second largest Asian subgroup (Hoeffel, Rastogi, Kim, & Shahid, 2012). Filipino Americans have high rates of cardiovascular disease (CVD) and associated risk factors such as obesity, diabetes and hypertension. Using the World Health Organization (WHO) Asian body mass index (BMI) categories, the prevalence of overweight/obesity in Filipinos is the highest among Asian subgroups, exceeds that of non-Hispanic Whites (NHW), and similar to that of African Americans and Latinos (Jih et al., 2014). Within a health maintenance organization in northern California, Filipinos had the second highest prevalence (16.1%) and the fourth highest incidence (14.7 per 1,000 person-years) of diabetes of all racial/ethnic groups (Karter et al., 2013). Among Asian Americans, Filipinos have the highest prevalence of hypertension (HTN) which is estimated to be at least 27% (Barnes, Adams, & Powell-Griner, 2008). The adjusted odds of coronary heart disease in Filipino men and women is 1.47 (95% CI 1.05-2.06) and 1.66 (95% CI 1.13-2.43) times as high as NHWs respectively (Holland, Wong, Lauderdale, & Palaniappan, 2011). Compared to NHW women, Filipino women have a higher risk for stroke (adjusted odds ratio 2.02, 95% CI 1.22-3.34) (Holland, Wong, Lauderdale, & Palaniappan, 2011).
Diet is key to the prevention and management of CVD and may be modifiable through patient-centered interventions. Cultural beliefs and values affect both dietary practices and perceptions of how diet relates to CVD (Cardiovascular Risk in the Filipino Community: Formative Research from Daly City and San Francisco, California, March 2003; Nordström, Coff, Jönsson, Nordenfelt, & Görman, 2013). Studies examining Filipino American dietary behaviors have focused on quantitative recall of food intake and preferences (dela Cruz, Lao, & Heinlein, 2013; Johnson-Kozlow et al., 2011). Common traditional dietary practices among Filipino Americans include consumption of steamed white rice at all meals; protein in the form of beef, chicken, pork, fish, shrimp and processed meat; mixed protein and vegetable dishes in broth or stir-fry that are frequently highly seasoned; and fresh fruits including bananas, guavas, and mangoes (dela Cruz, Lao, & Heinlein, 2013; Johnson-Kozlow et al., 2011). The quantitative recall of food intake and preferences may not fully explore the contextual factors affecting dietary habits in this priority population.
To develop interventions to reduce CVD among Filipino Americans, there is a need to understand psychosocial and cultural influences on dietary choices in this population. An approach is the use of Photovoice, a qualitative methodology that involves photo-taking by participants to show their experiences relevant to the health issue followed by dialogue, reflection and action around the issue through sharing of photos (Catalani & Minkler, 2010; Hergenrather, Rhodes, Cowan, Bardhoshi, & Pula, 2009; C. Wang & Burris, 1997). Photovoice has been used by minorities to identify and share experiences that may be difficult to communicate (Catalani & Minkler, 2010; Fitzpatrick et al., 2012; Hergenrather et al., 2009; C. Wang & Burris, 1997; C. C. Wang, 1999). Photovoice has empowered communities, improved health programs, and increased self-coping behaviors in adults with mental illness (Catalani & Minkler, 2010; Russinova et al., 2014; C. C. Wang, 1999). The objective of this study was to elicit attitudes and beliefs about dietary behaviors among Filipino Americans with CVD using Photovoice-guided focus groups and applying a socio-ecological model of health (Dahlgren, 1992). The socio-ecological model is a framework to examine the multilevel contextual factors that influence dietary behaviors, ranging from the community- and household-level characteristics (e.g. culture, household preferences) and physical environment (e.g. availability of kitchen) to interpersonal- and individual-level factors (e.g. interactions with healthcare providers, personal beliefs and values) (Dahlgren, 1992).
METHODS
Study design
This community-based observational study uses Photovoice-guided focus groups to explore attitudes and beliefs of dietary behaviors of Filipino Americans in San Francisco, California. The study period was February-June 2014. The study was conducted in collaboration with the Veterans Equity Center, which was established to serve Filipino World War II veterans and now has expanded services for low-income, seniors, immigrants, and adults with disabilities through case management and support services. The University of California San Francisco Institutional Review Board approved the study protocol.
Recruitment.
Bilingual staff members from the Veterans Equity Center recruited participants through word-of-mouth and flyers posted at the community center and community locations such as churches and stores. Inclusion criteria were: a) self-identification as Filipino or Filipino American; b) age 55-84; and c) self-report of having CVD or risk factors defined as coronary artery disease, myocardial infarction, heart failure, angina, hypertension, hyperlipidemia, diabetes, and stroke or transient ischemic attack. Potential participants were screened for eligibility by phone or in person at the community organization using a brief structured recruitment script that included an inclusion criteria checklist. At the end of eligibility screening, eligible participants were invited to attend an orientation session.
Study Procedures.
Eligible participants attended an orientation session held at the community organization to complete a written survey in English/Tagalog and then receive instruction on Photovoice, which involved using a disposable camera to depict their “food experience.” Food experience was defined as daily dietary choices and activities such as mealtime experiences, grocery shopping and food preparation. Participants were asked to take 2-3 photos daily in a 10-day period. They returned the used camera 1 week prior to the focus group so that the film could be developed prior to the group discussion (Figure 1).
Figure 1.
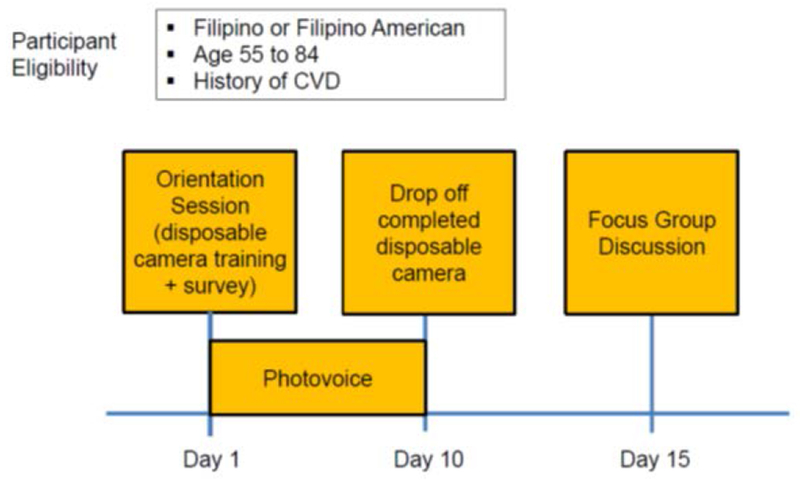
Study design and timeline.
Measures.
The written survey included questions about CVD and medical history, socio-demographics, and eating habits and opinions, including the 6-item U.S. Adult Food Security Survey Module (Bickel, Nord, Price, Hamilton, & Cook, 2000) to identify food insecurity defined as the uncertain or limited access to nutritionally adequate and safe foods. Participants self-reported CVD history (yes/no) and height and weight to calculate BMI. Socio-demographic variables assessed included age, sex, birthplace (Philippines versus U.S. versus other), years lived in the U.S., English proficiency according to the Census-limited English proficiency (LEP) question on a 4 point scale: “Very well,” “Well, “Not well,” and “Not at all” (Karliner, Napoles-Springer, Schillinger, Bibbins-Domingo, & Perez-Stable, 2008), highest educational attainment (< high school graduation versus > high school diploma versus other (e.g. vocational), marital status (married versus other), employment status (employed versus not employed) and annual household income (<$5000, $5000-$10,000, $10,000-$20,000, $20,000-$30,000, >$30,000 versus don’t know/no response). Self-rated health status was assessed by a single item that asked, “how would you rate your current health in general?” with response options of “excellent,” “very good,” “good,” “fair,” or “poor” (Idler & Benyamini, 1997). We assessed frequency of shopping at Filipino grocery stores using a 5 point scale: “2-3 times/week,” “once weekly,” “once or twice a month,” less than once a month,” and “never.” We assessed self-reported consumption of Filipino food at home and at restaurants using a 5 point scale: “always Filipino food,” “mostly Filipino food, some non-Filipino food,” “both Filipino and non-Filipino food,” “mostly non-Filipino food, some Filipino food,” and “always non-Filipino food.”
The English version of the survey had a readability level of 6th grade according to the Flesch-Kincaid Grade Level (Badarudeen & Sabharwal, 2010). Bilingual community organization staff members and research assistants were available to assist participants who had difficulty completing the survey themselves. The survey was translated from English to Tagalog by a professional bilingual English/Tagalog translator. Initial Tagalog survey translations were reviewed by bilingual team members and differences in translations were reconciled through consensus. Prior to study use, the English and Tagalog versions of the survey was pilot tested with community members receiving services at the community organization; feedback from the pilot testing was incorporated in the final English and Tagalog version of the survey.
Focus Groups.
A total of 6 audio-recorded focus groups, conducted primarily in Tagalog and each 1.5 hours long, were completed by an experienced bilingual (English/Tagalog) facilitator with the aid of at least 1 bilingual research assistant. All focus groups were held in a private room at the community organization. Each focus group ranged from 4-8 participants. To explore patterns in household and gender dynamics, 2 focus groups were composed of all female participants, 2 with all male participants, 1 with husband/wife pairs, and 1 with both female and male participants. We applied the principles of Photovoice, a community-based participatory research (CBPR) methodology to guide the discussion as participants shared photos representing their “food experience.” At the start of each discussion, each participant received a copy of their photos and were asked to select up to 5 photos that best illustrated their “food experience.” Each participant had an opportunity to share and show others at least 1 photo and to describe their personal narrative of the photo. Other participants were offered an opportunity to add any thoughts or comments after each participant finished sharing a photo. Using the ecological framework, the facilitator probed on potential multilevel influences on dietary behaviors including community, household, physical environment, interpersonal, and individual beliefs and attitudes. At the end of the focus group, participants were allowed to keep their photos. Participants received $25 after returning the used camera and $40 after the focus group for a total incentive of $65.
Analysis.
Focus groups were transcribed verbatim and translated from Tagalog to English as needed. Bilingual research team members verified translated transcripts against audio-recordings. English transcripts were analyzed using the qualitative data analysis software, Atlas.ti version 7. We used an iterative, grounded theory approach to analyze the transcripts. Two coders independently reviewed all transcripts and assigned a code that represented categories and subcategories of the socio-ecological framework to every identifiable segment of continuous speech or verbal utterance. Coders were trained through sequential cycles of independent coding, discussion and reconciliation for two focus group transcripts. Through this iterative process, we developed a detailed codebook and their definitions. Preliminary results were presented in a community forum attended by study participants and community organization staff. Feedback from this community forum and from academic-community research team meetings that included the coders were discussed and incorporated in the iterative refinement of the codebook. All transcripts were then re-reviewed using the final codebook. We did not conduct formal assessment of inter-rater reliability. Survey data was entered and analyzed in the Research Electronic Data Capture (REDCap), using the built-in function to generate descriptive data reports of our study population. The academic-community research team participated in several meetings to discuss themes, reach consensus and identify photos to illustrate key themes presented in this manuscript. Separate, structured content analysis of photos was not conducted.
RESULTS
A total of 38 participants were enrolled and 35 completed the study; 3 dropped out before the focus groups. Inadvertently, one participant, who did not have a personal history of CVD was included in a focus group, and could not be dropped from the analyses since we could not identify this person in the focus group transcript. Mean age of participants was 69.6 years old and 52.6% were female (Table 1). All were immigrants, residing in the U.S., an average of 16.8 years. More than half of participants reported LEP. Almost two-thirds had at least a high school diploma and about 75% of the participants reported an annual household income of less than $30,000. Mean self-reported BMI was 25.3 kg/m2 which is within the overweight range as defined by the WHO Asian BMI cut-points (Jih et al., 2014; World Health Organization, 2004). Hypertension (89.5%), hyperlipidemia (60.5%), and heart disease (31.6%) were the most prevalent self-reported CVDs. One-fourth of participants reported a history of diabetes. Half were food insecure.
Table 1.
Sociodemographic and Health Characteristics of Filipino American Participants (n=38)
| Female, % | 52.6 |
| Age, mean (years) ± SD | 69.6 ± 8.3 |
| Born in the Philippines, % | 100.0 |
| Years in the US, mean (years) ± SD | 16.8 ± 11.4 |
| Married, % | 60.5 |
| Limited English proficient, % | 52.6 |
| Tagalog spoken at home, % | 100.0 |
| Currently employed, % | 36.8 |
| Education, % | |
| Less than high school diploma or equivalent | 29.0 |
| Greater than equal to high school diploma or equivalent | 65.8 |
| Other | 5.3 |
| Income, % | |
| Less than $5000 | 23.7 |
| $5000 to less than $10,000 | 21.1 |
| 10,000 to less than $20,000 | 15.8 |
| $20,000 to less than $30,000 | 2.6 |
| Greater than $30,000 | 10.5 |
| Don’t know or no response | 26.4 |
| Have regular healthcare provider, % | 86.8 |
| Health status, % | |
| Excellent | 13.2 |
| Very good | 18.4 |
| Good | 31.6 |
| Fair/Poor | 34.2 |
| No response | 2.6 |
| Body mass index (BMI), mean (kg/m2) ± SD | 25.3 ± 3.5 |
| Self-reported cardiovascular disease*, % | |
| Congestive heart failure | 26.3 |
| Diabetes | 26.3 |
| Heart disease | 31.6 |
| Stroke | 18.4 |
| Hypertension | 89.5 |
| Hyperlipidemia | 60.5 |
| More than one cardiovascular disease | 68.4 |
| Food insecure, % | 50.0 |
| Types of food eaten at home, % | |
| Always Filipino food | 31.6 |
| Mostly Filipino food, some non-Filipino food | 34.2 |
| Both Filipino and non-Filipino food | 23.8 |
| Mostly non-Filipino food, some Filipino food | 7.9 |
| Always non-Filipino food | 0 |
| Frequency of shopping at Filipino grocery stores or markets, % | |
| 2-3 times/week | 26.3 |
| Once weekly | 36.8 |
| Once or twice a month | 18.4 |
| Less than once a month | 10.5 |
| Never | 0 |
| Types of food eaten at restaurants, % | |
| Always Filipino food | 28.9 |
| Mostly Filipino food, some non-Filipino food | 23.7 |
| Both Filipino and non-Filipino food | 31.6 |
| Mostly non-Filipino food, some Filipino food | 2.6 |
| Always non-Filipino food | 5.3 |
SD = standard deviation
Participants may report more than one category
Six themes influencing dietary behaviors, organized by the socio-ecological framework, were identified (Table 2). The themes are presented from the macro- to micro-level factors according to the framework: community-level, household-level, physical environment, interpersonal-level and individual-level factors. The six identified themes were: 1) importance of traditional foods to Filipino cultural identify (community-level); 2) cultural influences on health beliefs (community level); 3) balancing household members’ dietary preferences that conflict with a heart healthy diet (household-level); 4) constraints of living environment and financial resources (physical environment); 5) physician influence on changes in CVD health behaviors (interpersonal-level); and 6) beliefs that traditional dietary practices increase risk of CVD (individual-level). We found common themes across all focus groups and did not identify differences by gender. Thus, the findings are presented in aggregate. The academic-community research team identified representative participant quotes and/or photographs illustrating each theme that are presented in Table 2.
Table 2.
Multilevel factors influencing dietary behaviors among older Filipino American participants with cardiovascular disease
| Theme | Participant Quotes and/or Photographs Illustrating Theme | |
|---|---|---|
| Community-level Factors: Socio-Cultural Context | ||
|
Importance of traditional foods to Filipino cultural identity Participants expressed a desire maintain their connection with Filipino culture including modifying rather than abandoning Filipino recipes. |
 Male participant with his photo of Manila Oriental Market: “I shop, at the Filipino Market because we are all Pinoy (Filipino). We are loyal to our food.” |
 Female participant presenting her photo from the farmer’s market: “I also eat our food crops. But the ones they have here, we don’t eat them in the Philippines. But I got acquainted with them and now I eat them.” |
|
Cultural influences on health beliefs Cultural perspectives shaped health beliefs about food. |
 Male participant speaking about why this photograph is significant to him: “Because this food is good for the body. First of all, if fish is what we would eat, it’s easy to dissolve. Even a long time ago, my grandfather had long life because they always ate fish.” |
|
| Household-level Factors | ||
|
Balancing household members’ dietary preferences that conflict with a heart healthy diet Participants trying to adhere to a heart healthy diet described tension in resisting foods preferred by household members |
A male participant speaking of eating with his housemates who prefer a diet with more meat: “In a day, I only try a little of what they eat, just a bit.” A female participant speaking of influences to food preparation in her household: “When it’s like that I have in mind, I have to buy what he wants. I would say that for me, I’ll just have fruits, my apples, carrots, beets, whatever fruits are at home. I can eat them right away. As for him, when he sees something on the table, ay, you’ll see, his brows meet.” |
|
| Physical Environment | ||
|
Constraints of living environment and financial resources Meals prepared by participants were influenced by financial constraints and housing environment and shaped by food distribution assistance. |
 A female participant speaking of the corn, cucumbers, apple and broccoli in this photo that is a typical meal: “This is usually what we eat from the food bank. Whatever comes around, that’s what we do.” The fish is purchased separately and often is not affordable. |
 A male participant presenting this photo depicting his breakfast: “So this is what I usually eat in the morning ever since I went solo in 2003…Then I don’t even think of cooking in the morning. There is no kitchen where I live, only a microwave, refrigerator, no stove. It’s actually forbidden. Before, it’s okay until you’re caught, you’ll be given a warning. When you get caught again, you’re out of the house. So this is what seems to be my new habit now.” |
| Interpersonal-level Factors: Healthcare Interactions | ||
|
Physician influence on changes in CVD health behaviors Participants often cited their physician’s advice in modifying their dietary practices. |
 A female participant’s photograph of meal time in her household showing several traditional Filipino dishes (likely chicken tinola in the orange bowl, ginisang ampalay which is sautéed bitter melon in the farther green bowl, and pinakbet which is mixed vegetables steamed in fish sauce) enjoyed family style with a portion of rice for one individual. |
 A male participant sharing a photo he has selected: “Rice is a staple food in the Philippines. Although rice is very important, I don’t eat rice as often. Because it is something with carbohydrates. Not every day and when I do eat, only one cup. I don’t want too much of it because the doctor said it is this with carbohydrates. I know that I have diabetes and high blood pressure…that’s really bad. I’m recuperating but then I eat not too much rice.” |
| Individual-level Beliefs and Attitudes | ||
|
Beliefs that traditional dietary practices increase risk of CVD Participants often attributed their health problems to the Filipino diet and eating habits. |
A female participant speaking of having a stroke and learning she had diabetes: “Yes, I cut down on everything. Almost everything is forbidden. Rice is given to you in a cup only… Then salt. I cut back on that too. Plus food that taste good. Sweets, dessert. We would go to parties, they have custard. I just look at it… I miss it, food like that.” A male participant speaking about his diet after receiving hypertension diagnosis: “Potato chips, corn chips, Garlic Boy, pork crackling… I really had no control then. So, when I had high blood [pressure] I removed them slowly, but it was hard, especially when we had… parties. We ate, I got tempted to eat shrimp paste. There was kare-kare (oxtail in peanut sauce) there. Isn’t that delicious? Yes.” Female participant speaking of dietary behaviors and her diagnosis of hypertension: “Number one is salty. I had a sister-in-law, she was always being rushed to the hospital because her heart is floating on water. So they said not to eat salty food. That is what she died of. She couldn’t stop herself from eating salty food. She uses fish sauce, soy sauce.” |
|
Community-level factors: socio-cultural context
Importance of traditional foods to Filipino cultural identity.
Participants shared a desire to maintain a connection with Filipino culture and identity through food. Most participants indicated a preference for Filipino foods, a finding that was confirmed by the survey that found over 80% of participants shopped at Filipino grocery stores and ate Filipino foods at restaurants and at home. Participants sought to hold on to this cultural connection by modifying rather than abandoning Filipino recipes. One example was the modification of traditional Filipino recipes to incorporate beets, a vegetable common in the U.S. but not in the Philippines.
Cultural influences on health beliefs.
Health beliefs regarding food were shaped by participants’ cultural experiences as Filipino Americans. Cultural health beliefs included the use of herbal medications such as sambong (ngai camphor) and banaba (crepe myrtle) and the perception that some foods such as certain vegetables or fish provided health benefits. A male participant shared his preference for eating fish based on a culturally based belief and experience and his narrative and photo is included in Table 2. Word of mouth and peer influence also contributed to health beliefs and dietary choices, with participants often citing “they say/said” or sabi nila in Tagalog, a common expression that is used to explain the status quo or social norm.
Household-level factors
Balancing household members’ dietary preferences that conflict with a heart healthy diet.
Participants described the influence of household members (e.g. spouses, roommates, children or grandchildren) on their eating behaviors. Food preferences of household members greatly influenced the foods that were purchased and prepared for the household. Since meals were often enjoyed family style, participants trying to adhere to a heart healthy diet described the tension in resisting foods preferred by household members. For example, one female participant stated “my husband is fond of tocino (cured meat), sausages, and pork. And so sometimes I am also tempted to eat them. He doesn’t like it, when what is on the table are vegetables, he will say ‘I don’t want that’.” Some participants adapted to different household dietary preferences by preparing separate meals or having soy sauce on the side for household members. An emerging theme was that both men and women engaged in grocery shopping, meal planning and cooking, a departure from traditional gender roles.
Physical environment
Constraints of living environment and financial resources.
Participants living in single room occupancies spoke of challenges with cooking freshly prepared meals given a lack of full kitchen facilities and concerns for jeopardizing their housing situation if they chose to cook meals with small kitchen appliances that were not allowed in their rooms. Meals were also influenced by financial constraints and food distribution assistance. Half of the participants were food insecure. Many reported obtaining food weekly from food pantries and then supplementing that with food purchases, e.g., fish, which is a key part of the Filipino diet. Some participants received meal assistance (e.g. Meals on Wheels) but for one female participant, “I can’t learn to like them. I try to be patient because there’s nothing else to eat.” Emerging themes included intake of oatmeal for breakfast because it was affordable and often provided by food pantries.
Interpersonal-level factors: healthcare interactions
Physician influence on changes in CVD health behaviors.
Participants often cited physician’s advice as the reason for modifying their dietary practices. Several participants described receiving recommendations from their physicians to consume less salty and fatty foods, and less beef and pork. They also avoided or limited their rice intake, a Filipino meal staple. Some participants, however, admitted that eliminating salt and rice from their diet was difficult, and that they would consume “just a little” as an alternative. Fish and vegetables were viewed as healthier options and chicken and fish were seen as better alternatives to pork and beef. Participants described switching to healthier eating habits after being diagnosed with CVD, such as substituting chicken for pork in traditional Filipino dishes. For example, a female participant commented in reference to her favorite dish, sinigang (tamarind stew) that is usually made with pork: “It shouldn’t be with chicken. But we don’t want to eat pork and beef. That’s not allowed. But that should have been the main ingredient in this dish. We just modified it, so it won’t be bad for our body. So we just use chicken instead.” Overall, most participants valued their physicians’ advice on diet and nutrition but were often reluctant to disclose potentially unhealthy eating behaviors to their physicians. On the other hand, some participants saw little benefit in seeing the physician when asymptomatic; one participant said “if you don’t feel anything, they (doctors) shouldn’t check on you.”
Individual-level beliefs and attitudes
Beliefs that traditional dietary practices increase risk of CVD.
Participants often attributed their CVD-related health problems to the Filipino diet and traditional eating habits. In the survey, over 60% believed that eating habits affect their chance of getting heart disease. Participants were aware that high-fat and high-sodium foods were “bad” for the heart and commonly cited red meat, including pork as unhealthy. Participants often referred to unhealthy food as “forbidden,” using the Tagalog word bawal in describing food that they can no longer incorporate into their diet due to their CVD. Some participants shared that giving up old habits and adjusting to a new diet is challenging, especially when traditional Filipino cuisine is served at the dining table or during social events.
DISCUSSION
This study is the first community-based Photovoice study to explore dietary behaviors among older Filipino Americans with CVD. Through this innovative qualitative method, our study identified opposing acculturation dynamics that affected the dietary practices of Filipino immigrants in the U.S. with CVD. First, participants reported their efforts to retain connection to Filipino culture through food and eating habits shaped by cultural health beliefs. Second, they struggled to reconcile their traditional Filipino dietary practices, which they believed tended to be unhealthy, with the need to adhere to a heart healthy diet recommended by their physicians. While participants valued their physicians’ advice, they were reluctant to disclose when they were not adhering to a heart healthy diet. Social and physical environments, e.g. housing structure and household members’ food preferences, as well as food insecurity also shaped dietary habits.
In this population of older Filipino immigrants with CVD, we found that food was an integral part of Filipino American culture and identity, consistent with prior studies (dela Cruz et al., 2013; Johnson-Kozlow et al., 2011; Serafica, Ceria-Ulep, & Lane, 2015). Sharing a meal (pag sasalu-salo) is a significant aspect of daily Filipino life, and food is often the highlight of major celebrations and festivals, serving as a way to connect with family, friends, neighbors and the community. Foods traditionally shared during Filipino festivals are often high in carbohydrates, fat, and animal protein and supplemented with high sodium dipping sauces such as soy sauce (Azar, Chen, Holland, & Palaniappan, 2013). For Filipino Americans with CVD who try to adhere to a healthier diet, consuming “just a little” of traditional foods may be a way to accept the food that is being shared in a group, while attempting to follow a heart healthy diet.
The need to balance connection to Filipino culture through traditional foods and the use of ingredients available in the U.S. reflects the dynamic and multidimensional process of dietary acculturation among immigrants (Satia-Abouta, Patterson, Neuhouser, & Elder, 2002). Filipino immigrants may retain some traditional dietary habits and beliefs due to their greater attachment to their culture or of memories associated with foods consumed while living in their native country. Filipino Americans in our study believed that traditional Filipino dietary practices such as consumption of white rice, beef, pork or addition of shrimp paste increased risk of CVD. Due to this perception of Filipino dietary practices, participants often used the word bawal or “forbidden” to indicate the restriction on certain Filipino food items, which may have been reinforced by dietary counseling provided in the clinical setting. However, in an effort to adopt healthier eating habits to help address CVD diagnoses, some participants modified traditional recipes with healthier alternatives such as using leaner protein like chicken, reducing intake of white rice or strategically including vegetables accessible and affordable in the U.S. The potential to adapt Filipino food practices to make them healthier may be a viable public health strategy that preserves and respects important cultural dietary practices, while simultaneously promoting heart healthier diets than can reduce the risk of CVD and its complications.
Our participants reported a reluctance to disclose potentially unhealthy eating behaviors to their clinical providers. This could be due in part to English language anxiety of Filipino immigrants in communicating with their healthcare providers (Maneze et al., 2016) as about 50% of our study population reported LEP and all focus groups were conducted primarily in Tagalog. Healthcare providers may assume that their Filipino patients are proficient in English, which could lead to miscommunication of health recommendations including diet and nutrition during a clinical visit. Furthermore, providers who care for Filipino immigrants, would do well to avoid the use of “forbidding” or “prohibiting” when referring to elements of the Filipino diet to avoid negative connotations towards Filipino foods that are an essential part of Filipino culture. The use of Photovoice in this study may have made it easier for participants to talk about their dietary practices, including those they viewed as unhealthy, and could serve potentially as a communication tool in enhancing understanding of cultural beliefs influencing dietary behaviors for Filipino immigrants within the clinical setting.
Half of the participants were food insecure which is comparable to a prior study of San Francisco Chinese Americans that had a 59% prevalence of food insecurity (Lyles, Nord, Chou, Kwan, & Seligman, 2015). Coping strategies for food insecurity reported by our participants included using food distribution resources, cooking at home as opposed to eating out, maximizing use of food and minimizing waste. Food insecurity can lead to nutritional insufficiencies and contribute to the development or exacerbation of chronic diseases, including diabetes. Meeting the recommended diets for specific chronic conditions may be challenging in the context of economic constraints (Olson, 1999; Seligman, Jacobs, Lopez, Tschann, & Fernandez, 2012; Seligman, Laraia, & Kushel, 2010). Further research is needed to examine interrelationships between cultural factors, the impact of food insecurity on nutritional status, and chronic disease management among Asian American immigrants, particularly Filipino Americans.
Limitations of this study include a small sample size which limits our ability to assess differences by gender and household roles. In addition, our study focused on the contextual factors that influence dietary behaviors and did not assess actual dietary behaviors. Next, the participant photos and narratives could have been influenced by a social desirability bias. Lastly, our findings may not be fully generalizable to the general Filipino American population as we recruited participants from a convenience sample of Filipinos living in San Francisco. The strengths of this study include a mixed methods approach that included a survey, photos, and focus group data, the high retention rate, and the use of CBPR, including interpretation of the key findings by community partners.
CONCLUSION
We found that both cultural and socio-economic factors outside of the healthcare system and interactions with healthcare providers influenced dietary behaviors of Filipino immigrants with CVD. Participants perceived that common Filipino dietary practices contribute to an increased risk of CVD, but were willing to modify traditional foods for healthier alternatives. The application of Photovoice-led focus groups was feasible among older Filipinos and use of Photovoice may enhance reporting of dietary behaviors and our understanding of the dynamic forces that shape these. Further research should explore the use of photos as a way to enhance communication about diet between healthcare providers and Filipino patients and ways to incorporate heart healthy approaches to traditional diets.
ACKNOWLEDGEMENTS
We would like to thank the participants for their contributions to this study. This study was funded by the National Institute on Aging (NIA) Grant P30 AG15272 with additional support from NIA Grant R03 AG050880 and the National Center for Advancing Translational Sciences Grant UL1 TR000004.
Contributor Information
Jane Jih, University of California San Francisco.
Trish La Chica, Hawai’i Public Health Institute.
Luisa M. Antonio, Veterans Equity Center
Ofelia O. Villero, University of California San Francisco
Mary N. Roque, Veterans Equity Center
Joseph R. Domingo, Asian American Research Center on Health
Joshua F. Landicho, Veterans Equity Center
Anna M. Napoles, University of California San Francisco
Celia P. Kaplan, University of California San Francisco
Tung T. Nguyen, University of California San Francisco
REFERENCES
- Azar KM, Chen E, Holland AT, & Palaniappan LP (2013). Festival foods in the immigrant diet. J Immigr Minor Health, 15(5), 953–960. doi: 10.1007/s10903-012-9705-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badarudeen S, & Sabharwal S (2010). Assessing Readability of Patient Education Materials: Current Role in Orthopaedics. Clinical Orthopaedics and Related Research, 468(10), 2572–2580. doi: 10.1007/s11999-010-1380-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes PM, Adams PF, & Powell-Griner E (2008). Health characteristics of the Asian adult population: United States, 2004-2006. Adv Data(394), 1–22. [PubMed] [Google Scholar]
- Bickel G, Nord M, Price C, Hamilton W, & Cook J (2000). Guide to Measuring Household Food Security. Revised 2000. Alexandriaa, VA: U.S. Department of Agriculturee Food and Nutrition Service. [Google Scholar]
- Cardiovascular Risk in the Filipino Community: Formative Research from Daly City and San Francisco, California. (March 2003). Retrieved from https://www.nhlbi.nih.gov/files/docs/resources/heart/filipino.pdf
- Catalani C, & Minkler M (2010). Photovoice: a review of the literature in health and public health. Health Educ Behav, 37(3), 424–451. doi: 10.1177/1090198109342084 [DOI] [PubMed] [Google Scholar]
- Dahlgren G, Whitehead M (1992). Policies and strategies to promote social equity in health. World Health Organization. [Google Scholar]
- dela Cruz FA, Lao BT, & Heinlein C (2013). Level of acculturation, food intake, dietary changes, and health status of first-generation Filipino Americans in Southern California. Journal of the American Association of Nurse Practitioners, n/a-n/a. doi: 10.1111/1745-7599.12031 [DOI] [PubMed] [Google Scholar]
- Fitzpatrick AL, Steinman LE, Tu SP, Ly KA, Ton TG, Yip MP, & Sin MK (2012). Using photovoice to understand cardiovascular health awareness in Asian elders. Health Promot Pract, 13(1), 48–54. doi: 10.1177/1524839910364381 [DOI] [PubMed] [Google Scholar]
- Hergenrather KC, Rhodes SD, Cowan CA, Bardhoshi G, & Pula S (2009). Photovoice as community-based participatory research: a qualitative review. Am J Health Behav, 33(6), 686–698. [DOI] [PubMed] [Google Scholar]
- Hoeffel EM, Rastogi S, Kim MO, & Shahid H (2012). The Asian Population: 2010. (C2010BR-02). Washington, DC: U.S. Census Bureau; Retrieved from http://www.census.gov/prod/cen2010/briefs/c2010br-11.pdf. [Google Scholar]
- Holland AT, Wong EC, Lauderdale DS, & Palaniappan LP (2011). Spectrum of cardiovascular diseases in Asian-American racial/ethnic subgroups. Ann Epidemiol, 21(8), 608–614. doi: 10.1016/j.annepidem.2011.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Idler EL, & Benyamini Y (1997). Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav, 38(1), 21–37. [PubMed] [Google Scholar]
- Jih J, Mukherjea A, Vittinghoff E, Nguyen TT, Tsoh JY, Fukuoka Y, Kanaya AM (2014). Using appropriate body mass index cut points for overweight and obesity among Asian Americans. Prev Med, 65, 1–6. doi: 10.1016/j.ypmed.2014.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson-Kozlow M, Matt GE, Rock CL, de la Rosa R, Conway TL, & Romero RA (2011). Assessment of dietary intakes of Filipino-Americans: implications for food frequency questionnaire design. J Nutr Educ Behav, 43(6), 505–510. doi: 10.1016/j.jneb.2010.09.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karliner LS, Napoles-Springer AM, Schillinger D, Bibbins-Domingo K, & Perez-Stable EJ (2008). Identification of limited English proficient patients in clinical care. J Gen Intern Med, 23(10), 1555–1560. doi: 10.1007/s11606-008-0693-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karter AJ, Schillinger D, Adams AS, Moffet HH, Liu J, Adler NE, & Kanaya AM (2013). Elevated rates of diabetes in Pacific Islanders and Asian subgroups: The Diabetes Study of Northern California (DISTANCE). Diabetes Care, 36(3), 574–579. doi: 10.2337/dc12-0722 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyles CR, Nord M, Chou J, Kwan CML, & Seligman HK (2015). The San Francisco Chinese Food Security Module: Validation of a Translation of the US Household Food Security Survey Module. Journal of Hunger & Environmental Nutrition, 10(2), 189–201. doi: 10.1080/19320248.2014.962776 [DOI] [Google Scholar]
- Maneze D, Everett B, Kirby S, DiGiacomo M, Davidson PM, & Salamonson Y (2016). ‘I have only little English’: language anxiety of Filipino migrants with chronic disease. Ethn Health, 1–13. doi: 10.1080/13557858.2016.1143091 [DOI] [PubMed] [Google Scholar]
- Nordström K, Coff C, Jönsson H, Nordenfelt L, & Görman U (2013). Food and health: individual, cultural, or scientific matters? Genes Nutr, 8(4), 357–363. doi: 10.1007/s12263-013-0336-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olson CM (1999). Nutrition and Health Outcomes Associated with Food Insecurity and Hunger. J Nutr, 129(2), 521. [DOI] [PubMed] [Google Scholar]
- Russinova Z, Rogers ES, Gagne C, Bloch P, Drake KM, & Mueser KT (2014). A randomized controlled trial of a peer-run antistigma photovoice intervention. Psychiatr Serv, 65(2), 242–246. doi: 10.1176/appi.ps.201200572 [DOI] [PubMed] [Google Scholar]
- Satia-Abouta J, Patterson RE, Neuhouser ML, & Elder J (2002). Dietary acculturation: applications to nutrition research and dietetics. J Am Diet Assoc, 102(8), 1105–1118. [DOI] [PubMed] [Google Scholar]
- Seligman HK, Jacobs EA, Lopez A, Tschann J, & Fernandez A (2012). Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care, 35(2), 233–238. doi: 10.2337/dc11-1627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seligman HK, Laraia BA, & Kushel MB (2010). Food insecurity is associated with chronic disease among low-income NHANES participants. J Nutr, 140(2), 304–310. doi: 10.3945/jn.109.112573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Serafica RC, Ceria-Ulep CD, & Lane SH (2015). Hapag Kainan: Dietary Consumption of Fat, Sugar, Fruits and Vegetables Among Filipino Americans. J Cult Divers, 22(3), 95–104. [PubMed] [Google Scholar]
- Wang C, & Burris MA (1997). Photovoice: concept, methodology, and use for participatory needs assessment. Health Educ Behav, 24(3), 369–387. [DOI] [PubMed] [Google Scholar]
- Wang CC (1999). Photovoice: a participatory action research strategy applied to women’s health. J Womens Health, 8(2), 185–192. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2004). Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet, 363(9403), 157–163. [DOI] [PubMed] [Google Scholar]


