Abstract
Background:
In order to improve oxidation resistance, antioxidants such as vitamin-E are added to polyethylene used in the bearing surfaces of orthopaedic components. Currently, little is known about the efficacy of this treatment in vivo. This study therefore reports on the reasons for revision, surface damage mechanisms, and oxidation of retrieved vitamin-E stabilized highly crosslinked polyethylene (HXLPE) for total knee arthroplasty.
Methods:
We examined 103 retrieved knee inserts fabricated from vitamin E-stabilized HXLPE and 67 fabricated from re-melted HXLPE as a control. The implantation times were 1.2 ± 1.3 and 1.5 ± 1.3 years for the vitamin E and control cohorts, respectively. The inserts were evaluated for 7 surface damage mechanisms using a semi-quantitative scoring method and analyzed for oxidation using Fourier transformed infrared spectroscopy. Reasons for revision were also assessed using operative notes created at time of retrieval.
Results:
Both groups were revised primarily for instability, infection, and loosening. Burnishing, pitting, and scratching were the most common damage mechanisms observed, with the VE cohort demonstrating less surface damage than the control. Measured oxidation for the cohort was low, with a median oxidation index of 0.09 ± .05 for the articulating surface, 0.05 ± 0.06 for the backside, 0.08 ± 0.06 for the anterior/posterior surfaces, and 0.08 ± 0.05 for the stabilizing post. As compared to the control cohort, oxidation tended to be less for the VE group at the articulating (p<0.001) and backside (p=0.003) surfaces, though the median differences were minimal and may not be clinically significant.
Conclusion:
The results indicate positive fatigue damage resistance and oxidation resistance for the retrieved vitamin E-stabilized TKA inserts.
Keywords: vitamin E, total knee arthroplasty (TKA), retrieval analysis, highly crosslinked polyethylene (HXLPE), oxidation, surface damage
Introduction
Ultra-high molecular weight polyethylene (UHMWPE) has long been considered the gold standard for bearing surfaces in total joint arthroplasty, due to its superior physical and mechanical properties. Since its development, attempts at improving the material’s performance have required balancing its mechanical strength, wear resistance, and oxidative stability. Crosslinking by irradiation, for example, emerged as a method to greatly increase the material wear resistance and subsequently reduce instances of osteolysis. Post-irradiation thermal treatments, such as remelting, later followed in order to improve oxidative stability by reducing the residual free radicals resulting from crosslinking [1, 2]. Though bearing surfaces manufactured from this first-generation highly crosslinked polyethylene (HXLPE) material showed positive clinical results in both total hip arthroplasty (THA) and total knee arthroplasty (TKA) [2], the loss of fatigue strength due to thermal treatments has resulted in the emergence of second-generation HXLPE stabilized with antioxidants such as vitamin E (VE) [1, 3, 4].
The inclusion of alpha tocopherol (vitamin E), a free radical scavenger, allows for polyethylene crosslinking and oxidative stability without sacrificing mechanical strength [5]. The antioxidant can be added via diffusion or blending and has been shown to be effective even at very low concentrations [6, 7]. Early in vitro studies of VE HXLPE in both stock and implant form have shown promising results in regard to oxidative stability, wear resistance, and fatigue strength [1, 3, 4, 8–12]. Additionally, it has been reported that VE stabilization lowers the risk of osteolysis and implant loosening, as the biologic reaction to vitamin E polyethylene is reduced as compared to conventional UHMWPE [13, 14]. For these reasons, vitamin E-stabilized HXLPE inserts have been gaining popularity in total joint arthroplasty, thus far with positive outcomes [3, 4, 15–17].
Though numerous in vitro studies using VE bearing surfaces have resulted in positive findings [8, 10, 11, 18–26], far fewer in vivo results have been reported [27–32]. Even fewer investigate the in vivo surface damage and oxidation resistance behavior of VE HXLPE [28, 29]. In one such study, Rowell et al. examined the vitamin E-stabilized bearing surfaces of short-term THA and TKA retrievals, finding low instances of oxidation and reduced free radical content [28]. The study also reported unchanging amounts of an oxidation cascade byproduct, hydroperoxide, suggesting that the addition of vitamin E successfully suppressed the oxidation process, though only three knee retrievals were included in the study. In a similar study, Currier et al. investigated retrieved tibial inserts and reported lower oxidation for VE and pentaerythritol tetrakis [3-(3,5-di-tert-butyl-4-hydroxyphenyl)propionate] (PBHP)-stabilized polyethylene as compared to conventional and remelted HXLPE [29]. Despite these studies, clinical evidence of vitamin E-stabilized HXLPE in vivo behavior, particularly for TKA, is greatly lacking. Thus, this study aimed to determine whether vitamin E-stabilized tibial inserts demonstrated 1) similar reasons for revision; 2) improved surface damage resistance; and 3) improved oxidative stability as compared to remelted HXLPE (control) inserts.
Materials and Methods
Implant and Clinical Information
A total of 103 vitamin E-stabilized tibial inserts and 67 remelted HXLPE implanted between 2008 and 2017 were collected during routine revision surgery from eight clinics as part of a multi-institutional retrieval program. In this study, the remelted HXLPE served as a control in order to better understand the effect of the vitamin E treatment on material resistance to damage and oxidation. Eighty-eight of the VE cohort were identified as being manufactured via blending (Persona, Vivacit-E; Zimmer Biomet, Warsaw, IN) and 15 were manufactured via diffusion (Vanguard, E1; Zimmer Biomet). Components of the control cohort were manufactured from remelted HXLPE (Nexgen, Prolong; Zimmer Biomet), considered the predecessor of the Persona/Vivacit-E components. As little to no oxidation is expected to occur within the first year of use, only VE retrievals with an implantation time of 0.5 years or more were matched to controls, resulting in a HXLPE group of 67 retrievals. Previously, we reported the revision reasons, damage mechanisms, and oxidation for the remelted HXLPE cohort [33]. Prior to characterization, Prior to inspection, all components were cleaned by two 20-minute soaks in a 1:10 ratio of detergent (Discide®; AliMed, Dedham, MA) to water followed by two periods of ultrasonication in water. The inserts were then stored in a subzero freezer to minimize ex vivo oxidative changes according to methods previously described [34]. Fourteen cases had a history of a previous revision surgery (8 total revisions and 6 PE exchanges) for the VE cohort and 14 (9 total revisions and 5 PE exchanges) for the HXLPE cohort. The revision reason for each component, as determined by the surgeon at time of revision, was confirmed via analysis of operative notes. A summary of patient and device information is included in Table 1.
Table 1.
Summary of Clinical Information for the Cohort of Retrieved TKA.
| Vitamin E-Stabilized (N = 103) | Remelted HXLPE (N = 67) | |
|---|---|---|
| Gender (% male) | 52 | 45 |
| Age at insertion (y; mean ± SD) | 61 ± 10 | 65 ± 11 |
| BMI (kg/m2; mean ± SD) | 33.9 ± 6.4 | 33.4 ± 5.7 |
| UCLAmax scorea | 5 ± 2 | 6 ± 2 |
| Implantation time (y; mean ± SD) | 1.2 ± 1.3 | 1.5 ± 1.3 |
| (range, 0.0–6.5) | (range, 0.0–6.5) | |
| Device information | N | N |
| Post-stabilized | 95 | 66 |
| Cruciate-retaining | 8 | 1 |
TKA, total knee arthroplasty; HXLPE, highly crosslinked polyethylene; SD, standard deviation; BMI, body mass index; UCLA, University of California, Los Angeles.
UCLA score represents patient physical activity on a scale of 1 to 10.
Polyethylene Damage Evaluation
The surfaces of each polyethylene insert were visually inspected and assigned damage scores based on the presence and severity of seven distinct damage modes, according to methods previously discussed [35, 36]. The left and right condyles, backside, and post (if applicable) of each insert were divided into separate regions, and each region received a score of 0 – 3 for abrasion, burnishing, delamination, embedded debris, pitting, scratching, and surface deformation. Two investigators examined and scored each component individually, and any discrepancies were discussed and resolved to result in one score for each region and damage mode.
Oxidation Analysis
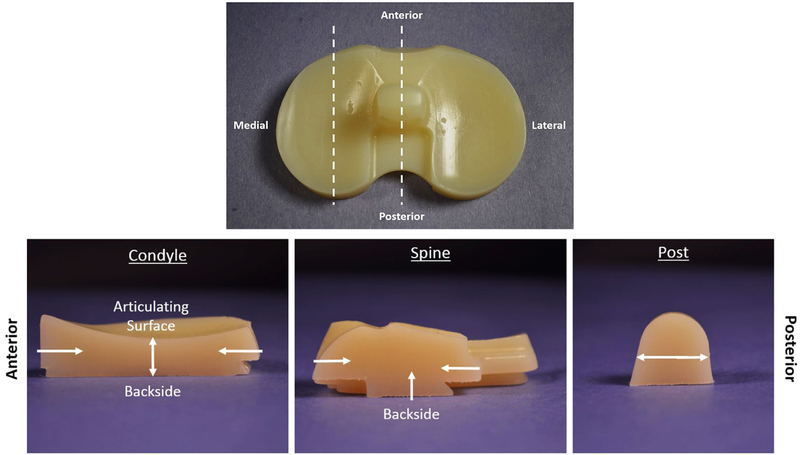
Each vitamin E-stabilized tibial insert was sectioned for analysis in three locations: medial condyle, the central spine, and the stabilizing post, if present (Figure 1). The inserts were cut by bandsaw to access the three areas of interest. To account for mechanical damage caused by the bandsaw as well as to level each sample, ~2–4 mm of material was microtomed away in increments of <100 microns. The final sample slices used for analysis were 200 ± 50 μm thick and verified by micrometer to ensure adequate results when analyzing oxidation level via Fourier Transform Infrared Spectroscopy (FTIR). Each sample slice was boiled in heptane for 6 hours to remove lipids that may have diffused into the polyethylene while implanted. After boiling in heptane, the slices were placed in an ultrasonic bath to further agitate lipid particles or leftover heptane to extract impurities. The sonication was done twice in clean water before allowing to dry. Utilizing FTIR (Nicolet iN10 Infrared Microscope with iZ10 FTIR module, Thermo Scientific, Waltham, MA), 3-mm line profiles (100-μm increments; 32 repeat scans/location; 4 cm−1 wavelength resolution) were taken perpendicular to the regions of interest (ROI), and oxidation index was subsequently calculated according to ASTM F2102–17 [37]. ROIs were the articulating surface, anterior/posterior (AP) surfaces, backside surface, and stabilizing post (Figure 1).
Figure 1.
(Top) Tibial insert sectioning locations and (bottom) regions of interest for FTIR profiles.
Statistical Analysis
All statistical analyses were performed using SPSS software, version 25.0 (SPSS Inc., Chicago, IL). The distributions of continuous variables were tested for normality using the Shapiro-Wilk test and were found to be non-normal, thus, nonparametric tests were used for the remaining statistical analyses. Differences in oxidative properties between regions within each sample were evaluated using the Friedman test with Bonferroni-corrected pairwise comparisons, and differences in categorical variables were determined using Pearson’s chi-squared test. Correlations between variables were evaluated using the Spearman rank correlation test. The significance value for all tests was p < 0.05.
Results
The most common reasons for revision were instability, infection, and loosening for each group, accounting for 69% of all VE HXLPE revisions and 78% of all remelted HXLPE revisions. Additional reasons for revision include hematoma, stiffness, periprosthetic fracture, allergic reaction to metal, wound drainage, traumatic dislocation, and unexplained pain. A summary of revision reasons for each group is provided in Table 2. The frequency of revision reasons differed between the two groups (χ2 = 0.012), with instability being the most common revision reason for the VE HXLPE group (28.2%) and infection (32.8%) for remelted HXLPE.
Table 2.
Summary of Revision Reasons Determined at Time of Surgery.
| Revision Reason | Number of Cases | |
|---|---|---|
| Vitamin E-Stabilized (N = 103) | HXLPE (N = 67) | |
| Instability | 29 (28.2%) | 13 (19.4%) |
| Infection | 24 (23.3%) | 22 (32.8%) |
| Loosening | 18 (17.5%) | 17 (25.4%) |
| Hematoma | 12 (11.7%) | 1 (1.5%) |
| Stiffness | 10 (9.7%) | 4 (6.0%) |
| Othera | 10 (9.7%) | 10 (14.9%) |
HXLPE, highly crosslinked polyethylene.
Other includes periprosthetic fracture, metal allergy, wound drainage, traumatic dislocation, and unknown.
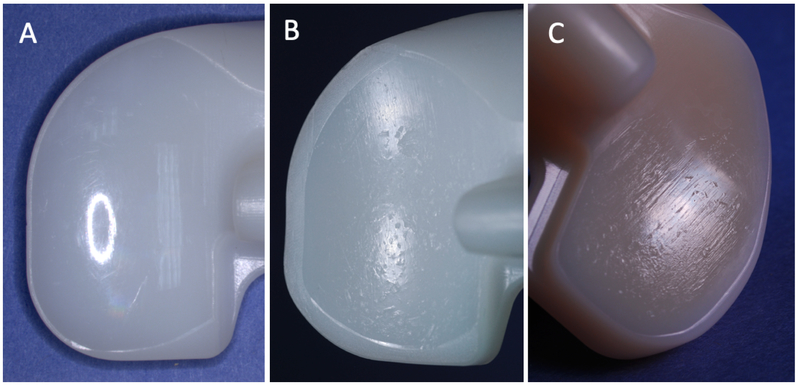
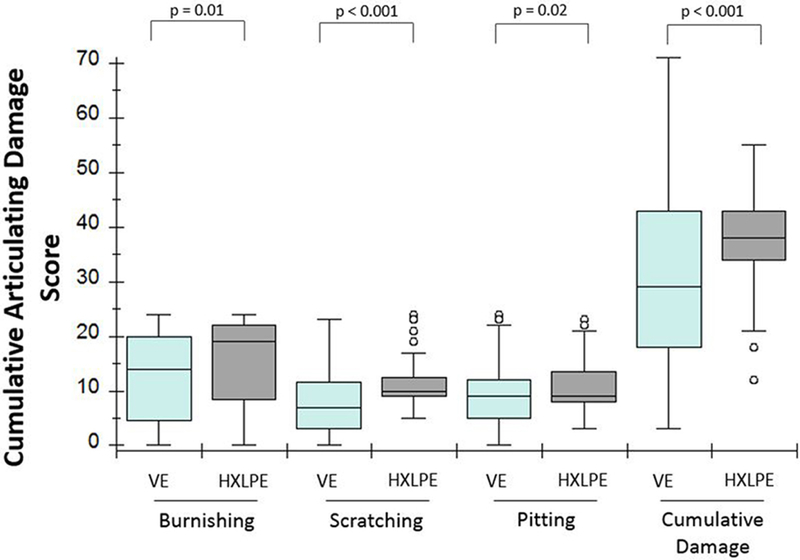
Burnishing, pitting, and scratching were the most common damage mechanisms observed on the articulating surfaces of each cohort (Figure 2). On the backsides of the inserts, scratching and pitting were the main damage modes. Overall, at least minimal burnishing was found in 99% (102/103) of VE HXLPE and 93% (62/67) of remelted HXLPE inserts, at least minimal pitting in 99% (102/103) of VE HXLPE and 100% (67/67) of remelted HXLPE inserts, and at least minimal scratching in 96% (99/103) of VE HXLPE and 100% (67/67) of remelted HXLPE inserts. We did not observe any instances of delamination in the VE HXLPE group or the remelted HXLPE group. At the articulating surface, the VE HXLPE cohort also exhibited less scratching (median score difference = 3, p<0.001), pitting (median score difference = 0, p=0.02), burnishing (median score difference = 5, p=0.01), and total cumulative damage (median score difference = 9, p<0.001) as compared to the controls (Figure 3). The cumulative articulating damage score was not found to correlate with implantation time for the VE HXLPE group (p=0.75), but for the remelted HXLPE group a positive correlation was observed (ρ=0.444, p<0.001). For both groups, the cumulative articulating damage scores were not found to correlate with BMI, weight, or age at insertion (p>0.05), though a weak correlation between total damage and maximum UCLA score was observed for the VE group (ρ =0.289, p=0.01). No difference in total damage was observed between the blended and diffused VE inserts or between reasons for revision.
Figure 2.
Examples of the most frequently-observed surface damage mechanisms: (A) burnishing: significant polishing of the surface, (B) pitting: small crater-like deformations, and (C) scratching: indented lines in the direction of articulation.
Figure 3.
Cumulative articulating surface damage scores for burnishing, scratching, pitting, and total combined damage in the VE and HXLPE cohorts.
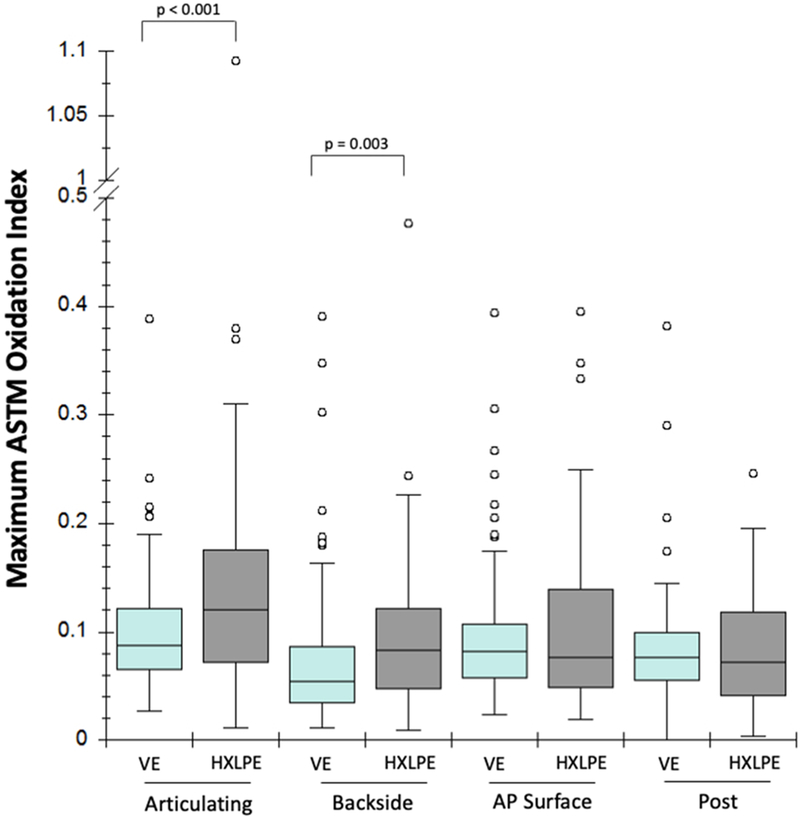
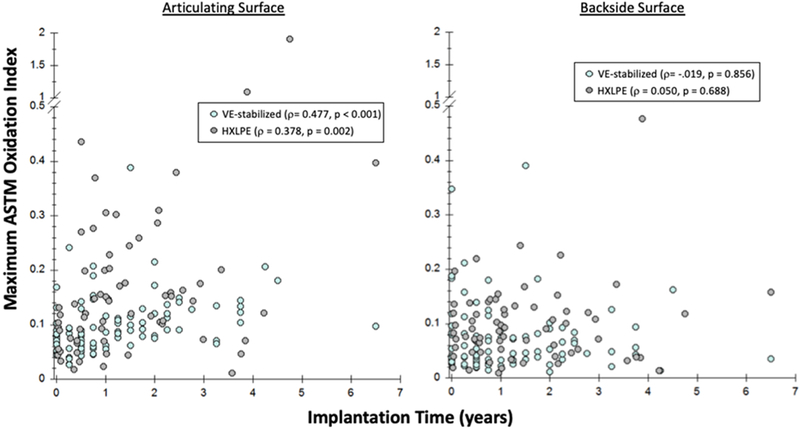
Observed oxidation for the VE HXLPE cohort was low, with a median (± standard deviation) ASTM oxidation index (OI) of 0.09 ± 0.05 (IQR 0.06 – 0.12) for the articulating surface, 0.05 ± 0.06 (IQR 0.03 – 0.08) for the backside, 0.08 ± 0.06 (IQR 0.06 – 0.11) for the anterior/posterior surfaces, and 0.08 ± 0.05 (IQR 0.06 – 0.10) for the stabilizing post (Figure 4). Maximum oxidation index tended to be greater for the remelted HXLPE group at the articulating (Median difference = 0.04, p < 0.001) and backside (Median difference = 0.04, p = 0.003) surfaces, but not for the A/P surface (p = 0.84) and stabilizing post (p = 0.45). For the VE HXLPE cohort, differences were observed between ROIs. Specifically, the backside surface had lower OIs than articulating surface (Median difference = 0.04, p<0.001), AP surfaces (Median difference = 0.03, p<0.001), and the stabilizing post (Median difference = 0.03, p<0.001). Additionally, the backside OI tended to be greater for the diffused VE compared to blended (Median difference = 0.07, p < 0.001), though a similar relationship was not found at the other ROIs. For the remelted HXLPE group, the articulating surface OI was observed to be greater than the OI for backside (Median difference = 0.04, p < 0.001), AP surface (Median difference = 0.05, p = 0.002), and stabilizing post (Median difference = 0.05, p < 0.001). Articulating surface OI was found to positively correlate with implantation time for both the VE HXLPE group (ρ= 0.477, p <0.001) and the remelted HXLPE group (ρ = 0.378, p = 0.002), though a similar correlation was not found at other ROIs (Figure 5). Additionally, no correlations were found between maximum oxidation index and age, BMI, weight, or UCLA score for either group, and no significant differences were observed based on reason for revision.
Figure 4.
Boxplots showing maximum oxidation index by area of interest for vitamin E-stabilized and HXLPE control inserts.
Figure 5.
Relationship between implantation time and maximum oxidation index at (left) articulating surface and (right) backside surface.
Discussion
Vitamin-E stabilization was clinically introduced to improve the oxidative stability, wear resistance, and mechanical properties of HXLPE in orthopaedic bearing surfaces. Although numerous studies have demonstrated the efficacy of this treatment in vitro, the in vivo results for vitamin E-stabilized HXLPE remain largely uninvestigated. In this retrieval study, the primary revision reasons, damage modes, and in vivo oxidation of 103 vitamin E-stabilized and 67 remelted HXLPE TKA inserts were assessed and compared.
The study had a number of limitations. First, the retrieved inserts were implanted for a relatively short amount of time, with a median implantation time of 1.2 years for the VE group. It is therefore unknown how the mechanisms studied may affect longer-term components. Though we were restricted in the amount of long-term retrieved vitamin E-stabilized inserts available, it should be noted that the inserts with relatively longer implantation times of three or more years still exhibited minimal amounts of oxidation. Second, only surface damage modes, not actual polyethylene wear, were studied. While semi-quantitative scoring of surface damage is a common tool in polyethylene retrieval analysis, damage scores may not always correlate with volumetric material loss. We are therefore unable to draw conclusions about implant wear. Also, surface damage was observed with the naked eye and stereomicroscope and not with scanning electron microscopy, which may further elucidate damage mechanisms [38]. Nevertheless, we achieved our goal of determining the presence and severity of surface damage mechanisms acting on vitamin E-stabilized TKA inserts in vivo, allowing for comparison with other polyethylene components. Finally, since the design comprising the control cohort is not available for vitamin E-stabilized HXLPE, each material corresponds to a different implant design. Since the design may affect the amount of damage and oxidation observed, we cannot attribute the differences between groups solely to the material type.
In this study, we found the primary reasons for revision to be instability, infection, and loosening. These results are consistent with other TKA retrieval studies, which often report aseptic loosening as the primary reason for revision and infection as the primary mode of early TKA failures [33, 39–42], and with the limited existing clinical findings specific to VE HXLPE [16, 28, 29]. Similarly, the primary observed damage modes, burnishing, pitting, and scratching, were consistent with previous reports for TKA HXLPE [33, 42]. For vitamin E-stabilized HXLPE specifically, the results of the present study also agree with the generally low damage scores reported by Rowell et al. and the burnishing damage reported by Schwiesau et al. [18, 28]. Of note, our VE cohort had no instances of delamination, a fatigue-related damage mode, similar to findings from Currier et al. [29]. This is consistent with results reported in two recent studies, which used a knee wear simulator and pin-on-plate testing to determine the delamination resistance of vitamin E-blended HXLPE [18, 19]. While Sakoda et al. demonstrated excellent delamination resistance, the related fatigue crack growth results were not consistent. Therefore, while the absence of delamination in the current study may point to improved fatigue strength of the vitamin E-stabilized inserts, more in-depth fatigue testing is warranted.
As expected, we detected a minimal amount of oxidation in our VE cohort. Previous in vitro studies have shown that vitamin E treatment significantly improves oxidative resistance in HXLPE, as many report low oxidation (OI < 1), with maximum indices often at or below 0.1 [7, 10–12, 18, 43]. Of note, an ASTM oxidation index less than 1 is generally considered below the threshold for degradation of mechanical and tribological properties. Early studies, which often utilized accelerated aging testing, consistently reported significantly lower oxidation for vitamin E-stabilized HXLPE compared to conventional, with little to no change in oxidation for the VE cohorts [13]. In a recent study, real-time aging of vitamin E-stabilized HXLPE blocks resulted in an average OI of 0.00 and maximum OI of 0.09 at 36 months [12]. Additionally, the authors report no increase in oxidation potential of the VE samples, suggesting long-term success of the VE treatment. Similar to these in vitro investigations, the current study reports minimal oxidation for the vitamin E-stabilized HXLPE inserts, with maximum OI values well below the threshold of clinical and mechanical significance.
In addition to in vitro studies, the present results also agree with the limited in vivo oxidation results available for comparison. Rowell et al., for example, investigated a cohort of short-term vitamin E-stabilized THA and TKA retrievals and reported minimal oxidation and little to no significant surface damage, along with evidence of successful free radical scavenging and oxidation cascade inhibition by the antioxidant [28]. The maximum oxidation indices reported for tibial inserts (median: 0.113, range: 0.108 – 0.130) are similar to that of the present study, though only three TKA retrievals were included in the Rowell et al. cohort. More recently, Currier et al. analyzed and compared antioxidant-stabilized, conventional, and HXLPE remelted tibial insert retrievals implanted for 0–3 years [29]. Similar to the current study, the authors reported low amounts of oxidation (median: 0.08, range: 0.06 – 0.13) for the antioxidant group and an overall correlation between oxidation index and implantation time. However, it should be noted that the cohort of 25 tibial inserts included UHMWPE treated with two different antioxidants (Vitamin E and PBHP), and the effect of antioxidant type is unknown. Ultimately, the present study as well as previous reports have shown oxidation of retrieved short-term vitamin E-stabilized implants to be minimal and currently not of clinical concern. Though we found oxidation values to be greater for the remelted HXLPE control group, the median differences were minimal and may not be clinically significant. It remains to be seen if these difference increase for longer-term retrievals.
In conclusion this retrieval study represents, to the authors’ knowledge, the largest investigation of in vivo behavior for vitamin E-stabilized TKA inserts. We report primary failure modes of instability, infection, and aseptic loosening and primary surface damage modes of burnishing, pitting, and scratching with no signs of fatigue-related damage. Oxidation for the VE cohort was minimal, with average indices well below the threshold for mechanical and tribological degradation. While the oxidation for the VE cohort tended to be less than the HXLPE controls at the articulating and backside surfaces, the actual differences were minimal and may not be clinically significant. Though the results for vitamin E-stabilized HXLPE are promising in the short term, analysis of long-term components may be of interest.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Oral E and Muratoglu OK, Vitamin E diffused, highly crosslinked UHMWPE: a review. Int Orthop, 2011. 35(2): p. 215–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kurtz SM, Gawel HA, and Patel JD, History and systematic review of wear and osteolysis outcomes for first-generation highly crosslinked polyethylene. Clin Orthop Relat Res, 2011. 469(8): p. 2262–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gigante A, Bottegoni C, Ragone V, Banci L. Effectiveness of vitamin-E-doped polyethylene in joint replacement: a literature review. J Funct Biomater 2015;6:889–900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bracco P, Bellare A, Bistolfi A, Affatato S. Ultra-high molecular weight polyethylene: influence of the chemical, physical and mechanical properties on the wear behavior. A Review. Materials (Basel) 2017;10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Oral E, Wannomae KK, Hawkins N, Harris WH, Muratoglu OK. Alpha-tocopherol-doped irradiated UHMWPE for high fatigue resistance and low wear. Biomaterials 2004;25:5515–5522. [DOI] [PubMed] [Google Scholar]
- 6.Oral E, Godleski Beckos C, Malhi AS, Muratoglu OK. The effects of high dose irradiation on the cross-linking of vitamin E-blended ultrahigh molecular weight polyethylene. Biomaterials 2008;29:3557–3560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kurtz SM, Dumbleton J, Siskey RS, Wang A, Manley M. Trace concentrations of vitamin E protect radiation crosslinked UHMWPE from oxidative degradation. J Biomed Mater Res A 2009;90:549–563. [DOI] [PubMed] [Google Scholar]
- 8.Grupp TM, Fritz B, Kutzner I, Schilling C, Bergmann G, Schwiesau J. Vitamin E stabilised polyethylene for total knee arthroplasty evaluated under highly demanding activities wear simulation. Acta Biomater 2017;48:415–422. [DOI] [PubMed] [Google Scholar]
- 9.Doshi B, Ward JS, Oral E, Muratoglu OK. Fatigue toughness of irradiated vitamin E/UHMWPE blends. J Orthop Res 2016;34:1514–1520. [DOI] [PubMed] [Google Scholar]
- 10.Oral E, Christensen SD, Malhi AS, Wannomae KK, Muratoglu OK. Wear resistance and mechanical properties of highly cross-linked, ultrahigh-molecular weight polyethylene doped with vitamin E. J Arthroplasty 2006;21:580–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haider H, Weisenburger JN, Kurtz SM, Rimnac CM, Freedman J, Schroeder DW, et al. Does vitamin E-stabilized ultrahigh-molecular-weight polyethylene address concerns of cross-linked polyethylene in total knee arthroplasty? J Arthroplasty 2012;27:461–469. [DOI] [PubMed] [Google Scholar]
- 12.Rowell SL, Oral E, and Muratoglu OK, Comparative oxidative stability of alpha-tocopherol blended and diffused UHMWPEs at 3 years of real-time aging. J Orthop Res, 2011. 29(5): p. 773–80. [DOI] [PubMed] [Google Scholar]
- 13.Turner A, Okubo Y, Teramura S, Niwa Y, Ibaraki K, Kawasaki T, et al. The antioxidant and nonantioxidant contributions of vitamin E in vitamin E blended ultra-high molecular weight polyethylene for total knee replacement. J Mech Behav Biomed Mater 2014;31:21–30. [DOI] [PubMed] [Google Scholar]
- 14.Galliera E, Ragone V, Marazzi MG, Selmin F, Banci L, Corsi Romanelli MM, et al. Vitamin Estabilized UHMWPE: biological response on human osteoblasts to wear debris. Clin Chim Acta 2018;486:18–25. [DOI] [PubMed] [Google Scholar]
- 15.Yamamoto K, Tateiwa T, and Takahashi Y, Vitamin E-stabilized highly crosslinked polyethylenes: The role and effectiveness in total hip arthroplasty. J Orthop Sci, 2017. 22(3): p. 384–390. [DOI] [PubMed] [Google Scholar]
- 16.Flament EM, Berend KR, Hurst JM, Morris MJ, Adams JB, Lombardi JA. Early experience with vitamin E antioxidant-infused highly cross-linked polyethylene inserts in primary total knee arthroplasty. Surg Technol Int 2016;29:334–340. [PubMed] [Google Scholar]
- 17.Sillesen NH, Greene ME, Nebergall AK, Huddleston JI, Emerson R, Gebuhr P, et al. 3-Year follow-up of a long-term registry-based multicentre study on vitamin E diffused polyethylene in total hip replacement. Hip Int 2016;26:97–103. [DOI] [PubMed] [Google Scholar]
- 18.Schwiesau J, Fritz B, Kutzner I, Bergmann G, Grupp TM. CR TKA UHMWPE wear tested after artificial aging of the vitamin E treated gliding component by simulating daily patient activities. Biomed Res Int 2014;2014:567374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sakoda H, Osaka Y, Uetsuki K, Okamoto Y, Haishima Y. Evaluating the durability of UHMWPE biomaterials used for articulating surfaces of joint arthroplasty using delamination tests. J Biomed Mater Res B Appl Biomater 2019;107(1):65–72. [DOI] [PubMed] [Google Scholar]
- 20.Grupp TM, Holderied M, Mulliez MA, Streller R, Jäger M, Blömer W, et al. Biotribology of a vitamin E-stabilized polyethylene for hip arthroplasty - influence of artificial ageing and thirdbody particles on wear. Acta Biomater 2014;10:3068–3078. [DOI] [PubMed] [Google Scholar]
- 21.Micheli BR, Wannomae KK, Lozynsky AJ, Christensen SD, Muratoglu OK. Knee simulator wear of vitamin E stabilized irradiated ultrahigh molecular weight polyethylene. J Arthroplasty 2012;27:95–104. [DOI] [PubMed] [Google Scholar]
- 22.Teramura S, Sakoda H, Terao T, Endo MM, Fujiwara K, Tomita N. Reduction of wear volume from ultrahigh molecular weight polyethylene knee components by the addition of vitamin E. J Orthop Res 2008;26:460–464. [DOI] [PubMed] [Google Scholar]
- 23.Vaidya C, Alvarez E, Vinciguerra J, Bruce DA, DesJardins JD. Reduction of total knee replacement wear with vitamin E blended highly cross-linked ultra-high molecular weight polyethylene. Proc Inst Mech Eng H 2011;225:1–7. [DOI] [PubMed] [Google Scholar]
- 24.Affatato S, Bracco P, Costa L, Villa T, Quaglini V, Toni A. In vitro wear performance of standard, crosslinked, and vitamin-E-blended UHMWPEIn vitro wear performance of standard, crosslinked, and vitamin-E-blended UHMWPE. J Biomed Mater Res A 2012;100:554–560. [DOI] [PubMed] [Google Scholar]
- 25.Takahashi Y, Tateiwa T, Pezzotti G, Shishido T, Masaoka T, Yamamoto K. Improved resistance to neck-liner impingement in second-generation highly crosslinked polyethylene-the role of vitamin E and crosslinks. J Arthroplasty 2016;31:2926–2932. [DOI] [PubMed] [Google Scholar]
- 26.Popoola OO, Kincaid BL, Mimnaugh K, Marqueling M. In vitro wear of ultrahigh-molecular-weight polyethylene and vitamin E blended highly cross-linked polyethylene in linked, semiconstrained total elbow replacement prostheses. J Shoulder Elbow Surg 2017;26:846–854. [DOI] [PubMed] [Google Scholar]
- 27.Salemyr M, Muren O, Ahl T, Bodén H, Chammout G, Stark A, et al. Vitamin-E diffused highly cross-linked polyethylene liner compared to standard liners in total hip arthroplasty. A randomized, controlled trial. Int Orthop 2015;39:1499–1505. [DOI] [PubMed] [Google Scholar]
- 28.Rowell SL and Muratoglu OK, Investigation of surgically retrieved, vitamin E-stabilized, crosslinked UHMWPE implants after short-term in vivo service. J Biomed Mater Res B Appl Biomater, 2016. 104(6): p. 1132–40. [DOI] [PubMed] [Google Scholar]
- 29.Currier BH, Currier JH, Holdcroft LA, Van Citters DW. Effectiveness of anti-oxidant polyethylene: what early retrievals can tell us. J Biomed Mater Res B Appl Biomater 2018;106(1):353–359. [DOI] [PubMed] [Google Scholar]
- 30.Nebergall AK, Greene ME, Laursen MB, Nielsen PT, Malchau H, Troelsen A. Vitamin E diffused highly cross-linked polyethylene in total hip arthroplasty at five years: a randomised controlled trial using radiostereometric analysis. Bone Joint J 2017;99–B:577–584. [DOI] [PubMed] [Google Scholar]
- 31.Scemama C, Anract P, Dumaine V, Babinet A, Courpied JP, Hamadouche M. Does vitamin E-blended polyethylene reduce wear in primary total hip arthroplasty: a blinded randomised clinical trial. Int Orthop 2017;41:1113–1118. [DOI] [PubMed] [Google Scholar]
- 32.Shareghi B, Johanson PE, and Karrholm J, Wear of Vitamin E-Infused Highly Cross-Linked Polyethylene at Five Years. J Bone Joint Surg Am, 2017. 99(17): p. 1447–1452. [DOI] [PubMed] [Google Scholar]
- 33.MacDonald DW, Higgs G, Parvizi J, Klein G, Hartzband M, Levine H, et al. Oxidative properties and surface damage mechanisms of remelted highly crosslinked polyethylenes in total knee arthroplasty. Int Orthop 2013;37:611–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kurtz SM, Hozack W, Turner J, Purtill J, MacDonald D, Sharkey P, et al. Mechanical properties of retrieved highly cross-linked crossfire liners after short-term implantation. J Arthroplasty 2005;20:840–849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.MacDonald D, Hanzlik J, Sharkey P, Parvizi J, Kurtz SM. In vivo oxidation and surface damage in retrieved ethylene oxide-sterilized total knee arthroplasties. Clin Orthop Relat Res 2012;470:1826–1833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hood RW, Wright TM, and Burstein AH, Retrieval analysis of total knee prostheses: a method and its application to 48 total condylar prostheses. J Biomed Mater Res, 1983. 17(5): p. 829–42. [DOI] [PubMed] [Google Scholar]
- 37.ASTM Standard F2102-17, Standard Guide for Evaluating the Extent of Oxidation in Polyethylene Fabricated Forms Intended for Surgical Implants, ASTM International: West Conshohocken, PA, 2017. [Google Scholar]
- 38.Utzschneider S, Harrasser N, Sadoghi P, Weber P, Schröder C, Pietschmann MF, et al. Crosslinked polyethylene in knee arthroplasty: a simulator study evaluating the positive influence on the tribocontact area in the fixed-bearing knee. Arch Orthop Trauma Surg 2010;130:1419–1424. [DOI] [PubMed] [Google Scholar]
- 39.Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today--has anything changed after 10 years? J Arthroplasty 2014;29:1774–1778. [DOI] [PubMed] [Google Scholar]
- 40.Dalury DF, Pomeroy DL, Gorab RS, Adams MJ. Why are total knee arthroplasties being revised? J Arthroplasty 2013;28(8 Suppl):120–121. [DOI] [PubMed] [Google Scholar]
- 41.Currier BH and Van Citters DW, A Novel Technique for Assessing Antioxidant Concentration in Retrieved UHMWPE. Clin Orthop Relat Res, 2017. 475(5): p. 1356–1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.MacDonald DW, Higgs GB, Chen AF, Malkani AL, Mont MA,Kurtz SM. Oxidation, damage mechanisms, and reasons for revision of sequentially annealed highly crosslinked polyethylene in total knee arthroplasty. J Arthroplasty 2018;33:1235–1241. [DOI] [PubMed] [Google Scholar]
- 43.Lerf R, Zurbrugg D, and Delfosse D, Use of vitamin E to protect cross-linked UHMWPE from oxidation. Biomaterials, 2010. 31(13): p. 3643–8. [DOI] [PubMed] [Google Scholar]