Abstract
Aim
This study investigated physiotherapists’ experiences using motor learning strategies (MLS) in gait-based interventions for children with cerebral palsy (CP). The objectives were to explore how child characteristics, physiotherapist decision-making, and treatment approach influenced intentional MLS use.
Methods
Semi-structured interviews were conducted with eight physiotherapists who provided gym- and/or Lokomat-based treatment to children with CP. Interviews were analyzed using directed content analysis and a modified constant comparison method.
Results
Three themes described their experiences: (1) MLS use is driven by the unique aspects of the child, physiotherapist, and intervention; (2) The use and description of motor learning content varies among physiotherapists; and (3) The Lokomat is “the same but different.” Child characteristics were at the forefront of MLS selection in both interventions. The terminology used to describe MLS use varied considerably among therapists. They used similar clinical decision-making in gym-and Lokomat-based interventions.
Conclusions
Conscious reflection on the factors affecting MLS use could facilitate related clinical decision-making in physiotherapy interventions for children with CP. Increased awareness of MLS and use of a structured framework for reporting MLS are required to promote intentional MLS use and generate CP-specific evidence-based MLS research.
Keywords: Cerebral palsy, clinical decision-making, motor learning, motor learning strategies, physiotherapy
Children with cerebral palsy (CP) present with varying motor, sensory, and cognitive deficits that affect their physical function and participation in daily activities (Bax et al., 2005; Burtner, Leinwand, Sullivan, Goh, & Kantak, 2014; Hemayattalab & Rostami, 2010; Valvano, 2004). There is potential to optimize a child’s motor function via therapeutic interventions that enhance the learning underlying experience-dependent neuroplasticity (Diaz Heijtz & Forssberg, 2015). Motor learning (ML) refers to the acquisition of a motor skill, achieved through practice, which can be transferred to new learning situations (Schmidt & Wrisberg, 2004). ML can be promoted in therapeutic interventions by using motor learning strategies (MLS) (Larin, 1998, 2007; Levac, Wishart, Missiuna, & Wright, 2009) which are implemented by a physiotherapist (PT) as observable actions involving the selection and manipulation of ML variables based on child- and task-specific factors (Levac, Missiuna, Wishart, DeMatteo, & Wright, 2011). PTs employ MLS with the ultimate goal of helping children with CP transfer newly acquired/refined skills from intervention to use in daily activities. As such, understanding the treatment approaches that most effectively promote ML is a key priority in optimizing the therapeutic intervention and enhancing associated functional outcomes (Valvano, 2004).
The integration of technology-based treatment approaches in physiotherapy, including active video gaming (Winkels, Kottink, Temmink, Nijlant, & Buurke, 2013), functional electrical stimulation (Pool, Blackmore, Bear, & Valentine, 2014), and robotic-assisted gait training (Meyer-Heim et al., 2009) is linked with the potential for enhancing ML in children with CP. However, studies evaluating these interventions rarely detail the extent to which the intervention protocol involved MLS (Borggraefe et al., 2010; Meyer-Heim et al., 2009; Pool et al., 2014; Wallard, Dietrich, Kerlirzin, & Bredin, 2018; Winkels et al., 2013). Additionally, ML outcomes are attributed to features of the technology, while the impact of therapist decision-making in selecting MLS to promote ML is overlooked (Borggraefe et al., 2010; Meyer-Heim et al., 2009; Wallard et al., 2018; Winkels et al., 2013). It is unknown if certain treatment approaches have increased potential for the implementation of specific MLS. Thus, it is imperative that the exploration of MLS use extends beyond traditional gym-based physiotherapy and also considers the application of novel approaches and/or technologies.
The desire to understand MLS use in physiotherapy interventions led to the creation of the Motor Learning Strategies Rating Instrument (MLSRI-20), a revised version of the original instrument (Levac et al. 2011). It measures the extent to which 20 MLS are observed within a video-recorded treatment session (Ryan, Wright, & Levac, 2016) (Table 1). While the MLSRI-20 is reliable in physiotherapy interventions for children with CP (Ryan, Levac, & Wright, 2019), it does not indicate PTs’ intentions when using specific MLS nor does it explain the decision-making that accompanies their selections. While there is a theoretical link between physiotherapy goals for children with CP and ML theory, studies suggest that PTs may not always be intentionally applying MLS (Atun-Einy & Kafri, 2018; Hayes, McEwen, Lovett, M’Lisa, & Smith, 1999). Consequently, one cannot assume that the observation of MLS indicates their purposeful use.
Table 1.
MLSRI-20 item description (Ryan et al., 2016).
| MLSRI-20 Category | Item | Description |
|---|---|---|
| What the Therapist SAYS | 1 | Encouragement |
| 2 | Instructions direct attention to object/environment | |
| 3 | Instructions direct attention to body movement | |
| 4 | Problem-solving involves asking (rather than telling) | |
| 5 | Feedback relates to movement performance | |
| 6 | Feedback relates to results | |
| 7 | Feedback relates to what was done well | |
| 8 | Feedback relates to what was done poorly | |
| 9 | Link activity being practiced to other activities | |
| 10 | Encourages mental practice | |
| What the Therapist DOES | 11 | Uses demonstration/modeling |
| 12 | Provides physical guidance | |
| 13 | Provides environment where errors are part of learning | |
| 14 | Recommends practice outside of therapy | |
| 15 | Provides education to client/caregiver | |
| How Practice IS Organized | 16 | Repetitive |
| 17 | Whole (rather than part) | |
| 18 | Variable (rather than constant) | |
| 19 | Random (rather than blocked) | |
| 20 | Progressive |
The purpose of this study was to explore how PTs apply MLS in gait-based physiotherapy interventions for children with CP. By investigating MLS selection in within an ongoing therapy-based research study involving both traditional gym-based interventions and physiotherapy in the Lokomat® robotic-assisted gait trainer, our team had a unique opportunity to identify differences in MLS use based on the PT, child, and/or treatment approach. Additionally, this study identified how PTs’ intentions to use MLS align with the MLS included in the MLSRI-20, which support its use in determining the key “active” ML ingredients in therapy sessions.
Methods
Design
This qualitative study used a descriptive interpretive approach, allowing investigators to enhance the understanding of clinical situations and promote the refinement of clinical practice (Teodoro et al., 2018).
Participants
Eight PTs were recruited from a team of 20 treating PTs (all women) working in one of three Lokomat clinical trials for children with CP at Holland Bloorview Kids Rehabilitation Hospital (HBKRH). Maximum heterogeneity sampling was used to capture a diverse range of PT characteristics (Patton, 2002), including their experience in pediatric physiotherapy and the Lokomat studies (Table 2). PTs had at least 3 months of experience with the Lokomat and provided intervention in both gym- and Lokomat-based sessions. While there is no established sample size for qualitative studies (Patton, 2002), studies using semi-structured interviews can be guided by information power, which is appraised by examining study aim, sample specificity, use of established theory, quality of dialog, and analysis strategy (Malterud, Siersma, & Guassora, 2016). A sample of eight PTs was determined based on the narrow study aim, dense sample specificity, use of the MLSRI-20 framework, and moderately estimated quality of dialog and analysis strategy.
Table 2.
Demographics of PT participants.
| PT | Pediatric physical therapy experiencea | Areas of clinical experience | Lokomat study experiencec | Video clips available |
|---|---|---|---|---|
| 1 | High | Inpatient, Home care | High | 2 |
| 2 | High | Outpatientb, School care | High | 2 |
| 3 | Low | Inpatient | High | 2 |
| 4 | High | Outpatient, Inpatient, Home care | High | 2 |
| 5 | High | Outpatient, School care | High | 1 |
| 6 | High | Outpatient, School care | Low | 0 |
| 7 | High | Outpatient, Inpatient, Home care | High | 2 |
| 8 | Low | School care, Home care | Low | 2 |
Pediatric physical therapy experience: high = >8 years, moderate = 3–8 years, low = <3 years.
Outpatient = children’s treatment center.
Lokomat study experience: high = >2 years, moderate = 1–2 years and treated 4 or more children in the study, low = <1 year or treated <4 children in the study.
Children (6–17 years, Gross Motor Function Classification Scale [Palisano et al., 2008] I–IV) in the Lokomat studies received twice-weekly intervention from two PTs for at least one 8-week block of Lokomat and/or gym-based interventions. Videos were recorded in at least two treatment sessions for each child. Tailored clips of these videos were used in the interviews. The first author created up to two 3-minute videos of the interviewed PT providing intervention with the goal of including gym and Lokomat sessions for each child; a range of MLS; effective and ineffective MLS use; and/or differing levels of child engagement and behavior.
The Research Ethics Boards at HBKRH and the University of Toronto approved the current study protocol. PTs provided written consent prior to participating in the interview. Written consent to use treatment videos was obtained from the parent and child.
Procedure
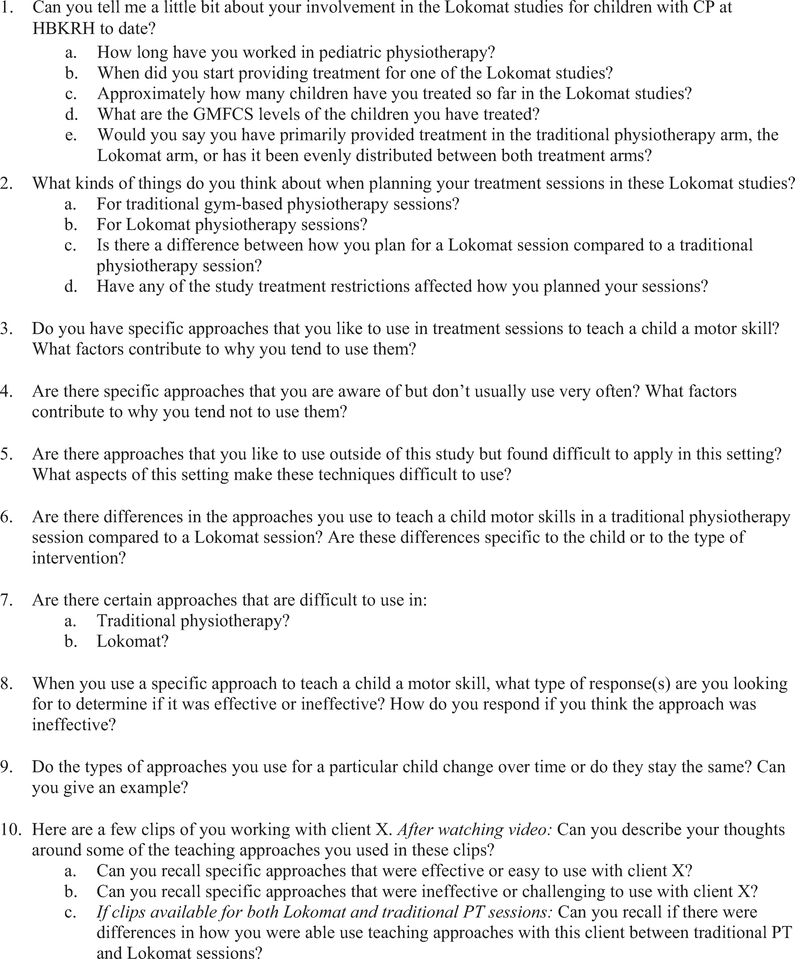
Individual semi-structured interviews (60-minute duration) were conducted with the aim of obtaining a range of perspectives on MLS use (Stalmeijer, McNaughton, & Van Mook, 2014). The interviews began with inductive questioning regarding the PTs’ clinical decision-making during gym- and Lokomat-based interventions and finished with the PTs reflecting on their MLS use in the video clips. The number of videos used in each interview depended on child consent and availability of video footage for each PT. Bias towards specific MLS was avoided by using open-ended rather than targeted questions (Hsieh & Shannon, 2005) (e.g., asking about “the things you do/say to teach children” rather than “the MLS you use to teach children”). Inductive questioning also prevented over-reporting of MLS and allow PTs to use their preferred vocabulary (Figure 1). The interviews were audio-recorded and transcribed.
Figure 1.
Interview guide.
Analysis
Primary coding occurred after each interview using NVivo 8.0. The first three transcripts were independently coded by the first author and a research assistant (RA) and compared to ensure consistency of coding. The remaining transcripts were either coded by the RA (three) or the first author (two). Three data analysis meetings took place throughout the interview period, where the study team reviewed coding, categorizing, and analysis to date. Directed content analysis involved data coding using a deductive approach (Hsieh & Shannon, 2005) where all instances of specific MLS identified in the transcripts were highlighted and coded with predetermined MLS from the items in the MLSRI-20 (Table 1). Any text that could not be categorized using the MLSRI-20 items was identified and coded using inductive category development (Hsieh & Shannon, 2005). The MLSRI-20 scoring system was not pertinent to the coding process.
As the data set expanded, analysis occurred within and between interviews, using a modified constant comparative method (CCM) (Boeije, 2002) where comparison occurred within and between PTs, within and between treatment approaches, and within and between children. These comparisons strengthened the internal and external validity of the study findings (Boeije, 2002). The analysis was considered complete once all alternative explanations were considered, and the resultant themes were consistent and defensible (Beveridge et al., 2015).
Results
Three themes representing the PTs’ decisions and experiences using MLS during intervention were developed during the analysis meetings. (All names are pseudonyms.)
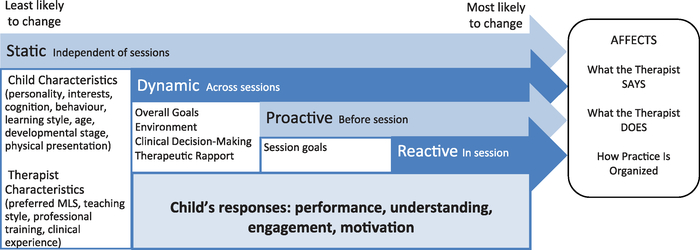
MLS use is influenced by child, PT, and intervention-related factors
MLS use is driven by the unique aspects of the child, PT, and intervention which are embedded in time-dependent static, dynamic, proactive, and reactive factors (Figure 2). “Static factors” comprise child and therapist characteristics that remain relatively unchanged in the immediate future (e.g., during a block of intervention), including child physical presentation, cognitive abilities, age, developmental stage, learning style, behavior; and therapist teaching style, professional training, and clinical experience. Participants indicated that child characteristics had the strongest influence on their MLS decision-making and use. They drew upon knowledge of a child’s characteristics to promote active involvement and optimize opportunities for ML.
Figure 2.
The factors influencing MLS use in pediatric physiotherapy intervention.
[I] see what sparks them, see when they start to pay more attention to what I’m saying, see what their language is and what they want to talk about. I really watch and listen and try to go with their lead … and then I say what I want to say but within their topic or [within] their ability to understand. (Brigette)
“Dynamic factors” refer to aspects of intervention likely to change over a number of sessions. They are based on the child’s goals coupled with the PT’s clinical decision-making, therapeutic environment, equipment available, and therapeutic rapport. The PT determines how the child responds to MLS by observing his/her performance, understanding, engagement, and motivation across the sessions. MLS use is continually adapted based on the child’s abilities.
… our starting point changes each time, as they can do more and more. So my verbal cues or my physical cues might change as they do more difficult things or they need less help with the previous things. (Brigette)
“Proactive factors” identify how the PT prepares for a single treatment session. She considers static and dynamic factors while developing session-specific goals. Reflection on the child’s past responses to MLS influences the tasks/strategies she plans to apply in the upcoming session. The child’s past engagement and motor performance influence how she varies and progresses tasks in subsequent sessions.
[I] think about what we did during the last session and hopefully, you know, you’ve seen some changes in what they’re doing … how can I progress the activities that we were already doing to kind of challenge them further? … If they’re bored with certain activities, then I’m … coming up with different ideas … (Justine)
“Reactive factors” are the least stable of the four factors, and refer to the PT’s immediate responses within a session. These clinical decisions are based on visual, auditory, and tactile observations. In addition to considering child characteristics and assessing immediate performance, the PT analyses behavior, engagement, and motivation. Reactive factors may be the most influential as they are context-specific and highly dependent upon the child’s actions/reactions to the MLS presented in the session, often resulting in the instantaneous adaptation of their plans.
I like to have that set treatment plan but what happens in a session … is somewhat directed by the kid … I have to react to everything they’re feeding me. (Kim)
The use and description of motor learning content varies among PTs
Inductive questioning allowed PTs to describe their clinical decision-making using their own vocabulary. “Motor learning” was mentioned infrequently and inconsistently (e.g., nine times by three of the eight PTs). Instead, therapists described ML using terminology such as “carryover,” “translate,” or “integrate.” While the MLSRI-20 categorizes MLS as “What the therapist SAYS,” “What the therapist DOES,” and how the “Practice IS” organized, the PTs described their approaches in terms of “verbal,” “tactile,” and “visual” cues.
… usually I use verbal instructions and verbal feedback. If I find that it’s not working … I tend to go to tactile stuff … and then I’ll use the visual. (Kaillie)
When asked to describe their approach to treatment, the PTs initially focused on session organization, indicating they planned several tasks prior to the session. They did not specifically plan what they would “do” or “say,” nor did they refer to current ML evidence. When probed, they stated that they begin tasks using verbal instruction and augment with demonstration and/or physical guidance, depending on child characteristics and initial task performance. They reworded instructions/feedback based on the child’s performance, understanding, and engagement.
At times, the PTs used the same words amongst each other to discuss the same concepts, while other times they used the same words to describe different concepts. For example, “visual” was used to convey multiple concepts, including:
External focus of attention: “Rather than saying ‘take a big step’ … we put a toy there so that his knee can come up to the toy … so there’s something visual for him to target.” (Tessa)
Demonstrating a task: “ … so some children do better with that visual demonstration and I have others who don’t like the visual … processing all that visual information is very challenging for them and often makes them more confused.” (Alex)
Use of visual feedback: “I try to use visual cues as well … if it’s an activity they can do in front of a mirror … I give that visual feedback for them as well, so it’s not just me describing … ” (Justine)
They used varying terminology within and among themselves to describe physical guidance, which was implemented as a form of instruction, feedback, and task progression.
He was a little bit more cognitively delayed, and so very simple tactile cues … were much more effective than me trying to use words to describe what I was hoping for. (Laurie)
… take away some of my support … have them do an activity without any guidance … take away … or vary my amount of assistance. (Brigette)
The following MLS were mentioned once across the eight interviews: recommending practice beyond therapy; mental practice; providing education; and random practice order. “Encouraging errors” and “linking an activity practiced in therapy to another activity” were not specifically discussed. However, encouraging errors was implied when the PTs mentioned progressing the challenge of a task, whereby they adjusted the level of difficulty to encourage a certain degree of failure without the child feeling that completing the task was impossible. Several MLS not included in the MLSRI-20 were discussed: “analogy learning,” “visual feedback,” and “auditory feedback.”
The Lokomat is the “same but different”
Both treatment approaches permitted the PTs to work toward gait-based ML goals. Using the Lokomat was compared to introducing a piece of equipment with unique properties in a gym-based session. Regardless of the equipment, the PTs used similar decision-making when integrating it within an intervention.
I don’t feel it’s very different in terms of the way that I do it … the Lokomat is just a different thing, right? There are the parallel bars, there is walking with a walker, there is the Lokomat. (Kaillie)
While the Lokomat has features/capabilities that differ from the equipment in gym-based interventions, the child’s characteristics remain constant. Given the focus on child characteristics for MLS-based decision-making, the PTs applied many of the same MLS across both types of intervention. They emphasized the importance of child engagement and repetition of practice across both treatment approaches. The PTs broke tasks down into components and emphasized part practice when initially addressing a skill. Then they consolidated the skill by combining the components together and emphasizing whole practice. While the process may appear slightly different between the gym- and Lokomat-based sessions, the PTs’ intentions were the same.
The PTs reported less “freedom” regarding task options in the Lokomat compared to gym-based intervention and expressed the desire to work on gait-related skills and “trunk control” in more situations than simply walking. Consequently, they had to be creative in how they addressed certain goals (e.g., strengthening a muscle group) when constrained by the Lokomat. At times they drew upon the Lokomat’s novel properties, such as augmentative feedback, to keep the child motivated. Fewer task options in the Lokomat led to less planning prior to intervention. However, similar to gym-based intervention, the PTs still focused on task progression in the Lokomat.
My ultimate goal [in the Lokomat] is if I can take off as much support as possible and get the [kids] as active as possible. (Tessa)
Physical guidance was an important MLS for children with greater motor impairment across both treatment approaches. However, when the Lokomat provided the guidance, the PTs could focus on other MLS, such as using more verbal instructions and feedback. The PTs felt their manual facilitation differed from the Lokomat’s support, which led to varied description of physical guidance between interventions. They described the physical guidance in gym-based sessions as “facilitating,” “finessing,” “cueing,” or “providing feedback” while the physical guidance in the Lokomat was described as “support.” Several PTs remarked that the Lokomat’s physical guidance “prevented” or “hid” mistakes.
Discussion
Rather than grounding clinical decision-making in ML evidence, child characteristics were at the forefront of the PTs’ MLS selection and implementation, regardless of treatment approach. These characteristics provided the foundation for the static, dynamic, proactive, and reactive factors that influenced how the PTs selected and used MLS. There were aspects of intervention that remained consistent over a block of treatment and elements that gradually changed. These findings confirm the need to plan for interventions based on the child’s goals and past performances, while acknowledging the inevitability of instantaneous clinical decision-making during intervention. Awareness of these influencing factors permit PTs to prepare for and reflect upon a treatment session, as well as identify and evaluate the effects of certain MLS with each child.
Similarities in the verbalizations used in gym- and Lokomat-based interventions were linked to child characteristics rather than PT preference or the properties of the treatment approach. However, differing MLS vocabulary made it challenging, at times, to distinguish between how the PTs’ individual style and/or clinical experience influenced MLS selection. PTs integrate observational skills, professional training, and clinical experience into their decision-making (Levac, Miller, & Missiuna, 2012; Wainwright, Shepard, Harman, & Stephens, 2011). Thus, some aspects of MLS implementation are inherently unique to the PT and are a product of accumulated clinical knowledge. Clinical decision-making extends beyond interpreting physical performance to analyzing the cognitive and affective factors that influence a child’s understanding and engagement in intervention (Levac et al., 2012; Wainwright et al., 2011).
While there are obvious differences in the Lokomat’s properties and the tasks performed within it, the PTs appeared to use decision-making similar to gym-based intervention. They considered the features of the Lokomat as they would consider the properties of equipment used in gym-based intervention and maximized opportunities for ML based on its capabilities and the child’s goals. The PTs reflected upon the successes and challenges of each session, which promotes continuing progress toward treatment goals (Wainwright et al., 2011).
The MLS documented in other Lokomat studies emphasize repetition and progression (Bang & Shin, 2016; Borggraefe et al., 2010; Meyer-Heim et al., 2009; Wallard et al., 2018) with occasional reference to augmentative feedback (Wallard et al., 2018), and verbal encouragement (Borggraefe et al., 2010). The PTs in this study reiterated the value of these MLS, and also identified increased opportunity for verbal feedback and visual demonstration with more physically involved children when the Lokomat provides the physical guidance instead of the PT. While the PTs acknowledged greater difficulty maintaining intensity and maximizing repetition in gym-based intervention, they identified the ability to practice of a greater range of functional movements which they associated with enhanced opportunity to generalize skills beyond intervention. In contrast with previous interview studies (Larsson, Miller, Liljedahl, & Gard, 2012; Levac et al., 2012), there was limited discussion about providing education or recommending practice beyond therapy, which may have been related to these MLS inherently occurring less frequently than conventional MLS (e.g., verbal instruction/feedback, physical guidance, repetition).
A lack of conclusive evidence supporting/refuting the use of specific MLS in children with CP complicates their implementation in intervention. Existing studies have small sample sizes (Burtner et al., 2014; Jongsma et al., 2016; Thorpe & Valvano, 2002), narrow sample specificity (e.g., unilateral CP) (Burtner et al., 2014; Cabral-Sequeira, Coelho, & Teixeira, 2016; Jongsma et al., 2016; van der Kamp, Steenbergen, & Masters, 2017), and focus on simple, lab-based movements (Burtner et al., 2014; Cabral-Sequeira et al., 2016; van der Kamp et al., 2017) which fails to reflect the diversity of CP and the motor skill complexity required for daily function. However, studying the controlled use of MLS in a therapeutic environment is often impractical due to the need to adjust MLS based on child characteristics and reactive factors arising during intervention. Differing MLS terminology among clinicians and researchers complicates literature searches and impedes the interpretation of study results, thus preventing PTs from reflecting upon and applying findings in their practice. Currently, PTs can choose to apply MLS based on limited CP-specific evidence, adapt adult-based ML theory using their clinical experience, or employ approaches that broadly use MLS groups (Levac et al., 2009) (e.g., cognitive orientation to occupational performance (Cameron et al., 2017), neuromotor task training (Schoemaker, Niemeijer, Reynders, & Smits-Engelsman, 2003), family-centered functional therapy (Law et al., 1998), and activity-focused motor interventions (Valvano, 2004)). This study identifies the need to adopt a common MLS language and systematically document MLS use within interventions, both of which can be accomplished using the MLSRI-20. The MLSRI-20 permits transparent reporting of research protocols, allows comparison between treatment approaches, and facilitates the study of the effects of MLS implementation on ML. Additionally, its implementation should enhance interprofessional communication and create greater awareness of the range of MLS, which would promote intentional MLS use in therapeutic intervention. Enhanced awareness and increased CP-specific MLS evidence will permit future development of practice guidelines for MLS use.
To the authors’ knowledge, this is the first published qualitative study addressing both ML and clinical decision-making in physiotherapy for children with CP. Comparing gym- and Lokomat-based interventions allowed investigation of possible differences in clinical rationale depending upon treatment approach. This study was nested within several ongoing clinical trials comparing the efficacy of gym- and Lokomat-based intervention. While the clinical trials mimicked child-centered clinical treatment, it is unknown if PTs’ perspectives would differ in a clinical setting. The primary reported difference was the reduced treatment duration in the clinical trial (e.g., 30 minutes), may have limited opportunities for using MLS requiring more in-depth explanation, such as education or mental practice. As a treating PT in the Lokomat studies, the first author has specific clinical experience that shaped the interpretation of data collected in this study. As the study interviewer, her familiarity with some study participants may have influenced their responses. Inductive questioning was used, in part, to offset interviewer influence and allow in-depth examination of the PTs’ vocabulary. Inductive questioning may have caused PTs to overlook specific MLS experiences that could have been captured using deductive questioning. However, deductive questioning would have biased the PTs’ responses toward the MLS outlined in the MLSRI-20.
Conclusions
This study highlights the influence of the child, therapist, and treatment approach in MLS implementation in gait-based physiotherapy intervention for children with CP. Adopting a common MLS language among PTs will increase communication, awareness, and intentional use of MLS. Not only does the MLSRI-20 provide the framework for using a common language, but it supports the comparison of novel treatment approaches and permits future study of the impact of MLS use on ML in children with CP.
Acknowledgments
The authors would like to thank the physiotherapist participants. We also extend our appreciation to Research Assistant Celia Cassiani and Research Manager Gloria Lee for their roles in data analysis and obtaining child/parent consent, respectively.
Funding
This study was funded by the Holland Bloorview Children’s Foundation Chair in Pediatric Rehabilitation.
About the Authors
Jennifer Ryan, PT, Msc, is a clinical physiotherapist at Holland Bloorview Kids Rehabilitation Hospital and a PhD student at the Rehabilitation Sciences Institute, University of Toronto. Her research interests include optimizing motor learning in interventions for children with neuromotor disabilities and studying the effects of innovative technologies as adjuncts to traditional treatment approaches.
Virginia Wright, PT, PhD, is a senior scientist at Bloorview Research Institute and Professor in the Department of Physical Therapy, University of Toronto. Her research includes the design and evaluation of advanced gross motor skills outcome measures. She also evaluates clinically-integrated innovative interventions that promote functional mobility, physical activity, and participation in children and youth of diverse abilities.
Danielle Levac, PT, PhD, is Assistant Professor at Northeastern University and the Director of the Rehabilitation Games and Virtual Reality Lab. Her research focuses on the evidence-based integration of virtual reality in rehabilitation and evaluating how it promotes motor learning in children and adults with neuromotor disabilities.
Footnotes
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Atun-Einy O, & Kafri M (2018). Implementation of motor learning principles in physical therapy practice: Survey of physical therapists’ perceptions and reported implementation. Physiotherapy Theory and Practice, 35(7), 633–644. doi: 10.1080/09593985.2018.1456585 [DOI] [PubMed] [Google Scholar]
- Bang DH, & Shin WS (2016). Effects of robot-assisted gait training on spatiotemporal gait parameters and balance in patients with chronic stroke: A randomized controlled pilot trial. NeuroRehabilitation, 38(4), 343–349. doi: 10.3233/NRE-161325 [DOI] [PubMed] [Google Scholar]
- Bax M, Goldstein M, Rosenbaum P, Leviton A, Paneth N, Dan B, … Damiano D (2005). Proposed definition and classification of cerebral palsy, April 2005. Developmental Medicine & Child Neurology, 47(8), 571–576. doi: 10.1017/S001216220500112X [DOI] [PubMed] [Google Scholar]
- Beveridge B, Feltracco D, Struyf J, Strauss E, Dang S, Phelan S, … Gibson BE (2015). “You gotta try it all”: Parents’ experiences with robotic gait training for their children with cerebral palsy. Physical & Occupational Therapy in Pediatrics, 35(4), 327–341. doi: 10.3109/01942638.2014.990547 [DOI] [PubMed] [Google Scholar]
- Boeije H (2002). A purposeful approach to the constant comparative method in the analysis of qualitative interviews. Quality and Quantity, 36(4), 391–409. [Google Scholar]
- Borggraefe I, Kiwull L, Schaefer JS, Koerte I, Blaschek A, Meyer-Heim A, & Heinen F (2010). Sustainability of motor performance after robotic-assisted treadmill therapy in children: An open, non-randomized baseline-treatment study. European Journal of Physical and Rehabilitation Medicine, 46(2), 125–131. [PubMed] [Google Scholar]
- Burtner PA, Leinwand R, Sullivan KJ, Goh HT, & Kantak SS (2014). Motor learning in children with hemiplegic cerebral palsy: Feedback effects on skill acquisition. Developmental Medicine & Child Neurology, 56(3), 259–266. doi: 10.1111/dmcn.12364 [DOI] [PubMed] [Google Scholar]
- Cabral-Sequeira AS, Coelho DB, & Teixeira LA (2016). Motor imagery training promotes motor learning in adolescents with cerebral palsy: Comparison between left and right hemiparesis. Experimental Brain Research, 234(6), 1515–1524. doi: 10.1007/s00221-016-4554-3 [DOI] [PubMed] [Google Scholar]
- Cameron D, Craig T, Edwards B, Missiuna C, Schwellnus H, & Polatajko HJ (2017). Cognitive Orientation to Daily Occupational Performance (CO-OP): A new approach for children with cerebral palsy. Physical & Occupational Therapy in Pediatrics, 37(2), 183–198. doi: 10.1080/01942638.2016.1185500 [DOI] [PubMed] [Google Scholar]
- Diaz Heijtz R, & Forssberg H (2015). Translational studies exploring neuroplasticity associated with motor skill learning and the regulatory role of the dopamine system. Developmental Medicine & Child Neurology, 57(s2), 10–14. doi: 10.1111/dmcn.12692 [DOI] [PubMed] [Google Scholar]
- Hayes MS, McEwen IR, Lovett D, M’Lisa MS, & Smith DW (1999). Next step: Survey of Pediatric physical therapists’ educational needs and perceptions of motor control, motor development and motor learning as they relate to services for children with developmental disabilities. Pediatric Physical Therapy, 11(4), 164–182. [Google Scholar]
- Hemayattalab R, & Rostami LR (2010). Effects of frequency of feedback on the learning of motor skill in individuals with cerebral palsy. Research in Developmental Disabilities, 31(1), 212–217. doi: 10.1016/j.ridd.2009.09.002 [DOI] [PubMed] [Google Scholar]
- Hsieh HF, & Shannon SE (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Jongsma ML, Baas CM, Sangen AF, Aarts PB, Van der Lubbe RH, Meulenbroek RG, & Steenbergen B (2016). Children with unilateral cerebral palsy show diminished implicit motor imagery with the affected hand. Developmental Medicine & Child Neurology, 58(3), 277–284. doi: 10.1111/dmcn.12819 [DOI] [PubMed] [Google Scholar]
- Larin H (2007). Quantifying instructional interventions in pediatric physical therapy with the Motor Teaching Strategies Coding Instrument (MTSCI-1): A pilot study. Internet Journal of Allied Health Sciences and Practice, 5(1), 8. [Google Scholar]
- Larin HM (1998). Motor learning: A practical framework for paediatric physiotherapy. Physiotherapy Theory and Practice, 14(1), 33–47. doi: 10.3109/09593989809070042 [DOI] [Google Scholar]
- Larsson I, Miller M, Liljedahl K, & Gard G (2012). Physiotherapists’ experiences of physiotherapy interventions in scientific physiotherapy publications focusing on interventions for children with cerebral palsy: A qualitative phenomenographic approach. BMC Pediatrics, 12(1), 90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Law M, Darrah J, Pollock N, King G, Rosenbaum P, Russell D, … Watt J (1998). Family-centred functional therapy for children with cerebral palsy: An emerging practice model. Physical & Occupational Therapy in Pediatrics, 18(1), 83–102. doi: 10.1080/J006v18n01_06 [DOI] [Google Scholar]
- Levac D, Miller P, & Missiuna C (2012). Usual and virtual reality video game-based physiotherapy for children and youth with acquired brain injuries. Physical & Occupational Therapy in Pediatrics, 32(2), 180–195. doi: 10.3109/01942638.2011.616266 [DOI] [PubMed] [Google Scholar]
- Levac D, Missiuna C, Wishart L, DeMatteo C, & Wright V (2011). Documenting the content of physical therapy for children with acquired brain injury: Development and validation of the Motor Learning Strategy Rating Instrument. Physical Therapy, 91(5), 689–699. doi: 10.2522/ptj.20100415 [DOI] [PubMed] [Google Scholar]
- Levac D, Wishart L, Missiuna C, & Wright V (2009). The application of motor learning strategies within functionally based interventions for children with neuromotor conditions. Pediatric Physical Therapy, 21(4), 345–355. doi: 10.1097/PEP.0b013e3181beb09d [DOI] [PubMed] [Google Scholar]
- Malterud K, Siersma VD, & Guassora AD (2016). Sample size in qualitative interview studies guided by information power. Qualitative Health Research, 26(13), 1753–1760. doi: 10.1177/1049732315617444 [DOI] [PubMed] [Google Scholar]
- Meyer-Heim A, Ammann-Reiffer C, Schmartz A, Schafer J, Sennhauser FH, Heinen F, … Borggraefe I (2009). Improvement of walking abilities after robotic-assisted locomotion training in children with cerebral palsy. Archives of Disease in Childhood, 94(8), 615–620. doi: 10.1136/adc.2008.145458 [DOI] [PubMed] [Google Scholar]
- Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, & Galuppi B (2008). Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine & Child Neurology, 39(4), 214–223. doi: 10.1111/j.14698749.1997.tb07414.x [DOI] [PubMed] [Google Scholar]
- Patton MQ (2002). Qualitative interviewing. Qualitative Research and Evaluation Methods, 3, 344–347. [Google Scholar]
- Pool D, Blackmore AM, Bear N, & Valentine J (2014). Effects of short-term daily community walk aide use on children with unilateral spastic cerebral palsy. Pediatric Physical Therapy, 26(3), 308–317. doi: 10.1097/PEP.0000000000000057 [DOI] [PubMed] [Google Scholar]
- Ryan JL, Levac DE, & Wright FV (2019). Reliability of the Motor Learning Strategies Rating Instrument in physiotherapy intervention for children with cerebral palsy. Developmental Medicine & Child Neurology. 10.1111/dmcn.14177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan JL, Wright FV, & Levac DE (2016). Motor learning strategies rating instrument instruction manual. Toronto: Bloorview Research Institute. [Google Scholar]
- Schmidt RA, & Wrisberg CA (2004). Motor learning and performance (4th ed.). Windsor: Human Kinetics. [Google Scholar]
- Schoemaker M, Niemeijer A, Reynders K, & Smits-Engelsman B (2003). Effectiveness of neuromotor task training for children with developmental coordination disorder: A pilot study. Neural Plasticity, 10(1–2), 155–163. doi: 10.1155/NP.2003.155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stalmeijer RE, McNaughton N, & Van Mook WN (2014). Using focus groups in medical education research: AMEE Guide No. 91. Medical Teacher, 36(11), 923–939. doi: 10.3109/0142159X.2014.917165 [DOI] [PubMed] [Google Scholar]
- Teodoro IPP, Rebouças VCF, Thorne SE, Souza NKM, Brito LSA, & Alencar AMPG (2018). Interpretive description: A viable methodological approach for nursing research. Escola Anna Nery, 22(3), 1–8. [Google Scholar]
- Thorpe DE, & Valvano J (2002). The effects of knowledge of performance and cognitive strategies on motor skill learning in children with cerebral palsy. Pediatric Physical Therapy, 14(1), 2–15. doi: 10.1097/00001577-200214010-00002 [DOI] [PubMed] [Google Scholar]
- Valvano J (2004). Activity-focused motor interventions for children with neurological conditions. Physical & Occupational Therapy in Pediatrics, 24(1–2), 79–107. doi: 10.1300/J006v24n01_04 [DOI] [PubMed] [Google Scholar]
- van der Kamp J, Steenbergen B, & Masters RS (2017). Explicit and implicit motor learning in children with unilateral cerebral palsy. Disability and Rehabilitation, 40(23), 2790–2797. [DOI] [PubMed] [Google Scholar]
- Wainwright SF, Shepard KF, Harman LB, & Stephens J (2011). Factors that influence the clinical decision making of novice and experienced physical therapists. Physical Therapy, 91(1), 87–101. doi: 10.2522/ptj.20100161 [DOI] [PubMed] [Google Scholar]
- Wallard L, Dietrich G, Kerlirzin Y, & Bredin J (2018). Effect of robotic-assisted gait rehabilitation on dynamic equilibrium control in the gait of children with cerebral palsy. Gait and Posture, 60, 55–60. doi: 10.1016/j.gaitpost.2017.11.007 [DOI] [PubMed] [Google Scholar]
- Winkels DG, Kottink AI, Temmink RA, Nijlant JM, & Buurke JH (2013). Wii™ – Habilitation of upper extremity function in children with cerebral palsy. An explorative study. Developmental Neurorehabilitation, 16(1), 44–51. doi: 10.3109/17518423.2012.713401 [DOI] [PubMed] [Google Scholar]