Abstract
Background
The popularity of social prescribing has grown in recent years following a series of high-profile recommendations in scientific reviews, political reports, and media coverage. Social prescribing has the potential to address multiple health and social problems, but few studies have examined how it works.
Aim
To explore the ways by which social prescribing may be beneficial to individuals undertaking socially prescribed activity (SPA).
Design and setting
A qualitative interview study involving people attending a range of SPA.
Method
Participants were purposively recruited from a multi-activity social prescribing provider. Data were collected using semi-structured face-to-face interviews. Analysis used a thematic approach, in which emerging themes were contextualised with interview transcripts and findings from existing literature.
Results
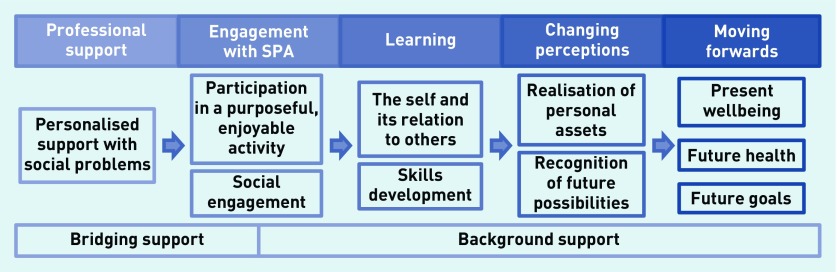
The study identified five themes, which together formed a journey of engagement and participation. While not always present for any one individual, the themes occurred in a consistent order: receiving professional support for social problems; engaging with others through participation in SPA; learning different ways to relate to other people and developing new skills; changing perceptions by realising personal assets and becoming open to the possibility of new futures; and developing a positive outlook on the present while moving forwards in pursuit of future goals and better health.
Conclusion
SPA appears to benefit individuals by a process that begins with personalised professional help to address social problems and moves through engagement with activities and others, to the recognition of personal and social assets and opportunities.
Keywords: community referrals, general practice, health inequalities, qualitative research, social medicine, social prescribing
INTRODUCTION
Social prescribing has been widely recommended as a means of addressing a wide range of illness, distress, and health-related behaviours in individuals and populations.1–10 It is generally understood as the referral of patients, with a variety of social, practical, and emotional needs, from healthcare providers to organisations in the non-statutory or voluntary sector.11,12 As such it provides an adjunct to conventional medical treatment, particularly in primary care.5,6,10,13 Although by no means a new concept,4,14,15 the popularity of social prescribing has grown in recent years following a series of high-profile recommendations in scientific reviews,1,16 government and health reports,5,17–19 and media coverage.
Social prescribing encompasses a broad range of activities, including befriending, welfare benefits advice, promotion of healthy behaviours, group activities, and volunteering.1,20,21 Perhaps unsurprisingly, given the diversity of activities, there is a paucity of quantitative evidence on the effectiveness of social prescribing, and systematic reviews have failed to make definitive conclusions on the objective effectiveness of social prescribing.21–23 However, there are many plausible mechanisms by which social prescribing may be beneficial. These include both the reversal of deficits and the promotion of assets. Deficits addressed include low self-esteem and confidence;9,24–35 poor mental wellbeing and mood;9,24,26–28,30 and anxiety and depression.9,24,26,28,30,33–35 Promotion of personal assets includes increased sociability, communication skills, and social connections;9,24,26–38 and increased motivation for future goals with increased hope, optimism, and meaning to life.9,24–34,36–38
This study aimed to explore the ways by which social prescribing may be beneficial to individuals undertaking socially prescribed activities (SPA).
METHOD
A qualitative study was conducted in which the adults involved in SPA were interviewed to identify how they perceived any benefits from it. Concurrently, a systematic search was carried out for published qualitative data on SPA and the emerging themes and model of the present study were tested against published findings.
Setting, participants, and sampling
All participants were purposively sampled from SOAR (https://soarcommunity.org.uk), a Sheffield-based social prescribing organisation between November 2017 and April 2018. SOAR provides a range of services and acts as a gateway to others. Clients are referred by local healthcare professionals and triaged by telephone or at an initial consultation. Following triage, clients are then signposted to relevant community groups or within the organisation to advocacy, health trainers, and social cafés.
How this fits in
| Social prescribing has been widely recommended as a means of addressing socially determined illness as an adjunct to primary care. Existing qualitative research suggests that socially prescribed activity (SPA) is beneficial for those who engage in it, but how such activity contributes to beneficial outcomes is poorly understood. The study found that people who benefit from social prescribing follow a series of steps from addressing social problems, through social engagement, to recognition of personal assets and opportunities. This work should help providers and commissioners of SPA to deliver social prescription packages that work well for patients. |
Adults attending SOAR were recruited to take part in the study using purposive sampling based on length of engagement, primary reason for referral, and the type of service accessed within the organisation. Recruitment continued to saturation on key themes, defined as two consecutive interviews in which no new major findings appeared. Participants were either invited directly by SOAR employees or approached opportunistically at SOAR social cafés. Individuals who expressed an interest in taking part were contacted by telephone to confirm their willingness to participate, their eligibility regarding the sampling criteria, and to arrange the interview. Participants were provided with a participant information sheet at least 48 hours prior to the interview and provided written consent to participate.
Interviews were mostly conducted one-to-one in rooms within SOAR or quiet public places in the local community. There were three exceptions to this arrangement in which the interviews took place following home visits by SOAR health trainers or advocacy workers.
Two clients were interviewed consecutively, so each was present for the other’s interview and, in a third, a family member was present intermittently.
Data collection
The interviews were semi-structured and followed a topic guide, which was allowed to evolve over the duration of the study to include new items based on ongoing analysis.
Interviews lasted an average of 60 minutes, allowing participants time to describe the trajectory of their health problems and their experience of change through SPA. Interviews were conducted, audio-recorded, and transcribed for analysis.
Analysis
The study was conducted from a realist perspective in which observed (or perceived) outcomes were the result of deeper mechanisms operating within various contexts. An approach based on interpretive phenomenological analysis was used since the study involved participants’ recalled and narrated accounts of their experience participating in SPA. This enabled the authors to hear participants’ lived experience while recognising that as researchers they were interpreting their accounts, and also that those accounts themselves were interpretations of reality.39,40 This approach led the authors more towards understanding processes and experiences than to listing or defining entities such as barriers and facilitators.
Analysis followed a series of stages: initial reading of entire transcripts, thematic coding, secondary coding, and theme generation, and was conducted in an iterative fashion in which newly emerging codes were checked against previous transcripts. All transcripts were read by two authors, while two other authors held weekly meetings at which coding was discussed and revised. The analysis was informed by a systematic search for and reading of published qualitative studies of participants’ experiences of SPA.
Systematic review
Nine databases were searched (MEDLINE via Ovid SP, PubMed, Cochrane Library Reviews, Scopus, Open Grey, CINAHL via EBSCO, ASSIA, Web of Knowledge, and Social Care Online) using four search terms relating to SPA (‘social prescribing’, ‘community referral’, ‘socially prescribed activity’, and ‘non-clinical referral’). Of the 4749 papers identified by the search, 17 papers were identified as evaluating client views of SPA using qualitative methodology. Quotations from clients of SPA services presented within the result sections of these papers were analysed for content and themes using the same methodology as for the interview transcripts.
RESULTS
In total, 17 interviews were conducted: participants were aged between 45 and 84 years; six were male and 11 female; 15 were white British. Participant postcodes indicated that the majority lived in areas of socioeconomic deprivation: nine participants lived in postcodes among the most deprived 10% in the UK and 14 lived in the most deprived 30%. In parallel, through a comprehensive review of the literature, 17 published studies were identified describing qualitative research into clients’ perceptions of social prescribing.9,24–38,41
Participants had begun their involvement in social prescribing for a range of reasons, commonly including adjustment to changing life circumstances and mental health.
They had been attending the social prescribing organisation for between 6 months and 5 years, and had engaged in a wide range of activities, including advocacy (including welfare benefits advice); physical activity (health trainer, exercise, swimming); wellbeing (yoga, walking groups, pain management course); skills (art, craft, modelling, cooking); social (social café, other groups); and volunteering. These data are summarised in Table 1.
Table 1.
Characteristics of SPA referral, activity of interview participants, and participant stage progression
| Pseudonym | Reason for referral | Engagement | Stagesa | Categories of social prescribing activity | |||||
|---|---|---|---|---|---|---|---|---|---|
| Advocacy | Physical | Wellbeing | Social | Creative | Volunteer | ||||
| Robert | Depression and isolation | 11 months | 1–5 | y | y | y | y | ||
| Dawn | Benefits advice | >1 year | 1 | y | |||||
| Amanda | Housing issues | >1 year | 1 | y | |||||
| Sharon | Smoking cessation and health | ∼9 months | 1–3 | y | y | y | y | ||
| Pamela | Exercise and something to do | 6 months | 2–5 | y | y | y | |||
| Linda | Exercise, adjustment to bereavement/retirement | 5 years | 2–5 | y | y | y | y | ||
| Tom | Something to do in winter to support mental health/socialise | >1 year | 2–5 | y | y | y | y | ||
| David | Social isolation and getting out the house | ∼1 year | 2–5 | y | |||||
| Karen | Smoking cessation, lifestyle improvements | >2 years | 1–5 | y | y | y | y | y | y |
| Janet | Something to do/getting out of the house | 3–4 years | 1–5 | y | y | y | y | ||
| Elizabeth | Depression and isolation | <1 year | 2–5 | y | y | y | |||
| Sumayah | Depression, bereavement, and isolation | 2–3 years | 1–5 | y | y | y | y | y | |
| Keith | Isolation and mental health | >1 year | 1–4 | y | |||||
| Susan | Depression and isolation | ∼1 year | 1–5 | y | y | y | y | ||
| Richard | Purposeful occupation post-rehabilitation | ∼3 years | 2–5 | y | y | y | y | y | |
| Tony | Improving health and fitness | >1 year | 1–5 | y | |||||
| Halima | Depression | >1 year | 1–5 | y | y | y | y | y | |
Stage 1 = Client received professional support from a member of the social prescribing team; Stage 2 = Client engaged with others and with socially prescribed activity after self-referral or referral by the social prescribing team; Stage 3 = Client learned new skills and ways of relating to others; Stage 4 = Client changed their perception of themselves and the future; Stage 5= Client began moving forwards towards future goals and better health with improved wellbeing. SPA = socially prescribed activity.
The thematic analysis produced five key themes — receiving professional support for social problems; engaging with others through participation in socially prescribed activity; learning different ways to relate to others and developing new skills; changing perceptions by realising personal assets and becoming open to the possibility of new futures; and developing a positive outlook on the present while moving forwards in pursuit of future goals and better health.
These themes formed a consistent sequence in participants’ accounts, giving insight into a journey from initial referral to progression beyond the service. The sequence of these five key themes and associated underlying sub-themes are summarised in Figure 1.
Figure 1.
Steps to benefit from social prescription. SPA = socially prescribed activity.
Receiving professional support for social problems
For the purpose of this study, professional support includes one-to-one support for welfare or lifestyle-based problems and personalised ‘linking’ to activities by SOAR triage workers, group coordinators, advocacy workers, or health trainers. Clients valued initial support that was personal (friendly and empathetic) and professional (reliable and conscientious):
‘Well, I mean usually you get people turning round and going oh I’ll see to this for you, I’ll see to that for you … and then they don’t do it. Whereas [health trainer] … she’s always done it … like today … she’s done it there and then.’
(Sharon)
As well as their association with successful outcomes and solutions to client problems, positive attributes of professionals enabled clients to engage with another person outside of their usual social circumstances.
For some clients, this acted as a stepping stone from isolation to group social interaction, providing the encouragement, confidence, and motivation they needed to engage with SPA:
‘I actually got first health referral and I didn’t go … ya know when you don’t talk to people and that you can’t make yourself go anywhere on your own. So anyway this time … [health trainer] met me, took me to [sports centre], took me to the gym, took me to meet the [swimming instructors] and … now they’ve given me that confidence, he didn’t have to take me every day, he only had to take me that once and I’m getting round more and more … like I say I’m meeting people in the street now what go to the social café and “How do! All right!” and tha knows I can spend ten, fifteen minutes chatting to them …’
(Robert)
Initial support was typically for practical, social problems, but clients also saw value in sources of support that helped in ‘bridging’ from one-to-one problem solving into more social activities. Thus, clients might not only be referred to SPA from professional support, but also accompanied by a member of the SPA team to their first sessions. Without support in making this step, many clients felt they would have been unable to access SPA and later stages of development:
‘I would never have got here on my own, but when somebody shows you … I can find my own way there … so they brought me a couple of times and now I come myself.’
(David)
Following this bridging, however, participants found it valuable to know that support was still there, in the background, for when it was needed:
‘You just pass your problem on to someone if you’ve got one … I know I can go up to ring [social café coordinator] any time I’ve got a letter or anything I need sorting out and [social café coordinator] will invite me in to sort it like.’
(Karen)
Staff members also provided information about groups, activities, and services in their local area, for clients to access and engage with of their own accord:
‘Oh he helped me a lot. Just with … he used to look like on the computer and everything and if anything came up erm, he thought I would be interested in, he would tell me and then I would like, go and try it.’
(Karen)
Similar themes relating to the role of social prescribing facilitators or ‘link workers’ could be found in existing qualitative studies.30,35
Participant accounts of these individuals are most often incorporated in sub-themes relating to reliability or trust, benefits to client confidence or self-esteem, and a friendly, informal approach to further referrals, in which clients felt in control and experienced a service tailored to them.
Engagement with others during socially prescribed activity
This theme incorporates clients’ engagement with purposeful, enjoyable activities and the forging of new connections with other people.
The activities primarily gave clients ‘something to do’ and provided routine and structure to their time. Several retired participants felt that the activity restored the sense of purpose they had felt in their previous working life:
‘I’ve got the structure for the week … otherwise you’d just veg wouldn’t you … you need a structure.’
(Linda)
Value was also given to the focus, direction, and pleasure that participating provided, as a source of distraction from difficult past and present situations:
‘Yeah it takes your mind away from things … otherwise I would go inwards … I’d go back into my past, which wasn’t good … if I was at home that’s what I would be thinking about … all the horrible things that happened.’
(Elizabeth)
Participants described changing perceptions of what they could do through their activities:
‘I’ve never made anything like that. It was really good and I enjoyed it although I couldn’t do everything, you know because since I had my stroke I’ve no use of my left side … I think for anyone who is on their own and not capable or feels that they’re not capable or that there’s nobody else. Join a social café, because you will be surprised at what you do, you really will.’
(Susan)
‘I mean, that exercise bike I can go on for twenty minutes and when I first went in for my induction I were knackered after two!’
(Tony)
Published studies also include themes pertaining to the value of SPA as a new opportunity that complemented the clients’ normal life as well as an opportunity to reduce social isolation.9,25,33,35 This was often represented by the perception that SPA as ‘something to do’ was beneficial for those retired or unemployed.
In contrast, a number of the interviewees, particularly those with significant responsibility in caring for others, valued SPA as a source of respite. Interacting with others was perceived as a key part of the enjoyable, purposeful nature of the activities as well as contributing to the comfortable nature of the environment.
Learning new skills and ways of relating to other people
As clients continued to engage with activities and other people, they were able to learn and develop socially as well as acquire new creative and practical skills.
They described becoming better able to relate to others in the group through the sharing of past experiences. In turn, this enabled clients to access new perspectives on their own experiences and the relative experiences of others. Reciprocal support networks began to develop within the group and sharing enabled many clients to understand that they were not alone in their difficulties, normalising their situation and reaffirming their place in the community:
‘I’ve met so many nice people and I realised … I’m not just the only person out there … at first I thought “Oh, what am I doing here?”, you know, “I don’t have anything in common with these women.” And I think I looked beyond that and I think I’ve realised how I did fit in, because we all had a story to tell and just slowly made my way back you know, to who I am now.’
(Halima)
‘Yeah, cause they come and talk to you don’t they, and they say to you you’re a nice guy, you’re a good guy, this and that and this and that and it’s totally the opposite from my childhood. You know, growing up like, you know what I mean.’
(Keith)
Clients learned confidence and coping strategies from others to become stronger, more resilient people. Structured opportunities for learning allowed clients to develop skills across variable areas of interest, such as: art, sport, cooking, information technology, support work, and community development. Engaging with one activity or group of people also allowed clients to learn about other opportunities to engage in their community and to broaden their experience:
‘I’ve learnt more now in the last two or three year than I probably did at school … How to interact with people, sit down, listen to people — that’s the main thing you have to do, listen.’
(Richard)
These client experiences were similar to perceptions of learning through SPA described in other research. Various findings outline the development of both personal and practical skills, and the value of shared experiences.25,27,28,33,37
Changing perceptions by realising personal assets and becoming open to the possibility of new futures
Social and personal development facilitated a change in client perceptions of their own assets and future. Improvement and positive reinforcement promoted client confidence, self-esteem, and appreciation of personal strengths, while SPA itself provided opportunities to employ those assets or develop new ones. Some felt that through this process they had developed new identities and that life was more constructive and fulfilling than it had been before. Such transitions promoted increased self-worth and realised potentials, leading to new client goals and ambitions for the future:
‘I don’t want to be retired, my goal is to probably be some kind of support worker … and you don’t need a lot of qualifications if you can get along with people.’
(Richard)
With the support of new social networks, improvements in self-perception enabled clients to become more confident, independent, and resilient despite the challenges they continued to face in everyday life. Improvements in communication and social skills allowed clients to be confident and assertive, and practical, life-based skills contributed to increased resilience and independence:
‘I know now that if there’s a problem I can text [social café coordinator], I can go into the office and say look I’ve got this problem I don’t know how to handle it …’
(Tom)
The learning and development of new skills demonstrated that clients were capable of improving themselves and gave insight into their future potential. These improvements also contributed to increases in confidence, self-esteem, and a positive outlook on new ambitions and opportunities for future development. For others, the purposeful activity provided ‘a reason to get out of bed in the morning’:
‘We did the [taster] course and I had no intention I was gonna do the [community development] course, but I enjoyed the [taster] course so much I decided to do it … it was the course which made me realise how much I miss working life.’
(Halima)
Exposure to other people with similar experiences allowed clients to reflect on their own progression and that of others relative to their own.
Clients shared their experiences with those who had progressed further from comparable situations and in doing so became open to the possibility that their future might also be different or better than the present — in other words, they gained a more hopeful outlook on their present situation. This was reflected in clients’ anticipation of future opportunities both within the group and in life more generally:
‘Well you think you’re the only one in the world and nobody’s gone through it like you, nobody knows about it, but people do and obviously they’re further on … they show you how they cope … They still miss their partners … but they’re coping. And I think oh that might be me in a couple of years’ time … I’m getting there …’
(David)
Again various aspects of this theme could be found within published studies, including ideas of increased confidence, new identities, self-esteem, and sense of purpose — although how these related to other aspects of SPA was not always clear.26,28,33,38
Hope too was a significant feature, and similarities in the process of achieving hope through shared experiences and learning new ways of relating to others are well demonstrated in the following quote from Stickley,33 and the previous quote by David:
‘There’s people doing better than you and there’s people doing worse than you and you’re on some kind of continuum … but I think when you meet people … who also have had problems, it kind of reminds you that you’re not alone and that there’s hope because … you’re all in it together …’ 33
Developing a positive outlook on the present while moving forwards in pursuit of future goals and better health
A sense of hope and recognition of personal assets contributed to client perceptions that life was more enjoyable and fulfilling than it had been previously. Alongside improvements in mental and physical health, this reduced the impact of barriers to goal pursuit and formed a foundation upon which clients could move forwards in pursuit of future goals and better health:
‘Because somebody is actually listening and taking an interest in what you’re saying. They want to know how you went on. You know, they want to know what happened to you, and just as much as you want to know what happened to them! … It’s done me the world of good. It really has, er I feel — I’m not frightened of going out and I’m definitely not frightened of speaking my own mind now either.’
(Susan)
Improvements in confidence, self-esteem, independence, and motivation enabled clients not only to set new goals, but also to actively pursue them. This was also facilitated by hope and optimism for the future, with regard to a client’s potential to succeed:
‘… since I’ve lost weight I feel a lot better in my health so I’ve got to carry on … I don’t want to be in that predicament again … I’ve got a lot of work to do, I’ve got to lose some weight and get healthier, and I’m hoping when we get swimming and things it’ll give me motivation.’
(Pamela)
For some clients, SPA facilitated engagement in health-promoting behaviours such as exercise, smoking cessation, and healthy eating. Clients engaging in exercise-based activities reported positive physical health outcomes such as weight loss and reduced blood pressure. Less formal activities increased client activity by simply ‘getting out of the house’ and were still seen as beneficial in terms of increased mobility and reduced pain.
However, the pursuit of health goals requires a positive perception of both the self and future. Clients perceived health education as a valuable part of SPA, but were unlikely to engage in positive health behaviours without a reasonable degree of self-worth, perceived self-potential, and acceptance of the possibility that the future could be different from the present. Client health outcomes and changed perceptions of the self and future thus contributed to further goals in health improvement:
‘Like I say the first health referral they gave me I thought no, I wanted to kill myself I thought I’m not going, I’m not going to get fit. Like I say, I’ve already explained once I tried to give myself a heart attack. But now I’m going in the opposite direction.’
(Robert)
Sequence of steps
All five stages of the model were present in succession for seven of the seventeen participants. Six participants ‘skipped’ the first stage and self-referred to SPA following recommendations by GPs or other health professionals, as opposed to being ‘linked’ to social activities following a period of one-to-one support. Once engaged with SPA, these clients progressed through the subsequent stages of the model. These clients tended to have a lesser burden of social, medical, and psychological problems when compared with those progressing from the first stage.
Few participants described explicit steps from one stage to another; rather, the sequence was inferred from the narrative arc of interviewee accounts.
Two participants had not progressed beyond initial engagement and advocacy, three participants described only the social café, and the remaining 12 described participation in between two and six activities.
Not all clients progressed from their start point to the final stage. Dawn and Amanda remained at stage 1, Sharon at stage 3, and Keith at stage 4. These clients progressed through fewer stages but retained the common order of succession. These clients also described subsequent stages of the model in aspects of their narrative pertaining to future goals, often describing a clear barrier to their progression to the subsequent stage.
For example, Keith struggled with his sleep and mental health, which day-to-day affected his function and motivation, limiting his ability to find work as a carer as he now aspired to. Although his perception of himself and the future had improved, he remained unable to move forwards into employment for this reason:
‘I only go to the social café cause I’ve got nowt else to — my mind won’t let me do owt else. I wanna go back into care work, you know look after the old ‘uns. I enjoyed that … but I’ve got my own problems to sort out first … you’ve gotta … have your wits about you …’
(Keith)
Sharon was learning new things from her group and interacting more with others. Although she looked forward to future SPA attendance and aspired to attend more groups, she felt unable to change her perception about the future beyond SPA and set new goals because of upcoming surgery:
‘So like I say now I’ve got to have … surgery and they’ve told me it’s going to be more dangerous than the operation I went through last year … It affects me a lot because I just think of my grandson really. I just … I just want to see him grow up … I’ve stopped smoking to try and help me … [health trainer]’s got me into yoga … I’ve just got to get through this operation now.’
(Sharon)
Participants at earlier stages did report improvements in wellbeing as a result of professional support and engagement with the activity, but these improvements appeared to be temporary and not significant enough to facilitate the confidence, hope, and resilience for clients moving forwards without continued support.
DISCUSSION
Summary
People who engaged in SPA described a consistent set of steps that led to perceived benefit. These formed a sequence, from receiving professional support for personally identified problems, through developing new skills and ways of relating to others, to changed perceptions and intentions for the future. This sequence provides a plausible, and inherently social, account of how people in receipt of social prescribing gain benefit.
Strengths and limitations
Although recruitment was from only one centre, SOAR serves a large catchment in a traditional working-class area with high levels of chronic diseases, for which social determinants play a major role. The participants were broadly representative of those attending SOAR, although none were aged <45 years and the majority of participants were white British, despite the wealth of cultural diversity in the local area. At the time of recruitment, participants were engaging in a range of activities but only two were engaged in advocacy work alone, which limited the ability to explore how advocacy relates to some of the broader mechanisms taken from SPA overall. However, several participants had engaged with advocacy services as an initial problem-solving stage, which served as a stepping stone to further engagement and activity in other areas.
The coding process was designed to be rigorous with regular coding meetings of the team and with re-reading of all transcripts after compilation of the initial set of codes to find areas that might be better recoded.
The interviews and analysis were conducted alongside integration of themes from published literature. This may have introduced forms of bias when compared with a complete ‘ground-up’ set of codes; however, it added strength to the findings by anchoring them within other research. No published synthesis of the individual qualitative studies or over-arching model of the mechanisms by which social prescribing may be effective was found. An interest from the outset in concepts of hope and personal assets are a significant part of this study, and were included in both the research questions and topic guide. It is likely that this contributed to an increased proportion of client perceptions relating to these concepts in the results.
Finally, several participants demonstrated a keen awareness of the difficulty community organisations face in securing funding, alongside a relatively pessimistic view of what would happen were the organisation or group to close. This factor may have led to exaggerated accounts as to how beneficial the service had been for participants.
Comparison with existing literature
Each of the key themes is mirrored in published research about social prescribing and this is described in each thematic section of the results. However, none of these studies includes all of the themes identified within the present study, and none identifies a sequence of steps. This research thus extends knowledge about the ways by which social prescribing is likely to be beneficial.
Implications for research and practice
There are two important implications from the present research. The first is that this study has outlined a plausible sequence of processes by which people engaging in SPA gain benefit. This can be used to inform services and those who commission them. The second is an emphasis on the social components of social prescribing. The processes outlined here are inherently social, relating to the interactions of individuals rather than the individuals themselves.
Together, these mean that GPs and commissioners need to be aware of the essential interpersonal, or social, components of social prescribing. This has three implications for delivering social prescribing at scale.
First is the importance of work to engage individuals, many of whom are quite socially disengaged. For such people this goes well beyond simple signposting.
Second, despite the present study’s finding of a sequence of processes, participants provided highly individual accounts: there is a danger in trying to standardise services that this will be lost. Social interaction — through which benefit seems to accrue — cannot be protocolised or tightly managed.
Third, a focus on ‘downstream’ targets such as healthier behaviour or return to work may miss important improvements in living well, which participants of the present study described. A focus on these would run the risk of pushing people away rather than letting them develop at their own pace or to their own level.
In terms of further research, although the study has proposed a sequence of processes, this needs to be tested in further work, preferably over longer timescales and following individuals prospectively, in order to gain fuller understanding of the mechanisms by which social prescribing works.
For the moment, research should build on this work by describing and delineating the mechanisms by which social prescribing is beneficial. Social prescribing appears to benefit patients in a series of steps from professional engagement and support dealing with personal problems, through wider social engagement, to identification of personal and social assets and opportunities. These steps provide a useful framework with which to develop and evaluate social prescribing services.
Acknowledgments
We wish to thank staff and service users of SOAR for their support of this study.
Funding
No external funding was used for this study.
Ethical approval
Ethical approval for the study was obtained from the University of Sheffield Ethics Committee (reference number: 016163).
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Discuss this article
Contribute and read comments about this article: bjgp.org/letters
REFERENCES
- 1.Thomson LJ, Camic PM, Chatterjee HJ. Social prescribing A review of community referral schemes. University College London: Canterbury Christ Church University; 2015. http://www.artshealthresources.org.uk/wp-content/uploads/2017/01/2015-Thompson-Social_Prescribing_Review.pdf (accessed 18 Oct 2019) [Google Scholar]
- 2.Friedli L, Jackson C, Abernethy H, Stansfield J. Social prescribing for mental health — a guide to commissioning and delivery. 2008. Care Services Improvement Partnership, North West Development Centre, Hyde. https://www.centreforwelfarereform.org/uploads/attachment/339/social-prescribing-for-mental-health.pdf (accessed 28 Oct 2019)
- 3.Woodall J, South J. The evaluation of the CHAT social prescribing scheme in Bradford South & West PCT. Leeds Metropolitan University; 2005. [Google Scholar]
- 4.Grant C, Goodenough T, Harvey I, Hine C. A randomised controlled trial and economic evaluation of a referrals facilitator between primary care and the voluntary sector. BMJ. 2000;320(7232):419–423. doi: 10.1136/bmj.320.7232.419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Royal College of General Practitioners Spotlight on the 10 high impact actions. 2018 http://www.rcgp.org.uk/policy/general-practice-forward-view/spotlight-on-the-10-high-impact-actions.aspx (accessed 18 Oct 2019) [Google Scholar]
- 6.Popay J, Kowarzik U, Mallinson S, et al. Social problems, primary care and pathways to help and support: addressing health inequalities at the individual level. Part II: lay perspectives. J Epidemiol Community Health. 2007;61(11):972–977. doi: 10.1136/jech.2007.061945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Roy MJ, Donaldson C, Baker R, Kerr S. The potential of social enterprise to enhance health and well-being: a model and systematic review. Soc Sci Med. 2014;123:182–193. doi: 10.1016/j.socscimed.2014.07.031. [DOI] [PubMed] [Google Scholar]
- 8.Mossabir R, Morris R, Kennedy A, et al. A scoping review to understand the effectiveness of linking schemes from healthcare providers to community resources to improve the health and well-being of people with long-term conditions. Health Soc Care Community. 2015;23(5):467–484. doi: 10.111/hsc.12176.. [DOI] [PubMed] [Google Scholar]
- 9.Dayson C, Bashir N. The social and economic impact of the Rotherham Social Prescribing Pilot: main evaluation report. Sheffield Hallam University; 2014. https://www4.shu.ac.uk/research/cresr/sites/shu.ac.uk/files/social-economic-impact-rotherham.pdf (accessed 18 Oct 2019) [Google Scholar]
- 10.Cawston P. Social prescribing in very deprived areas. Br J Gen Pract. 2011. [DOI] [PMC free article] [PubMed]
- 11.Brandling J, House W. Social prescribing in general practice: adding meaning to medicine. Br J Gen Pract. 2009. [DOI] [PMC free article] [PubMed]
- 12.Brandling J, House W. Investigation into the feasibility of a social prescribing service in primary care: a pilot project. University of Bath, Bath and North East Somerset NHS Primary Care Trust; 2007. https://purehost.bath.ac.uk/ws/portalfiles/portal/426828 (accessed 18 Oct 2019) [Google Scholar]
- 13.South J, Higgins TJ, Woodall J, White SM. Can social prescribing provide the missing link? Prim Health Care Res Dev. 2008;9(4):310. [Google Scholar]
- 14.Graham N. GPs and voluntary organizations. Br J Gen Pract. 1995;45(394):272–273. [Google Scholar]
- 15.Abbott S. Prescribing welfare benefits advice in primary care: is it a health intervention, and if so, what sort? J Public Health Med. 2002;24(4):307–312. doi: 10.1093/pubmed/24.4.307. [DOI] [PubMed] [Google Scholar]
- 16.Daly S, Allen J. Voluntary sector action on the social determinants of health. University College London Institute of Health Equity; 2017. http://www.instituteofhealthequity.org/resources-reports/voluntary-sector-action-on-the-social-determinants-of-health/voluntary-sector-action-on-the-sdoh-evidence-review.pdf (accessed 18 Oct 2019) [Google Scholar]
- 17.Department of Health and Social Care Healthy lives, healthy people: our strategy for public health in England. 2010. https://www.gov.uk/government/publications/healthy-lives-healthy-people-our-strategy-for-public-health-in-england (accessed 18 Oct 2019)
- 18.NHS England Universal personalised care. Implementing the comprehensive model. Version 1. 2019. https://www.england.nhs.uk/wp-content/uploads/2019/01/universal-personalised-care.pdf (accessed 18 Oct 2019)
- 19.NHS England The NHS Long Term Plan. 2019 https://www.longtermplan.nhs.uk/wp-content/uploads/2019/01/nhs-long-term-plan.pdf (accessed 18 Oct 2019) [Google Scholar]
- 20.Kinsella S. Social prescribing: a review of the evidence. Wirral Council Business & Public Health Intelligence Team; 2015. https://www.wirralintelligenceservice.org/media/1077/social-prescribing-literature-review-v5.pdf (accessed 18 Oct 2019) [Google Scholar]
- 21.Bickerdike L, Booth A, Wilson PM, et al. Social prescribing: less rhetoric and more reality. A systematic review of the evidence. BMJ Open. 2017;7(4):e013384. doi: 10.1136/bmjopen-2016-013384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kilgarriff-Foster A, O’Cathain A. Exploring the components and impact of social prescribing. J Public Ment Health. 2015;14(3):127–134. [Google Scholar]
- 23.University of York Centre for Reviews and Dissemination Evidence to inform the commissioning of social prescribing. 2015. https://www.york.ac.uk/media/crd/Evbriefing_social_prescribing.pdf (accessed 18 Oct 2019)
- 24.Barley EA, Robinson S, Sikorski J. Primary-care based participatory rehabilitation: users’ views of a horticultural and arts project. Br J Gen Pract. 2012. [DOI] [PMC free article] [PubMed]
- 25.Carnes D, Sohanpal R, Frostick C, et al. The impact of a social prescribing service on patients in primary care: a mixed methods evaluation. BMC Health Serv Res. 2017;17(1):835. doi: 10.1186/s12913-017-2778-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Makin S, Gask L. ‘Getting back to normal’: the added value of an art-based programme in promoting ‘recovery’ for common but chronic mental health problems. Chronic Illn. 2012;8(1):64–75. doi: 10.1177/1742395311422613. [DOI] [PubMed] [Google Scholar]
- 27.Todd C, Camic PM, Lockyer B, et al. Museum-based programs for socially isolated older adults: understanding what works. Health Place. 2017;48:47–55. doi: 10.1016/j.healthplace.2017.08.005. [DOI] [PubMed] [Google Scholar]
- 28.Abbotts J, Spence W. Art and wellbeing in a deprived Scottish community. J Public Ment Health. 2013;12(2):58–69. [Google Scholar]
- 29.Howarth ML, McQuarrie C, Withnell N, et al. The influence of therapeutic horticulture on social integration. J Public Ment Health. 2016;15(3):136–140. [Google Scholar]
- 30.Moffatt S, Steer M, Lawson S, et al. Link worker social prescribing to improve health and well-being for people with long-term conditions: qualitative study of service user perceptions. BMJ Open. 2017;7(7):e015203. doi: 10.1136/bmjopen-2016-015203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Morton L, Ferguson M, Baty F. Improving wellbeing and self-efficacy by social prescription. Public Health. 2015;129(3):286–289. doi: 10.1016/j.puhe.2014.12.011. [DOI] [PubMed] [Google Scholar]
- 32.Stickley T, Hui A, Souter G, Mills D. A community arts programme for older people: an evaluation. Mental Health and Social Inclusion. 2016;20(1):22–28. [Google Scholar]
- 33.Stickley T, Hui A. Social prescribing through arts on prescription in a U.K. city: participants’ perspectives (part 1) Public Health. 2012;126(7):574–579. doi: 10.1016/j.puhe.2012.04.002. [DOI] [PubMed] [Google Scholar]
- 34.Vogelpoel N, Jarrold K. Social prescription and the role of participatory arts programmes for older people with sensory impairments. J Integr Care. 2014;22(2):39–50. [Google Scholar]
- 35.White JM. Social prescribing: the perspectives of service users, providers and prescribers. Glasgow Caledonian University; 2012. Online thesis. http://ethos.bl.uk/OrderDetails.do?uin=uk.bl.ethos.570733 (accessed 18 Oct 2019) [Google Scholar]
- 36.Blickem C, Kennedy A, Vassilev I, et al. Linking people with long-term health conditions to healthy community activities: development of Patient-Led Assessment for Network Support (PLANS) Health Expect. 2013;16(3):e48–e59. doi: 10.1111/hex.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Greenwood N, Smith R, Akhtar F, Richardson A. A qualitative study of carers’ experiences of dementia cafés: a place to feel supported and be yourself. BMC Geriatr. 2017;17(1):164. doi: 10.1186/s12877-017-0559-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Stickley T, Eades M. Arts on prescription: a qualitative outcomes study. Public Health. 2013;127(8):727–734. doi: 10.1016/j.puhe.2013.05.001. [DOI] [PubMed] [Google Scholar]
- 39.Brocki JM, Wearden AJ. A critical evaluation of the use of interpretative phenomenological analysis (IPA) in health psychology. Psychology and Health. 2006;21(1):87–108. [Google Scholar]
- 40.Carmichael M. Successful qualitative research: a practical guide for beginners. Thousand Oaks, CA: Sage Publications; 2013. [Google Scholar]
- 41.Kimberlee R. What is the value of social prescribing? Advances in Social Sciences Research Journal. 2016;3(3):29–35. [Google Scholar]