Abstract
Objectives The main objective of this article is to describe endoscopic management of intraoperative massive bleeding from jugular bulb injury during exclusively transcanal endoscopic procedures for middle ear pathologies.
Design Case series with chart review.
Setting Tertiary referral center.
Participants We retrospectively reviewed two patients who experienced jugular bulb injury during endoscopic transcanal approach for glomus tympanicum and chronic otitis media. The surgical videos and charts were carefully investigated and analyzed.
Main Outcome Measures Feasibility and suitability of exclusive endoscopic management of jugular bulb bleeding and description of surgical maneuvers that should be performed to obtain safe and effective hemostasis.
Results In both patients, jugular bulb bleeding was progressively controlled by means of exclusive endoscopic approach with no need to convert to microscopic approach. None of the cases required a second surgeon helping in keeping the endoscope during hemostatic maneuvers. Both patients had a normal postoperative period with no recurrence of hemorrhage.
Conclusions Endoscopic management of jugular bulb bleeding is feasible by using the technique described with reasonable efficacy and with no additional risk or morbidity to the procedure. Knowledge of anatomy and its variants, preoperative evaluation of imaging, and the ability of the surgeon to adapt the surgical technique to the specific case are recommended to prevent vascular complications during endoscopic ear surgery.
Keywords: endoscopic ear surgery, bleeding management, jugular bulb dehiscence, high-positioned JB
Introduction
Vascular injuries during otologic surgery are rare but may give rise to serious consequences. The jugular bulb (JB) and the petrous portion of internal carotid artery (ICA) lie within millimeters with respect to the tympanic cavity and may inadvertently be injured while performing surgical maneuvers. Various anatomical variants of both the petrous ICA and the JB have been reported. They may concern position and course of the vessels (high riding JB; lateralized or aberrant ICA) or their bony covering (dehiscent JB and ICA). 1 Massive inflammation (e.g., massive cholesteatoma of the middle ear) of the middle ear cleft might also lead to accidental damage to these vascular structures. Indeed, this situation can cause the erosion of the hypotympanic bone and the consequent dehiscence of these vessels. Transcanal endoscopic ear surgery (TEES) has already been demonstrated to be a valuable surgical option and its indications have progressively widened. However, an instructive description of vascular injuries during endoscopic ear surgery and their management is still lacking in the literature. We aim to describe our experience in the management of JB injuries during TEES.
Methods
This is a retrospective descriptive study that involved two patients that underwent surgery between 2013 and 2017 for otologic disease and experienced an intraoperative lesion to the JB. Preoperative assessment consisted of general ENT evaluation, audiometric tests, and imaging (e.g., high-resolution computed tomography [HRCT] and/or magnetic resonance imaging). Surgical videos were reviewed by present authors. All the data were summarized in a dedicated chart.
Results
Standard Transcanal Endoscopic Surgical Procedure
The external auditory canal (EAC) is cleaned up and the tympanic membrane is visualized by means of a 0° degree 3-mm outer diameter 15 cm length endoscope (Karl Storz, Tuttlingen, Germany). The incision is made clockwise from 6 o'clock to the 12 o'clock, 1.0 cm from the tympanic membrane using a round knife. The tympanomeatal flap is elevated using a microdissector, applying traction with the cottonoids on the bone of the EAC. The flap is elevated anteriorly until the fibrous annulus is identified. An underlay dissection of the annulus is performed in order to access the middle ear cavity, and then the relationship between the pathologic tissue and the ossicular chain, facial nerve and vascular structures of the middle ear are determined. The pathology is gently removed and the completeness of its removal is carefully assessed before the repositioning of the tympanomeatal flap. If needed, an ossiculoplasty and/or a myringoplasty is performed. Once the flap is back at its previous position, the EAC is packed with Gelfoam soaked with saline solution.
Case Series
Patient 1 was 68 years old female with no major comorbidities that underwent TEES to remove a glomus tympanicum, type A2 (modified Fisch-Mattox Classification), 2 and experienced a massive bleeding coming from the JB due to an injury provoked by cauterization and drilling of the vascular pedicle of the tumor, coming from the Jacobson nerve area. 3
Patient 2 was a 71 years old female with no major comorbidities that underwent TEES for chronic otitis media and experienced massive bleeding from the JB due to an accidental injury caused during the elevation of the tympanomeatal flap.
Both patients underwent HRCT of the petrous bone showing a high-positioned JB, of which one was even dehiscent.
In both patients, massive bleeding coming from an injured area on the JB occurred during the procedure, blinding all the surgical field. This situation was initially managed by using suction, cottonoids soaked with epinephrine (1:1000) and Tabotamp (Ethicon, Neuchatel, Switzerland) or Spongostan (Ethicon, Neuchatel, Switzerland), applying manual compression on the vessel. In such cases, bigger suction tubes might be used to obtain a faster identification of the injured area on the JB. Once the major bleeding was reduced, the surgical field was progressively enlarged by completing the elevation of the tympanomeatal flap, detaching it from the handle of the malleus. Then, an atticotomy was performed to improve the identification of the vascular structures and the other anatomic landmarks (e.g., facial nerve, ossicular chain), to better the clarity of the surgical space, which could be also reduced by the presence of blood clots, and to obtain a wider space of work.
Once the bleeding was controlled and the surgical field was stabilized, surgery could restart performing careful dissection of the pathology avoiding the removal of the hemostatic material from the hypotympanic region ( Fig. 1 ).
Fig. 1.
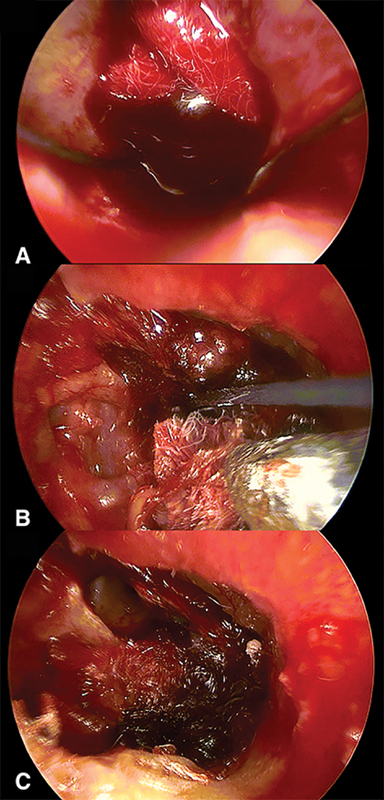
Panel A : Massive bleeding from a vascular injury on the jugular bulb (JB); Panel B : Mechanic compression by suction and cottonoids soaked with epinephrine (1:1000) on the injured area of JB; Panel C : Hemostatic plugging with Tabotamp and Spongostan.
None of the cases required a second surgeon helping in keeping the endoscope during hemostatic maneuvers. Duration of surgical procedures was 165 minutes in the first case and 135 in the second. Patient 2 was transferred to intensive care unit after surgery to allow a gradual awakening after general anesthesia. Both patients had a normal postoperative period with no recurrence of hemorrhage from the JB and were discharged after 4 days with good general condition. During a mean follow-up period of 3.2 years, both patients did not experience any late complications.
Discussion
The ICA and the JB, two of the main head and neck vascular structures, lie adjacent to the tympanic cavity. These vessels are normally contained in a complete bony canal which is surrounded by a variable amount of pneumatized bone. Nevertheless, a certain variability of these structures exists and may lead to ICA and JB iatrogenic injuries. These vascular structures might also be exposed and jeopardized in presence of middle ear pathologies, such as cholesteatoma, and in previously operated ears. 3 A variable anatomy of the JB is not rare, even if the frequency of high JB varies between 6 and 34% in dependence on investigation method and definitions. 4 More rarely, a jugular diverticulum can be found. 1 Otomicroscopic/otoendoscopic evaluation and temporal bones HRCT usually allow preoperative identification of patients at risk of JB injury ( Fig. 2 ).
Fig. 2.
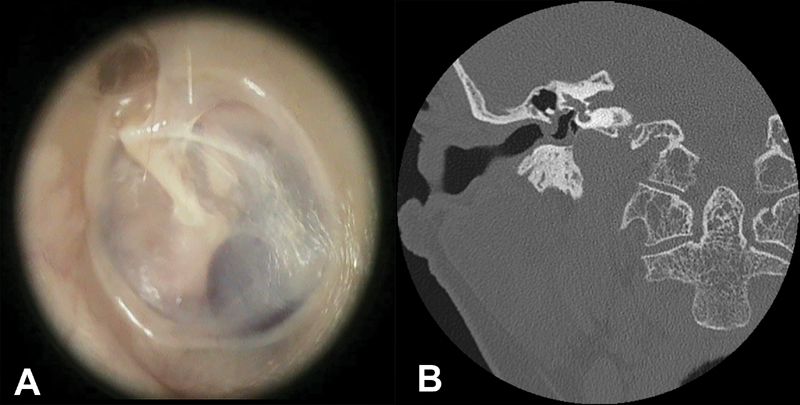
Panel A : Left ear. Endoscopic view. A high positioned and dehiscent jugular bulb in contact with the tympanic membrane at the posteroinferior quadrant of the middle ear cavity; Panel B : Computed tomography scan. Coronal view. Right side. Presence of high positioned and dehiscent jugular bulb partially covering the round window niche.
However, surgeons should be aware that vascular anomalies could be an unanticipated intraoperative finding. When the disease (cholesteatoma or massive mucosal hypertrophy) encroaches an exposed ICA or JB, or if revision surgery has to be performed after the previous iatrogenic vascular injury, surgery should be conducted after appropriate imaging study. Thus, maneuvers in the hypotympanum and protympanum should be preferentially performed with extreme caution. The JB may be damaged during myringocentesis, tympanomeatal flap elevation, and removal of disease in hypotympanic and protympanic areas. 5 Surgical maneuvers in the regions at risk for vessel injury should be performed as last steps, after disease clearing, cavity regularization, and hemostasis. Dissection should be performed bluntly, using cottonoids soaked with epinephrine and in a medial to lateral way, avoiding pulling mucosal tissue. Moreover, in case of a vascular anomalies, some authors advocate for open mastoidectomy techniques to obtain a large surgical field to easily identify all the surgical landmarks. 5 TEES is gaining popularity almost in every field of otologic surgery, including pediatrics and lateral skull base. 6 7 8 The main advantage is the enhanced visibility of the anatomy and pathology due to wide-angled view and the capability to look around the corner which permits to explore hidden recesses, such as the retro- and hypotympanum. 9 Nevertheless, the one-handed technique can be challenging for the surgeon and bleeding is a major concern. For this reason, powered instruments that allow both suction and dissection simultaneously might be used in case of need (i.e., surgery for glomus tympanicum). Due to the limited space in the EAC and tympanic cavity, a clean surgical field is required to benefit from the endoscopic vision. Thus, the knowledge of different procedures to ensure the hemostasis is very important. Anschuetz et al published a description of their experience in the management of regular bleeding during TEES, but description of massive bleeding due to vascular injuries to JB has never been described. 10
Our experience shows that even massive bleeding coming from JB injuries can be managed by means of an exclusive endoscopic approach. As previously described in the results subheading, specific surgical maneuvers should be performed to progressively reduce the bleeding and, if possible, complete the surgical intervention ( Table 1 ).
Table 1. Endoscopic management of jugular bulb bleeding.
| Adrenalized cottonoid on to the vascular injury |
| Suction on to the cottonoid and mechanic compression |
| Enlargement of the surgical field (+/− three hand technique) |
| Oxidized cellulose and/or gelatin absorbable sponge placement on to the jugular bulb injured area |
| Completion of surgical procedure (if possible) avoiding the removal of the hypotympanic packing |
In fact, similarly to what is frequently done during microscopic procedures, a bleeding coming from dural venous sinuses is usually controlled by plugging the vascular lesion with cottonoids and hemostatic agents, whereas vascular suture is intended for bigger defects.
Moreover, during these steps, a second surgeon could help by holding the suction onto a cottonoid to clean the surgical field and let the first surgeon to complete his maneuvers (three hand technique), especially when the anatomic conformation of the EAC is favorable or after a canalplasty.
Nevertheless, only experienced surgeons could deal with this kind of complication because it is wise to have thorough knowledge of middle ear endoscopic anatomy and to be extremely precise to avoid injuring important anatomic structures, such as the ossicular chain, the facial nerve, and the cochlea. Thus, a long learning curve is required to manage middle ear disease by means of exclusively endoscopic approach and appropriate training models have been proposed to facilitate that process. 11 However, in case of trouble, intraoperative bleeding from the JB can be stopped by packing the middle ear cavity and closing the sigmoid sinus and the jugular vein, if an adequate contralateral circulation is present. 5 Indeed, an adequate knowledge of traditional microscopic procedures is mandatory for every otologic surgeon. Limitations of the present study are its retrospective design and the small size of the group of patients. Nevertheless, since the present authors have a wide experience in dealing with middle ear diseases endoscopically, the small number of patients with major vascular complications might also be considered as an indirect proof of the safety of endoscopic ear surgery in terms of vascular injury prevention, probably thanks to an enhanced visualization of anatomic structures.
Conclusion
Knowledge of anatomy and its variants, preoperative evaluation of imaging, and the ability of the surgeon to adapt the surgical technique to the specific case are the basis for the prevention of vascular complications. Endoscopic management of JB bleeding is feasible by using the technique described with reasonable efficacy and with no additional risk or morbidity to the procedure.
Funding Statement
Funding Disclosures No funding is reported for the present study.
Footnotes
Conflict of Interest The authors declare no conflict of interest.
References
- 1.Koesling S, Kunkel P, Schul T. Vascular anomalies, sutures and small canals of the temporal bone on axial CT. Eur J Radiol. 2005;54(03):335–343. doi: 10.1016/j.ejrad.2004.09.003. [DOI] [PubMed] [Google Scholar]
- 2.Sanna M, Fois P, Pasanisi E, Russo A, Bacciu A. Middle ear and mastoid glomus tumors (glomus tympanicum): an algorithm for the surgical management. Auris Nasus Larynx. 2010;37(06):661–668. doi: 10.1016/j.anl.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 3.Welling D B, Glasscock M E, III, Tarasidis N. Management of carotid artery hemorrhage in middle ear surgery. Otolaryngol Head Neck Surg. 1993;109(06):996–999. doi: 10.1177/019459989310900604. [DOI] [PubMed] [Google Scholar]
- 4.Atmaca S, Elmali M, Kucuk H. High and dehiscent jugular bulb: clear and present danger during middle ear surgery. Surg Radiol Anat. 2014;36(04):369–374. doi: 10.1007/s00276-013-1196-z. [DOI] [PubMed] [Google Scholar]
- 5.Di Lella F, Falcioni M, Piccinini S et al. Prevention and management of vascular complications in middle ear and cochlear implant surgery. Eur Arch Otorhinolaryngol. 2017;274(11):3883–3892. doi: 10.1007/s00405-017-4747-9. [DOI] [PubMed] [Google Scholar]
- 6.Marchioni D, Soloperto D, Rubini A et al. Endoscopic exclusive transcanal approach to the tympanic cavity cholesteatoma in pediatric patients: our experience. Int J Pediatr Otorhinolaryngol. 2015;79(03):316–322. doi: 10.1016/j.ijporl.2014.12.008. [DOI] [PubMed] [Google Scholar]
- 7.Presutti L, Marchioni D, Mattioli F, Villari D, Alicandri-Ciufelli M. Endoscopic management of acquired cholesteatoma: our experience. J Otolaryngol - Head Neck Surg. 2008;37:481–487. [PubMed] [Google Scholar]
- 8.Marchioni D, Alicandri-Ciufelli M, Rubini A, Presutti L. Endoscopic transcanal corridors to the lateral skull base: initial experiences. Laryngoscope. 2015;125 05:S1–S13. doi: 10.1002/lary.25203. [DOI] [PubMed] [Google Scholar]
- 9.Bonali M, Anschuetz L, Fermi M et al. The variants of the retro- and hypotympanum: an endoscopic anatomical study. Eur Arch Otorhinolaryngol. 2017;274(05):2141–2148. doi: 10.1007/s00405-017-4492-0. [DOI] [PubMed] [Google Scholar]
- 10.Anschuetz L, Bonali M, Guarino P et al. Management of bleeding in exclusive endoscopic ear surgery: pilot clinical experience. Otolaryngol Head Neck Surg. 2017;157(04):700–706. doi: 10.1177/0194599817726982. [DOI] [PubMed] [Google Scholar]
- 11.Anschuetz L, Bonali M, Ghirelli M et al. An ovine model for exclusive endoscopic ear surgery. JAMA Otolaryngol Head Neck Surg. 2017;143(03):247–252. doi: 10.1001/jamaoto.2016.3315. [DOI] [PubMed] [Google Scholar]


