Abstract
Background
BRAF V600E mutations are associated with aggressive biology and limited response to standard chemotherapy, especially during second-line and beyond therapies. BRAF V600E mutant and wild-type colorectal cancers (CRCs) differ in their expression profiles, and preclinical evidence suggests that microtubule inhibitors have an antitumour effect on xenograft models of BRAF V600E mutant CRCs. Eribulin has the best growth inhibitory activity in vitro of the microtubule inhibitors. Also, we have evidenced a hint of activity for patients with BRAF V600E mutant metastatic CRC (mCRC) with tumour shrinkage following eribulin treatment.
Trial design
The BRAVERY study is a multicentre phase II study to evaluate the efficacy and safety of eribulin in patients with BRAF V600E mutant mCRC detected in either tumour tissues (primary analysis part) or circulating tumour DNA assays (liquid biopsy part). Key eligibility criteria are refractoriness and intolerance to at least one regimen (including irinotecan or oxaliplatin) containing fluoropyrimidine and Eastern Cooperative Oncology Group performance status of 0–1. Eribulin is to be administered intravenously at a dose of 1.4 mg/m2 on days 1 and 8 and repeated every 21 days. The primary endpoint is the confirmed objective response rate (ORR) by investigator’s assessment. We calculated the sample size of the primary analysis part at 27 patients using a two-stage design with 25% ORR deemed promising and 5% unacceptable (one-sided α, 0.05; β, 0.1). Secondary endpoints include disease control rate, progression-free survival, overall survival and adverse events. Moreover, we will collect pretreated tissue and serial blood samples for biomarker analyses, focusing on gene expression associated with BRAF mutant-like CRC to find predictive markers and acquired gene alterations to detect resistance mechanisms to eribulin. We initiated patient enrolment in March 2018, completed the primary analysis on May 2019, and are currently continuing with the liquid biopsy part.
Trial registration number
UMIN000031221 and 000031552.
Keywords: chemotherapy, investigator-initiated trial
Introduction
The development of new cytotoxic drugs has increased the median survival time (MST) for patients with metastatic colorectal cancer (mCRC) from 8 to approximately 30 months over the past two decades.1–3 However, BRAF V600E mutations occur in 8%–11% of patients with mCRC in western countries4 5 and in 4%–6% in Japan6 7 leading to poor prognoses and limited response to first-line fluoropyrimidine-based doublet chemotherapy plus targeted agents. The use of aggressive upfront chemotherapy with FOLFOXIRI plus/minus bevacizumab has the potential to improve prognoses.8 Conversely, second-line and beyond treatments have little efficacy, with response rates (RRs) at 0%–11%, median progression-free survivals (mPFSs) at 1.5–3.5 months and MSTs at 1.8–6.7 months.9 10 The development of new drugs is needed to improve outcomes in second-line and beyond therapies.
BRAF V600E mutant and wild-type tumours present different gene expression profiles. Vecchione et al found that RANBP2 increased microtubule outgrowth from the kinetochores and that shRANBP2 impaired BRAF V600E mutant CRC cell line proliferation, but not BRAF and KRAS wild-type cell lines, suggesting that the BRAF V600E mutant CRC may be vulnerable to mitosis.11 They also showed that only the BRAF V600E mutant CRC cell line had greater sensitivity to microtubule inhibitors, suggesting that microtubule inhibitors have antitumour activity against BRAF V600E mutant CRC cells.11
Eribulin is a microtubule inhibitor and has been used worldwide for patients with metastatic breast cancer or soft tissue tumours. Towle et al found that eribulin had greater growth inhibitory activity against the BRAF V600E mutant CRC cell line than either vinblastine or paclitaxel (IC50, 0.71±0.05 vs 2.4±0.02 or 7.8±1.5 nM, respectively).12 Eribulin had greater growth inhibitory activity against the BRAF V600E mutant CRC cell line and the BRAF V600E mutant melanoma and breast cancer cell lines than did vinblastine or paclitaxel, suggesting that eribulin has antitumour activity against BRAF V600E mutant cells that are not limited to CRC.12 Moreover, after analysing The Cancer Genome Atlas data, we found that the expression level of ABCB1 (ATP-binding cassette subfamily B member 1, also known as MDR1, and involved in eribulin resistance) in BRAF V600E mutant CRC cells was significantly lower than that in BRAF V600E wild-type CRC cells.13 We followed four patients with BRAF V600E mutant mCRC treated with eribulin. One patient had a confirmed partial response (PR) with 39% decrease from baseline CT. Another one had a stable disease (SD) with 7% decrease from baseline CT and 6 months of progression-free survival (PFS).13 Based on these results, we planned a multicentre phase II study of eribulin in patients with BRAF V600E mutant mCRC.
Study design and treatment
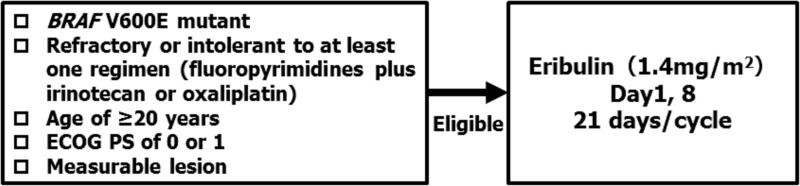
This study is a multicentre, open-label, single-arm phase II study to evaluate the efficacy and safety of eribulin monotherapy in patients with BRAF V600E mutant mCRC (figure 1). For this study, we divided patients into two study sections, one for primary analysis part and the other one for liquid biopsy parts. We identified patients as harbouring BRAF V600E mutant CRC based on next-generation sequencer-based and PCR-based assays using tumour tissues for the primary analysis part. Among the patients identified as harbouring BRAF V600E mutations based on a liquid biopsy test, we classified those showing positivity for the same mutation according to the analysis of tumour tissues into the primary analysis part and patients showing negativity for the same mutation by analysis of tumour tissues (or those unanalysable) into the liquid biopsy part (table 1).
Figure 1.
Study design. ECOG PS, Eastern Cooperative Oncology Group Performance Status.
Table 1.
Patients and study components
| Study patients | Tumour tissues | ||
| BRAF V600E mutant | BRAF V600E mutation negative or unanalysable | ||
|
Blood sample (ctDNA analysis) |
BRAFV600E mutant | Primary analysis part | Liquid biopsy part |
| BRAFV600E mutation negative or not evaluated | Primary analysis part | Not enrolled in the study | |
ctDNA, circulating tumor DNA.
For the primary analysis part, we will administer the protocol treatment, eribulin monotherapy, to 27 individuals in the Full Analysis Set (FAS: all enrolled patients who received at least one dose of eribulin and met eligibility criteria mentioned below) to evaluate its efficacy and safety. For the liquid biopsy part, we will administer the protocol treatment to 15 individuals at the most to evaluate its efficacy and safety. We initiated the patient enrolment in March 2018, completed the primary analysis on May 2019, and are currently continuing with the liquid biopsy analysis (a 12-month follow-up period after the last patient is enrolled). Eribulin at a dose of 1.4 mg/m2 is intravenously administered over 2–5 min on days 1 and 8 of a 3-week cycle. The protocol treatment is repeated until each subject meets any of the discontinuation criteria. We are conducting this study in accordance with the guidelines for Good Clinical Practice of the International Council on Harmonisation of Technical Requirements for Pharmaceuticals for Human Use, as well as with the ethical guidelines for medical and health research involving human subjects. Patients have to provide written informed consent prior to participation.
For the translational research, we have and will collect pretreated tissues and serial blood samples at three time points (before the start of the treatment protocol, on the scheduled start day of cycle 2, and after the discontinuation of the treatment protocol) for biomarker analysis, focusing on gene expressions associated with BRAF mutant-like CRC as a predictive marker, on BRAF mutant allele frequencies in ctDNA for early efficacy detection, and on acquired gene alterations to detect resistance mechanisms to eribulin.
During our study, we will use Guardant360, a liquid biopsy test developed by Guardant Health to identify BRAF V600E mutations for patient screening and to evaluate acquired gene alterations for translational research in blood samples. Guardant360 includes a panel for detecting 74 cancer-associated genomic alterations with ctDNA extracted from blood samples, using a digital sequencing technology that detects single nucleotide variation with a sensitivity of 99.9% and a positive predictive value of 99.6%.14
We registered this study with the University Hospital Medical Information Network.
Patients
Patients with BRAF V600E mutant unresectable CRCs and refractoriness or intolerance to at least one regimen (including irinotecan or oxaliplatin) containing fluoropyrimidine are eligible for inclusion. Additional eligibility criteria are listed in box 1.
Box 1. Eligibility criteria.
Inclusion criteria:
Patients from whom voluntary written informed consent for study participation has been obtained.
Patients 20 years or older at the time of providing informed consent.
Patients with a definitive diagnosis of advanced or metastatic colorectal adenocarcinoma by histological diagnosis.
Patients unresponsive or intolerant to at least one of the chemotherapy regimens with fluoropyrimidines (including irinotecan or oxaliplatin) and with indications for second-line or later-line treatments.
Patients with BRAF V600E mutant colorectal cancer (CRC) diagnosed based on the result of a genetic test with relevant records available.
Patients with a measurable lesion based on the Response Evaluation Criteria in Solid Tumors guideline (V.1.1).
Patients who can provide formalin-fixed, paraffin-embedded specimens of CRC tissues collected before registration in this study.
Patients with Eastern Cooperative Oncology Group Performance Status of 0 or 1.
Patients expected to survive for at least 3 months.
Patients confirmed to have adequate organ function as shown by laboratory data (listed below) obtained within 7 days before registration (a test 7 days before registration, on the same day of the week, is permitted). However, patients who have received blood transfusion or haematopoietic factor products, such as granulocyte colony-stimulating factor products, within 7 days before the test are excluded.
-
Women of child-rearing age who test negative in a urine pregnancy test conducted within 14 days before registration (a test conducted 14 days before registration, on the same day of the week, is permitted). When the urine test indicates a positive result or does not confirm a negative result, a serum pregnancy test will be conducted to confirm a negative result. Both men and women should have agreed to use appropriate contraceptive measures from the day of providing their informed consent and up to 90 days after the last dose of the investigational drug.
Neutrophil count ≥1500/mm3.
Platelet count ≥1 00 000/mm3.
Haemoglobin (Hb) ≥90.0 g/L.
Serum creatinine ≤1.5 mg/dL or calculated or measured creatinine clearance ≥50 mL/min.
T-Bil ≤1.5 mg/dL.
Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) ≤100 IU/L or ≤150 IU/L in the case of liver metastasis.
Resolution of diarrhoea, oral mucositis, peripheral sensory neuropathy, nausea and fatigue, which are adverse events to prior treatments, to grade 1 or below.
Exclusion criteria:
Patients with a history of treatment with eribulin.
Patients with symptomatic brain metastasis or meningeal dissemination.
Patients with leptomeningeal metastasis.
Patients with clinically significant cardiac disease (requiring treatment).
Patients with synchronous or metachronous multiple primary cancer with a disease-free period ≤3 years at registration.
Patients with a history of any of the following therapies:
-
Patients with confirmed HIV infection (those not screened for HIV antibody may register).
Chemotherapy and the last dose of regorafenib received within 14 days before registration.
Cetuximab, panitumumab, bevacizumab, aflibercept, or ramucirumab received within 3 weeks before registration.
Administration of a biological product (excluding cetuximab, panitumumab, bevacizumab, aflibercept and ramucirumab), immunotherapy, or unapproved anticancer drugs within 4 weeks before registration.
Prior radiotherapy targeted to ≥30% of the bone marrow.
Major surgery (excluding minor surgery, such as lymph node biopsy, needle biopsy, or port implantation) within 2 weeks before registration.
Patients with positive HBs antigen.
Patients diagnosed with hepatic cirrhosis.
Pregnant or breastfeeding women.
Patients with other medically significant abnormalities.
Endpoints and assessments
The primary endpoint is confirmed objective response rate (ORR) by investigators’ assessment. The secondary endpoints are PFS, duration of response (DoR), disease control rate (DCR) by investigators’ assessment, overall survival (OS), and incidence of adverse events (AEs). We will evaluate efficacy according to the Response Evaluation Criteria in Solid Tumors (RECIST), V.1.1, using CT scans every 6 weeks plus/minus 1 week for the first three times and every 8 weeks plus/minus 2 weeks from the fourth evaluation onward. We will calculate ORR as the proportion of patients with complete response (CR) or PR. We defined OS as the period from the registration to death from any cause and will censor it at the last day the patient is alive. We defined PFS as the period from the registration to progression or death from any cause and will censor it at the last day when the patient is alive without progression. We defined DoR as the period from the first response to progression or death from any cause and will censor it at the last day when the patient is alive without progression. We will calculate DCR as the proportion of patients with CR, PR, or SD based on RECIST criteria. We will assess AEs according to the Common Terminology Criteria for Adverse Events, V.4.0, before administration of the investigational drug on the administration day. We will assess the same endpoints during the liquid biopsy analysis.
Statistical analysis
Since RR has been reported at 0%–11% after second-line and beyond treatments in patients with BRAF V600E mutant mCRC, we set a threshold ORR at 5%. Therefore, we calculated a sample size for the primary analysis part at 27 (FAS) using an optimal two-stage design15 with ORR of 25% deemed promising and 5% unacceptable (one-sided α, 0.05; β, 0.1), promising DCR at 70%, threshold DCR at 50%, and Yule’s correlation coefficient between ORR and DCR at 0.5. Our planned sample size of the liquid biopsy part is 15 patients at most in an exploratory manner. For the primary analysis cohort, we have planned an interim analysis when the response evaluation for the first 12 patients enrolled becomes available. If we find less than six patients having CR, PR, or SD (ie, the point estimate of DCR by investigators’ assessment is <50%), we plan to discuss on discontinuing the study due to futility; otherwise, we will continue the study. We will confirm the ORR by investigators’ assessment and will estimate its 90% CI using the exact binomial method. We plan to meet the primary endpoint if we observe four or more responder patients (ie, ORR ≥14.8%). For the FAS of the primary analysis part, we will present PFS, DoR and DCR by investigators’ assessment and OS using appropriate statistical methods. We will tabulate the incidences of AEs in the safety population.
Conclusion
The BRAVERY study (EPOC1701) is the first phase II study to evaluate the efficacy and safety of eribulin in patients with BRAF V600E mutant mCRC. We anticipate that our findings will contribute to establishing the efficacy and safety of eribulin in this patient population.
Footnotes
Funding: The investigational drug is to be provided by Eisai. The Japan Agency for Medical Research and Development (AMED) is funding this study (18lk0201065h0002).
Competing interests: TM has received honoraria from Takeda, Chugai, Merck Serono, Taiho, Bayer, Lilly Japan, Yakult Honsha, and Sanofi and has received research funding from Yakult Honsha, MSD, Daiichi Sankyo, and Ono; HT has received honoraria from Takeda, Chugai, Merck Serono, Taiho, Bayer, Lilly Japan, and Yakult Honsha, Sanofi; DK has received honoraria from Takeda, Chugai, Lilly and Merck Serono; HB has received honoraria from Taiho and Eli Lilly Japan and has received research funding from Taiho, Astrazeneca and Sysmex; YK has received honoraria Takeda, Chugai, Bristol-Myers Squibb, Ono, Merck Biopharma, Taiho, Bayer, Lilly, Yakult Honsha, Sanofi, Nipro, Moroo, Asahi Kasei, Mitsubishi Tanabe, Otsuka, Medical Review, and Shiseido and has received research funding from MSD, Daiichi Sankyo, NanoCarrier, Eisai, Sysmex, Shionogi, IQVIA, Parexel International, Astellas, Mediscience, Sumitomo Dainippon, A2 Healthcare, Ono, Taiho, Bayer, Yakult Honsha, and Sanofi, ES has received honoraria from Taiho, Yakult, Chugai, Lilly, Sanofi, Merck bioparm, and Takeda; TEN has received honoraria from Takeda, Chugai, Merck Serono, Taiho, Bayer, Lilly Japan, Sanofi, Kyowa Hakko Kirin, Sawai, Bristol-Myers Squibb Japan, Ono, Dainippon Sumitomo Pharma, MSD, Nippon Kayaku, Celltrion Healthcare Japan, and Teijin and has received research funding from Takeda, Chugai, Merck Serono, Taiho, Lilly Japan, Sanofi, Ono, Dainippon Sumitomo Pharma, MSD, Nippon Kayaku, Eisai, Daiichi Sankyo, A2 Healthcare and Solasia Pharma; TS has received honoraria from Chugai, Merck Serono, Bristol-Myers Squibb, Takeda, Yakult Honsha, Lilly, Bayer Yakuhin, Ono, Merck, Astellas Pharma, Taiho and Nihonkayaku, has received consulting or advisory role from Bayer, Lilly, Ono, Takara Bio, Merck Serono, and Nihonkayaku, and has received research funding from Yakult Honsha, Chugai, Ono, Sanofi, Lilly, Daiichi Sankyo, Merck Serono, Gilead Sciences, and Dainippon Sumitomo; TE has received honoraria from Lilly, Taiho, Bristol-Myers Squibb Japan, Eisai, Daiichi Sankyo, Merck Serono, Chugai, Ono, Takeda, Bayer, and Sanofi and has received research funding from Daiichi Sankyo, Merck Serono, MSD, Novartis, Dainippon Sumitomo, Ono, Astellas Pharma, Lilly, Bayer, Nihonkayaku, Pfizer, and Bristol-Myers Squibb Japan; MW has received honoraria from Chugai and Johnson and Johnson; SN has received honoraria from Taiho and Astrazeneca, AS has received research funding from MSD, Eisai, Ono, Taiho, Takeda, and Bayer, Atsushi Ohtsu has received honoraria from Ono, BMS, Chugai, Taiho, Eisai, and Amgen and has received research funding from Bristol-Myers Squibb and immediate family member of Atsushi Ohtsu have been employed by Celgene, and Takayuki Yoshino has received research funding from Novartis, MSD, Sumitomo Dainippon, Chugai, Sanofi, Daiichi Sankyo, Parexel, Ono, GlaxoSmithKline and Boehringer Ingelheim.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; internally peer reviewed.
Data availability statement: No data are available.
References
- 1.Simmonds PC. Palliative chemotherapy for advanced colorectal cancer: systematic review and meta-analysis. colorectal cancer Collaborative group. BMJ 2000;321:531–5. 10.1136/bmj.321.7260.531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heinemann V, von Weikersthal LF, Decker T, et al. . Folfiri plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment for patients with metastatic colorectal cancer (FIRE-3): a randomised, open-label, phase 3 trial. Lancet Oncol 2014;15:1065–75. 10.1016/S1470-2045(14)70330-4 [DOI] [PubMed] [Google Scholar]
- 3.Yamazaki K, Nagase M, Tamagawa H, et al. . Randomized phase III study of bevacizumab plus FOLFIRI and bevacizumab plus mFOLFOX6 as first-line treatment for patients with metastatic colorectal cancer (WJOG4407G). Ann Oncol 2016;27:1539–46. 10.1093/annonc/mdw206 [DOI] [PubMed] [Google Scholar]
- 4.Pai RK, Jayachandran P, Koong AC, et al. . Braf-Mutated, microsatellite-stable adenocarcinoma of the proximal colon: an aggressive adenocarcinoma with poor survival, mucinous differentiation, and adverse morphologic features. Am J Surg Pathol 2012;36:744–52. 10.1097/PAS.0b013e31824430d7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saridaki Z, Tzardi M, Sfakianaki M, et al. . Brafv600E mutation analysis in patients with metastatic colorectal cancer (mCRC) in daily clinical practice: correlations with clinical characteristics, and its impact on patients' outcome. PLoS One 2013;8:e84604 10.1371/journal.pone.0084604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yokota T, Ura T, Shibata N, et al. . Braf mutation is a powerful prognostic factor in advanced and recurrent colorectal cancer. Br J Cancer 2011;104:856–62. 10.1038/bjc.2011.19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yamazaki K, Yoshino T, Tsuchihara K, et al. . Clinical impact of expanded BRAF mutational status on the outcome for metastatic colorectal cancer patients with anti-EGFR antibody: an analysis of the BREAC trial. J Clin Oncol 2015;33. [Google Scholar]
- 8.Cremolini C, Loupakis F, Antoniotti C, et al. . Folfoxiri plus bevacizumab versus FOLFIRI plus bevacizumab as first-line treatment of patients with metastatic colorectal cancer: updated overall survival and molecular subgroup analyses of the open-label, phase 3 tribe study. Lancet Oncol 2015;16:1306–15. 10.1016/S1470-2045(15)00122-9 [DOI] [PubMed] [Google Scholar]
- 9.Seligmann JF, Fisher D, Smith CG, et al. . Investigating the poor outcomes of BRAF-mutant advanced colorectal cancer: analysis from 2530 patients in randomised clinical trials. Ann Oncol 2017;28:562–8. 10.1093/annonc/mdw645 [DOI] [PubMed] [Google Scholar]
- 10.Karapetis CS, Jonker D, Daneshmand M, et al. . PIK3CA, BRAF, and PTEN status and benefit from cetuximab in the treatment of advanced colorectal cancer--results from NCIC CTG/AGITG CO.17. Clin Cancer Res 2014;20:744–53. 10.1158/1078-0432.CCR-13-0606 [DOI] [PubMed] [Google Scholar]
- 11.Vecchione L, Gambino V, Raaijmakers J, et al. . A vulnerability of a subset of colon cancers with potential clinical utility. Cell 2016;165:317–30. 10.1016/j.cell.2016.02.059 [DOI] [PubMed] [Google Scholar]
- 12.Towle MJ, Salvato KA, Budrow J, et al. . In vitro and in vivo anticancer activities of synthetic macrocyclic ketone analogues of halichondrin B. Cancer Res 2001;61:1013–21. [PubMed] [Google Scholar]
- 13.Masuishi T, Taniguchi H, Sugiyama K, et al. . Eribulin in BRAF V600E-mutant metastatic colorectal cancer: case series and potential rationale. Ann Oncol 2018;29:1330–1. 10.1093/annonc/mdy107 [DOI] [PubMed] [Google Scholar]
- 14.Lanman RB, Mortimer SA, Zill OA, et al. . Analytical and clinical validation of a digital sequencing panel for quantitative, highly accurate evaluation of cell-free circulating tumor DNA. PLoS One 2015;10:e0140712 10.1371/journal.pone.0140712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kunz CU, Wason JM, Kieser M. Two-Stage phase II oncology designs using short-term endpoints for early stopping. Stat Methods Med Res 2017;26:1671–83. 10.1177/0962280215585819 [DOI] [PubMed] [Google Scholar]