Abstract
I.V. fluid therapy plays a fundamental role in the management of hospitalized patients. While the correct use of i.v. fluids can be lifesaving, recent literature demonstrates that fluid therapy is not without risks. Indeed, the use of certain types and volumes of fluid can increase the risk of harm, and even death, in some patient groups. Data from a recent audit show us that the inappropriate use of fluids may occur in up to 20% of patients receiving fluid therapy. The delegates of the 12th Acute Dialysis Quality Initiative (ADQI) Conference sought to obtain consensus on the use of i.v. fluids with the aim of producing guidance for their use. In this article, we review a recently proposed model for fluid therapy in severe sepsis and propose a framework by which it could be adopted for use in most situations where fluid management is required. Considering the dose–effect relationship and side-effects of fluids, fluid therapy should be regarded similar to other drug therapy with specific indications and tailored recommendations for the type and dose of fluid. By emphasizing the necessity to individualize fluid therapy, we hope to reduce the risk to our patients and improve their outcome.
Keywords: adults, critical care, fluid therapy, resuscitation
I.V. fluid therapy plays a vital role in establishing and maintaining cellular homeostasis in hospitalized patients. I.V. fluid administration is one of the most frequently used therapies provided in hospitals. The most common indications for fluid bolus therapy in critically ill patients include the management of severe hypovolaemia, sepsis, perioperative correction of large volume losses, and haemodynamic alterations, oliguria, or both that is believed to be volume responsive.
When used appropriately i.v. fluids can obviously improve outcomes.1 However, in view of the physiological complexity of the considerations underpinning the use of fluid resuscitation, many physicians prescribing fluid therapy appear to lack appropriate expertise or an appreciation for its potential to cause harm. This concern was highlighted in ‘Knowing the Risk, a review of the perioperative care of surgical patients’, reported in 2011 by the National Confidential Enquiry into Patient Outcome and Death in the UK (http://www.ncepod. org.uk/2011report2/downloads/POC_fullreport.pdf). This report found inappropriate fluid therapy, although rarely reported, may occur in as many as one in five patients. The inappropriate use of i.v. fluids ranges from inadequate resuscitation or rehydration leading to tissue hypoperfusion to excessive fluid infusion leading to tissue oedema and severe electrolyte derangement. This results in high levels of morbidity, prolongation of hospitalization, and even excess mortality. Adverse effects of i.v. infusions include fluid overload, organ damage or failure (to the lungs, brain, and kidneys), hyponatraemia and hypernatraemia, hyperchloraemic metabolic acidosis because of excess chloride administration, coagulation abnormalities, increased need for transfusion with blood products, and increased fatalities with certain solutions.2–7 For this reason, it has been recommended that the use of fluid therapy should be accorded similar status as drug prescribing.8,9 Current evidence teaches us that similar to other drugs, the adverse effects of fluids are dependent on the type and dose of fluid administered and the specific context in which they are given. For instance, the 6S study found a higher mortality and incidence of acute kidney injury (AKI) in patients with severe sepsis who received hydroxyethylstarch solutions compared with the carrier solution of Ringer’s acetate.5 Also, in a subanalysis of the SAFE study, there was a higher mortality rate in patients with traumatic brain injury who were treated with albumin solutions.10 As such, fluids should be considered as any other drug, with specific indications and contraindications. The type of fluid, rate of fluid administration, and dose should also be carefully considered.9,11
Given these considerations, the steering committee of the 12th Acute Dialysis Quality Initiative (ADQI) conference dedicated a workgroup with the task of considering when and how fluids should be administered for resuscitation in critically ill patients. More specifically, the working group was asked to address three questions:
-
(i)
To define the goals of i.v. fluid therapy.
-
(ii)
To identify the monitors of fluid need and effect (including traditional and novel devices).
-
(iii)
To identify fluid therapy in different contexts, for example, the pre-hospital setting or emergency room, in the operating theatre, and in the intensive care unit.
These questions served as a starting point for a consensus statement.
Methods
For the specific methodology used in this ADQI conference, we refer readers to the introductory article accompanying this paper in the current issue of the Journal.12 Before the start of the conference, the working group discussed the proposed questions by electronic mail and subsequently identified and shared the relevant literature on which to base discussion and eventual consensus. A formal systematic review was not conducted.
Results
The use of fluid resuscitation therapy is not dependent on a specific location of the patient in or outside of the hospital, but rather on the indication for fluid therapy [for instance, a patient with septic shock will be administered a similar fluid resuscitation regime in the emergency department and the intensive care unit (ICU)].13 Also, many different endpoints and methods of achieving those endpoints have been described, frequently describing differing therapies using the same terminology.
The workgroup appreciated that the answer to the questions posed would depend on the clinical context, the environment, and the endpoints that are used in individual research studies. This was recently demonstrated in the Fluid Expansion as Supportive Therapy study, where children on admission to hospital in Africa with severe infection were randomized to receive no fluid boluses (control, standard of care), or to receive fluid boluses with either saline (NaCl 0.9%) or albumin.14 At 1 h, more patientswho received fluid boluses demonstrated reversal of shock compared with patients who did not receive a fluid bolus. However, when 48 h mortality was evaluated, patients who received fluid boluses had higher mortality compared with control patients (relative risk 1.45, 95% confidence interval 1.13–1.86, P=0.003).15 This trial was conducted in resource poor hospitals with no access to ventilation to optimize the management of sepsis and similar conditions in this setting.
The group felt that greater clarity was required in the terminology used to describe fluid therapy and sought to obtain consensus on a set of definitions that could be applied across a wide variety of clinical situations where fluids are administered. The focus centred on the escalation and de-escalation of resuscitation fluids, and did not specifically cover the use of maintenance fluids and electrolyte therapy (type/indication/rates) in any depth.
Definitions
The workgroup defined the terminology relevant for the topic of fluid administration, which captured (i) time-dependent, phase of illness, or both (Box 1) and (ii) rate and volume of fluid administration (Box 2). The timeor phase-dependent variables in fluid management largely drew on the recent review by one of the workgroup members (J.-L.V.).16 The lexicon describing volume–rate-dependent variables was considered to be less clearly standardized in the literature, so group members agreed both to draw on existing definitions (referenced in Box 2) and to define, by consensus, appropriate terms that encompassed modes of, indications for, fluid administration, or both.
Box 1. Time-dependent considerations.
Resuscitation: administration of fluid for immediate management of life-threatening conditions associated with impaired tissue perfusion
Titration: adjustment of fluid type, rate and amount based upon context to achieve optimization of tissue perfusion
De-escalation: minimization of fluid administration; mobilization of extra fluid to optimize fluid balance
Box 2. Terminology.
Fluid bolus: a rapid infusion to correct hypotensive shock. It typically includes the infusion of at least 500 ml over a maximum of 15 min
Fluid challenge: 100–200 ml over 5–10 min with reassessment to optimize tissue perfusion17
Fluid infusion: continuous delivery of i.v. fluids to maintain homeostasis, replace losses, or prevent organ injury (e.g. prehydration before operation or for contrast nephropathy)
Maintenance: fluid administration for the provision of fluids for patients who cannot meet their needs by oral route. This should be titrated to patient need and context and should include replacement of ongoing losses. In a patient without ongoing losses, this should probably be no more than 1–2 ml kg−1h−1
Daily fluid balance: daily sum of all intakes and outputs
Cumulative fluid balance: sum total of fluid accumulation over a set period of time18
Fluid overload: cumulative fluid balance expressed as a proportion of baseline body weight. A value of 10% is associated with adverse outcomes19
The workgroup elected not to consider fluid resuscitation/administration for children (<16 yr), pregnant women, burns patients, and patients with acute shock who have chronic conditions (chronic renal failure, hepatic failure, diabetic ketoacidosis, and hyperosmolar states). Even though we recognize its importance, we decided not to discuss the process of administration of fluids, for example, what route of administration, type of catheters, or pumps should be used.
The workgroup recommends that fluid therapy should be tailored to the specific indications and the context of the patient. We therefore proposed to consider and reflect upon the concept of ‘Fit for Purpose Fluid Therapy’ (Table 1).
Table 1.
Characteristics of different stages of resuscitation: ‘Fit for purpose fluid therapy’. GDT, goal directed therapy; DKA, diabetic keto acidosis PO, nil per os; ATN, acute tubular necrosis; SSC, surviving sepsis campaign
| Rescue | Optimization | Stabilization | De-escalation | |
|---|---|---|---|---|
| Principles | Lifesaving | Organ rescue | Organ support | Organ recovery |
| Goals | Correct Shock | Optimize and maintain tissue perfusion | Aim for zero or negative fluid balance | Mobilize fluid accumulated |
| Time (usual) | Minutes | Hours | Days | Days to weeks |
| Phenotype | Severe shock | Unstable | Stable | Recovering |
| Fluid therapy | Rapid boluses | Titrate fluid infusion conservative use of fluid challenges | Minimal maintenance infusion only if Oral intake inadequate | Oral intake if possible possible Avoid unnecessary i.v. fluids |
| Typical clinical scenario | - Septic shock - Major trauma |
- Intraoperative GDT - Burns - DKA |
- NPO postoperative patient - ‘Drip and suck’ management of pancreatitis |
- Patient on full enteral feed in recovery phase of critical illness - Recovering ATN trauma |
| Amount | Guidelines, for example, SSC, pre-hospital resuscitation, trauma, burns, etc. | |||
Stages of fluid therapy
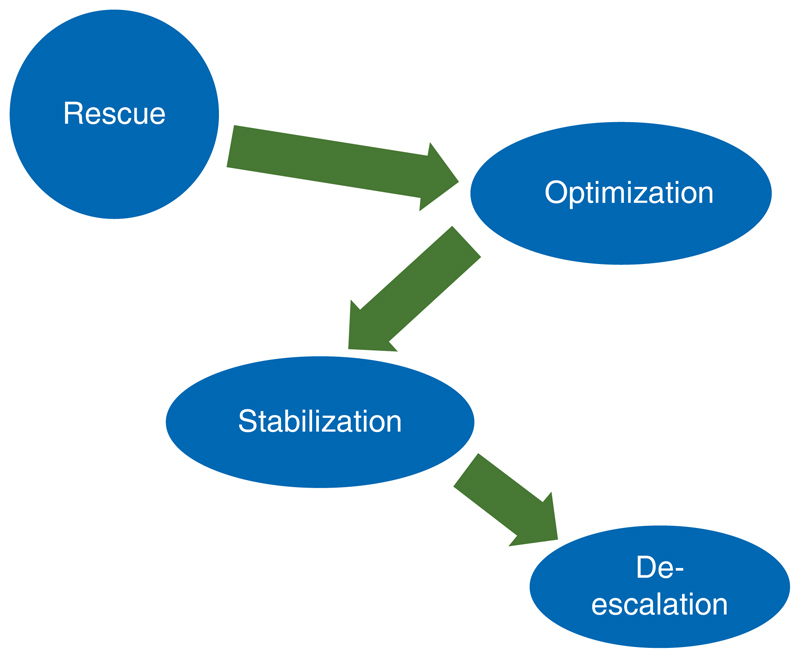
The framework recently proposed by Vincent and De Backer16 recognizes four distinct phases or stages of resuscitation: Rescue, Optimization, Stabilization, and De-escalation (ROS-D) (Table 1 and Fig. 1). Logically, these describe the four different clinical phases of fluid therapy, occurring over a timecourse in which patients experience a decreasing severity of illness.
Fig 1. Relationship between the different stages of fluid resuscitation.
Reproduced with permission from ADQI (www.ADQI.org).
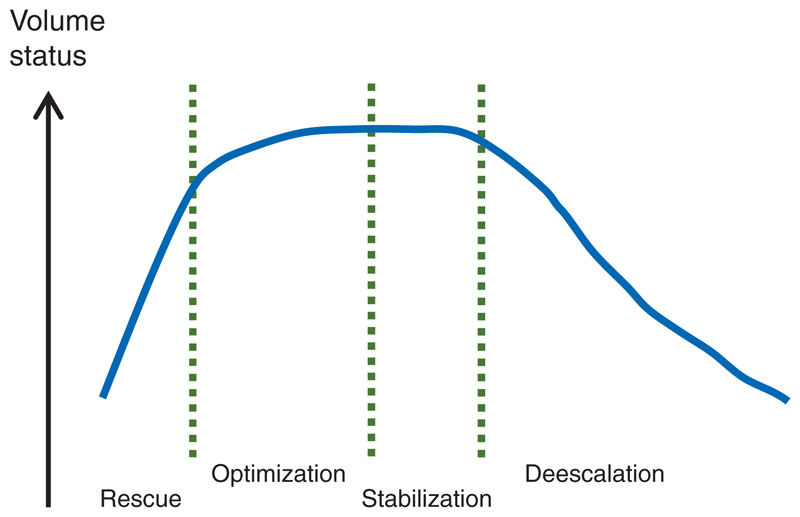
The Rescue phase anticipates an immediate escalation of fluid therapy, for resuscitation of the patient with life-threatening shock (characterized by low arterial pressure, signs of impaired perfusion, or both), and characterized by the use of fluid bolus therapy (see Box 2). In Optimization, the patient is no longer in immediate life-threatening danger but is in a stage of compensated shock (but at high risk of decompensation) and any additional fluid therapy is given more cautiously, and titrated with the aim of optimizing cardiac function to improve tissue perfusion with ultimate goal of mitigating organ dysfunction. The workgroup felt strongly that a clear distinction had to be made between a ‘fluid bolus’, that is, large volume given rapidly to rescue, without close monitoring, and a ‘fluid challenge’ (see Box 2 for definition) which was considered as a test where the effects of a more modest volume given more slowly are assessed, in order to prevent inadvertent fluid overload (also defined in Box 2). Stabilization reflects the point at which a patient is in a steady state so that fluid therapy is now only used for ongoing maintenance either in setting of normal fluid losses (i.e. renal, gastrointestinal, insensible), but this could also be fluid infusion (including rehydration) if the patient was experiencing ongoing losses because of unresolved pathology. However, this stage is distinguished from the prior two by the absence of shock (compensated or uncompensated) or the imminent threat of shock. Finally, while in the first three stages (‘SOS’), fluids are usually administered, in the last stage (D), fluids will also be removed from the patient and usually, the goal will be to promote a negative fluid balance (Fig. 2).
Fig 2. Patients’ volume status at different stages of resuscitation.
Reproduced with permission from ADQI (www.ADQI.org).
Typically, most patients requiring fluid resuscitation will enter this conceptual framework in the Rescue phase (Fig. 1). However, some may enter at the Optimization phase, as they do not have hypotension and they are either in a compensated state or are at imminent risk for shock, where fluid challenges rather than fluid boluses are the initial management. All patients will then proceed to Stabilization and De-escalation as their clinical condition improves, and the prioritization for fluid management now switches to prevention of its adverse effects. The group recognized that this is a dynamic process where patients may experience temporary deterioration, for example, as a consequence of a severe infection, necessitating switching from a Stabilization strategy back to Optimization. Less often, the clinical condition is again life threatening, for example, as a consequence of septic or haemorrhagic shock, moving the patient back into the Rescue phase.
Monitoring and reassessment
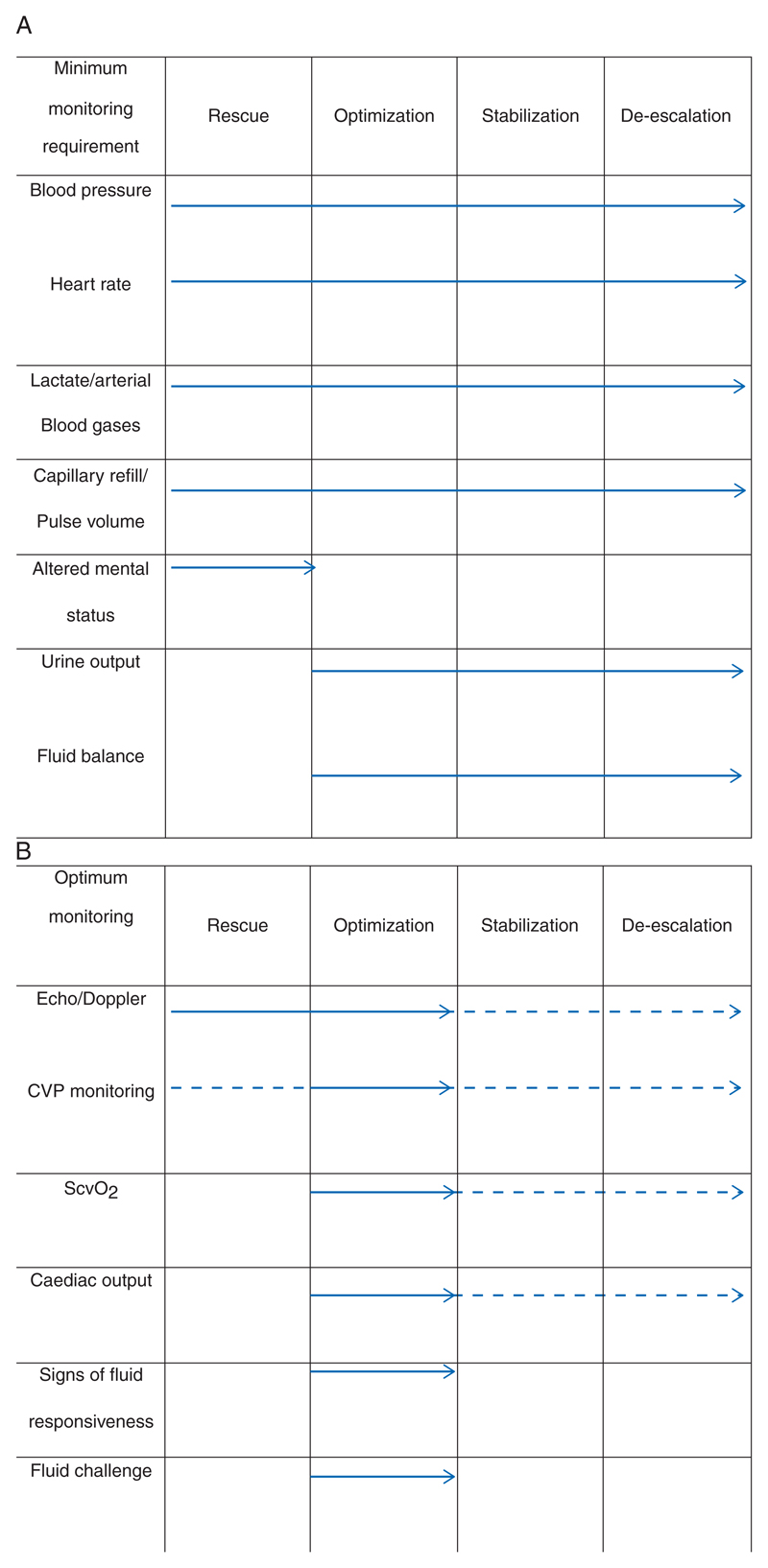
A most important aspect of this new conceptual framework for fluid therapy is the individual assessment of the patient’s fluid requirements, the timely administration of that fluid, and then the frequent re-assessment of response and ongoing needs. All too often, the ‘recipe’ fluid therapy that is ‘one size (dose) fits all’ is chosen for reasons of convenience or possibly because clinicians do not actually think about why they are giving fluids in the first place. While daily fluid and electrolyte requirements can be reasonably well estimated for the average person, it is becoming more apparent that patients, and certainly seriously ill patients, are not ‘average’ and have widely varying and individual requirements. To enable the clinician to assess fluid requirements, we propose a minimum and desirable monitoring set at each stage of fluid therapy (Fig. 3A and B).
Fig 3. Assessment of fluid requirements.
Reproduced with permission from ADQI (www.ADQI.org). (a) Minimum monitoring set at each stage of fluid therapy. (b) Desirable monitoring set at each stage of fluid therapy.
In the Rescue phase, initial management should be initiated using a combination of clinical and haemodynamic parameters together with near-patient diagnostics and without need for sophisticated initial assessment such as echocardiography (Fig. 3A). In this phase, reassessment and re-challenge should be performed without the clinician leaving the bedside; it requires constant observation of the patient’s haemodynamic situation in order to prevent life-threatening over- or under-treatment. Once fluid boluses have been given and the clinician has determined that the patient has been ‘rescued’, additional patient-centred data obtained by monitoring responses by Echo/Doppler, CVP, and/or SCVO2 catheters to provide additional goal-directed endpoints for further management (Fig. 3B) can beused. These additional parameters will help determine the appropriate time to transition from Rescue to Optimization.
In the Optimization phase, the emphasis of fluid therapy moves away from saving the life of the patient to ensuring adequate blood and therefore oxygen delivery to at-risk organs. The aim in this phase is to prevent subsequent organ dysfunction and failure because of both hypoperfusion and tissue oedema.
In the Stabilization and De-escalation phase, in contrast to the Rescue and Optimization phase, the patient may only need to be seen once every few hours with the clinician either prescribing i.v. fluids (or potentially diuretics if there is evidence of symptomatic volume overload) on the basis of physical examination, blood chemistry, and the likely clinical course (Fig. 3B).
Discussion
Stages of fluid therapy: relevance to clinical trials
Several trials in recent years have examined the effect of different compositions of i.v. fluids in varying scenarios. Identifying the stage of fluid resuscitation in which these trials were conducted may affect the way they are interpreted. The FIRST trial described a group of patients undergoing resuscitation after major trauma.20 These patients were severely injured with high injury severity scores and significantly elevated plasma lactate levels. The patients required in excess of 5 litre of i.v. fluid within the first 24 h demonstrating that this trial took part in the Rescue phase of resuscitation. Similarly, the CRISTAL trial enrolled severely hypotensive septic patients who required very large volumes of fluid—again demonstrating a ‘Rescue Trial’.21
In contrast, when we examine the baseline characteristics of the large SAFE and CHEST studies, which both included ∼7000 ICU patients, most patients were not, at the point of entry into the trial, in the Rescue phase.6,22 These patients were more commonly (at the point of ICU admission) in either the Optimization phase of resuscitation as evidenced by the significantly lower volumes of fluid administered and longer time from presentation to enrolment. In a similar vein, the majority of trials in the perioperative fluid therapy have generally been conducted within the Optimization phase.
Fluid resuscitation in the perioperative period
One particular subgroup of patients is those receiving fluids in the perioperative setting (typically in the Optimization phase). In this category, several clinical trials (and indeed metaanalyses and systematic reviews) have demonstrated the benefit of using minimally invasive monitors of fluid responsiveness to guide goal-directed fluid therapy in order to optimize tissue oxygen delivery.23–33 However, this evidence may need to be reconsidered, as the respiratory conditions used in these studies may have been suboptimal. A recent large study found that in patients at risk for pulmonary complications who underwent major abdominal surgery, a lungprotective (low tidal volume) ventilation strategy during the operation resulted in less pulmonary and extra-pulmonary complications within the first week after surgery compared with a non-protective mechanical ventilation.34 This change in ventilation management with lower tidal volumes will lead to a reduction in changes in intra-thoracic pressure during the respiratory cycle and a subsequent decrease in variation in venous return and resulting stroke volume/systolic pressure.
Fluid therapy for the prevention of organ damage in specific cohorts
Fluid may also be administered to patients without significant, or even any, fluid losses. For example, fluid may be given for the prevention of organ damage, for example, before contrast administration, in cirrhotic patients with spontaneous bacterial peritonitis, or maintenance fluid administration in patients who cannot tolerate oral fluid intake. In these situations, fluid infusions are generally utilized; however, the amount and type of fluid may vary. Consensus guidelines for preventing contrast nephropathy recommend using crystalloids (saline or bicarbonate-based solutions) at rates of 1–1.5 ml kg−1 h−1 for 12 h before and 12 h after the contrast procedure.35,36 These recommendations are based on achieving urine volumes >150 ml h−1 as these levels have been associated with decreased risk for AKI. For emergent cases, when a 12 h prehydration regimen is not possible, 3 ml kg−1 h−1 is recommended for 1 h before and continued for 6 h after the procedure.37 In contrast, in cirrhotic patients, albumin solutions are preferred to manage spontaneous bacterial peritonitis and to reduce the effects of large-volume paracentesis.38 It should be emphasized that fluid management (fluid infusion: see Box 2) in these cases is designed to optimize tissue perfusion and reduce risk for organ toxicity; however, it needs to be carefully titrated based on underlying co-morbidities, particularly decreased renal function and heart failure. Appropriate deescalation of fluids and fluid mobilization are equally important in these situations to prevent the cumulative effect of fluid administration during the patient’s hospital course. Maintenance fluids given for patients who cannot tolerate oral fluids or who are awaiting surgical or radiological procedures are similarly subject to wide variation. Underlying co-morbidities including diabetes and chronic kidney disease often dictate the amount and type of fluid used. We recommend that underlying co-morbidities should be considered in the same context of ‘fit for purpose’ to individualize maintenance fluid therapy with careful monitoring to prevent fluid accumulation.
Conclusions
I.V. fluid therapy can be lifesaving but like all medical interventions carries with it a degree of risk. The aims of the workgroup were to define ‘Fit for purpose fluid therapy’ tailored to the specific indications, time-, phase-dependent variables, or both, and the context of the patient. We created a conceptual framework on which future guidelines or research could be modelled and expanded. The group aimed to move away from a ‘one size fits all’ approach for the early phases of fluid therapy (introducing a distinction between a fluid bolus and that of a fluid challenge), towards a bespoke, carefully managed approach in order to optimize patient outcome.
Supplementary Material
Supplementary material is available at British Journal of Anaesthesia online.
Editor’s key points.
The authors explore the risks of i.v. fluid therapy, explaining that up to 20% of patients receiving i.v. fluid may be subject to inappropriate fluid therapy.
They propose a model of fluid therapy that considers i.v. fluid therapy as a drug therapy, with dose–response relationships and side-effects.
They suggest that individualized fluid therapy has the potential to reduce risk to patients.
Funding
ADQI XII was funded by unrestricted educational grants from Astute Medical Inc, Baxter Healthcare Corporation, Edwards Inc, FAST Biomedical Inc, Fresenius Kabi, Gambro Inc, Grifols Inc, LIDCO Ltd and NxStage Inc.
Footnotes
Authors’ contributions
E.A.H., K.M., C.S.B., R.M., J.-L.V., and D.Y. all contributed to the pre-conference and post-conference e-mail discussions on this review. In addition, all contributed to the group breakout sessions during the ADQI XII conference. E.A.H. drafted the first manuscript, and K.M., C.S.B., R.M., D.Y., J.-L.V., A.D.S., J.A.K., and M.G.M. helped develop subsequent drafts.
Declaration of interest
E.H. has received speakers fees from Astute Medical and Pfizer. C.S.B. received honoraria from Phoenix medical, Hospira, Orion, Covidien, and LiDCO, and functioned in the advisory board of Grifols. R.M. consulted for Baxter, Grifols, Abbvie, Gambro, Takeda, Astute, Astellas, GSK, CSL Behring, and Eli-Lilly. J.A.K. has received grant support from Baxter, and serves as a paid consultant for Baxter and Grifols. M.G.M. has received honoraria for speaking/consultation and/or travel expenses from Baxter, BBraun, Covidien, Fresenius-Kabi, Hospira, LidCo, and as a consultant to AQIX (start up company with a novel crystalloid solution-pre-clinical). He is a director of Medical Defence Technologies LLC (“Gastrostim” patented) and a coinventor of “QUENCH” IP being exploited by UCL Business. M.G.M.’s chair at UCL is endowed by Smiths Medical Ltd and this company provide charitable donations to the department on an annual basis. Deltex Medical also provide unrestricted grant funds to M.G.M.’s Department. M.G.M. is a member of the IV Fluids Guideline Development Group for the National Institute of Clinical Excellence (NICE) and he is a co-author of the GIFTASUP fluid guidelines. A.S. received grant support from Baxter Healthcare related to Plasmalyte, and serves as a paid consultant for Baxter and Grifols. K.M., J.L., and D.Y. have none to declare.
References
- 1.Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001;345:1368–77. doi: 10.1056/NEJMoa010307. [DOI] [PubMed] [Google Scholar]
- 2.Brunkhorst FM, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–39. doi: 10.1056/NEJMoa070716. [DOI] [PubMed] [Google Scholar]
- 3.Shaw AD, Bagshaw SM, Goldstein SL, et al. Major complications, mortality, and resource utilization after open abdominal surgery: 0.9% saline compared to Plasma-Lyte. Ann Surg. 2012;255:821–9. doi: 10.1097/SLA.0b013e31825074f5. [DOI] [PubMed] [Google Scholar]
- 4.Yunos NM, Bellomo R, Hegarty C, Story D, Ho L, Bailey M. Association between a chloride-liberal vs chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. J Am Med Assoc. 2012;308:1566–72. doi: 10.1001/jama.2012.13356. [DOI] [PubMed] [Google Scholar]
- 5.Perner A, Haase N, Guttormsen AB, et al. Hydroxyethyl starch 130/0.4 versus Ringer’s acetate in severe sepsis. N Engl J Med. 2012;367:124–34. doi: 10.1056/NEJMoa1204242. [DOI] [PubMed] [Google Scholar]
- 6.Myburgh JA, Finfer S, Bellomo R, et al. Hydroxyethyl starch or saline for fluid resuscitation in intensive care. N Engl J Med. 2012;367:1901–11. doi: 10.1056/NEJMoa1209759. [DOI] [PubMed] [Google Scholar]
- 7.Shaw AD, Kellum JA. The risk of AKI in patients treated with intravenous solutions containing hydroxyethyl starch. Clin J Am Soc Nephrol. 2013;8:497–503. doi: 10.2215/CJN.10921012. [DOI] [PubMed] [Google Scholar]
- 8.Murugan R, Kellum JA. Fluid balance and outcome in acute kidney injury: is fluid really the best medicine? Crit Care Med. 2012;40:1970–2. doi: 10.1097/CCM.0b013e31824e1a1f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Myburgh JA, Mythen MG. Resuscitation fluids. N Engl J Med. 2013;369:1243–51. doi: 10.1056/NEJMra1208627. [DOI] [PubMed] [Google Scholar]
- 10.Myburgh J, Cooper DJ, Finfer S, et al. Saline oralbuminfor fluid resuscitation in patients with traumatic brain injury. N Engl J Med. 2007;357:874–84. doi: 10.1056/NEJMoa067514. [DOI] [PubMed] [Google Scholar]
- 11.Reinhart K, Perner A, Sprung CL, et al. Consensus statement of the ESICM task force on colloid volume therapy in critically ill patients. Intensive Care Med. 2012;38:368–83. doi: 10.1007/s00134-012-2472-9. [DOI] [PubMed] [Google Scholar]
- 12.Kellum JA, Mythen MG, Shaw AD, for the ADQI XII Investigators Group Br J Anaesth; The 12th consensus conference of the Acute Dialysis Quality Initiative (ADQI XII); 2014. pp. 729–31. [DOI] [PubMed] [Google Scholar]
- 13.Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med. 2013;39:165–228. doi: 10.1007/s00134-012-2769-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Maitland K, Kiguli S, Opoka RO, et al. Mortality after fluid bolus in African children with severe infection. N Engl J Med. 2011;364:2483–95. doi: 10.1056/NEJMoa1101549. [DOI] [PubMed] [Google Scholar]
- 15.Maitland K, George EC, Evans JA, et al. Exploring mechanisms of excess mortality with early fluid resuscitation: insights from the FEAST trial. BMC Med. 2013;11:68. doi: 10.1186/1741-7015-11-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vincent JL, De Backer D. Circulatory shock. N Engl J Med. 2013;369:1726–34. doi: 10.1056/NEJMra1208943. [DOI] [PubMed] [Google Scholar]
- 17.Vincent JL, Weil MH. Fluid challenge revisited. Crit Care Med. 2006;34:1333–7. doi: 10.1097/01.CCM.0000214677.76535.A5. [DOI] [PubMed] [Google Scholar]
- 18.Macedo E, Bouchard J, Soroko SH, et al. Fluid accumulation, recognition and staging of acute kidney injury in critically-ill patients. Crit Care. 2010;14:R82. doi: 10.1186/cc9004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vaara ST, Korhonen A-M, Kaukonen K-M, et al. Fluid overload is associated with an increased risk for 90-day mortality in critically ill patients with renal replacement therapy: data from the prospective FINNAKI study. Crit Care. 2012;16:R197. doi: 10.1186/cc11682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.James MF, Michell WL, Joubert IA, Nicol AJ, Navsaria PH, Gillespie RS. Resuscitation with hydroxyethyl starch improves renal function and lactate clearance in penetrating trauma in a randomized controlled study: the FIRST trial (Fluids in Resuscitation of Severe Trauma) Br J Anaesth. 2011;107:693–702. doi: 10.1093/bja/aer229. [DOI] [PubMed] [Google Scholar]
- 21.Annane D, Siami S, Jaber S, et al. Effects of fluid resuscitation with colloids vs crystalloids on mortality in critically ill patients presenting with hypovolemic shock: the CRISTAL randomized trial. J Am Med Assoc. 2013;310:1809–17. doi: 10.1001/jama.2013.280502. [DOI] [PubMed] [Google Scholar]
- 22.Finfer S, Bellomo R, Boyce N, French J, Myburgh J, Norton R. A comparison of albumin and saline for fluid resuscitation in the intensive care unit. N Engl J Med. 2004;350:2247–56. doi: 10.1056/NEJMoa040232. [DOI] [PubMed] [Google Scholar]
- 23.Poeze M, Greve JW, Ramsay G. Meta-analysis of hemodynamic optimization: relationship to methodological quality. Crit Care. 2005;9:R771–9. doi: 10.1186/cc3902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Giglio MT, Marucci M, Testini M, Brienza N. Goal-directed haemodynamic therapy and gastrointestinal complications in major surgery: a meta-analysis of randomized controlled trials. Br J Anaesth. 2009;103:637–46. doi: 10.1093/bja/aep279. [DOI] [PubMed] [Google Scholar]
- 25.Gurgel ST, do Nascimento PJ. Maintaining tissue perfusion in high-risk surgical patients: a systematic review of randomized clinical trials. Anesth Analg. 2011;112:1384–91. doi: 10.1213/ANE.0b013e3182055384. [DOI] [PubMed] [Google Scholar]
- 26.Hamilton MA, Cecconi M, Rhodes A. A systematic review and meta-analysis on the use of preemptive hemodynamic intervention to improve postoperative outcomes in moderate and high-risk surgical patients. Anesth Analg. 2011;112:1392–402. doi: 10.1213/ANE.0b013e3181eeaae5. [DOI] [PubMed] [Google Scholar]
- 27.Dalfino L, Giglio MT, Puntillo F, Marucci M, Brienza N. Haemodynamic goal-directed therapy and postoperative infections: earlier is better. A systematic review and meta-analysis. Crit Care. 2011;15:R154. doi: 10.1186/cc10284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Challand C, Struthers R, Sneyd JR, et al. Randomized controlled trial of intraoperative goal-directed fluid therapy in aerobically fit and unfit patients having major colorectal surgery. Br J Anaesth. 2012;108:53–62. doi: 10.1093/bja/aer273. [DOI] [PubMed] [Google Scholar]
- 29.Giglio M, Dalfino L, Puntillo F, Rubino G, Marucci M, Brienza N. Haemodynamic goal-directed therapy in cardiac and vascular surgery. A systematic review and meta-analysis. Interact Cardiovasc Thorac Surg. 2012;15:878–87. doi: 10.1093/icvts/ivs323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Prowle JR, Chua HR, Bagshaw SM, Bellomo R. Clinical review: volume of fluid resuscitation and the incidence of acute kidney injury—a systematic review. Crit Care. 2012;16:230. doi: 10.1186/cc11345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aya HD, Cecconi M, Hamilton M, Rhodes A. Goal-directed therapy in cardiac surgery: a systematic review and meta-analysis. Br J Anaesth. 2013;110:510–7. doi: 10.1093/bja/aet020. [DOI] [PubMed] [Google Scholar]
- 32.Cecconi M, Corredor C, Arulkumaran N, et al. Clinical review: goal-directed therapy—what is the evidence in surgical patients? The effect on different risk groups. Crit Care. 2013;17:209. doi: 10.1186/cc11823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Davies SJ, Minhas S, Wilson RJ, Yates D, Howell SJ. Comparison of stroke volume and fluid responsiveness measurements in commonly used technologies for goal-directed therapy. J Clin Anesth. 2013;25:466–74. doi: 10.1016/j.jclinane.2013.04.010. [DOI] [PubMed] [Google Scholar]
- 34.Futier E, Constantin J-M, Paugam-Burtz C, et al. A trial of intraoperative low-tidal-volume ventilation in abdominal surgery. N Engl J Med. 2013;369:428–37. doi: 10.1056/NEJMoa1301082. [DOI] [PubMed] [Google Scholar]
- 35.Kidney disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. 2012;2:1–138. [Google Scholar]
- 36.Lameire N, Kellum JA. Contrast-induced acute kidney injury and renal support for acute kidney injury: a KDIGO summary (Part 2) Crit Care. 2013;17:205. doi: 10.1186/cc11455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Merten GJ, Burgess WP, Gray LV, et al. Prevention of contrast-induced nephropathy with sodium bicarbonate: a randomized controlled trial. J Am Med Assoc. 2004;291:2328–34. doi: 10.1001/jama.291.19.2328. [DOI] [PubMed] [Google Scholar]
- 38.EASL clinical practice guidelines on the management of ascites, spontaneous bacterial peritonitis, and hepatorenal syndrome in cirrhosis. J Hepatol. 2010;53:397–417. doi: 10.1016/j.jhep.2010.05.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.