Abstract
Background
Emergency department (ED) crowding is a critical problem in the delivery of acute unscheduled care. Many causes are external to the ED, but antiquated operational traditions like triage also contribute. A physician intake model has been shown to be beneficial in a single-centre study, but whether this solution is generalisable is not clear. We aimed to characterise the current state of front-end intake models in a national sample of EDs and quantify their effects on throughput measures.
Methods
We performed a descriptive mixed-method analysis of ED process changes implemented by a cross section of self-selecting institutions who reported 2 years of demographic/operational data and structured process descriptions of any ‘new front-end processes to replace traditional nurse-based triage’.
Results
Among 25 participating institutions, 19 (76%) provided data. While geographically diverse, most were urban, academic adult level 1 trauma centres. Thirteen (68%) reported implementing a new intake process. All were run by attending emergency physicians, and six (46%) also included advanced practice providers. Daily operating hours ranged from 8 to 16 (median 12, IQR 10.25–15.85), and the majority performed labs, imaging and medication administration and directly discharged patients. Considering each site’s before-and-after data as matched pairs, physician-driven intake was associated with mean decreases in arrival-to-provider time of 25 min (95% CI 13 to 37), ED length of stay 36 min (95% CI 12 to 59), and left before being seen rate 1.2% (95% CI 0.6% to 1.8%).
Conclusions
In this cross section of primarily academic EDs, implementing a physician-driven front-end intake process was feasible and associated with improvement in operational metrics.
Keywords: emergency department, healthcare quality improvement, implementation science, management, teamwork
Introduction
Background and importance
For many years, emergency department (ED) crowding has been highlighted as a critical barrier to the delivery of acute, episodic and unscheduled care.1 The roots of crowding are multifactorial and have inspired interventions ranging from demand reduction (eg, financial incentives or patient education to decrease ED demand)2 to organisational principles and practices to streamline patient flow out of the ED.3 In addition, many have targeted ED throughput by developing innovative methods of optimising patient flow, maximising the utility of ED resources and improving clinically relevant metrics, such as door-to-provider time, which are used in benchmarking ED operational performance.4 ED throughput optimisation interventions have been heterogeneous and have included use of nurse-driven order protocols,5 advanced practice providers (APPs) as front-end providers6 and use of point-of-care laboratory tests in front-end processes.7
One large academic ED recently detailed the design and implementation of a novel split-flow model using an attending physician-driven front-end process and demonstrated clinically important improvements in patient-centred operational metrics, including length of stay (LOS), left before being seen (LBBS) rates and arrival-to-provider time.8 This model completely removes antiquated nurse-based triage and is distinctly different from ‘provider-in-triage’, which is usually described as a provider (physician or APP) assigned to see patients during or immediately after a nurse completes a triage assessment.9 While such models clearly decrease arrival-to-provider time, these models have not shown demonstrable improvement in overall ED flow and have not been sustainable.9 A physician-driven intake model has been shown to be viable and beneficial in large single-centre studies,8 9 but it is not yet clear whether this model represents a generalisable solution. The fundamental theory of physician-driven intake is that patients do not come to an ED to be triaged to wait, and attending providers are uniquely positioned to rapidly assess and disposition patients (including perform a medical screening exam and discharge). Neither registered nurses nor resident trainees are typically allowed by hospital by-laws to independently make an ED discharge decision.
Timeliness of care is a measure of quality, correlates with safety as an outcome10 and has been shown to improve patient experience.11 The ability to successfully scale patient-centred operational innovations nationally is relevant and important to ED patient care.
Goals of this investigation
In this study, we assess the dissemination of a novel intervention among participants of an on-site peer-to-peer coaching session led by the sentinel best-practice site who implemented physician-in-intake in order to evaluate the scalability of this model. We aimed to characterise the current state of front-end process models in this national sample of ED sites and attempt to quantify the effects of provider-driven front-end processes on throughput measures at multiple EDs.
Methods
Study design and setting
We performed a descriptive mixed-method analysis of ED front-end process changes implemented by a cross section of national institutions, all of whom self-selected to participate in a structured site visit, best practice sharing and consultation related to ED flow redesign between 2013 and 2017.
Selection of participants
Study participants were selected from institutions that had taken part in on-site consulting sessions and ED tours at the University of Colorado. These visits consisted of half-day or full-day sessions, which included a structured ED visit, peer coaching sessions (eg, chief nursing officer to chief nursing officer) and a leadership journey presentation with detailed descriptions of the operational implementation success measures and cultural change engagement characteristics that led to marked and sustained improvement in ED metrics and patient experience.8 Participants were either planning to implement a future operational change within their own organisation or had already embarked on process redesign and were seeking consultation advice. Most institutional participant delegations consisted of departmental leaders (eg, nurse manager or director, medical director and quality specialist) and senior executives (eg, hospital vice president, chief nursing officer and chief operating officer). During their visit, participants were notified of the intent to evaluate the effect of the learnings from the visit on operational implementations. In the fall of 2017, 2–3 years after an institution’s site visit (which provided sufficient time for process changes to have been fully implemented), we identified the lead contact for each participating institution and contacted them via email to request participation in the study to evaluate the effect of participation in the onsite programme.
Patient and public involvement
There were no funds or time allocated for patient and public involvement, so we were unable to involve patients in this study, although individual sites may have involved patients in implementing ED process changes without our knowledge. We have invited patients to help us develop our dissemination strategy.
Measurements and data collection
Study institutions were contacted by up to three attempts via an electronically delivered unique survey via Research Electronic Data Capture,12 a secure, web-based application designed to support data capture.
Study sites provided self-reported ED demographic data for the prior year (annual volume, proportion of paediatric patients, median patient age, hospital admission rate, transfer rate, trauma designation, academic and environmental setting, and observation unit presence). The structured survey questions included whether the institution had implemented any ‘new front-end processes to replace traditional nurse-based triage’, and if the answer was affirmative, we cascaded additional questions pertaining to the old and new process descriptions, operating hours, activities performed and staffing model. Respondents who reported implementing a process change were asked to report their standard ED operational metrics4 13 before and after the process change. We requested 1 year of data for each time period; however, participants were able to report a different time interval if they had not yet accumulated 1 year of data after a process implementation. Examples of the survey instrument and data dictionary are included in the online supplementary materials.
bmjoq-2019-000817supp001.pdf (158.7KB, pdf)
Data processing and analysis
We considered participants answering one or more questions to have responded and reported missing data in each analysis. We screened continuous responses for outliers that may have suggested a data entry error and validated continuous responses for correct units and ranges, as defined in the data dictionary (see online supplementary materials). We calculated descriptive statistics, preferentially reporting 95% two-sided CIs for comparisons, rather than hypothesis tests, because they can help assess both practical and statistical significance. We avoided distributional assumptions and calculated CIs for medians and IQRs using smoothed empirical likelihood quantile estimates based on a kernel density function.12 For analysis of matched pairs, we also calculated mean differences with 95% CIs. Participants provided consent at the beginning of the survey, and the study was approved by our institutional review board. Analyses were conducted using JMP Pro V.14.1 (SAS Institute, Cary, NC, USA).
Results
Characteristics of study subjects
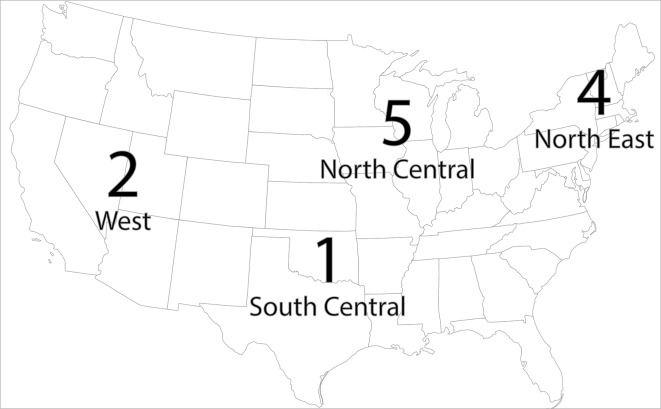
Among the 25 institutions participating in onsite visits who agreed to provide contact information for follow-up in the study, 19 (76%) responded to the survey. Demographics of responding EDs are provided in table 1. Participants were geographically diverse, representing all regions of the USA, and included one international site (figure 1). Major regional trends were not identified, so we chose not to report results by region due to the risk of individual institution identification. Most institutions were urban, academic EDs designated as level 1 trauma centres, caring for a primarily adult patient population. Among 16 EDs who reported evaluating paediatric patients, 9 (56%) used a different front-end process for this population. Most commonly, these EDs used a separate paediatric area or department with direct rooming.
Table 1.
Demographic data of participating EDs
| Annual ED census volume | |
| Median (IQR) | 73 000 (55 000–89 900) |
| Participants reporting, n (%) | 15 (79) |
| Paediatric mix (%) | |
| Median (IQR) | 2.7 (0.0–19.0) |
| Participants reporting, n (%) | 15 (79) |
| Median patient age | |
| Median (IQR) | 44.7 (42.0–52.5) |
| Participants reporting, n (%) | 9 (47) |
| ED admission rate (%) | |
| Median (IQR) | 27 (20–36) |
| Participants reporting, n (%) | 15 (79) |
| Transfer out rate (%) | |
| Median (IQR) | 1.0 (0.9–1.1) |
| Participants reporting, n (%) | 13 (68) |
| Setting, n (%) | |
| Urban | 13 (68) |
| Suburban | 3 (16) |
| Rural | 0 |
| Did not respond | 3 (16) |
| Educational affiliation, n (%) | |
| Academic | 14 (74) |
| Community | 1 (5) |
| Other | 1 (5) |
| Did not respond | 3 (16) |
| Trauma centre designation, n (%) | |
| Level 1 | 10 (52) |
| Level 2 | 2 (11) |
| Level 3 | 2 (11) |
| Other designated | 1 (5) |
| Non-designated | 1 (5) |
| Did not respond | 3 (16) |
| ED observation unit, n (%) | |
| None | 6 (31) |
| Outside ED | 3 (16) |
| Inside ED | 7 (37) |
| Did not respond | 3 (16) |
ED, emergency department.
Figure 1.
Geographical distribution of participating EDs. One ED was located in Singapore (not pictured). ED, emergency department.
Main results
Thirteen EDs (68% of total respondents) reported implementing a new front-end intake process. All reported that the prior process was a traditional nurse-based triage system. EDs varied as to the services and activities performed in the front-end (table 2) and patient exclusion criteria (table 3), but all reported staffing the new process with an attending emergency physician. Twelve EDs staffed intake with a dedicated attending physician, and one ED described sharing an attending physician between intake and another ED treatment area. Six EDs added an APP, in addition to the attending physician. Other staffing decisions are described in table 4.
Table 2.
Services and activities performed in new front-end processes
| Laboratory studies | 11 (85%) |
| Imaging studies | 10 (77%) |
| Medication administration | 8 (62%) |
| Discharge patients directly | 8 (62%) |
| Assignment of triage score | 7 (54%) |
| Consultations | 3 (23%) |
Table 3.
Patient exclusion criteria from front-end processes
| EMS arrivals | 4 (31%) |
| Vital sign abnormalities | 9 (69%) |
| Critical presentation | 3 (23%) |
| Limited English proficiency | 0 |
EMS, emergency medical services.
Table 4.
Front-end process dedicated staffing
| Attending physician | 12 (92%) |
| Advanced practice provider | 6 (46%) |
| Resident physician | 3 (23%) |
| Medical scribe | 7 (54%) |
| Registered nurse | 9 (69%) |
| Technician | 7 (54%) |
| Phlebotomist | 1 (8%) |
| ECG technician | 4 (31%) |
| Security staff | 5 (38%) |
Treatment spaces dedicated to the front-end ranged from 0 to 16 (median 4, IQR 3–7) and most commonly employed reclining chairs. Twelve EDs reported opening intake during scheduled hours, eight of which were open every day, and four were open only Monday through Friday. Daily scheduled operating hours ranged from 8 to 16 hours per day (median 12, IQR 10.25–15.85). One ED reported that intake was not open during scheduled hours, and direct bedding was used in the main ED with intake opening only as a surge plan.
Six EDs (50%) had a structured quality monitoring programme for the front-end process. Seven EDs (54%) described a predefined surge plan to add additional resources to the front end if needed. Additional textual and qualitative process descriptions are provided in online supplementary tables S1–S3.
Table 5 reports ED operational metrics before and after front-end implementation. EDs reported significant reductions in arrival-to-provider time, overall LOS and LBBS rates after front-end implementation, with no changes in median daily census or median daily boarding hours.
Table 5.
ED operational metrics before and after front-end process implementation
| Before implementation | After implementation | Mean change (95% CI) (each ED as matched pair) | |
| Median arrival-to-provider time (min) | −25 (−37 to −13) | ||
| Median (95% CI) | 60 (37 to 71) | 31 (21 to 42) | |
| IQR | 41–77 | 22–39 | |
| Range | 16–80 | 10–54 | |
| Median ED length of stay for all patients (min) | −36 (−59 to −12) | ||
| Median (95% CI) | 298 (260 to 341) | 261 (222 to 307) | |
| IQR | 243–350 | 225–312 | |
| Range | 230–377 | 180–347 | |
| Overall left before being seen rate (%) | −1.2 (−1.8 to −0.6) | ||
| Median (95% CI) | 2.6 (1.4 to 7.0) | 1.4 (0.7 to 6.1) | |
| IQR | 1.0–3.5 | 0.5–1.6 | |
| Range | 0.7–8.6 | 0.4–6.8 | |
ED, emergency department.
Limitations
This study had several important limitations. Our data collection was limited to a relatively small number of sites, all of which had self-selected to participate in ED front-end consulting sessions and, therefore, may not represent a generalisable sample. All of the sites participating in the study had an annualised census of greater than 55 000 patients, and most were academic, potentially limiting the applicability of results to lower-volume or community EDs.
While specific guidance and standardised definitions for each metric were provided using standard accepted data definitions13 14 data were self-reported and not directly verifiable by the authors. Data were limited to the number of operational metrics provided for reporting. Although subprocess measures (eg, provider-to-disposition decision and disposition decision-to-departure times) and measures stratified by split-flow area (eg, LOS for intake patients vs non-intake patients) are helpful to evaluate the implementation of a process, they were not available from nearly all institutions. Similarly, descriptions of the actual intake process were limited to self-reporting across a few dimensions and did not include a site visit or standardised process rubric to ensure that the processes implemented at each site truly reflected that at the exemplar site.
While descriptive data likely accurately reflect the front-end processes in place at the participating institutions, before-and-after operational metric comparisons may be subject to a number of known limitations, including unmeasured confounders and parallel process changes, flawed distributional assumptions, narrowing of variation that may not shift central tendency and outlier effect modification. Repeated measures over time (including a longer baseline period prior to intake implementation) would permit evaluation of level changes and slope changes associated with intake process changes. However, we had only aggregate before-and-after data, which limit our ability to assess whether improvements were under way prior to intake implementation or to ascertain how rapidly each metric changed after implementation. This study design is certainly unable to establish a causal relationship between front-end process change and improvement of operational metrics.
Discussion
Because replacement of traditional nurse triage with a physician intake process has only been described since 2016,8 it remains unclear how many EDs in the USA are currently using such a model and how variable the models are. Original descriptions of physician intake make clear that it is the integration of physicians, scribes, nurses, technicians, signalling, flow processes and symbiosis with an APP-led midtrack that allows the process to achieve results. Without substantive process redesign, singularly adding a provider to triage (or replacing a nurse in triage with a provider in triage) is unlikely to have much impact. Our results suggest that achieving full implementation of physician intake is challenging but feasible and effective, even though a few sites reported only partial implementations. However, we believe this still represents the largest study to date and the only multicentre description of ED front-end processes.9 The results suggest that implementation of a physician intake model has positive improvements on operational metrics, at least among EDs with more than 43 000 annual visits.
While most processes share common elements, we observed between-site heterogeneity in the way they are designed and implemented. Importantly, all systems involved an attending physician, and at 92% of sites, the attending was dedicated to intake. At one location, attending oversight was provided by a physician with additional patient care responsibilities outside of intake. Just under half of the sites also included a dedicated APP, although job responsibilities varied. In some models, APPs evaluated newly arriving patients, and in others, APPs primarily followed up on results, performed procedures and discharged patients. Most sites included dedicated nurses, technicians and support staff (including phlebotomists, EKG technicians and registration staff). As some sites did not provide a detailed narrative discussion of staffing decisions, we presume that EDs who reported not having dedicated nurses or technicians shared staff between the front end and other areas of the ED. Interestingly, only half of models included a dedicated scribe, and despite most sites being academically affiliated, a minority included residents. It remains to be seen whether different design choices translate to different outcomes, as most EDs in this sample reported similar overall operational improvements. How to best train residents to perform as future attending-level intake providers and how to ensure that residents have an opportunity to initiate workup of undifferentiated patients already seen by an intake attending also remain open questions.
Several other findings were surprising. All institutions who implemented a physician intake process also reported eliminated nurse triage. However, just under half of sites (6 of 13) eliminated the assignment of ‘triage scores’ (ie, Emergency Severity Index), a process created to estimate expected resource intensity and to decide which patients can wait to see a physician,15 which, obviously, has no applicability when a physician is performing intake. In the physician intake model, patients see a physician nearly immediately, and initial resource needs are known as soon as the physician places orders, so triage scores would appear to be invalid or not useful, yet are still commonly assigned. More research is needed to determine a new prioritisation classification system for patients who are seen by a physician at intake and must later wait to be roomed (eg, in an internal waiting room), as existing scoring systems were created and validated under a nurse triage paradigm.
The ability to have a physician evaluate a patient on arrival not only improves productive waiting later in the visit but also allows for appropriate patients to be discharged immediately after a medical screening exam is completed and no need for additional ED resources is identified. This is an important distinction between physician intake and provider-in (behind)-triage models. However, 38% of respondents reported not discharging patients through their new front-end processes, a practice that potentially results in longer lengths of stay and increased use of ED resources (namely, beds). The reason for this practice is unclear but is also worthy of further study, as expedited discharge or referral to alternative venues of care would seem to be a major advantage of attending physician-driven intake models.
Dissemination and implementation of best practices in ED operations remain challenging16 and are heavily dependent on organisational characteristics, including executive leadership involvement, hospital-wide coordinated strategies, data-driven management and performance accountability.3 Even among a cross section of EDs with forward-thinking leaders who invested in a multidisciplinary on-site coaching visit, study participants reported a number of classic organisational and change-management barriers to implementing physician-driven intake. Capital needs were commonly mentioned, as most EDs reported that the physical layout of traditional triage areas was not conducive to creating highly performing intake systems. Similarly, space constraints in the processes immediately postintake assessment (eg, phlebotomy, imaging, movement to main ED treatment spaces and availability of internal waiting areas) were described as limiting as well. Boarding was specifically mentioned by multiple respondents, as movement of patients from intake areas to main ED treatment spaces is quite difficult when a large proportion of ED spaces are occupied by boarding inpatients. Despite all respondents having participated in site visits that explicitly invited the participation of hospital executives, obtaining buy-in from hospital leaders was frequently mentioned as a barrier to implementation. Given the self-selecting nature of this study cohort, dissemination of physician intake among less highly performing institutions is likely to be exponentially more challenging.
In summary, our analysis suggests that a modest number of EDs appear to have implemented physician-driven front-end intake processes. Understanding that our methodology has significant limitations, we found that these EDs reported improvement in three meaningful operational metrics: door-to-provider time, LOS and LBBS rates. Implementing physician-driven intake models appears feasible in this cross section of larger, primarily academic EDs.
Acknowledgments
The authors thank Drs Sanjeev Malik, Michael Schmidt, James Adams and Daniel Cruz (Northwestern University); Drs Azita Hamedani, Josh Ross, Michael Safa, Brian Sharp, Dina Geier and Anne Rifleman (University of Wisconsin); Dr Sam Shen (Stanford University); Drs Robert Poirier and Chandra Aubin and Blake Exline and Holly Watson (Washington University); Drs Chris Baugh, Janet Gorman, Hillary Cornish, Jonny McCabe and Jay Schuur (Brigham and Women's Hospital); and Houston Methodist Hospital. Some contributors also elected to remain anonymous.
Footnotes
Contributors: JLW, DB, KB and RZ conceived of the study. DB, SSM and JLW supervised the data collection. SSM and DB managed the data, and SSM provided statistical advice on the study design and analysed the data. All authors had access to the data. SSM and DB drafted the manuscript, and all authors contributed substantially to its revision. SSM takes responsibility for the paper as a whole.
Funding: This work was unfunded but did rely upon infrastructure within the Colorado Clinical & Translational Sciences Institute (CCTSI) with Development and Informatics Service Center grant support (National Institutes of Health/National Center for Research Resources CCTSI grant number UL1 RR025780).
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: This study was approved by the Colorado Multiple Institutional Review Board (13-2273).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1. Institute of Medicine Hospital-Based emergency care. Washington, DC: National Academies Press, 2007. [Google Scholar]
- 2. Morgan SR, Chang AM, Alqatari M, et al. Non-emergency department interventions to reduce ED utilization: a systematic review. Acad Emerg Med 2013;20:969–85. 10.1111/acem.12219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Chang AM, Cohen DJ, Lin A, et al. Hospital strategies for reducing emergency department crowding: a mixed-methods study. Ann Emerg Med 2018;71:497–505. 10.1016/j.annemergmed.2017.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Welch SJ, Stone-Griffith S, Asplin B, et al. Emergency department operations dictionary: results of the second performance measures and benchmarking Summit. Acad Emerg Med 2011;18:539–44. 10.1111/j.1553-2712.2011.01062.x [DOI] [PubMed] [Google Scholar]
- 5. Retezar R, Bessman E, Ding R, et al. The effect of triage diagnostic standing orders on emergency department treatment time. Ann Emerg Med 2011;57:89–99. 10.1016/j.annemergmed.2010.05.016 [DOI] [PubMed] [Google Scholar]
- 6. Hayden C, Burlingame P, Thompson H, et al. Improving patient flow in the emergency department by placing a family nurse practitioner in triage: a quality-improvement project. J Emerg Nurs 2014;40:346–51. 10.1016/j.jen.2013.09.011 [DOI] [PubMed] [Google Scholar]
- 7. Singer AJ, Taylor M, LeBlanc D, et al. Early point-of-care testing at triage reduces care time in stable adult emergency department patients. J Emerg Med 2018;55:172–8. 10.1016/j.jemermed.2018.04.061 [DOI] [PubMed] [Google Scholar]
- 8. Wiler JL, Ozkaynak M, Bookman K, et al. Implementation of a front-end Split-Flow model to promote performance in an urban academic emergency department. Jt Comm J Qual Patient Saf 2016;42:271–4. 10.1016/S1553-7250(16)42036-2 [DOI] [PubMed] [Google Scholar]
- 9. Wiler JL, Gentle C, Halfpenny JM, et al. Optimizing emergency department front-end operations. Ann Emerg Med 2010;55:142–60. 10.1016/j.annemergmed.2009.05.021 [DOI] [PubMed] [Google Scholar]
- 10. Gaieski DF, Agarwal AK, Mikkelsen ME, et al. The impact of ED crowding on early interventions and mortality in patients with severe sepsis. Am J Emerg Med 2017;35:953–60. 10.1016/j.ajem.2017.01.061 [DOI] [PubMed] [Google Scholar]
- 11. Pines JM, Iyer S, Disbot M, et al. The effect of emergency department crowding on patient satisfaction for admitted patients. Acad Emerg Med 2008;15:825–31. 10.1111/j.1553-2712.2008.00200.x [DOI] [PubMed] [Google Scholar]
- 12. Chen SX, Hall P. Smoothed empirical likelihood confidence intervals for Quantiles. The Annals of Statistics 1993;21:1166–81. 10.1214/aos/1176349256 [DOI] [Google Scholar]
- 13. Welch SJ, Asplin BR, Stone-Griffith S, et al. Emergency department operational metrics, measures and definitions: results of the second performance measures and benchmarking Summit. Ann Emerg Med 2011;58:33–40. 10.1016/j.annemergmed.2010.08.040 [DOI] [PubMed] [Google Scholar]
- 14. Wiler JL, Welch S, Pines J, et al. Emergency department performance measures updates: proceedings of the 2014 emergency department benchmarking alliance consensus Summit. Acad Emerg Med 2015;22:542–53. 10.1111/acem.12654 [DOI] [PubMed] [Google Scholar]
- 15. Gilboy N, Tanabe P, Travers D, et al. Emergency severity index implementation Handbook. 4 edn Rockville, MD: Agency for Healthcare Research and Quality, 2018. http://www.ahrq.gov/professionals/systems/hospital/esi/ [Google Scholar]
- 16. Rabin E, Kocher K, McClelland M, et al. Solutions to emergency department 'boarding' and crowding are underused and may need to be legislated. Health Aff 2012;31:1757–66. 10.1377/hlthaff.2011.0786 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjoq-2019-000817supp001.pdf (158.7KB, pdf)