Abstract
Objectives:
The present study evaluates the items of the Hearing Handicap Inventory for the Elderly and Hearing Handicap Inventory for Adults (HHIE/A) using Mokken scale analysis, a type of nonparametric item response theory, and develops updated tools with optimal psychometric properties.
Design:
In a longitudinal study of age-related hearing loss, 1447 adults completed the HHIE/A and audiometric testing at baseline. Discriminant validity of the emotional consequences and social/situations effects subscales of the HHIE/A was assessed and nonparametric item response theory was used to explore dimensionality of the items of the HHIE/A and to refine the scales.
Results:
The HHIE/A items form strong unidimensional scales measuring self-perceived hearing handicap, but with a lack of discriminant validity of the two distinct subscales. Two revised scales, the 18-item Revised Hearing Handicap Inventory (RHHI) and the 10-item Revised Hearing Handicap Inventory – Screening (RHHI-S), were developed from the common items of the original HHIE/A that met the assumptions of Mokken scale analysis. The items on both of the revised scales can be ordered in terms of increasing difficulty.
Conclusions:
The results of the present study suggest that the newly developed RHHI and RHHI-S are strong unidimensional, clinically informative measures of self-perceived hearing handicap that can be used for adults of all ages. The real-data example also demonstrated that Mokken scale analysis is a valuable alternative to classical psychometric analysis.
INTRODUCTION
It is well-known that hearing loss is one of the most common chronic conditions of aging. The magnitude of hearing loss is typically evaluated in clinical settings using behavioral measures such as pure-tone audiometry and speech recognition. However, these tests do not assess the perceived handicap associated with a hearing loss or effects of hearing loss on an individual’s quality of life (Ventry & Weinstein 1982). Cross-sectional studies report only modest associations between perceived hearing handicap and measured clinical outcomes, suggesting that increased hearing handicap is not completely explained by increased pure-tone thresholds or reduced speech recognition (e.g. Matthews et al. 1990; Newman et al. 1990; Weinstein & Ventry 1983). In light of the relatively poor predictive value of these traditional clinical outcome measures, patient-reported outcome measures (PROMs; see Table 1 for a list of abbreviations), such as self-reported hearing handicap, should be included as a component in the comprehensive assessment of the functional communication abilities of individuals with hearing loss. Results of PROMs could also guide decisions on who may best benefit from interventions with services and technologies.
Table 1.
Abbreviations.
| Abbreviation | Definition |
|---|---|
| AISP* | Automated Item Selection Procedure |
| CFA | Confirmatory Factor Analysis |
| CTT | Classical Test Theory |
| DMM | Double Monotonicity Model |
| EFA | Exploratory Factor Analysis |
| GA | Genetic Algorithm |
| HHIA | Hearing Handicap Inventory for Adults |
| HHIE | Hearing Handicap Inventory for the Elderly |
| HHIE/A | Hearing Handicap Inventory for the Elderly and Hearing Handicap Inventory for Adults |
| HTMT | Heterotrait-Monotrait |
| IIO | Invariant Item Ordering |
| IRF | Item Response Function |
| IRT | Item Response Theory |
| ISRF | Item Step Response Function |
| MHM | Monotone Homogeneity Model |
| MIIO | Manifest Invariant Item Ordering |
| MSA | Mokken Scale Analysis |
| MUSC | Medical University of South Carolina |
| PROM | Patient-Reported Outcome Measure |
| PTA | Pure-Tone Average |
| RHHI | Revised Hearing Handicap Inventory |
| RHHI-S | Revised Hearing Handicap Inventory – Screening |
| ROC | Receiver Operating Characteristic |
| SD | Standard Deviation |
| SE | Standard Error |
Introduced in Supplemental Digital Content 1.
Developed in 1982 (Ventry & Weinstein), the Hearing Handicap Inventory for the Elderly (HHIE) was one of the first hearing-related PROMs intended for clinical use. The HHIE has 25 questions, or items, designed to assess self-perceived hearing handicap in older adults on two subscales, emotional consequences and social/situational effects due to hearing loss. In 1990, Newman et al. developed the Hearing Handicap Inventory for Adults (HHIA) by modifying three questions of the HHIE that were more specific to older adults and were substituted with questions that were deemed more appropriate for younger adults (two of which refer to the workplace). The items comprising the HHIE and HHIA are listed in the second column of Tables 2 and 3, respectively. Both of the 25-item clinical instruments were also reduced to 10-item screening tools with 5 items from each subscale (Newman et al. 1991; Ventry & Weinstein 1983). The items comprising the screening versions are denoted with an asterisk (*) in Tables 2 and 3.
Table 2.
Descriptive statistics for the Hearing Handicap Inventory for the Elderly (HHIE).
| ID | Item | n | Mean (SD) | Median | Range | Assigned “0” response (%) |
|---|---|---|---|---|---|---|
| S-1. | Does a hearing problem cause you to use the phone less often than you would like? | 1064 | 0.45 (1.12) | 0 | 0-4 | 901 (84.7) |
| E-2.* | Does a hearing problem cause you to feel embarrassed when meeting new people? | 1064 | 0.70 (1.22) | 0 | 0-4 | 766 (72.0) |
| S-3. | Does a hearing problem cause you to avoid groups of people? | 1064 | 0.54 (1.15) | 0 | 0-4 | 849 (79.8) |
| E-4. | Does a hearing problem make you irritable? | 1063 | 0.68 (1.17) | 0 | 0-4 | 764 (71.9) |
| E-5.* | Does a hearing problem cause you to feel frustrated when talking to members of your family? | 1064 | 1.08 (1.43) | 0 | 0-4 | 627 (58.9) |
| S-6. | Does a hearing problem cause you difficulty when attending a party? | 1064 | 1.32 (1.57) | 0 | 0-4 | 569 (53.5) |
| E-7. | Does a hearing problem cause you to feel “stupid” or “dumb”? | 1064 | 0.48 (1.06) | 0 | 0-4 | 865 (81.3) |
| S-8.* | Do you have difficulty hearing when someone speaks in a whisper? | 1064 | 2.30 (1.58) | 2 | 0-4 | 266 (25.0) |
| E-9.* | Do you feel handicapped by a hearing problem? | 1064 | 0.82 (1.34) | 0 | 0-4 | 740 (69.5) |
| S-10.* | Does a hearing problem cause you difficulty when visiting friends, relatives, or neighbors? | 1064 | 0.84 (1.28) | 0 | 0-4 | 705 (66.3) |
| S-11.* | Does a hearing problem cause you to attend religious services less often than you would like? | 1064 | 0.17 (0.71) | 0 | 0-4 | 999 (93.9) |
| E-12. | Does a hearing problem cause you to be nervous? | 1064 | 0.37 (0.94) | 0 | 0-4 | 901 (84.7) |
| S-13. | Does a hearing problem cause you to visit friends, relatives, or neighbors less often than you would like? | 1063 | 0.20 (0.76) | 0 | 0-4 | 985 (92.7) |
| E-14.* | Does a hearing problem cause you to have arguments with family members? | 1064 | 0.55 (1.10) | 0 | 0-4 | 828 (77.8) |
| S-15.* | Does a hearing problem cause you difficulty when listening to TV or radio? | 1064 | 1.49 (1.54) | 2 | 0-4 | 485 (45.6) |
| S-16. | Does a hearing problem cause you to go shopping less often than you would like? | 1064 | 0.10 (0.53) | 0 | 0-4 | 1020 (95.9) |
| E-17. | Does any problem or difficulty with your hearing upset you at all? | 1064 | 1.10 (1.40) | 0 | 0-4 | 607 (57.0) |
| E-18. | Does a hearing problem cause you to want to be by yourself? | 1064 | 0.25 (0.81) | 0 | 0-4 | 959 (90.1) |
| S-19. | Does a hearing problem cause you to talk to family members less often than you would like? | 1064 | 0.30 (0.88) | 0 | 0-4 | 940 (88.3) |
| E-20.* | Do you feel that any difficulty with your hearing limits or hampers your personal or social life? | 1064 | 0.72 (1.26) | 0 | 0-4 | 766 (72.0) |
| S-21.* | Does a hearing problem cause you difficulty when in a restaurant with relatives or friends? | 1064 | 1.31 (1.48) | 0 | 0-4 | 538 (50.6) |
| E-22. | Does a hearing problem cause you to feel depressed? | 1064 | 0.22 (0.73) | 0 | 0-4 | 969 (91.1) |
| S-23. | Does a hearing problem cause you to listen to TV or radio less often than you would like? | 1064 | 0.33 (0.99) | 0 | 0-4 | 945 (88.8) |
| E-24. | Does a hearing problem cause you to feel uncomfortable when talking to friends? | 1064 | 0.68 (1.13) | 0 | 0-4 | 751 (70.6) |
| E-25. | Does a hearing problem cause you to feel left out when you are with a group of people? | 1064 | 0.89 (1.31) | 0 | 0-4 | 691 (64.9) |
Item included on the HHIE screening version. Items with “S” and “E” prefix comprised the original social/situational and emotional subscales, respectively.
Table 3.
Descriptive statistics for the Hearing Handicap Inventory for Adults (HHIA).
| ID | Item | n | Mean (SD) | Median | Range | Assigned “0” response (%) |
|---|---|---|---|---|---|---|
| S-1. | Does a hearing problem cause you to use the phone less often than you would like? | 305 | 0.37 (0.90) | 0 | 0-4 | 257 (84.3) |
| E-2.* | Does a hearing problem cause you to feel embarrassed when meeting new people? | 305 | 0.45 (0.99) | 0 | 0-4 | 248 (81.3) |
| S-3. | Does a hearing problem cause you to avoid groups of people? | 305 | 0.28 (0.81) | 0 | 0-4 | 270 (88.5) |
| E-4. | Does a hearing problem make you irritable? | 305 | 0.58 (1.14) | 0 | 0-4 | 234 (76.7) |
| E-5.* | Does a hearing problem cause you to feel frustrated when talking to members of your family? | 305 | 0.64 (1.23) | 0 | 0-4 | 231 (75.7) |
| S-6. | Does a hearing problem cause you difficulty when attending a party? | 305 | 0.75 (1.29) | 0 | 0-4 | 219 (71.8) |
| S-7.* | Does a hearing problem cause difficulty hearing/understanding coworkers, clients, or customers? | 305 | 0.85 (1.33) | 0 | 0-4 | 206 (67.5) |
| E-8.* | Do you feel handicapped by a hearing problem? | 305 | 0.37 (0.94) | 0 | 0-4 | 260 (85.2) |
| S-9.* | Does a hearing problem cause you difficulty when visiting friends, relatives, or neighbors? | 305 | 0.50 (1.04) | 0 | 0-4 | 240 (78.7) |
| E-10. | Does a hearing problem cause you to feel frustrated when talking to coworkers, clients, or customers? | 305 | 0.65 (1.21) | 0 | 0-4 | 228 (74.8) |
| S-11* | Does a hearing problem cause you difficulty in the movies or theater? | 305 | 0.49 (1.09) | 0 | 0-4 | 247 (81.0) |
| E-12. | Does a hearing problem cause you to be nervous? | 305 | 0.21 (0.63) | 0 | 0-4 | 274 (89.8) |
| S-13. | Does a hearing problem cause you to visit friends, relatives, or neighbors less often than you would like? | 305 | 0.10 (0.53) | 0 | 0-4 | 292 (95.7) |
| E-14.* | Does a hearing problem cause you to have arguments with family members? | 305 | 0.36 (0.90) | 0 | 0-4 | 258 (84.6) |
| S-15.* | Does a hearing problem cause you difficulty when listening to TV or radio? | 305 | 0.88 (1.32) | 0 | 0-4 | 200 (65.6) |
| S-16. | Does a hearing problem cause you to go shopping less often than you would like? | 305 | 0.04 (0.32) | 0 | 0-4 | 300 (98.4) |
| E-17. | Does any problem or difficulty with your hearing upset you at all? | 305 | 0.62 (1.14) | 0 | 0-4 | 228 (74.8) |
| E-18. | Does a hearing problem cause you to want to be by yourself? | 304 | 0.18 (0.68) | 0 | 0-4 | 281 (92.4) |
| S-19. | Does a hearing problem cause you to talk to family members less often than you would like? | 305 | 0.20 (0.72) | 0 | 0-4 | 281 (92.1) |
| E-20.* | Do you feel that any difficulty with your hearing limits or hampers your personal or social life? | 305 | 0.39 (0.95) | 0 | 0-4 | 255 (83.6) |
| S-21.* | Does a hearing problem cause you difficulty when in a restaurant with relatives or friends? | 305 | 0.69 (1.20) | 0 | 0-4 | 220 (72.1) |
| E-22. | Does a hearing problem cause you to feel depressed? | 305 | 0.15 (0.62) | 0 | 0-4 | 286 (93.8) |
| S-23. | Does a hearing problem cause you to listen to TV or radio less often than you would like? | 305 | 0.15 (0.60) | 0 | 0-4 | 285 (93.4) |
| E-24. | Does a hearing problem cause you to feel uncomfortable when talking to friends? | 305 | 0.37 (0.81) | 0 | 0-4 | 251 (82.3) |
| E-25. | Does a hearing problem cause you to feel left out when you are with a group of people? | 305 | 0.45 (0.99) | 0 | 0-4 | 248 (81.3) |
Item included on the HHIA screening version.
Most hearing-specific PROMs, including the Hearing Handicap Inventory for the Elderly and Hearing Handicap Inventory for Adults (HHIE/A) and their screening versions, were developed and validated using traditional psychometric analysis techniques known as classical test theory (CTT), utilizing methods such as Cronbach’s alpha and factor analysis (Boeschen Hospers et al. 2016; Newman et al. 1990; Ventry & Weinstein 1982). However, an assumption of CTT is interval-level measurement of the items, that is the differences between values is meaningful. The responses of many PROMs are ordered-categorical (for example: “yes”, “sometimes”, and “no” response categories of the HHIE/A), which violate the interval-level measurement assumption of CTT.
At the time of the development of the HHIE/A and their screening versions, the internal consistency of the scales was evaluated using Cronbach’s alpha but the other key measurement property of PROMs, validity, was not directly assessed. Specifically, despite extensive use of the HHIE/A in clinical and research settings, no verification was reported showing that the items underlying the subscales actually identified two distinct underlying, or latent, constructs. This property, where two conceptually similar constructs are distinct, is known as discriminant validity. The reported Pearson correlation between the emotional and social/situational subscales was high to very high [r = 0.87 and r = 0.84-0.96 for the HHIE (Ventry & Weinstein 1982) and HHIA (Newman et al. 1990), respectively] strongly suggesting that the two subscales do not measure distinct constructs, and that there is a lack of discriminant validity.
Evidence from exploratory factor analysis (EFA) has suggested that the HHIE may not resolve into the two defined subscales (Noble et al. 2008). Additionally, EFA of Filipino translated screening versions of the HHIE/A did not identify the purported subscales (Sjahalam-King & Newall 2016). However, EFA is a CTT-based method and using it to explore the dimensionality (the number of subscales represented by the items) is likely to lead to retention of too many factors or over-dimensionalization (van der Eijk & Rose 2015). This is true even when using polychoric correlation (a measure of the correlation between two observed ordered-categorical variables with an assumed latent normal distribution; van der Eijk & Rose 2015). In this study, we formally evaluate the discriminant validity of the two defined subscales using the heterotrait-monotrait (HTMT) ratio of polychoric correlations, which is a method that does not rely on CTT.
Modern psychometric techniques known collectively as item response theory (IRT) are designed to analyze ordered-categorical responses, such as those in the HHIE/A. Recently, these psychometric techniques have been used (often in combination with traditional methods) to develop and validate other hearing-related PROMs (Boeschen Hospers et al. 2016; Chenault et al. 2013; Demorest et al. 2011; Heffernan et al. 2018; Jessen et al. 2018; McRackan et al. 2018; Mokkink et al. 2010), but have not been applied to HHIE/A. In addition, dimensionality can be evaluated using Mokken scale analysis (MSA), which includes tools to evaluate IRT models (Cassarly et al. in press). Dimensionality results obtained from MSA for ordered-categorical items are more valid than results from EFA (van der Eijk & Rose 2015). Here, MSA is applied to the HHIE/A to explore dimensionality of the items and to examine their psychometric properties.
The first goal of the current study is to assess the discriminant validity of the two subscales of the HHIE/A. The second goal is to explore the dimensionality of the items of the HHIE/A using MSA. Following the assessment of dimensionality, MSA is used to evaluate and refine the original scales to construct updated tools.
MATERIALS AND METHODS
Outcome Measures
The outcome measures in the current study are the HHIE/A, which were designed to assess the effects of hearing loss on two subscales. The first subscale aims to explore the emotional consequences of hearing loss with 13 items. The second subscale aims to explore social and situational effects with 12 items. All of the 25 items are measured using an ordered response with three possible answers: “yes”, “sometimes”, or “no” (indicating either disagreement or not applicable), which are assigned scores of 4, 2, and 0, respectively. If subjects use hearing aids, they are instructed to answer as if unaided. The total score ranges from 0 to 100, the emotional subscale score ranges from 0 to 52, and the social/situational subscale score ranges from 0 to 48. Higher scores are indicative of greater perceived handicap. Descriptive statistics were used to summarize demographic and hearing-related characteristics of the subjects, as well as the HHIE/A item scores.
Data Sample
The protocols for this study were approved by the Institutional Review Board at the Medical University of South Carolina (MUSC). Data were obtained from an ongoing longitudinal study of age-related hearing loss at MUSC. In this study, which began in 1987, adults 18 years of age and older and in good general health are recruited through advertisements and subject referral. This cohort and the study protocol have been previously described in Lee et al. (2005), Matthews et al. (1997), and Dubno et al. (1995). Subjects with normal and impaired hearing who show no evidence of conductive hearing loss, active otologic disease, or significant cognitive decline are enrolled. Mean pure-tone averages (PTA) of hearing thresholds at 500, 1000, 2000, and 4000 Hz in the worse of the two ears for enrolled subjects are presented in Table 4. Subjects undergo a battery of tests, scheduled over the course of 3 to 6 visits, including conventional and extended high-frequency pure-tone air conduction thresholds, speech recognition measures in quiet and in noise, middle ear measurements, otoacoustic emissions, auditory brainstem responses, clinical blood chemistries, and a cognitive test battery. PROMs and other questionnaires are also completed and include self and family medical histories, hearing handicap, hearing health history (including noise history and hearing-aid use), and demographic information (ethnicity/race, sex, education level, marital status, and occupation). The HHIE/A is administered by paper and pencil to subjects before they answer any questions about hearing health history and prior to any audiological testing and knowledge of test results. After the initial test battery is completed, subjects are scheduled annually to obtain updated demographic information and medical and hearing health histories, and an audiogram. The full test battery is repeated every 2 to 3 years.
Table 4.
Characteristics of the subjects aged 60 years or older who completed the Hearing Handicap Inventory for the Elderly (HHIE), subjects less than 60 years old who completed the Hearing Handicap Inventory for Adults (HHIA), and all subjects who completed the initial test battery regardless of age.
| Completed HHIE (n = 1064) | Completed HHIA (n = 305) | All subjects (N = 1447) | |
|---|---|---|---|
| Age – years (mean ± SD) | 70.4 ± 6.7 | 44.0 ± 13.0 | 63.8 ± 14.0 |
| Sex – no. (%) | |||
| Female | 609 (57.2) | 162 (53.1) | 805 (55.6) |
| Male | 455 (42.8) | 143 (46.9) | 642 (44.4) |
| Race – no. (%) | |||
| White | 909 (85.4) | 160 (52.5) | 1140 (78.9) |
| Nonwhite | 154 (14.5) | 144 (47.2) | 305 (21.1) |
| Unknown | 1 (0.1) | 1 (0.3) | 2 (0.1) |
| Marital Status – no. (%) | |||
| Married | 649 (61.0) | 78 (25.6) | 778 (53.8) |
| Not Married | 380 (35.7) | 222 (72.8) | 624 (43.12) |
| Unknown | 35 (3.3) | 5 (1.6) | 45 (3.1) |
| Pure-tone average – dB HL (mean ± SD)* | 31.2 ± 15.7 | 15.3 ± 11.4 | 27.6 ± 16.3 |
Pure-tone average of audiometric thresholds at 500, 1000, 2000, and 4000 Hz in the worse ear; missing for 1 subject who completed the HHIE.
After an amendment to the study protocol in 2015, all subjects are administered a modified version of the HHIE/A that includes all 28 items from the HHIE and the HHIA, regardless of subjects’ age. Per the protocol, the HHIE for subjects aged 60 and older at the time of assessment is scored using the 25 items from the HHIE and the HHIA for subjects who are less than 60 years old is scored using the 25 HHIA items. Before 2015, the HHIE was administered to subjects aged 60 years and older and the HHIA was administered to subjects less than 60 years old. In the years before the HHIA was developed, the HHIE was administered to all subjects, regardless of age.
A total of 1447 subjects from the study completed the initial test battery, including the HHIE/A. At the time of completion of the baseline HHIE/A, 1068 subjects were aged 60 years or older and 379 were less than 60 years old. A total of 74 subjects less than 60 years old completed the HHIE and 4 subjects aged 60 years and older completed the HHIA; these subjects were excluded from the dimensionality assessment. Thus, the 1064 subjects who completed the HHIE and the 305 who completed the HHIA were included in the analysis exploring dimensionality of the scales.
Psychometric Analysis
The following section introduces the method used to evaluate the discriminant validity of the original subscales of the HHIE/A in addition to the nonparametric IRT approaches used to explore dimensionality of the items and reevaluate the scales.
Discriminant Validity: Evaluating the Distinctiveness of the Subscales
The HTMT ratio of polychoric correlations was used to evaluate the discriminant validity of the two latent constructs (emotional and social/situational) of the HHIE/A (Henseler et al. 2015). The HTMT is an estimate of the correlation between two constructs and as such, values that are smaller than one suggest that the two constructs differ. The estimated correlation between the two constructs includes two types of correlations: a. the correlations between items from different constructs (i.e. one item from emotional and one item from social/situational); and b. the correlations between items from the same construct (which can either be the correlation between two items from emotional or the correlation between two items from social/situational). The HTMT is an average of correlations of items from different constructs (described in a.), divided by the average of correlations of items from the same construct (described in b.). This ratio of average correlations is interpreted as an estimate of correlation between the two constructs, where values close to one indicate a lack of discriminant validity. The HTMT can be used as a criterion to assess discriminant validity by comparing it to a predefined cutoff value. HTMT higher than the cutoff provides evidence of a lack of discriminant validity. Based on results from simulation studies, a conservative cutoff of 0.85 was selected for this study (Henseler et al. 2015; Voorhees et al. 2016).
Mokken Scale Analysis (MSA): Reevaluating the Scales
Due to the risk of over-dimensionalization with EFA, dimensionality of the HHIE/A was explored using IRT. Nonparametric IRT methods were used because they are more appropriate when the goal is to explore dimensionality, whereas the more commonly used parametric IRT models (the Rasch model, for example; Wright & Masters 1982) are used to verify dimensionality (Sijtsma & Meijer 2006). Another advantage of nonparametric IRT models is that they relax strong assumptions about the behavior of response probabilities required by parametric IRT models (Sijtsma & Meijer 2006). In the Rasch model and other parametric models, items could potentially be discarded because the responses do not fit the assumed form, which is usually S-shaped (logistic, for example; Stochl et al. 2012).
Two nonparametric IRT models were originally defined by Mokken (1971) for dichotomous items with two response categories and later extended by Molenaar (1997) for polytomous items, or items with more than two response categories (like the HHIE/A). The first of these two Mokken models is the monotone homogeneity model (MHM), which is defined by three assumptions: unidimensionality, local independence of the items, and monotonicity. Unidimensionality means that the scale (or subscale) measures a single latent trait (for example, self-perceived hearing handicap). Local independence means that the items are conditionally independent if the latent trait is held constant. In other words, only the latent trait explains why the items are related to each other. Monotonicity means that the probability of a more extreme response increases as the level of the underlying trait increases. Importantly, if the items on a scale meet the assumptions of the MHM, ordering of subjects with respect to their latent ability using the sum score of observed responses is justified (Sijtsma & Verweij 1992; van der Ark & Bergsma 2010).
Dimensionality Assessment
MSA includes algorithms for item selection that are particularly useful when the goal is to explore dimensionality. In this study, we used the Genetic Algorithm (GA) available from MSA, which considers all possible groupings of subsets of items and returns unidimensional groups of items (Straat et al. 2013). The item scalability coefficients, Hi, represent how well item i separates subjects relative to other items (Loevinger 1947). Based on recommendations from MSA experts, items with Hi > 0.3 were considered for inclusion. The scalability coefficient for the whole scale, H, represents how well the scale can order subjects with respect to the latent ability and can be interpreted as follows: H < 0.3, the scale is not unidimensional; 0.3 ≤ H < 0.4, the scale is weak; 0.4 ≤ H < 0.5, the scale is medium strength; H ≥ 0.5, the scale is strong (Sijtsma & Molenaar 2002). Details about the scalability coefficients and item selection algorithms are provided in Supplemental Digital Content 1.
CTT and IRT methods are often recommended to be used together in psychometric analysis so confirmatory factor analysis (CFA) of the scales obtained from the MSA was also performed to examine common fit indices. Because the responses are ordered-categorical, the CFA was performed using polychoric correlations and a robust estimation technique (weighted least squares-mean and variance adjusted estimation; Oberski 2014).
Assumption of Local Independence
Local independence was evaluated by examining residual correlations of a single-factor CFA. Item pairs with residual correlation greater than 0.2 were considered violations of the local independence assumption.
Assumption of Monotonicity
Nonparametric regression of the item scores on the total score of all of the other items (the “rest score”) were fit and tested for deviations from monotonicity.
Manifest Invariant Item Ordering (MIIO)
In addition to dimensionality exploration, MSA can provide evidence to support another useful result, manifest invariant item ordering (MIIO). MIIO means that the order of items by popularity is the same across different levels of the latent ability, or that the items can be ordered by their mean score (Ligtvoet et al. 2010; Sijtsma et al. 2011). MIIO is a useful result because not only can subjects be ordered with respect to the latent trait, but the total score can also be interpreted as a summary of a set of symptoms (Sijtsma et al. 2011). With MIIO, it can be said that compared to a subject with a lower score, a subject with a higher score has the same symptoms plus more. When MIIO holds, the scalability coefficient, HT indicates how well subjects order the items invariantly. The magnitude of the scalability coefficient, HT can be interpreted as follows: (HT < 0.3, item ordering is not accurate enough to be useful; 0.3 ≤ HT < 0.4, items ordered with low accuracy; 0.4 ≤ HT < 0.5, items ordered with medium accuracy; H ≥ 0.5, items ordered with high accuracy; Ligtvoet et al. 2010). In this study, we used MIIO to investigate the ordering of the HHIE/A items. Technical details about MIIO can be found in Supplemental Digital Content 1.
Cutoff Score Selection
Based on results from the MSA analysis introduced above, we present two revised scales to assess hearing handicap based on the HHIE/A items. For the purpose of quantifying self-perceived hearing handicap, cutoff scores that designate subcategories of handicap (such as mild-to-moderate or significant) are not recommended as the total score is more informative than arbitrary categorization of self-perceived handicap. For screening purposes, cutoff scores of the new scales for detecting hearing impairment were obtained using the receiver operating characteristic (ROC) curve. The ROC curve is a graphical representation of the true positive rate (sensitivity) against the false positive rate (1-specificity) for different cutoff values. The cutoff value is reported that maximizes the Youden Index, which selects the optimal cutoff where sensitivity and specificity are equally important (Youden 1950). Hearing impairment was defined as the PTA of hearing thresholds at 500, 1000, 2000, and 4000 Hz > 25 dB HL in the worse of the two ears (Cruickshanks et al. 1998). Worse ear PTA was used in this definition in order to detect unilateral and asymmetrical impairment, as well as bilateral impairment. Sensitivity and specificity to detect hearing impairment were calculated and presented for several cutoff values in tabular form, as well as in the form of an ROC curve (sensitivity, 1-specificity).
MSA and CFA were performed using the R statistical software (v3.5.1; R Core Team 2018) and the mokken (van der Ark 2007, 2012) and lavaan (Rosseel 2012) packages. The ROC curve analysis was generated using SAS software version 9.4 and the %ROCPLOT macro (SAS 2013).
RESULTS
The demographic and hearing-related characteristics of the subjects at baseline are presented in Table 4. Overall, subjects who completed the HHIE were more likely to be older and female. Younger subjects were more likely to be nonwhite and not married. Tables 2 and 3 (columns 3-7) present descriptive statistics about the items on the HHIE and HHIA, respectively. Missing values were minimal in these data – 2 subjects were each missing a single item score on the HHIE and 1 subject was missing a single item score on the HHIA. Missing item scores were imputed using two-way imputation (Sijtsma & van der Ark 2017). Many items were assigned a response of “0” by high percentages of participants, indicating either disagreement with the item or not applicable (column 7).
Discriminant Validity
For both the HHIE and HHIA, the HTMT was 0.98, which exceeds the cutoff of 0.85. Therefore, discriminant validity was not supported and the social and emotional constructs cannot be adequately distinguished on either scale. Because of the lack of discriminant validity, all 25 items of each scale were considered for an exploratory MSA to reevaluate the dimensionality of the scales.
Dimensionality Assessment
Dimensionality was assessed for the HHIE and HHIA using data from the 1064 and 305 subjects who completed the scales, respectively. For the HHIE, item coefficients for all items were 0.38 < Hi < 0.68, which suggests that all of the items are sufficiently homogeneous. In addition, H = 0.58 [standard error (SE) = 0.02], which suggests that the items formed a strong unidimensional measure. Similarly, for the HHIA, item coefficients for all items were 0.44 < Hi < 0.72 and the items formed a strong scale (H = 0.59, SE = 0.03). CFA fit indices also suggested good fit of the unidimensional model for the HHIE/A.
Given the unidimensionality of the items of the HHIE and HHIA, with 22 items common to both scales, we were interested in determining the impact to scalability if the 3 unique items were removed from each scale. After removing the three items from the HHIE (E-7, S-8, and S-11) that are not included on the HHIA, the scalability was unchanged (H = 0.58, SE = 0.02). After removing the items from the HHIA (S-7, E-10, and S-11) that do not appear on the HHIE, the scalability also did not change significantly (H = 0.57, SE = 0.03).
Without a significant impact to scalability, the remainder of the analysis was performed on the 22 items common to both scales. For the analysis of common items, baseline responses from all 1447 subjects were included and are shown in Table 5. In the 22-item analysis, all His ranged from 0.40 to 0.65 and the items formed a strong scale (H = 0.58, SE = 0.01). In order to justify the use of the total score on the scale to order subjects, however, the fit of the MHM (i.e., the local independence and monotonicity assumptions) also had to be evaluated.
Table 5.
Descriptive statistics for the 22 items common to the Hearing Handicap Inventory for the Elderly (HHIE) and the Hearing Handicap Inventory for Adults (HHIA).
| ID | Item | n | Mean (SD) | Median | Range | Assigned “0” response (%) |
|---|---|---|---|---|---|---|
| S-1. | Does a hearing problem cause you to use the phone less often than you would like? | 1447 | 0.44 (1.09) | 0 | 0-4 | 1223 (84.5) |
| E-2. | Does a hearing problem cause you to feel embarrassed when meeting new people? | 1447 | 0.66 (1.17) | 0 | 0-4 | 1062 (73.4) |
| S-3. | Does a hearing problem cause you to avoid groups of people? | 1447 | 0.49 (1.10) | 0 | 0-4 | 1174 (81.1) |
| E-4. | Does a hearing problem make you irritable? | 1446 | 0.67 (1.17) | 0 | 0-4 | 1045 (72.3) |
| E-5. | Does a hearing problem cause you to feel frustrated when talking to members of your family? | 1447 | 0.99 (1.40) | 0 | 0-4 | 903 (62.4) |
| S-6. | Does a hearing problem cause you difficulty when attending a party? | 1447 | 1.22 (1.54) | 0 | 0-4 | 825 (57.0) |
| E-9.1 | Do you feel handicapped by a hearing problem? | 1447 | 0.73 (1.28) | 0 | 0-4 | 1051 (72.6) |
| S-10.2 | Does a hearing problem cause you difficulty when visiting friends, relatives, or neighbors? | 1447 | 0.78 (1.25) | 0 | 0-4 | 990 (68.4) |
| E-12. | Does a hearing problem cause you to be nervous? | 1447 | 0.34 (0.88) | 0 | 0-4 | 1239 (85.6) |
| S-13. | Does a hearing problem cause you to visit friends, relatives, or neighbors less often than you would like? | 1446 | 0.18 (0.71) | 0 | 0-4 | 1350 (93.4) |
| E-14. | Does a hearing problem cause you to have arguments with family members? | 1447 | 0.51 (1.06) | 0 | 0-4 | 1142 (78.9) |
| S-15. | Does a hearing problem cause you difficulty when listening to TV or radio? | 1447 | 1.37 (1.52) | 2 | 0-4 | 719 (49.7) |
| S-16. | Does a hearing problem cause you to go shopping less often than you would like? | 1447 | 0.09 (0.48) | 0 | 0-4 | 1396 (96.5) |
| E-17. | Does any problem or difficulty with your hearing upset you at all? | 1447 | 1.02 (1.37) | 0 | 0-4 | 868 (60.0) |
| E-18. | Does a hearing problem cause you to want to be by yourself? | 1446 | 0.24 (0.79) | 0 | 0-4 | 1307 (90.4) |
| S-19. | Does a hearing problem cause you to talk to family members less often than you would like? | 1447 | 0.28 (0.84) | 0 | 0-4 | 1291 (89.2) |
| E-20. | Do you feel that any difficulty with your hearing limits or hampers your personal or social life? | 1447 | 0.66 (1.21) | 0 | 0-4 | 1072 (74.1) |
| S-21. | Does a hearing problem cause you difficulty when in a restaurant with relatives or friends? | 1447 | 1.20 (1.46) | 0 | 0-4 | 791 (54.7) |
| E-22. | Does a hearing problem cause you to feel depressed? | 1447 | 0.21 (0.71) | 0 | 0-4 | 1323 (91.4) |
| S-23. | Does a hearing problem cause you to listen to TV or radio less often than you would like? | 1447 | 0.30 (0.94) | 0 | 0-4 | 1297 (89.6) |
| E-24. | Does a hearing problem cause you to feel uncomfortable when talking to friends? | 1447 | 0.62 (1.08) | 0 | 0-4 | 1053 (72.8) |
| E-25. | Does a hearing problem cause you to feel left out when you are with a group of people? | 1447 | 0.80 (1.27) | 0 | 0-4 | 987 (68.2) |
E-8 on the HHIA
S-9 on the HHIA
Monotone Homogeneity Model (MHM) Fit: Ordering of Subjects
In order to determine whether the MHM fit the data, we assessed monotonicity and the local independence assumptions for the 22-item scale. None of the items displayed deviations from monotonicity (see Figure, Supplemental Digital Content 2, which displays the monotonicity plots for the 22 common items of the HHIE/A). In addition, examination of the residual correlation matrix of the single-factor CFA did not result in any flagged potentially dependent item pairs (all pairs < 0.2). Therefore, the MHM appears to fit the items well and the use of the total score is justified.
Manifest Invariant Item Ordering (MIIO): Ordering of Items
The assessment of MIIO resulted in a subset of 18 of the 22 items (all except items E-2, E-4, E-14, and S-21, which violated the assumption) that exhibit medium accuracy in terms of invariant item ordering (HT = 0.41). This suggests that the order by popularity of the 18 items is the same for all individuals. We refer to this 18-item Mokken scale, which contains items that are appropriate for all adults regardless of age as the Revised Hearing Handicap Inventory (RHHI; Supplemental Digital Content 3). Table 6 displays the hierarchical ordering of the 18 RHHI items that have the MIIO property.
Table 6.
Manifest invariant item ordering hierarchy of the Mokken scale of the Revised Hearing Handicap Inventory (RHHI).
| RHHI ID | HHIE ID | Item | Mean Score | Hi |
|---|---|---|---|---|
| 1. | S-15. | Does a hearing problem cause you difficulty when listening to TV or radio? | 1.37 | 0.63 |
| 2. | S-6. | Does a hearing problem cause you difficulty when attending a party? | 1.22 | 0.66 |
| 3. | E-17. | Does any problem or difficulty with your hearing upset you at all? | 1.02 | 0.58 |
| 4. | E-5. | Does a hearing problem cause you to feel frustrated when talking to members of your family? | 0.99 | 0.58 |
| 5. | E-25. | Does a hearing problem cause you to feel left out when you are with a group of people? | 0.80 | 0.63 |
| 6. | S-10.1 | Does a hearing problem cause you difficulty when visiting friends, relatives, or neighbors? | 0.78 | 0.65 |
| 7. | E-9.2 | Do you feel handicapped by a hearing problem? | 0.73 | 0.62 |
| 8. | E-20. | Do you feel that any difficulty with your hearing limits or hampers your personal or social life? | 0.66 | 0.63 |
| 9. | E-24. | Does a hearing problem cause you to feel uncomfortable when talking to friends? | 0.62 | 0.65 |
| 10. | S-3. | Does a hearing problem cause you to avoid groups of people? | 0.49 | 0.59 |
| 11. | S-1. | Does a hearing problem cause you to use the phone less often than you would like? | 0.44 | 0.51 |
| 12. | E-12. | Does a hearing problem cause you to be nervous? | 0.34 | 0.53 |
| 13. | S-23. | Does a hearing problem cause you to listen to TV or radio less often than you would like? | 0.30 | 0.54 |
| 14. | S-19. | Does a hearing problem cause you to talk to family members less often than you would like? | 0.28 | 0.54 |
| 15. | E-18. | Does a hearing problem cause you to want to be by yourself? | 0.24 | 0.55 |
| 16. | E-22. | Does a hearing problem cause you to feel depressed? | 0.21 | 0.55 |
| 17. | S-13. | Does a hearing problem cause you to visit friends, relatives, or neighbors less often than you would like? | 0.18 | 0.62 |
| 18. | S-16. | Does a hearing problem cause you to go shopping less often than you would like? | 0.09 | 0.55 |
S-10 on the Hearing Handicap Inventory for the Elderly (HHIE); S-9 on the Hearing Handicap Inventory for Adults (HHIA)
E-9 on the HHIE; E-8 on the HHIA
Scale Reduction
MSA results can be used to guide decisions for scale length reduction. To create a screening version, a subset of 10 items with the largest item coefficients was selected from the 18-item RHHI. Results from MSA of this 10-item subset and the screening version of the HHIE were compared. The 10 items selected based on the MSA (S-3, E-5, S-6, E-9, S-10, S-13, S-15, E-20, E-24, and E-25) were found to form a strong unidimensional scale (H = 0.66, SE = 0.01) that can order subjects by total score. In addition, the results of MIIO analysis implied invariant item ordering for the 10-item scale (HT = 0.35). This means that there is some evidence that the items can be ordered by popularity as in Table 7. The MSA results were comparable in the subset of 1064 subjects with complete responses on the HHIE (H = 0.65, SE = 0.02; HT = 0.35). We refer to this 10-item Mokken scale that contains items that are appropriate for all adults regardless of age as the Revised Hearing Handicap Inventory-Screening (RHHI-S; Supplemental Digital Content 4).
Table 7.
Manifest invariant item ordering hierarchy of the screening version of the Revised Hearing Handicap Inventory – Screening (RHHI-S).
| RHHI-S ID | HHIE ID | Item | Mean Score | Hi |
|---|---|---|---|---|
| 1. | S-15. | Does a hearing problem cause you difficulty when listening to TV or radio? | 1.37 | 0.64 |
| 2. | S-6. | Does a hearing problem cause you difficulty when attending a party? | 1.22 | 0.69 |
| 3. | E-5. | Does a hearing problem cause you to feel frustrated when talking to members of your family? | 0.99 | 0.61 |
| 4. | E-25. | Does a hearing problem cause you to feel left out when you are with a group of people? | 0.80 | 0.67 |
| 5. | S-10.1 | Does a hearing problem cause you difficulty when visiting friends, relatives, or neighbors? | 0.78 | 0.68 |
| 6. | E-9.2 | Do you feel handicapped by a hearing problem? | 0.73 | 0.65 |
| 7. | E-20. | Do you feel that any difficulty with your hearing limits or hampers your personal or social life? | 0.66 | 0.65 |
| 8. | E-24. | Does a hearing problem cause you to feel uncomfortable when talking to friends? | 0.62 | 0.67 |
| 9. | S-3. | Does a hearing problem cause you to avoid groups of people? | 0.49 | 0.64 |
| 10. | S-13. | Does a hearing problem cause you to visit friends, relatives, or neighbors less often than you would like? | 0.18 | 0.68 |
S-10 on the Hearing Handicap Inventory for the Elderly (HHIE); S-9 on the Hearing Handicap Inventory for Adults (HHIA)
E-9 on the HHIE; E-8 on the HHIA
The original HHIE screening version was also subjected to MSA to compare to the psychometric properties of the RHHI-S. MSA suggests that the original HHIE screening version (E-2, E-5, S-8, E-9, S-10, S-11, E-14, S-15, E-20, S-21) is also a strong unidimensional scale, though slightly weaker than the RHHI-S (H = 0.60, SE = 0.02). Ordering subjects by total score on the original screening version is justified, with no violations of monotonicity or local independence. The results from MIIO of the original HHIE screening items suggest strong invariant item ordering of most items (HT = 0.55). However, upon inspection of the item response functions (IRFs; see Figure, Supplemental Digital Content 5, which displays the monotonicity plots for the original HHIE screening version), item S-8 (difficulty hearing when someone speaks in a whisper) had more positive responses than the other items and the IRF was flagged as an outlier. The results from an assessment of MIIO can be misleading if any items are included that have IRFs that are outliers compared to the other IRFs (Watson et al. 2014). Thus, inclusion of this item could exaggerate the existence of MIIO so it was removed to determine how the scalability coefficient was affected. The results of MIIO excluding item S-8 no longer support strong invariant item ordering but suggest that eight of the items (item E-14 does not fit the MIIO pattern) could be weakly ordered (HT = 0.37). Therefore, 8 of the 10 on the original HHIE screening version can be ordered by difficulty with low accuracy.
ROC Analysis: Cutoff Score Selection
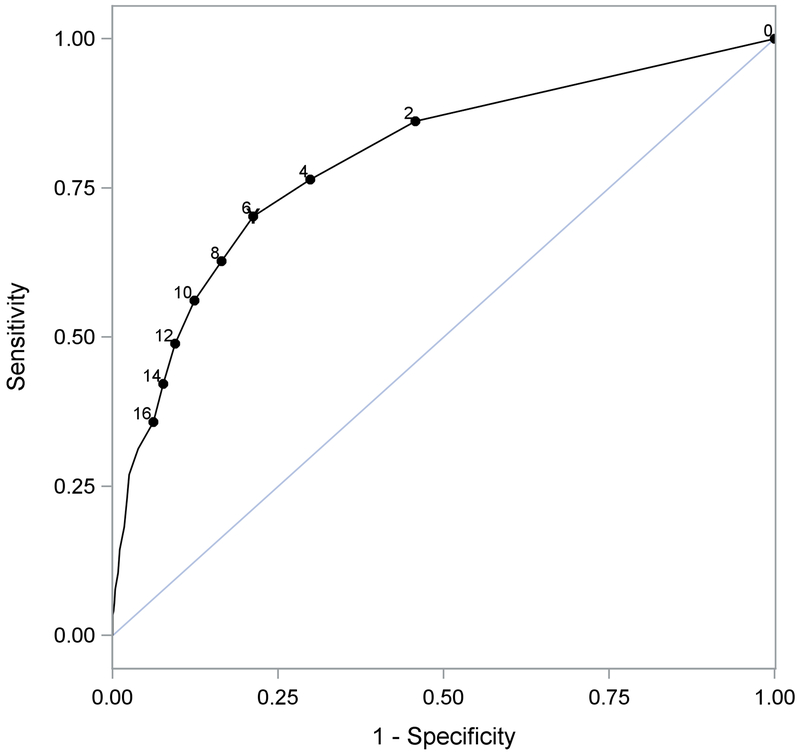
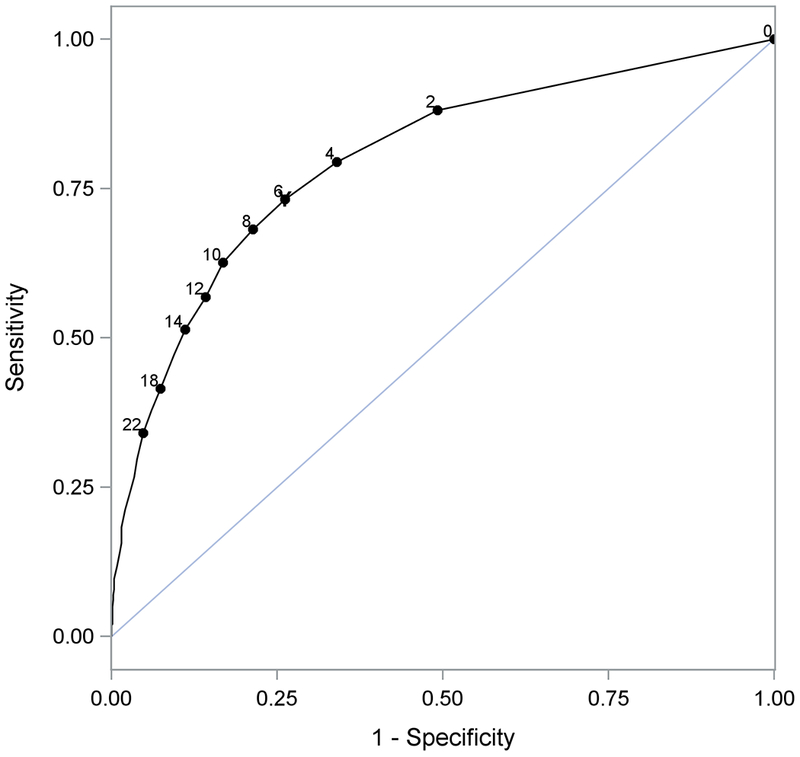
The RHHI and RHHI-S responses are assigned scores of 4, 2, and 0 (for “yes”, “sometimes”, or “no”, respectively) to remain consistent with the original tools. The ROC curves for using the RHHI and RHHI-S to predict hearing impairment [defined as PTA (500, 1000, 2000, 4000 Hz) > 25 dB HL in the worse ear] are displayed in Figures 1 and 2, respectively. Based on the Youden Index, a score ≥6 on the RHHI detected hearing impairment with 73.2% sensitivity and 73.8% specificity (Table 8, top). For the RHHI-S a score ≥6 detected hearing impairment with 70.3% sensitivity and 78.8% specificity (Table 8, bottom)1. Using cutoff scores of ≥6 for both tools, a total of 715 (49.4%) and 658 (45.5%) subjects with increased risk of hearing loss were identified on the RHHI and RHHI-S, respectively.
Figure 1.
Receiver operating characteristic curve for using the Revised Hearing Handicap Inventory (RHHI) score to predict hearing loss. The cutoff with maximum Youden Index (≥6) is labeled with the symbol Y.
Figure 2.
Receiver operating characteristic curve for using the Revised Hearing Handicap Inventory – Screening (RHHI-S) score to predict hearing loss. The cutoff with maximum Youden Index (≥6) is labeled with the symbol Y.
Table 8.
Sensitivity and specificity and 95% confidence interval for hearing loss at selected Revised Hearing Handicap Inventory (RHHI) and Revised Hearing Handicap Inventory – Screening (RHHI-S) cutoff values. The bold indicates the cutoff value of ≥6 recommended for each tool.
| Positive if greater than or equal to | Sensitivity | Specificity |
|---|---|---|
| RHHI | ||
| 2 | 88.1 (85.8, 90.5) | 50.8 (47.2, 54.5) |
| 4 | 79.5 (76.5, 82.4) | 66.0 (62.6, 69.5) |
| 6 | 73.2 (69.9, 76.4) | 73.8 (70.7, 77.0) |
| 8 | 68.2 (64.7, 71.6) | 78.6 (75.7, 81.6) |
| 10 | 62.6 (59.0, 66.1) | 83.2 (80.4, 85.9) |
| 12 | 56.8 (53.2, 60.5) | 85.8 (83.2, 88.3) |
| 14 | 51.4 (47.7, 55.1) | 88.9 (86.6, 91.2) |
| RHHI-S | ||
| 2 | 86.2 (83.6, 88.7) | 54.3 (50.6, 57.9) |
| 4 | 76.4 (73.3, 79.5) | 70.1 (66.8, 73.5) |
| 6 | 70.3 (66.9, 73.6) | 78.8 (75.8, 81.7) |
| 8 | 62.7 (59.2, 66.3) | 83.6 (80.9, 86.3) |
| 10 | 56.2 (52.5, 59.8) | 87.7 (85.3, 90.1) |
| 12 | 48.9 (45.2, 52.5) | 90.6 (88.4, 92.7) |
| 14 | 42.2 (38.6, 45.8) | 92.3 (90.4, 94.3) |
DISCUSSION
This study highlighted the benefits of using rigorous approaches for psychometric analysis of scales with ordered-categorical responses that are commonly used on hearing-related PROMs. These methods can be used to develop new scales, as well as to refine scales that were developed using classical methods, such as CTT. Using nonparametric IRT analysis of data collected in an ongoing study of age-related hearing loss, we found that the Hearing Handicap Inventories developed in the 1980s and 1990s are composed of items that form strong scales. Evidence in this study did not support discriminant validity for the HHIE/A, which suggests that the two subscales of the original scales are not truly distinct. This implies that the items are not specific to emotional consequences and social/situational effects due to hearing loss. Despite the lack of evidence for the two distinct subscales, results from MSA (and CFA) suggest that the items of the HHIE/A form a strong unidimensional scale that instead measures one underlying construct, self-perceived hearing handicap.
Removal of the three unique items to the HHIE/A did not significantly impact scalability, so we chose to simplify the assessment of hearing handicap by evaluating the items common to both scales so that the resulting scale can be administered to adults of all ages. Using MSA, we developed the RHHI (see Supplemental Digital Content 3), which includes 18 of the original HHIE/A items that have optimal psychometric properties. First, evidence strongly supports ordering individuals by total score for these 18 items with respect to the underlying latent trait, self-perceived hearing handicap. Higher scores are indicative of greater perceived handicap. Second, evidence supports the ordering of the items by popularity and suggests that the ordering is the same for all individuals. A scale that has this property has a more informative total score that can also indicate items with which patients are more likely to report problems. For example, a patient with a total RHHI score of 4 is likely to have difficulty when listening to the TV or radio and/or when attending a party (items 1 and 2, respectively). Similarly, a patient who endorses a less popular item also tends to endorse the more popular items. For example, a patient who reports that their hearing problem causes them to feel frustrated when talking to members of their family (item 4) is also likely to report difficulty when listening to the TV or radio (item 1), difficulty when attending a party (item 2), and any problem or difficulty with their hearing that upsets them (item 3). A practical result of this scale property is that abnormal patterns can easily be detected in a clinical setting and may help guide decisions for patients with unexpected patterns of responses. For these reasons, we suggest that for clinical and research purposes, the total score on the scale is more informative than creating self-perceived hearing handicap subcategories (such as mild-to-moderate and significant handicap). The use of the total score can also prompt a discussion between patient and clinician to determine methods for remediation of any self-perceived hearing handicap, identifying the specific problems the patient faces.
MSA was also used to develop the 10-item RHHI-S (see Supplemental Digital Content 4), which shares the important psychometric properties discussed above. Both the RHHI and RHHI-S can be administered to adults of all ages, as an alternative to the age-specific HHIE/A and their screening versions. Thus, we propose the use of the RHHI and the RHHI-S for all adults, reducing the burden for clinicians (only one form to administer) and patients (fewer items). If the tools are used to screen for or detect hearing loss, we have proposed a cutoff of ≥6 for optimal detection.
In summary, the Revised Hearing Handicap Inventory (RHHI) and the Revised Hearing Handicap Inventory – Screening (RHHI-S) are strong unidimensional scales that can be used to quantify self-perceived hearing handicap for adults of all ages. The results also suggest that the items can be ordered in terms of popularity. Due to this hierarchy, items with which patients are more likely to report problems can be identified. In addition, ROC curve analysis determined a cutoff score (≥6 for both the RHHI and RHHI-S) that is useful to screen for or detect hearing impairment, which may indicate the need for referral for an audiologic evaluation. This research study relied on the voluntary participation of healthy adults in the Charleston, South Carolina metropolitan area. Thus, further research is needed to assess the generalizability of the cutoff score to screen for or detect hearing impairment in other populations.
Supplementary Material
ACKNOWLEDGEMENTS
The authors thank the subjects who participated in this study.
This work was supported (in part) by research grant P50 DC000422 from NIH/NIDCD and by the South Carolina Clinical and Translational Research (SCTR) Institute, with an academic home at the Medical University of South Carolina, NIH/NCATS Grant number UL1 TR001450.
This investigation was conducted in a facility constructed with support from Research Facilities Improvement Program Grant Number C06 RR14516 from the NIH/NCRR.
Footnotes
The authors declare no conflicts of interest.
Portions of this article were presented at the Hearing Across the Lifespan 2018 conference, Cernobbio, Lake Como, Italy, June 7, 2018.
Other commonly used PTAs were also subjected to ROC analysis and cutoff scores selected to detect > 25 dB HL in the worse ear; a cutoff score of ≥6 was consistently selected. Using PTA (500, 1000, 2000, 4000 Hz) > 25 dB HL in the better ear, very similar cutoff scores were selected based on the Youden Index for the RHHI and RHHI-S (≥8 and ≥6, respectively).
REFERENCES
- Boeschen Hospers JM, Smits N, Smits C, et al. (2016). Reevaluation of the Amsterdam Inventory for Auditory Disability and Handicap using item response theory. J Speech Lang Hear Res, 59, 373–383. [DOI] [PubMed] [Google Scholar]
- Cassarly C, Matthews LJ, Simpson AN, et al. Development and refinement of patient-reported outcomes for hearing: A brief introduction to nonparametric item response theory. Am J Audiol, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chenault M, Berger M, Kremer B, et al. (2013). Quantification of experienced hearing problems with item response theory. Am J Audiol, 22, 252–262. [DOI] [PubMed] [Google Scholar]
- Cruickshanks KJ, Wiley TL, Tweed TS, et al. (1998). Prevalence of hearing loss in older adults in Beaver Dam, Wisconsin. The Epidemiology of Hearing Loss Study. Am J Epidemiol, 148, 879–886. [DOI] [PubMed] [Google Scholar]
- Demorest ME, Wark DJ, Erdman SA (2011). Development of the Screening Test for Hearing Problems. Am J Audiol, 20, 100–110. [DOI] [PubMed] [Google Scholar]
- Dubno JR, Lee FS, Klein AJ, et al. (1995). Confidence limits for maximum word-recognition scores. J Speech Hear Res, 38, 490–502. [DOI] [PubMed] [Google Scholar]
- Dubno JR, Lee FS, Matthews LJ, et al. (1997). Age-related and gender-related changes in monaural speech recognition. J Speech Lang Hear Res, 40, 444–452. [DOI] [PubMed] [Google Scholar]
- Heffernan E, Maidment DW, Barry JG, et al. (2018). Refinement and validation of the Social Participation Restrictions Questionnaire: An application of Rasch analysis and traditional psychometric analysis techniques. Ear Hear, Publish Ahead of Print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henseler J, Ringle CM, Sarstedt M (2015). A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci, 43, 115–135. [Google Scholar]
- Jessen A, Ho AD, Corrales CE, et al. (2018). Improving measurement efficiency of the Inner EAR scale with item response theory. Otolaryngol Head Neck Surg, 158, 1093–1100. [DOI] [PubMed] [Google Scholar]
- Lee FS, Matthews LJ, Dubno JR, et al. (2005). Longitudinal study of pure-tone thresholds in older persons. Ear Hear, 26, 1–11. [DOI] [PubMed] [Google Scholar]
- Ligtvoet R, van der Ark LA, te Marvelde JM, et al. (2010). Investigating an invariant item ordering for polytomously scored items. Educ Psychol Meas, 70, 578–595. [Google Scholar]
- Loevinger J (1947). A systematic approach to the construction and evaluation of tests of ability. Psychol Monogr, 61. [Google Scholar]
- Matthews LJ, Lee FS, Mills JH, et al. (1997). Extended high-frequency thresholds in older adults. J Speech Lang Hear Res, 40, 208–214. [DOI] [PubMed] [Google Scholar]
- McRackan TR, Hand BN, Velozo CA, et al. (2018). Development of the Cochlear Implant Quality of Life item bank. Ear Hear. 2018 December 6 [ePub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mokken RJ (1971). A theory and procedure of scale analysis: With applications in political research. Berlin, Germany: De Gruyter Mouton. [Google Scholar]
- Mokkink LB, Knol DL, van Nispen RM, et al. (2010). Improving the quality and applicability of the Dutch scales of the Communication Profile for the Hearing Impaired using item response theory. J Speech Lang Hear Res, 53, 556–571. [DOI] [PubMed] [Google Scholar]
- Molenaar IW (1997). Nonparametric models for polytomous responses In van der Linden WJ, Hambleton RK (Eds.), Handbook of modern item response theory (pp. 369–380). New York, NY: Springer New York. [Google Scholar]
- Newman CW, Weinstein BE, Jacobson GP, et al. (1990). The Hearing Handicap Inventory for Adults: Psychometric adequacy and audiometric correlates. Ear Hear, 11, 430–433. [DOI] [PubMed] [Google Scholar]
- Newman CW, Weinstein BE, Jacobson GP, et al. (1991). Test-retest reliability of the Hearing Handicap Inventory for Adults. Ear Hear, 12, 355–357. [DOI] [PubMed] [Google Scholar]
- Noble W, Tyler R, Dunn C, et al. (2008). Hearing handicap ratings among different profiles of adult cochlear implant users. Ear Hear, 29, 112–120. [DOI] [PubMed] [Google Scholar]
- Oberski D (2014). lavaan.survey: An R package for complex survey analysis of structural equation models. J Stat Softw, 57, 27. [Google Scholar]
- R Core Team (2018). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria: URL https://www.R-project.org/. [Google Scholar]
- Rosseel Y (2012). lavaan: An R Package for Structural Equation Modeling. J Stat Softw, 48, 36. [Google Scholar]
- SAS (2013). SAS and all other SAS Institute Inc. product or service names are registered trademarks or trademarks of SAS Institute Inc. SAS Institute Inc., Cary, NC, USA. [Google Scholar]
- Sijtsma K, & Meijer RR (2006). Nonparametric item response theory and special topics In Rao CR, Sinharay S (Eds.), Handbook of Statistics 26 - Psychometrics (pp. 719–746). Amsterdam: Elsevier. [Google Scholar]
- Sijtsma K, Meijer RR, van der Ark LA (2011). Mokken scale analysis as time goes by: An update for scaling practitioners. Pers Individ Dif, 50, 31–37. [Google Scholar]
- Sijtsma K, & Molenaar IW (2002). Introduction to Nonparametric Item Response Theory. Thousand Oaks, California: SAGE Publications. [Google Scholar]
- Sijtsma K, & van der Ark LA (2017). A tutorial on how to do a Mokken scale analysis on your test and questionnaire data. Br J Math Stat Psychol, 70, 137–158. [DOI] [PubMed] [Google Scholar]
- Sijtsma K, & Verweij AC (1992). Mokken scale analysis: Theoretical considerations and an application to transitivity tasks. Appl Meas Educ, 5, 355–373. [Google Scholar]
- Sjahalam-King J, & Newall J (2016). Measuring hearing handicap for hearing impaired adults in the Philippines: A profound conundrum. Speech Lang Hear, 19, 238–246. [Google Scholar]
- Stochl J, Jones PB, Croudace TJ (2012). Mokken scale analysis of mental health and well-being questionnaire item responses: A non-parametric IRT method in empirical research for applied health researchers. BMC Med Res Methodol, 12, 74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Straat JH, van der Ark LA, Sijtsma K (2013). Comparing optimization algorithms for item selection in Mokken scale analysis. J Classif, 30, 75–99. [Google Scholar]
- van der Ark LA (2007). Mokken Scale Analysis in R. J Stat Softw, 20, 19. [Google Scholar]
- van der Ark LA (2012). New developments in Mokken scale analysis in R. J Stat Softw, 48, 27. [Google Scholar]
- van der Ark LA, & Bergsma WP (2010). A note on stochastic ordering of the latent trait using the sum of polytomous item scores. Psychometrika, 75, 272–279. [Google Scholar]
- van der Eijk C, & Rose J (2015). Risky business: Factor analysis of survey data – Assessing the probability of incorrect dimensionalisation. PLOS ONE, 10, e0118900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventry IM, & Weinstein BE (1982). The Hearing Handicap Inventory for the Elderly: A new tool. Ear Hear, 3, 128–134. [DOI] [PubMed] [Google Scholar]
- Ventry IM, & Weinstein BE (1983). Identification of elderly people with hearing problems. ASHA, 25, 37–42. [PubMed] [Google Scholar]
- Voorhees CM, Brady MK, Calantone R, et al. (2016). Discriminant validity testing in marketing: an analysis, causes for concern, and proposed remedies. J Acad Mark Sci, 44, 119–134. [Google Scholar]
- Watson R, Wang W, Thompson DR, et al. (2014). Investigating invariant item ordering in the Mental Health Inventory: An illustration of the use of different methods. Pers Individ Dif, 66, 74–78. [Google Scholar]
- Weinstein BE, & Ventry IM (1983). Audiometric correlates of the Hearing Handicap Inventory for the elderly. J Speech Hear Disord, 48, 379–384. [DOI] [PubMed] [Google Scholar]
- Wright BD, & Masters G (1982). Rating scale analysis. Chicago, IL: MESA Press. [Google Scholar]
- Youden WJ (1950). Index for rating diagnostic tests. Cancer, 3, 32–35. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.