Abstract
Purpose
To evaluate whether health-related quality-of-life measures can be improved in a senior population by increasing participation in an exercise program.
Methods
The study involved a nationwide sample of adults aged 65 and older (mean age 73.2 in first study year) who participated in the SilverSneakers fitness program between 2010 and 2016. We analyzed data from 7 years of program participation records and annual participant surveys. Study members completed ≥ 2 annual surveys (n = 46,564). Participation frequency change was measured by average visits per week (AVPW) to a fitness center from the initial survey year to follow-up years. Quality-of-life measures included the 12-Item Short Form Health Survey (SF-12), Self-Rated Health, and BRFSS Healthy Days measures. Longitudinal analyses evaluated whether an increase in visit frequency among active members of SilverSneakers was associated with change in quality-of-life measures, controlling for age and gender.
Results
Participants with more frequent visits (higher AVPW) had better SF-12 Physical and Mental Component Scores, Self-Rated Health Status, and fewer physically and mentally unhealthy days (p < 0.001 for all measures); furthermore, participants who increased AVPW longitudinally saw improvements in all outcome measures (p < 0.001).
Conclusion
SilverSneakers participation frequency is associated with higher quality of life for seniors.
Keywords: Seniors, Physical activity, Quality of life, SF-12, Healthy days, General health
Purpose
Americans 65 and older are expected to outnumber children by 2035 [1], a shift that has never occurred before in U.S. history, and by 2060, almost 1 in 4 Americans will be at least 65 years old [2]. These dramatic changes in demographics, driven in part by increases in life expectancy [3], underscore the important public health goal of maintaining and improving quality of life for aging populations [4, 5]. One pathway to improve quality of life may be via increasing one’s physical activity levels [6]. Physical activity has been shown to benefit various aspects of quality of life such as physical functioning, mental health, and social connection cross-sectionally, including in senior populations [7–13]. However, research that longitudinally evaluates whether increasing the frequency of older adults’ physical activity results in greater improvement in quality of life is sparse, particularly research that uses widely adopted metrics for health-related quality of life (HRQOL).
Health-related quality of life is an important metric to target as it is associated with mortality and hospitalizations in older adults [14–16]. Prominent efforts to identify and measure the factors that improve health-related quality of life in older adults in the US include the Healthy People 2020 goals [4, 5], the Medicare Health Outcomes Survey [17], and Medicare Part C (“Medicare Advantage”) Star ratings [18]. The purpose of this study is to longitudinally evaluate whether increasing participation frequency among members of a nationwide fitness program for older adults, SilverSneakers, is associated with improved HRQOL.
Methods
SilverSneakers is a program that provides seniors with access to a nationwide network of over 15,000 fitness centers and a variety of specialized group exercise classes for older adults across the US.
The study population included seniors (65 years and older), who were members of SilverSneakers via their Medicare Advantage health plan, and who made at least 12 visits to a fitness center in the prior 12 months, with at least one visit in the prior 6 months. Participants had to complete at least two annual surveys from 2010–2016; however, to increase generalizability while maximizing evaluation of longitudinal outcomes, survey response years were not required to be consecutive. The total number of participants who met these criteria was 46,564.
We collected data via a recurring annual member survey (AMS) which is administered via a mailed paper survey in September every year. The average completion rate for this survey was 48% across the study timeframe. Included within the survey instrument were quality-of-life measures (SF-12, Self-Rated Health, and BRFSS Healthy Days measures), age, and sex. All measures were not available in every year of the annual survey: SF-12 items were assessed from 2010–2015, Self-Rated Health from 2010–2016, and Healthy Days from 2010–2011 and 2016.
The quality-of-life measures in this study are included in the surveys of major national initiatives. Healthy People 2020 quality-of-life measures include the BRFSS Healthy Days measure [19] and Self-Rated Health status [5] (SRH), a standalone item in the 12-Item Short Form Health Survey (SF-12) [20]. The SF-12, derived from the SF-36 used in the Medicare Health Outcomes Survey [17], is used to evaluate Medicare Part C (“Medicare Advantage”) Star ratings in the form of the Veterans RAND 12-Item Health Survey [18].
The scales for the quality-of-life dependent variables were SF-12 physical and mental component scores [20, 21], assessed on a scale from 0–100 with higher scores being better; Self-Rated Health [5] (“In general, would you say your health is:”), scored as 1–5 (“excellent” to “poor” with a higher number being worse); and Healthy Days which is the reported number of days in the past 30 days that mental and physical health were “not good,” [19], assessed as the number of unhealthy days, with a higher number being worse.
The primary independent variable was frequency of program participation, measured objectively by average visits per week (AVPW) to a SilverSneakers fitness location from recorded visits in internal accounting systems. AVPW was calculated on an annual basis for each calendar year that a participant completed a survey and evaluated as 4 tiers: < 1 visit per week, 1 up to < 2, 2 up to < 3, and 3 or more. “3 or more” was selected as the top tier of participation frequency as it echoes WHO exercise recommendations [22], and exercising at least 3 times per week has shown to be a threshold for positive impacts on mental health [23].
Statistical tests of the cross-sectional association between AVPW and quality-of-life measures used the Friedman test as there are more than two tiers and they are not necessarily independent (the same participant can be in different tiers of AVPW over time).
Longitudinal analyses were performed using generalized linear modeling utilizing generalized estimating equations, controlling for age and sex. Data were first transformed into long form by year, and the participant ID was identified as the class statement and the repeated subject. Since most of the participants did not have more than three time points in which they had survey responses, the model was run with an unstructured correlation matrix.
All analyses were conducted using SAS Enterprise Guide 7.1
Results
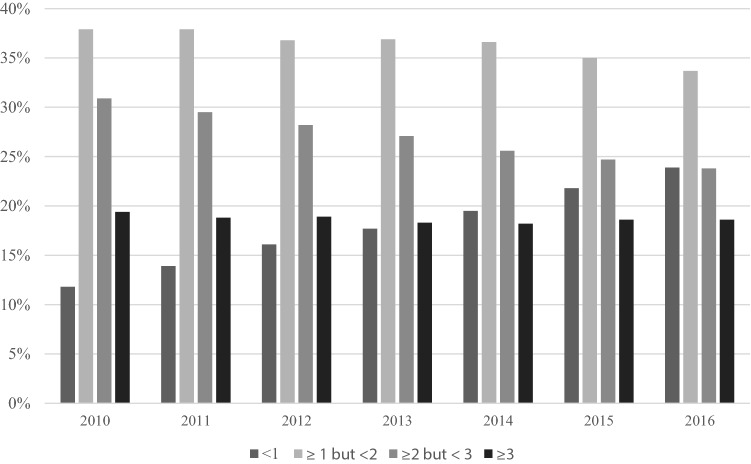
Descriptive statistics by year are presented in Table 1 and percentages by AVPW by year are shown in Fig. 1. Evaluation of the relationship between AVPW and each outcome variable found that more frequent visits to a fitness center were associated with significantly better outcomes across all quality-of-life measures (Table 2; p-values < 0.001).
Table 1.
Descriptive statistics for control and dependent variables by year
| Variable | Year | N | Mean | Std. Dev. |
|---|---|---|---|---|
| Age | 2010 | 15,895 | 73.22 | 6.06 |
| 2011 | 21,347 | 73.93 | 6.23 | |
| 2012 | 21,730 | 73.73 | 6.38 | |
| 2013 | 20,350 | 73.66 | 6.58 | |
| 2014 | 18,146 | 73.45 | 6.57 | |
| 2015 | 14,217 | 74.13 | 6.49 | |
| 2016 | 3697 | 75.01 | 6.64 | |
| Percent female | 2010 | 62% | ||
| 2011 | 62% | |||
| 2012 | 61% | |||
| 2013 | 60% | |||
| 2014 | 59% | |||
| 2015 | 58% | |||
| 2016 | 57% | |||
| SF-12: physical component score | 2010 | 14,437 | 48.55 | 8.90 |
| 2011 | 18,282 | 47.99 | 9.35 | |
| 2012 | 19,602 | 48.22 | 9.34 | |
| 2013 | 18,269 | 48.43 | 9.24 | |
| 2014 | 18,126 | 48.45 | 9.20 | |
| 2015 | 12,774 | 48.39 | 9.14 | |
| SF-12: mental component score | 2010 | 14,437 | 55.70 | 6.88 |
| 2011 | 18,282 | 55.50 | 7.04 | |
| 2012 | 19,602 | 55.52 | 7.09 | |
| 2013 | 18,269 | 55.55 | 7.08 | |
| 2014 | 18,126 | 55.58 | 7.06 | |
| 2015 | 12,774 | 55.65 | 6.99 | |
| Self-rated health | 2010 | 15,831 | 2.29 | 0.78 |
| 2011 | 21,133 | 2.32 | 0.79 | |
| 2012 | 21,509 | 2.30 | 0.79 | |
| 2013 | 20,161 | 2.29 | 0.79 | |
| 2014 | 19,767 | 2.27 | 0.80 | |
| 2015 | 14,086 | 2.27 | 0.79 | |
| 2016 | 3660 | 2.31 | 0.81 | |
| Physically unhealthy days | 2010 | 14,155 | 2.52 | 6.15 |
| 2011 | 19,966 | 2.32 | 6.05 | |
| 2016 | 3173 | 2.79 | 6.96 | |
| Mentally unhealthy days | 2010 | 14,248 | 1.76 | 4.92 |
| 2011 | 20,175 | 1.57 | 4.55 | |
| 2016 | 3302 | 1.47 | 5.01 |
Fig. 1.
Percent of population by tier of average visits per week, by year
Table 2.
Descriptive statistics per AVPW (average visits per week) for all dependent variables across all available data
| AVPW | N | Mean | Std Dev | |
|---|---|---|---|---|
| SF-12: physical component score* | < 1 | 13,659 | 47.05 | 9.79 |
| ≥ 1 but < 2 | 38,104 | 47.75 | 9.42 | |
| ≥ 2 but < 3 | 29,412 | 48.72 | 8.94 | |
| ≥ 3 | 20,133 | 49.72 | 8.57 | |
| SF-12: mental component score* | < 1 | 13,659 | 54.84 | 7.65 |
| ≥ 1 but < 2 | 38,104 | 55.52 | 7.10 | |
| ≥ 2 but < 3 | 29,412 | 55.75 | 6.79 | |
| ≥ 3 | 20,133 | 55.94 | 6.74 | |
| Self-rated Healtha* | < 1 | 15,898 | 2.39 | 0.81 |
| ≥ 1 but < 2 | 43,551 | 2.32 | 0.79 | |
| ≥ 2 but < 3 | 33,272 | 2.26 | 0.77 | |
| ≥ 3 | 22,829 | 2.20 | 0.79 | |
| Physically unhealthy daysa* | < 1 | 4640 | 3.33 | 7.19 |
| ≥ 1 but < 2 | 14,071 | 2.64 | 6.39 | |
| ≥ 2 but < 3 | 11,134 | 2.13 | 5.70 | |
| ≥ 3 | 7116 | 1.87 | 5.47 | |
| Mentally unhealthy daysa* | < 1 | 4720 | 2.01 | 5.32 |
| ≥ 1 but < 2 | 14,198 | 1.67 | 4.72 | |
| ≥ 2 but < 3 | 11,269 | 1.54 | 4.53 | |
| ≥ 3 | 7186 | 1.41 | 4.52 |
The sample size for each tier of AVPW can exceed the sample size for any given year because the analysis aggregates data from all years and participants are represented at least twice in the dataset
aFor these measures, a smaller number signifies better health
*Results from the Friedman test indicate that mean values differ by tier of AVPW (P value < 0.001)
In longitudinal analyses, increasing frequency of visits from baseline to follow-up was associated with significant improvements in all quality-of-life-dependent variables analyzed, with all p-values falling below 0.001 (Table 3). For each incremental increase in AVPW, on average, SF-12 physical component score increased by 0.75 and mental component score increased by 0.33, Self-Rated Health decreased by 0.05, and physically and mentally unhealthy days decreased by 0.47 and 0.15, respectively.
Table 3.
Longitudinal analyses using generalized linear modeling with generalized estimating equations
| Measure | P-value | Effect size estimate | Average annual value |
|---|---|---|---|
| sf-12: physical component score | < .0001 | 0.75 | 48.33 |
| SF-12: mental component score | < .0001 | 0.33 | 55.57 |
| Self-rated healtha | < .0001 | − 0.05 | 2.29 |
| Physically unhealthy daysa | < .0001 | − 0.47 | 2.44 |
| Mentally unhealthy daysa | < .0001 | − 0.15 | 1.63 |
aFor these measures, a negative estimate signifies better health
Therefore, for each incremental tier increase in AVPW, on average, SF-12 physical and mental component scores increased by 1.5% and 0.6% respectively, Self-Rated Health improved by 2.4%, and physically and mentally unhealthy days decreased by 19.4% and 9.5%, respectively.
Discussion
Decreasing quality of life has typically been associated with the aging process, but these declines are in large part attributable to the consequences of decreasing physical activity [24, 25]. Therefore, increasing one’s physical activity should result in increased quality of life. This study indicates that even in older adults who are already physically active, quality of life may be further enhanced by increasing participation in SilverSneakers. For example, on average, an increase from less than 1 fitness center visit per week to at least 3 visits per week was associated with a reduction in physically unhealthy days of more than 1.4 days per month, and a reduction in mentally unhealthy days of almost 0.5 days per month. Not only do reductions in unhealthy days positively impact quality of life for the individual, but research by a major Medicare Advantage health plan provider has estimated a healthcare cost of $15.64 for each additional unhealthy day per person per month [26], further demonstrating the value of reducing unhealthy days.
The significant longitudinal effect observed for each of the study measures may also have clinical significance. In particular, the SF-12, Self-Rated Health, and unhealthy days measures predict hospitalizations and mortality, suggesting that increasing participation in SilverSneakers may influence these outcomes. The potential for this clinical impact is supported by prior research that demonstrated the relationship between SilverSneakers participation and hospitalizations [27, 28].
This study used a large sample, followed across multiple years, but there were some limitations. Survey responses were not available for every year and were not always contiguous. Also, due to a change in survey sampling in 2016, later years had a smaller useable sample size. Since the study was retrospective in nature and not originally structured to include a control group, there was not one available for inclusion in analyses. Finally, as the participants were not observed by the researchers during fitness center visits, it is not possible to attribute results directly to physical activity (e.g., intensity or duration), and other aspects of the program, such as socialization with peers, may have contributed to the observed relationship between visits and HRQOL. We posit that the primary driver of this relationship is higher physical activity levels, supplemented by the program’s social benefits, as was observed in a recent cross-sectional study of SilverSneakers members [29].
The survey sample for this study was limited to older adults with at least some physical activity, whereas 28% of adults 50 years and older are physically inactive [30]. Future research should focus on a cohort that increases physical activity from a baseline of no regular exercise. An inactive cohort would likely demonstrate a much larger effect size of increasing activity since the benefits of exercise on health and parameters of quality of life are most pronounced when someone moves from being physically inactive to engaging in some level of activity [31, 32], congruent with a study demonstrating SF-12 physical and mental differences between older adult exercisers and non-exercisers [33].
Overall, this study supports that increasing participation in the SilverSneakers fitness program is an effective strategy to improve health-related quality of life among older adults. These results show that it is never too late to improve one’s quality of life, nor are the benefits of increasing exercise frequency reserved for those of any particular age.
Acknowledgements
We thank Dr. Sandro Galea for his critical review of the study and manuscript. We also thank Dr. Justin Barclay and Dr. Ashley Crossman for their expert assistance in data provision and support.
Compliance with ethical standards
Conflict of interest
Dr. Kell and Dr. Rula were employed by Tivity Health during the course of the study, and Dr. Rula holds stock in Tivity Health.
Ethical approval
Due to the retrospective nature of this study, formal consent was not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.USCB (2018). Older people projected to outnumber children for first time in U.S. History. https://www.census.gov/newsroom/press-releases/2018/cb18-41-population-projections.html. Accessed 7 January 2019.
- 2.Mather MJL, Pollard KM (2015). Aging in the United States. In P. R. Bureau (Ed.), Population bulletin (Vol. 70). https://www.prb.org/wp-content/uploads/2016/01/aging-us-population-bulletin-1.pdf. Accessed 7 January 2019.
- 3.NCHS (2018). United States, 2017: With special feature on mortality. Table 15. Life expectancy at birth, at age 65, and at age 75, by sex, race, and Hispanic origin: United States, selected years 1900–2016. https://www.cdc.gov/nchs/data/hus/2017/015.pdf. Accessed 7 January 2019. Hyattsville, Maryland.
- 4.CDC Healthy People 2020. General Health Status. Physically and mentally unhealthy days. https://www.healthypeople.gov/2020/about/foundation-health-measures/General-Health-Status#Physically. Accessed 6 December 2018.
- 5.Office of Disease Prevention and Health Promotion. HealthyPeople. Foundation Health Measures Archive. General Health Status. Accessible at. https://www.healthypeople.gov/2020/about/foundation-health-measures/General-Health-Status#selfAssessed. Accessed 6 December 2018.
- 6.Raggi A, Corso B, Minicuci N, Quintas R, Sattin D, De Torres L, et al. Determinants of quality of life in ageing populations: Results from a cross-sectional study in Finland, Poland and Spain. PLoS ONE. 2016;11(7):e0159293. doi: 10.1371/journal.pone.0159293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Taylor D. Physical activity is medicine for older adults. Postgraduate Medical Journal. 2014;90(1059):26–32. doi: 10.1136/postgradmedj-2012-131366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bauman A, Merom D, Bull FC, Buchner DM, Fiatarone Singh MA. Updating the evidence for physical activity: Summative reviews of the epidemiological evidence, prevalence, and interventions to promote “active aging”. The Gerontologist. 2016;56:S268–S280. doi: 10.1093/geront/gnw031. [DOI] [PubMed] [Google Scholar]
- 9.Brady S, D’Ambrosio LA, Felts A, Rula EY, Kell KP, Coughlin JF. Reducing isolation and loneliness through membership in a fitness program for older adults: Implications for health. Journal of Applied Gerontology. 2018 doi: 10.1177/0733464818807820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kolt GS, George ES, Rebar AL, Duncan MJ, Vandelanotte C, Caperchione CM, et al. Associations between quality of life and duration and frequency of physical activity and sedentary behaviour: Baseline findings from the WALK 2.0 randomised controlled trial. PLOS ONE. 2017;12(6):e0180072. doi: 10.1371/journal.pone.0180072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Heesch KC, van Uffelen JGZ, van Gellecum YR, Brown WJ. Dose–response relationships between physical activity, walking and health-related quality of life in mid-age and older women. Journal of Epidemiology and Community Health. 2012;66(8):670–677. doi: 10.1136/jech-2011-200850. [DOI] [PubMed] [Google Scholar]
- 12.Lustyk MK, Widman L, Paschane AA, Olson KC. Physical activity and quality of life: assessing the influence of activity frequency, intensity, volume, and motives. Behavioral Medicine. 2004;30(3):124–131. doi: 10.3200/BMED.30.3.124-132. [DOI] [PubMed] [Google Scholar]
- 13.Rosenkranz RR, Duncan MJ, Rosenkranz SK, Kolt GS. Active lifestyles related to excellent self-rated health and quality of life: Cross sectional findings from 194,545 participants in The 45 and Up Study. BMC Public Health. 2013;13(1):1071. doi: 10.1186/1471-2458-13-1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dorr DA, Jones SS, Burns L, Donnelly SM, Brunker CP, Wilcox A, et al. Use of health-related, quality-of-life metrics to predict mortality and hospitalizations in community-dwelling seniors. Journal of the American Geriatrics Society. 2006;54(4):667–673. doi: 10.1111/j.1532-5415.2006.00681.x. [DOI] [PubMed] [Google Scholar]
- 15.Benyamini Y. Why does self-rated health predict mortality? An update on current knowledge and a research agenda for psychologists. Journal of Psychology and Health. 2011 doi: 10.1080/08870446.2011.621703. [DOI] [PubMed] [Google Scholar]
- 16.Dominick KL, Ahern FM, Gold CH, Heller DA. Relationship of health-related quality of life to health care utilization and mortality among older adults. Aging Clinical and Experimental Research. 2002;14(6):499–508. doi: 10.1007/BF03327351. [DOI] [PubMed] [Google Scholar]
- 17.Jones N, Jones SL, Miller NA. The medicare health outcomes survey program: Overview, context, and near-term prospects. Health and Quality of Life Outcomes. 2004;2(1):33. doi: 10.1186/1477-7525-2-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Iqbal SU, Rogers W, Selim A, Qian S, Lee A, Ren X, et al. (2007) The Veterans RAND 12 Item Health Survey (VR-12): what it is and how it is used. CHQOERs VA Medical Center. Bedford, MA: CAPP Boston University School of Public Health. https://www.bu.edu/sph/files/2015/01/veterans_rand_12_item_health_survey_vr-12_2007.pdf. Accessed 6 December 2018.
- 19.Moriarty DG, Kobau R, Zack MM, Zahran HS. Tracking healthy days—a window on the health of older adults. Preventing Chronic Disease. 2005;2(3):A16. [PMC free article] [PubMed] [Google Scholar]
- 20.Jakobsson U. Using the 12-item Short Form health survey (SF-12) to measure quality of life among older people. Aging Clinical and Experimental Research. 2007;19(6):457–464. doi: 10.1007/BF03324731. [DOI] [PubMed] [Google Scholar]
- 21.Ware J, Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 22.WHO (2011). Global recommendations on physical activity for health: 65 years and above. http://www.who.int/dietphysicalactivity/physical-activity-recommendations-65years.pdf?ua=1. Accessed 4 December 2018.
- 23.Blay SL, Landerman LR, Fillenbaum GG. Is higher frequency of physical activity associated with reduced prevalence of depression among older community residents? A study from Brazil. Journal of the American Geriatrics Society. 2016;64(9):e42. doi: 10.1111/jgs.14335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mechling H, Netz Y. Aging and inactivity—Capitalizing on the protective effect of planned physical activity in old age. European Review of Aging and Physical Activity. 2009;6(2):89. doi: 10.1007/s11556-009-0052-y. [DOI] [Google Scholar]
- 25.Rejeski WJ, Brawley LR. Functional health: innovations in research on physical activity with older adults. Medicine and Science in Sports and Exercise. 2006;38(1):93–99. doi: 10.1249/01.mss.0000183191.65316.0a. [DOI] [PubMed] [Google Scholar]
- 26.Renda A, Shah M, Zack M. A health plan’s investigation of healthy days and chronic conditions. American Journal of Managed Care. 2017;23(10):e323–e330. [PubMed] [Google Scholar]
- 27.Nguyen HQ, Ackermann RT, Berke EM, Cheadle A, Williams B, Lin E, et al. Impact of a managed-Medicare physical activity benefit on health care utilization and costs in older adults with diabetes. Diabetes Care. 2007;30(1):43–48. doi: 10.2337/dc06-1013. [DOI] [PubMed] [Google Scholar]
- 28.Nguyen HQ, Ackermann RT, Maciejewski M, Berke E, Patrick M, Williams B, et al. Managed-medicare health club benefit and reduced health care costs among older adults. Preventing Chronic Disease. 2008;5(1):A14. [PMC free article] [PubMed] [Google Scholar]
- 29.Brady S, D’Ambrosio LA, Felts A, Rula EY, Kell KP, Coughlin JF. Reducing isolation and loneliness through membership in a fitness program for older adults: Implications for health. Journal of Applied Gerontology. 2018 doi: 10.1177/0733464818807820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shi Y, Sears LE, Coberley CR, Pope JE. The association between modifiable well-being risks and productivity: A longitudinal study in pooled employer sample. Journal of Occupational and Environmental Medicine. 2013;55(4):353–364. doi: 10.1097/JOM.0b013e3182851923. [DOI] [PubMed] [Google Scholar]
- 31.Minton J, Dimairo M, Everson-Hock E, Scott E, Goyder E. Exploring the relationship between baseline physical activity levels and mortality reduction associated with increases in physical activity: A modelling study. British Medical Journal Open. 2013;3(10):e003509. doi: 10.1136/bmjopen-2013-003509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Woodcock J, Franco OH, Orsini N, Roberts I. Non-vigorous physical activity and all-cause mortality: Systematic review and meta-analysis of cohort studies. International Journal of Epidemiology. 2010;40(1):121–138. doi: 10.1093/ije/dyq104. [DOI] [PubMed] [Google Scholar]
- 33.Resnick B, Nahm ES. Reliability and validity testing of the revised 12-item short-form health Survey in older adults. Journal of Nursing Measurement. 2001;9(2):151–161. doi: 10.1891/1061-3749.9.2.151. [DOI] [PubMed] [Google Scholar]